RI Asthma Control Program Comprehensive Asthma Care Julian
- Slides: 29
RI Asthma Control Program: Comprehensive Asthma Care Julian Rodriguez-Drix Program Manager
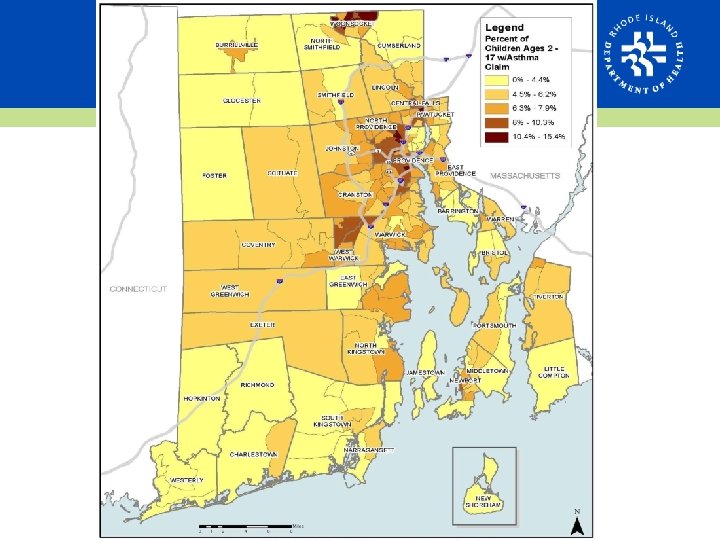
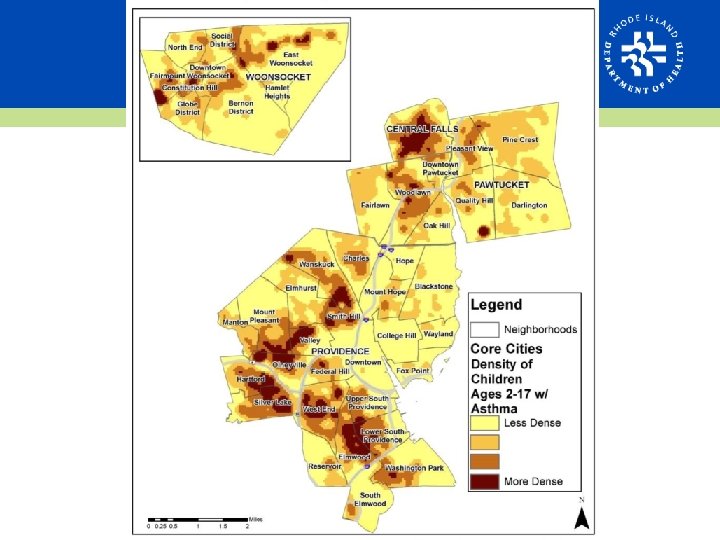
ASTHMA • An estimated 112, 000 people in RI currently have asthma. • Adults: 15. 9% lifetime, 10. 8% current • Pediatric: 13. 1% lifetime, 9. 1% current • Cause and control related to indoor and outdoor environment • Disparities based on age, race, and income
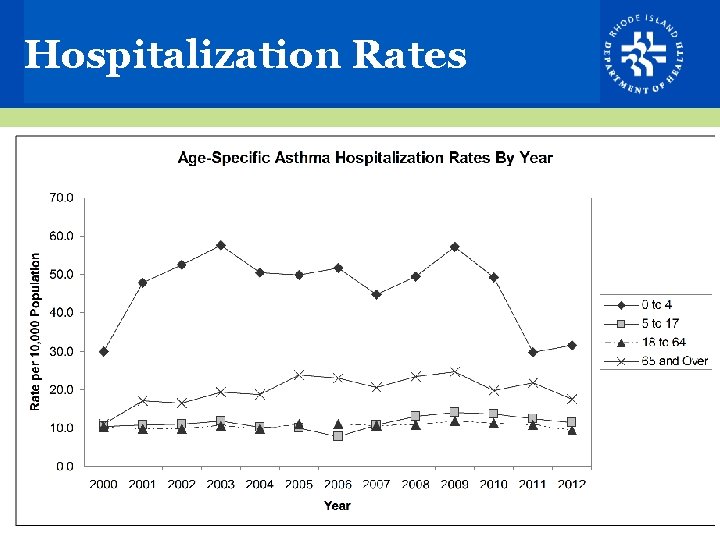
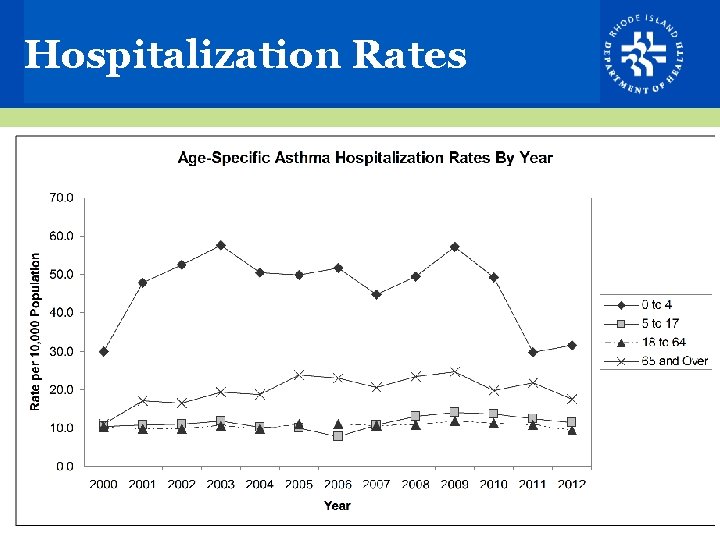
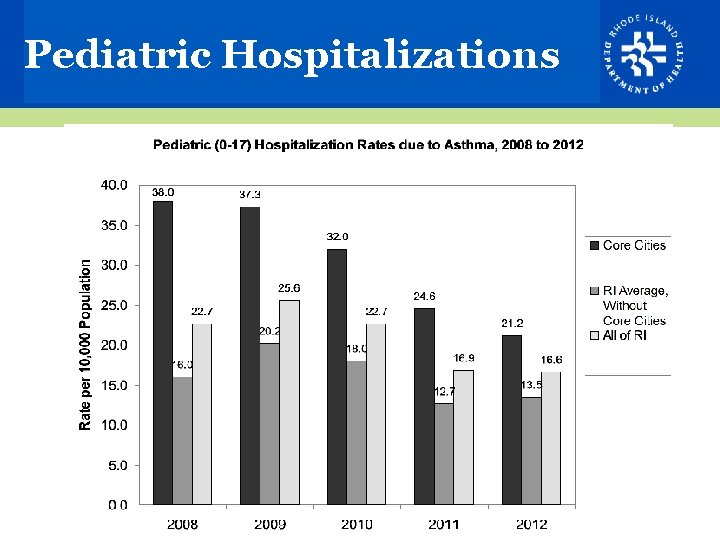
Hospitalization Rates
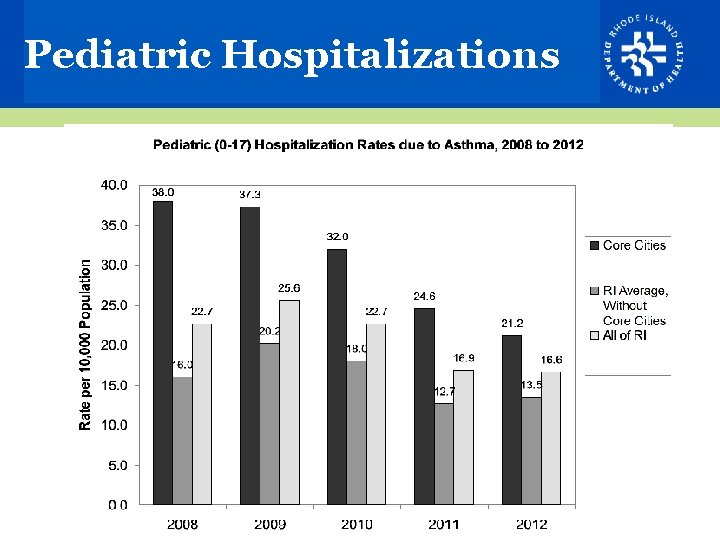
Pediatric Hospitalizations
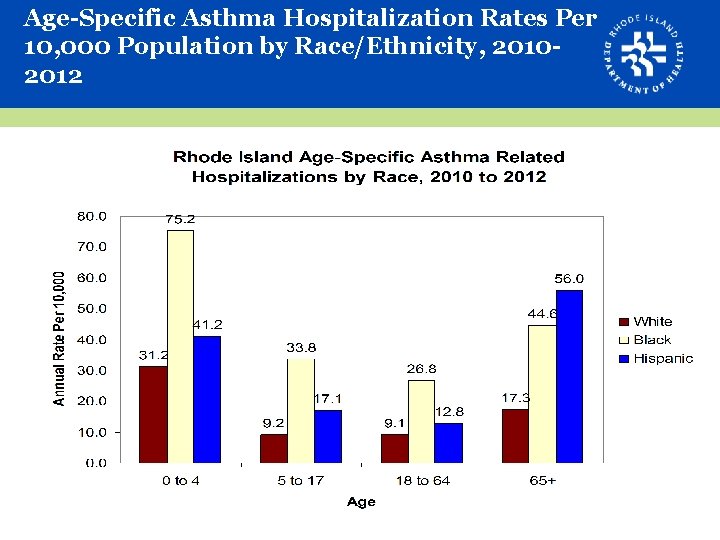
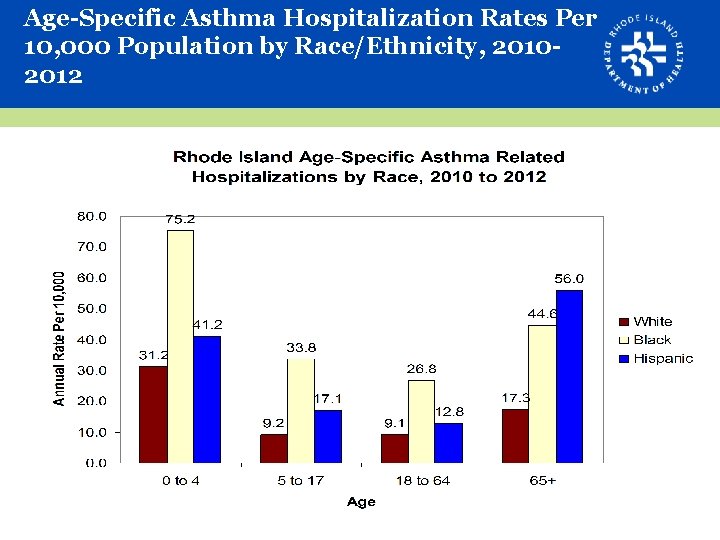
Age-Specific Asthma Hospitalization Rates Per 10, 000 Population by Race/Ethnicity, 20102012
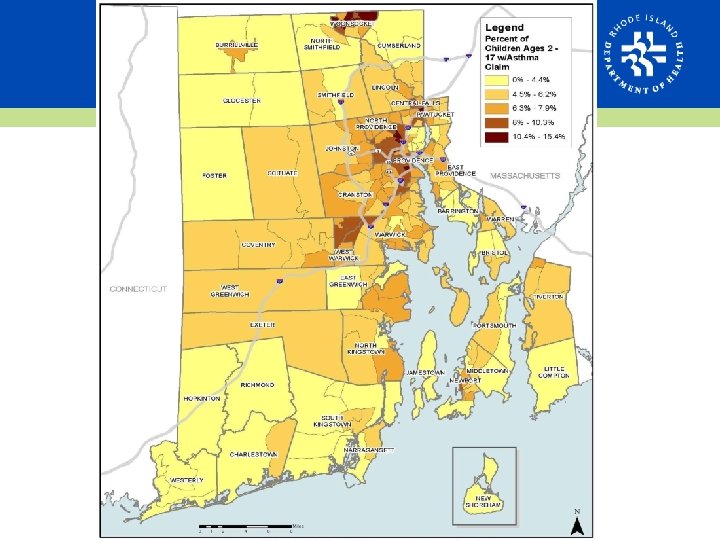
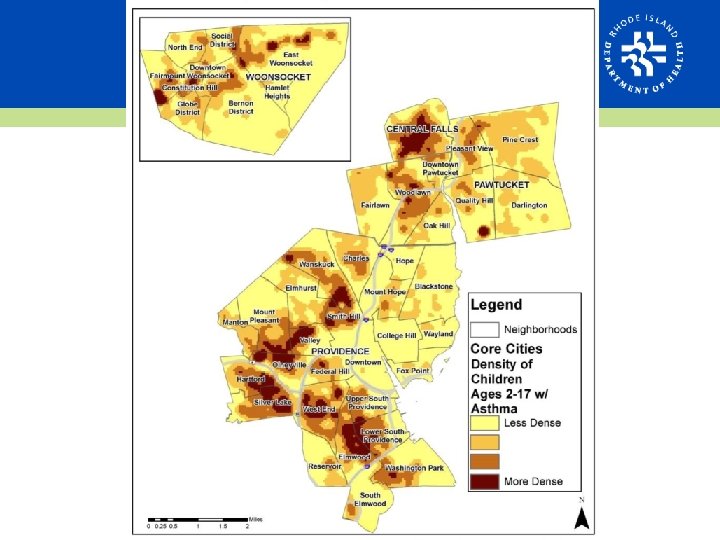
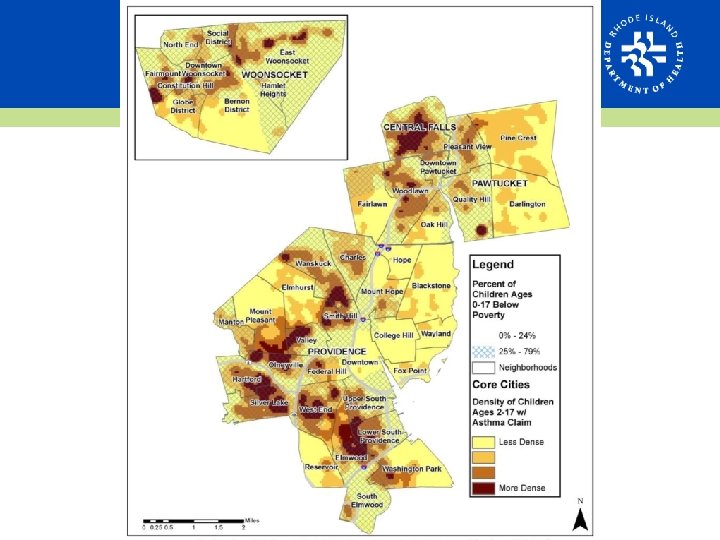
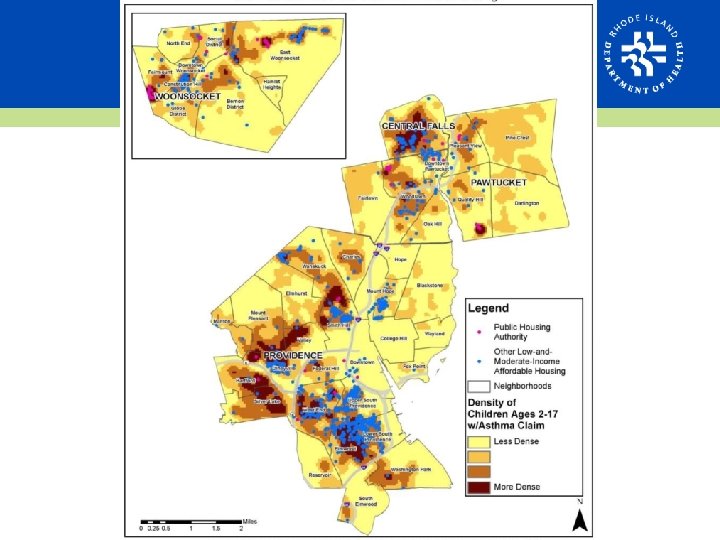
Asthma and Poverty • Asthma prevalence significantly higher in adults with an annual income less than $25, 000 • The highest rates of poverty in RI cluster in urban areas • Highest childhood poverty rates up to 79%
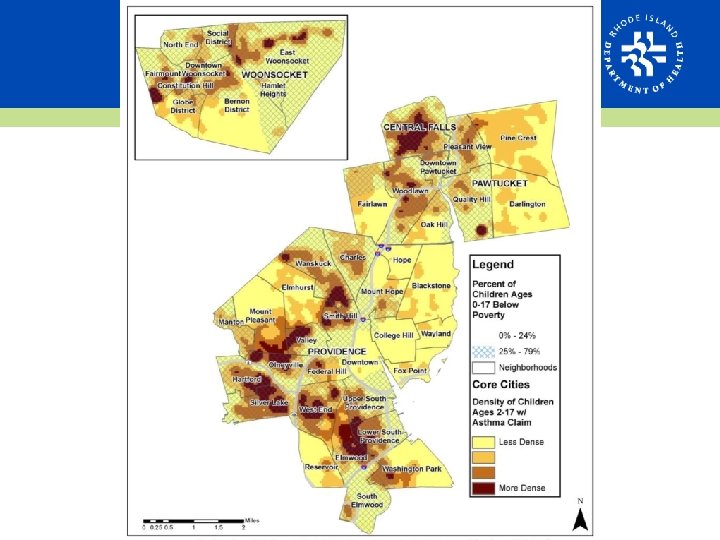
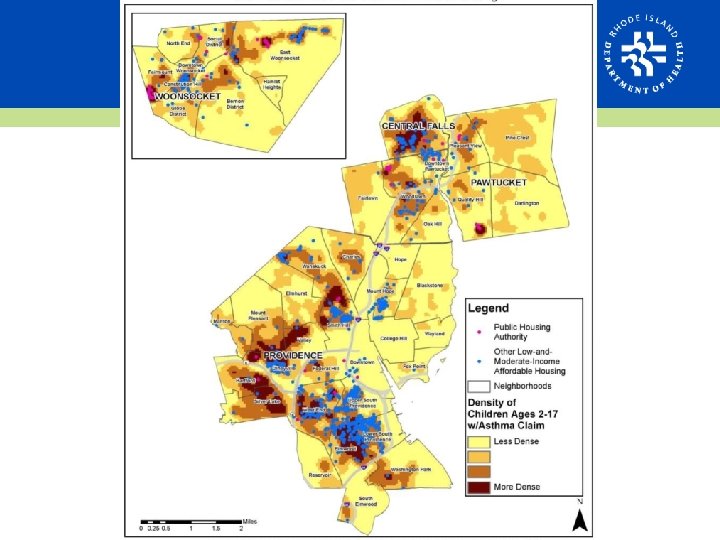
Asthma and Housing • Housing conditions often linked with poverty • Known indoor asthma triggers – Mold – Smoke – Pest (mice and cockroaches) – Mildew • Neighborhood condition asthma triggers – Air quality: ozone, smog, exhaust, particulate matter – Stress and intense emotions
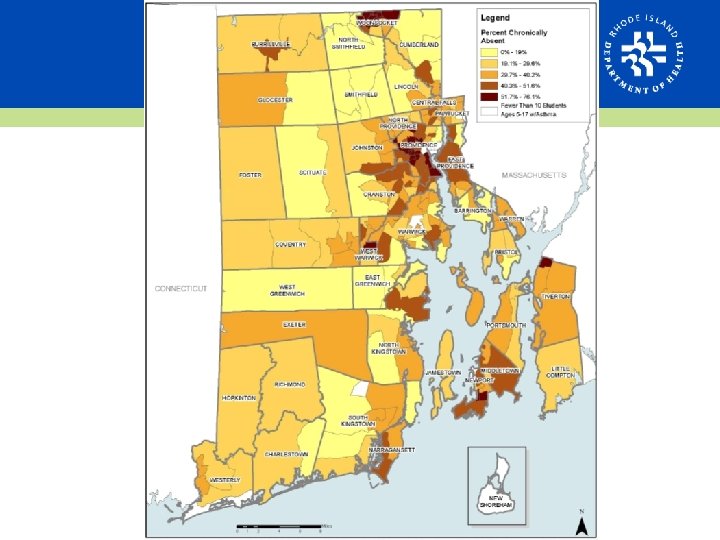
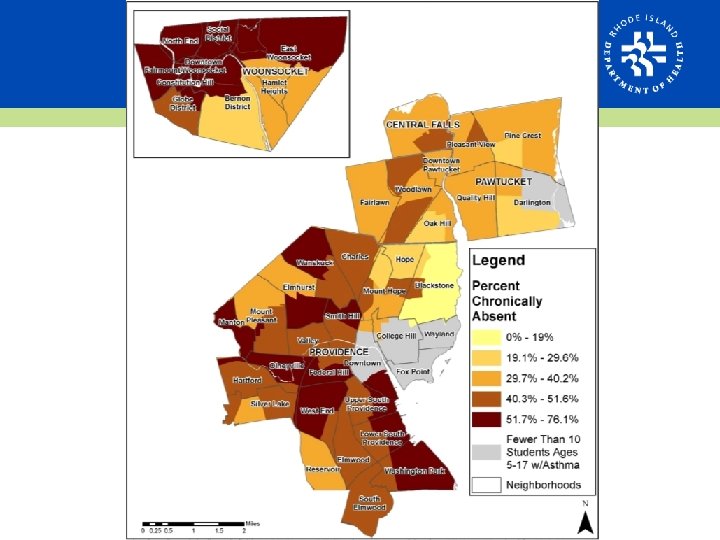
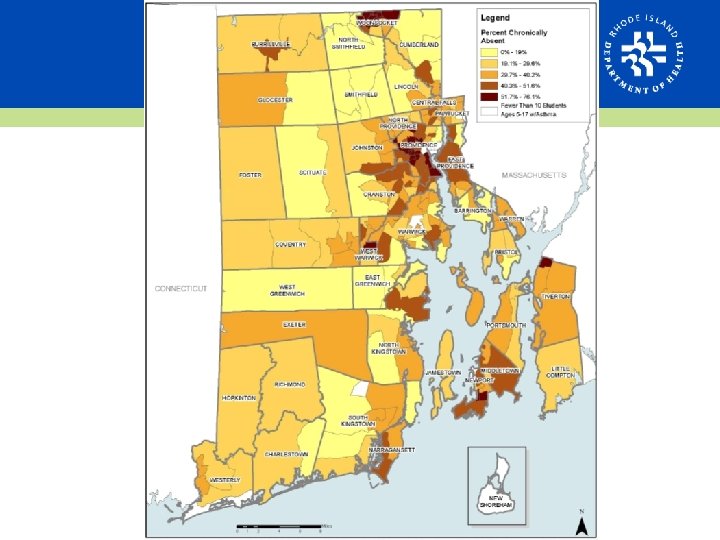
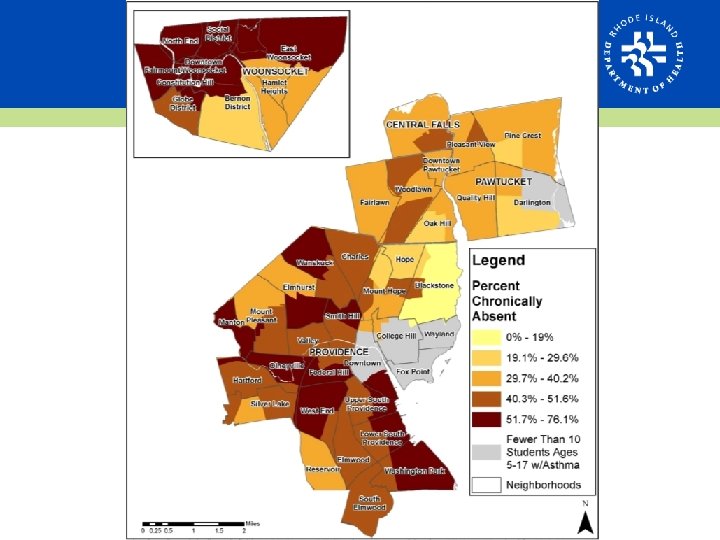
Asthma in Schools • Chronic absenteeism – Missing 10% or more of total school days per year • 37% of public school students with asthma were chronically absent from school in either 2010, 2011 or 2012 • Highest rates of chronic absenteeism cluster in urban areas • May reflect impact of other disadvantages of those with asthma
Asthma Care Guidelines • NHBLI’s NAEPP EPR-3 Guidelines: – From National Institutes of Health (NIH) National Heart, Lung, and Blood Institute – National Asthma Education and Prevention Program: Expert Panel Review • Proper diagnosis of severity, medication therapy, and assessment of asthma control • Asthma self-management education • Control of environmental factors Source: http: //www. nhlbi. nih. gov/health-pro/guidelines/current/asthma-guidelines/full-report
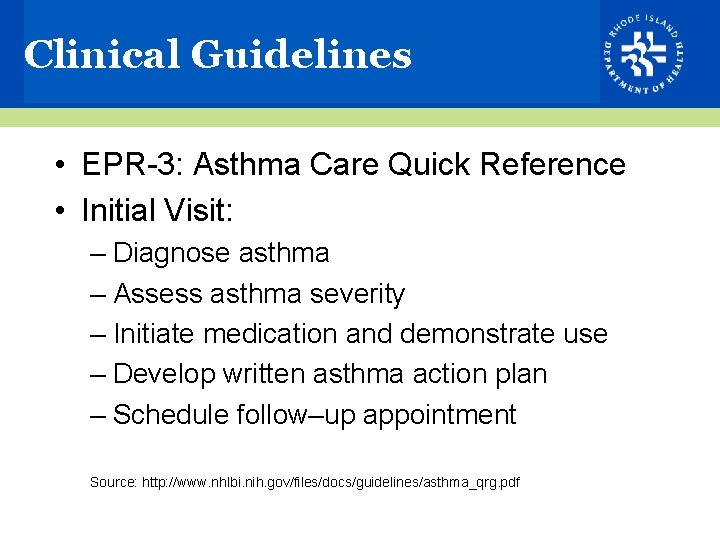
Clinical Guidelines • EPR-3: Asthma Care Quick Reference • Initial Visit: – Diagnose asthma – Assess asthma severity – Initiate medication and demonstrate use – Develop written asthma action plan – Schedule follow–up appointment Source: http: //www. nhlbi. nih. gov/files/docs/guidelines/asthma_qrg. pdf
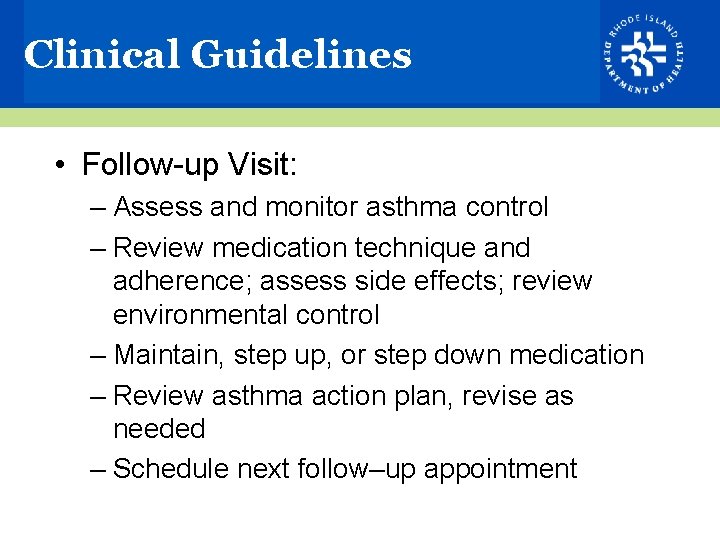
Clinical Guidelines • Follow-up Visit: – Assess and monitor asthma control – Review medication technique and adherence; assess side effects; review environmental control – Maintain, step up, or step down medication – Review asthma action plan, revise as needed – Schedule next follow–up appointment
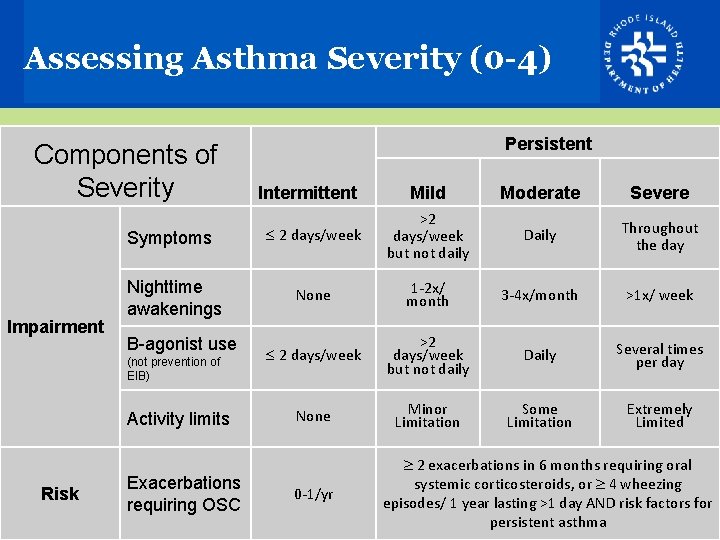
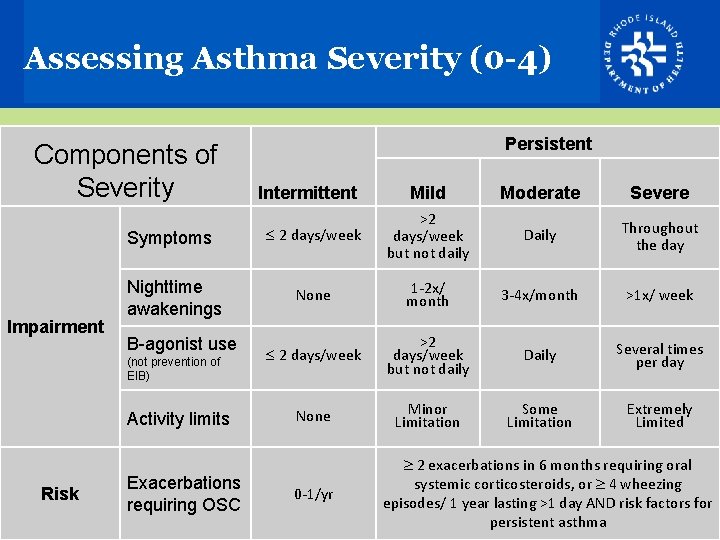
Assessing Asthma Severity (0 -4) Components of Severity Symptoms Impairment Nighttime awakenings B-agonist use (not prevention of EIB) Activity limits Risk Exacerbations requiring OSC Persistent Mild Moderate Severe 2 days/week >2 days/week but not daily Daily Throughout the day None 1 -2 x/ month 3 -4 x/month >1 x/ week 2 days/week >2 days/week but not daily Daily Several times per day None Minor Limitation Some Limitation Extremely Limited Intermittent 0 -1/yr 2 exacerbations in 6 months requiring oral systemic corticosteroids, or 4 wheezing episodes/ 1 year lasting >1 day AND risk factors for persistent asthma
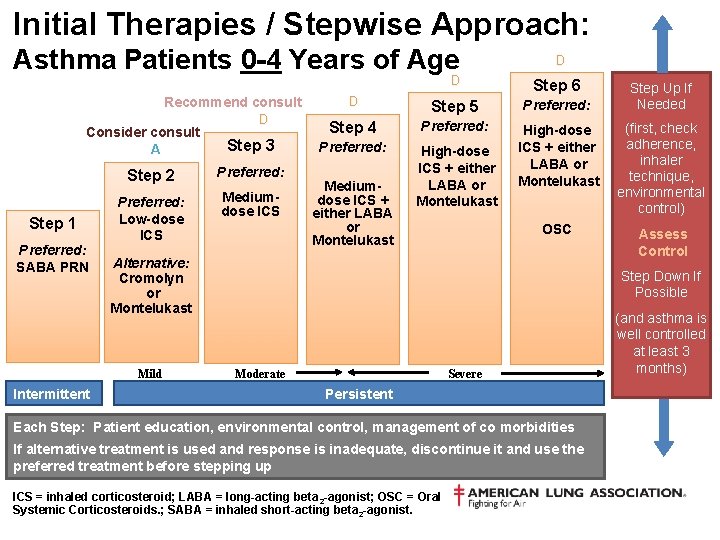
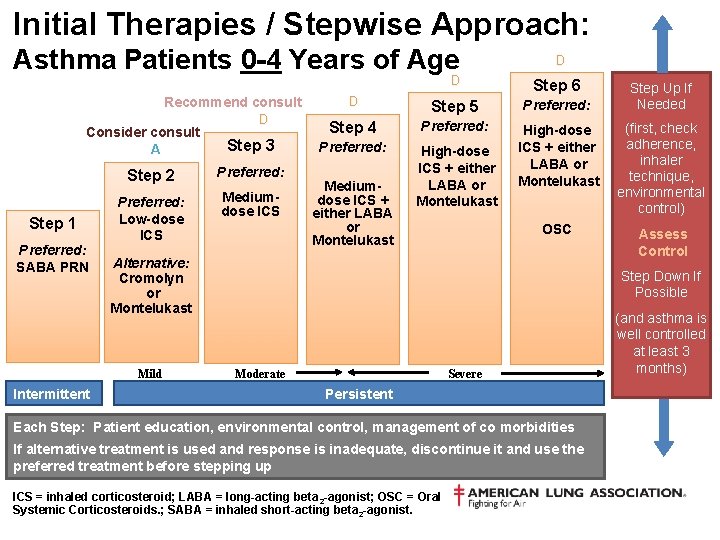
Initial Therapies / Stepwise Approach: Asthma Patients 0 -4 Years of Age Recommend consult Consider consult A Step 1 Preferred: SABA PRN Step 3 Step 2 Preferred: Low-dose ICS Mediumdose ICS D D Step 6 Step 5 Preferred: Step 4 Preferred: High-dose ICS + either LABA or Montelukast (first, check adherence, inhaler technique, environmental control) OSC Assess Control Mediumdose ICS + either LABA or Montelukast Alternative: Cromolyn or Montelukast Mild Intermittent D D Step Up If Needed Step Down If Possible Moderate Severe Persistent Each Step: Patient education, environmental control, management of co morbidities If alternative treatment is used and response is inadequate, discontinue it and use the preferred treatment before stepping up ICS = inhaled corticosteroid; LABA = long-acting beta 2 -agonist; OSC = Oral Systemic Corticosteroids. ; SABA = inhaled short-acting beta 2 -agonist. (and asthma is well controlled at least 3 months)
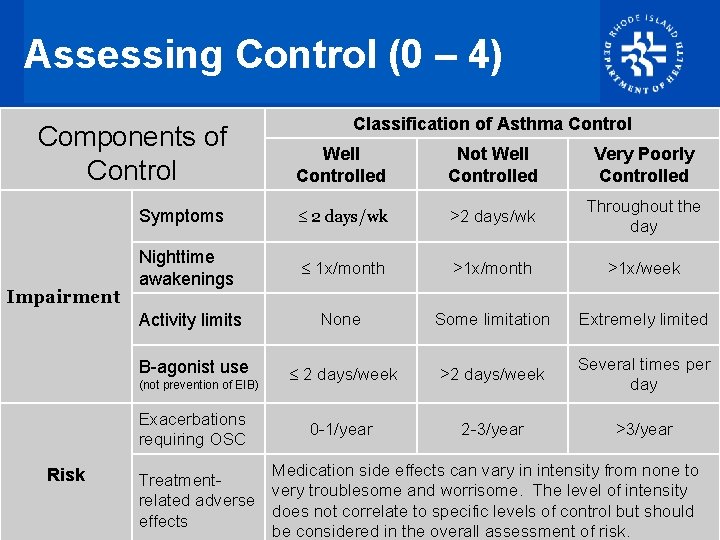
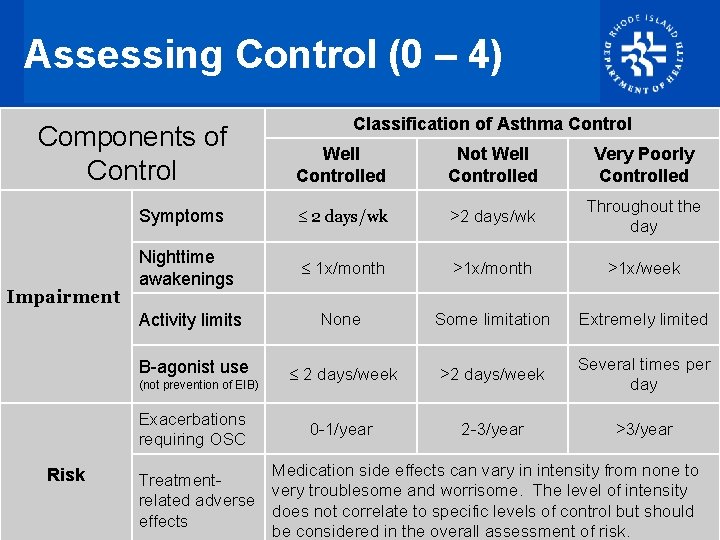
Assessing Control (0 – 4) Classification of Asthma Control Components of Control Well Controlled Not Well Controlled Very Poorly Controlled Symptoms 2 days/wk >2 days/wk Throughout the day Nighttime awakenings 1 x/month >1 x/week Activity limits None Some limitation Extremely limited B-agonist use 2 days/week >2 days/week Several times per day 0 -1/year 2 -3/year >3/year Impairment (not prevention of EIB) Exacerbations requiring OSC Risk Medication side effects can vary in intensity from none to Treatmentvery troublesome and worrisome. The level of intensity related adverse does not correlate to specific levels of control but should effects be considered in the overall assessment of risk.
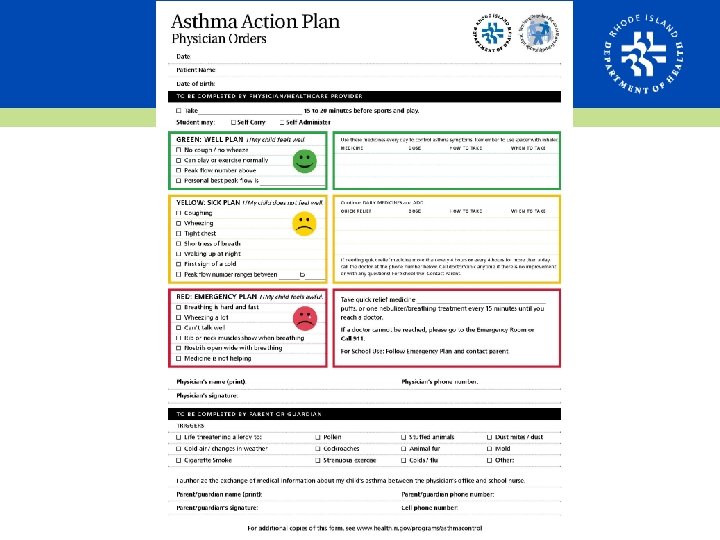
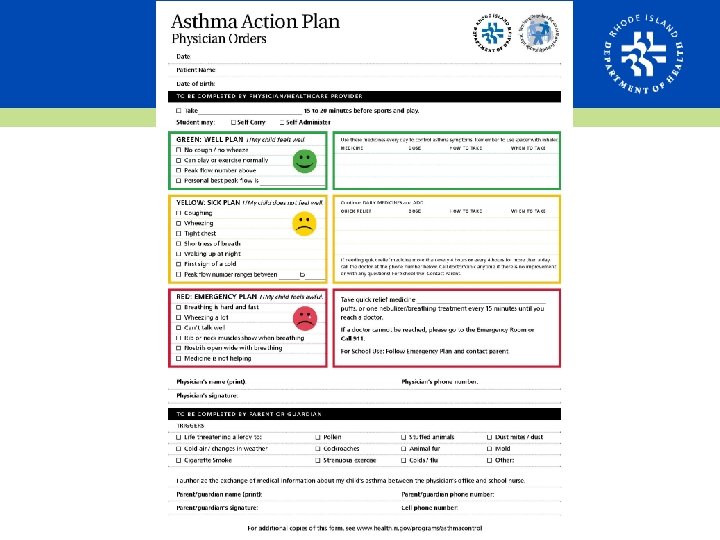
Self-management education • Essential to provide patients with the skills necessary to control asthma and improve outcomes • Provide all patients with written asthma action plan that includes 2 elements: – Daily management – How to recognize and handle worsening symptoms Source: http: //www. nhlbi. nih. gov/files/docs/guidelines/05_sec 3_comp 2. pdf
Self-management education • Regular review, by an informed clinician, of the status of a patient’s asthma control is an essential part of asthma selfmanagement education • Encourage development and evaluation of community-based interventions that provide opportunities to reach a wide population of patients and their families, especially those at high risk
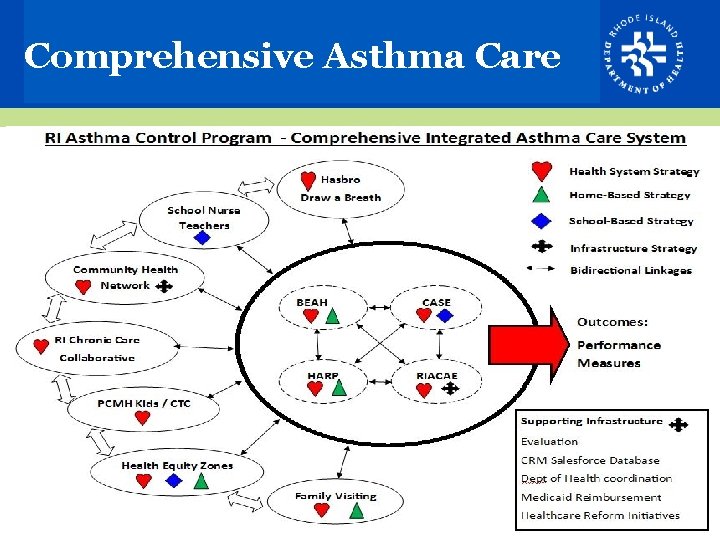
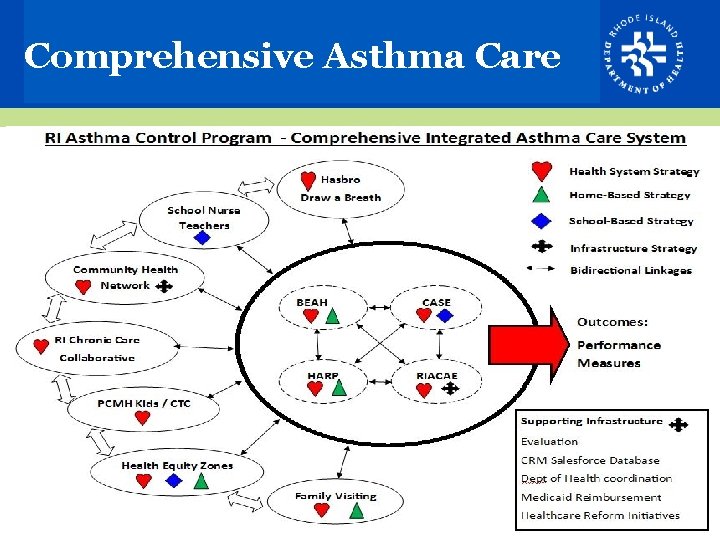
Comprehensive Asthma Care
HARP: Home Asthma Response Program • Pediatric asthma home visiting – Prior asthma related ED visit / hospitalization – Certified Asthma Educator (AE-C) and Community Health Worker (CHW) – 3 home visits: asthma self-management education, trigger reduction, environmental supplies • Results: improved health outcomes, reduced utilization/costs
BEAH: Breathe Easy at Home • Medical referral to code enforcement – For extreme situations when provider suspects that a child’s asthma is caused by housing conditions – Referral made through KIDSNET – Includes educational materials for family and landlord, legal support as needed – Currently available in four core cities: Providence, Pawtucket, Central Falls, Woonsocket
Certified Asthma Educators • AE-Cs play a critical role in team-based care • NAECB: National Asthma Educator Certification Board • Prep-courses offered twice per year • Encourage Nurse Care Managers, and/or other member of care team to become certified as an AE-C • Referrals for AE-Cs will be available through Community Health Network (like CDOEs)
Julian Rodriguez-Drix Program Manager, RI Asthma Control Program 401. 222. 7742 Julian. Drix@health. ri. gov