RISK AND CRISIS MANAGEMENT IN INTRAOPERATIVE HEMORRHAGE Review
- Slides: 31
RISK AND CRISIS MANAGEMENT IN INTRAOPERATIVE HEMORRHAGE 가톨릭대학교 의과대학 마취통증의학과교실 서울성모병원 이재민
• Review article of KJA by Kazuo Irita - in press • Jpn J Anesth (Masui) 2009; 58: 109 -23 - present status of preparatory measure for massive hemorrhage • Acta Anaesthesiol Scand 2010; 54: 1039 -49 - management of major blood loss: an update • Br J Haematol 2006; 135: 634 -41 - British committee for standards in haematology - guidelines on the management of massive blood loss • Anesthesiology 2009; 111: 327 -33 - moderate exposure to allogenic blood product is not associated with reduced long-term survival after surgery for coronary artery disease
• JSA survey of JSA-certified training hospital - from 2004 to 2008 - n = 5, 235, 940 anesthetics - cardiac arrest 4. 38/10, 000 - death within 30 postoperative days 6. 85/10, 000 - hemorrhage was responsible for 33% of cardiac arrest 47% of death No. 1 killer in the operating room is hemorrhage!!
Each surgeon and each anesthesiologist are partly responsible for critical hemorrhage. 1. How can we prevent critical hemorrhage? 2. How can we deal with those cases caused by surgical procedures in particular?
1. Critical hemorrhage 1 -1. rapid loss of large amount of blood 1 -2. human factors affecting hemorrhagic critical events 1 -3. emergency or massive transfusion practices: present status 1 -4. hemolytic reactions due to emergency transfusion practices 2. Crisis management 2 -1. declaration of emergency 2 -2. blood transfusion 2 -3. surgical procedures 2 -4. establishment of hospital actions 2 -5 centralization
1. Critical Hemorrhage 1 -1. rapid loss of large amount of blood • Definition of massive hemorrhage (volume, speed) (i) blood loss exceeding circulating blood volume within 24 -hour period (ii) blood loss of 50% circulating blood volume within 3 -hour period (iii) blood loss exceeding 150 ml/min (iv) blood loss that necessitates plasma and platelet transfusion no universal definition!
1. Critical Hemorrhage 1 -1. rapid loss of large amount of blood • Survey concerning critical hemorrhage caused by surgical procedures - conducted by JSA, from 2003 to 2005 - n = 1, 105 - 37% of patients had blood loss of less than one circulating blood volume - 49% of patients had blood loss less than 120 ml/min ★ blood loss that does not meet a general definition of massive hemorrhage can threaten patients in the OR. ★ some factors other than the volume or the speed of blood loss threatened surgical patients.
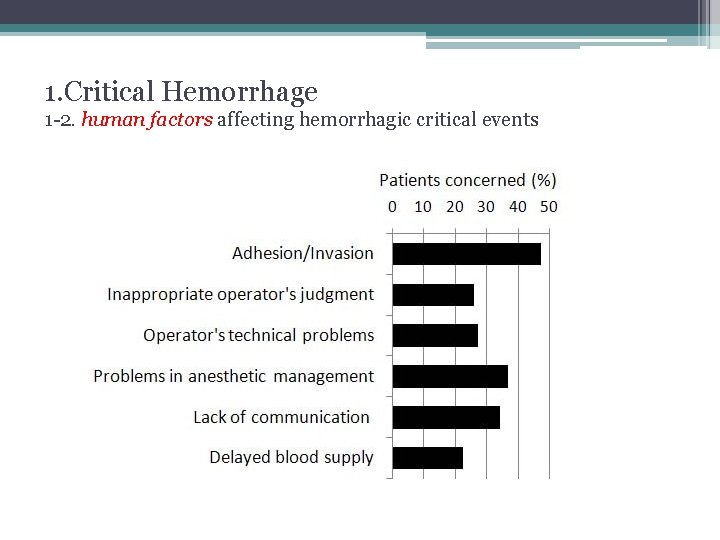
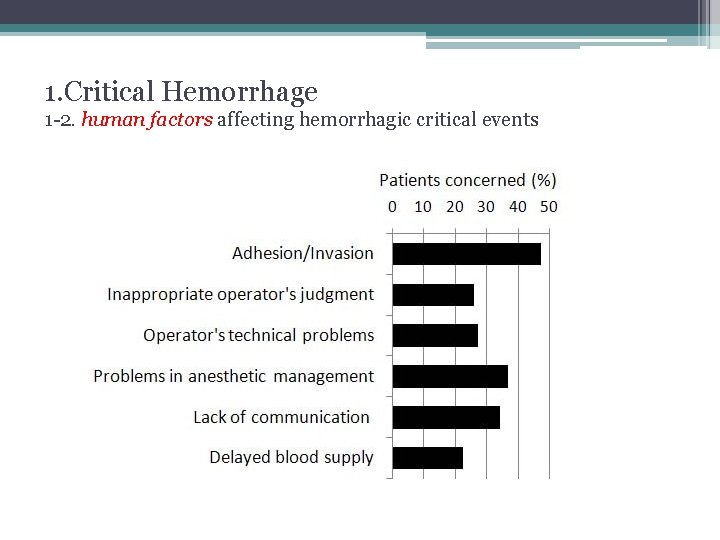
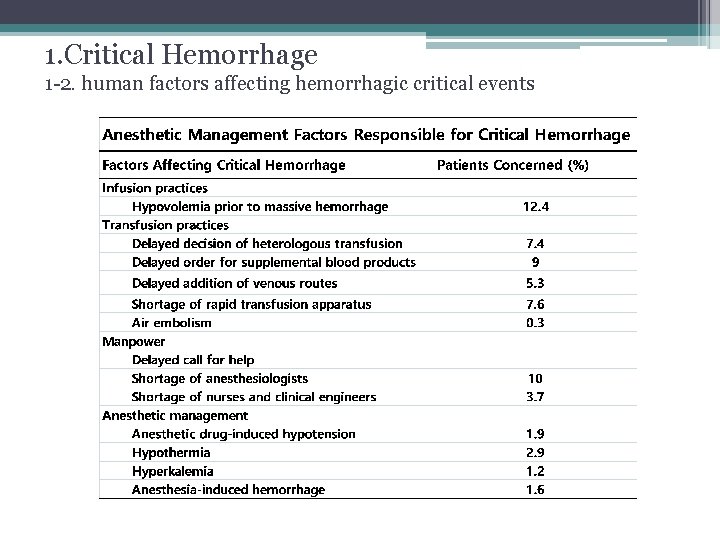
1. Critical Hemorrhage 1 -2. human factors affecting hemorrhagic critical events
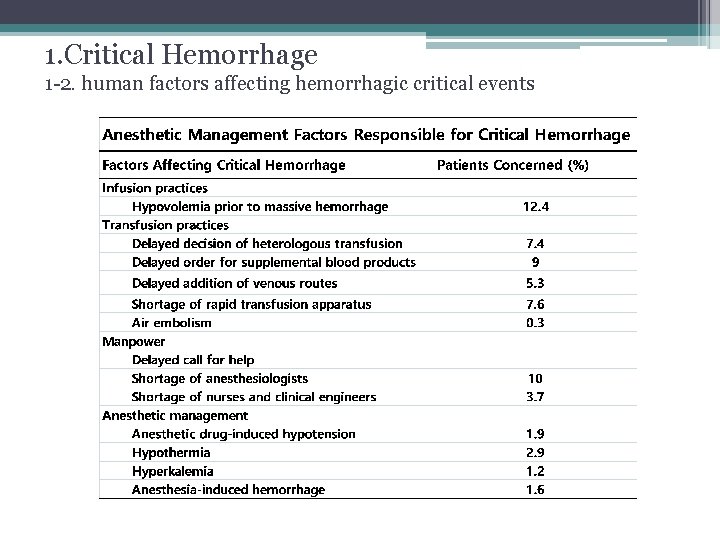
1. Critical Hemorrhage 1 -2. human factors affecting hemorrhagic critical events
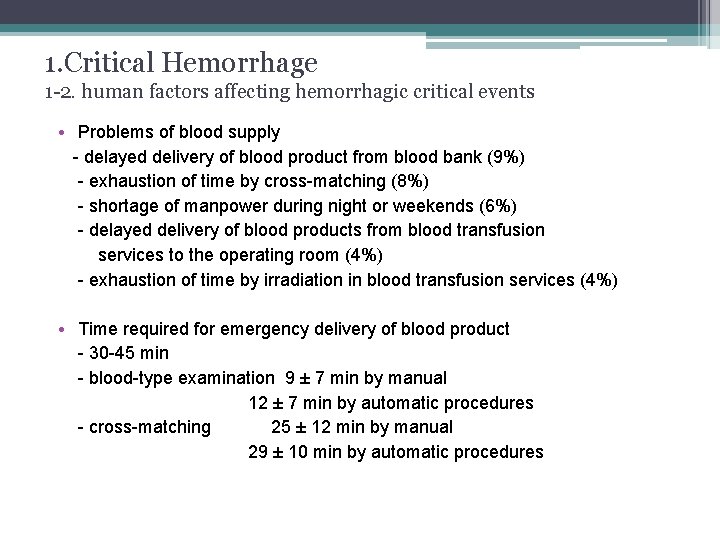
1. Critical Hemorrhage 1 -2. human factors affecting hemorrhagic critical events • Problems of blood supply - delayed delivery of blood product from blood bank (9%) - exhaustion of time by cross-matching (8%) - shortage of manpower during night or weekends (6%) - delayed delivery of blood products from blood transfusion services to the operating room (4%) - exhaustion of time by irradiation in blood transfusion services (4%) • Time required for emergency delivery of blood product - 30 -45 min - blood-type examination 9 ± 7 min by manual 12 ± 7 min by automatic procedures - cross-matching 25 ± 12 min by manual 29 ± 10 min by automatic procedures
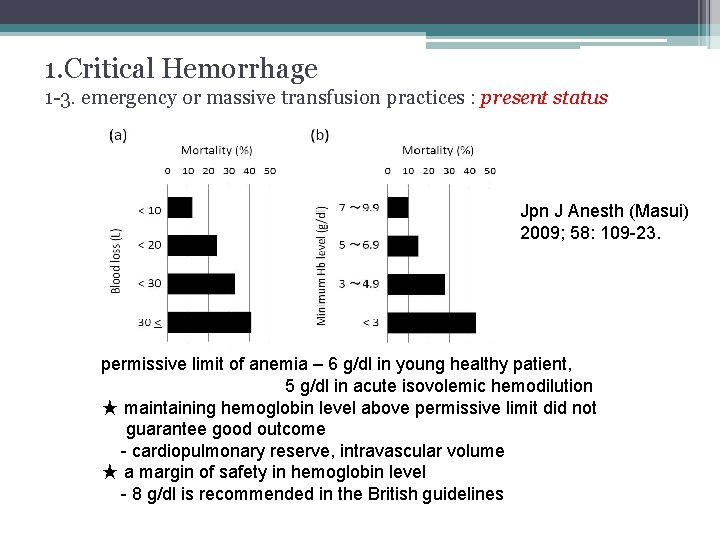
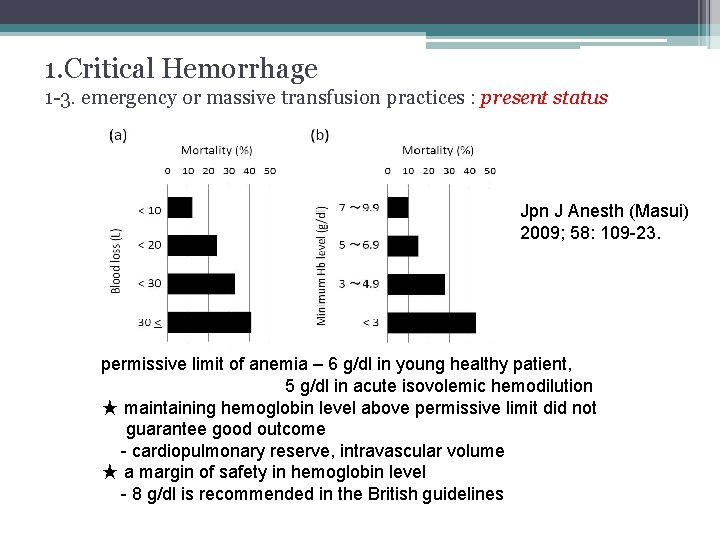
1. Critical Hemorrhage 1 -3. emergency or massive transfusion practices : present status Jpn J Anesth (Masui) 2009; 58: 109 -23. permissive limit of anemia – 6 g/dl in young healthy patient, 5 g/dl in acute isovolemic hemodilution ★ maintaining hemoglobin level above permissive limit did not guarantee good outcome - cardiopulmonary reserve, intravascular volume ★ a margin of safety in hemoglobin level - 8 g/dl is recommended in the British guidelines
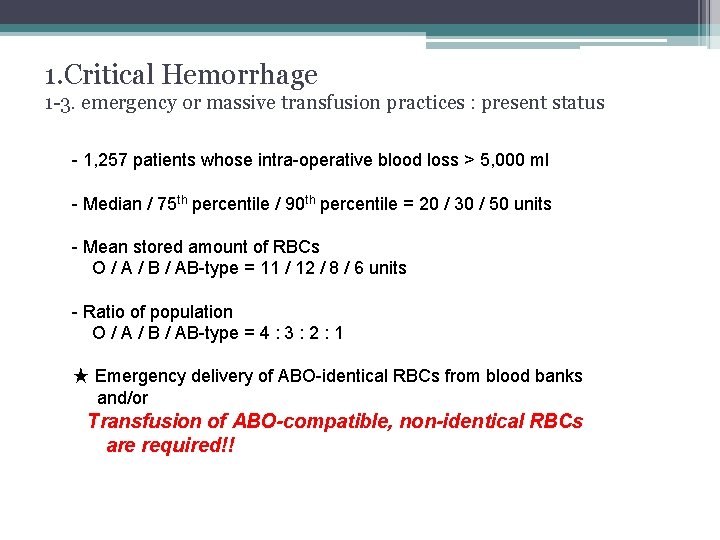
1. Critical Hemorrhage 1 -3. emergency or massive transfusion practices : present status - 1, 257 patients whose intra-operative blood loss > 5, 000 ml - Median / 75 th percentile / 90 th percentile = 20 / 30 / 50 units - Mean stored amount of RBCs O / A / B / AB-type = 11 / 12 / 8 / 6 units - Ratio of population O / A / B / AB-type = 4 : 3 : 2 : 1 ★ Emergency delivery of ABO-identical RBCs from blood banks and/or Transfusion of ABO-compatible, non-identical RBCs are required!!
1. Critical Hemorrhage 1 -3. emergency or massive transfusion practices : present status 2, 597 patients with peri-op blood loss > 5, 000 ml, other than O-type overall mortality 19% uncross-matched ABO-identical 9% ABO-compatible, non-identical RBCs 1. 7% 407 patients whose minimum Hb < 5 g/dl overall mortality 37% uncross-matched ABO-identical 20% ABO-compatible, non-identical RBCs 5. 4% 164 patients who required cardiac massage in OR overall mortality 73% uncross-matched ABO-identical 20% ABO-compatible, non-identical RBCs 7. 9%
1. Critical Hemorrhage 1 -4. hemolytic reactions due to emergency transfusion practices • What disturb emergency blood transfusion practice in OR? - ‘ 2009 4 th edition of guidelines by Ministry of Health, Labor, and Welfare - “ABO-compatible, non-identical RBCs are permitted in exceptional circumstances. ” • What is the level of safety of uncross-matched, ABO-compatible, non-identical RBC transfusion? - if no Ab. screening test, hemolytic reaction by irregular Ab. is 0. 5% (anti-Rh. E, anti-Fya&b, anti-Jka&b Ab) by Rh. D negative is 0. 5% - Vietnam War, 100. 419 units of emergency O-type RBC transfusion no lethal complications - same period, cross-matched or type-specific blood 24 lethal hemolytic reactions owing to clerical error.
1. Critical Hemorrhage 1 -4. hemolytic reactions due to emergency transfusion practices - civilian trauma, 790 patients, 2, 041 units of uncross-matched, O-type RBCs safe! i) immunosuppression associated with massive hemorrhage or shock ii) transfused RBCs are lost so rapidly that they cannot induce immune reaction (Dutton et al. ’s study, J Trauma, 2005; 59: 1445 -9. ) ★ Mortality rate is 19% when blood loss > 5, 000 ml ∴ Risk-benefit analysis shows … there is no rationale to abandon emergency transfusion practice to avoid associated complications.
2. Critical Management 2 -1. declaration of emergency ☞ Disaster medicine C S C A T T T ☞ Bleeding patient in the OR command declare safety →→→ S safety of a bleeding patient communication assessment triage treatment transport →→→ T transport of blood product from blood bank to hospital • Major problems underlying disaster medicine - hesitation to declare an emergency! 늑장대처!!
2. Critical Management 2 -1. declaration of emergency • A “commander” needs to be appointed - senior physicians of the anesthesiology department • The first task of the commander - medical assessment of the hemodynamic status - (most likely course of ongoing bleeding) - declare an emergency!
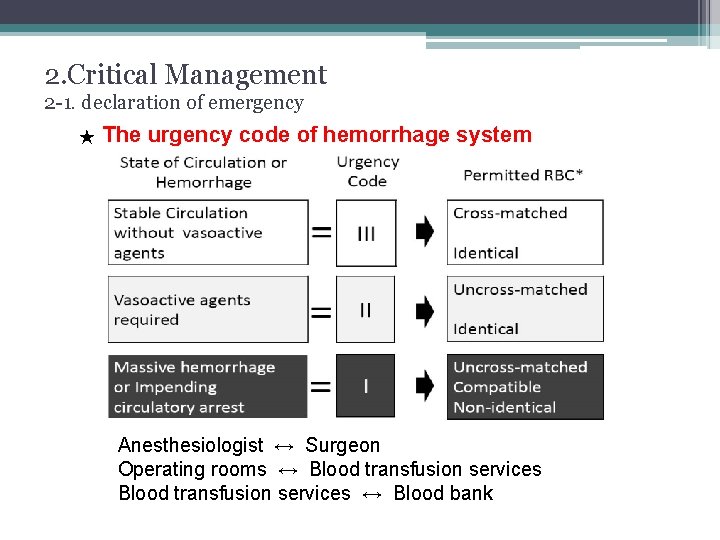
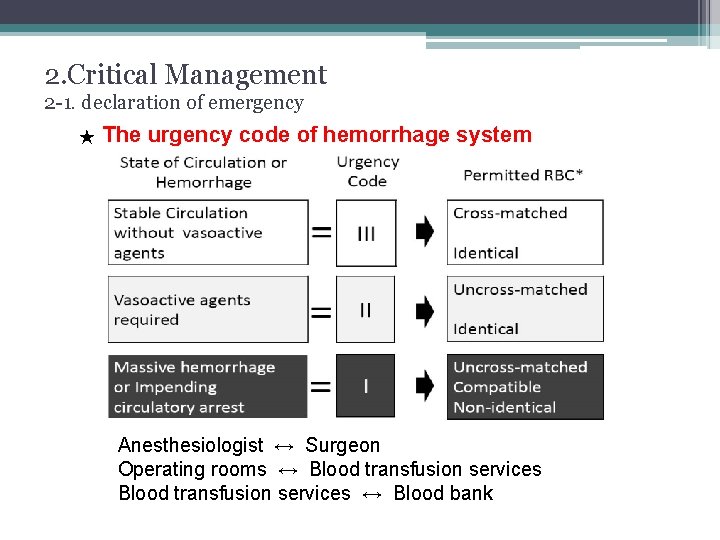
2. Critical Management 2 -1. declaration of emergency ★ The urgency code of hemorrhage system Anesthesiologist ↔ Surgeon Operating rooms ↔ Blood transfusion services ↔ Blood bank
2. Critical Management 2 -1. declaration of emergency Professional pride Fear of criticism of calling many staff unnecessarily Escape from the difficult situation → indecision of declaring code I None of these is acceptable! Survival of the patient has to be prioritized!!
2. Critical Management 2 -1. declaration of emergency • Role of the “commander” - declaration of an emergency - assess hemodynamics, test data, hemostatic condition of patient - assess blood product supply system - consult the surgeon continuation of planned surgery change of surgical procedure • Virtue of the “commander” - prompt decision-making - concrete as well as concise instructions - following the algorithm - watching for violations by medical staff - confirmation of exact time recording - cancel an emergency - offer an opportunity to evaluate the validity of the responses later
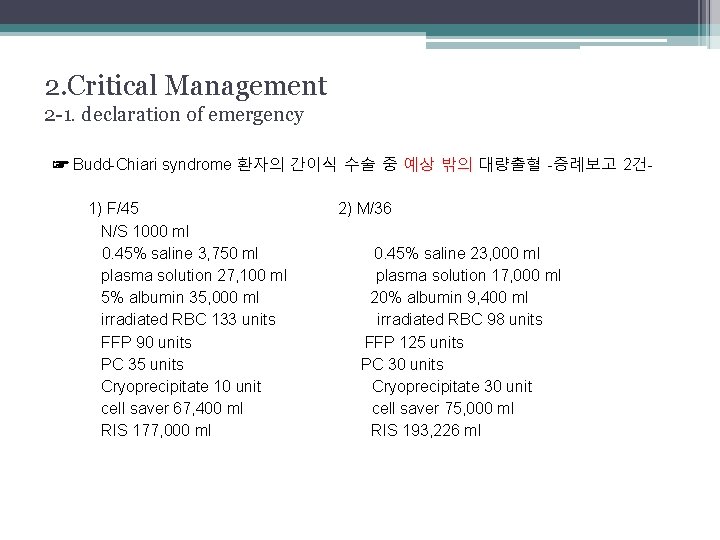
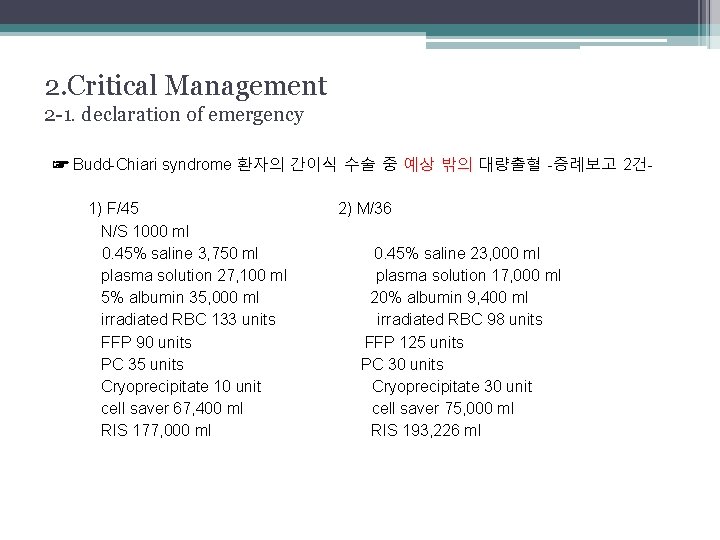
2. Critical Management 2 -1. declaration of emergency ☞ Budd-Chiari syndrome 환자의 간이식 수술 중 예상 밖의 대량출혈 -증례보고 2건 1) F/45 N/S 1000 ml 0. 45% saline 3, 750 ml plasma solution 27, 100 ml 5% albumin 35, 000 ml irradiated RBC 133 units FFP 90 units PC 35 units Cryoprecipitate 10 unit cell saver 67, 400 ml RIS 177, 000 ml 2) M/36 0. 45% saline 23, 000 ml plasma solution 17, 000 ml 20% albumin 9, 400 ml irradiated RBC 98 units FFP 125 units PC 30 units Cryoprecipitate 30 unit cell saver 75, 000 ml RIS 193, 226 ml
2. Critical Management 2 -2. blood transfusion • RBC salvage (cell saver) - transfusion of autologous blood recovered from the surgical field - can minimize allogenic RBC transfusion - contraindication (? ) during resection of malignant tumor may cause dissemination of malignancy recommended to avoid hemorrhagic death - contraindication (? ) during C/S presence of fetal RBCs, fetal skin surface cells, amniotic fluid ASA recommend RBC salvage in an hemorrhagic C/S should be considered after the delivery of fetus and placenta - absolute contraindication is wound contamination
2. Critical Management 2 -2. blood transfusion • Irradiation - post-transfusion graft-versus-host disease is lethal - mandatory for RBCs and PC - blood transfusion service should start irradiation before OR orders supplemental blood products • Fresh Frozen Plasma (FFP) - acute endogenous coagulopathy develops before coagulation factor depletion in the presence of tissue hypoperfusion (Chest 2010) - general indication to transfuse FFP loss of more than one circulating blood volume PT-INR > 2. 0 - British Guideline (Br J Haematol 2006) therapeutic target of PT-INR < 1. 5 consider FFP without PT-INR examination
2. Critical Management 2 -2. blood transfusion • Platelet Concentrate (PC) - general indication to transfuse PC platelet count < 50, 000/mm 3 blood loss > 1. 5 Ⅹ blood volume - British guideline platelet count should be targeted > 75, 000/mm 3 - 10 units of PC → increase the count by about 25, 000/mm 3 • Proactive administration of plasma and platelets - 1 : 1 ratio of RBC : FFP : PC improves survival rates in massive hemorrhage in military and civilian trauma - early identification and management of coagulopathy → better control hemorrhage, reduce hemorrhagic mortality - compatible, non-identical FFP and PC is possible
2. Critical Management 2 -3. surgical procedures • Discuss and Decide Surgical Procedures - accomplishment of scheduled procedures - change to the minimum procedures - bimanual compression of the bleeding point - temporary packing - clamps of the artery or the aorta - damage control surgery
2. Critical Management 2 -4. establishment of hospital actions • “Hospital Transfusion Committee” “Hospital regulations” on actions to be taken against critical bleeding ☞ Establishing hospital actions enables a strong hospital against critical hemorrhage!!
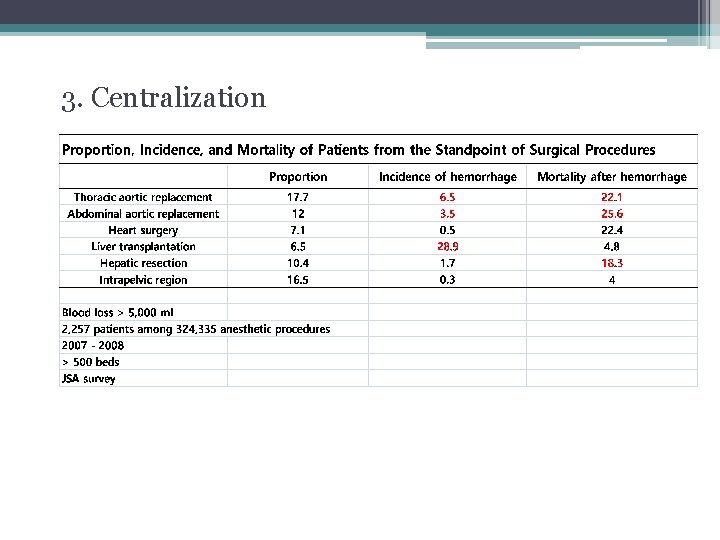
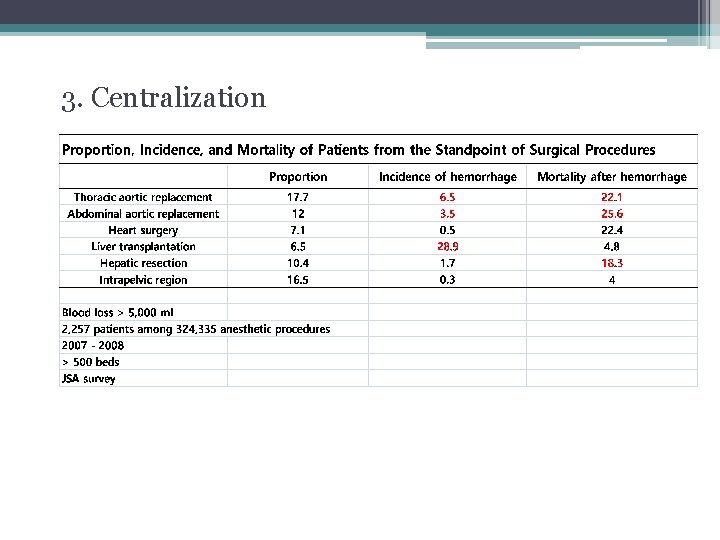
3. Centralization
Summary • Many human factors are involved in the development of hemorrhage into critical events. • Transfusion of ABO-compatible, non-identical RBCs are required!! • Hemorrhagic mortality and morbidity in the operating room can be reduced by a systemic, not an individual approach. • Establishment of hospital actions must be taken.
Thank you !!