Revive Initiative at Stanford Childrens Health Synergy Pediatric










- Slides: 30
Revive Initiative at Stanford Children’s Health Synergy Pediatric Resuscitation Program Lynda J. Knight RN, MSN, CPN
Presenter Disclosure Information Lynda J. Knight, MSN, RN Improving Code Team Performance and Survival Outcomes: Implementation of Pediatric Resuscitation Team Training FINANCIAL DISCLOSURE: § No Financial Disclosures UNLABELED/UNAPPROVED USES DISCLOSURE: § NONE
“the interaction or cooperation of two or more organizations …to produce a combined effect greater than the sum of their separate effects”
The IOM Report June 30 th, 2015 “A national responsibility exists to improve the likelihood of survival and favorable neurologic out- comes following a cardiac arrest. This will require immediate changes in cardiac arrest reporting, research, training, and treatment.
The IOM Report June 30 th, 2015 • • • Should adopt formal, continuous quality improvement programs for cardiac arrest response that assign responsibility, authority, and accountability within each organization Implement core technical and nontechnical training, simulation, and debriefing protocols to ensure that EMS and hospital personnel can respond competently to both adult and pediatric cardiac arrests; and Actively collaborate and share data to facilitate national, state, and local benchmarking for quality improvement.

The IOM Report June 30 th, 2015 • Should adopt formal, continuous quality improvement programs for cardiac arrest response that assign responsibility, authority, and accountability within each organization
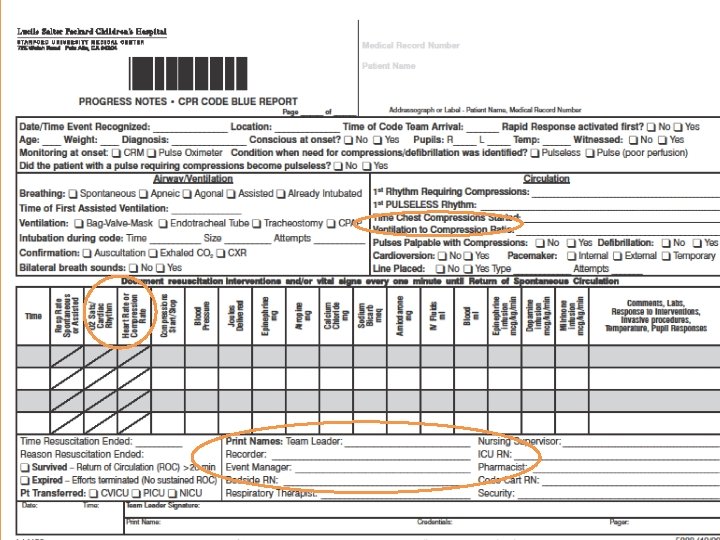
Code Committee reviews RRT & Codes monthly and identified: üPractice variability üBest practice standards not met consistently üRole Confusion and Crowd Control issues üHesitation in timely escalation of deterioration üIncomplete documentation and “hot”debrief üLack of confidence and competence due to low incidence events
The IOM Report June 30 th, 2015 • Implement core technical and nontechnical training, simulation, and debriefing protocols to ensure that EMS and hospital personnel can respond competently to both adult and pediatric cardiac arrests; and

What we know about training in teams
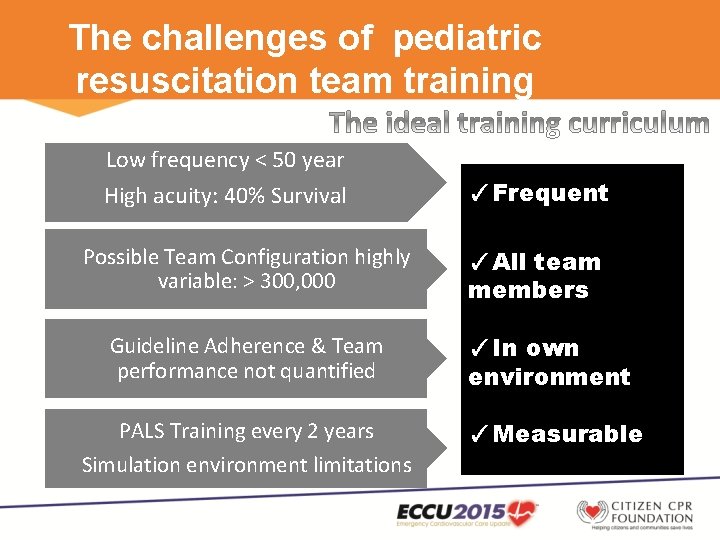
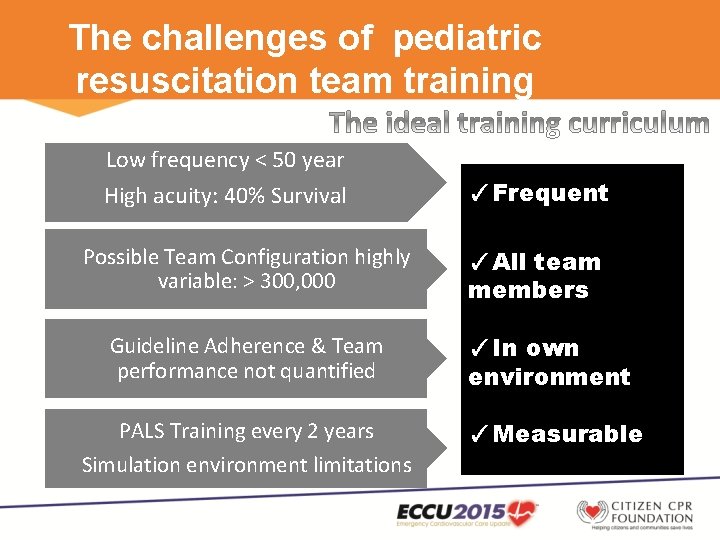
The challenges of pediatric resuscitation team training Low frequency < 50 year High acuity: 40% Survival Possible Team Configuration highly variable: > 300, 000 ✓Frequent ✓All team members Guideline Adherence & Team performance not quantified ✓In own environment PALS Training every 2 years ✓Measurable Simulation environment limitations
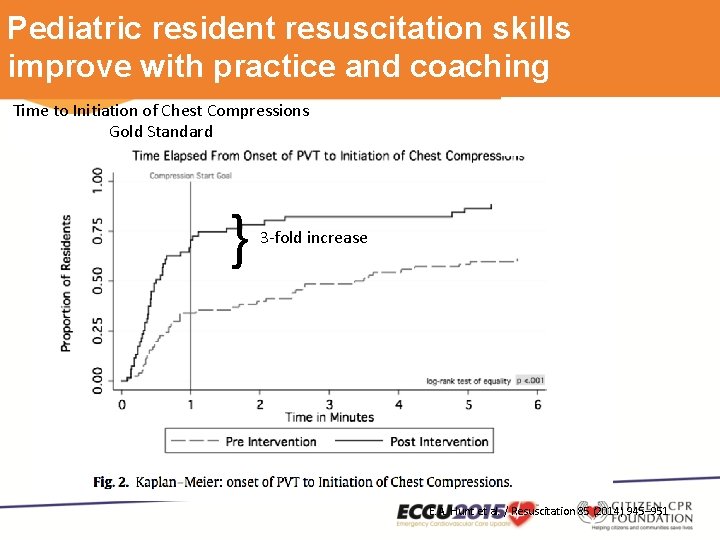
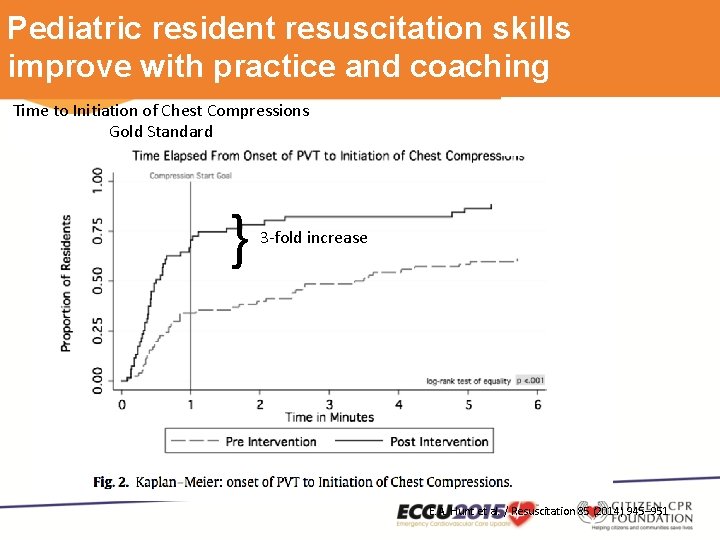
Pediatric resident resuscitation skills improve with practice and coaching Time to Initiation of Chest Compressions Gold Standard } 3 -fold increase E. A. Hunt et al. / Resuscitation 85 (2014) 945– 951
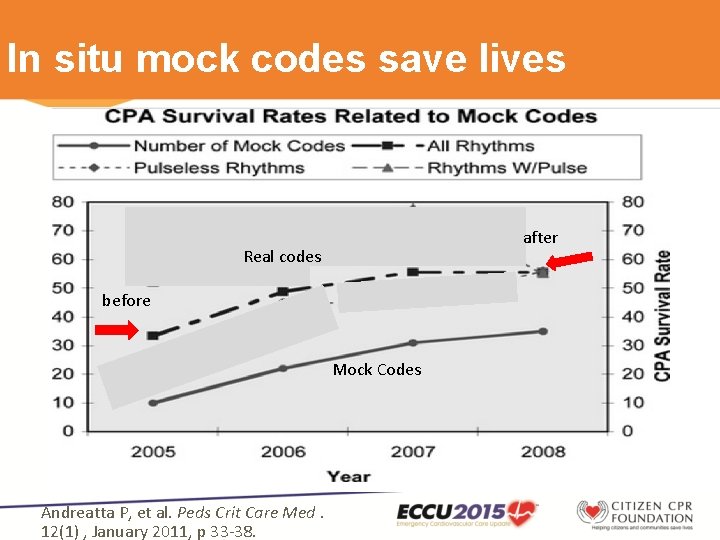
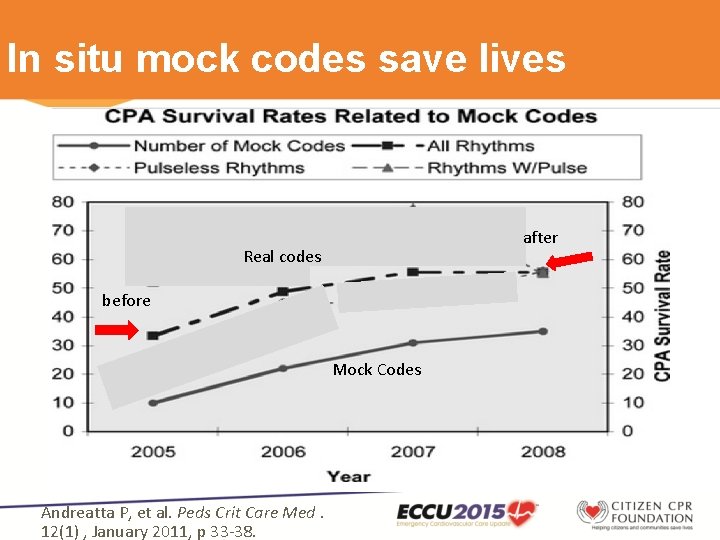
In situ mock codes save lives after Real codes before Mock Codes Andreatta P, et al. Peds Crit Care Med. 12(1) , January 2011, p 33 -38.

Could in situ training of all team members Improve survival and team performance? ✔ ✔ ✔ Knight L, et al. Crit Care Med: Volume 42(2) February 2014, p 243 -251
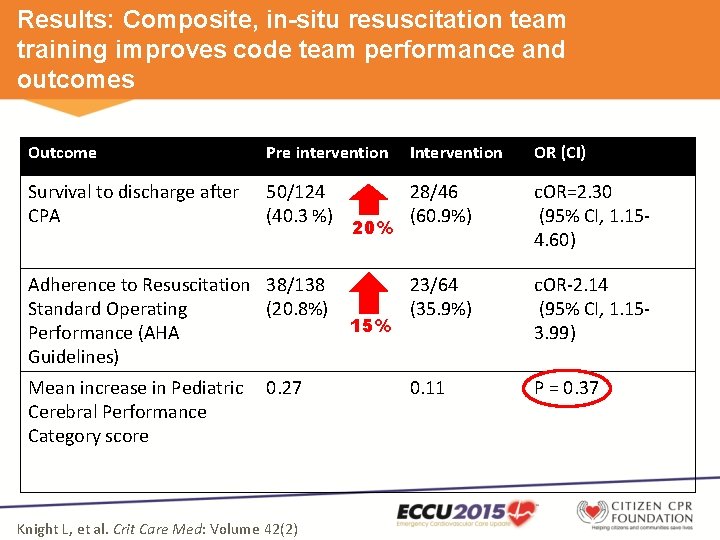
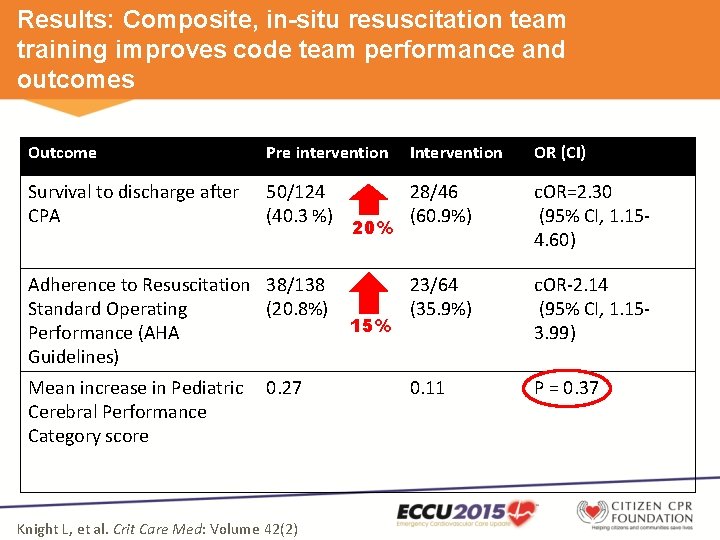
Results: Composite, in-situ resuscitation team training improves code team performance and outcomes Outcome Pre intervention Intervention OR (CI) Survival to discharge after CPA 50/124 (40. 3 %) 28/46 (60. 9%) c. OR=2. 30 (95% CI, 1. 154. 60) 23/64 (35. 9%) c. OR-2. 14 (95% CI, 1. 153. 99) 0. 11 P = 0. 37 Adherence to Resuscitation 38/138 Standard Operating (20. 8%) Performance (AHA Guidelines) Mean increase in Pediatric Cerebral Performance Category score 0. 27 Knight L, et al. Crit Care Med: Volume 42(2) 20% 15%
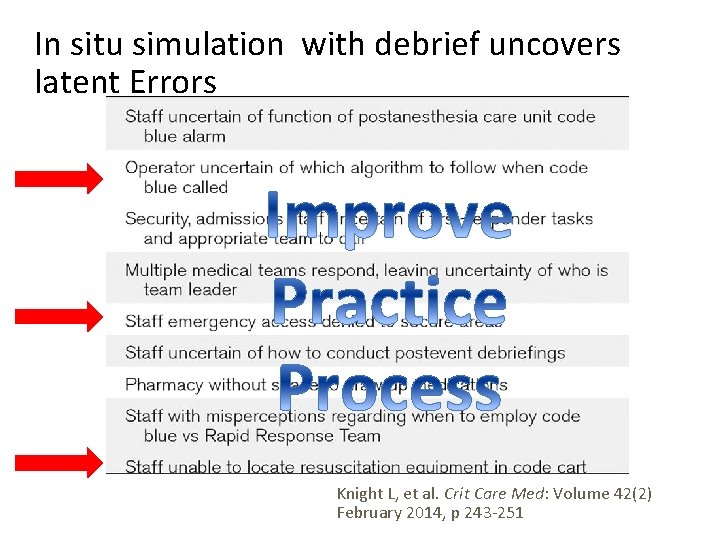
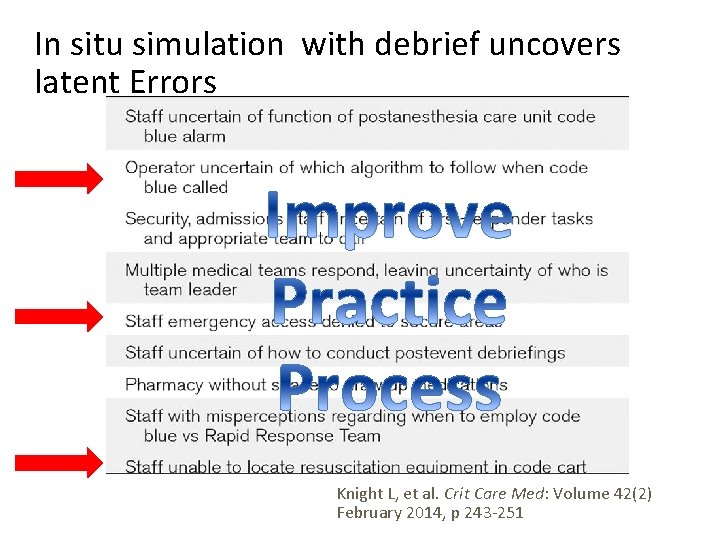
In situ simulation with debrief uncovers latent Errors Knight L, et al. Crit Care Med: Volume 42(2) February 2014, p 243 -251

IMSH 2015 Simmy Award • Add video

In-Situ Unit Schedule
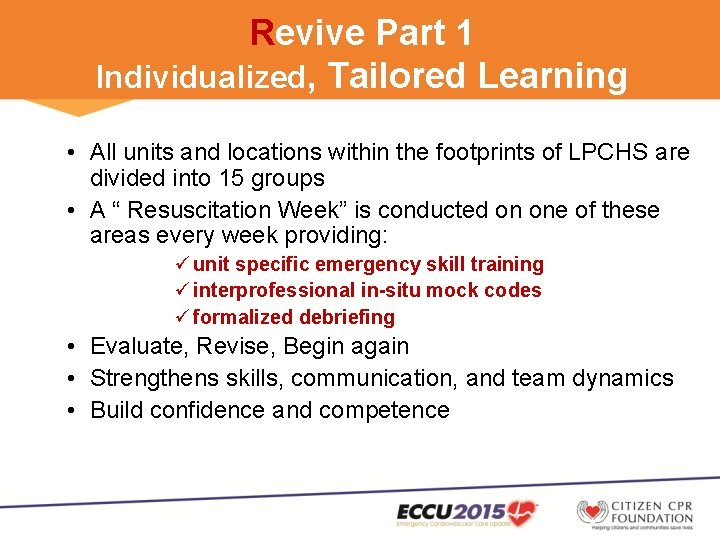
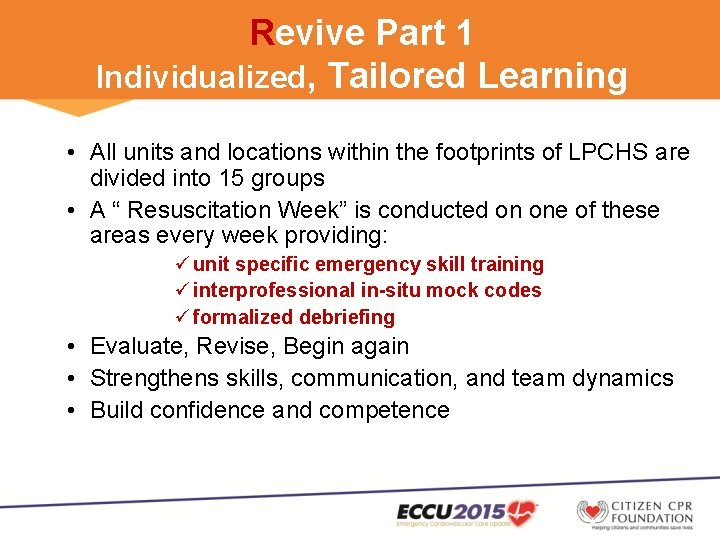
Revive Part 1 Individualized, Tailored Learning • All units and locations within the footprints of LPCHS are divided into 15 groups • A “ Resuscitation Week” is conducted on one of these areas every week providing: ü unit specific emergency skill training ü interprofessional in-situ mock codes ü formalized debriefing • Evaluate, Revise, Begin again • Strengthens skills, communication, and team dynamics • Build confidence and competence
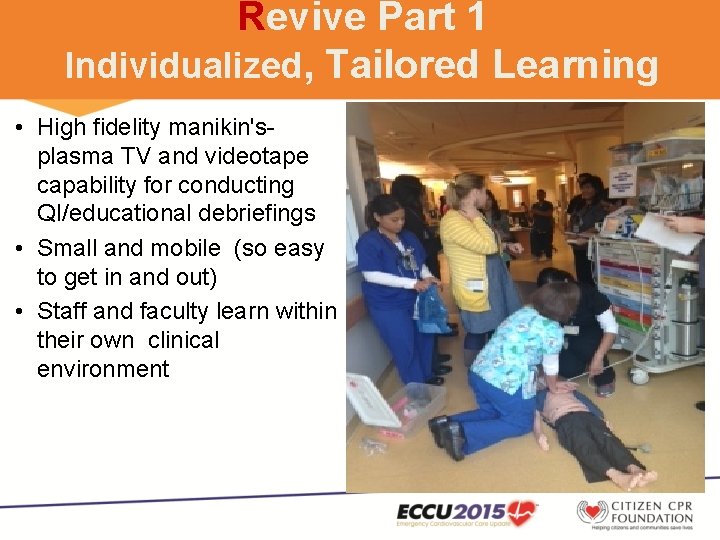
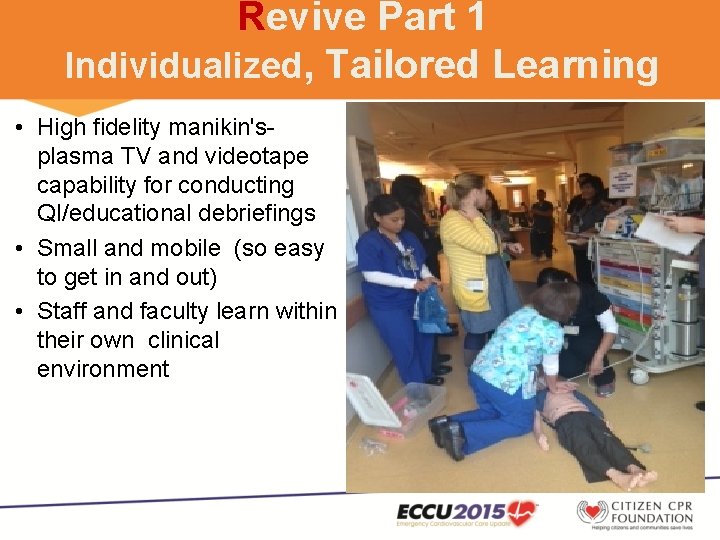
Revive Part 1 Individualized, Tailored Learning • High fidelity manikin's- plasma TV and videotape capability for conducting QI/educational debriefings • Small and mobile (so easy to get in and out) • Staff and faculty learn within their own clinical environment

Revive Part 2 Team Training Unannounced In-Situ Mock Codes • • Monthly in-situ un-announced mock codes in locations where Code Teams respond and perform as an actual event Pre-defined Learning objectives: – Clear code roles and responsibilities – Effective communication and team dynamics – Identified system errors or process improvements • Code Team performance assessed – PALS, NRP, ACLS, AHA Gold Standard – Equipment competency and effective communication • Formalized Debrief
Shannon video
The IOM Report June 30 th, 2015 • Actively collaborate and share data to facilitate national, state, and local benchmarking for quality improvement.

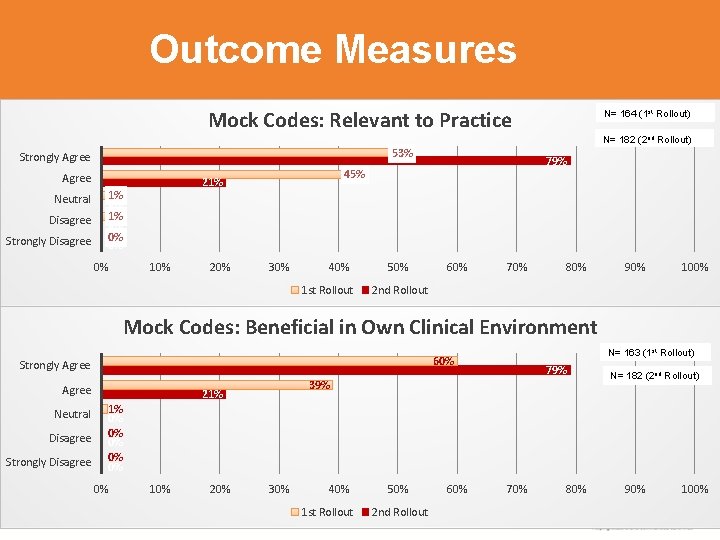
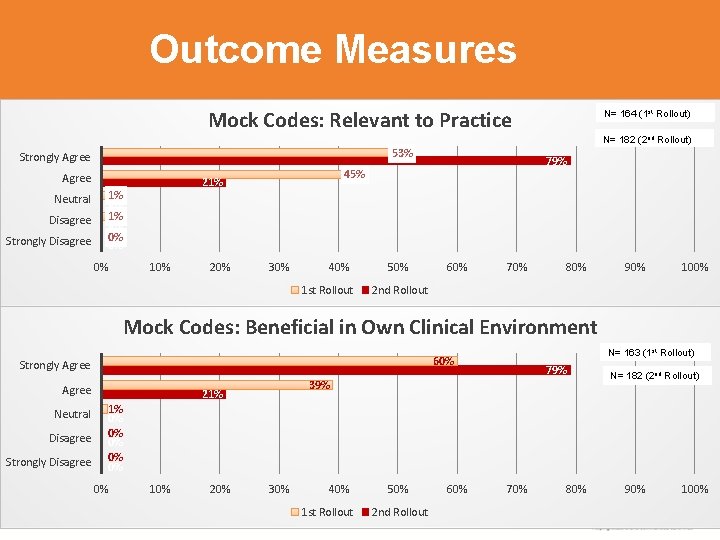
Outcome Measures Mock Codes: Relevant to Practice N= 164 (1 st Rollout) N= 182 (2 nd Rollout) 53% Strongly Agree Neutral Disagree Strongly Disagree 21% 1% 0% 0% 10% 20% 79% 45% 30% 40% 1 st Rollout 50% 60% 70% 80% 90% 100% 2 nd Rollout Mock Codes: Beneficial in Own Clinical Environment Strongly Agree Neutral Disagree Strongly Disagree N= 163 (1 st Rollout) 60% 79% 39% 21% N= 182 (2 nd Rollout) 1% 0% 0% 0% 10% 20% 30% 40% 1 st Rollout 50% 2 nd Rollout 60% 70% 80% 90% 100%

Participant Evaluation Results – Program Overall N= 160 (1 st Rollout) N= 176 (2 Rollout) Program Overall: Valuable Experience nd 49% Strongly Agree 79% 49% Agree Neutral Disagree Strongly Disagree 21% 1% 0% 0% 10% 20% 30% 40% 1 st Rollout 50% 2 nd Rollout 60% 70% 80% 90% 100%
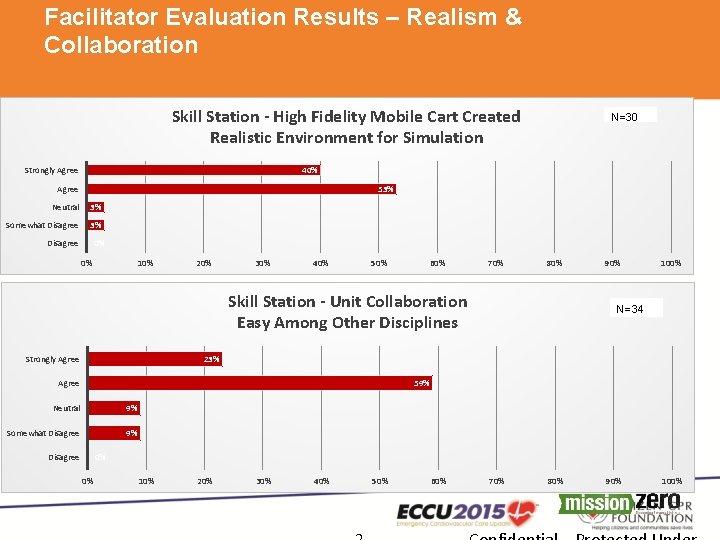
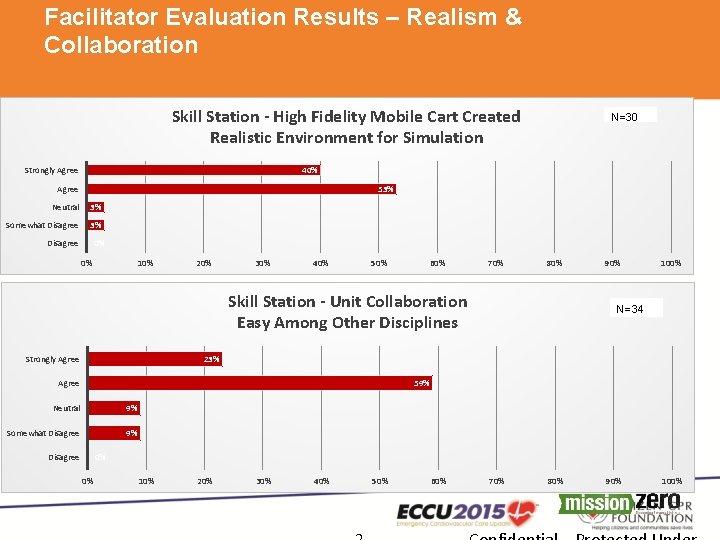
Facilitator Evaluation Results – Realism & Collaboration Skill Station - High Fidelity Mobile Cart Created Realistic Environment for Simulation N=30 40% Strongly Agree 53% Neutral 3% Somewhat Disagree 3% Disagree 0% 0% 10% 20% 30% 40% 50% 60% 70% 80% Skill Station - Unit Collaboration Easy Among Other Disciplines Strongly Agree 90% 100% N=34 23% Agree 59% Neutral 9% Somewhat Disagree 9% Disagree 0% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100%

Revive Initative at Stanford Children’s Health ü Mobile Simulation Ongoing Team training ü Rapid Response Initiative/PEWS work ü Policies and protocols in regards to a deteriorating child and emergency response ü Research (Single & Multi- Centered) examining measurable survival and program outcomes ü Get with The Guideline -Resuscitation Quality International Database contributor ü Resuscitation/Code Committee actual code and RRT reviews/education ü Examining Real Time CPR feedback ü International organizational participation and presentations ü Outreach

Next steps …… • We will identify gaps in CPR performance during simulated codes compared to AHA standards, differences in CPR performance during simulated codes compared to actual CPA events, and differences in CPR performance during simulated codes compared to student and facilitator perceptions of performance. • We will conduct two in-hospital simulated codes weekly over a 6 -month period collecting data for seven parameters from the defibrillator (compression rate, depth, fraction, and percent in target, ventilation rate and longest pre- and post-shock pause).
Next steps…. • Each simulated code participant (students and facilitator) will complete a post-event survey to assess their perceptions on whether the CPR performed met AHA standards. • To identify gaps in CPR performance, we will compare data-driven feedback from the defibrillator for each simulated code to AHA standards, data-driven feedback obtained during actual CPA events during the same 6 -month period, and the student and facilitator survey results. We will use these results to restructure and optimize our simulation education program with emphasis on addressing the gaps identified.
 Revive your work in the midst of the years
Revive your work in the midst of the years Revive thy work o lord
Revive thy work o lord Revive us again meaning
Revive us again meaning I run over fields and woods all day
I run over fields and woods all day Grizzly energy, llc
Grizzly energy, llc Revive me lord
Revive me lord Moli texas childrens
Moli texas childrens Christian childrens fund
Christian childrens fund Childrens services
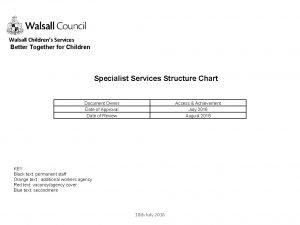
Childrens services Childrens services walsall
Childrens services walsall Levine childrens
Levine childrens 23 april international children's day turkey
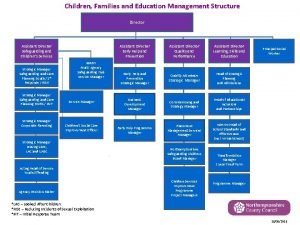
23 april international children's day turkey Multi agency assessment
Multi agency assessment World book day quiz
World book day quiz Childrens university of manchester
Childrens university of manchester Longman children's dictionary
Longman children's dictionary Black childrens memorial
Black childrens memorial Toddler fever 102
Toddler fever 102 History of childrens literature
History of childrens literature Colorado children's book award
Colorado children's book award Douglas county mental health initiative
Douglas county mental health initiative Stanford occupational health
Stanford occupational health Synergy lcps
Synergy lcps Ue management
Ue management Success through synergy
Success through synergy Getting to synergy action plan
Getting to synergy action plan Objective of synergy
Objective of synergy Synergy business park goregaon east
Synergy business park goregaon east Upspace institutional repository
Upspace institutional repository Synergy armenia
Synergy armenia Sai synergy llp
Sai synergy llp