Role of Placental Transfusion to Reduce Complications of


- Slides: 20
Role of Placental Transfusion to Reduce Complications of Prematurity A Multi-site Quality Improvement Project Sponsored by the Indiana State Department of Health Presenter: Sandra Hoesli, MD, MS
Objectives • Describe the Indiana Vermont Oxford Network Quality Collaborative (IVON QC). • Share the successful outcome of a previous IVON QC project that lead to funding for the current placental transfusion project. • Define the goals of the placental transfusion for preterm infants project and its current progress.
IVON QC: The Creation of a Quality Collaborative for Indiana • Organized in 2009 as an outgrowth of a statewide NICU medical directors network • Vision of becoming a robust state collaborative of Indiana’s perinatal care providers • Work together on QI projects to improve pregnancy outcomes and reduce infant mortality in Indiana by disseminating evidence-based clinical practices and processes • First project in 2011 aimed to increase human milk use in preterm infants demonstrated the ability of NICUs in Indiana to collaborate on a single quality improvement project

Example State Perinatal Quality Improvement Collaboratives

State Perinatal Quality Collaboratives http: //www. cdc. gov/reproductivehealth/Maternal. Infant. Health/PQC-States. html
Example Quality Improvement Projects by State Collaboratives • Neonatal – Central line associated infection prevention – Health care associated infection prevention – Breast milk promotion – Delivery room management for preterm infants – Care and management of late preterm infants – Neonatal abstinence syndrome – Promotion of safe sleep practices
Example Quality Improvement Projects by State Collaboratives • Maternal – Reduce elective delivery before 39 weeks gestation – Maternal mortality – Promote antenatal corticosteroids – Reduce postpartum hemorrhage – Cardiovascular disease during pregnancy – Preeclampsia toolkits
Promoting Human Milk to Reduce Necrotizing Enterocolitis in Preterm Infants • First IVON QC project aimed to increase human milk use in preterm infants admitted to participating NICUs – 12 sites included – Primary goals were to work on a common project, use quality improvement methods, and share data on breast milk use between sites – Secondary goal was to reduce the aggregate NEC rate in infants <1500 grams admitted to participating Indiana NICUs that reported to Vermont Oxford Network (VON)
Promoting Human Milk to Reduce Necrotizing Enterocolitis in Preterm Infants • Outcomes – Initiation of a NICU collaboration focused on a single QI project – Developed infrastructure for performing multi-site QI projects – Reduction in aggregate rate of NEC for participating NICUs from 8% in 2010 (n=652) to 3. 9% in 2011 -2012 (n=1272) – Reduction in aggregate rate of surgical NEC from 2. 9% to 1. 6%
Promoting Human Milk to Reduce Necrotizing Enterocolitis in Preterm Infants • Outcomes – Trend of increased survival from 81. 5% to 84. 3% during the IVON QC project • Likely associated with emphasis on human milk, a reduction in the incidence of NEC and other unmeasured factors – This reduction in mortality could translate to 23 more infants surviving extreme prematurity each year in Indiana.
Placental Transfusion in Preterm Infants Born Less than 34 weeks of Gestation…Role of Delayed Cord Clamping and Umbilical Cord Milking to Reduce Complications of Prematurity Multi-Site IVON QC Project Sponsored by the Indiana State Department of Health William Engle, MD Frank Schubert, MD Kenneth Herman, MD Sandra Hoesli, MD
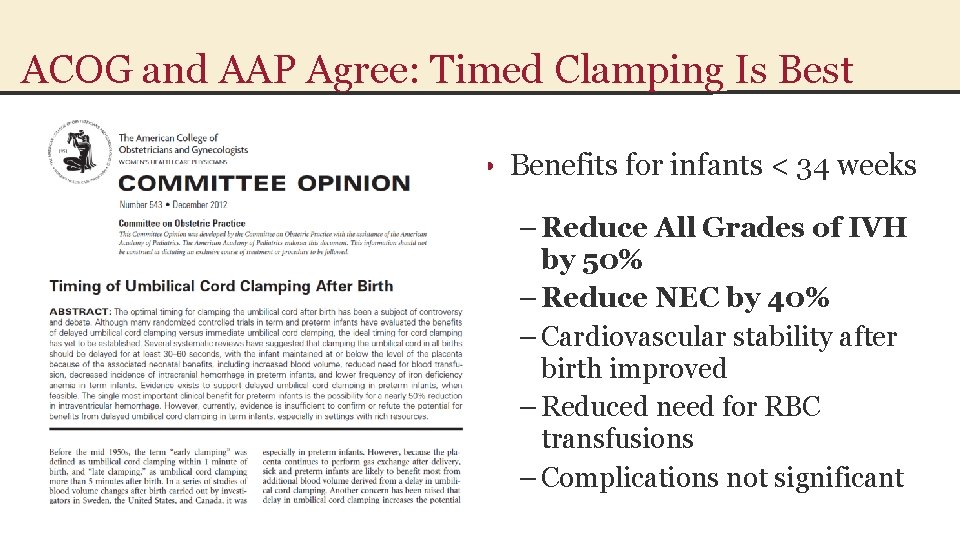
ACOG and AAP Agree: Timed Clamping Is Best • Benefits for infants < 34 weeks – Reduce All Grades of IVH by 50% – Reduce NEC by 40% – Cardiovascular stability after birth improved – Reduced need for RBC transfusions – Complications not significant
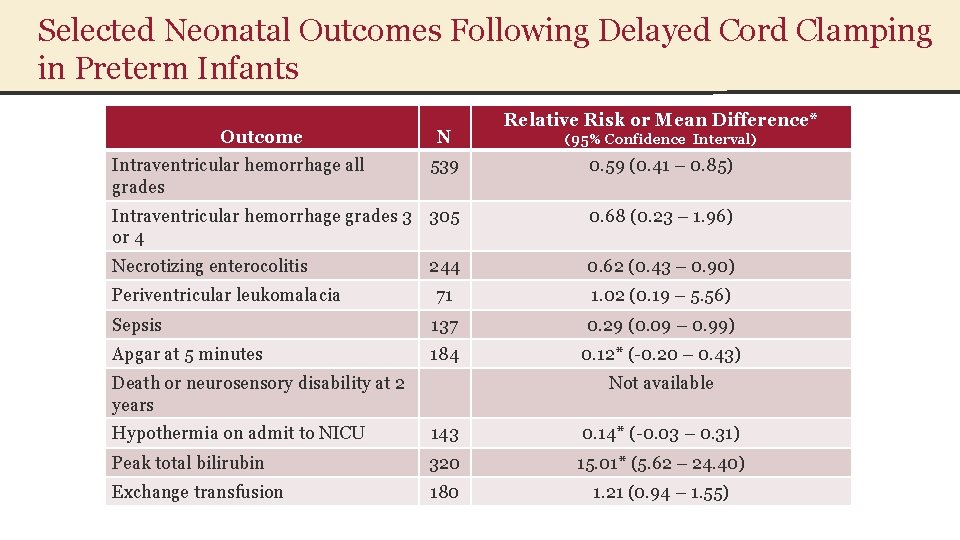
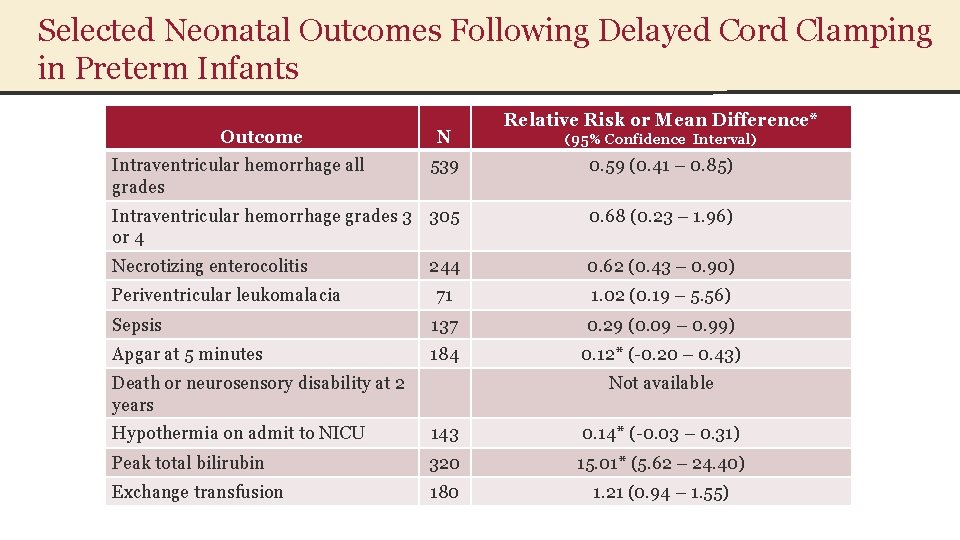
Selected Neonatal Outcomes Following Delayed Cord Clamping in Preterm Infants Outcome Intraventricular hemorrhage all grades N Relative Risk or Mean Difference* (95% Confidence Interval) 539 0. 59 (0. 41 – 0. 85) Intraventricular hemorrhage grades 3 305 or 4 0. 68 (0. 23 – 1. 96) Necrotizing enterocolitis 244 0. 62 (0. 43 – 0. 90) Periventricular leukomalacia 71 1. 02 (0. 19 – 5. 56) Sepsis 137 0. 29 (0. 09 – 0. 99) Apgar at 5 minutes 184 0. 12* (-0. 20 – 0. 43) Death or neurosensory disability at 2 years Not available Hypothermia on admit to NICU 143 0. 14* (-0. 03 – 0. 31) Peak total bilirubin 320 15. 01* (5. 62 – 24. 40) Exchange transfusion 180 1. 21 (0. 94 – 1. 55)
IVON QC Placental Transfusion QI Project • Purpose: Disseminate the practice of placental transfusion at the time of birth of premature infants throughout the 9 participating hospitals. – These hospitals care for over half of infants born less than 34 weeks gestation in Indiana – Statistical estimates calculate that as many of 15 neonatal deaths in this group of preterm infants will be prevented by implementing delayed cord clamping – Additionally, reducing NEC and IVH will reduce important morbidities and healthcare costs
IVON QC Placental Transfusion QI Project • Target: Gestational Age less 34 weeks gestation • Absence of Contraindications • placental abruption/severe vaginal bleeding/vasaprevia/uterine rupture • tight true knot in umbilical cord/tight nuchal cord • suspected twin-twin transfusion syndrome (monochorionic-mono amniotic and monochorionic-diamniotic twins) • maternal resuscitation at delivery/perimortem circumstances • neonate who is a non-resuscitation candidate • clinician preference—if OB has any questions may wish to discuss with Neonatology • other conditions with blood volume overload (eg: hydrops, heart failure)
IVON QC Placental Transfusion QI Project • Protocol – Hold baby supine, below the level of the placenta for 30 -60 seconds • 60 seconds for infants <27 weeks • 30 seconds for infants 28 -33 weeks – Cord milking should be reserved for when expedited delivery is necessary • Less supporting data available from clinical studies • Approximately 20 cm of cord is milked toward the infant 4 times over 15 -20 seconds – The baby is dried and stimulated during placental transfusion – Continue resuscitation per NRP guidelines
IVON QC Placental Transfusion QI Project • Quality Improvement Metrics to be collected – Percent of infants without contraindications receiving placental transfusion – Percent of infants with contraindications who received placental transfusion – Infants <30 weeks gestation or <1500 grams • • IVH all stages IVH grades 3 or 4 PVL NEC Sepsis Death Exchange transfusion
IVON QC Placental Transfusion QI Project • Progress to date – All centers have completed education regarding placental transfusion to OB and NICU teams – All centers have begun implementing changes to achieve delayed cord clamping for preterm infants as of October 1, 2014 – Data from centers is being entered into centralized REDCap data base – Report cards being sent to each site with progress report – Working on consistent documentation at all sites
Key Points to Remember • The goal of this QI project is to implement the recommended practice of delayed cord clamping for infants born less than 34 wk gestation • Delayed cord clamping has significant benefits for preterm infants: – 50% reduction in intraventricular hemorrhage – 40% reduction in necrotizing enterocolitis – Improved cardiovascular stability for the first 48 hours postnatally – Reduced risk of late onset sepsis – Reduced need for PRBC transfusion • No clinically significant risk to preterm infants identified • Cord milking for preterm infants should be reserved for situations when delayed cord clamping cannot be achieved and the OB/NICU team feels the baby would benefit from placental transfusion
Selected References • ACOG Committee Opinion Number 543. Timing of umbilical cord clamping after birth. Obstet Gynecol 2012; 120(6): 1522 -1526 • Aladangady N, Mc. Hugh S, Aitchison TC, Wardrop CAJ and Holland BM. Infants’ blood volume in a controlled trial of placental transfusion at preterm delivery. Pediatrics 2006; 117: 93 -98 • Bauer K, Brace RA, Stonestreet BS. Fluid distribution in the fetus and neonate. In Polin RA, Fox WW, Abman SH (eds) Fetal and Neonatal Physiology 4 th edition 2011 Elsevier Philadelphia, PA: 1436 -150 ? year • Dock DS, Kraus WL, Mc. Guire LB, Hyland JW, Haynes FW, Dexter L. The pulmonary blood volume in man. J Clin Invest 1961; 40(2): 317 -328 • Hutton EK, Hassan ES. Late vs early clamping of the umbilical cord in full-term neonates. Systematic review and meta-analysis of controlled trials. JAMA 2007; 297: 1241 -1252 • Kakkilaya V, Pramanik AK, Ibrahim H, Hussein S. Effect of placental transfusion on the blood volume and clinical outcome of infants born by cesarean section. Clin Perinatol 2008; 35: 561 -570 • Rabe H et al. Cochrane Database of Systematic Reviews 2012 Issue 8 Art Nl. CD 003248 doi: 10. 1002/14651858. CD 003248. pub 3. • Rabe H, Jewison A, Alvarez RF, Crook D, Stilton D, Bradley R, Holden D; Brighton Perinatal Study Group. Milking compared with delayed cord clamping to increase placental transfusion in preterm neonates: a randomized controlled trial. Obstet Gynecol. 2011 Feb; 117(2 Pt 1): 205 -11. • Raju TNK. Optimal timing for clamping of the umbilical cord after birth. Clin Perinatol 2012; 39 (4): 889 -900 • Raju TNK. Timing of umbilical cord clamping after birth for optimizing placental transfusion. Curr Opin Pediatr 2013; 25: 180 -187 • Weeks A. Umbilical cord clamping after birth. Better not to rush. MJ 2007; 335: 312 -313 • Yao AC, Hirvensalo M, Lind J. Placental transfusion rate and uterine contraction. Lancet 1968; 1: 380 -383 • Yao AC, Lind J. Effect of gravity of placental transfusion. The Lancet 1969; September; 505 -508