Role of androgen therapy in women with urinary

- Slides: 29
Role of androgen therapy in women with urinary incontinence Leor T Arbel, MS 4 USF Urology AI
Introduction Background/Review Current Standards of Treatment Outline Androgen Therapy Limitations Conclusions References Questions
Transdermal testosterone effective in augmenting tx of hypoactive sexual desire in surgically postmenopausal women Recent study found significant association between low testosterone level & Stress and Mixed Urinary Incontinence (AUA 2017) Introduction Women in lowest quartile of testosterone level had ↑ odds of Stress & Mixed Urinary Incontinence (48% and 65% increase, respectively) No association between testosterone levels and urge incontinence Mechanism of stress/mixed incontinence relates to pelvic floor muscle integrity; urge incontinence results from detrusor instability Androgens → anabolic effect on skeletal muscle Could testosterone also provide a benefit in the treatment of female pts with stress (or mixed) incontinence?
Background: Significance Urinary Incontinence (UI) is a major health concern: Substantial direct/indirect costs: Estimated $19. 5 billion in U. S. (2000), 75% of which was for mgmt of female pts Prevalence: 26 -61% in community dwelling women, 40 -77% in residents of nursing homes Impact on health-related Qo. L: Comparable to other major chronic conditions eg COPD, osteoporosis, stroke Caregiver burden: 6 -10% of nursing home admissions in the US are due to UI
UI = Involuntary loss of urine Background: UI Review Stress Urinary Incontinence (SUI): UI a/w ↑ abdominal pressure (eg with effort, physical exertion, sneezing, laughing or coughing) Sphincter dysfunction Urgency Urinary Incontinence (UUI): UI a/w strong or sudden urge to void Bladder dysfunction Mixed Urinary Incontinence: Both SUI and UUI features Sphincter & Bladder dysfunction
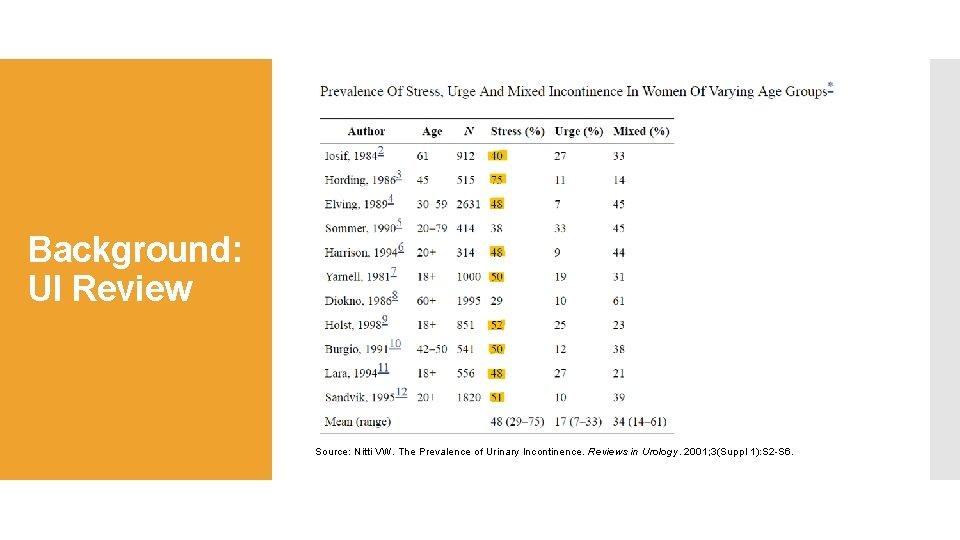
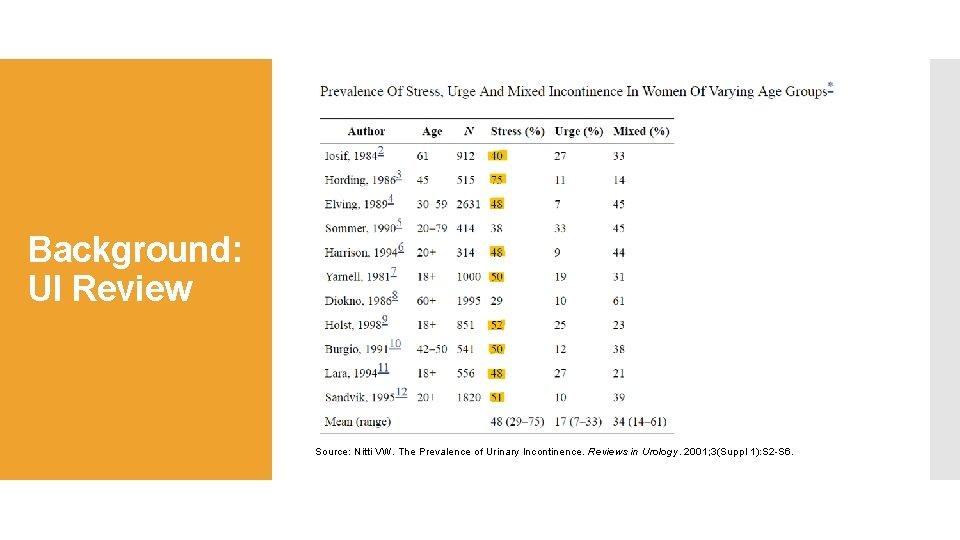
Background: UI Review Source: Nitti VW. The Prevalence of Urinary Incontinence. Reviews in Urology. 2001; 3(Suppl 1): S 2 -S 6.
Epidemiology: F > M (3: 1) ~50% of all women will experience SUI in their lifetime Risk Factors: ↑ age, obesity, white race, parity Background: SUI Review Etiology: Women: Weakness of pelvic floor muscles/ligaments → poor support of vesicourethral sphincteric unit Mechanisms: Urethral hypermobility: Insufficient pelvic floor support → When intraabdominal pressure (eg cough or sneeze) ↑, muscular tube of urethra fails to close Like “stepping on a hose in sand” Intrinsic sphincteric deficiency: Loss of urethral tone Workup: GU/Rectal Exam, Cough test, Labs, PVR, Voiding Diary, Questionnaires, Urodynamics (not for uncomplicated UI), U/A to rule out UTI
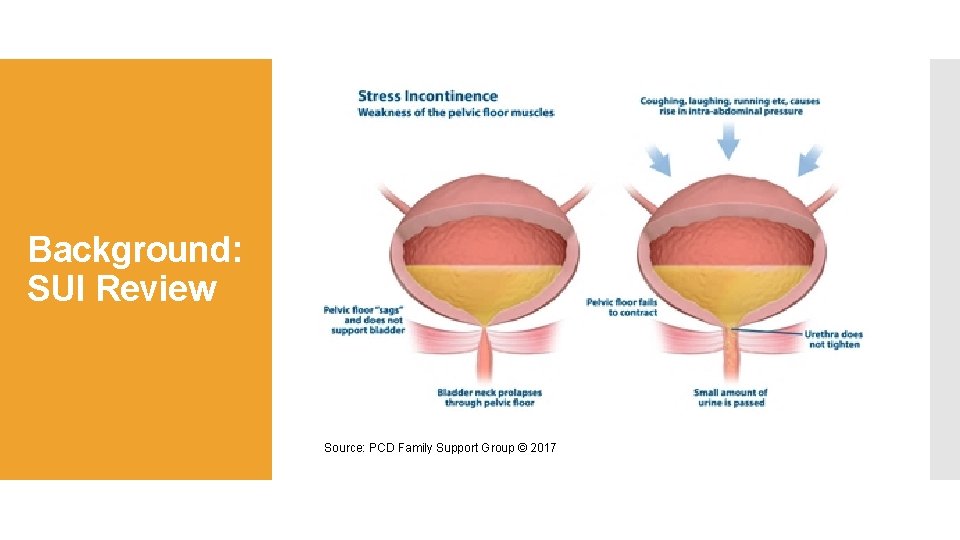
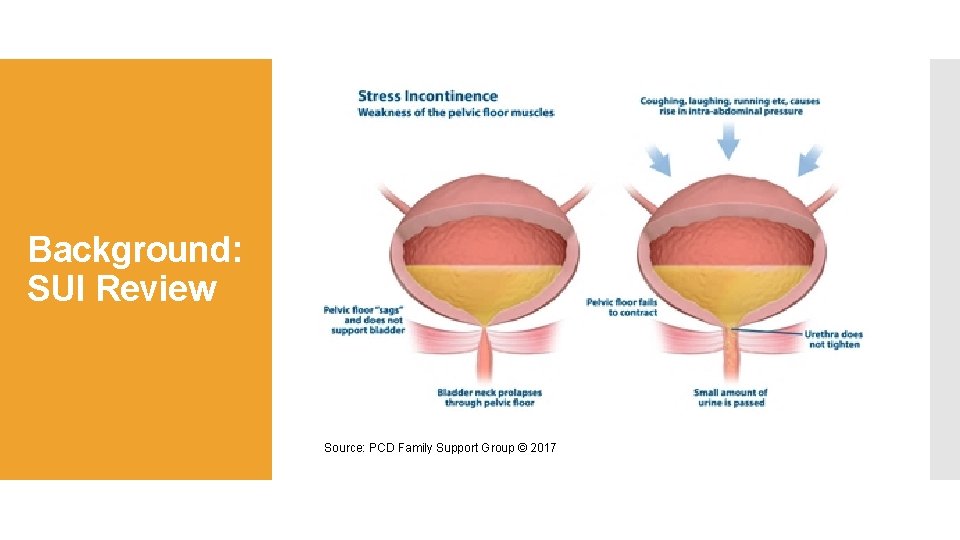
Background: SUI Review Source: PCD Family Support Group © 2017
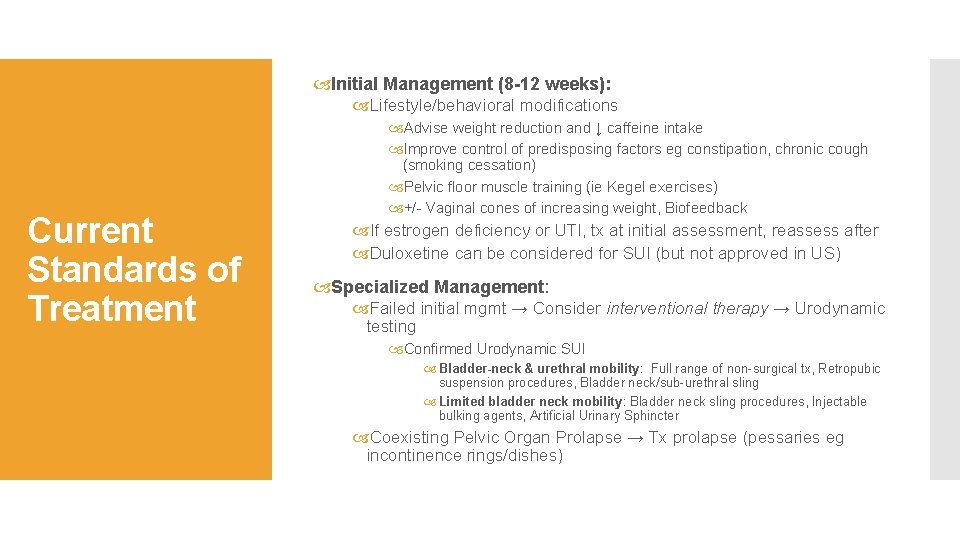
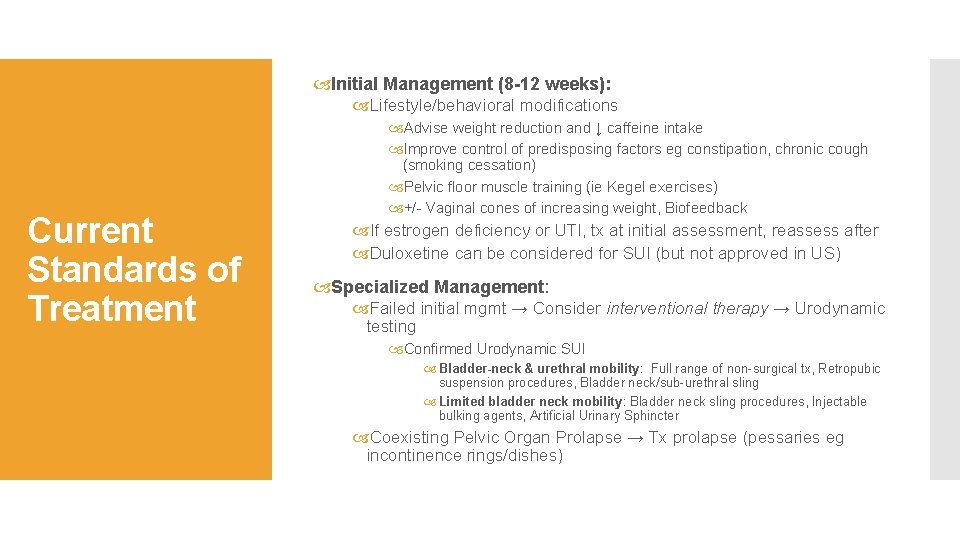
Initial Management (8 -12 weeks): Lifestyle/behavioral modifications Current Standards of Treatment Advise weight reduction and ↓ caffeine intake Improve control of predisposing factors eg constipation, chronic cough (smoking cessation) Pelvic floor muscle training (ie Kegel exercises) +/- Vaginal cones of increasing weight, Biofeedback If estrogen deficiency or UTI, tx at initial assessment, reassess after Duloxetine can be considered for SUI (but not approved in US) Specialized Management: Failed initial mgmt → Consider interventional therapy → Urodynamic testing Confirmed Urodynamic SUI Bladder-neck & urethral mobility: Full range of non-surgical tx, Retropubic suspension procedures, Bladder neck/sub-urethral sling Limited bladder neck mobility: Bladder neck sling procedures, Injectable bulking agents, Artificial Urinary Sphincter Coexisting Pelvic Organ Prolapse → Tx prolapse (pessaries eg incontinence rings/dishes)
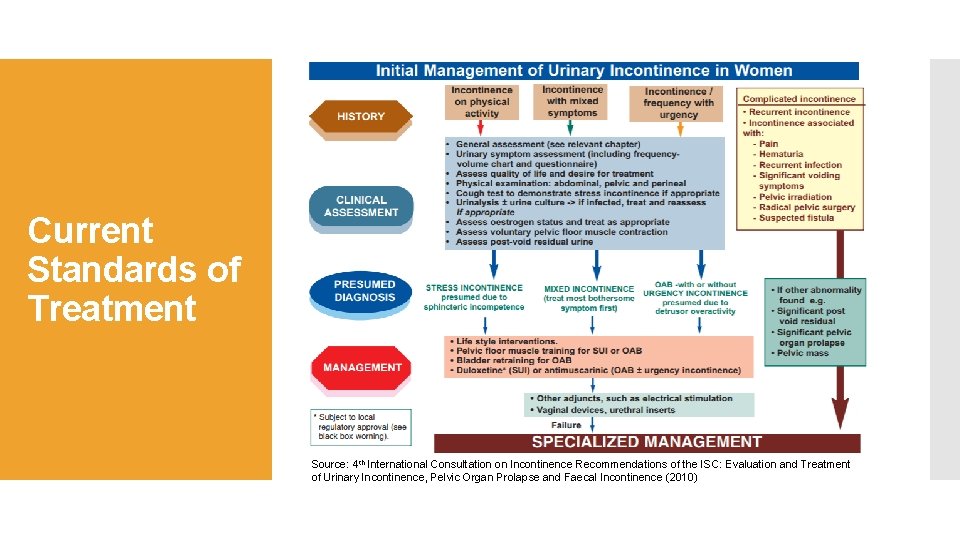
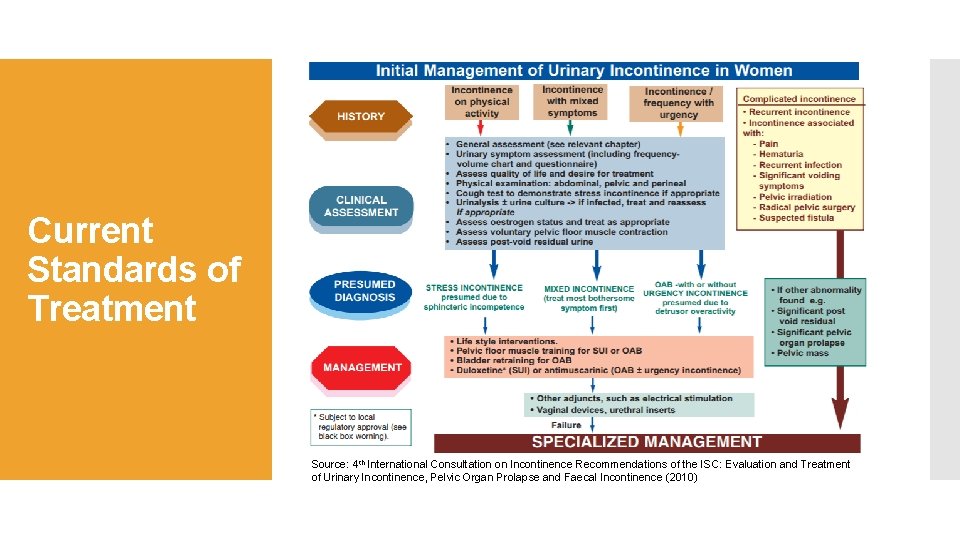
Current Standards of Treatment Source: 4 th International Consultation on Incontinence Recommendations of the ISC: Evaluation and Treatment of Urinary Incontinence, Pelvic Organ Prolapse and Faecal Incontinence (2010)
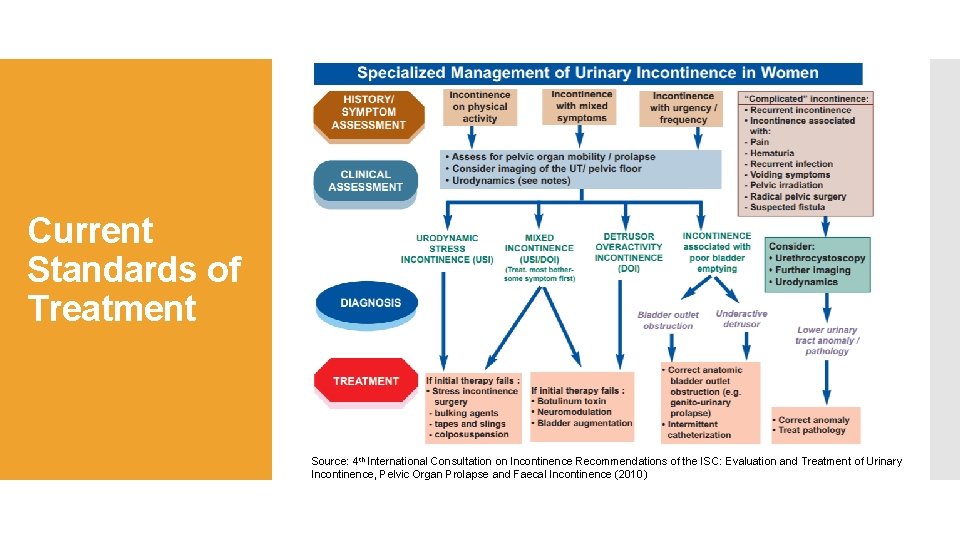
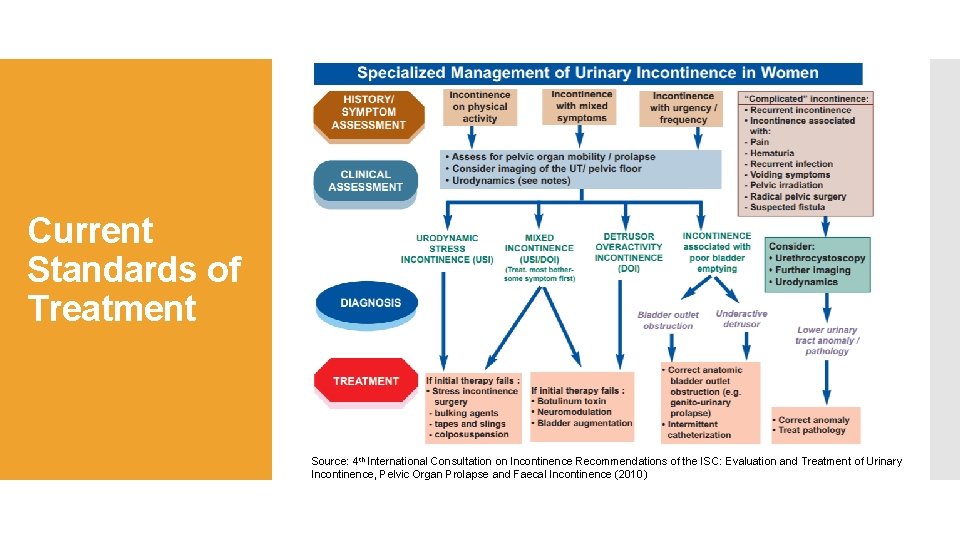
Current Standards of Treatment Source: 4 th International Consultation on Incontinence Recommendations of the ISC: Evaluation and Treatment of Urinary Incontinence, Pelvic Organ Prolapse and Faecal Incontinence (2010)
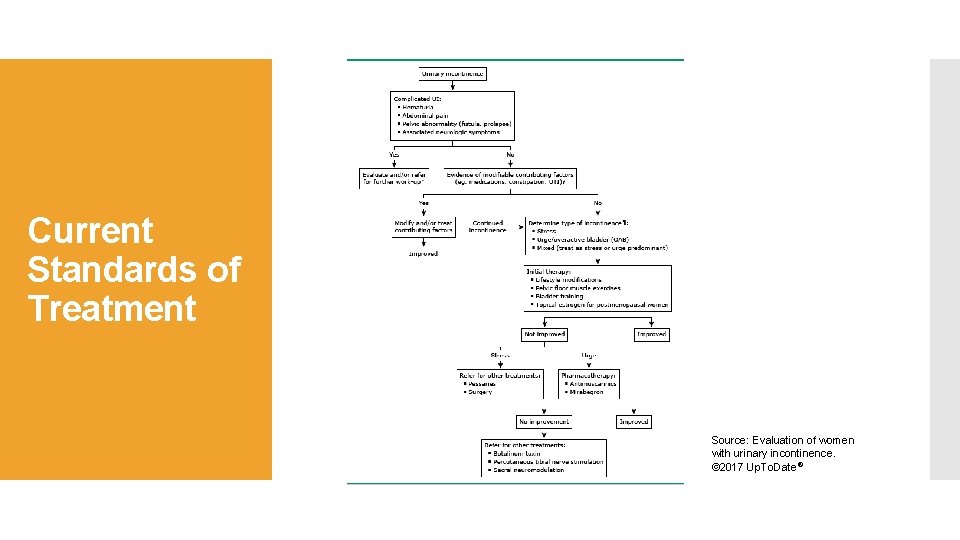
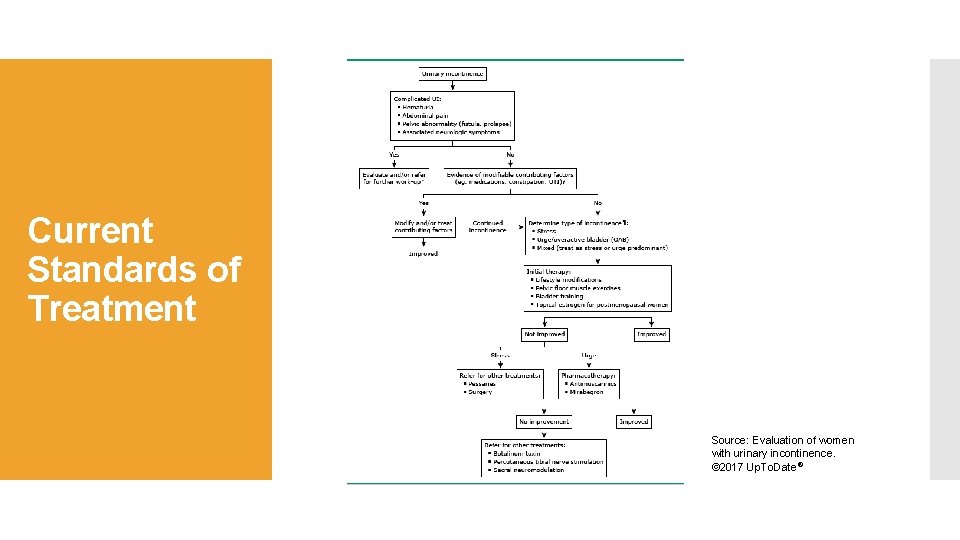
Current Standards of Treatment Source: Evaluation of women with urinary incontinence. © 2017 Up. To. Date®
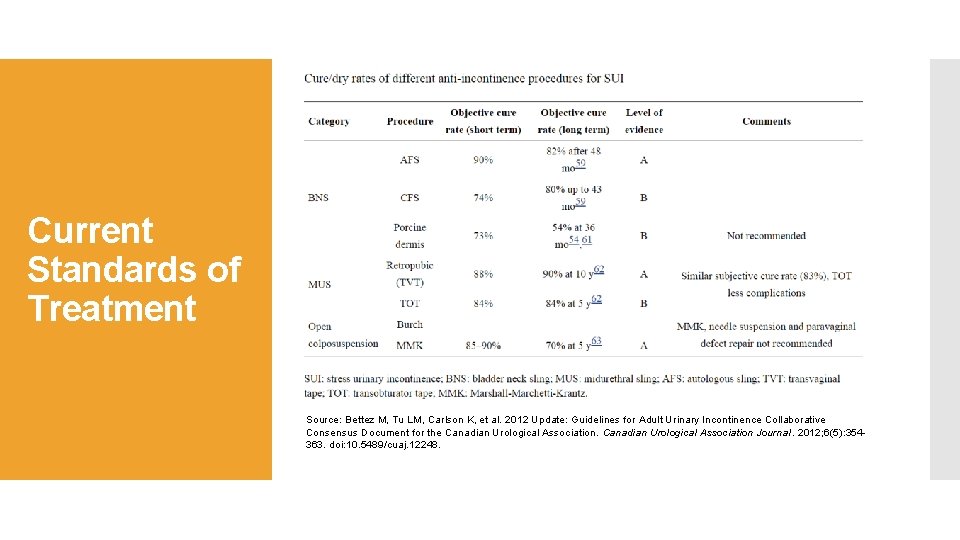
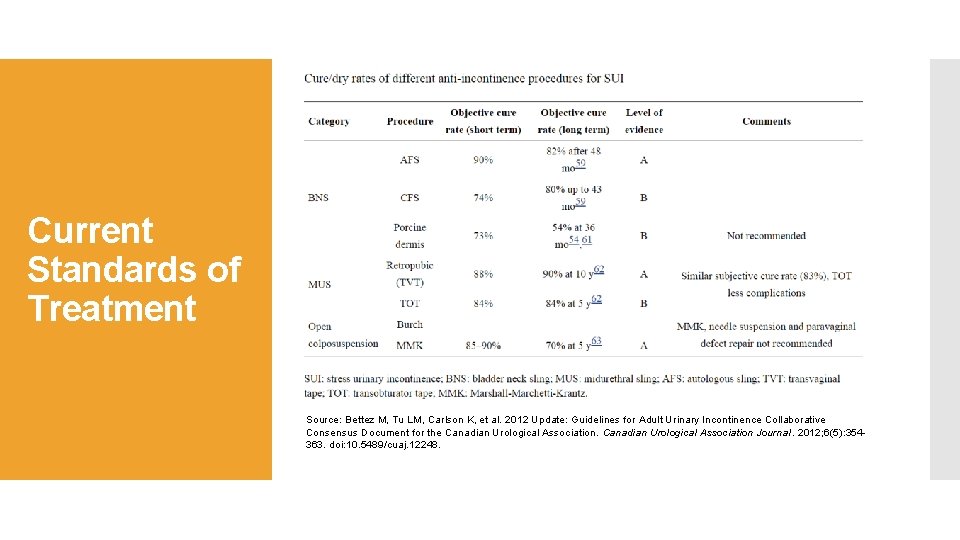
Current Standards of Treatment Source: Bettez M, Tu LM, Carlson K, et al. 2012 Update: Guidelines for Adult Urinary Incontinence Collaborative Consensus Document for the Canadian Urological Association Journal. 2012; 6(5): 354363. doi: 10. 5489/cuaj. 12248.
Role of androgen therapy in women is currently very limited Androgen Therapy Sexual Interest/Arousal Disorder - Endocrine Society guidelines endorse a short trial of T only in postmenopausal women with a dx of female sexual interest/ arousal disorder Sexual dysfunction due to Hypopituitarism – Clinical trial data have shown improved sexual function in women with corticotropin and gonadotropin deficiency Other – In uncontrolled studies, T has shown benefit in improving vasomotor flushes, cognitive function, mood, and bone mineral density Use of exogenous testosterone limited due to lack of FDA approved and commercially available formulations for women
Androgen receptors densely located in pelvic floor muscles and lower urinary tract Androgen Therapy Higher levels of androgen receptor expression have been found in levator ani muscle than other skeletal muscles in rats (Joubert, Tobin & Lebart, 1994) Levator ani is exceptionally responsive to androgens compared to other skeletal muscles in rats (Nnodim, 1999) In women, expression of androgen receptors in levator ani muscle and its fascia has been demonstrated (Ho, Bhatia & Bhasin, 2004) Periurethral striated muscle of the levator ani facilitates urethral closure during events that require a rapid, short lived ↑ in urethral resistance (Gosling et al. , 1999) Androgen receptors in the bladder and urethra have also been demonstrated in women (Ho et al. , 2004) Receptors were mainly localized at the bladder neck and in urothelium, with no receptor expression in deeper tissues of the bladder (Celayir, Ilce & Dervisoglu, 2002)
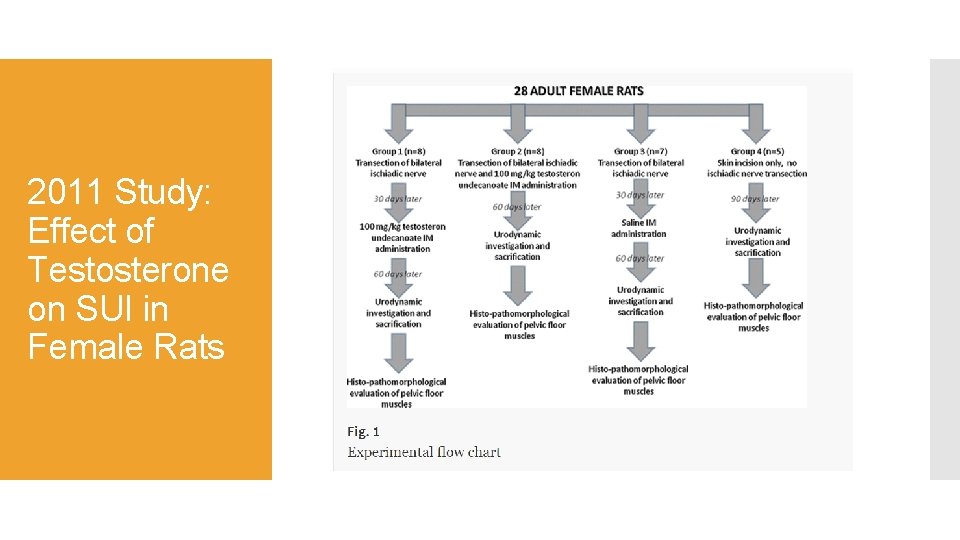
Androgens may influence neurotransmission Androgen receptors present in pudendal motoneurons which control the external urethral sphincter of female rats (Blanchet et al. , 2005) Androgen Therapy Exogenous androgen therapy for experimentally induced SUI Study examining the effect of intramuscular testosterone undecanoate on urodynamics in rats with experimentally induced SUI demonstrated both preventive and curative effects on rat models of experimental SUI (Mammadov et al. , 2011)
Clinical Trial: Testosterone Replacement in Postmenopausal Women with Stress Urinary Incontinence Androgen Therapy Matthew Ho, Charles Drew University of Medicine and Science Prospective randomized double-blind placebo-controlled trial on 60 postmenopausal women w/SUI and low Testosterone Duration: 36 weeks (Wks 1 -3 screening, 4 -28 application of placebo/testosterone patch, 29 -36 recovery time/assessment of effects) Primary Outcome: Change in levator ani muscle with correlation in improvement in SUI as determined by MRI, Urodynamic studies and pad tests Secondary Outcomes: Change in urethral pressure profile, pelvic floor muscle strength (perineometer), subjective quality of life Estimated completion date: December 31, 2018
Androgens have been shown to increase muscle mass Muscles in the pelvic floor and lower urinary tract, esp the levator ani, are highly sensitive to testosterone Androgen receptors are found throughout the pelvic floor and lower urinary tract in both animals and humans Androgens may further contribute to urinary continence via neuromodulation Conclusion These data together with a basic understanding of the mechanism of androgen action at the cellular level suggest androgens may play an important role in pelvic-floor and lower-urinary-tract function But we still have not elucidated the exact role of androgens in these systems and further investigations are needed Long-term side effects of testosterone and other androgen related therapies eg Selective Androgen Receptor Modulators also largely unknown, deserve further study Due to constraints in studying human tissues, the effects of androgen on the pelvic floor and lower urinary tract are more easily investigated in animal models.
Kingsberg S. Testosterone treatment for hypoactive sexual desire disorder in postmenopausal women. J Sex Med. 2007 Mar; 4 Suppl 3: 227 -34. Pub. Med PMID: 17394595. Kim M, Chaudhry Z, Oliver J, Kreydin E. Low serum testosterone is associated with increased stress and mixed incontinence in women. [abstract] J Urol 2017; 197(4 S); e 981 -e 182. Oral presentation at the American Urological Association 2017 annual meeting in Boston on May 15, 2017. Abstract PD 50 -07. Lue TF, Tanagho EA. Chapter 30. Urinary Incontinence. In: Mc. Aninch JW, Lue TF. eds. Smith and Tanagho's General Urology, 18 e New York, NY: Mc. Graw-Hill; 2013. Lukacz ES. Evaluation of women with urinary incontinence. Post TW, ed. Up. To. Date. Waltham, MA: Up. To. Date Inc. http: //www. uptodate. com (Accessed on August 19, 2017. ) References Nitti VW. The Prevalence of Urinary Incontinence. Reviews in Urology. 2001; 3(Suppl 1): S 2 -S 6. Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014 Mar 12; 311(10): 1052 -60. Pub. Med PMID: 24618967. Moore C. Definition and classification of UI and other pelvic floor disorders. AUA University. 2016. Available from: https: //university. auanet. org/core_topic. cfm? coreid=153 Abrams P, Andersson KE, Birder L, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and Treatment of Urinary Incontinence, Pelvic Organ Prolapse and Fecal Incontinence. Neurourol Urodyn. 2010; 29(1): 213– 40. Bettez M, Tu LM, Carlson K, et al. 2012 Update: Guidelines for Adult Urinary Incontinence Collaborative Consensus Document for the Canadian Urological Association Journal. 2012; 6(5): 354 -363. doi: 10. 5489/cuaj. 12248. Udoff LC. Overview of androgen deficiency and therapy in women. Post TW, ed. Up. To. Date. Waltham, MA: Up. To. Date Inc. http: //www. uptodate. com (Accessed on August 20, 2017. )
Joubert Y, Tobin C, Lebart MC. Testosterone-induced masculinization of the rat levator ani muscle during puberty. Dev Biol 1994. 162: 104– 110. Nnodim JO. Quantitative study of the effects of denervation and castration on the levator ani muscle of the rat. Anat Rec. 1999; 255: 324– 33. Axell AM, Mac. Lean HE, Plant DR, Harcourt LJ, Davis JA, et al. Continuous testosterone administration prevents skeletal muscle atrophy and enhances resistance to fatigue in orchidectomized male mice. Am J Physiol Endocrinol Metab. 2006; 291: E 506– 16. References Gosling JA, Dixon JS, Critchley HOD, Thompson SA. A comparative study of the human external sphincter and periurethral levator ani muscles. Br J Urol. 1981. 53: 35 -41. Copas P, Bukovsky A, Asbury B, et al. Estrogen, progesterone, androgen receptor expression in levator ani muscle and fascia. J Women Health Gend Based Med 2001; 10: 785 -795. Celayir S, Ilce Z, Dervisoglu S. The sex hormone receptors in the bladder in childhood-I: preliminary report in male subjects. Eur J Pediatr Surg 2002; 12: 312 -317. Blanchet P, Yaici el-D, Cayzergues L, Giuliano F, Jardin A, et al. Identification of androgen receptors in the motoneurons of the external urethral sphincter in the spinal cord of female rats. Eur Urol. 2005 Jan; 47(1): 118 -24. Pub. Med PMID: 15582260. Mammadov R, Simsir A, Tuglu I, Evren V, Gurer E, et al. The effect of testosterone treatment on urodynamic findings and histopathomorphology of pelvic floor muscles in female rats with experimentally induced stress urinary incontinence. Int Urol Nephrol. 2011 Dec; 43(4): 1003 -8. Pub. Med PMID: 21442470.
Questions?
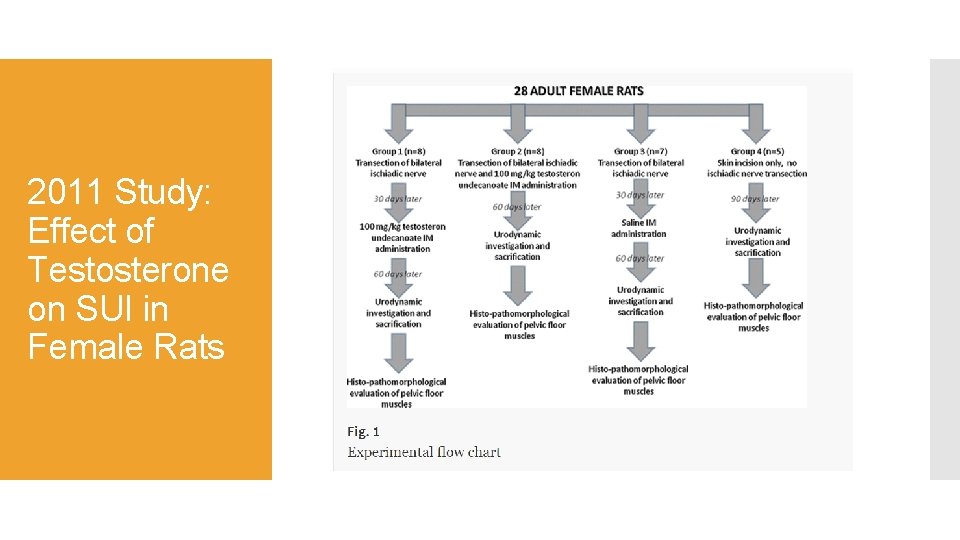
2011 Study: Effect of Testosterone on SUI in Female Rats
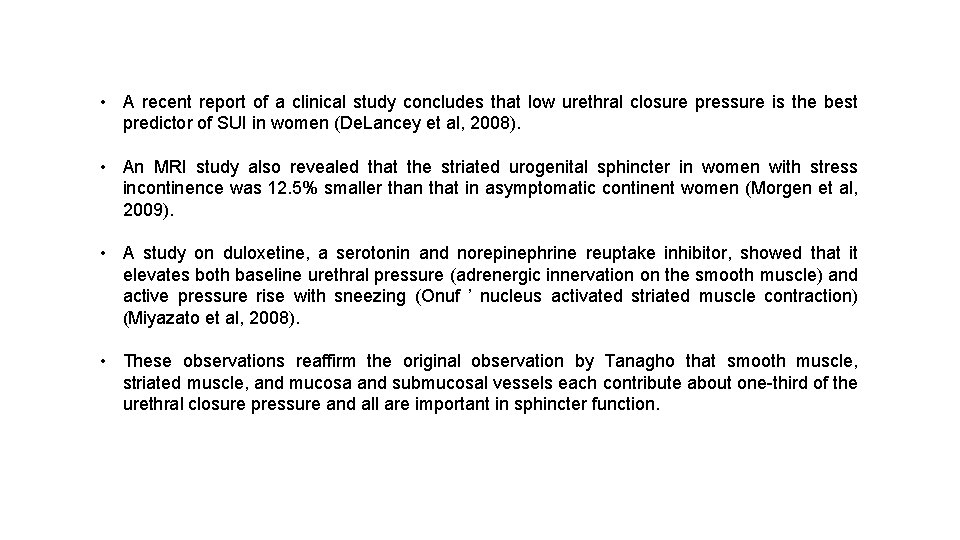
• A recent report of a clinical study concludes that low urethral closure pressure is the best predictor of SUI in women (De. Lancey et al, 2008). • An MRI study also revealed that the striated urogenital sphincter in women with stress incontinence was 12. 5% smaller than that in asymptomatic continent women (Morgen et al, 2009). • A study on duloxetine, a serotonin and norepinephrine reuptake inhibitor, showed that it elevates both baseline urethral pressure (adrenergic innervation on the smooth muscle) and active pressure rise with sneezing (Onuf ’ nucleus activated striated muscle contraction) (Miyazato et al, 2008). • These observations reaffirm the original observation by Tanagho that smooth muscle, striated muscle, and mucosa and submucosal vessels each contribute about one-third of the urethral closure pressure and all are important in sphincter function.
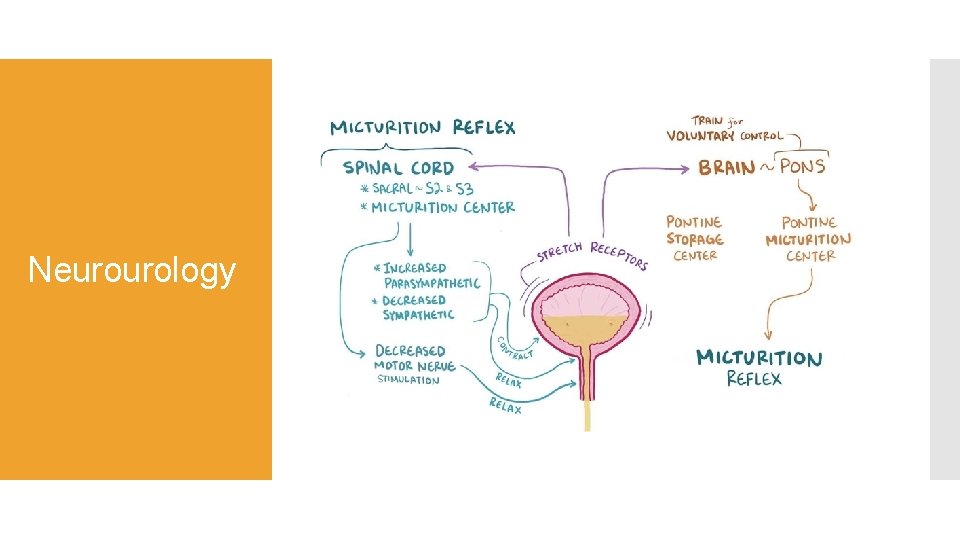
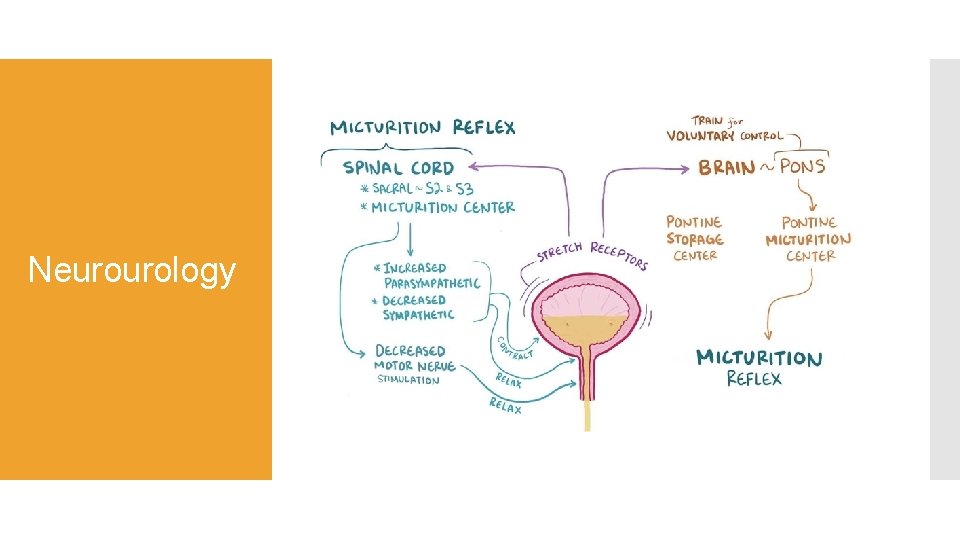
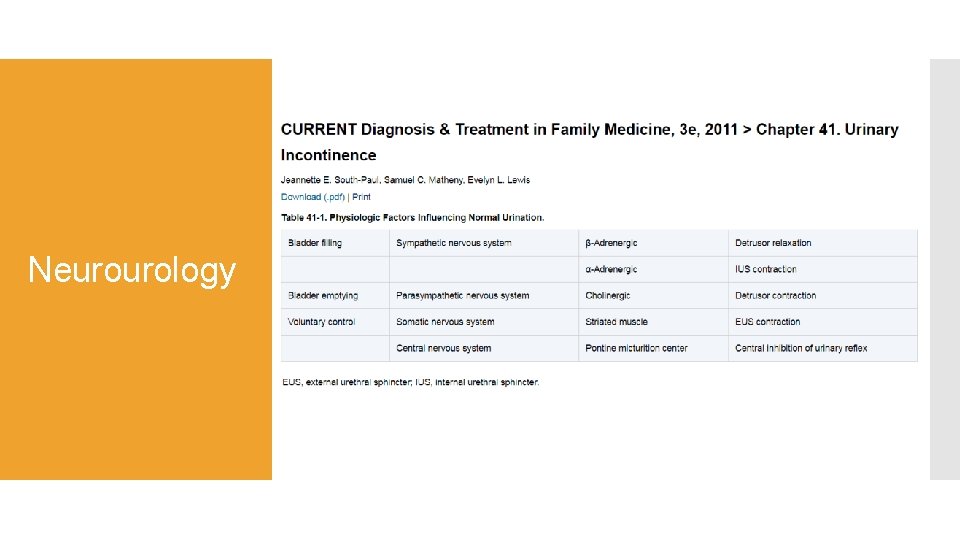
Neurourology
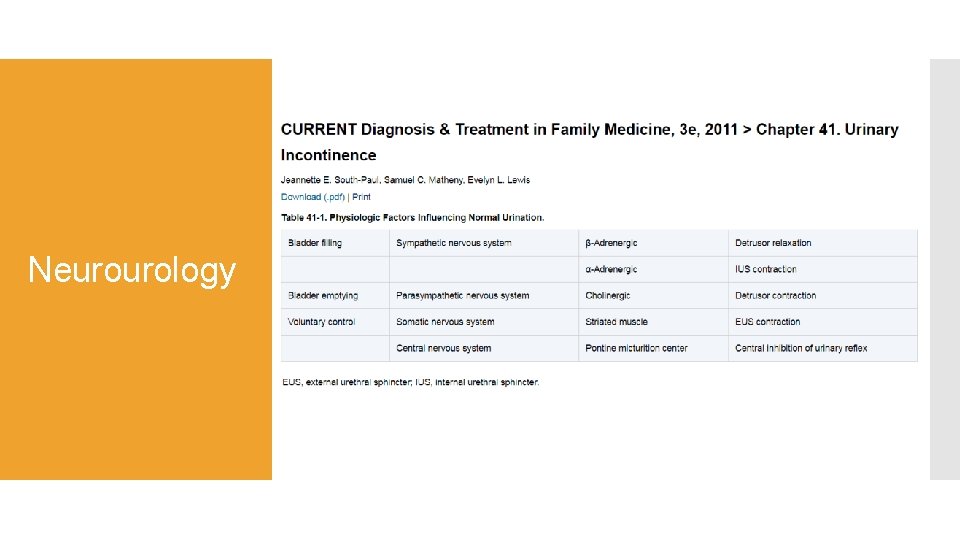
Neurourology
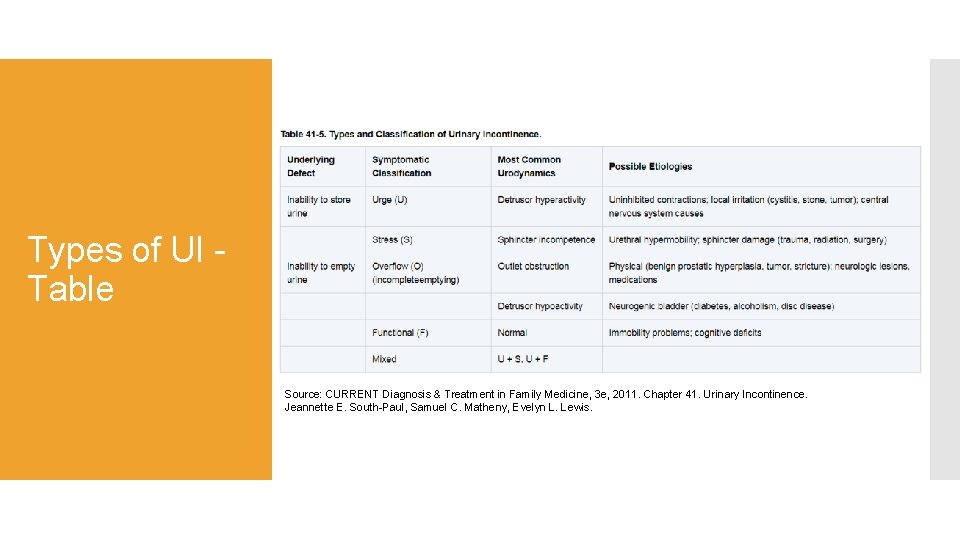
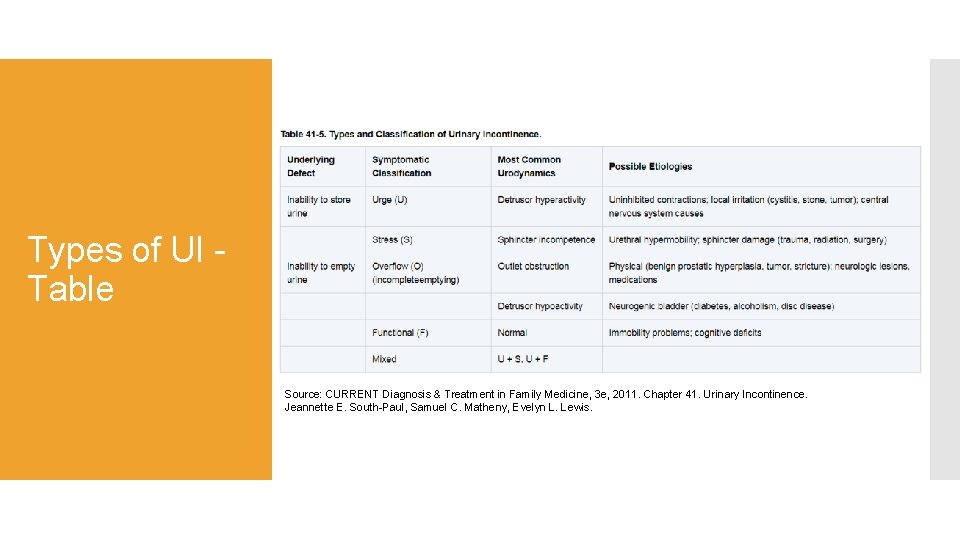
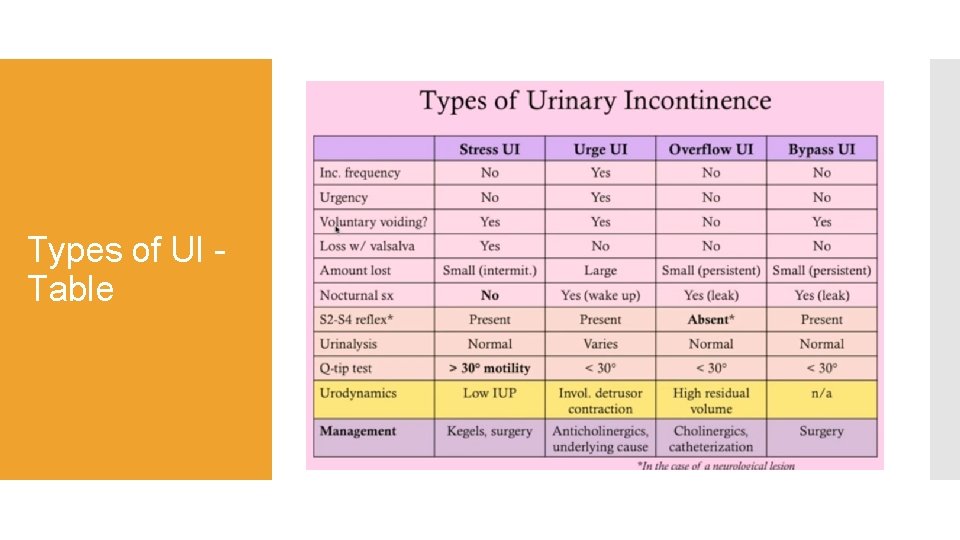
Types of UI - Table Source: CURRENT Diagnosis & Treatment in Family Medicine, 3 e, 2011. Chapter 41. Urinary Incontinence. Jeannette E. South-Paul, Samuel C. Matheny, Evelyn L. Lewis.
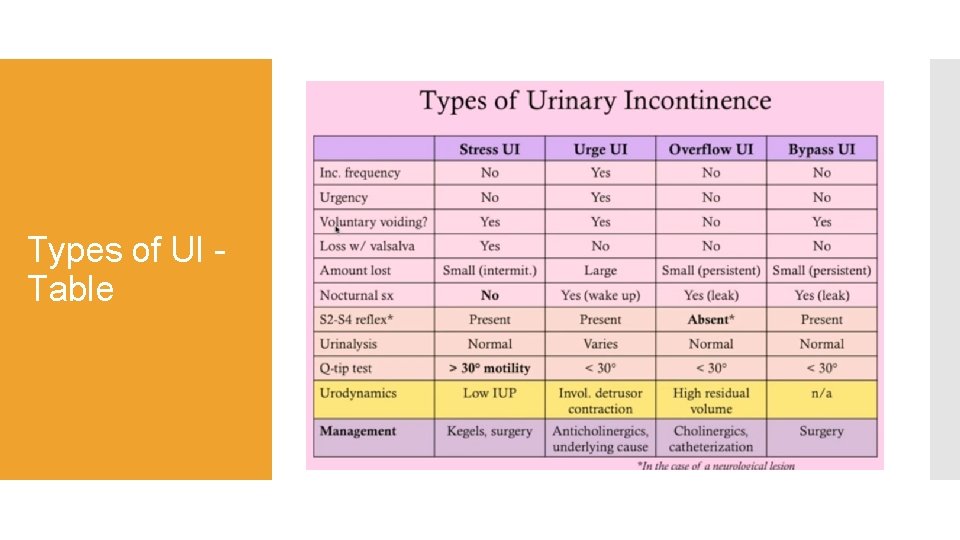
Types of UI - Table

Medications that can precipitate incontinence Diuretics Antidepressants Sedative hypnotics Adrenergic agonists or blockers Anticholinergics CCBs
Using Presenter View is a great way to view your presentation with speaker notes on one computer (your laptop, for example), while your audience views the notes-free presentation on a different monitor (like a larger screen you're projecting to). NOTE: Make sure the device you're using for your presentation supports the use of multiple monitors. Check with your manufacturer for up-to-date information about multiple monitor support. 2016, 2013, 20102007 To do this procedure, you must be connected to the second screen. Set up Power. Point to use Presenter view with two monitors 1. On the Slide Show tab, in the Monitors group, select Use Presenter View. Windows Display Settings should open. 2. In the Display Settings dialog box, on the Monitor tab, select the monitor icon that you want to use to view your speaker notes, and then select the This is my main monitor check box. If the This is my main monitor check box is selected and unavailable, the monitor is already designated as the primary monitor. 3. Select the monitor icon for the second monitor—the one the audience will watch, and then select the Extend my Windows Desktop onto this monitor check box. NOTES: If the display settings don't open, do the following: • Windows 10: Click Start > Settings > System > Display. At the top, under Customize your display, is a diagram of the screens connected to your computer, with each screen numbered. If you are connected to a project, typically it will be represented in the diagram as screen 2. Select screen 1 in the diagram, then scroll downward. Ensure that the check box named Make this my main display is selected. Above that check box, in the Multiple displays list, select Extend these displays. • Windows 8: Right-click the Windows Start button, click Control Panel >Display > Adjust resolution. In the Multiple displays list, click Extend these displays. Select the monitor on which you want to view your speaker notes, and click Make this my main display. • Windows 7: Click Start > Control Panel, and under Appearance and Personalization, click Adjust screen resolution. In the Multiple displays list, click Extend these displays. Select the monitor on which you want to view your speaker notes, and click Make this my main display. You can use Power. Point on your smartphone as a remote control to run your presentation and view your speaker notes. See Using a laser pointer on your smartphone when presenting in Power. Point for more information, including a brief video. Deliver your presentation on two monitors 1. On the Slide Show tab, in the Set Up group, click Set Up Slide Show. 2. In the Set Up Show dialog box, choose the options that you want, and then click OK. If you choose Automatic, the monitor you selected as your main display will show your speaker notes. (Power. Point 2010) To see your speaker notes on your primary monitor. select your secondary monitor from the Display slide show on list. 3. To begin delivering your presentation, on the Slide Show tab, click From the Beginning, or click the Slide Show button at the bottom of the Power. Point window.