Rhythm 12 Lead EKG Review Electrical Cardiac Cells

- Slides: 62

Rhythm & 12 Lead EKG Review
Electrical Cardiac Cells • Automaticity – the ability to spontaneously generate and discharge an electrical impulse • Excitability – the ability of the cell to respond to an electrical impulse • Conductivity – the ability to transmit an electrical impulse from one cell to the next
Myocardial Cells • Contractility – the ability of the cell to shorten and lengthen its fibers • Extensibility – the ability of the cell to stretch
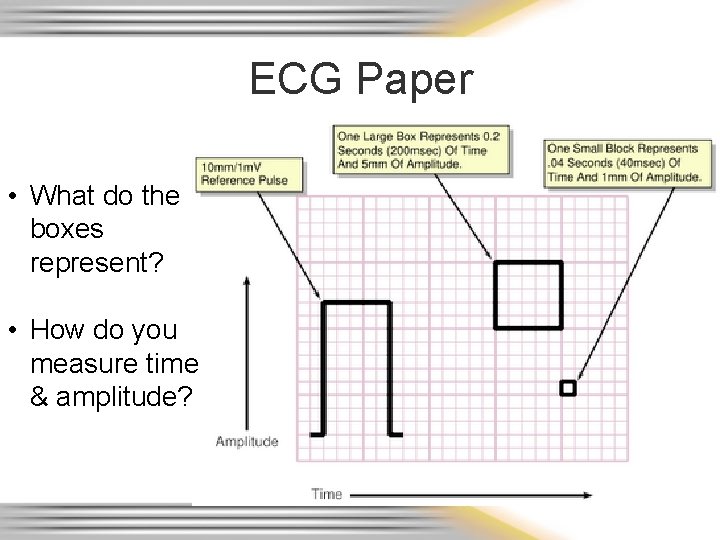
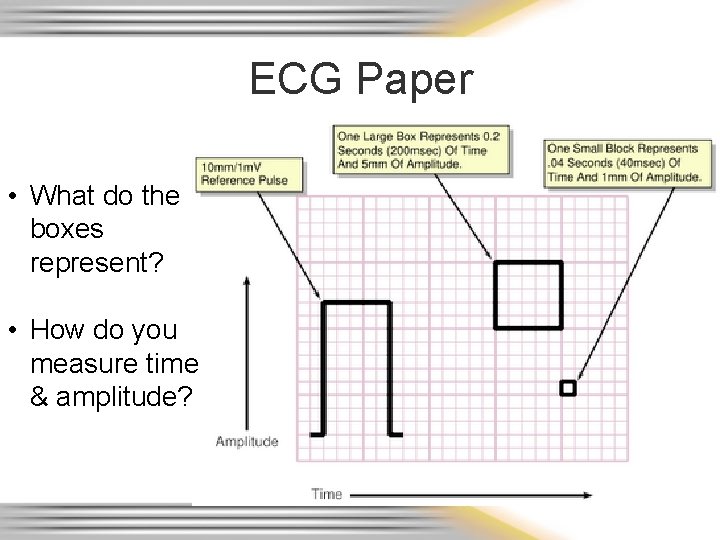
ECG Paper • What do the boxes represent? • How do you measure time & amplitude?
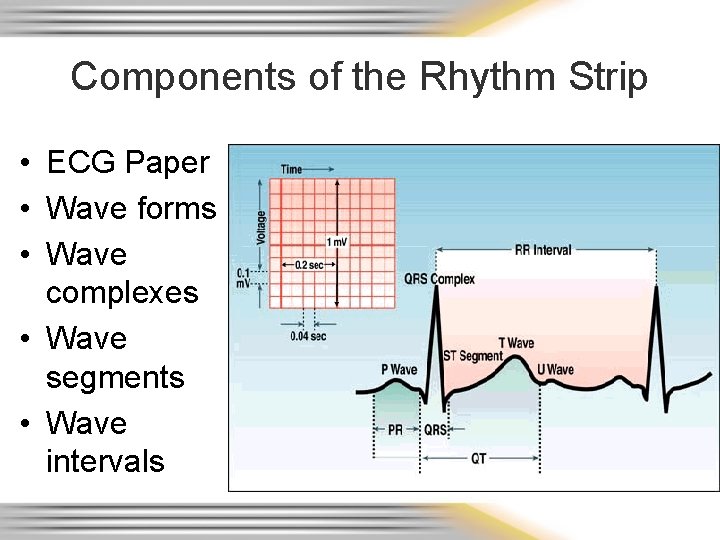
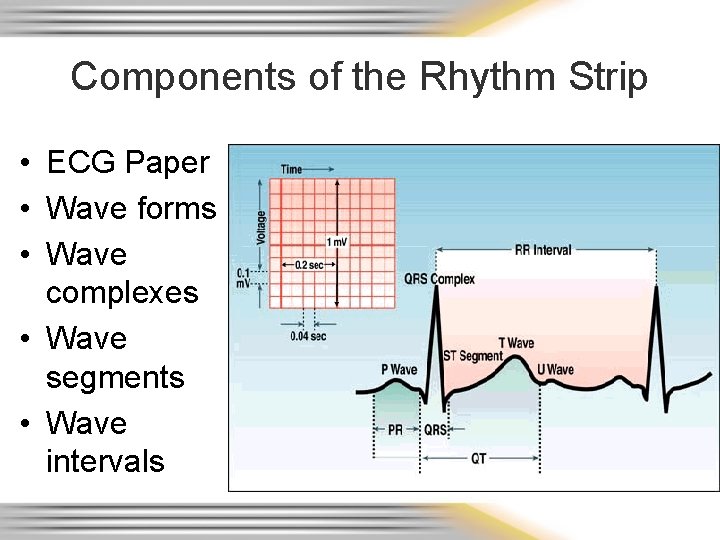
Components of the Rhythm Strip • ECG Paper • Wave forms • Wave complexes • Wave segments • Wave intervals
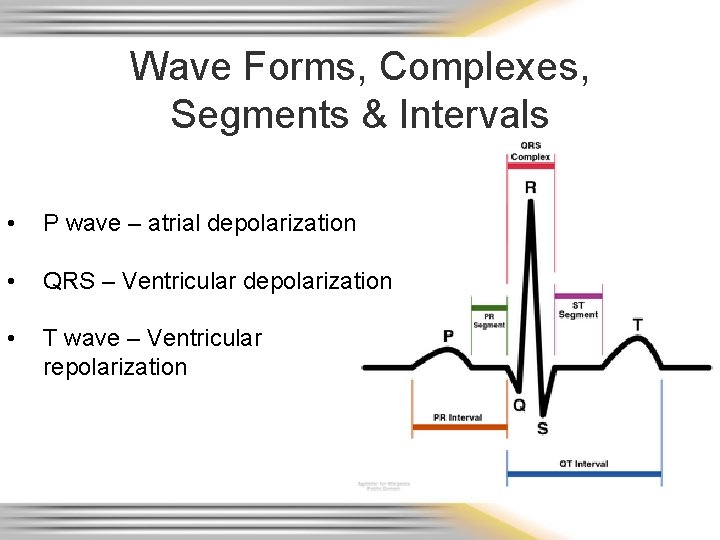
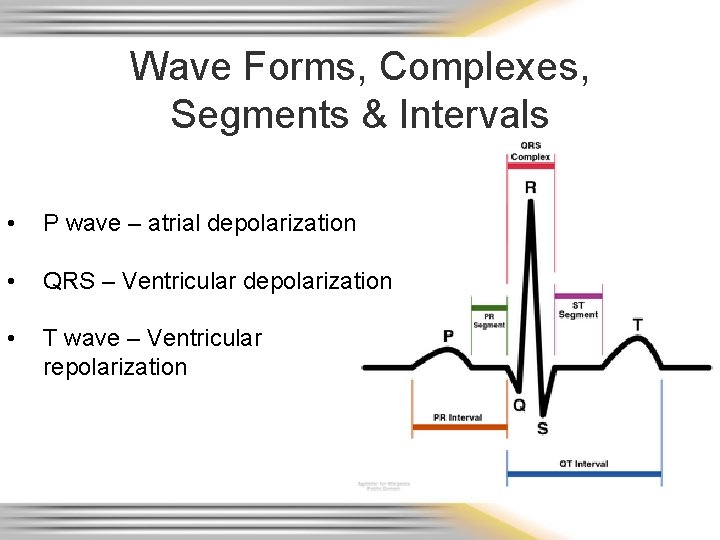
Wave Forms, Complexes, Segments & Intervals • P wave – atrial depolarization • QRS – Ventricular depolarization • T wave – Ventricular repolarization
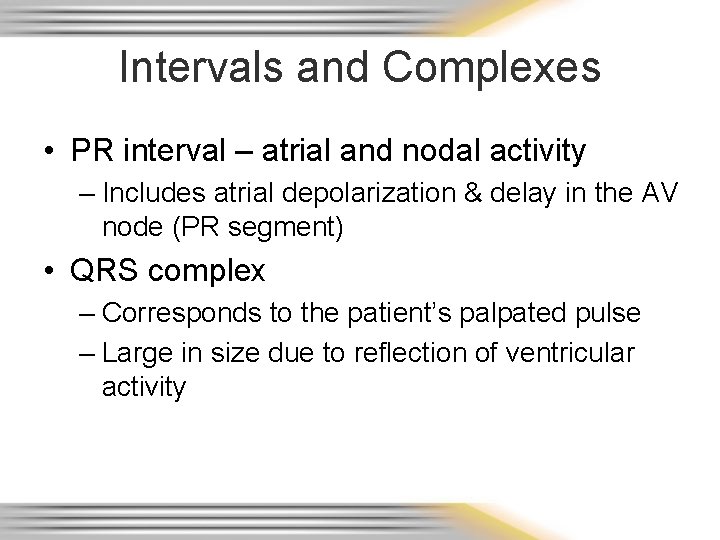
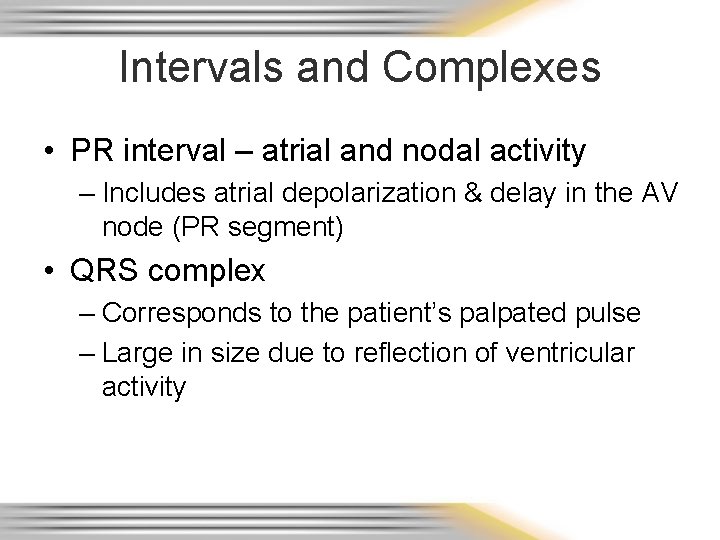
Intervals and Complexes • PR interval – atrial and nodal activity – Includes atrial depolarization & delay in the AV node (PR segment) • QRS complex – Corresponds to the patient’s palpated pulse – Large in size due to reflection of ventricular activity
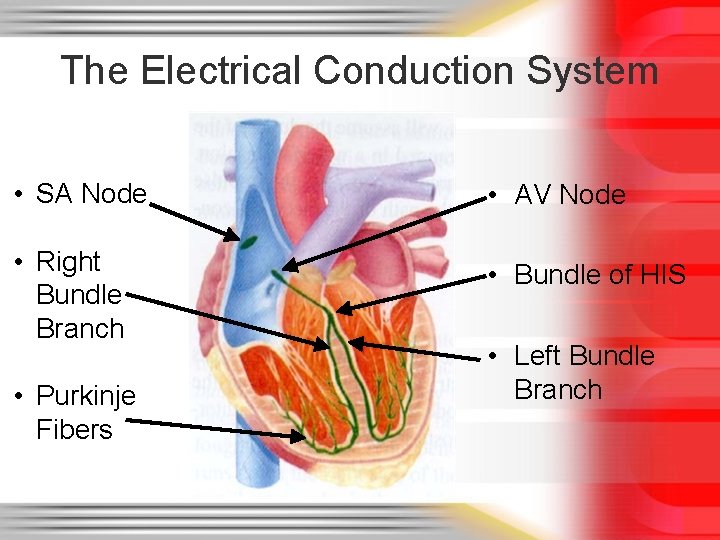
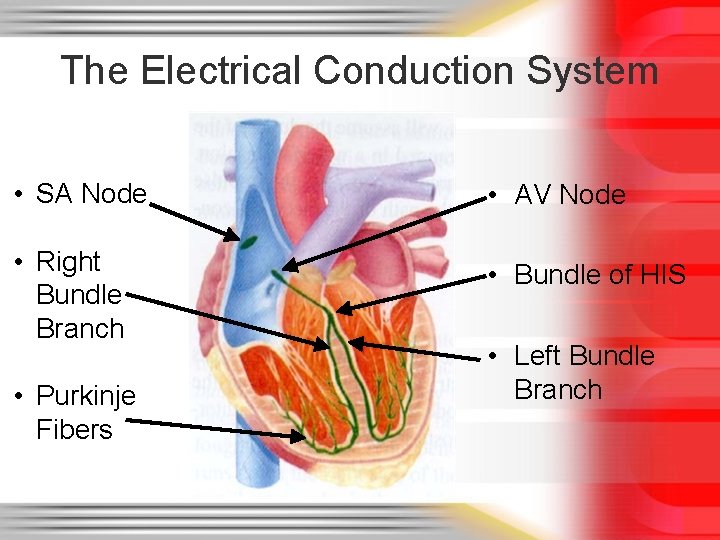
The Electrical Conduction System • SA Node • AV Node • Right Bundle Branch • Bundle of HIS • Purkinje Fibers • Left Bundle Branch
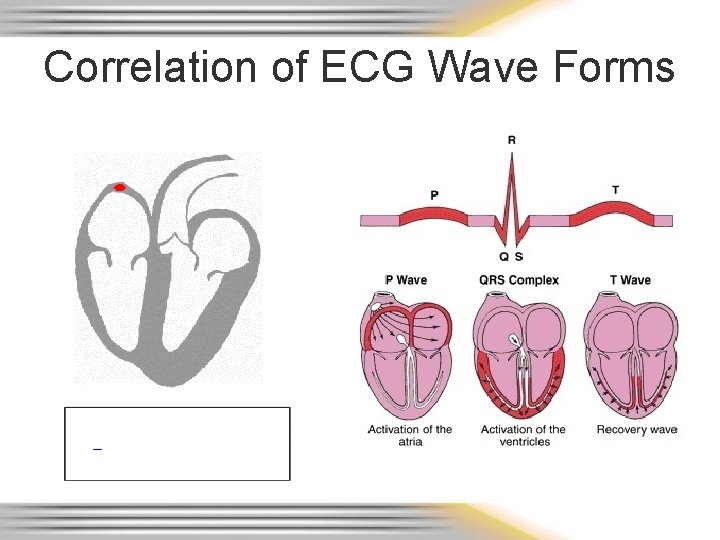
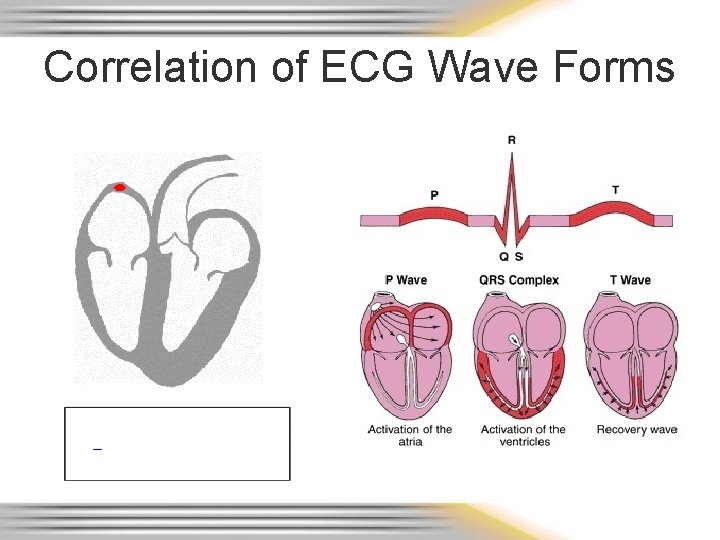
Correlation of ECG Wave Forms
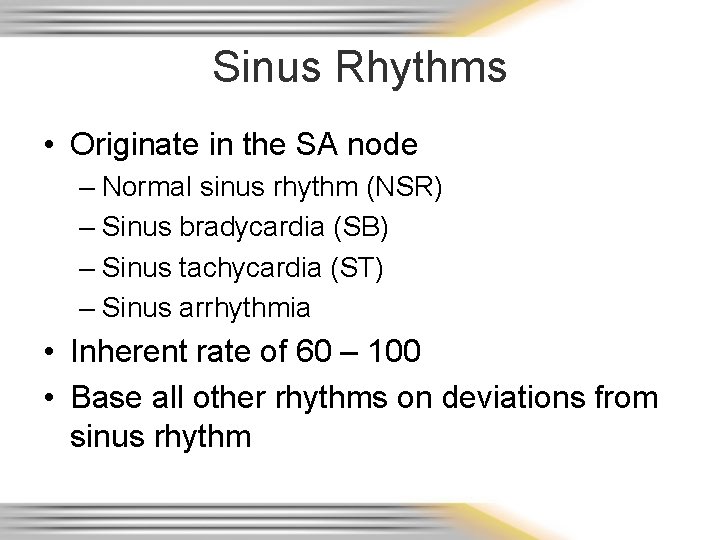
Sinus Rhythms • Originate in the SA node – Normal sinus rhythm (NSR) – Sinus bradycardia (SB) – Sinus tachycardia (ST) – Sinus arrhythmia • Inherent rate of 60 – 100 • Base all other rhythms on deviations from sinus rhythm
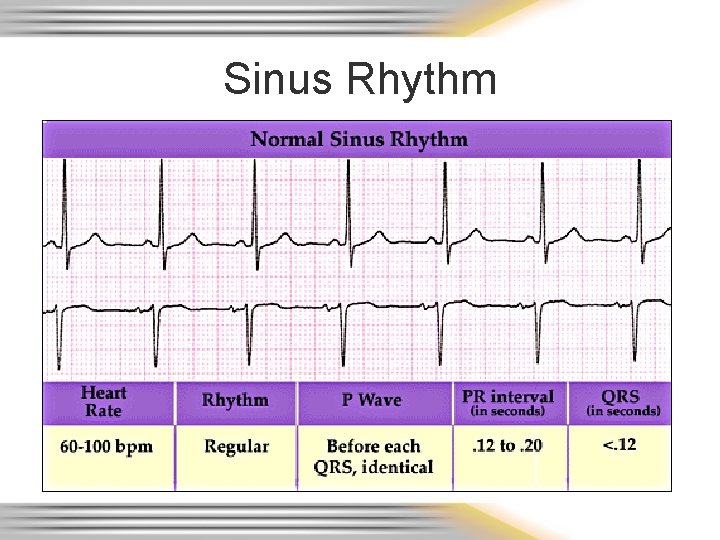
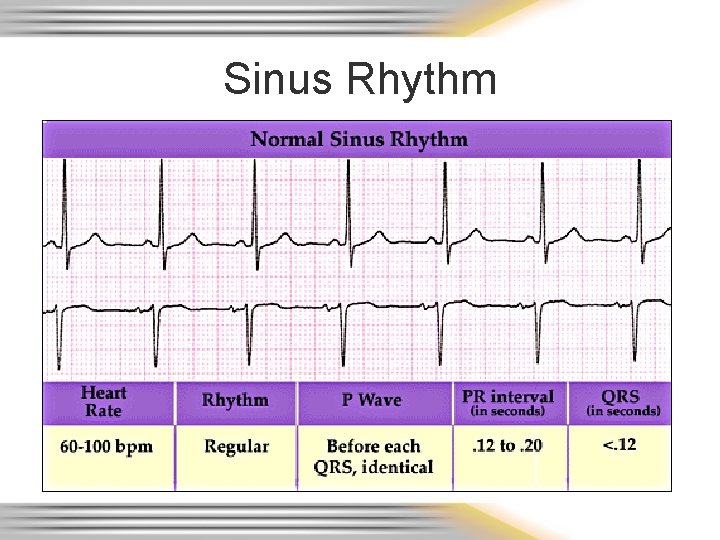
Sinus Rhythm
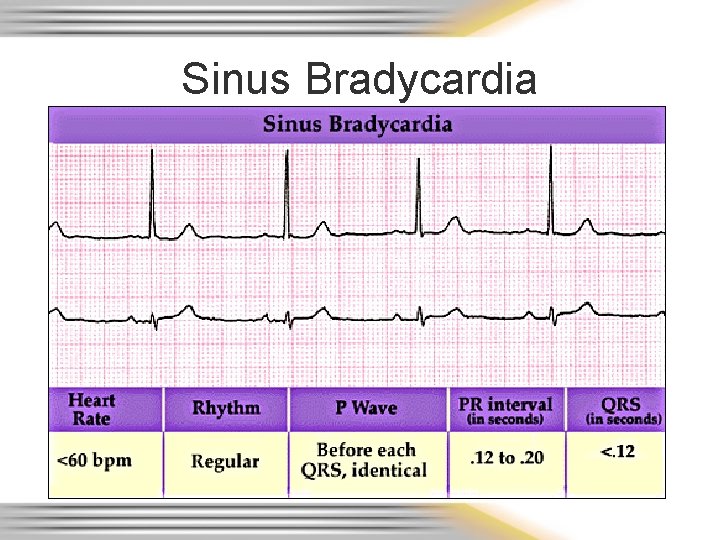
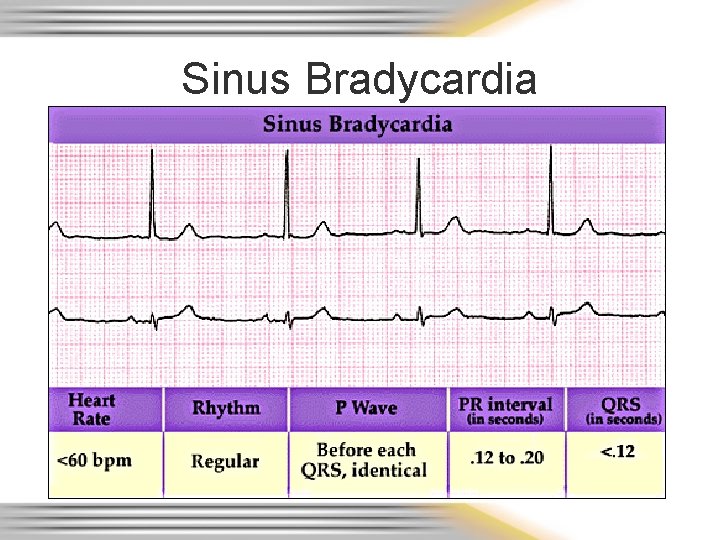
Sinus Bradycardia
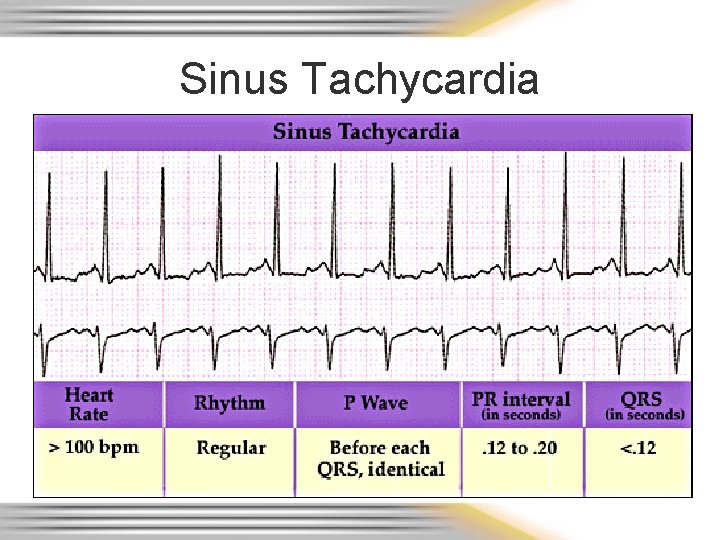
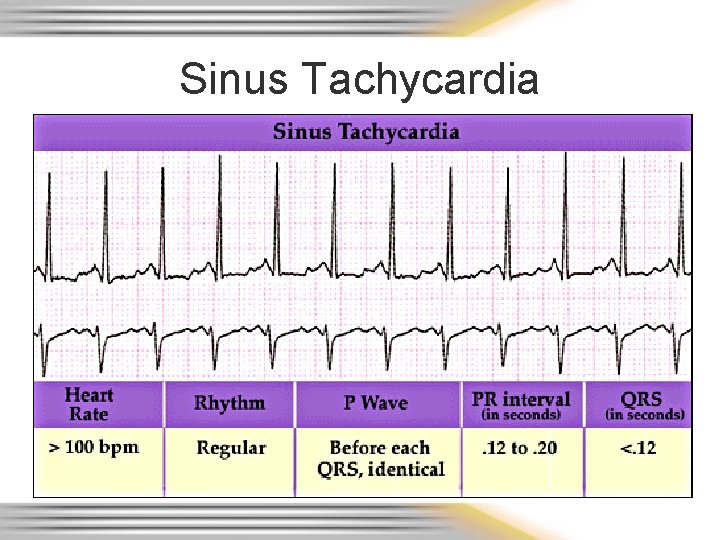
Sinus Tachycardia
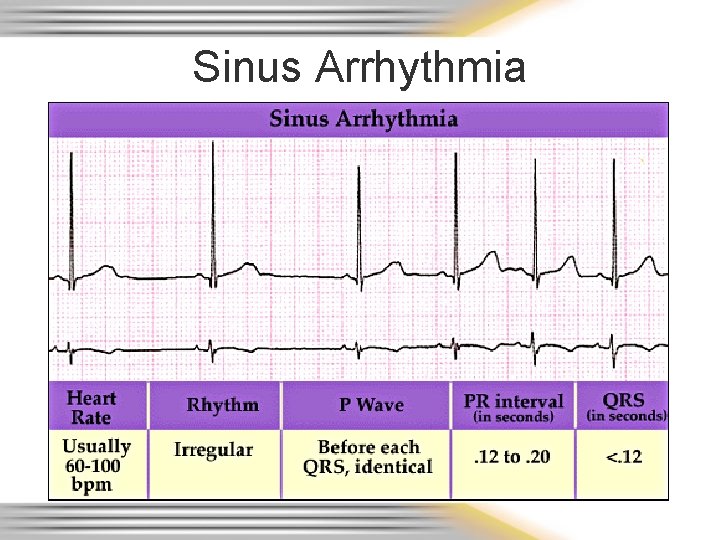
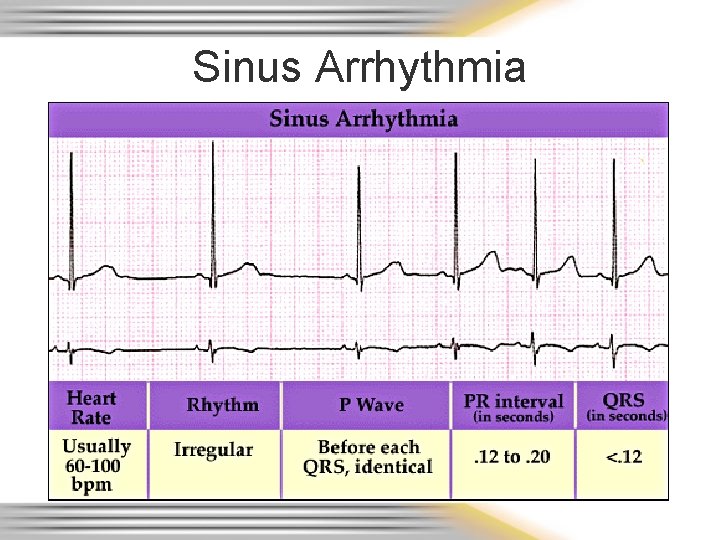
Sinus Arrhythmia
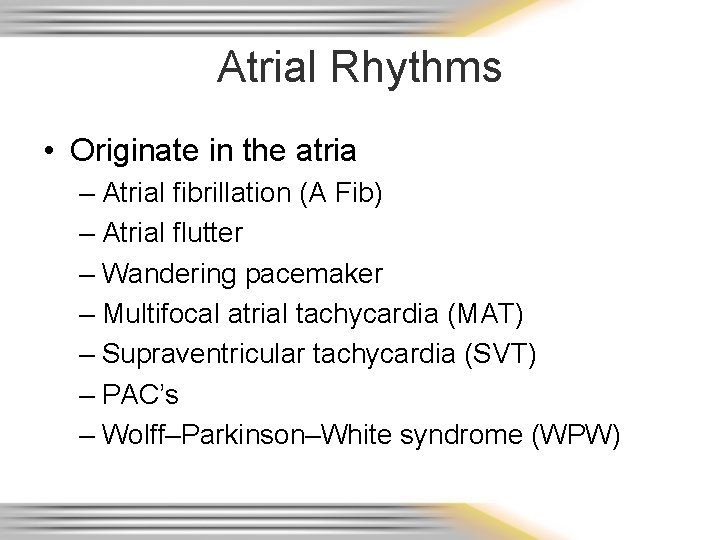
Atrial Rhythms • Originate in the atria – Atrial fibrillation (A Fib) – Atrial flutter – Wandering pacemaker – Multifocal atrial tachycardia (MAT) – Supraventricular tachycardia (SVT) – PAC’s – Wolff–Parkinson–White syndrome (WPW)
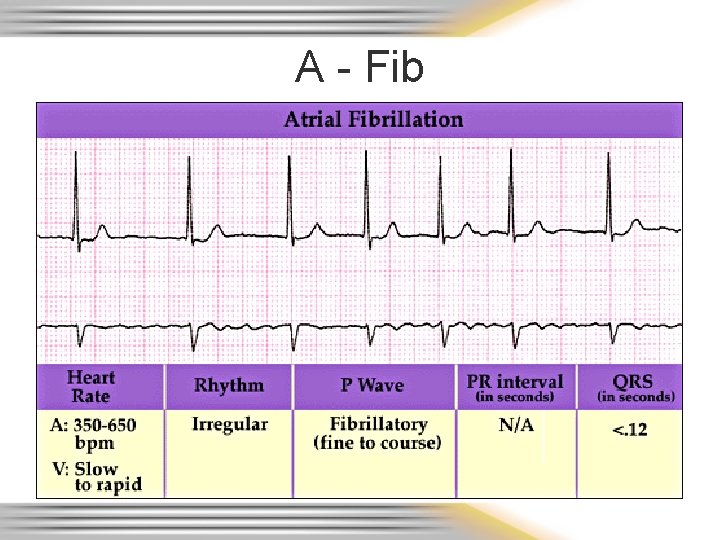
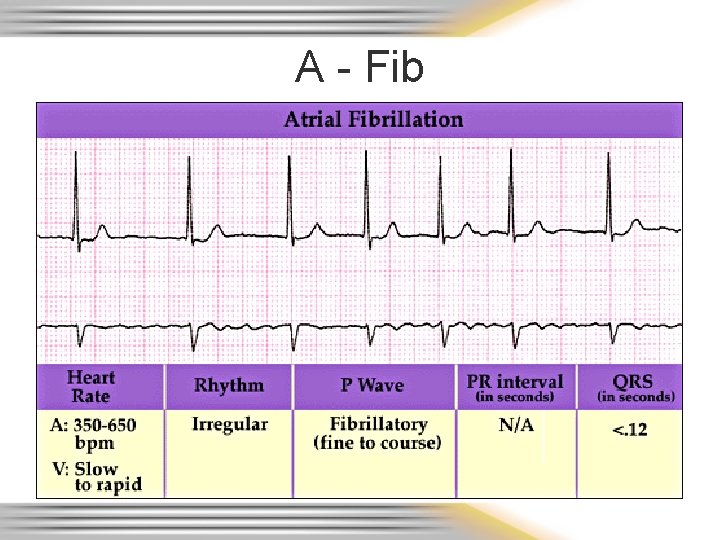
A - Fib
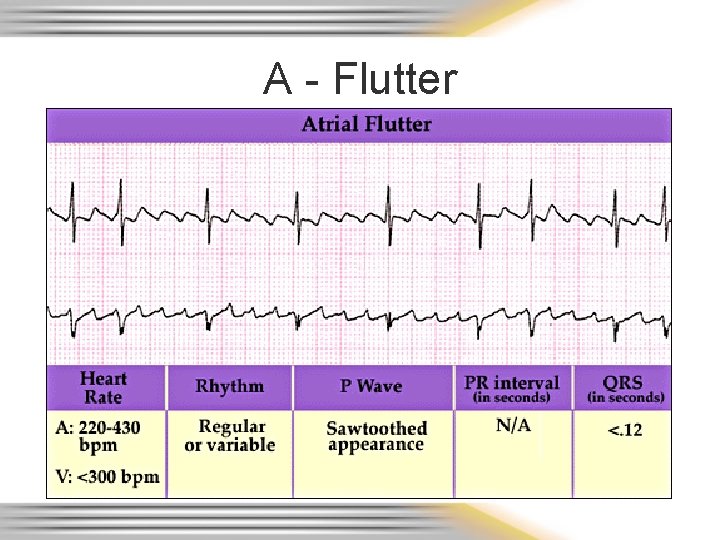
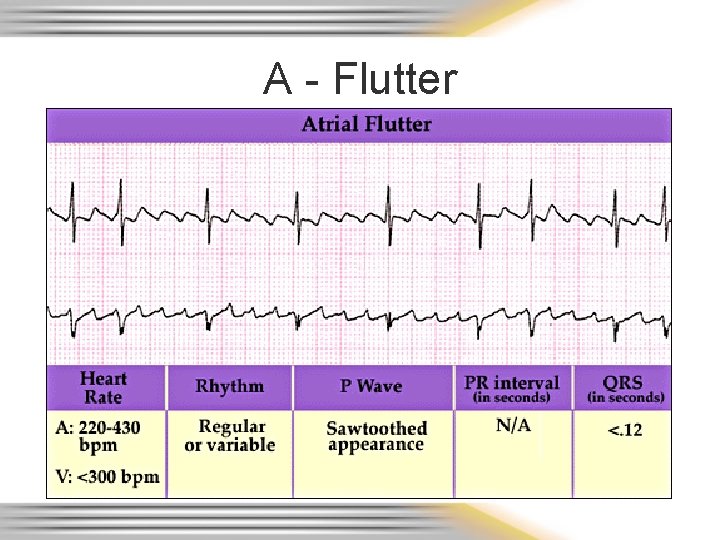
A - Flutter
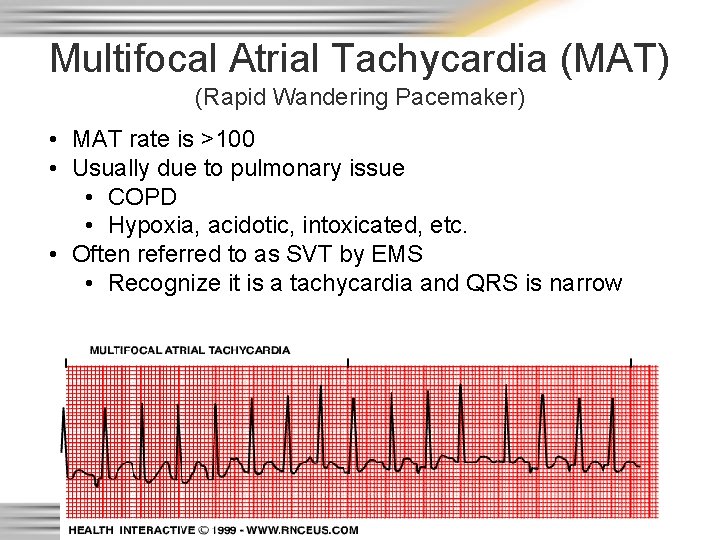
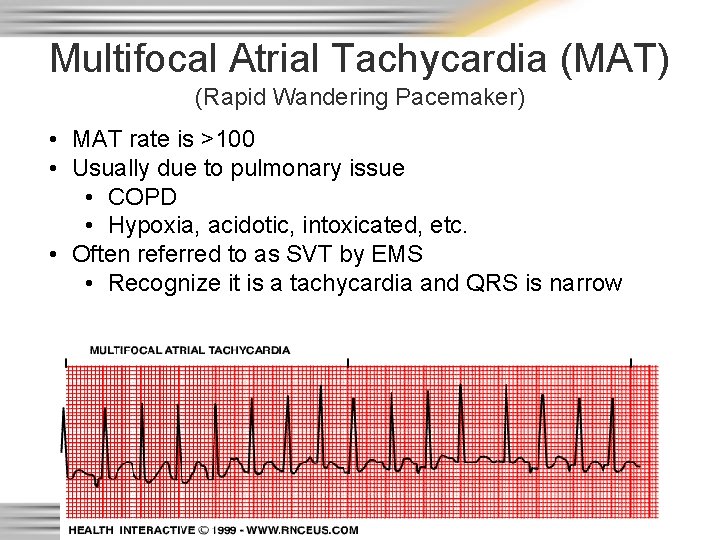
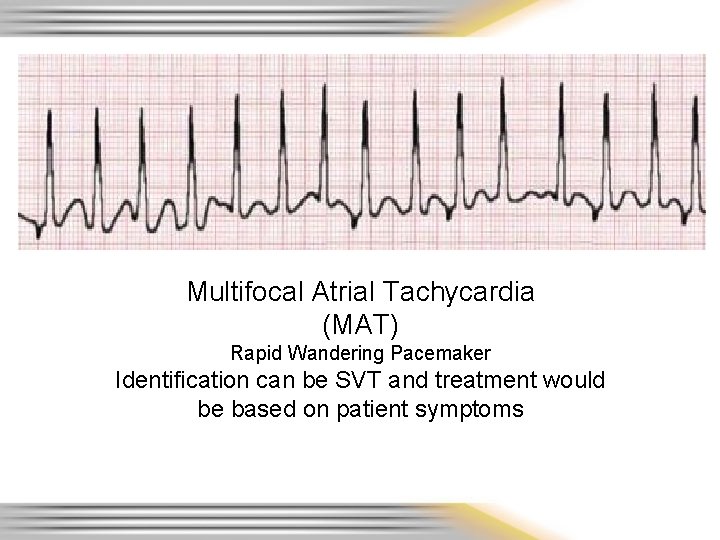
Multifocal Atrial Tachycardia (MAT) (Rapid Wandering Pacemaker) • MAT rate is >100 • Usually due to pulmonary issue • COPD • Hypoxia, acidotic, intoxicated, etc. • Often referred to as SVT by EMS • Recognize it is a tachycardia and QRS is narrow
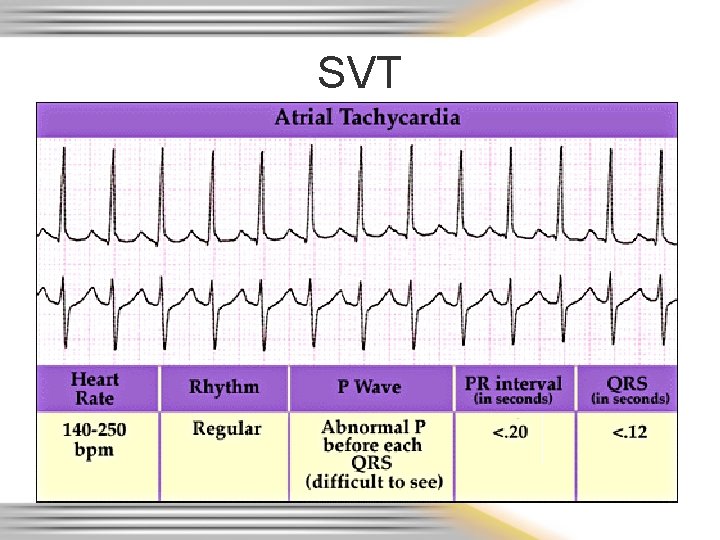
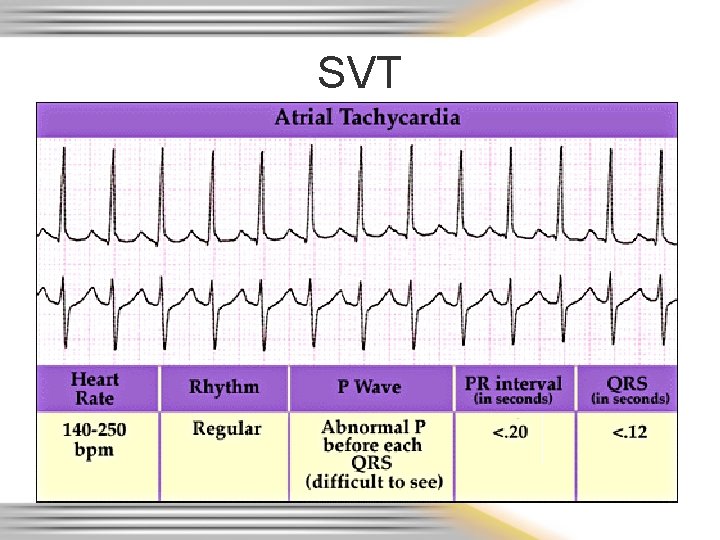
SVT
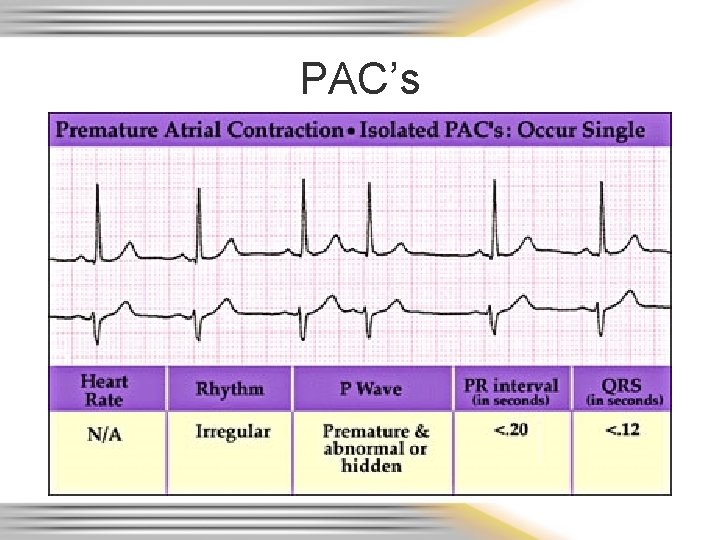
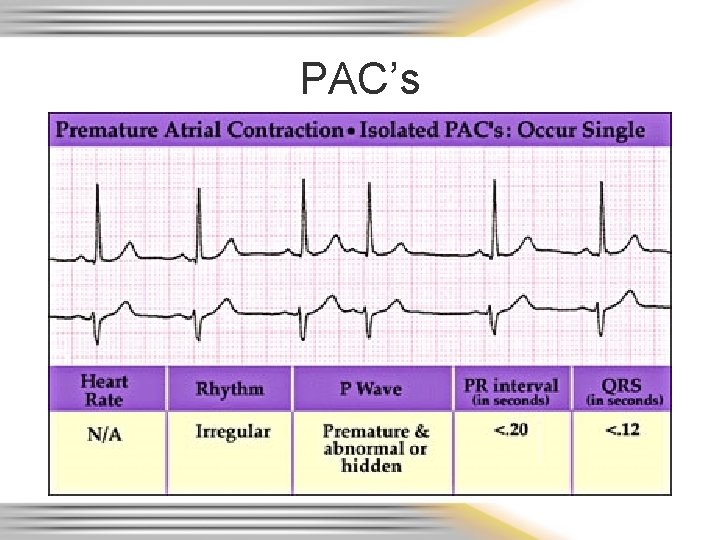
PAC’s
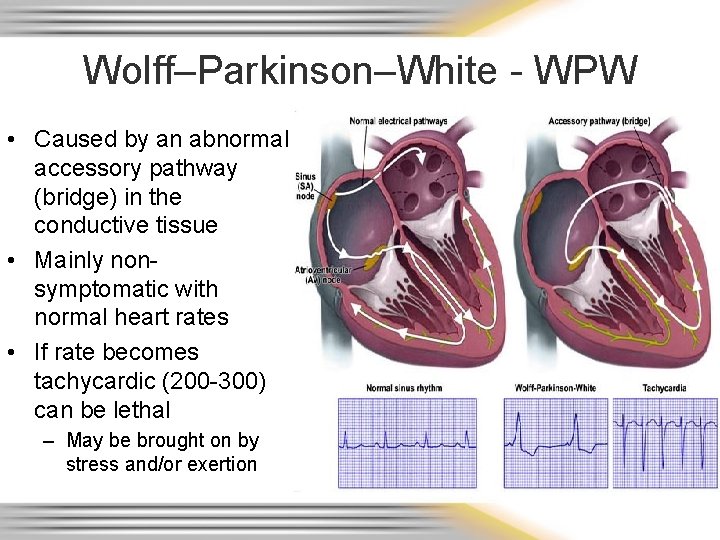
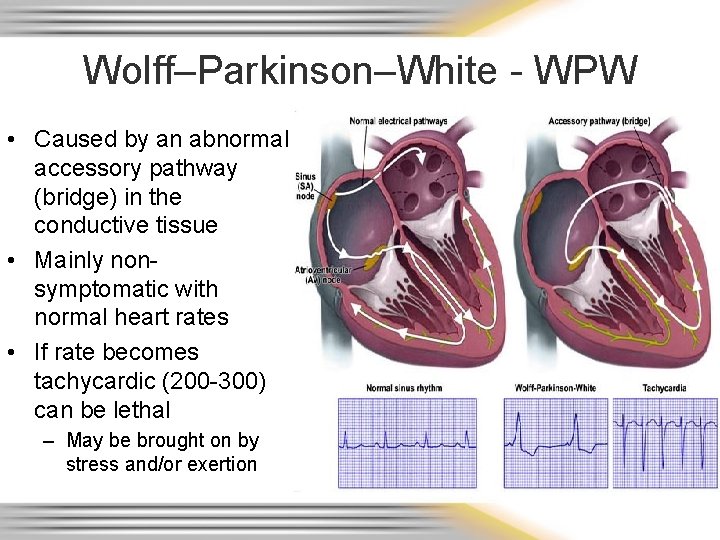
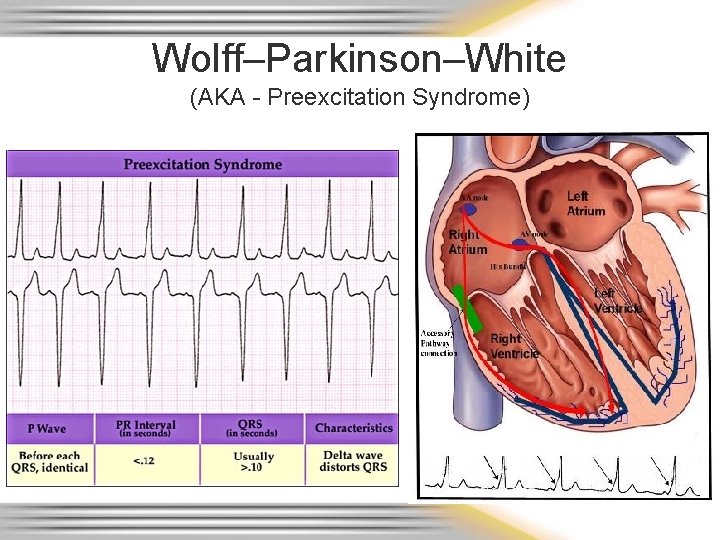
Wolff–Parkinson–White - WPW • Caused by an abnormal accessory pathway (bridge) in the conductive tissue • Mainly nonsymptomatic with normal heart rates • If rate becomes tachycardic (200 -300) can be lethal – May be brought on by stress and/or exertion
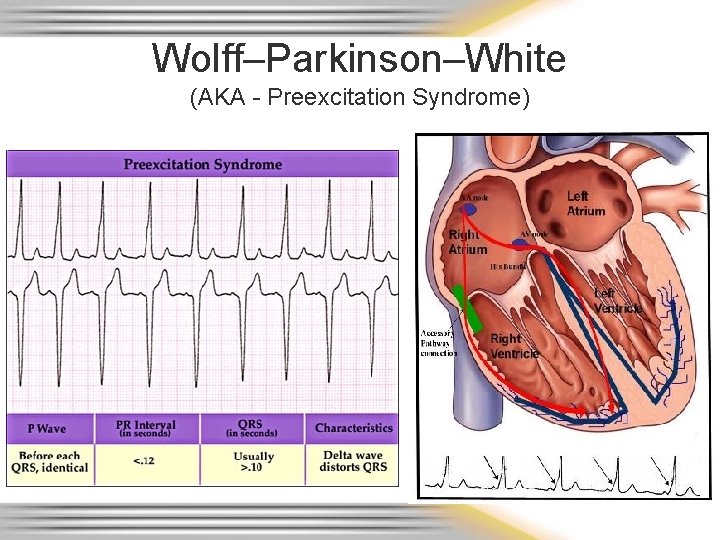
Wolff–Parkinson–White (AKA - Preexcitation Syndrome)
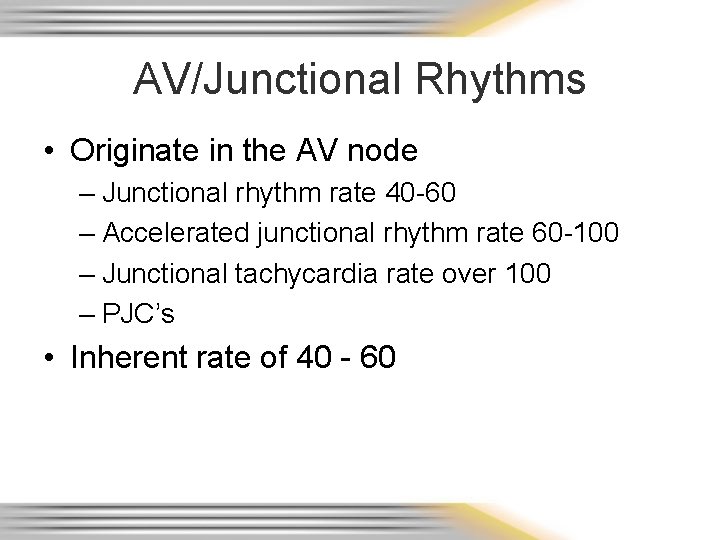
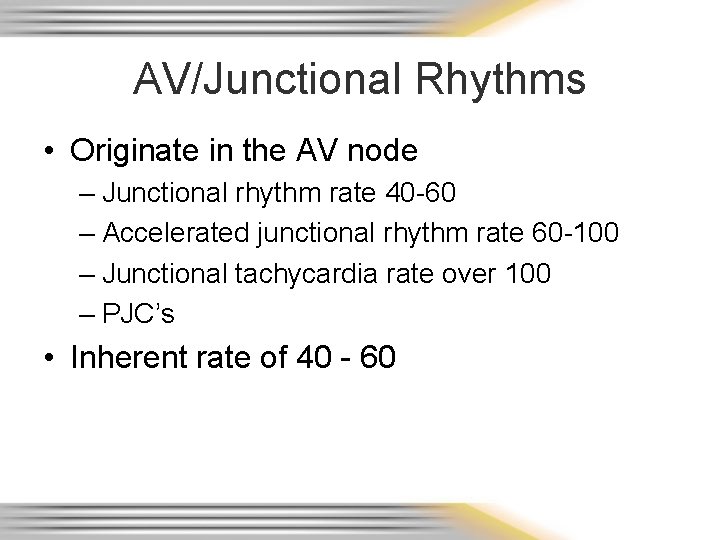
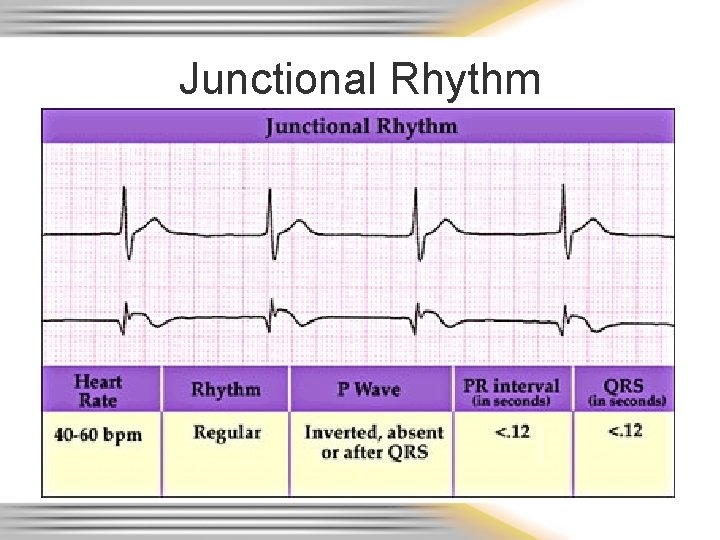
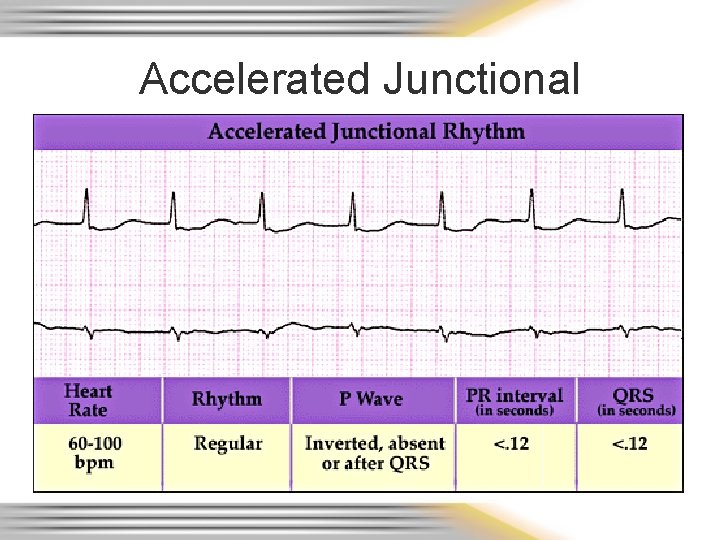
AV/Junctional Rhythms • Originate in the AV node – Junctional rhythm rate 40 -60 – Accelerated junctional rhythm rate 60 -100 – Junctional tachycardia rate over 100 – PJC’s • Inherent rate of 40 - 60
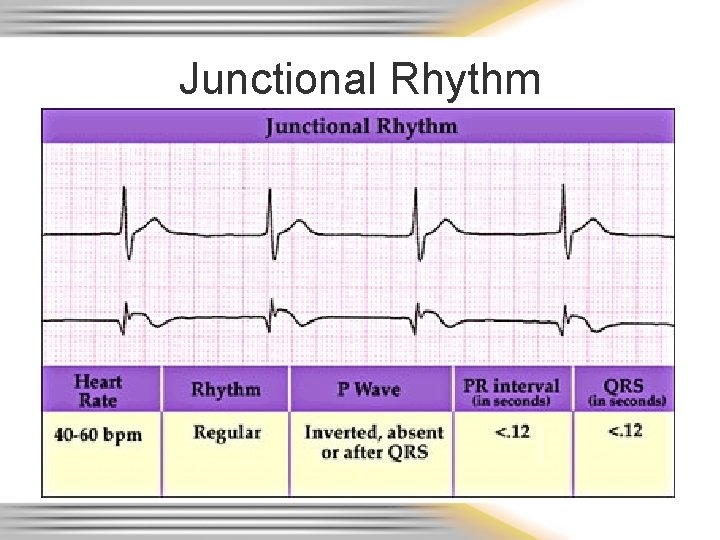
Junctional Rhythm
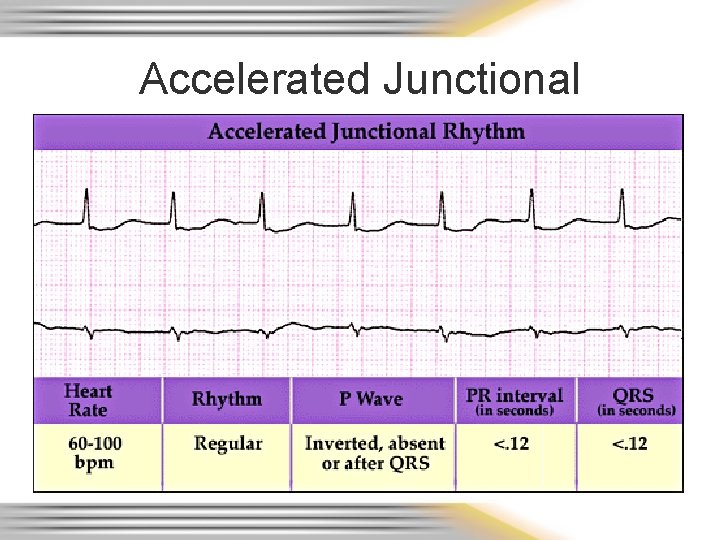
Accelerated Junctional
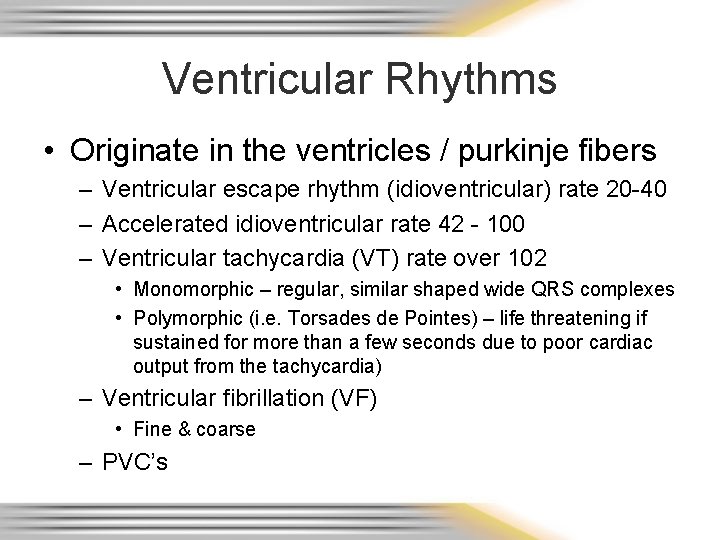
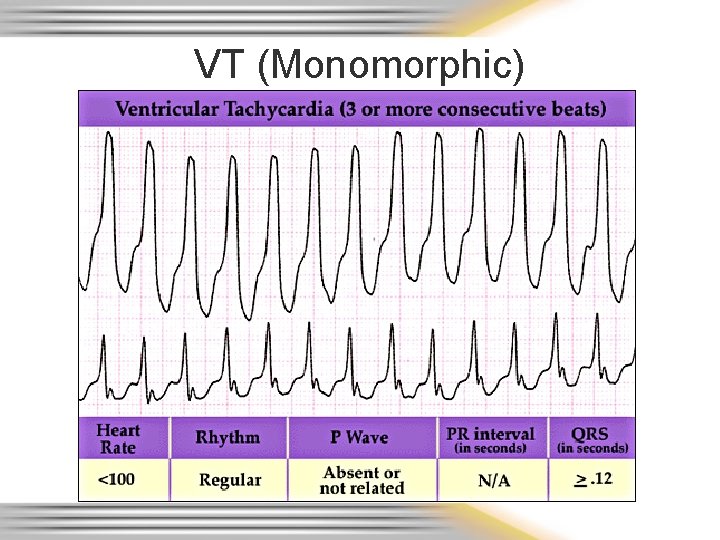
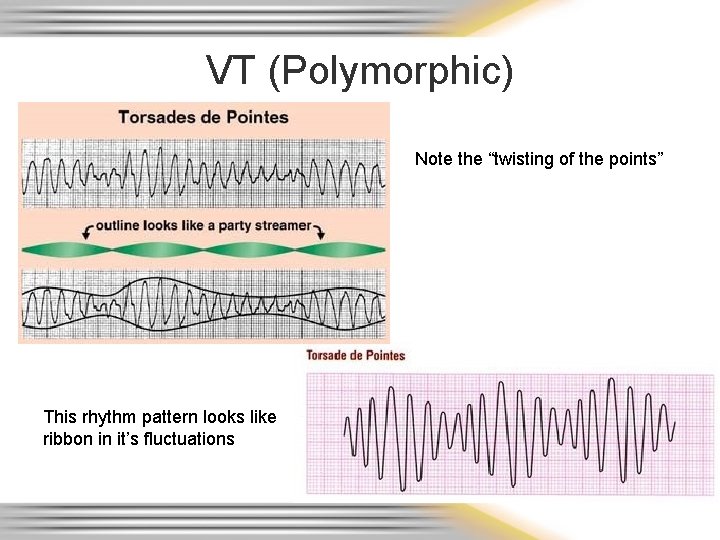
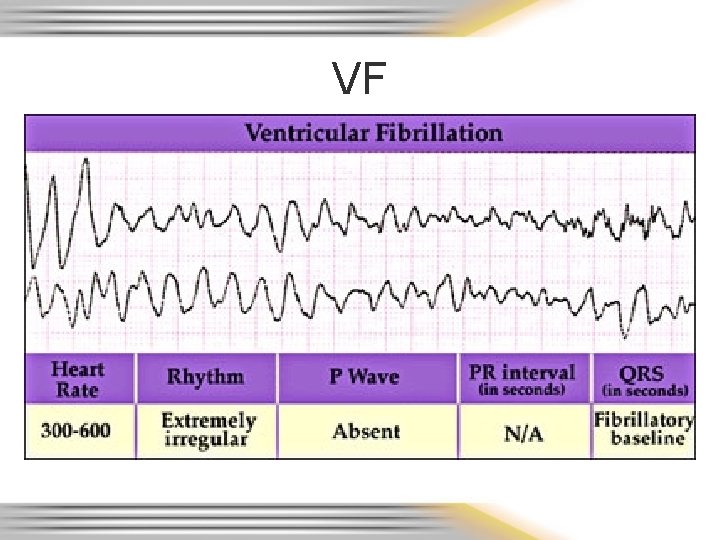
Ventricular Rhythms • Originate in the ventricles / purkinje fibers – Ventricular escape rhythm (idioventricular) rate 20 -40 – Accelerated idioventricular rate 42 - 100 – Ventricular tachycardia (VT) rate over 102 • Monomorphic – regular, similar shaped wide QRS complexes • Polymorphic (i. e. Torsades de Pointes) – life threatening if sustained for more than a few seconds due to poor cardiac output from the tachycardia) – Ventricular fibrillation (VF) • Fine & coarse – PVC’s
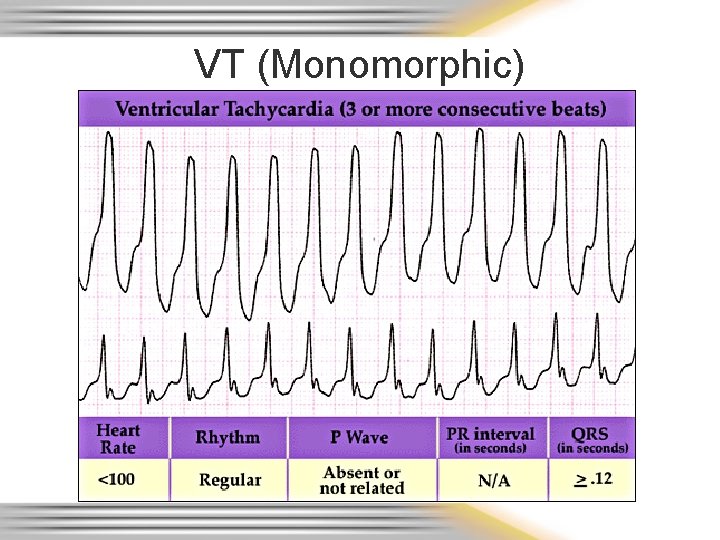
VT (Monomorphic)
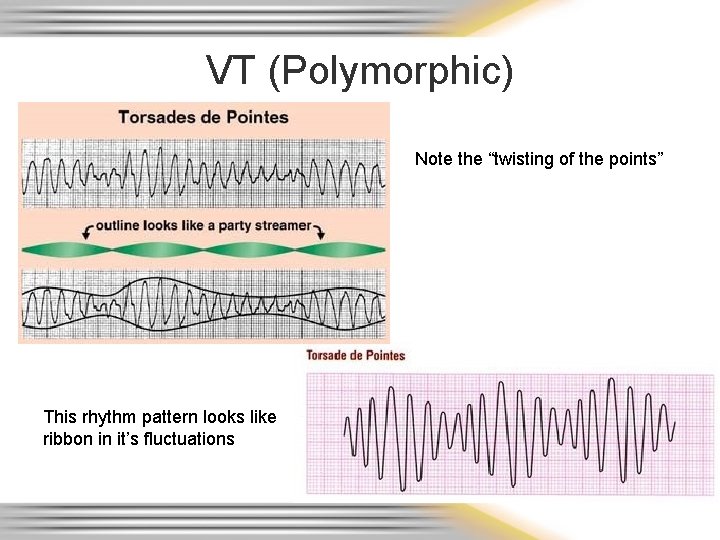
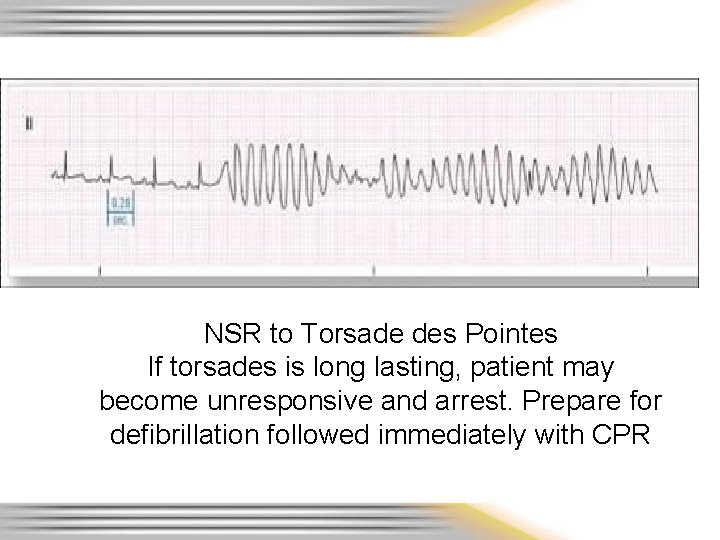
VT (Polymorphic) Note the “twisting of the points” This rhythm pattern looks like ribbon in it’s fluctuations
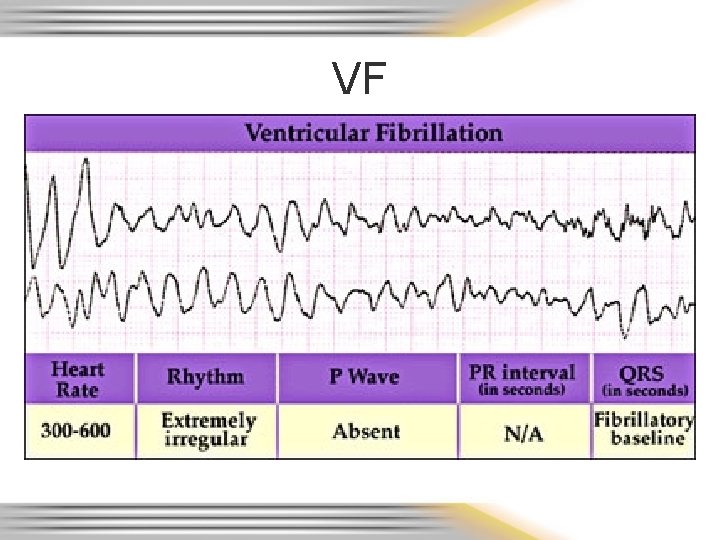
VF
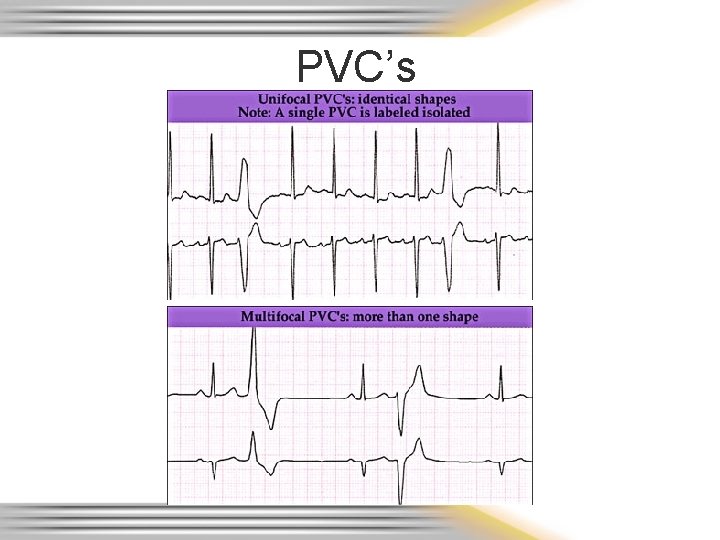
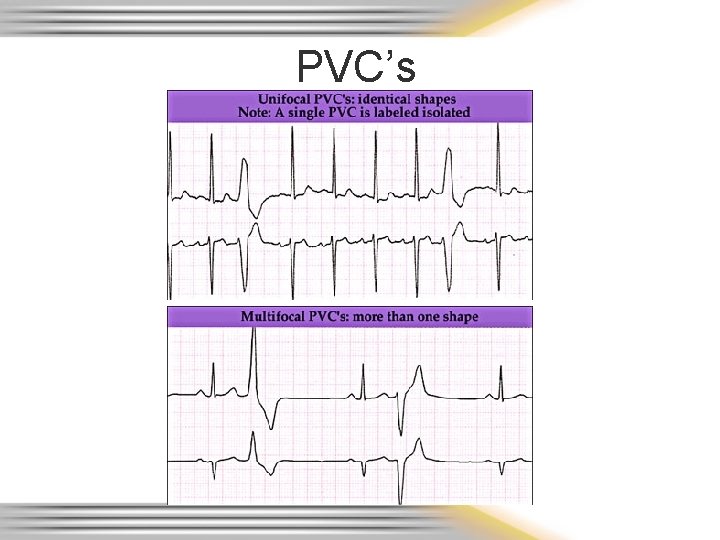
PVC’s
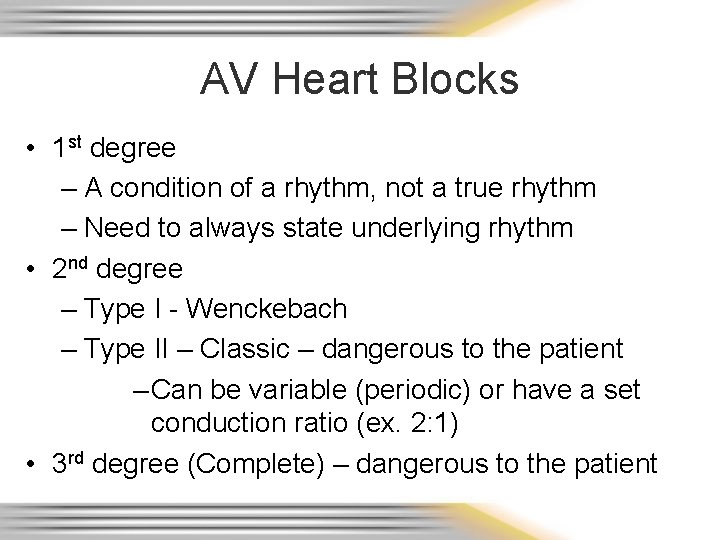
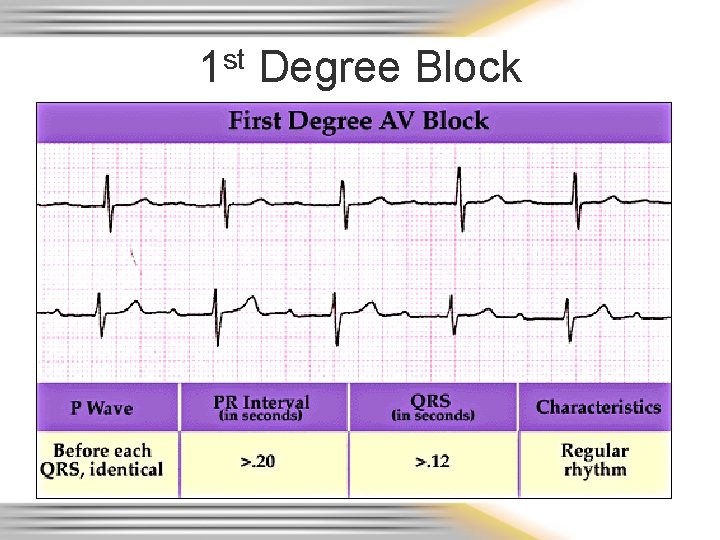
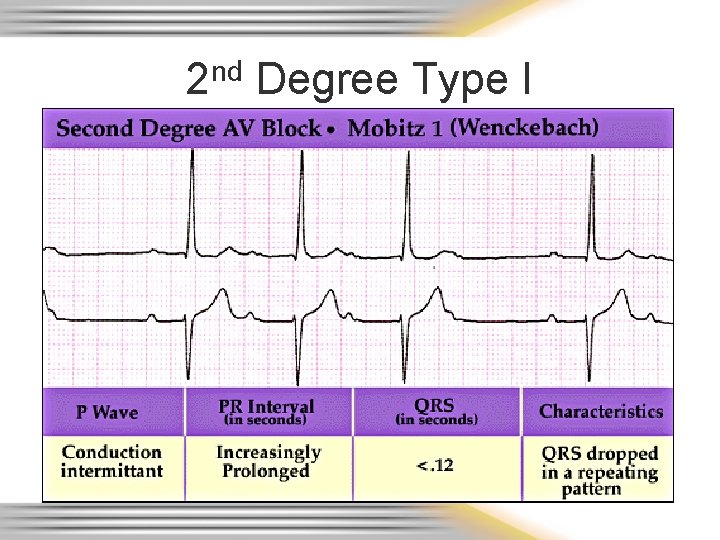
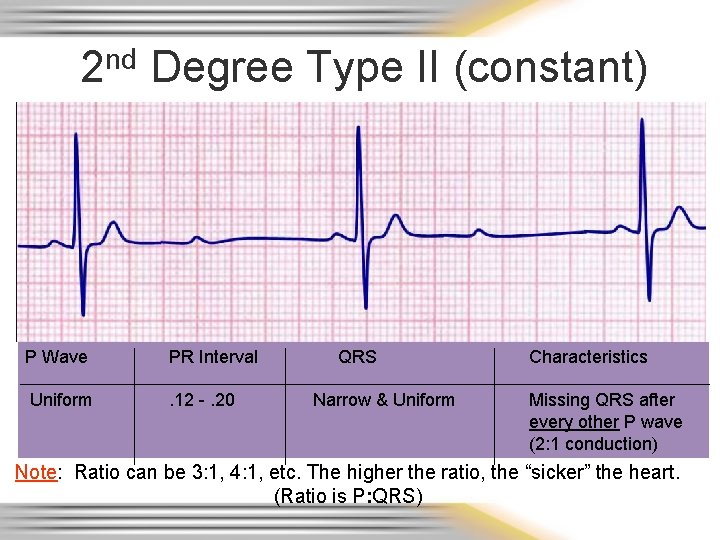
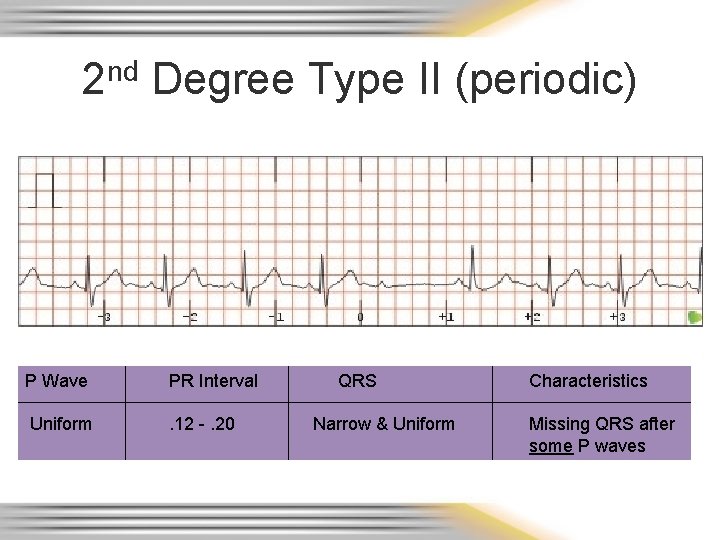
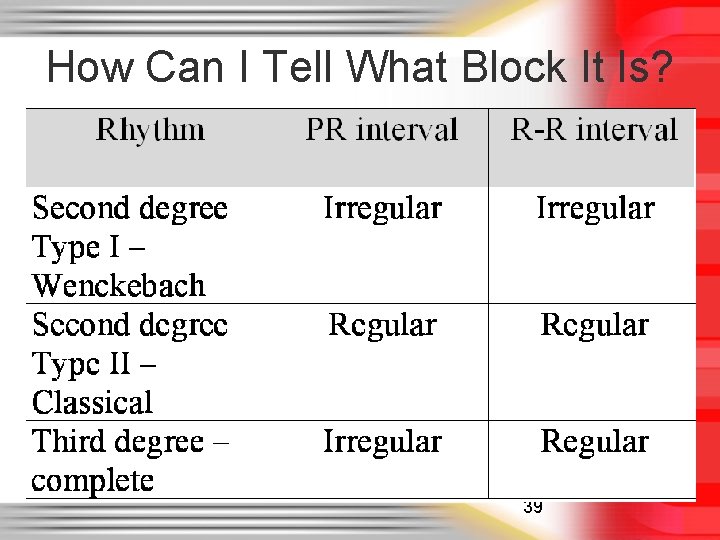
AV Heart Blocks • 1 st degree – A condition of a rhythm, not a true rhythm – Need to always state underlying rhythm • 2 nd degree – Type I - Wenckebach – Type II – Classic – dangerous to the patient – Can be variable (periodic) or have a set conduction ratio (ex. 2: 1) • 3 rd degree (Complete) – dangerous to the patient
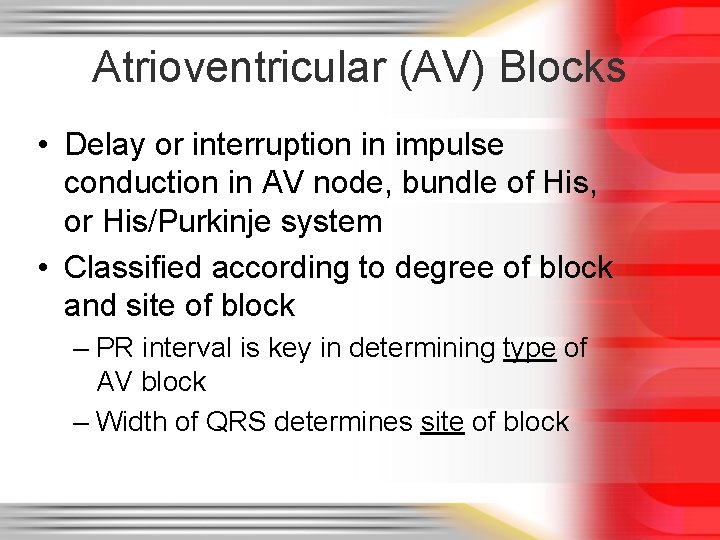
Atrioventricular (AV) Blocks • Delay or interruption in impulse conduction in AV node, bundle of His, or His/Purkinje system • Classified according to degree of block and site of block – PR interval is key in determining type of AV block – Width of QRS determines site of block
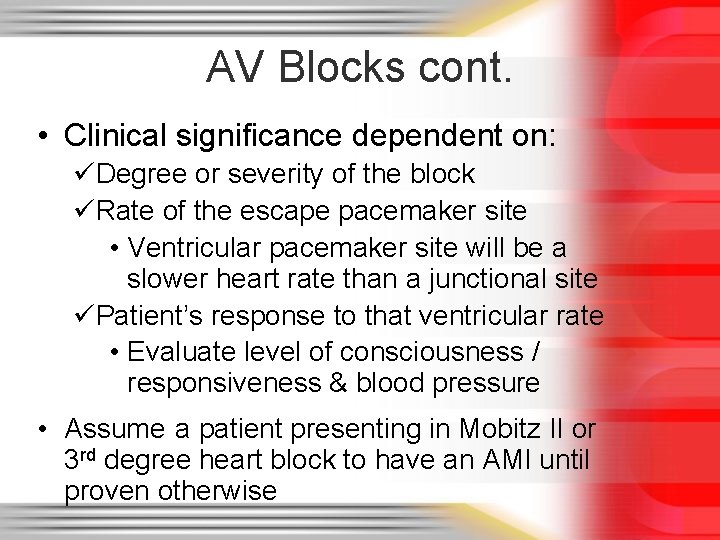
AV Blocks cont. • Clinical significance dependent on: üDegree or severity of the block üRate of the escape pacemaker site • Ventricular pacemaker site will be a slower heart rate than a junctional site üPatient’s response to that ventricular rate • Evaluate level of consciousness / responsiveness & blood pressure • Assume a patient presenting in Mobitz II or 3 rd degree heart block to have an AMI until proven otherwise
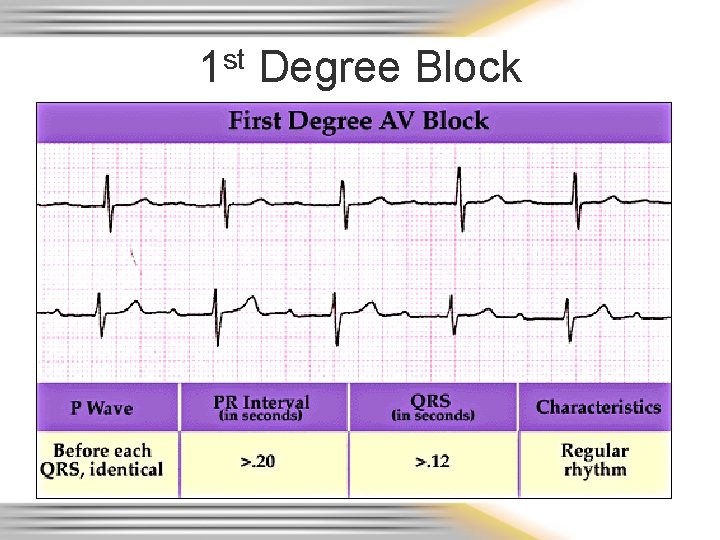
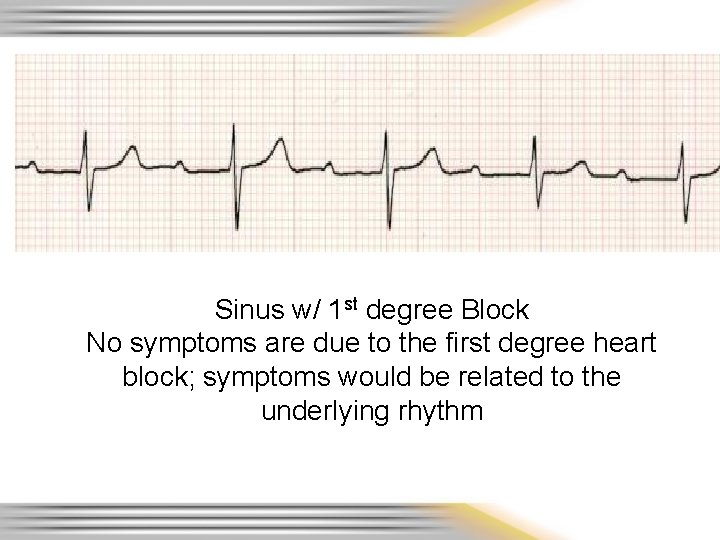
1 st Degree Block
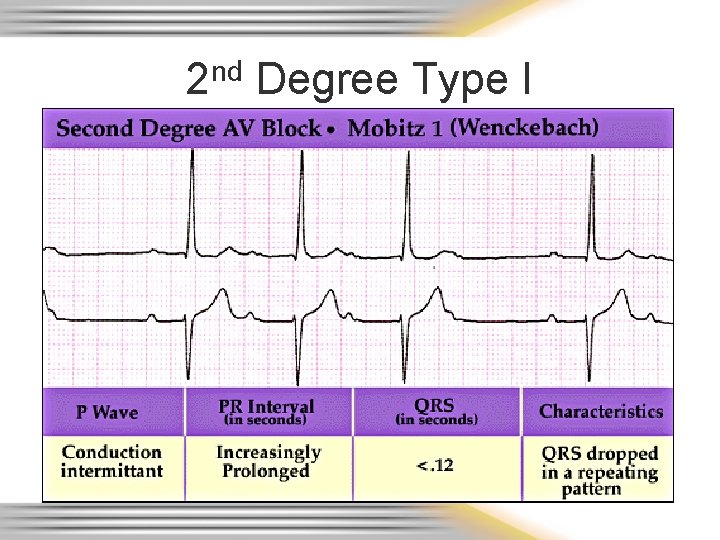
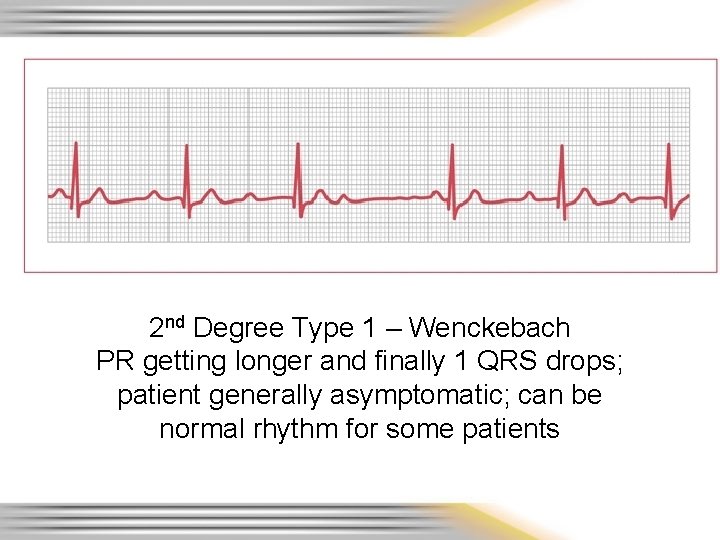
2 nd Degree Type I
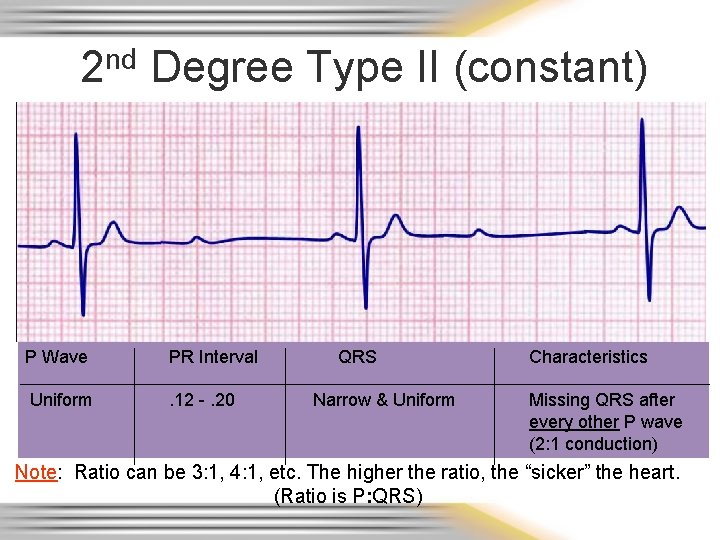
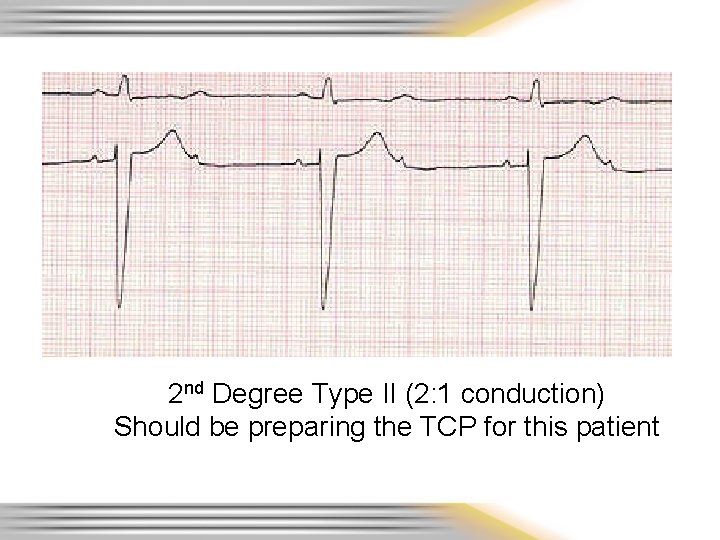
2 nd Degree Type II (constant) P Wave PR Interval Uniform . 12 -. 20 QRS Narrow & Uniform Characteristics Missing QRS after every other P wave (2: 1 conduction) Note: Ratio can be 3: 1, 4: 1, etc. The higher the ratio, the “sicker” the heart. (Ratio is P: QRS)
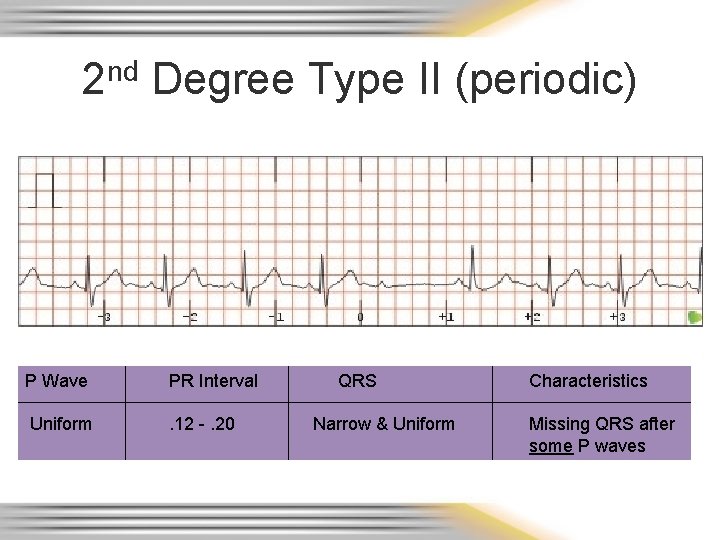
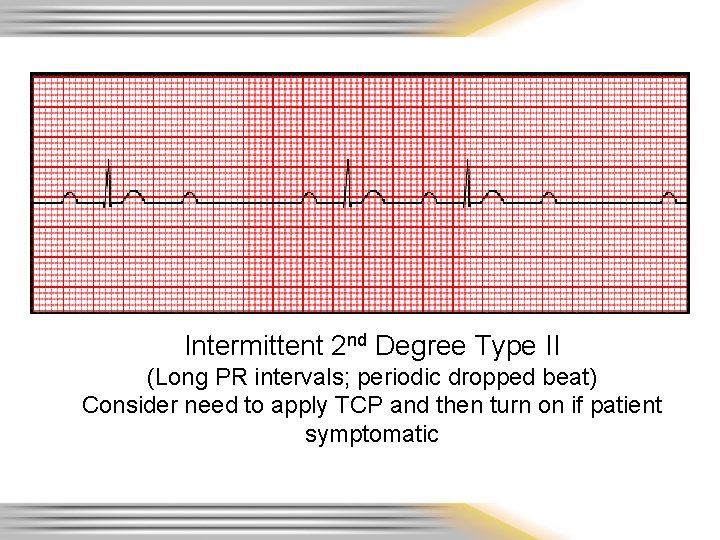
2 nd Degree Type II (periodic) P Wave PR Interval Uniform . 12 -. 20 QRS Narrow & Uniform Characteristics Missing QRS after some P waves
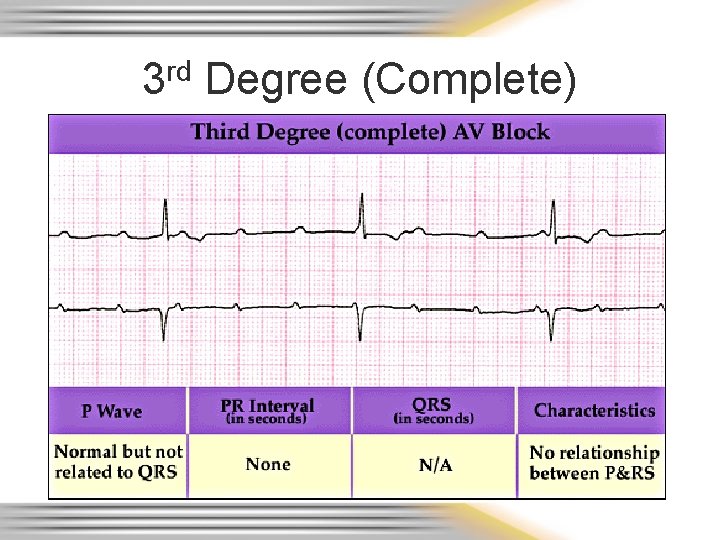
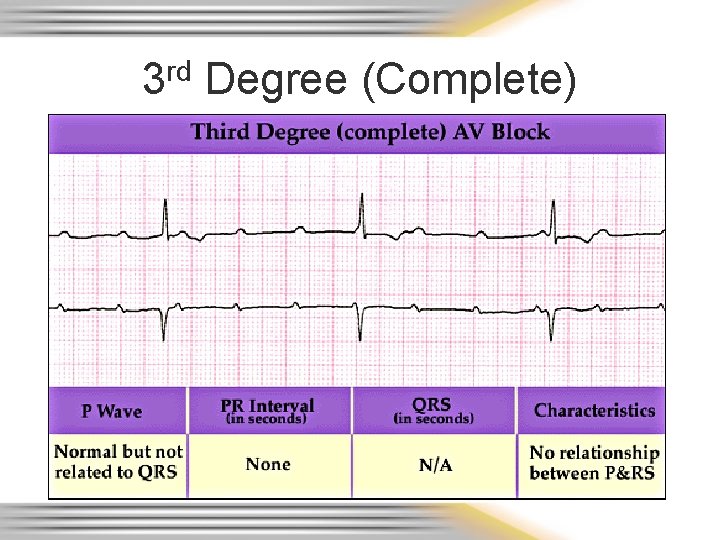
3 rd Degree (Complete)
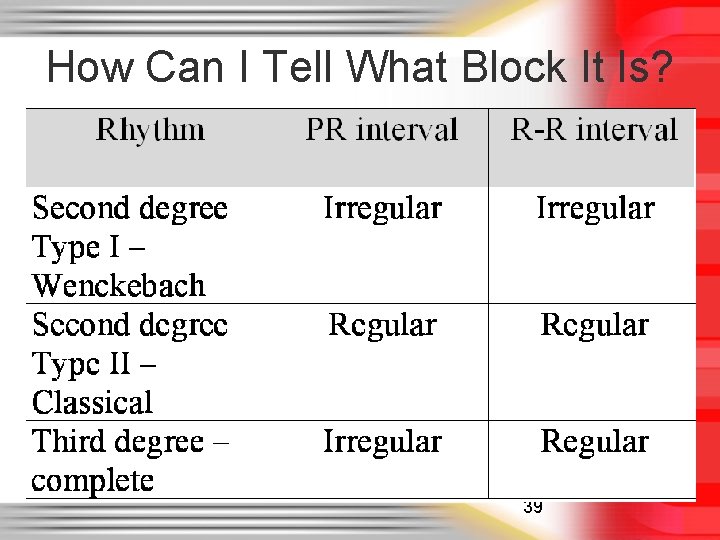
How Can I Tell What Block It Is? 39
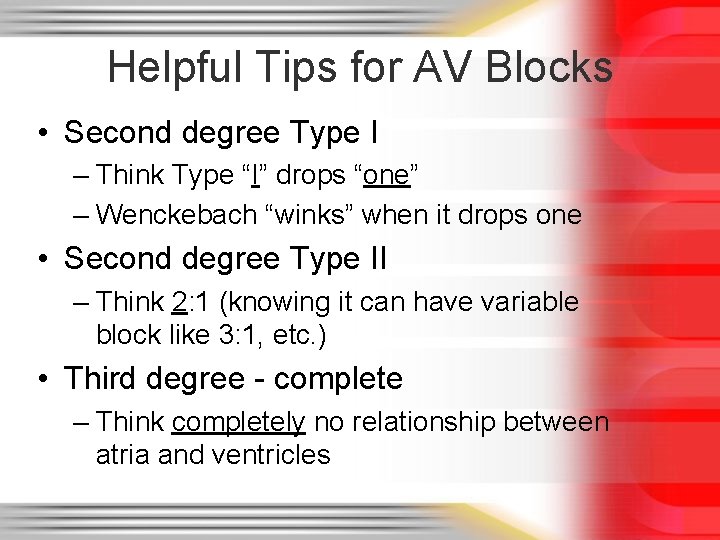
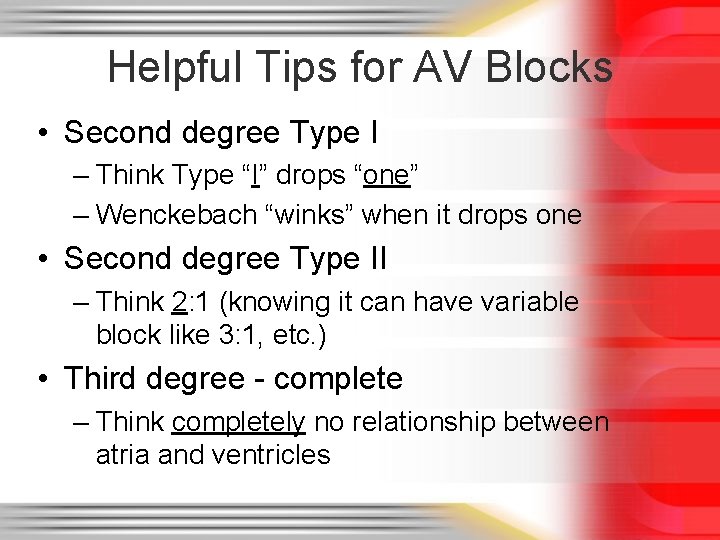
Helpful Tips for AV Blocks • Second degree Type I – Think Type “I” drops “one” – Wenckebach “winks” when it drops one • Second degree Type II – Think 2: 1 (knowing it can have variable block like 3: 1, etc. ) • Third degree - complete – Think completely no relationship between atria and ventricles
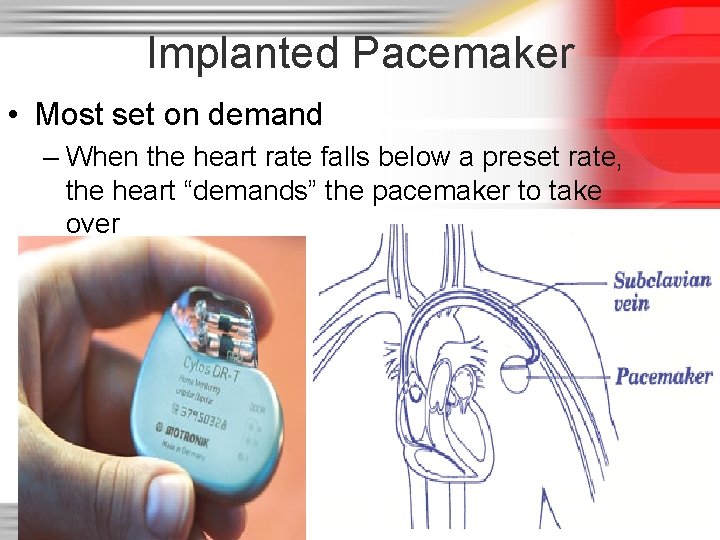
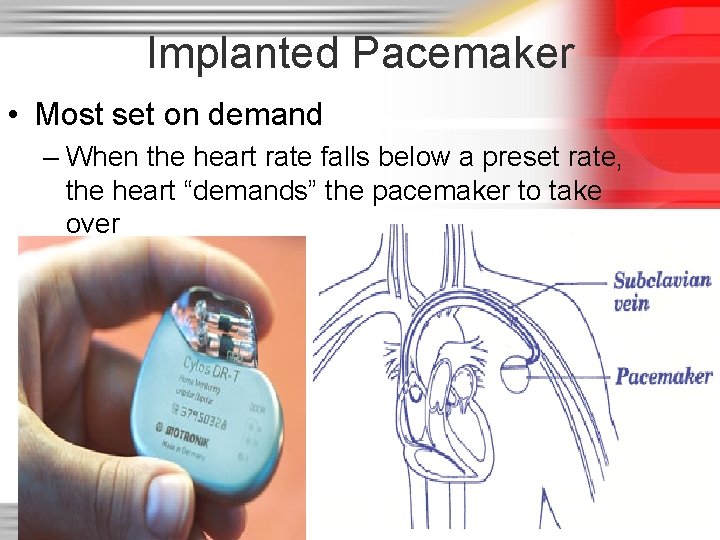
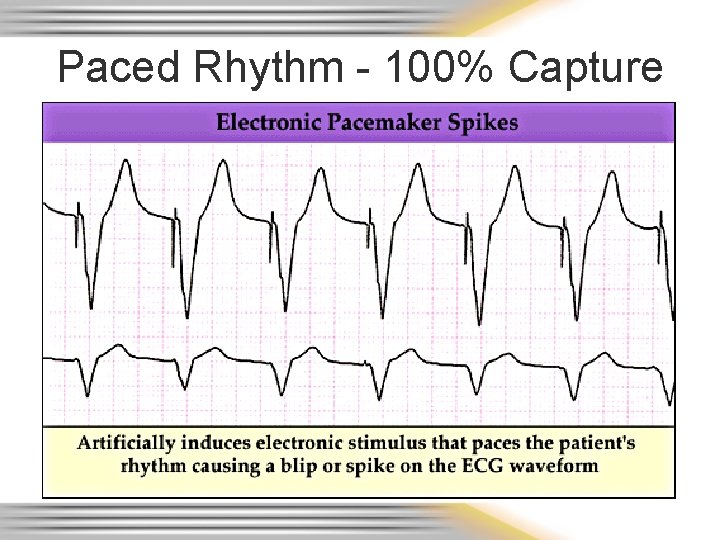
Implanted Pacemaker • Most set on demand – When the heart rate falls below a preset rate, the heart “demands” the pacemaker to take over 41
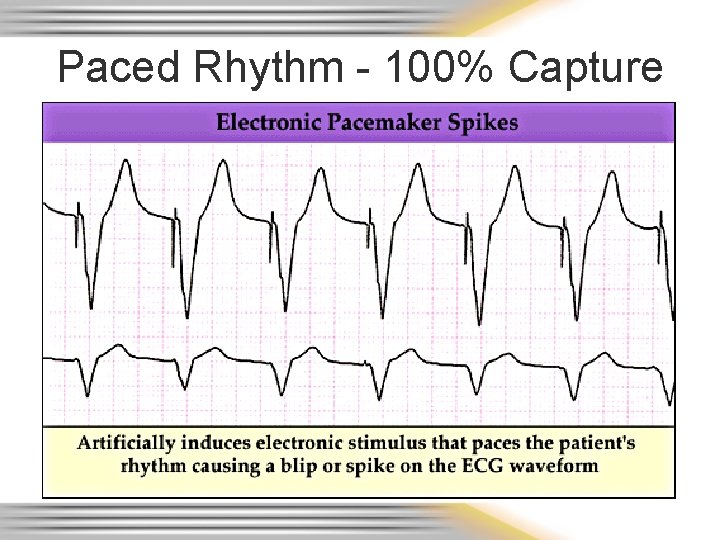
Paced Rhythm - 100% Capture
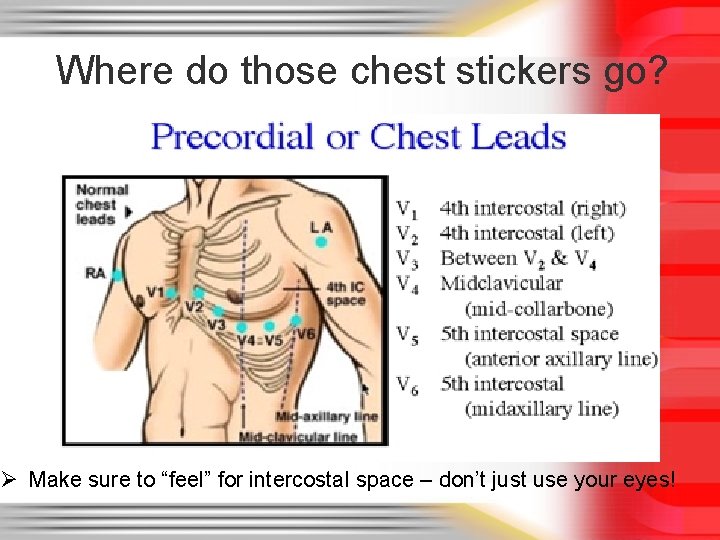
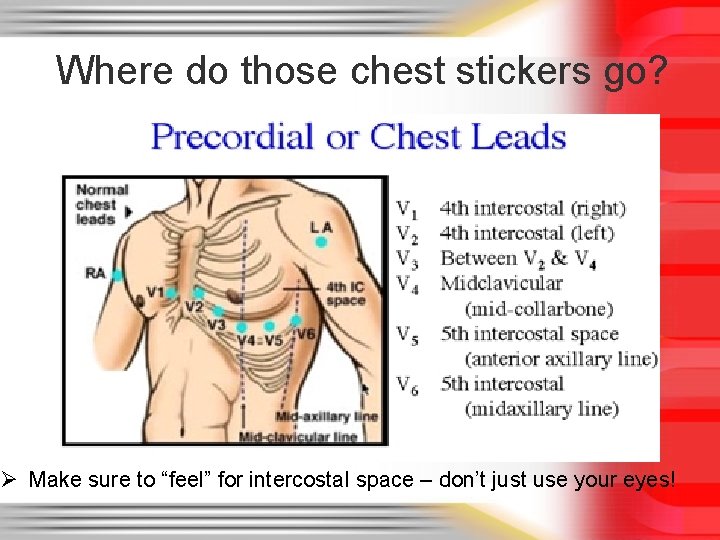
Where do those chest stickers go? Ø Make sure to “feel” for intercostal space – don’t just use your eyes!
……and the FEMALES • Not all nipple lines are created equal • Measure intercostal spaces to be accurate in electrode placement – All 12 leads measured from same electrode placement
Lead Placement in the Female • Avoid placing electrodes on top of breast tissue • Use the back of the hand to displace breast tissue out of the way to place electrode – Avoids perception of “groping” – Can ask the patient to move left breast out of way.
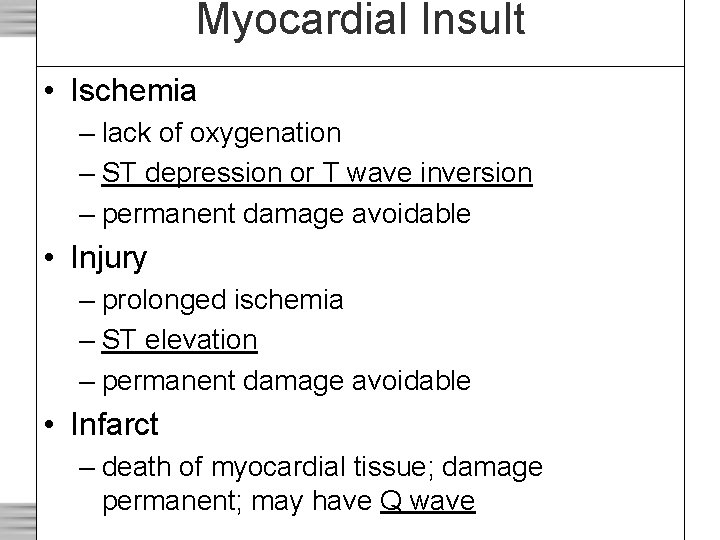
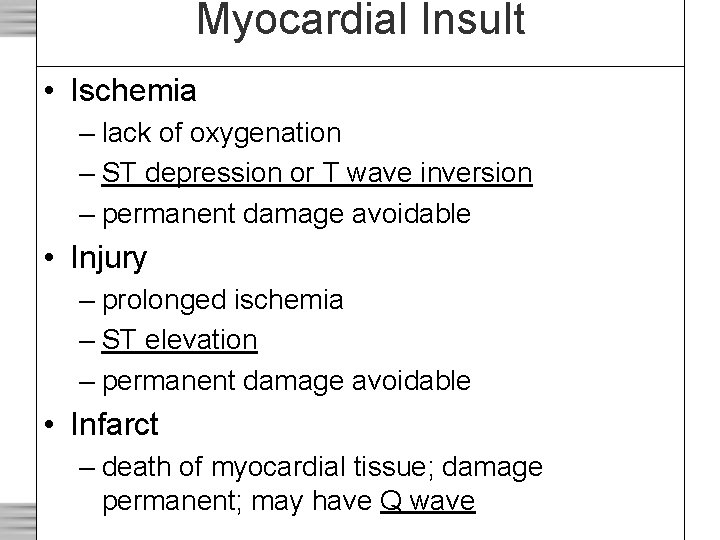
Myocardial Insult • Ischemia – lack of oxygenation – ST depression or T wave inversion – permanent damage avoidable • Injury – prolonged ischemia – ST elevation – permanent damage avoidable • Infarct – death of myocardial tissue; damage permanent; may have Q wave
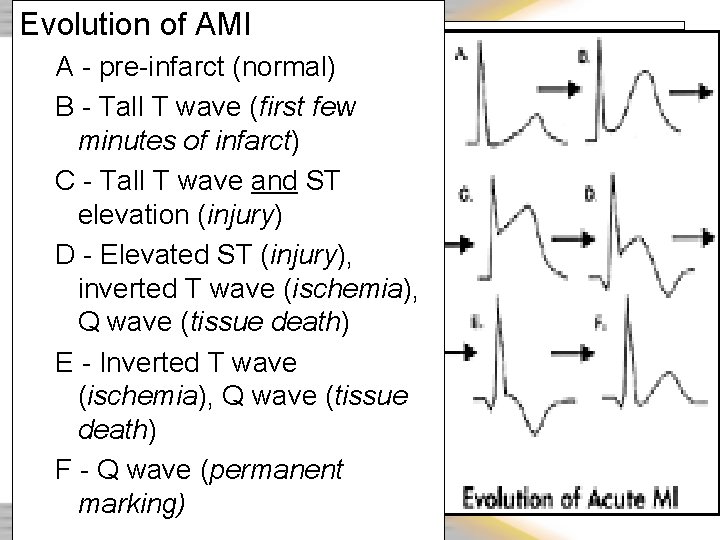
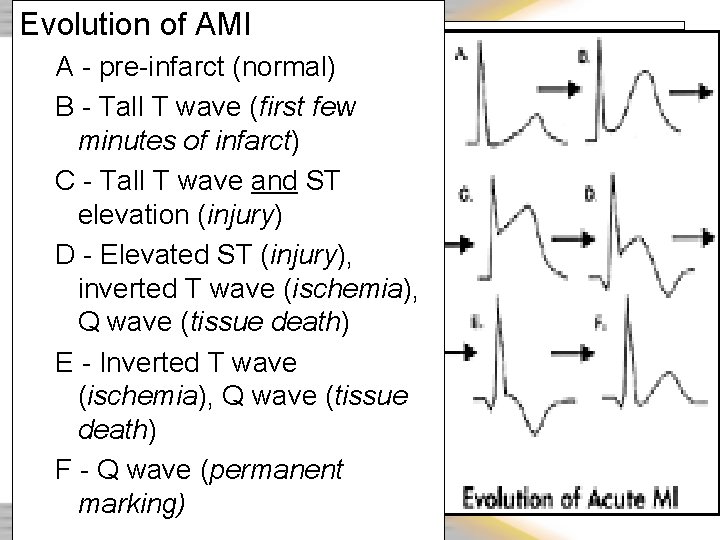
Evolution of AMI A - pre-infarct (normal) B - Tall T wave (first few minutes of infarct) C - Tall T wave and ST elevation (injury) D - Elevated ST (injury), inverted T wave (ischemia), Q wave (tissue death) E - Inverted T wave (ischemia), Q wave (tissue death) F - Q wave (permanent marking)
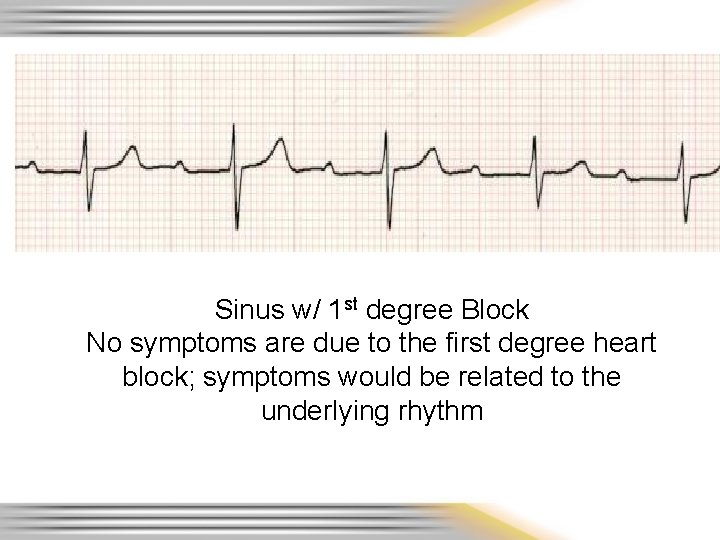
Sinus w/ 1 st degree Block No symptoms are due to the first degree heart block; symptoms would be related to the underlying rhythm
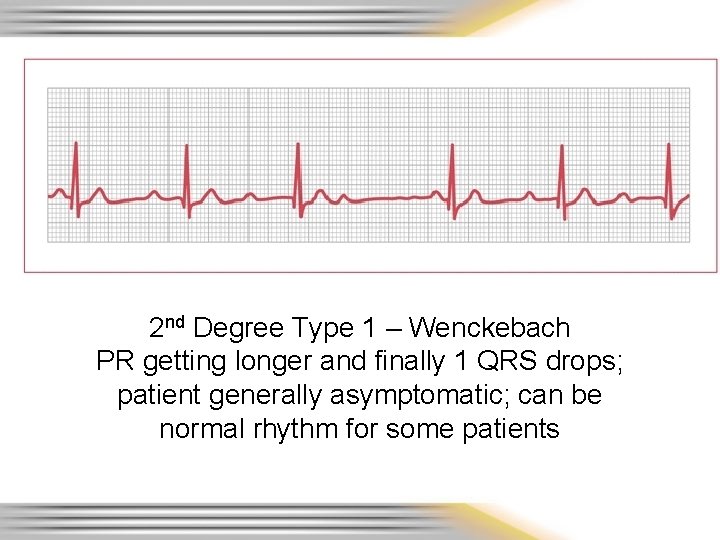
2 nd Degree Type 1 – Wenckebach PR getting longer and finally 1 QRS drops; patient generally asymptomatic; can be normal rhythm for some patients
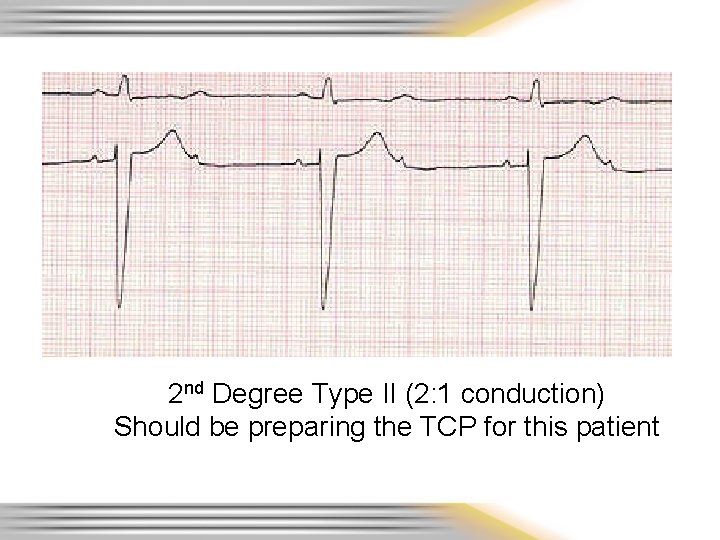
2 nd Degree Type II (2: 1 conduction) Should be preparing the TCP for this patient
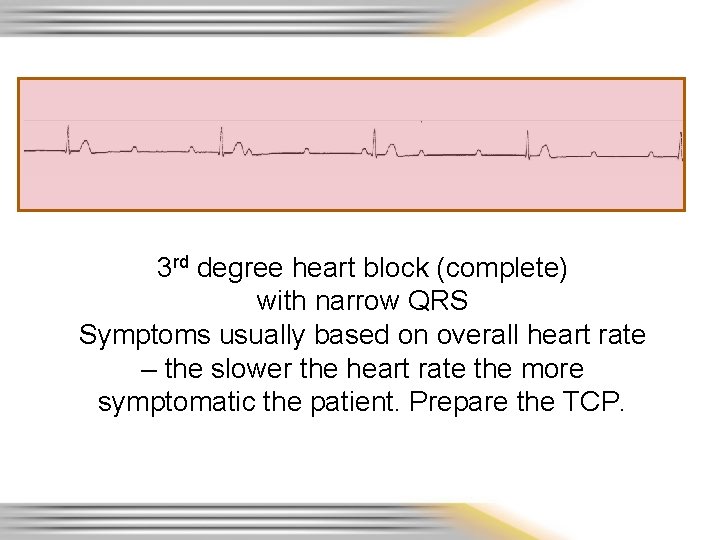
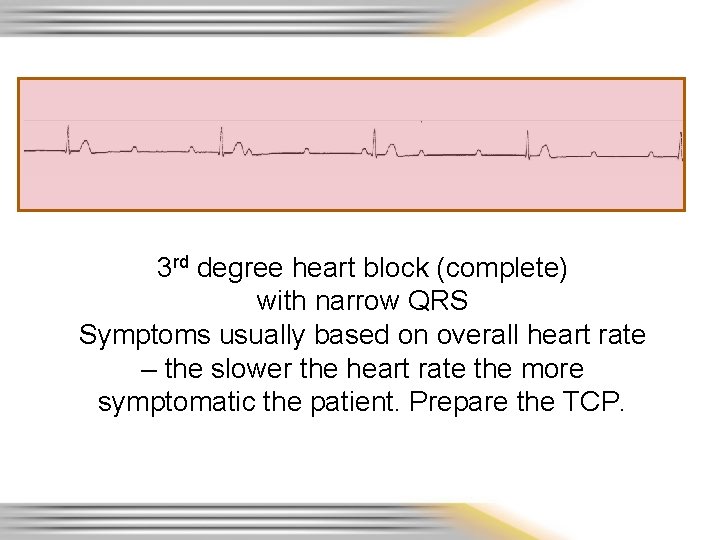
3 rd degree heart block (complete) with narrow QRS Symptoms usually based on overall heart rate – the slower the heart rate the more symptomatic the patient. Prepare the TCP.
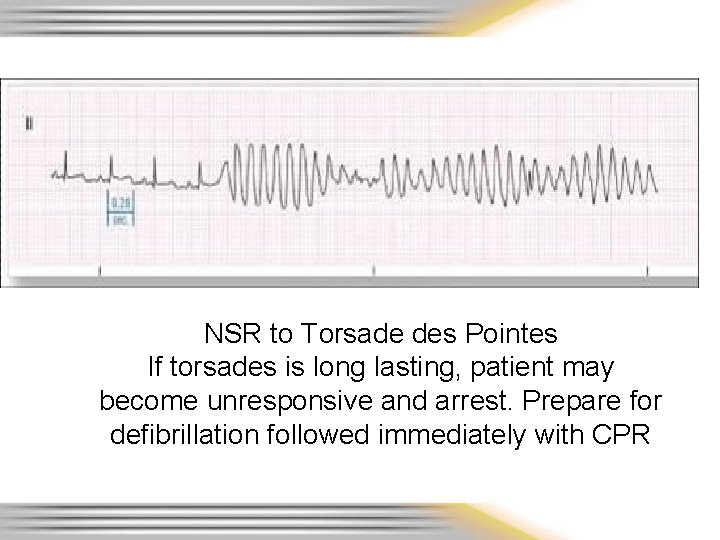
NSR to Torsade des Pointes If torsades is long lasting, patient may become unresponsive and arrest. Prepare for defibrillation followed immediately with CPR
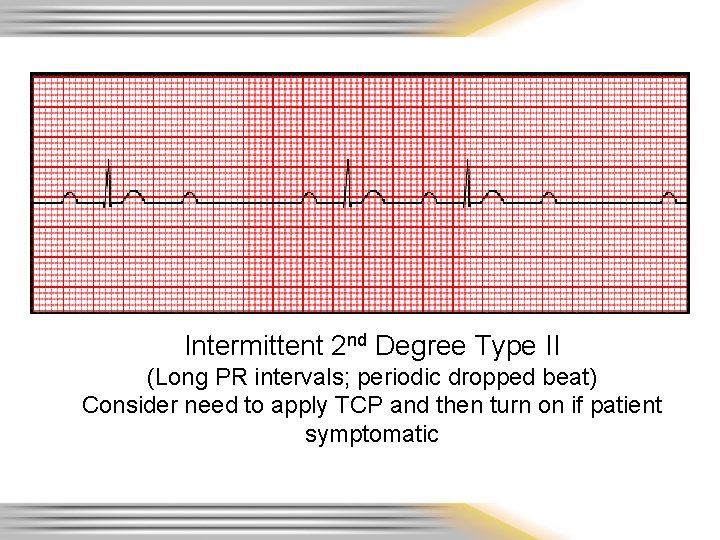
Intermittent 2 nd Degree Type II (Long PR intervals; periodic dropped beat) Consider need to apply TCP and then turn on if patient symptomatic
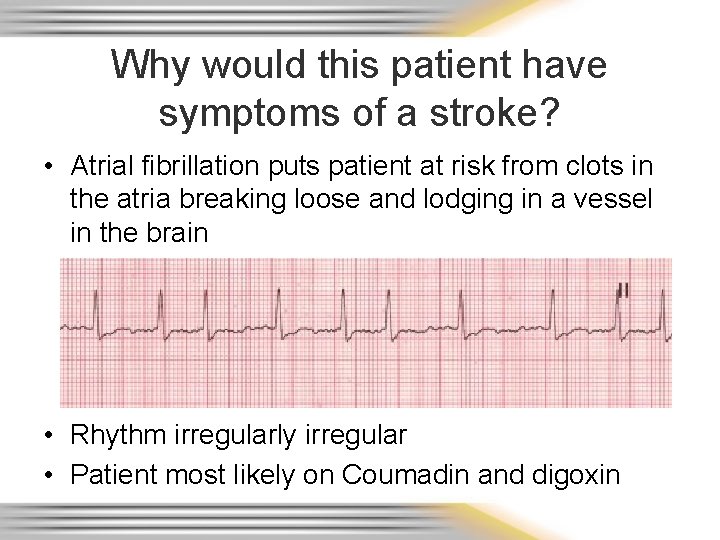
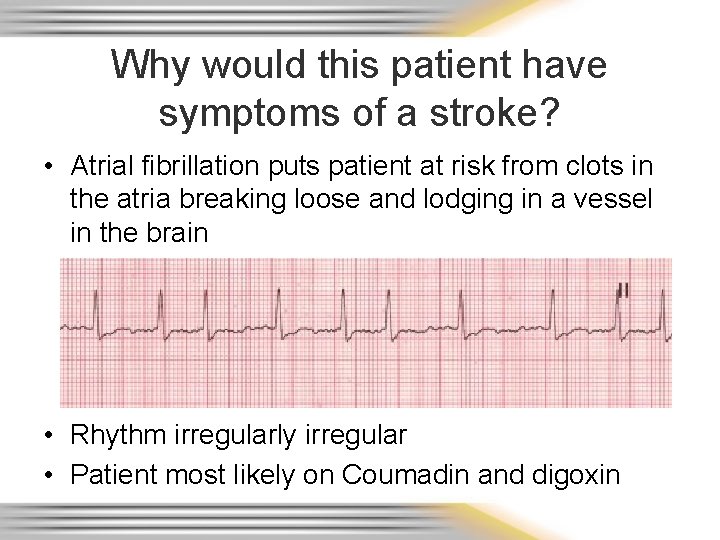
Why would this patient have symptoms of a stroke? • Atrial fibrillation puts patient at risk from clots in the atria breaking loose and lodging in a vessel in the brain • Rhythm irregularly irregular • Patient most likely on Coumadin and digoxin
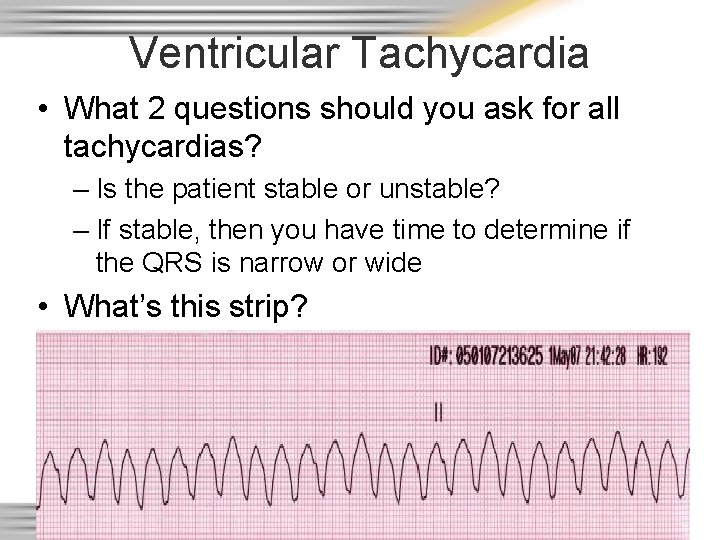
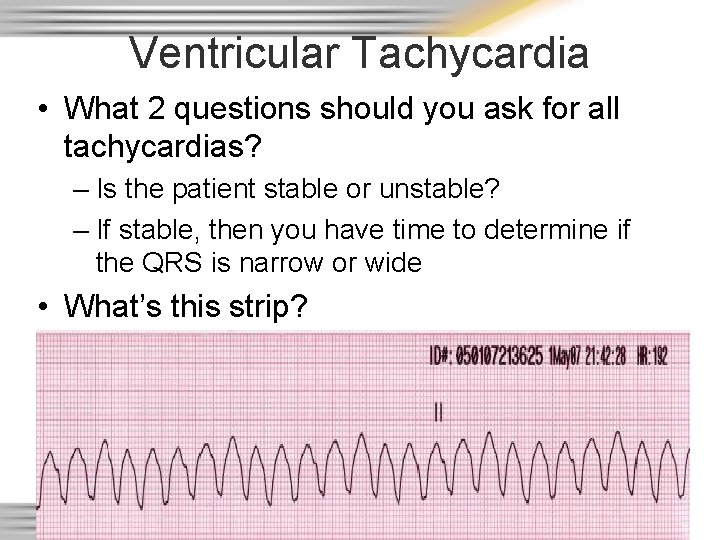
Ventricular Tachycardia • What 2 questions should you ask for all tachycardias? – Is the patient stable or unstable? – If stable, then you have time to determine if the QRS is narrow or wide • What’s this strip?
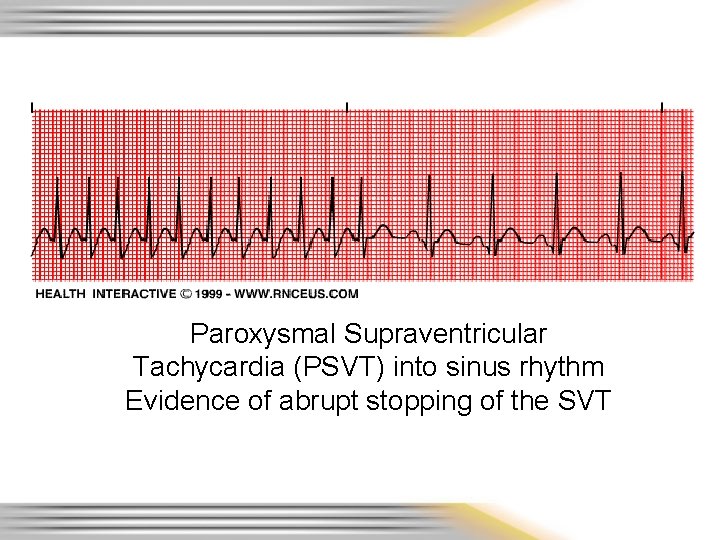
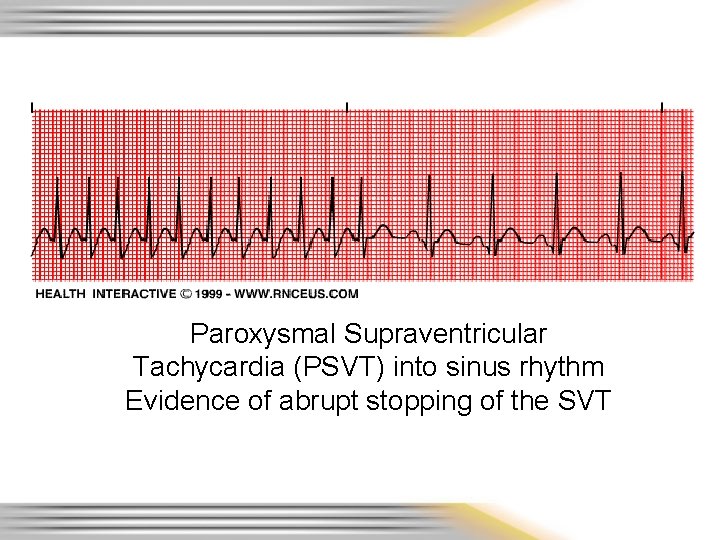
Paroxysmal Supraventricular Tachycardia (PSVT) into sinus rhythm Evidence of abrupt stopping of the SVT
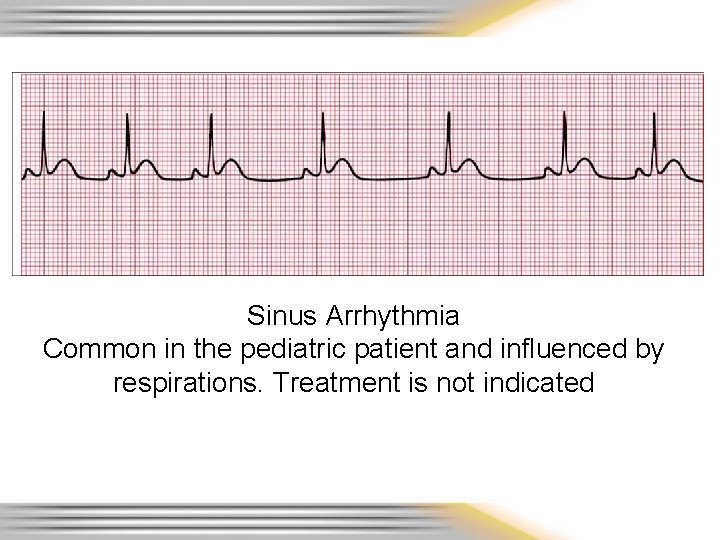
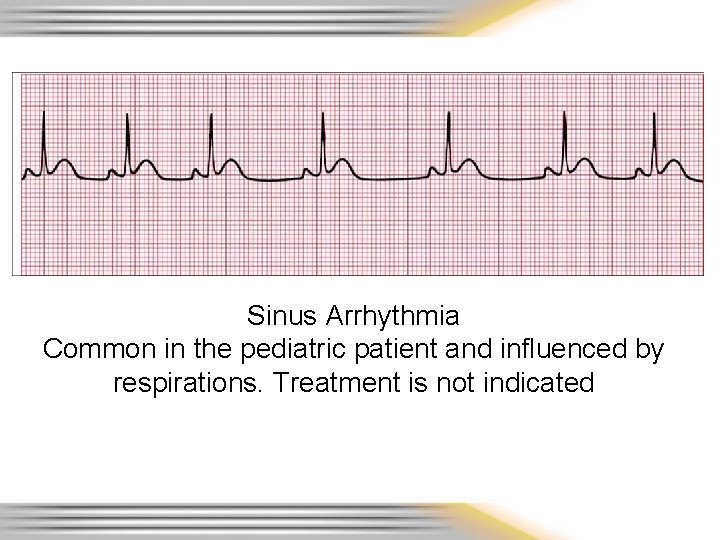
Sinus Arrhythmia Common in the pediatric patient and influenced by respirations. Treatment is not indicated
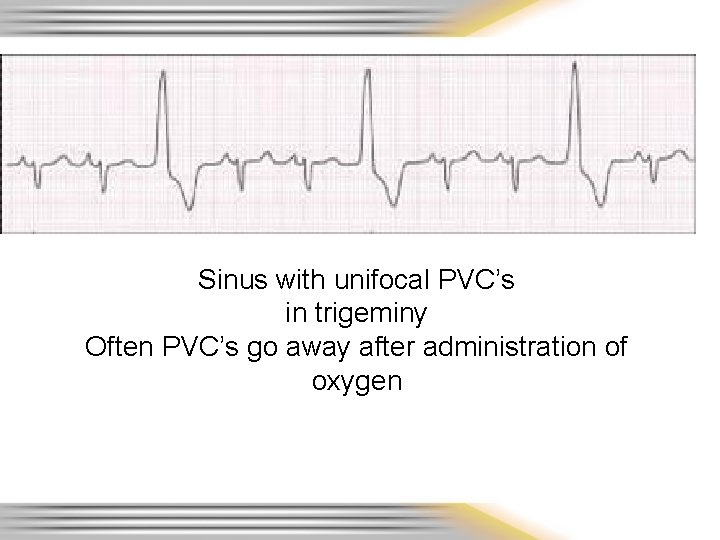
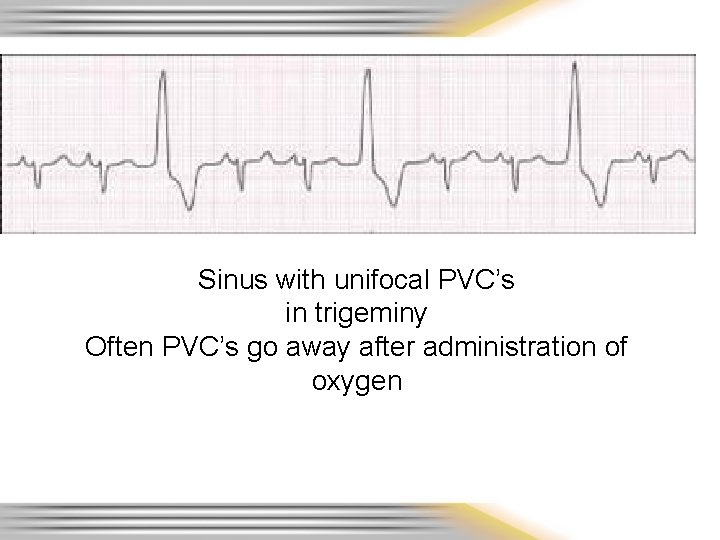
Sinus with unifocal PVC’s in trigeminy Often PVC’s go away after administration of oxygen
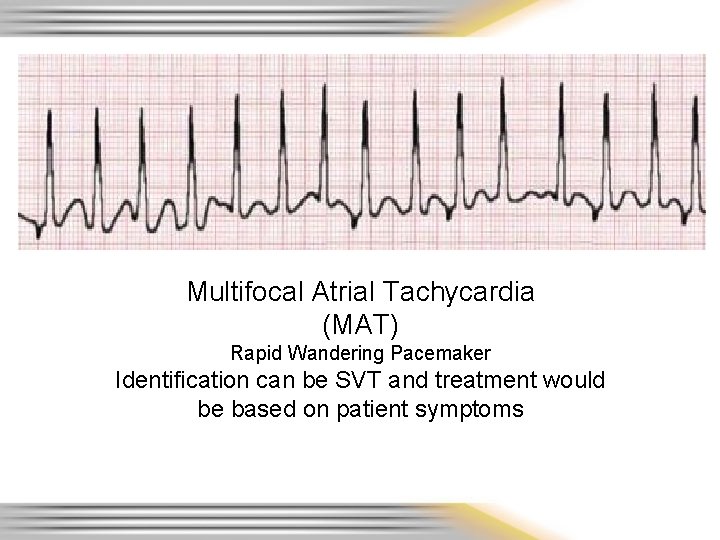
Multifocal Atrial Tachycardia (MAT) Rapid Wandering Pacemaker Identification can be SVT and treatment would be based on patient symptoms
12 – Lead Time! • Same as Lead II strips – Identify ST elevation and try to give anatomical locations • May not be able to view grid lines but should be able to pick up ST elevation when present – Remember to be watchful for typical complications based on location of infarct and blocked coronary vessel
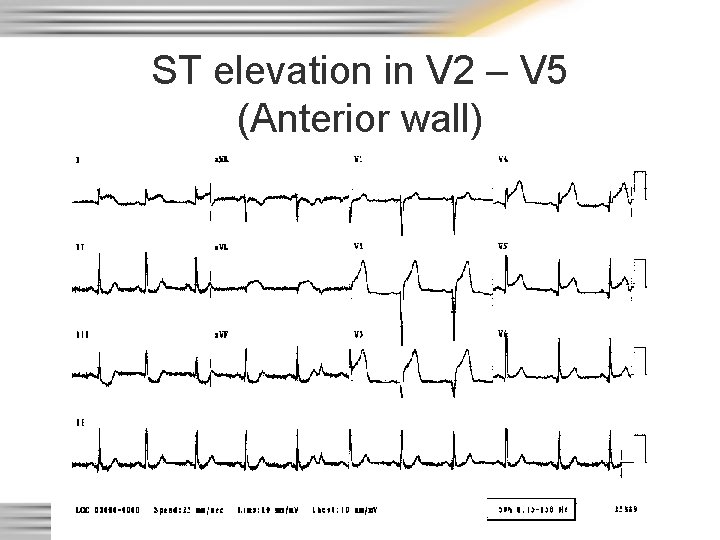
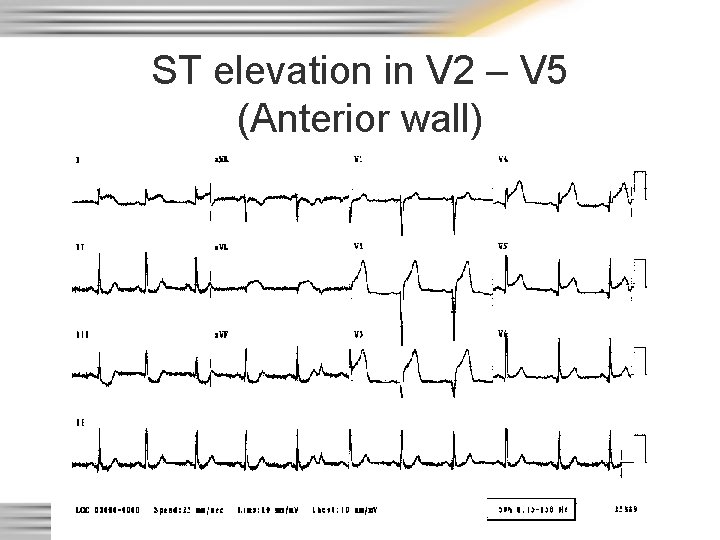
ST elevation in V 2 – V 5 (Anterior wall)
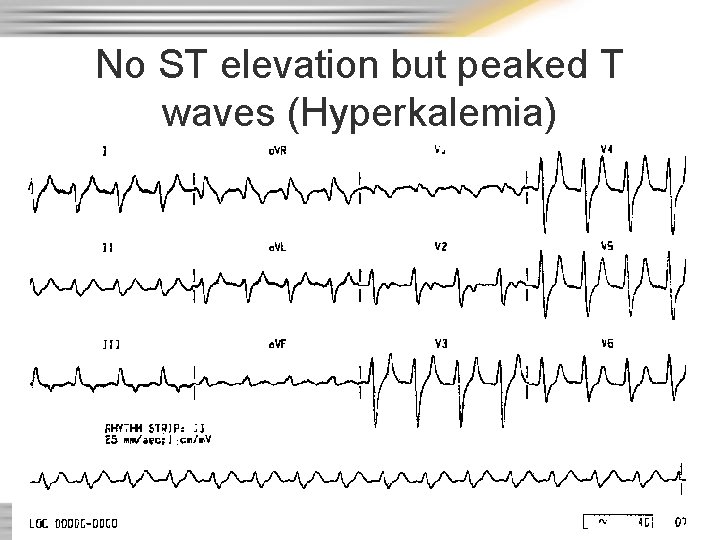
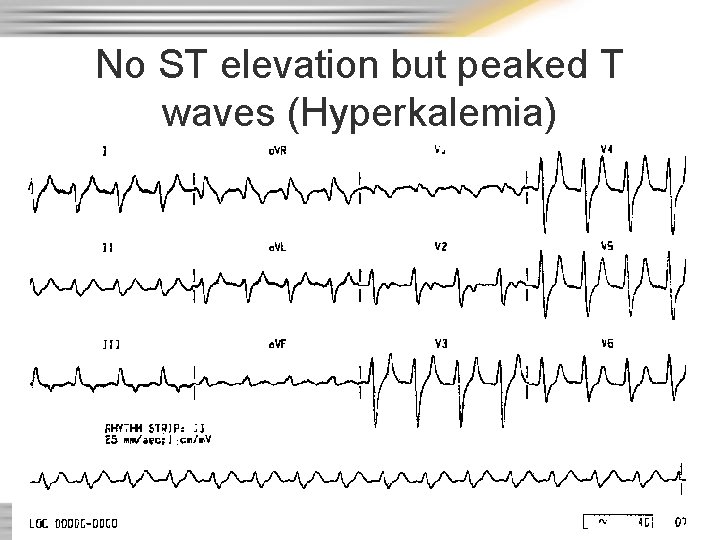
No ST elevation but peaked T waves (Hyperkalemia)