Risk Management Benefits Administration 101 By Scott Kramer

Risk Management Benefits Administration - 101 By: Scott Kramer
Benefit Types • Core Benefits (Employer Paid) • Health Care • Dental • Prescription Drugs • Vision • Mental Health • Life Insurance • Primary Care and Wellness Clinics

Benefit Types • Supplemental Benefits • Additional Life Insurance • Long Term Disability • Short Term Disability • Critical Care • Cancer Policies • Gap Policies • Hospital Confinement • Vision (it can be in both core & supplemental categories) • Gym/Fitness Clubs/YMCA subsidized memberships
Health Care Benefits • Understanding the Marketplace • Tiers of Coverage – Bronze (60%), Silver (70%), Gold (80%) & Platinum (90%) • Higher the metallic level = plan will pay more benefits, but higher premiums • Lower metallic level = plan will pay less benefits, but lower premiums • ACA – 10 essential benefits:
Health Care Benefits • Affordable Care Act – 10 essential benefits: • • • Outpatient services – physician’s office, outpatient surgery Emergency services Hospitalization Laboratory Services / Testing Maternity / Newborn care Mental Health & Addiction Treatment Rehabilitative Services – Occupational / Physical Therapy Pediatric Services for Infants and Children Prescription Drugs Preventive / Wellness Services – Physicals, Immunizations, Screenings
Health Care Benefits • Health Care - comprehensive plan • Covered / Non-covered expenses - Benefits applying to the item or service • Deductibles / Co-pays • Employer / Employee contributions • Retiree Benefits – under 65, over 65
Health Care Benefits • Have a Strategy • Controlling Costs • Traditional Plan vs Consumer Driven Plan
Benefits Financing • Fully Insured • Self Insured • Combination of Both • Employer Paid • Employee Paid • Combination of Both • One Vendor for All • Carved Out Among Different Vendors
Example of Traditional Plan Design Hospital Inpatient • $300 Deductible Per Admission • Additional $50 co-pay for Day 3 • Preadmission certification – Required for all admissions except maternity • Emergency admissions require notification within 48 hours of admission
Example of Traditional Plan Design (continued) Hospital Outpatient • Outpatient Hospital Visit: • Accidental Injury, no deductible; $100 copay • Surgery, no deductible; $150 copay • Diagnostic Lab / X-Rays, no deductible or copay • Medical emergency • no deductible; $150 copay for facility; $50 copay for physician • If determined Non-Medical Emergency, $200 deductible; 20% copay
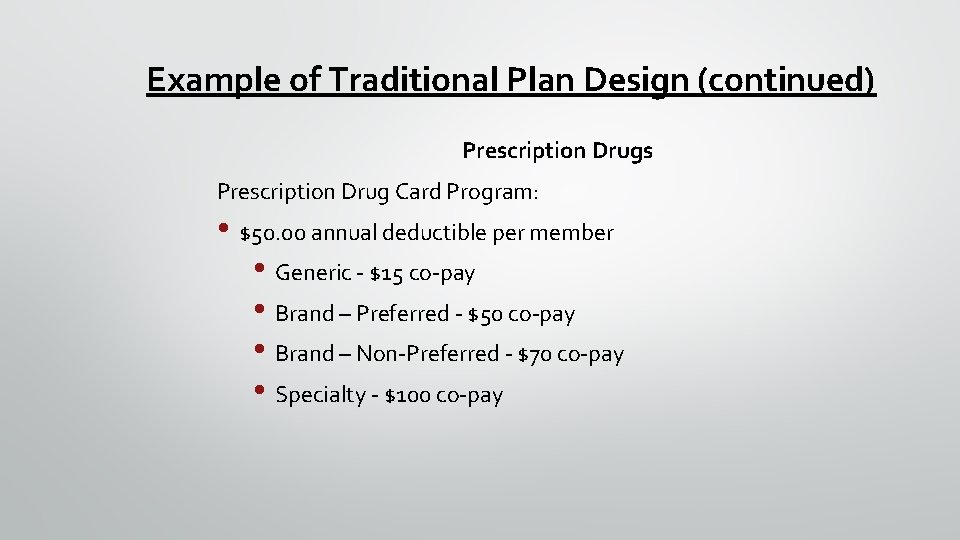
Example of Traditional Plan Design (continued) Prescription Drugs Prescription Drug Card Program: • $50. 00 annual deductible per member • Generic - $15 co-pay • Brand – Preferred - $50 co-pay • Brand – Non-Preferred - $70 co-pay • Specialty - $100 co-pay

Example of Traditional Plan Design (continued) Preferred Medical Doctor (PMD) • Services that are 100% covered • Diagnostic X-ray, lab pathology, surgery, second surgical opinion, anesthesia, chemotherapy, radiation therapy & maternity • Regular doctor visits are: • $35 co-pay – Primary Care • $50 co-pay - Specialists • Emergency Room Physician Fee $50 copay

Example of Traditional Plan Design (continued) Preferred Medical Doctor (PMD) Deductible - $300 calendar year 80% of covered expenses, until out-of-pocket maximum is met • • • Allergy Testing and Treatment Ambulance Services Dialysis Services Durable Medical Equipment (prosthetics, leg braces, etc. ) Occupational / Physical Therapy • Out of Pocket Max – Single - $1500 / Family - $3000
Definitions in Healthcare • Deductible • the amount of covered expenses that an individual pays for out-of-pocket before payments are made by the health plan • these are increasing in consumer driven plans
Definitions in Healthcare • Co-payments • Fixed dollar payments the patient makes for a doctor visit or prescription. • Examples include paying $10 for a generic prescription
Definitions in Healthcare • Coinsurance • the percentage of an insurance claim for which the patient is responsible for. • an example is the employee paying 10% of a hospital claim
Definitions in Healthcare • Dependent • An individual that a health insurance company covers under an individual’s health plan • Under ACA, an adult child that does not have access to health coverage from his or her employer may remain under the parent’s family plan until age 26.
Definitions in Healthcare • Chronic Conditions • A condition that lasts indefinitely or recurs frequently • Can be treated but not cured • The focus of most wellness programs to make an impact on costs • Examples include diabetes, hypertension and cholesterol
Definitions in Healthcare • Pharmacy Benefit Manager (PBM) • a third-party administrator (TPA) of prescription drug programs for health plans • PBMs are primarily responsible for developing and maintaining the formulary, contracting with pharmacies, negotiating discounts and rebates with drug manufacturers, and processing and paying prescription

Definitions in Healthcare • Formulary • The list of drugs covered fully or in part by a health plan • Some prescriptions may be excluded from the formulary, for example injectibles or men’s health prescriptions
Definitions in Healthcare • Out-of-pocket maximum or limit • A maximum limit on the out-of-pocket expenses a participant pays during the plan year. • These amounts include deductibles, co-payments or co-insurance and kept as a running total (excludes insurance premiums). • Once the participant reaches the plan’s limit for the year, remaining eligible expenses are covered at 100% regardless of the plan’s copayment or co-insurance arrangements.
Definitions in Healthcare • Life Event • A change in a participant’s personal situation that results in the gain or loss of eligibility for a health plan or a dependent’s health plan. • Examples of life events to be eligible to make changes to your benefit coverages include: • Marriage or Divorce, adoption or birth of child, death of a spouse or child, spouse’s loss of coverage, child’s loss of eligibility, change in employment status
Definitions in Healthcare • Certificate of Creditable coverage • evidence of prior coverage • provided by insurer once coverage ends • avoids a gap in care and limitations with preexisting conditions
Definitions in Healthcare • PPO – Preferred Provider Organization • An arrangement between doctors and other medical service providers and an insurer to offer services at a discounted rate in exchange for the insurer sending patients to their doctors or facilities.
Definitions in Healthcare • In-network provider • A health care provider (such as a hospital or doctor) contracted to be part of the network. • The provider agrees to the managed care organization’s rules and fee schedules in order to be part of the network and agrees not to balance bill patients for amounts beyond the agreed upon fee.
Definitions in Healthcare • In-network provider • A health care provider (such as a hospital or doctor) contracted to be part of the network. • The provider agrees to the managed care organization’s rules and fee schedules in order to be part of the network and agrees not to balance bill patients for amounts beyond the agreed upon fee.
Definitions in Healthcare • Consumer Driven (High Deductible) Health Plan • Includes a high deductible and higher out of pocket costs compared to the traditional health insurance plans • The purpose of these types of plans is to outline the real costs associated with medical care. • The premiums are generally lower than the traditional health insurance plans

Example of Consumer Driven Plan Design • Calendar Year Deductible • $1500 – Individual; $3000 – Family • Health Reimbursement Account – Individual Deductible • • • Employee responsible for first $250 County Plan responsible for next $750 Employee responsible for next $500 • Health Reimbursement Account – Family Deductible • • • Employee responsible for first $500 County Plan responsible for next $1500 Employee responsible for next $1000
Example of Consumer Driven Plan Design (continued) • Coinsurance • 80% covered by plan • 20% covered by individual • Out of Pocket Maximum • $3000 – Individual; $6000 – Family

Example of Consumer Driven Plan Design (continued) • Health Reimbursement Account – funded by County to offset some of the deductible costs • 1 st Layer in meeting deductible - Threshold amount – Employee • • • Family coverage - $500 2 nd Layer in meeting deductible - Health Reimbursement Account – County • • • Individual coverage - $250 Individual coverage - $750 Family Coverage - $1500 3 rd Layer in meeting deductible – Employee You can bank unused Health Reimbursement Account monies for one year After deductible is met, the employee will pay 20% of costs
Example of Consumer Driven Plan Design (continued) Prescription Drugs Prescription Drug Card Program: • $100. 00 annual deductible per member • • Generic - $15 co-pay Brand – Preferred - $50 co-pay Brand – Non-Preferred - $70 co-pay Specialty – 25% co-pay
Definitions in Healthcare • Rollover contribution • Distribution of an account balance from one financial institution and redepositing it in another, or from one type of account to another. • Examples include Health Reimbursement Accounts (HRA), Flexible Spending Accounts (FSA) and Health Savings Accounts (HSA).
Definitions in Healthcare • Exchange • A government regulated marketplace of insurance plans with different tiers or levels of coverage. • Offered to individuals without coverage or to small companies
Definitions in Healthcare • Flexible Spending Account (FSA) • An arrangement that allows employees to set aside pre-tax earnings to pay for benefits or expenses not paid by their insurance or benefit plans • Examples include deductibles and co-pays • Generally saves employees 25% of every dollar in the FSA

Definitions in Healthcare • Employee Assistance Program • A confidential employee benefit that covers all or part of the cost for employees to receive counseling, referrals, an advice in dealing with stressful life issues. • Examples of stressful life issues include, financial, parenting, caregiver and mental health
Definitions in Healthcare • Health Insurance Portability and Accountability ACT (HIPPA) • Limits the exclusion of pre-existing conditions • Permits special enrollment when certain life events occur • Prohibits discrimination against employees and dependents based on health status • Establishes strict standards for using and sharing private health information

Definitions in Healthcare • COBRA – Consolidated Omnibus Budget Reconciliation Act of 1985 • Provides temporary continuation of group health plan coverage after a qualifying event to certain employees and family members who are qualified beneficiaries • Cost is the 102% of the employer and employee contributions
Definitions in Healthcare • Medicare – health insurance program for 65 and older • Part A - pays for inpatient stays, care in a skilled nursing facility, hospice care and some health care (no premium cost). • Part B – helps pay for doctors’ services, outpatient hospital care, durable medical equipment and other medical services. • Part C – Medicare Advantage Plans provided through private insurance • Part D – stand alone prescription drug coverage insurance
Definitions in Healthcare • Medicare Part D “donut hole” • The gap between the maximum spending amount Medicare Part D will cover and the minimum spending amount to qualify for catastrophic prescription drug coverage. • The beneficiary is responsible for 100 percent of all costs between these amounts.
Definitions in Healthcare • Medicare supplement (Medigap) insurance • Private insurance that supplements Medicare and Medicare Advantage plans. • It reimburses out-of-pocket costs not covered by Medicare and that are the beneficiary’s share of health care costs.
Definitions in Healthcare • Home Health Care / Hospice Care • Home Health Care – skilled nursing and related care supplied to a patient at home. Many plans have limited coverage usually associated with discharge planning. • Hospice Care – care given to terminally ill patients, generally those with six months or less to live and that emphasizes meeting emotional needs and coping with pain. Care may be given in the patient’s home or at a facility.
General Exclusions in Healthcare Plans • Many items are generally exclude from health plans and these are identified in the summary plan document. Some examples include: • Cosmetic Surgery – procedures directed at improving the patient’s appearance, but does not prevent or treat illness or disease.
General Exclusions in Healthcare Plans (cont’d) • Nutritional Supplements – Vitamins, herbal supplements, natural medicines, etc. unless recommended by a medical practitioner as treatment for a specific medical condition diagnosed by a physician. • Over the counter medications- any biologicals, unless prescribed by a provider to treat a specific medical condition. • Long term care - a variety of services which help meet both the medical and non-medical needs of people with a chronic illness or disability who cannot care for themselves for long periods.
Primary Care and Wellness Clinics • Advantages • Healthier Population • Reduced costs • Health Risk Assessments • Disadvantages • Increased costs if not managed correctly.
Example of Controlling Cost With On-Site Clinic • Free Medical Care - No-copays or deductibles for acute care and chronic conditions • Limited (if any) waiting time • Voluntary Basis • Increased convenience and access • More on one time with the physician • Appointments are made through website or 1 -800 number • Webinars and Live Classes
Example of Wellness Programs • Discounted YMCA Memberships – with $20 contribution from the Employer • Exercise Classes – Free – After Work • Professional Trainer • At-Work Weight Watchers Classes • Discounted prices based on participation

Questions? ? Scott Kramer Autauga County Commission Administrator Scott. Kramer@Autauga. com (334) 358 -6701
- Slides: 47