Risk factors and antenatal suspicion for placenta previa
- Slides: 1
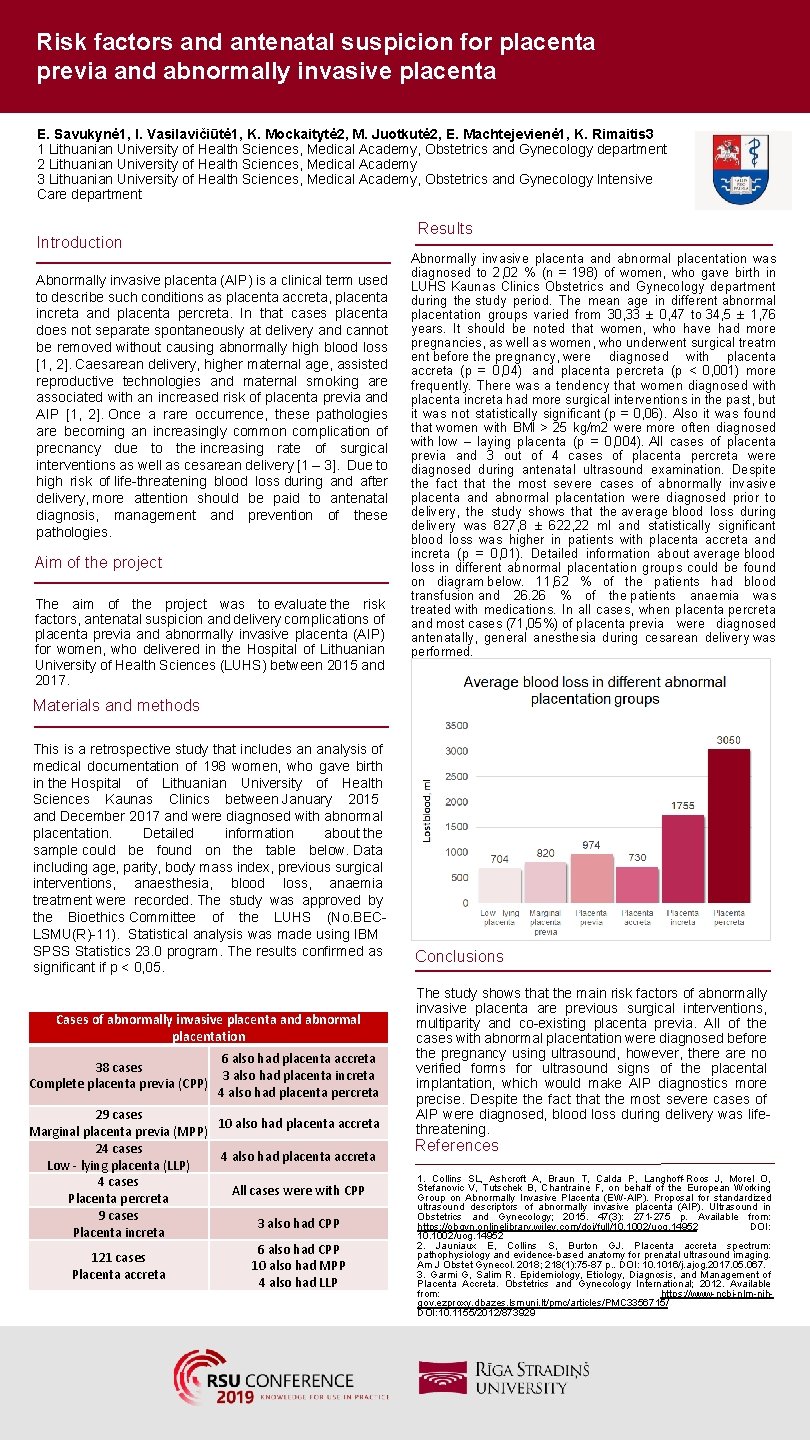
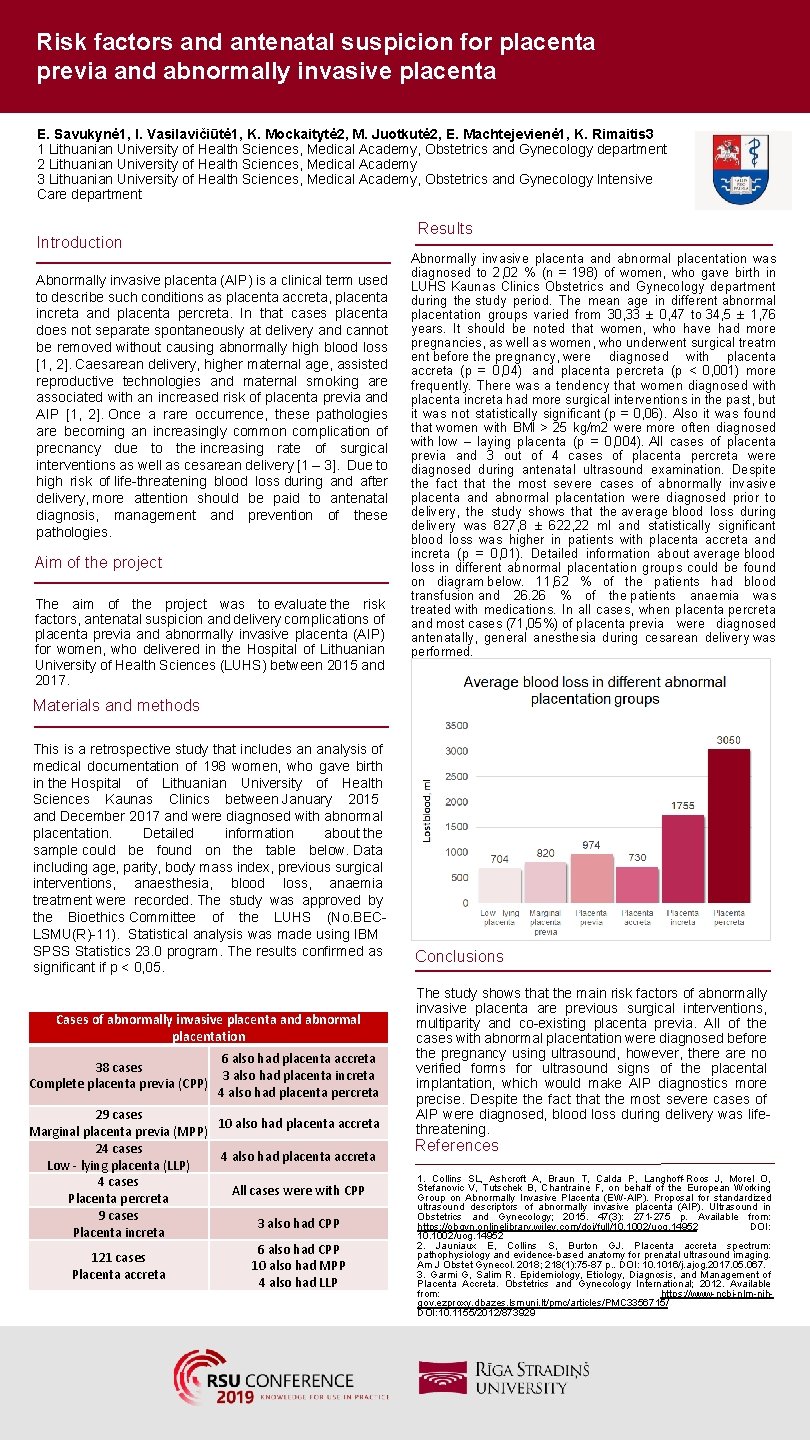
Risk factors and antenatal suspicion for placenta previa and abnormally invasive placenta E. Savukynė 1, I. Vasilavičiūtė 1, K. Mockaitytė 2, M. Juotkutė 2, E. Machtejevienė 1, K. Rimaitis 3 1 Lithuanian University of Health Sciences, Medical Academy, Obstetrics and Gynecology department 2 Lithuanian University of Health Sciences, Medical Academy 3 Lithuanian University of Health Sciences, Medical Academy, Obstetrics and Gynecology Intensive Care department Results Introduction Abnormally invasive placenta (AIP) is a clinical term used to describe such conditions as placenta accreta, placenta increta and placenta percreta. In that cases placenta does not separate spontaneously at delivery and cannot be removed without causing abnormally high blood loss [1, 2]. Caesarean delivery, higher maternal age, assisted reproductive technologies and maternal smoking are associated with an increased risk of placenta previa and AIP [1, 2]. Once a rare occurrence, these pathologies are becoming an increasingly common complication of precnancy due to the increasing rate of surgical interventions as well as cesarean delivery [1 – 3]. Due to high risk of life-threatening blood loss during and after delivery, more attention should be paid to antenatal diagnosis, management and prevention of these pathologies. Aim of the project The aim of the project was to evaluate the risk factors, antenatal suspicion and delivery complications of placenta previa and abnormally invasive placenta (AIP) for women, who delivered in the Hospital of Lithuanian University of Health Sciences (LUHS) between 2015 and 2017. Abnormally invasive placenta and abnormal placentation was diagnosed to 2, 02 % (n = 198) of women, who gave birth in LUHS Kaunas Clinics Obstetrics and Gynecology department during the study period. The mean age in different abnormal placentation groups varied from 30, 33 ± 0, 47 to 34, 5 ± 1, 76 years. It should be noted that women, who have had more pregnancies, as well as women, who underwent surgical treatm ent before the pregnancy, were diagnosed with placenta accreta (p = 0, 04) and placenta percreta (p < 0, 001) more frequently. There was a tendency that women diagnosed with placenta increta had more surgical interventions in the past, but it was not statistically significant (p = 0, 06). Also it was found that women with BMI > 25 kg/m 2 were more often diagnosed with low – laying placenta (p = 0, 004). All cases of placenta previa and 3 out of 4 cases of placenta percreta were diagnosed during antenatal ultrasound examination. Despite the fact that the most severe cases of abnormally invasive placenta and abnormal placentation were diagnosed prior to delivery, the study shows that the average blood loss during delivery was 827, 8 ± 622, 22 ml and statistically significant blood loss was higher in patients with placenta accreta and increta (p = 0, 01). Detailed information about average blood loss in different abnormal placentation groups could be found on diagram below. 11, 62 % of the patients had blood transfusion and 26. 26 % of the patients anaemia was treated with medications. In all cases, when placenta percreta and most cases (71, 05%) of placenta previa were diagnosed antenatally, general anesthesia during cesarean delivery was performed. Materials and methods This is a retrospective study that includes an analysis of medical documentation of 198 women, who gave birth in the Hospital of Lithuanian University of Health Sciences Kaunas Clinics between January 2015 and December 2017 and were diagnosed with abnormal placentation. Detailed information about the sample could be found on the table below. Data including age, parity, body mass index, previous surgical interventions, anaesthesia, blood loss, anaemia treatment were recorded. The study was approved by the Bioethics Committee of the LUHS (No. BECLSMU(R)-11). Statistical analysis was made using IBM SPSS Statistics 23. 0 program. The results confirmed as significant if p < 0, 05. Cases of abnormally invasive placenta and abnormal placentation 38 cases Complete placenta previa (CPP) 6 also had placenta accreta 3 also had placenta increta 4 also had placenta percreta 29 cases 10 also had placenta accreta Marginal placenta previa (MPP) 24 cases 4 also had placenta accreta Low - lying placenta (LLP) 4 cases All cases were with CPP Placenta percreta 9 cases 3 also had CPP Placenta increta 6 also had CPP 121 cases 10 also had MPP Placenta accreta 4 also had LLP Conclusions The study shows that the main risk factors of abnormally invasive placenta are previous surgical interventions, multiparity and co-existing placenta previa. All of the cases with abnormal placentation were diagnosed before the pregnancy using ultrasound, however, there are no verified forms for ultrasound signs of the placental implantation, which would make AIP diagnostics more precise. Despite the fact that the most severe cases of AIP were diagnosed, blood loss during delivery was lifethreatening. References 1. Collins SL, Ashcroft A, Braun T, Calda P, Langhoff-Roos J, Morel O, Stefanovic V, Tutschek B, Chantraine F, on behalf of the European Working Group on Abnormally Invasive Placenta (EW-AIP). Proposal for standardized ultrasound descriptors of abnormally invasive placenta (AIP). Ultrasound in Obstetrics and Gynecology; 2015. 47(3): 271 -275 p. Available from: https: //obgyn. onlinelibrary. wiley. com/doi/full/10. 1002/uog. 14952 DOI: 10. 1002/uog. 14952 2. Jauniaux E, Collins S, Burton GJ. Placenta accreta spectrum: pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am J Obstet Gynecol. 2018; 218(1): 75 -87 p. . DOI: 10. 1016/j. ajog. 2017. 05. 067. 3. Garmi G, Salim R. Epidemiology, Etiology, Diagnosis, and Management of Placenta Accreta. Obstetrics and Gynecology International; 2012. Available from: https: //www-ncbi-nlm-nihgov. ezproxy. dbazes. lsmuni. lt/pmc/articles/PMC 3356715/ DOI: 10. 1155/2012/873929