Review of the Urinary System Vi Nguyen Bobbi
Review of the Urinary System Vi Nguyen Bobbi Carriger Christiane dos Santos Joo Hee Joa Pam Owens Jofel Bartolome
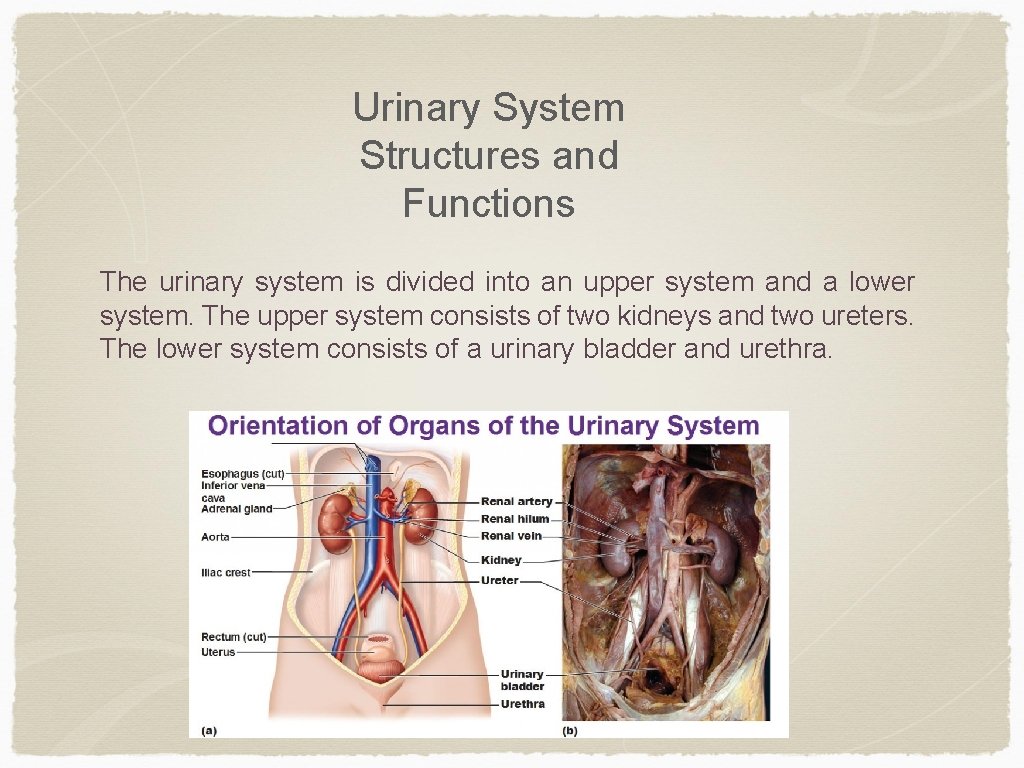
Urinary System Structures and Functions The urinary system is divided into an upper system and a lower system. The upper system consists of two kidneys and two ureters. The lower system consists of a urinary bladder and urethra.
Kidneys • Primary functions of the kidneys: - Regulate the volume and composition of extracellular fluid (ECF) - Excrete waste products from the body • The outer layer is the cortex, and the inner layer is the medulla • Urine formation is the result of a multistep process of filtration, reabsorption, secretion, and excretion of water, electrolytes, and metabolic waste products.
Kidney function • Produces erythropoietin during hypoxia and decreased renal blood flow; stimulates the production of RBCs in the bone marrow • Vitamin D is activated in the kidneys; Vitamin D is essential for calcium balance and bone health • Renin is integral in the regulation of BP and is produced and excreted by the kidneys • Prostaglandin (PG) synthesis (primarily PGE 2 and PGI 2) occurs in the medulla; PGs have a vasodilating action that increases renal blood flow and promotes Na+ excretion
Ureters and Bladder • Ureters are one way tubes that carry urine from the kidneys to the bladder • Made of smooth muscle that contract to move urine downward • The bladder is located behind symphysis pubis and anterior to the vagina and rectum • Primary purpose is to serve as a stretchable reservoir for urine and to help the body eliminate waste • 200 -250 ml is the typical amount of urine in bladder that causes moderate distention and the urge to urinate
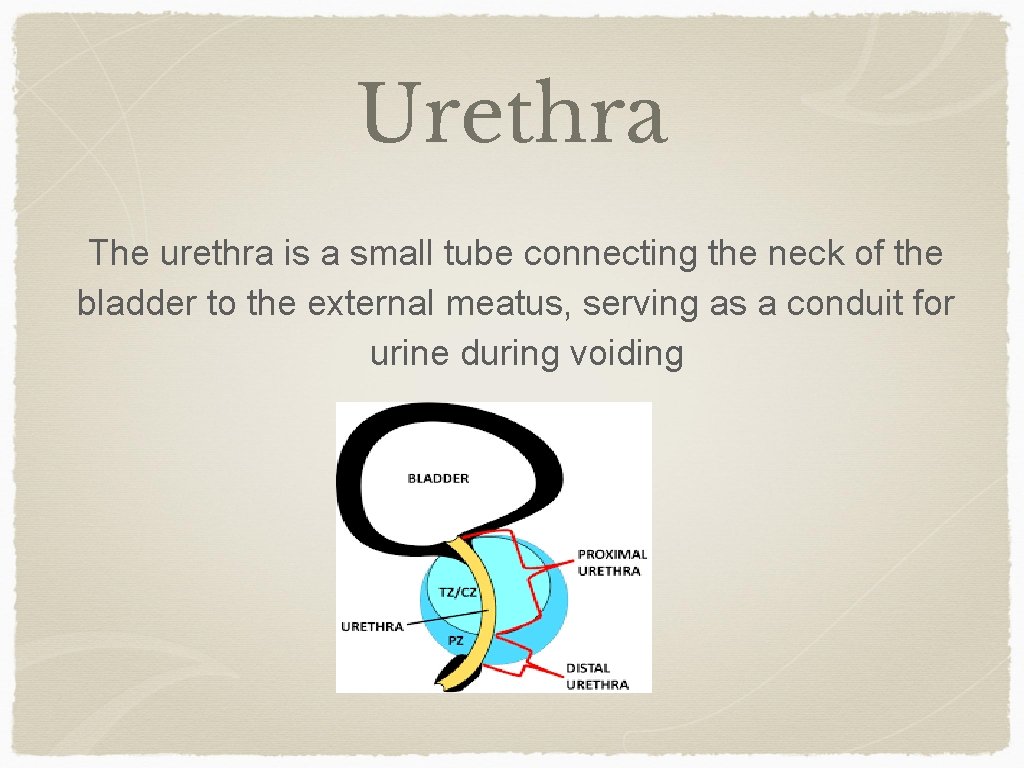
Urethra The urethra is a small tube connecting the neck of the bladder to the external meatus, serving as a conduit for urine during voiding
Urethrovesical Unit Bladder, urethra, and pelvic floor muscles form the urethrovesical unit - Receives neuronal input from the ANS - Normal control of this unit is defined as continence Any disease or trauma that affects function of the brain, spinal cord, or nerves that directly innervate the bladder, bladder neck, external sphincter, or pelvic floor can affect bladder function
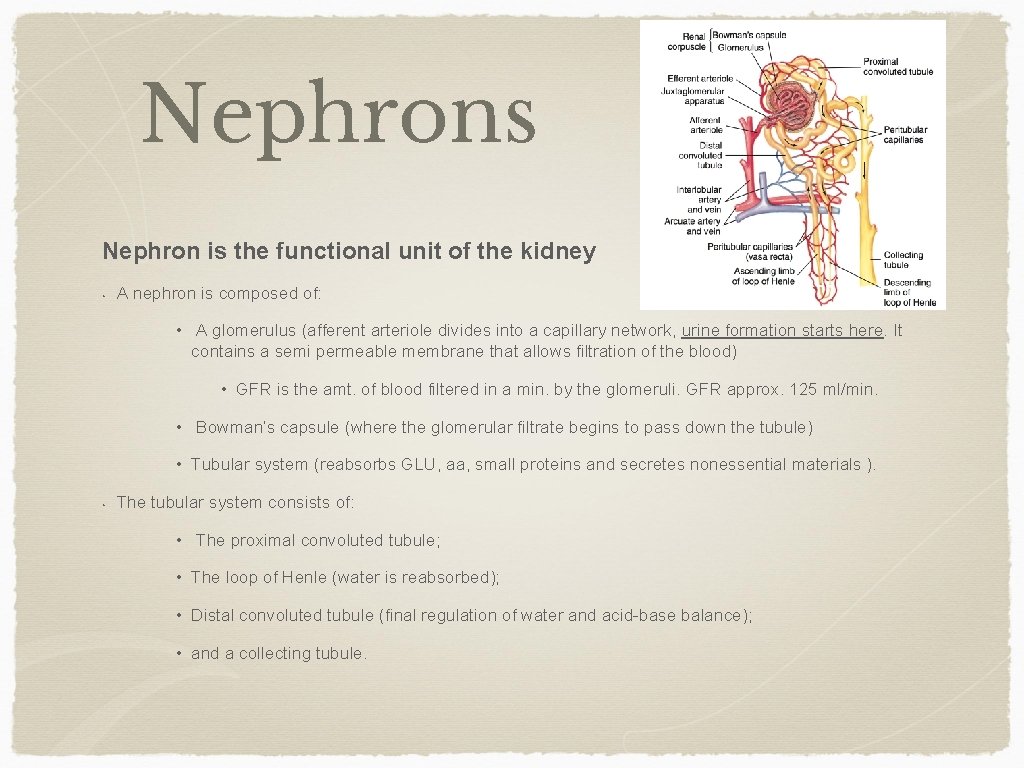
Nephrons Nephron is the functional unit of the kidney • A nephron is composed of: • A glomerulus (afferent arteriole divides into a capillary network, urine formation starts here. It contains a semi permeable membrane that allows filtration of the blood) • GFR is the amt. of blood filtered in a min. by the glomeruli. GFR approx. 125 ml/min. • Bowman’s capsule (where the glomerular filtrate begins to pass down the tubule) • Tubular system (reabsorbs GLU, aa, small proteins and secretes nonessential materials ). • The tubular system consists of: • The proximal convoluted tubule; • The loop of Henle (water is reabsorbed); • Distal convoluted tubule (final regulation of water and acid-base balance); • and a collecting tubule.
Review • • • ♣ Antidiuretic hormone (ADH): required for water reabsorption ♣ Aldosterone: reabsorption of Na+ and water; In exchange for Na+, potassium ions (K+) are excreted ♣ Acid-base regulation: reabsorption and conservation of bicarbonate (HCO 3) and secretion of excess H+ ♣ Atrial natriuretic peptide (ANP): increases sodium excretion ♣ Parathyroid hormone (PTH): acts on renal tubules to increase reabsorption of calcium to maintain the appropriate level of calcium in the blood

Fetus Urinary System • Urogenital system develops during 4 th week • Intermediate mesoderm → Pronephros → Mesonephros→ Metanephric mesoderm • By 9 th week, kidneys are formed and continually develop • By 3 months, waste products are produced and eliminated in the placenta • Waste circulates through mother’s blood circulation and eliminated through the mother’s urinary system
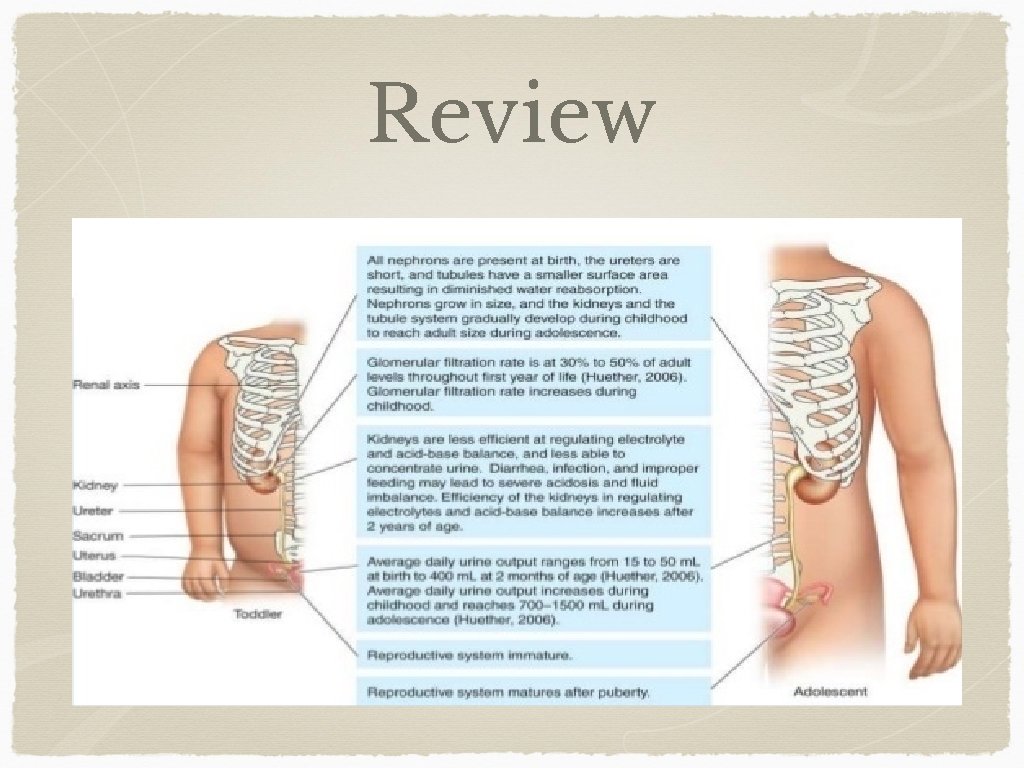
Newborn & Infant Urinary System • Born with adult number of nephrons • Capacity to concentrate urine is still immature • Not sensitive to retain water as adult’s kidneys → higher risk of dehydration • More sensitive to excessive salt intake → low mineral water with infant formulas • Low glomerular filtration and absorption • Short Loop of Henle: Decrease in ability to reabsorb Na + and H 20 • Main two functions: 1. Body Water Regulation 2. Waste Elimination (Lower rate) • Less efficient regulating electrolyte and acid-base balance: • Low excretions on H + & Low secretion of acid and plasma HCO 3 • By age 1 to 2 years, kidney function is the same as an adult yet, continues to grow until body growth complete
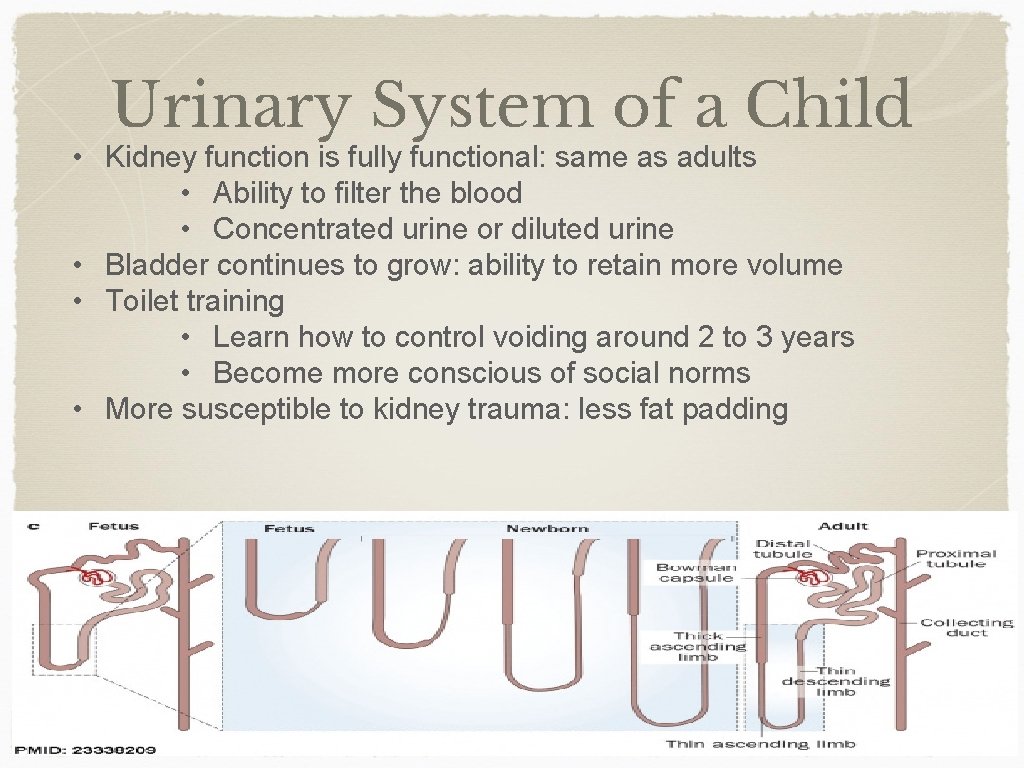
Urinary System of a Child • Kidney function is fully functional: same as adults • Ability to filter the blood • Concentrated urine or diluted urine • Bladder continues to grow: ability to retain more volume • Toilet training • Learn how to control voiding around 2 to 3 years • Become more conscious of social norms • More susceptible to kidney trauma: less fat padding
Adolescent Urinary System • The growth of the urinary system is complete • By age 12, the sensation of urge to urinate and ability to control the voiding of their bladder • Urinary function and micturition pattern are similar to adults • Teenage girls and young women are more at risk of urinary tract infection (between 15 to 29 years)
Review
Women vs. Men • -Women are more at risk for urinary tract infections than men due to anatomical differences • The location and the length of the female urethra (close to vagina as well as rectum) increases the risk of UTI • Escherichia coli, the bacteria that causes most UTIs, is usually found in the rectum or the vagina; incorrect cleaning after urinating (from back to front) can bring E. coli to the entrance of the vagina where the urethra is • Pregnant women are more at risk of pyelonephritis due to higher frequency of urination and persistent urge to urinate
Kidney Stones • Kidney stones are common in adults but affect mainly men • Differences in diet between men and women: men eat in larger quantity with more waste to eliminate than women • Men’s kidneys have an increased ability to concentrate urine compared to women ; men are able to produce more concentrated urine, which is known to be a risk factor for kidney stones • Men are advised to drink more water than women (2 L/day for men and women 1. 6 L/day); this can decrease the risk of kidney stones
Elderly Changes associated with aging in kidney and bladder function: • Kidneys: -Amount of kidney tissue decreases (20%-25% from age 30 -80 year of age); kidneys become less capable of regulating water balance • Elderly have a reduced capacity to conserve body water during high temperatures and are at risk for dehydration -Number of filtering units (nephrons) decreases; because nephrons filter waste material from the blood , the elderly decline in ability to excrete waste products and drugs ; geriatric medication dosage may be lower as a result. - Blood supply to kidneys decreases (d/t fatty deposits, cholesterol, calcium and other substances that are deposited in the inner lining of the arteries) ; narrowing or blockage of renal artery causes kidneys to filter blood more slowly; HTN causes reduced kidney function which is the most common cause of kidney failure in elderly
Elderly • Bladder: -The bladder wall changes, the elastic tissue becomes tough and the bladder becomes less stretchy and unable to hold as much urine - The bladder muscles weaken and can cause urinary retention • Urethra can become blocked: -In women, this can be due to weakened muscles that cause the bladder or vagina to fall out of position (prolapse) -In men, it can be due to an enlarged prostate gland • In a healthy aging person, kidney function can remain normal; illness, medicine, and other conditions can affect kidney function
Elderly • COMMON PROBLEMS: • Bladder control issues: leakage, urinary incontinence, urinary retention • Bladder and other urinary tract infections (UTIs) • Chronic kidney disease
Nephrotic Syndrome • Glomerulus is excessively permeable to plasma protein causing proteinuria • Low plasma albumin and tissue edema • Associated with systemic illness: Diabetes and Lupus • Patho: Metabolic, biochemical, or physiochemical disturbance in the basement membrane of the glomeruli • Glomerular membrane is permeable to protein especially albumin which leads to hyperalbuminuria. • Hypoalbuminemia is reduced which decreases colloidal osmotic pressure • Fluid collects in the abdominal cavity (ascites) • Hypovolemia stimulates the renin-angiotensin system and the secretion of antidiuretic hormone and aldosterone • Tubular reabsorption increase sodium and water to increase intravascular volume
Etiology of Nephrotic Syndrome • Primary Glomerulus Disease • Membranous proliferation • Primary nephrotic syndrome • Focal glomerulonephritis • Inherited nephrotic disease
Types of Nephrotic Syndrome • Minimal Change Nephrotic Syndrome (MCNS) • Mainly a disease that affects preschool children • Cause of MCNS is unknown: viral upper respiratory tract infection • Secondary Nephrotic Syndrome • Occur after or is link with glomerular damage: acute glomerulonephritis and chronic glomerulonephritis are prominent causes of glomerular damage • Less common: course of collagen vascular disease or result of toxicity to drugs, stings, or venom • Presenting symptom of renal disease in pediatric patients with AIDS • Congenital Nephrotic Syndrome • Caused by recessive gene or an autosome • Disease does not respond to usual therapy and in 1 -2 years of life, if infant does not receive dialysis or successful kidney transplant, death can occur
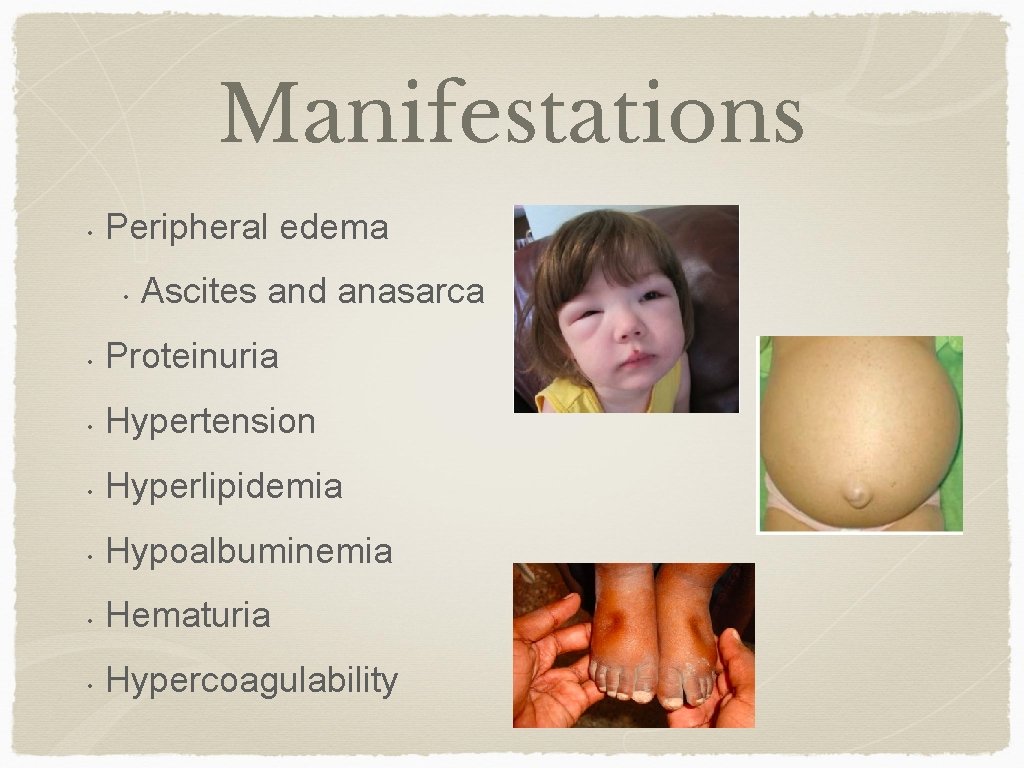
Manifestations • Peripheral edema • Ascites and anasarca • Proteinuria • Hypertension • Hyperlipidemia • Hypoalbuminemia • Hematuria • Hypercoagulability
Labs - Decreased serum albumin - Decreased total serum protein - Increased serum cholesterol
Collaborative Care Objectives: • • • Early detection & treatment to minimize renal damage Protein free urine Acute infections prevented Edema absent or minimal Nutrition maintained
Nursing Care Supportive • • • Strict I’s & O’s Daily weights and abdominal girth measurements Vital signs to detect complications Salt restrictions if edema is present Skin care Frequent position changes
Collaborative Care: Drug Therapy • • Corticosteroid Therapy • Prednisone Immunosuppressant Therapy • Cyclophosphamide Diuretics • Thiazide and loop diuretics Plasma Volume Expanders • Albumin (Human)
Teaching • • • Diet modification Signs & Symptoms of relapse Self urine check for albumin • Daily while on meds • Twice weekly in remission Side effects of medications • Effects of corticosteroid therapy Avoid exposure to persons with known infections
Prognosis • • Generally good for steroid sensitive patient Steroid resistant patients are thought to have a high risk of developing chronic renal failure
NCLEX Review Question #1: Because of normal changes due to aging, the nurse anticipates that a 75 -year-old patient's serum creatinine level might be which of the following? 1. 0. 3 mg/d. L 2. 2. 4 mg/d. L 3. 4. 8 mg/d. L 4. 6. 4 mg/d. L
Answer: Correct Answer: 1 Rationale: Lower than normal is correct because serum creatinine level reflects the by-product of muscle breakdown, and an older adult with less muscle mass can be expected to have a lower-than -normal level. Normal creatine is 0. 6 -1. 2 mg/d. L
Question #2: A nurse is caring for a patient who asks the nurse why females are more likely than males to contract bladder infections. The nurse knows teaching has been effective when the patient identifies which of the following as a female risk factor for bladder infections? 1. The p. H of the female urethra is more conducive to infection 2. The urinary meatus is farther from the anus than most males 3. The urinary meatus is closer to the bladder than in most males 4. Females urinate more frequently than males, increasing risk
Answer: Correct Answer: 3 Rationale: In females, the urethra is approximately 1. 5 inches (3 to 5 cm) long, and the urinary meatus is anterior to the vaginal orifice. In males, the urethra is approximately 8 inches (20 cm) long. The shorter distance of the female urethra creates a mechanism by which more females than males contract bladder infections. The female urinary meatus is closer, not farther from the anus than in most males, also increasing risk for bladder infections.
Question #3: A true statement describing the differences in the pediatric genitourinary system compared with the adult genitourinary system is that 1) After 6 years of age, urinary system is nearly like that of an adult 2) The young infant’s kidneys can more effectively concentrate urine than an adult’s kidneys 3) Newborns and infants void more frequently with a high specific gravity 4) Young children have shorter urethras, which can predispose them to UTIs
Answer: Correct Answer: 4 Rationale: Kidneys are fully function by 2 years old, yet both kidneys and bladder continue to grow until 12 years old. The young infant’s kidneys are not fully developed and capacity to concentrate urine is still immature and has a low specific gravity. Young children, especially females have shorter urethras (about 1. 5 inches long).
The End
References Aging changes in the kidneys and bladder. (2016, August 22). Retrieved April 23, 2017, from https: //medlineplus. gov/ency/article/004010. htm Kidney through ages. (2011). Retrieved April 24, 2017, from http: //www. kidneyfacts. com/kidneys-health/kidney-through-ages/ Danone Research, France Lewis, S. M. , Dirksen, S. R. , Heitkemper, M. M. , Bucher, L. , & Harding, M. (2014). Medical-surgical nursing: Assessment and management of clinical problems. Wong, D. L. , Hockenberry, M. J. , & Wilson, D. (2015). Wong's nursing care of infants and children (10 th ed. ). St. Louis: Elsevier.
- Slides: 37