Risk Stratification of Severe Symptomatic Aortic Stenosis Patients
![Absolute Reduction in Mortality at 3 Year in Inoperable Patients HR [95% CI] = Absolute Reduction in Mortality at 3 Year in Inoperable Patients HR [95% CI] =](https://slidetodoc.com/presentation_image_h2/5f47794a3d58be8a417f272394570518/image-4.jpg)
![Reduction in Repeat Hospitalization in Inoperable Patients Rehospitalization 125% HR [95% CI] = 0. Reduction in Repeat Hospitalization in Inoperable Patients Rehospitalization 125% HR [95% CI] = 0.](https://slidetodoc.com/presentation_image_h2/5f47794a3d58be8a417f272394570518/image-5.jpg)
- Slides: 12
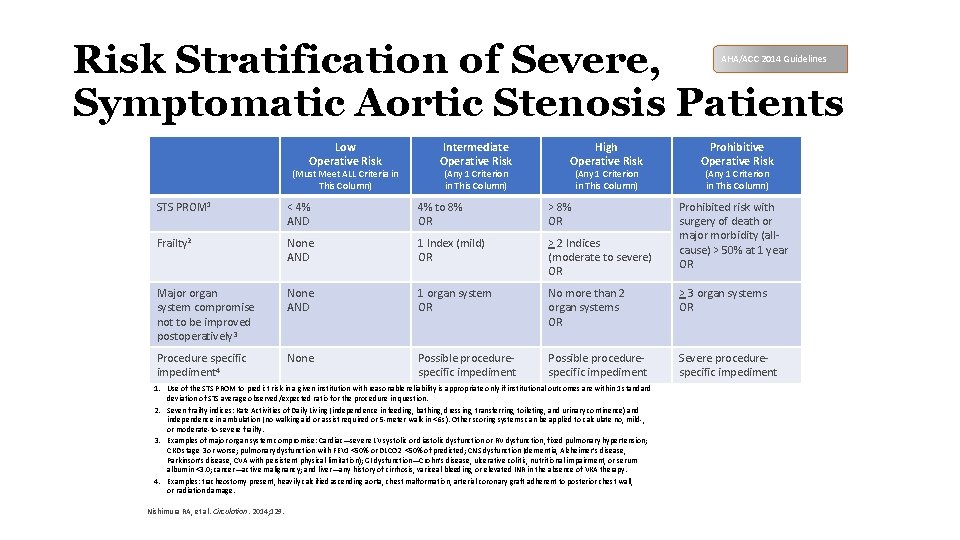
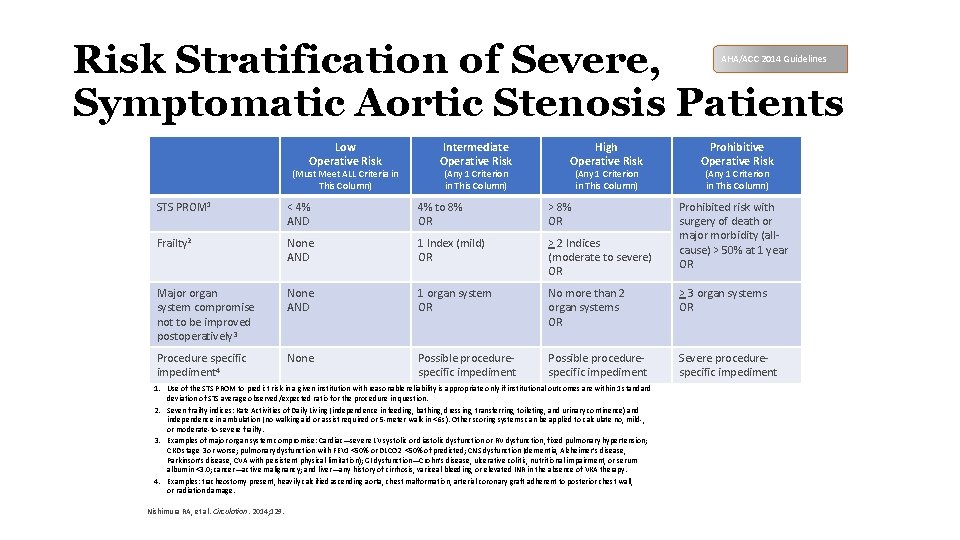
Risk Stratification of Severe, Symptomatic Aortic Stenosis Patients AHA/ACC 2014 Guidelines Low Operative Risk Intermediate Operative Risk (Must Meet ALL Criteria in This Column) (Any 1 Criterion in This Column) High Operative Risk (Any 1 Criterion in This Column) Prohibitive Operative Risk (Any 1 Criterion in This Column) STS PROM 1 < 4% AND 4% to 8% OR > 8% OR Frailty 2 None AND 1 Index (mild) OR > 2 Indices (moderate to severe) OR Major organ system compromise not to be improved postoperatively 3 None AND 1 organ system OR No more than 2 organ systems OR > 3 organ systems OR Procedure specific impediment 4 None Possible procedurespecific impediment Severe procedurespecific impediment 1. Use of the STS PROM to predict risk in a given institution with reasonable reliability is appropriate only if institutional outcomes are within 1 standard deviation of STS average observed/expected ratio for the procedure in question. 2. Seven frailty indices: Katz Activities of Daily Living (independence in feeding, bathing, dressing, transferring, toileting, and urinary continence) and independence in ambulation (no walking aid or assist required or 5 -meter walk in <6 s). Other scoring systems can be applied to calculate no, mild-, or moderate-to-severe frailty. 3. Examples of major organ system compromise: Cardiac—severe LV systolic or diastolic dysfunction or RV dysfunction, fixed pulmonary hypertension; CKD stage 3 or worse; pulmonary dysfunction with FEV 1 <50% or DLCO 2 <50% of predicted; CNS dysfunction (dementia, Alzheimer’s disease, Parkinson’s disease, CVA with persistent physical limitation); GI dysfunction—Crohn’s disease, ulcerative colitis, nutritional impairment, or serum albumin <3. 0; cancer—active malignancy; and liver—any history of cirrhosis, variceal bleeding, or elevated INR in the absence of VKA therapy. 4. Examples: tracheostomy present, heavily calcified ascending aorta, chest malformation, arterial coronary graft adherent to posterior chest wall, or radiation damage. Nishimura RA, et al. Circulation. 2014; 129. Prohibited risk with surgery of death or major morbidity (allcause) > 50% at 1 year OR
Transcatheter Therapy • First explored for in-operable AS patients • No other interventional options available • Outcomes far superior than what was expected
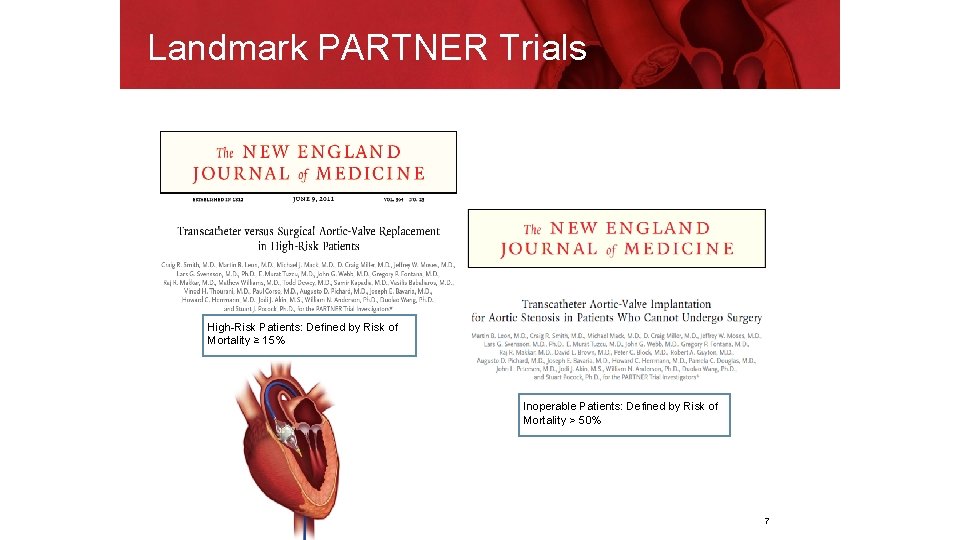
Landmark PARTNER Trials High-Risk Patients: Defined by Risk of Mortality ≥ 15% Inoperable Patients: Defined by Risk of Mortality > 50% 7
![Absolute Reduction in Mortality at 3 Year in Inoperable Patients HR 95 CI Absolute Reduction in Mortality at 3 Year in Inoperable Patients HR [95% CI] =](https://slidetodoc.com/presentation_image_h2/5f47794a3d58be8a417f272394570518/image-4.jpg)
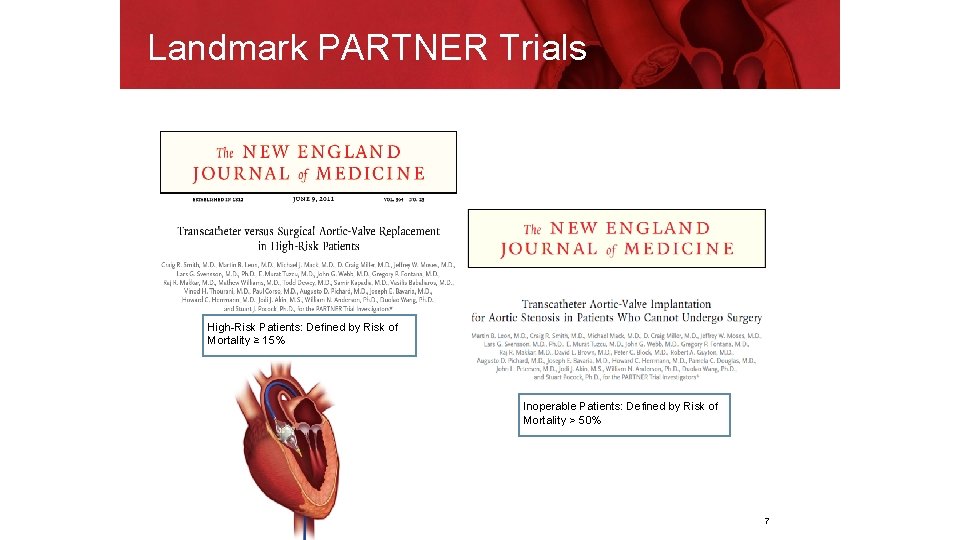
Absolute Reduction in Mortality at 3 Year in Inoperable Patients HR [95% CI] = 0. 53 [0. 41, 0. 68] p (log rank) < 0. 0001 Standard Rx 100% TAVR 80. 9% All Cause Mortality (%) 80% 68. 0% 26. 8% 50. 8% 60% 25. 0% 54. 1% 20. 1% 40% NNT = 3. 7 pts 43. 0% NNT = 4. 0 pts 30. 7% 20% NNT = 5. 0 pts 0% 0 6 12 18 24 30 36 Months Numbers at Risk Standard Rx 179 121 85 62 46 27 17 TAVR 138 124 110 101 88 70 179 8
![Reduction in Repeat Hospitalization in Inoperable Patients Rehospitalization 125 HR 95 CI 0 Reduction in Repeat Hospitalization in Inoperable Patients Rehospitalization 125% HR [95% CI] = 0.](https://slidetodoc.com/presentation_image_h2/5f47794a3d58be8a417f272394570518/image-5.jpg)
Reduction in Repeat Hospitalization in Inoperable Patients Rehospitalization 125% HR [95% CI] = 0. 39 [0. 28, 0. 54] p (log rank) < 0. 0001 Standard Rx TAVR Rehospitalization (%) 53. 9% 75% 26. 9 42. 3% 34. 9% 25% NNT = 3. 0 pts NNT = 2. 7 pts 27. 0% NNT = 3. 7 pts 6, 0000 Days Alive Out of Hospital Median [IQR] Numbers at Risk Standard Rx 179 TAVR 179 33. 4% 37. 6% 50% 0% 0, 0000 75. 7% 72. 5% 100% 86 115 12, 0000 18, 0000 24, 0000 30, 0000 36, 0000 Months TAVR 944 [233 - Standard Rx 368 [147 - p <. 0001 1096] 49 30 19 11 7 100 89 77 64 49 9
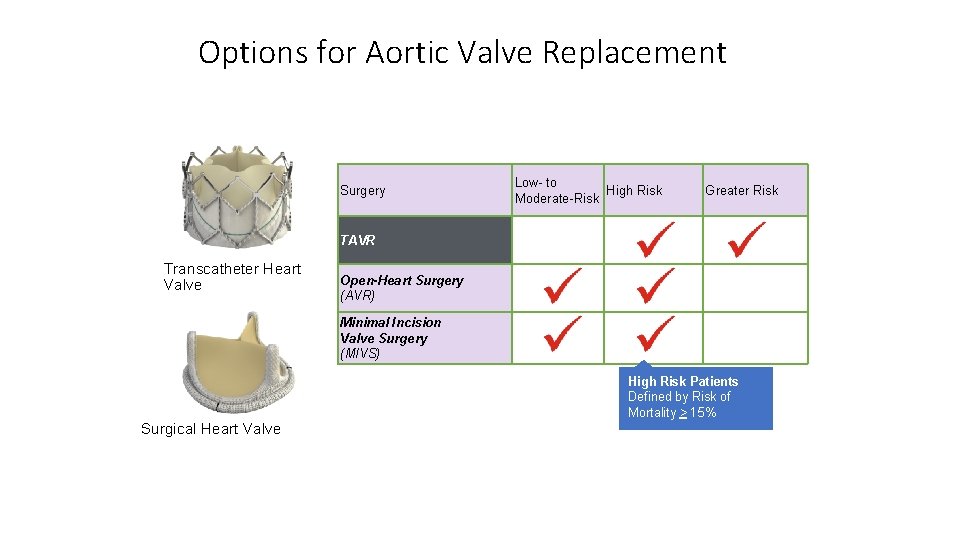
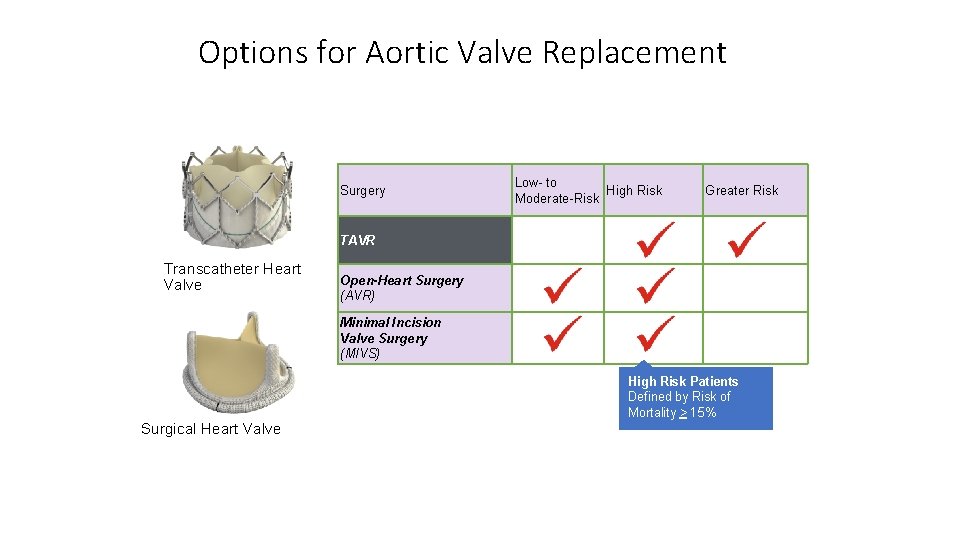
Options for Aortic Valve Replacement Surgery Low- to High Risk Moderate-Risk Greater Risk TAVR Transcatheter Heart Valve Open-Heart Surgery (AVR) Minimal Incision Valve Surgery (MIVS) High Risk Patients Defined by Risk of Mortality > 15% Surgical Heart Valve
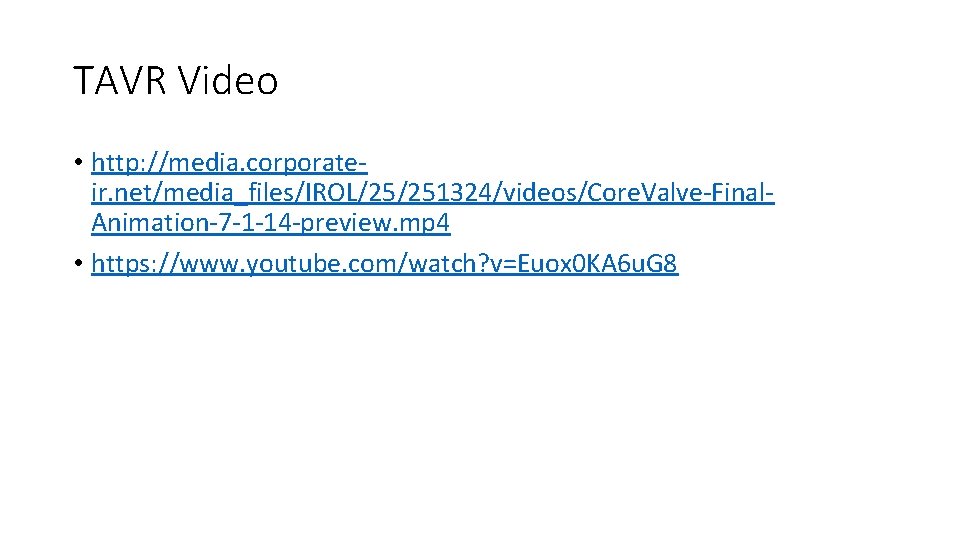
Access Routes for TAVR
TAVR Video • http: //media. corporateir. net/media_files/IROL/25/251324/videos/Core. Valve-Final. Animation-7 -1 -14 -preview. mp 4 • https: //www. youtube. com/watch? v=Euox 0 KA 6 u. G 8
TAVR Trials at SMH • SURTAVI - Intermediate Risk • Low Risk TAVR Trial
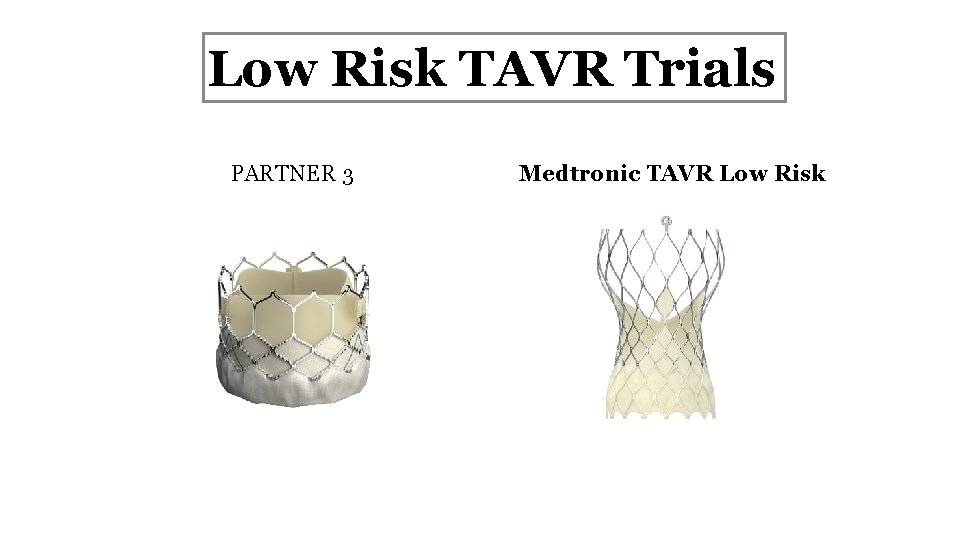
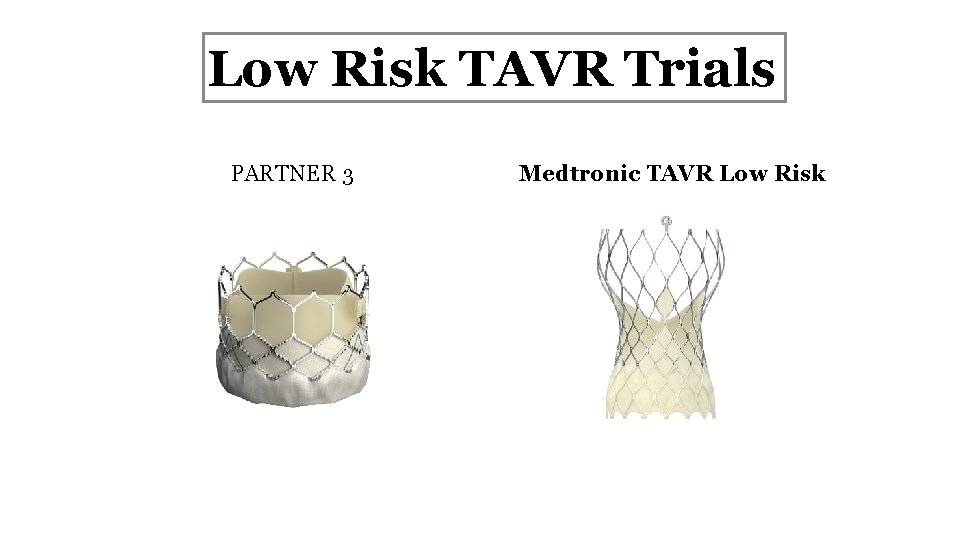
Low Risk TAVR Trials PARTNER 3 Medtronic TAVR Low Risk
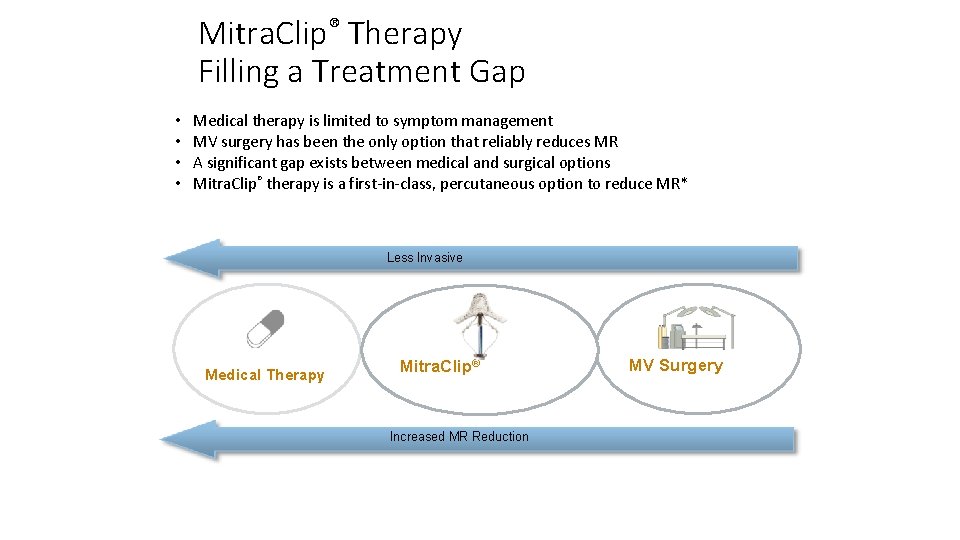
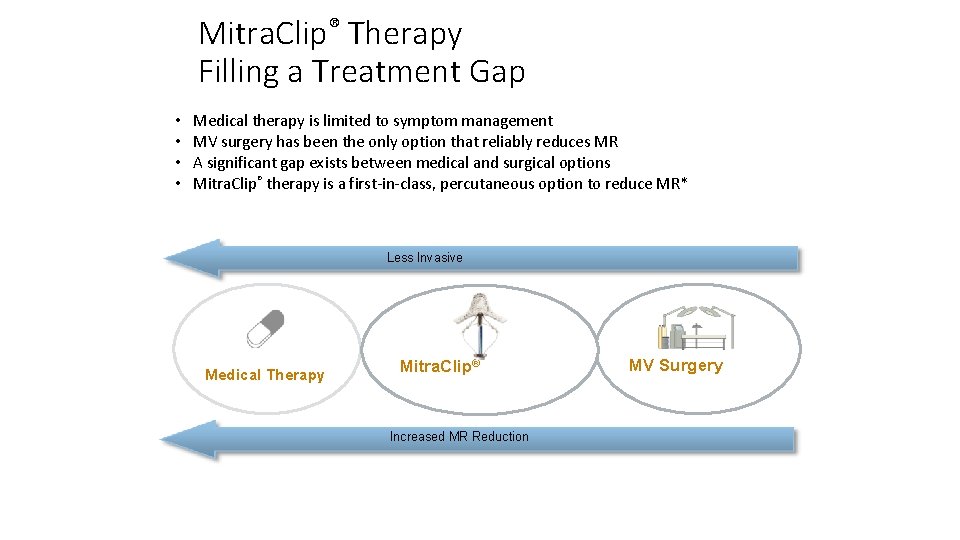
Mitra. Clip® Therapy Filling a Treatment Gap • • Medical therapy is limited to symptom management MV surgery has been the only option that reliably reduces MR A significant gap exists between medical and surgical options Mitra. Clip® therapy is a first-in-class, percutaneous option to reduce MR* Less Invasive Medical Therapy Mitra. Clip® Increased MR Reduction *Reference Source: Instructions For Use See important safety information referenced within MV Surgery
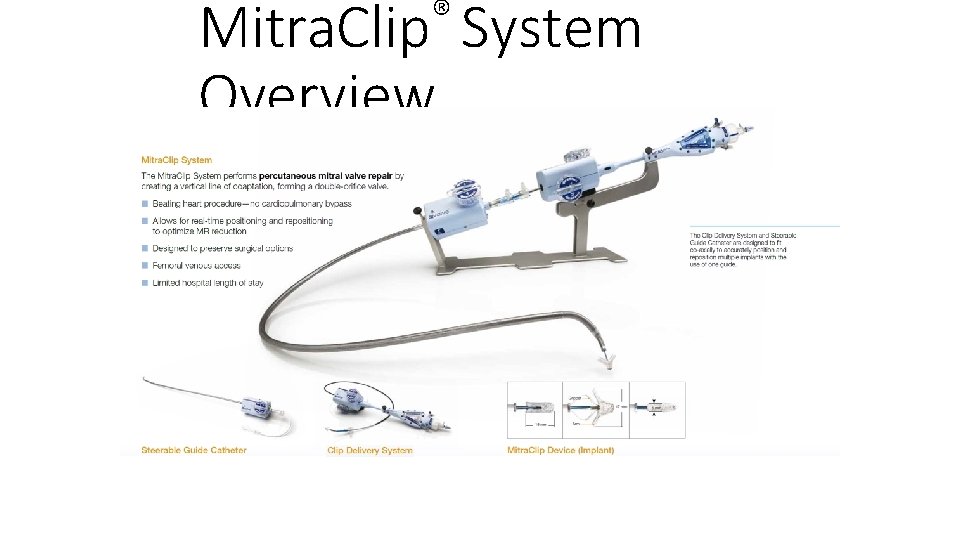
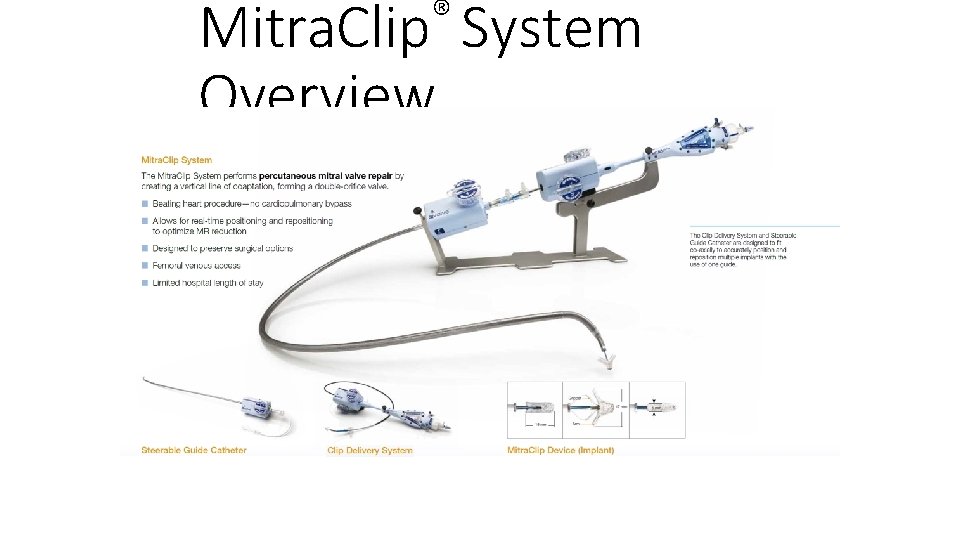
® Mitra. Clip System Overview