Role Faith Community Nurses in EvidenceBased Practice Mary
Role Faith Community Nurses in Evidence-Based Practice Mary Lynne Knighten, DNP, RN, NEA-BC Adjunct Faculty Azusa FCN Foundations Educator Pacific University Health Ministry Director, St. Dominic Catholic Church Los Angeles, CA Westberg Symposium April 2020
Learning Objectives Upon completion of this learning activity, participants will be able to: • Define Evidence-Based Practice (EBP) and describe their role as faith community nurses (FCN) in EBP. • Articulate the seven steps of EBP, and use the PICOT (P-Patient/Problem, I-Intervention, C-Comparison, OOutcome, and T-Time) framework to develop a spirit of inquiry. • Evaluate and appraise the evidence utilizing a valid and reliable appraisal tool.
Learning Outcome Current State: Nurses traditionally practice based on what they were taught and based on their experience. Practice tends to be individual rather than professional. Future State: At the conclusion of this presentation, participants will be able to support, apply, and engage in evidence-based practice in their faith communities and in the profession.

Research in Faith Community Nursing • New and translational research is conducted in areas of nursing, health, faith practices, and spirituality. • The faith community nurse should implement practice based on the best known research and evidence. • Drawn from nursing for this evidence • Contributions from other disciplines
Research in Faith Community Nursing • Dyess, Chase, & Newlin (2009) embarked on the first review of research literature for faith community nursing, dating back to 1993. • No review of research literature was previously published in 20 years of faith community nursing history. • Four major content areas in the faith community nursing research literature: 1) Development and implementation of faith community nursing practices; 2) Roles and activities of FCNs; 3) FCN evaluation and documentation; and 4) Congregation perceptions of faith community nursing. • Recommendations: establish structure, process, and outcomes to measure faith community nursing work, and analyze data to evaluate the efficacy of this specialty practice.
Research in Faith Community Nursing • Solari-Twadell & Ziebarth (in 2019) document the ongoing effort to identify a faith community nursing research agenda. • Forums for developing the FCN research agenda include dedicated meetings and pre-conference sessions at the annual Westberg Symposium. • FCNs are able to participate and contribute • Research agenda is modified regularly • Advance with the maturation of the specialty practice • Pace with the larger nursing research agenda.

Research in Faith Community Nursing • The purposes of developing research priorities for FCN specialty practice are: 1) Demonstrate contribution of FCNs to healthcare outcomes 2) Identify cost effective strategies for prevention and care across the continuum of care 3) Identify the faith community as a strategic partner in promoting health and wholeness 4) Advance faith community nursing as a specialty nursing practice (Solari-Twadell & Ziebarth, 2019)
EBP and Faith Community Nursing • Research conducted at NIH and academic institutions • Relationship between spiritual practices and health • Expands the knowledge base for the faith community nursing specialty (ANA & HMA, 2012) • Standard 13 of the Faith Community Nursing Scope and Standards of Practice states: • FCNs integrate evidence and research into practice (ANA & HMA, 2017, p. 74) • Underpinnings of evidence shape the scope and standards, define the specialty, and set forth competencies for the practice
EBP and Faith Community Nursing • In 2019, the Westberg Institute supported development of a position statement regarding the role of the faith community nurse in evidence-based practice (EBP). • The position statement is: “The faith community nurse supports, applies, and engages in evidence-based practice” (Knighten, 2019). • FCNs are in an ideal position to lead the faith community • Create structures, models, and processes • Integrate research and evidence-based practices into faith-based ministries (Lashley, 2013)
Evidence-Based Practice • Nurses are called to ensure their practice is best practice and based on evidence. • Many nurses do not understand what evidence is, where to find, or how to evaluate it. • Research findings, to be of true worth to practice, require translation into nursing practice. • Practice drives research and research drives practice.
Evidence-Based Practice • The primary role of the FCN is to provide intentional care of the spirit • Address the needs of their patients—body, mind, and spirit • Promote health and prevent/minimize disease • In the context of faith beliefs and traditions and the larger community (ANA & HMA, 2017) • When delivered in the context of a caring, supportive practice situation, the highest quality and best patient and family outcomes can be achieved (Knighten, 2019).
Evidence-Based Practice • The conscientious use of current best practice in making decisions about patient care (Sackett, Straus, Richardson, Rosenberg, & Haynes, 2000)—a classic definition still pertinent today. • Subsequently, the scope of the definition has broadened to infer a reliable and enduring problem-solving approach. (Melnyk and Fineout-Overholt, 2015).
Evidence-Based Practice • That problem-solving approach integrates: • A systematic search for, critical appraisal of, and synthesis of the best, most relevant research • Answers an urgent or crucial clinical question • The practitioner’s own clinical expertise • • • Practice Quality improvement projects Systematic patient assessment Evaluation Use of key available resources • Patient preferences, beliefs, and values (Melnyk & Fineout-Overholt, 2015) • …to result in preferred patient outcomes
Faith Community Nursing and EBP • FCNs derive best practice from nursing evidence. • Faith Community Nursing research vs. general nursing research • Other disciplines, such as chaplaincy, pastoral care, or theology as possible sources of evidence. • Whole-person health and spirituality • Alleviate suffering • Achieve healing • Even if cure is not possible
Challenges and Barriers to EBP for FCNs • Research evidence, tends to be more highly valued than other sources of evidence in the delivery of healthcare. • Concentration has been on getting research evidence produced, synthesized, disseminated, and used in practice. • This has meant the relative neglect of other forms of evidence (Rycroft-Malone, 2003) • Research evidence base for practice is rarely constant, but is evolving; should be viewed as provisional (Upsher, 2001). • There is lack of a clear, standard pathway by which academic research is translated into direct practice.
Challenges and Barriers to EBP for FCNs • Too much volume of evidence is being produced to efficiently review and apply it. • Nurses feel they do not have authority to implement EBP to change practice. • There is insufficient time at work. • Difficulty is expressed in understanding statistical analysis. • Research terminology is not understood.
Overcoming Challenges to EBP for FCNs • Main & Ogaz (2016) published an article that reviewed basic statistical concepts, define common statistical tests, and facilitate analysis of test results. • FCN Network has an organizational commitment to strengthen research infrastructure, and increase awareness of EBP amongst FCNs. • Faith Community Nurses International, has an active Research Committee, recently launched a Practice Committee, and offers a mentoring hour to FCNs conducting research and implementing EBP projects.
Overcoming Challenges to EBP for FCNs • Centers that gather and disseminate evidence reports, highlight the importance of—and the need for—evidence-based practice. • Practice Guideline Clearinghouse at the Agency for Health and Research Quality (AHRQ) in the United States, • Cochrane Collaboration in the United Kingdom • Joanna Briggs Institute for EBP in Australia (Olade, 2004) • Registered Nurses’ Association of Ontario (RNAO) in Canada • American Health. Care Research and Quality (AHRQ) archives
Equipping FCNs for EBP: Competencies The faith community nurse demonstrates the following basic competencies in regards to EBP (ANA & HMA, 2017): • Verbalizes how research is applied in a relevant manner in the healthcare setting and practice • Poses questions in the practice and care delivery setting and identifies the intersections of health, spirituality, and spiritual care where research may be applied or replicated • Uses current and relevant evidence-based knowledge to guide professional practice, including research and outcomes from practice
Equipping FCNs for EBP: Competencies The faith community nurse demonstrates the following basic competencies in regards to EBP (ANA & HMA, 2017), continued: • Utilizes evidence when implementing nursing practice, process, or behavior changes • Participates, as appropriate, to formulate evidence-based practice through research and quality improvement projects to expand the body of knowledge on a topic or practice area • Upholds ethical and moral principles of research in their personal professional practice and the faith community nursing practice setting (see also Code of Ethics, Provision 7, ANA & HMA, 2017 pg. 21)
Equipping FCNs for EBP: Competencies The faith community nurse demonstrates the following basic competencies in regards to EBP (ANA & HMA, 2017), continued: • Reviews and evaluates research and evidence-based knowledge, data, and outcomes to apply it in the best possible way • Shares peer-reviewed evidence with colleagues to promote growth and the integration of new knowledge into faith community nursing practice (ANA & HMA, 2017)
Equipping FCNs for EBP: Competencies Additional advanced FCN competencies (14) for APRNs and nurses prepared at the graduate level: • Integrates research-based practice in all settings and uses research/evidence to improve quality • Enhances role performance, and expands skills, knowledge, skills, abilities, and judgment by using current healthcare research findings and other evidence • Connects theory to research by using critical thinking • Encourages other nurses to develop research skills Standard 13. ANA & HMA, 2017
Equipping FCNs for EBP: Competencies Additional advanced FCN competencies (14) for APRNs and nurses prepared at the graduate level, continued: • Recognizes the need to measure research in the spiritual dimensions of diagnosis, interventions, and outcomes that improve health and wholeness • Contributes to the body of nursing knowledge by conducting or synthesizing research and other evidence to improve healthcare outcomes • Designs strategies and tactics to meet complex needs of healthcare consumers, as well as population health programs Standard 13. ANA & HMA, 2017
Equipping FCNs for EBP: Competencies Additional advanced FCN competencies (14) for APRNs and nurses prepared at the graduate level, continued: • Leads design and development of interprofessional processes • Designs innovative nursing practices to improve the health and well-being of individuals and populations • Performs rigorous critique of evidence to generate meaningful evidence for practice Standard 13. ANA & HMA, 2017
Equipping FCNs for EBP: Competencies Additional advanced FCN competencies (14) for APRNs and nurses prepared at the graduate level, continued: • Advocates for the ethical conduct of research and translational scholarship • Promotes a climate of collaborative research and clinical inquiry • Disseminates research [and quality improvement] findings through presentations, publications, consultation, journal clubs, blogs, etc. Standard 13. ANA & HMA, 2017
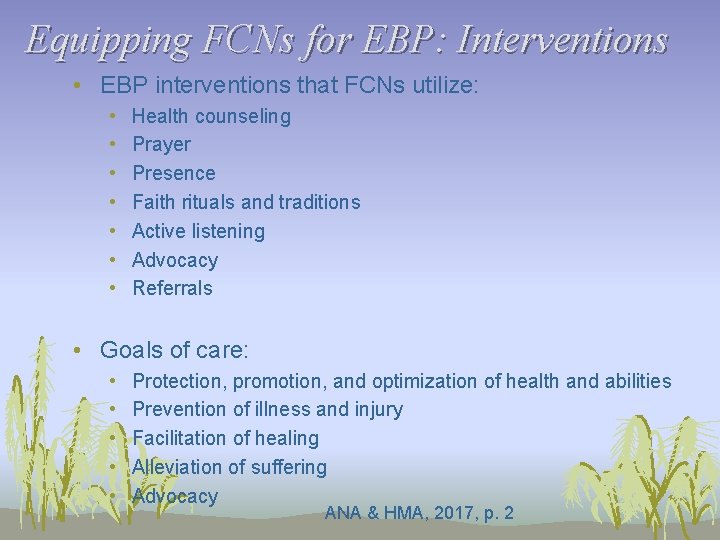
Equipping FCNs for EBP: Interventions • EBP interventions that FCNs utilize: • • Health counseling Prayer Presence Faith rituals and traditions Active listening Advocacy Referrals • Goals of care: • • • Protection, promotion, and optimization of health and abilities Prevention of illness and injury Facilitation of healing Alleviation of suffering Advocacy ANA & HMA, 2017, p. 2
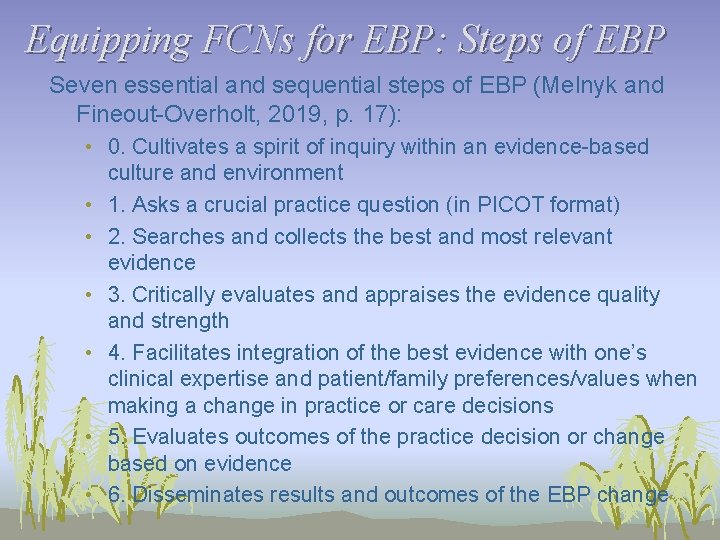
Equipping FCNs for EBP: Steps of EBP Seven essential and sequential steps of EBP (Melnyk and Fineout-Overholt, 2019, p. 17): • 0. Cultivates a spirit of inquiry within an evidence-based culture and environment • 1. Asks a crucial practice question (in PICOT format) • 2. Searches and collects the best and most relevant evidence • 3. Critically evaluates and appraises the evidence quality and strength • 4. Facilitates integration of the best evidence with one’s clinical expertise and patient/family preferences/values when making a change in practice or care decisions • 5. Evaluates outcomes of the practice decision or change based on evidence • 6. Disseminates results and outcomes of the EBP change
Equipping FCNs for EBP: PICOT • PICOT is an acronym that describes the elements of a good clinical question: • • • P - Patient/Problem I - Intervention C - Comparison O - Outcome T - Time. • Writing a good PICOT question clarifies the issue to be addressed, drives the evidence search, and facilitates identifying the right solution(s).
Equipping FCNs for EBP: PICOT • Example of a well-written PICOT question: Do congregants (P) who participate in a blood pressure (BP) clinic conducted by a FCN in their faith community (I) as compared to congregants who only measure their BP at home or at their physician’s office (C) have better hypertension management (O) over a six month period (T)? • Example of a poorly written PICOT question: What is the best intervention for hypertension management in the community?
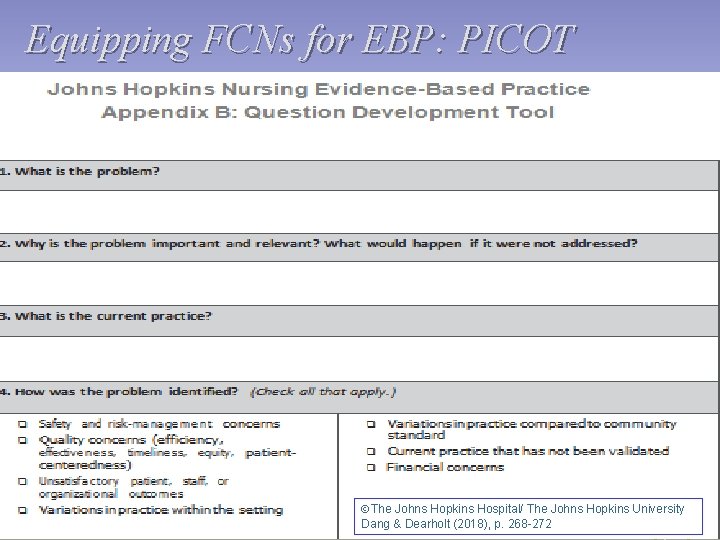
Equipping FCNs for EBP: PICOT ÓThe Johns Hopkins Hospital/ The Johns Hopkins University Dang & Dearholt (2018), p. 268 -272
Equipping FCNs for EBP: PICOT • Does anyone have an example of a problem that exists in your FCN practice? • What is the current practice? • What would happen if that problem was not addressed? Add your responses to these three questions to the Chat Box and we will review a few…
Equipping FCNs for EBP: PICOT • Experiential Exercise– Take two minutes to write a PICOT question that is reflective of a clinical question in your faith community practice. • PICOT is an acronym that describes the elements of a good clinical question: • • • P-Patient/Problem I-Intervention C-Comparison O-Outcome T-Time Please enter your PICOT question in the Chat Box and we will review a few…
Equipping FCNs for EBP: PICOT • Example of a well-written PICOT question: Do congregants (P) who participate in a blood pressure (BP) clinic conducted by a FCN in their faith community (I) as compared to congregants who only measure their BP at home or at their physician’s office (C) have better hypertension management (O) over a six month period (T)? • Key terms from the PICOT question to guide the search for evidence:
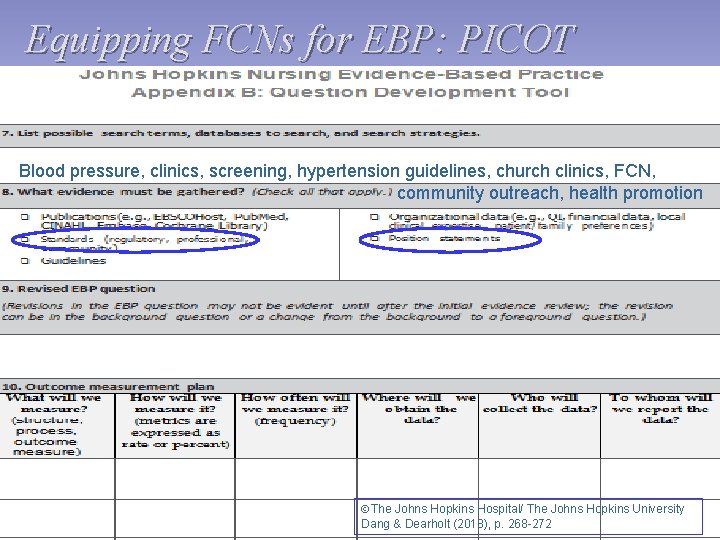
Equipping FCNs for EBP: PICOT Blood pressure, clinics, screening, hypertension guidelines, church clinics, FCN, community outreach, health promotion ÓThe Johns Hopkins Hospital/ The Johns Hopkins University Dang & Dearholt (2018), p. 268 -272
Equipping FCNs for EBP: Evidence Search • Resource #1 ($50. 00 for six mos. available for FCNI members) Lees-Mc. Rae College May School of Nursing and Health Sciences Dr. Teresa Darnall 191 Main St. Banner Elk, NC 28604 E-mail: tbdarnall@gmail. com vs. darnallt@lmc. edu FCNI Membership info: https: //www. fcninternational. org/membership. html contact@fcninternational. org
Equipping FCNs for EBP: Evidence Search • Resource #2 (Free, limited) University of San Francisco Curated Research Guides to Finding and Using Library Research Sources https: //guides. usfca. edu/? b=t • Other Resources • Google Scholar • Public Library • Local hospital or university libraries
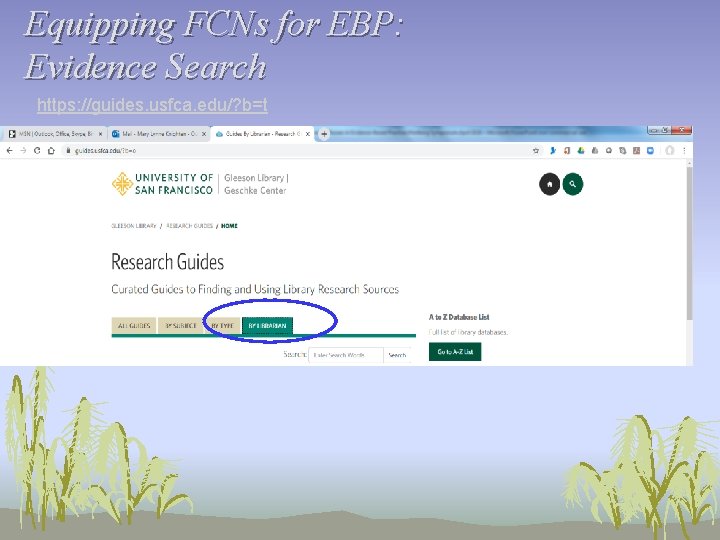
Equipping FCNs for EBP: Evidence Search https: //guides. usfca. edu/? b=t
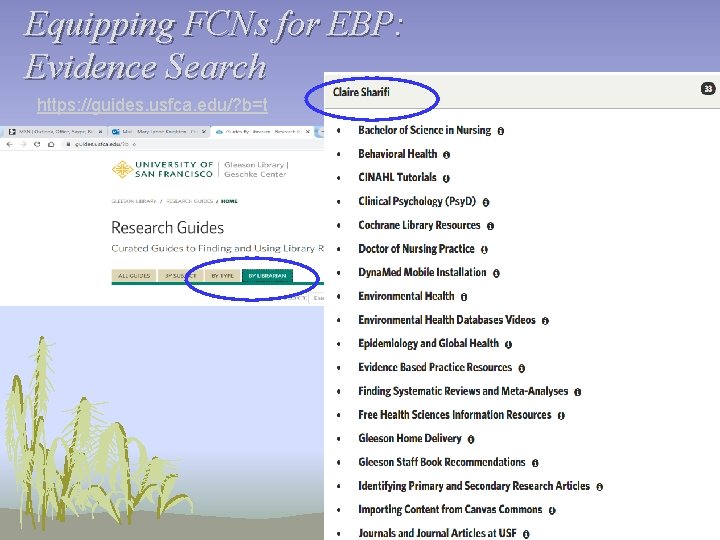
Equipping FCNs for EBP: Evidence Search https: //guides. usfca. edu/? b=t
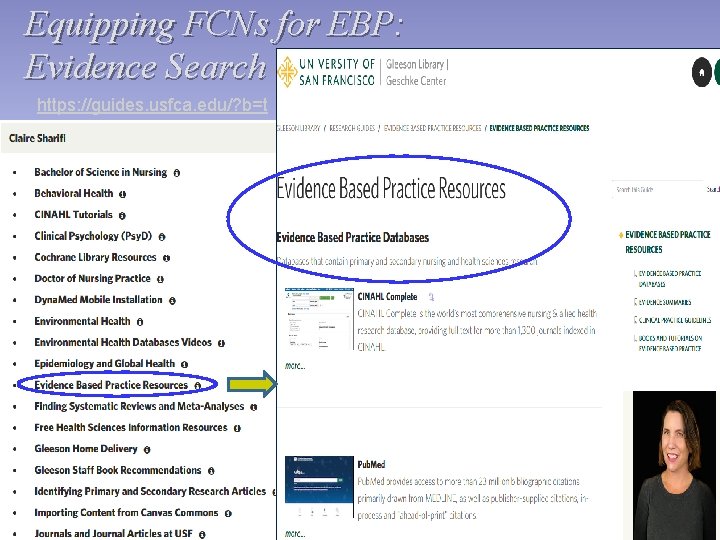
Equipping FCNs for EBP: Evidence Search https: //guides. usfca. edu/? b=t
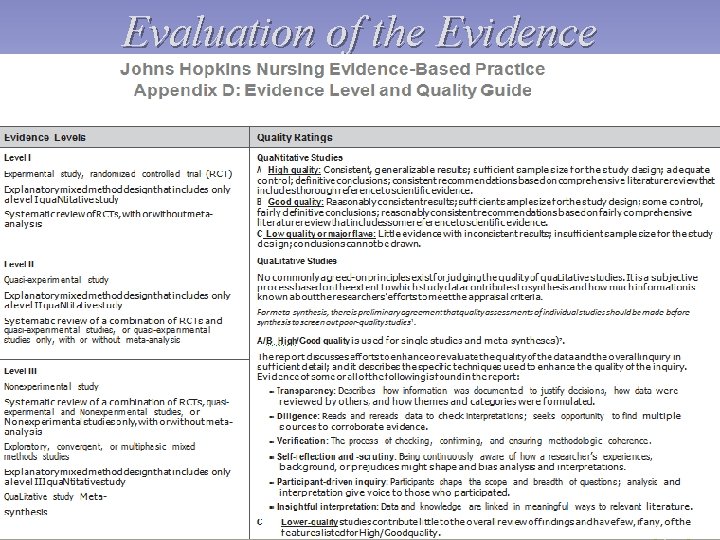
Evaluation of the Evidence
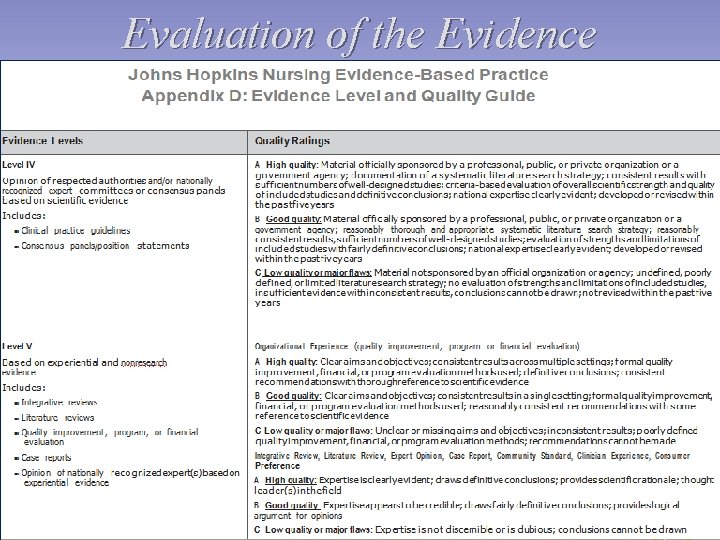
Evaluation of the Evidence
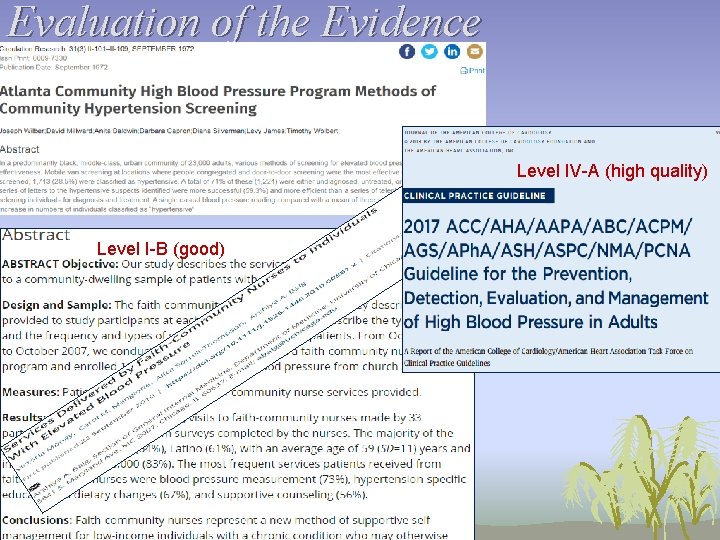
Evaluation of the Evidence Level IV-A (high quality) Level I-B (good)

Type questions into the Q&A Box Dr. Mary Lynne Knighten knightenmarylynne@hotmail. com 310 -386 -1539
References American Nurses Association & Health Ministries Association, Inc (2012). Faith community nursing: Scope and standards of practice, 2 nd Edition. Silver Spring, MD: Nurse. Books. org. American Nurses Association & Health Ministries Association, Inc (2017). Faith community nursing: Scope and standards of practice, 3 rd Edition. Silver Spring, MD: Nurse. Books. org. Dang, D. , & Dearholt, S. L. (2018). Johns Hopkins nursing evidence-based practice: Model and guidelines (3 rd ed. ). Indianapolis, IN: Sigma Theta Tau International. Hughes, B. P. , De. Gregory, C. , Elk, R. , Graham, D. , Hall, E. J. , & Ressallat, J. (March 2017). Spiritual care and nursing: A nurse’s contribution and practice [White Paper]. Health. Care Chaplaincy Network. Knighten (2019). Evidence Based Practice: Faith Community Nurses. [Position Statement]. Memphis, TN: Westberg Institute for Faith Community Nursing. Main, M. E. , & Ogaz, V. L. (2016). Common statistical tests and interpretation in nursing research. International Journal of Faith Community Nursing, 2(3), Article 2.
References, cont’d. Majid, S. , Foo, S. , Luyt, B. , Zhang, X. , Theng, Y. , Chang, Y. , & Mokhtar, I. A. (2011). Adopting evidence-based practice in clinical decision. making: Nurses' perceptions, knowledge, and barriers. Journal of the Medical Library Association, 99(3), 229 -36. doi: 10. 3163/1536 - 5050. 99. 3. 010 Melnyk, B. M. & Fineout-Overholt, E. (2019). Evidence-based practice in nursing and healthcare: A guide to best practice, 4 th Edition. Philadelphia: Lippincott Williams & Wilkins. Olade, R. A. (2004). Strategic Collaborative Model for Evidence-Based Nursing Practice. Worldviews on Evidence-Based Nursing 2004, 1, 60– 68. Rycroft-Malone, J. , Seers, K. , Titchen, A. , Harvey, G. , Kitson, A. , & Mc. Cormack, B. (2003). What counts as evidence in evidence-based practice? Journal of Advanced Nursing, 47(1), 81– 90. Solari-Twadell P. A. , Ziebarth D. J. (2020) Research Agenda in Faith Community Nursing. In: Solari-Twadell P. , Ziebarth D. (Eds. ), Faith community nursing. New York: Springer, Cham (pp. 341 -356). Pravikoff, D. , Tanner, A. B. , & Pierce, S. T. (2005). Readiness of U. S. nurses for evidence-based practice. Am J Nurs. 2005 Sep, 105(9), 40 -51; quiz 52. Upshur R. E. G. (2001). The status of qualitative research as evidence. In Morse J. M. , Swanson J. M. & Kuzel A. J. , (Eds. ), The nature of qualitative evidence. Thousand Oaks, CA: Sage, 5– 26.
- Slides: 45