Review of the principles of fracture management AO





- Slides: 47
Review of the principles of fracture management AO Trauma Advanced Principles Course
Learning objectives • Explain principles of fracture fixation that will lead to early functional aftertreatment • Realize how correct reduction technique respects the soft-tissue envelope • Understand concepts of stability, effect on bone healing, and correct application of implants
Goal—restore normal function ASAP
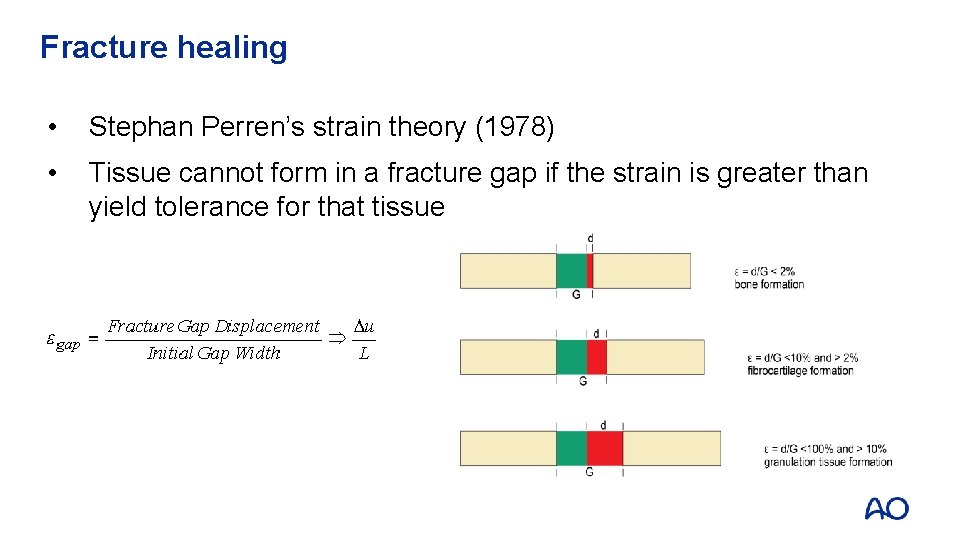
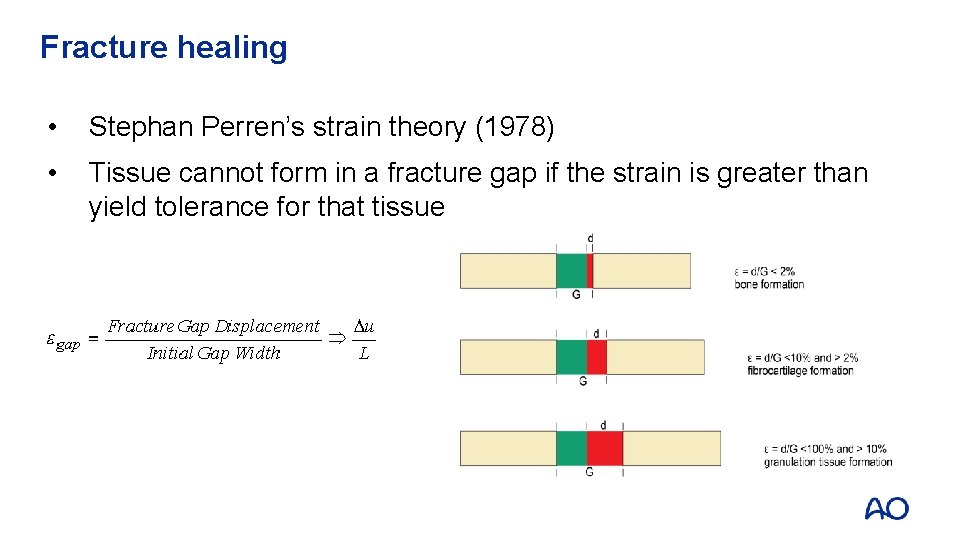
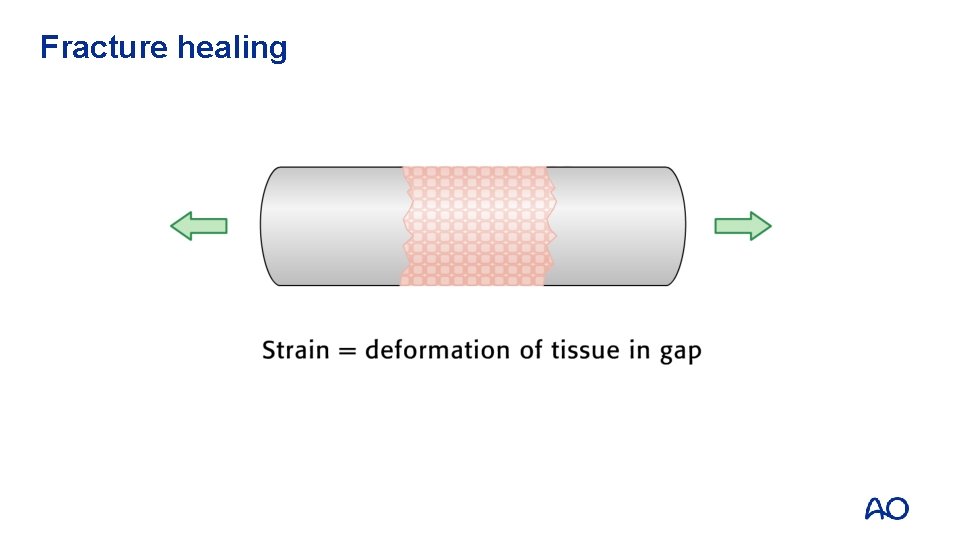
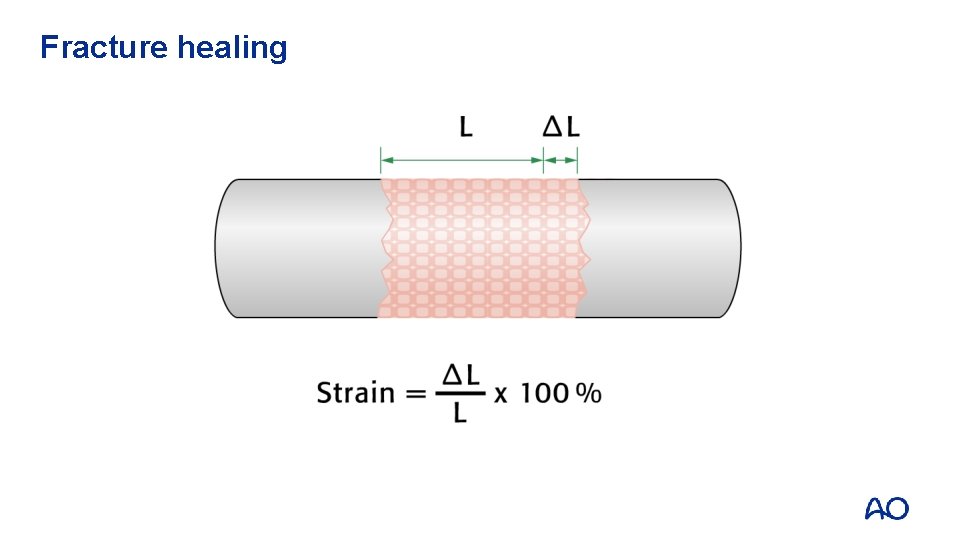
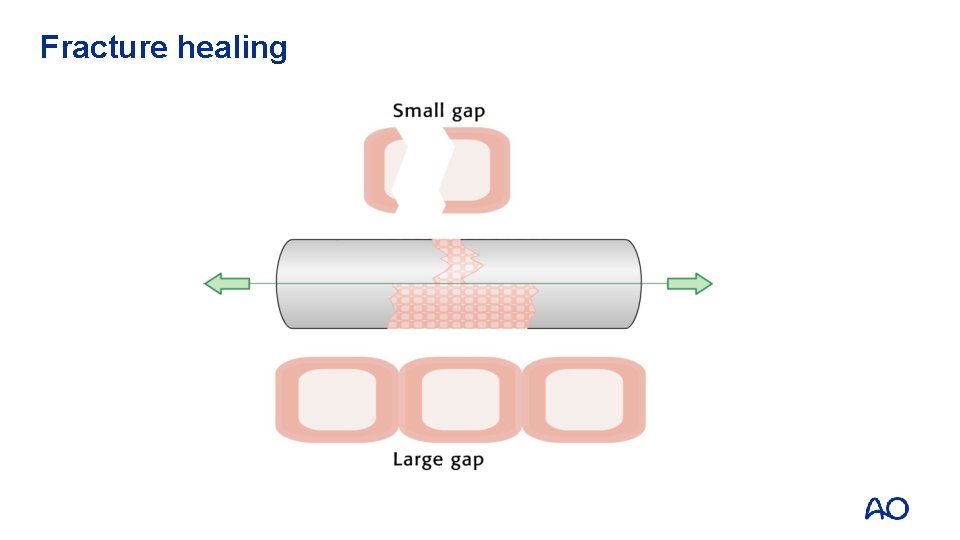
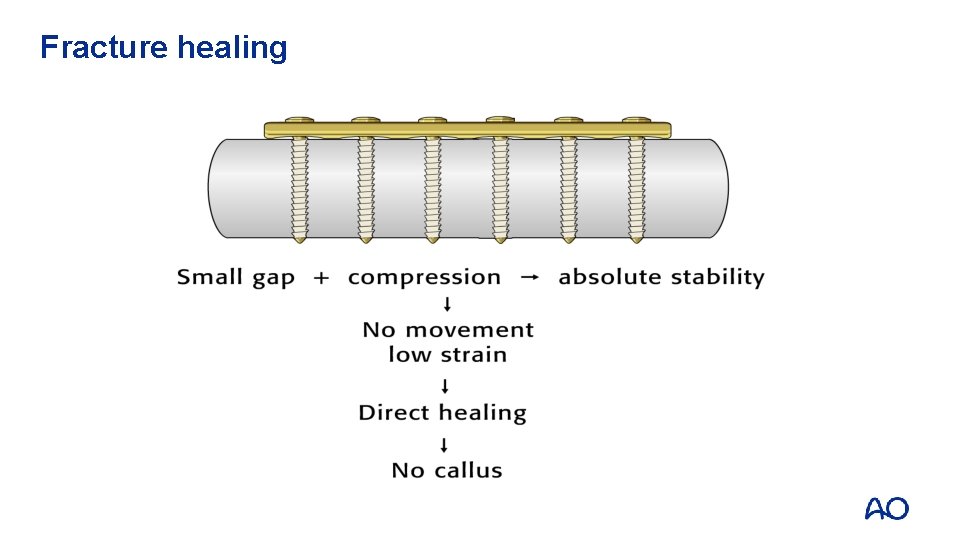
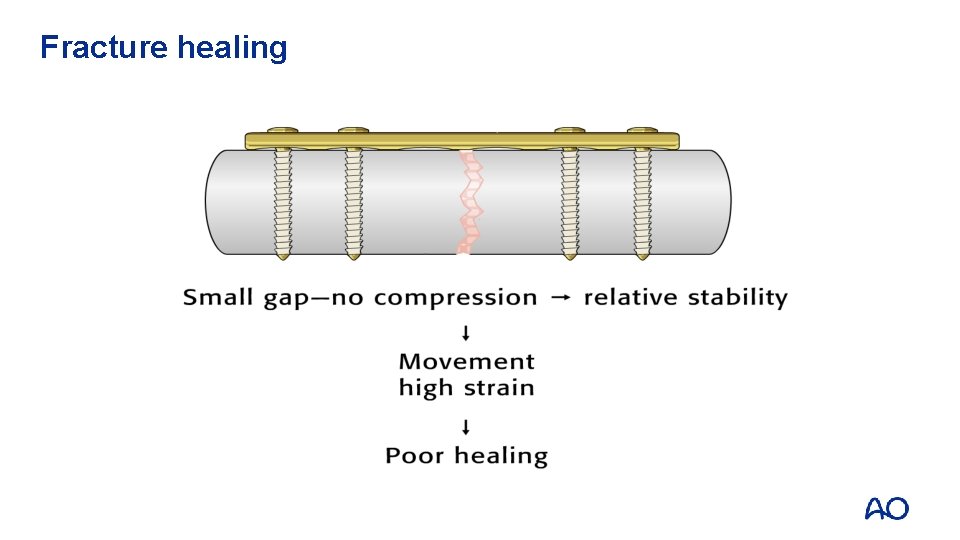
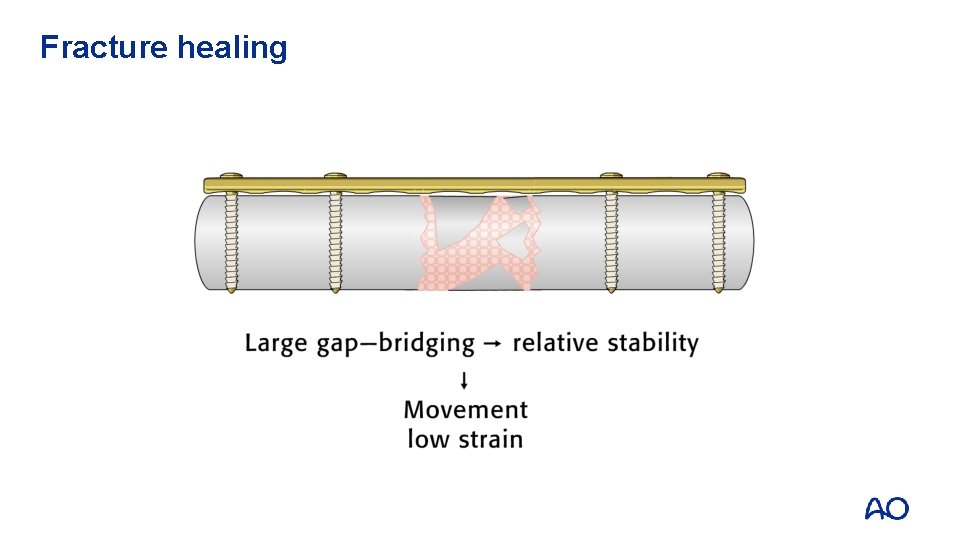
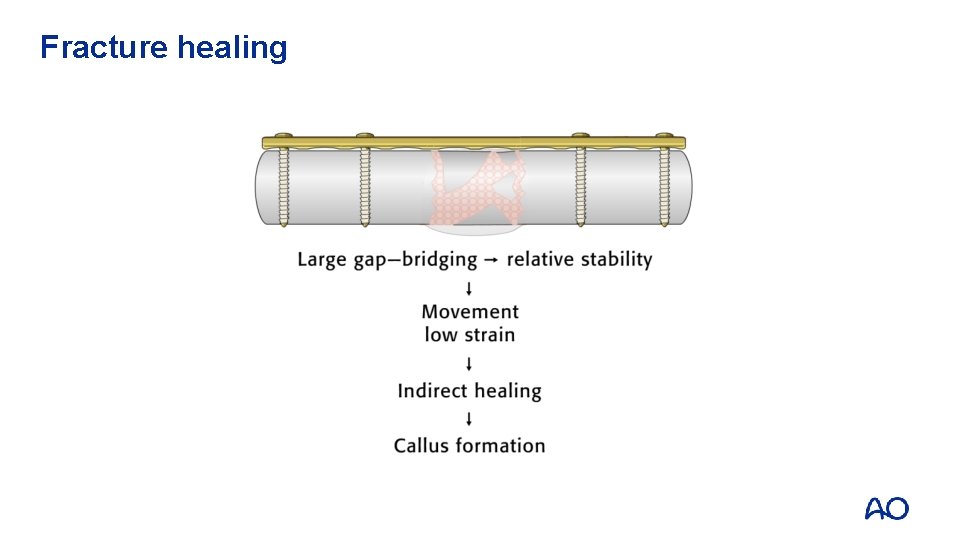
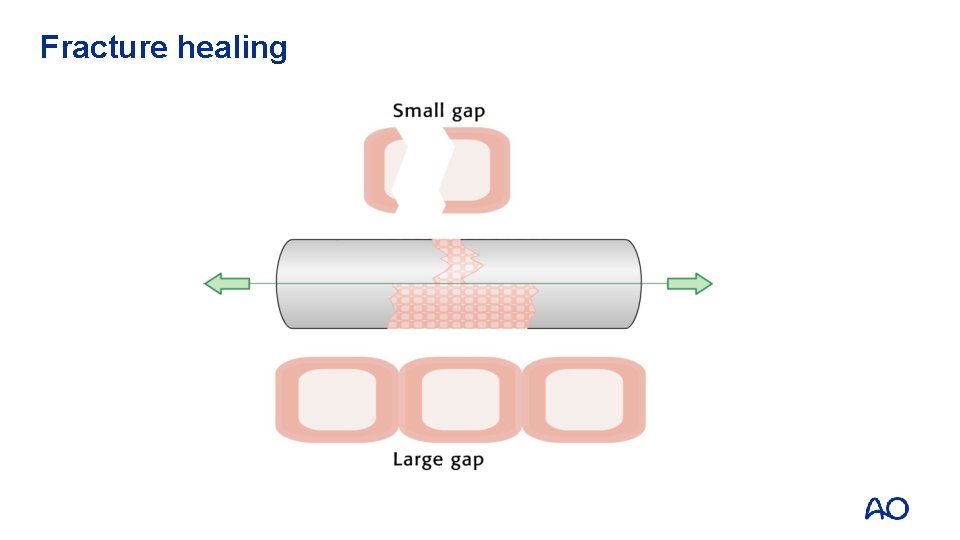
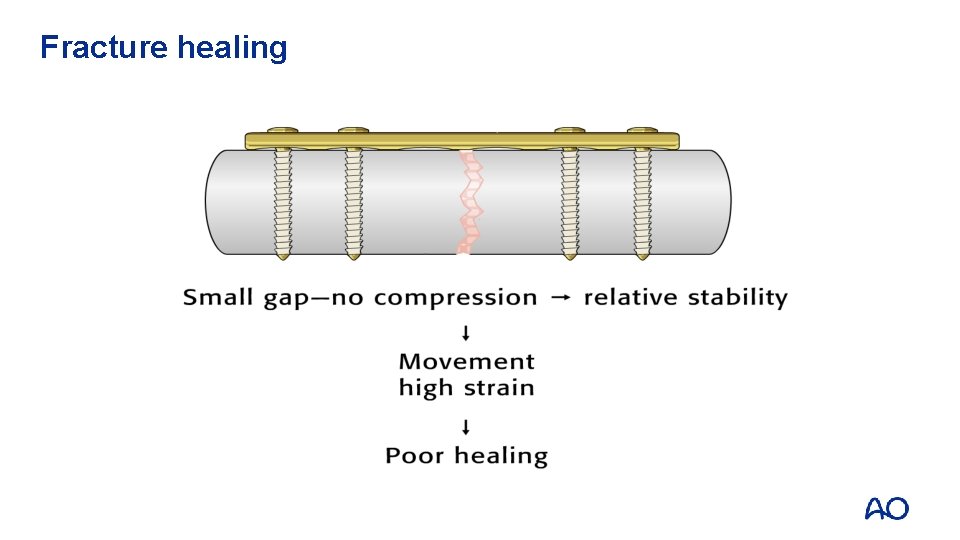
Fracture healing • Stephan Perren’s strain theory (1978) • Tissue cannot form in a fracture gap if the strain is greater than yield tolerance for that tissue
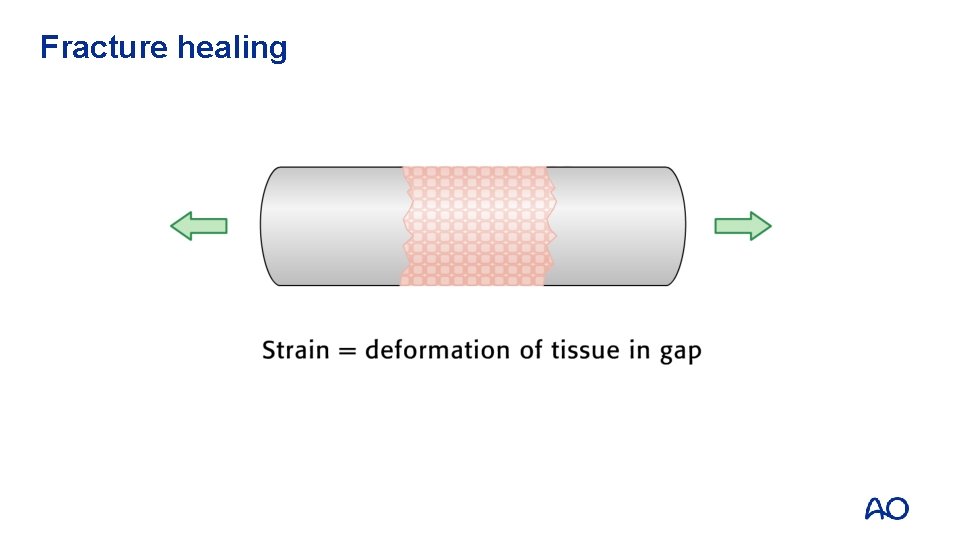
Fracture healing
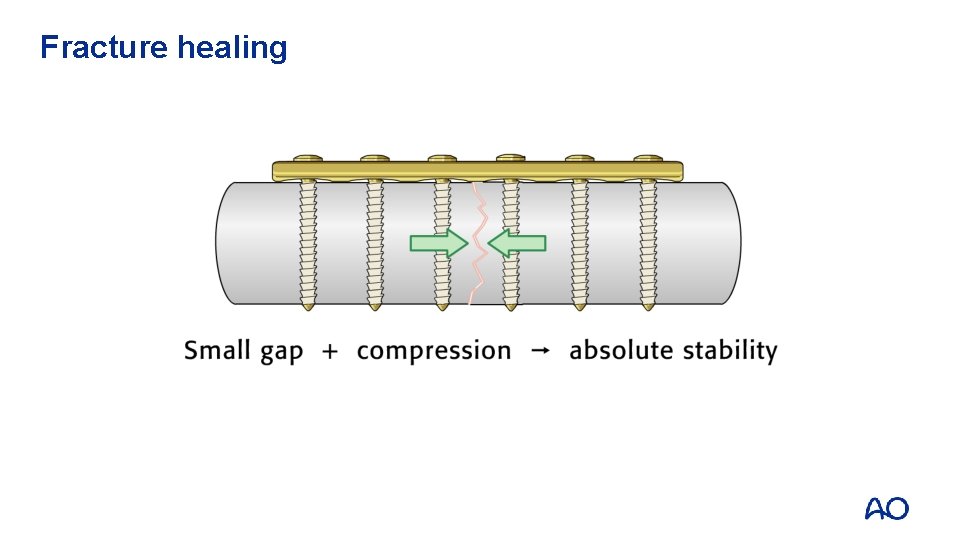
Fracture healing
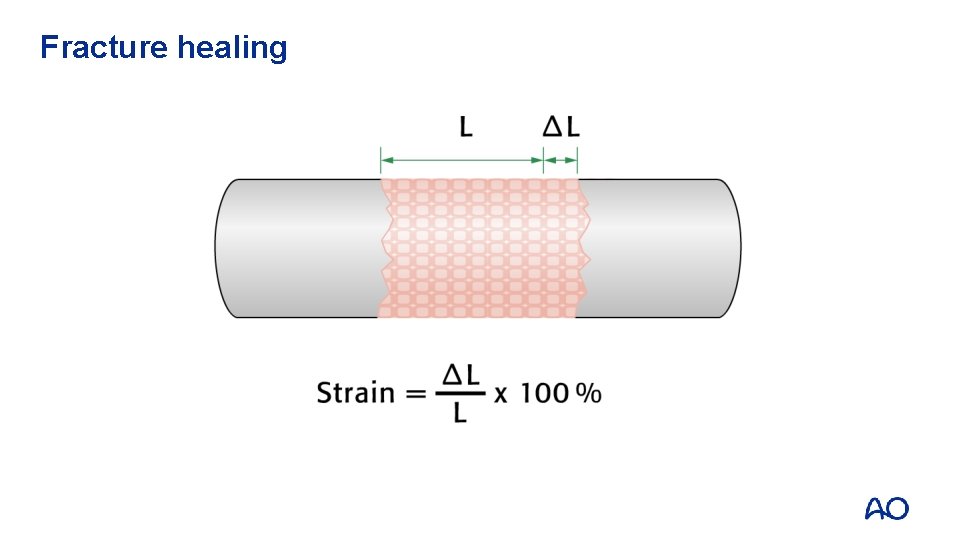
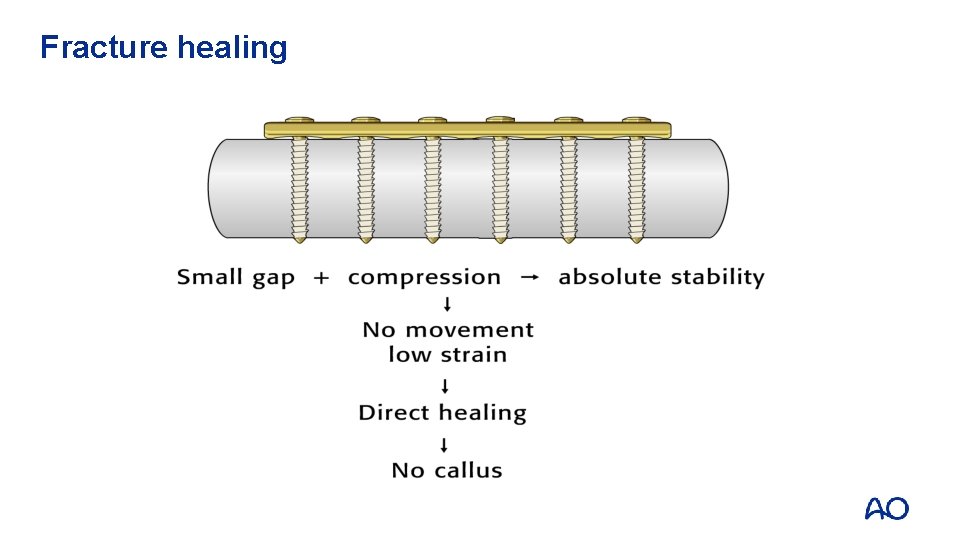
Fracture healing
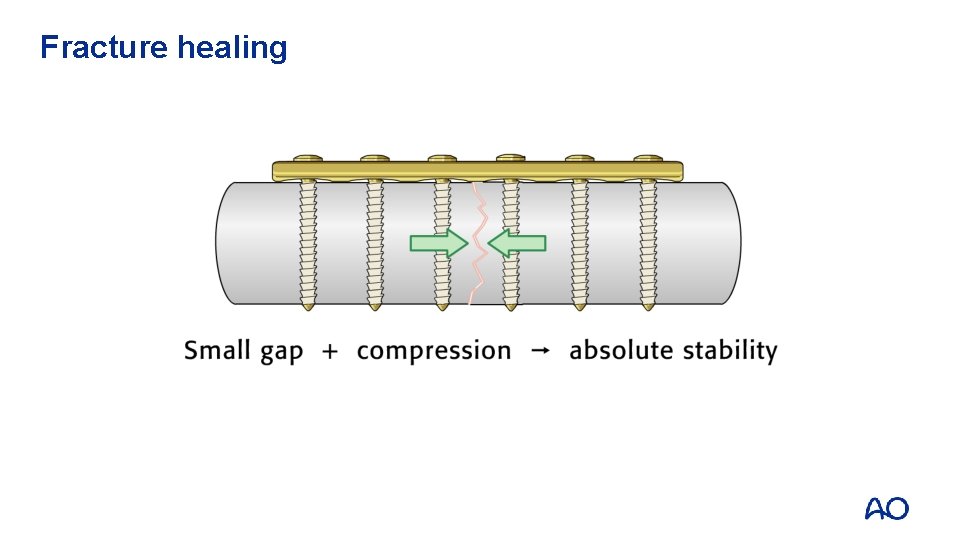
Fracture healing
Fracture healing
Fracture healing
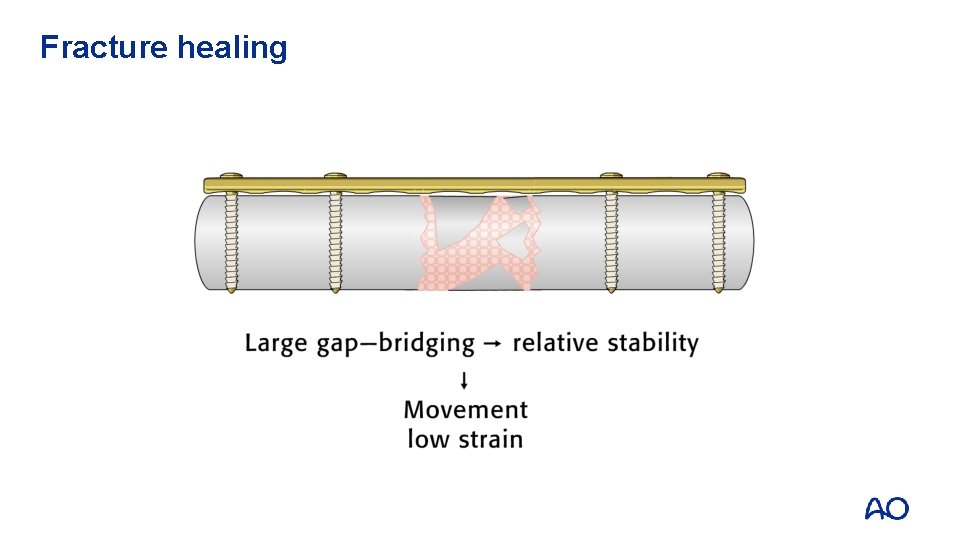
Fracture healing
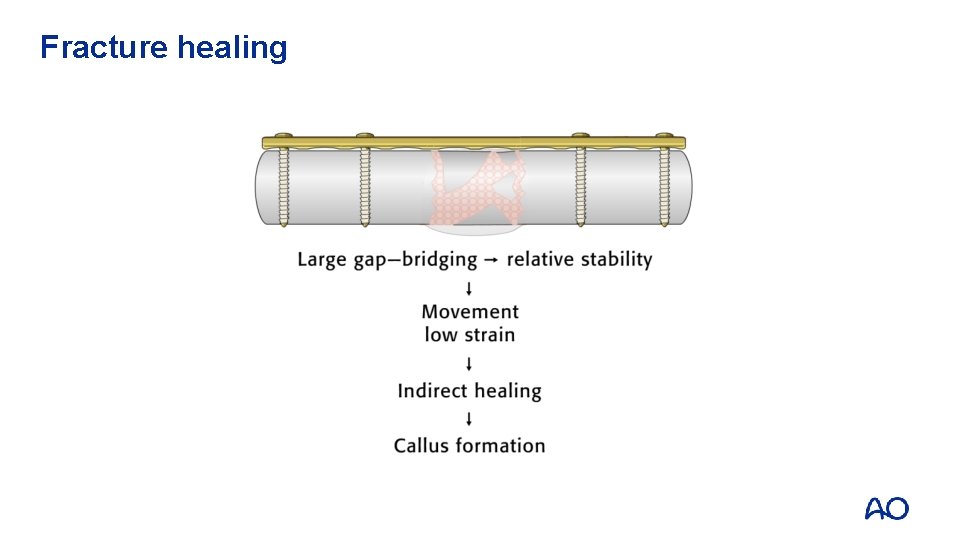
Fracture healing

Is anatomy crucial?

al ? i c u r c y Anatom Yes - ORIF No – choose implant
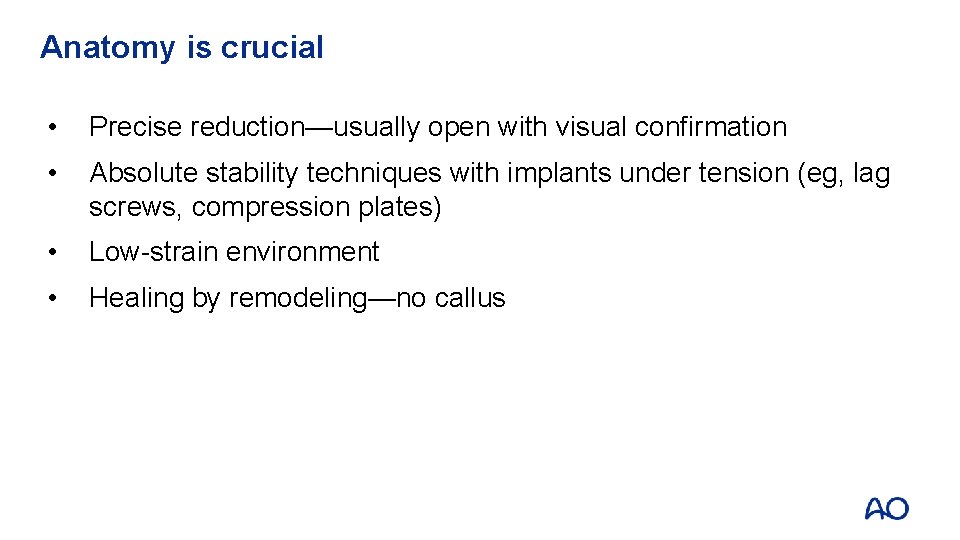
Anatomy is crucial • Precise reduction—usually open with visual confirmation • Absolute stability techniques with implants under tension (eg, lag screws, compression plates) • Low-strain environment • Healing by remodeling—no callus
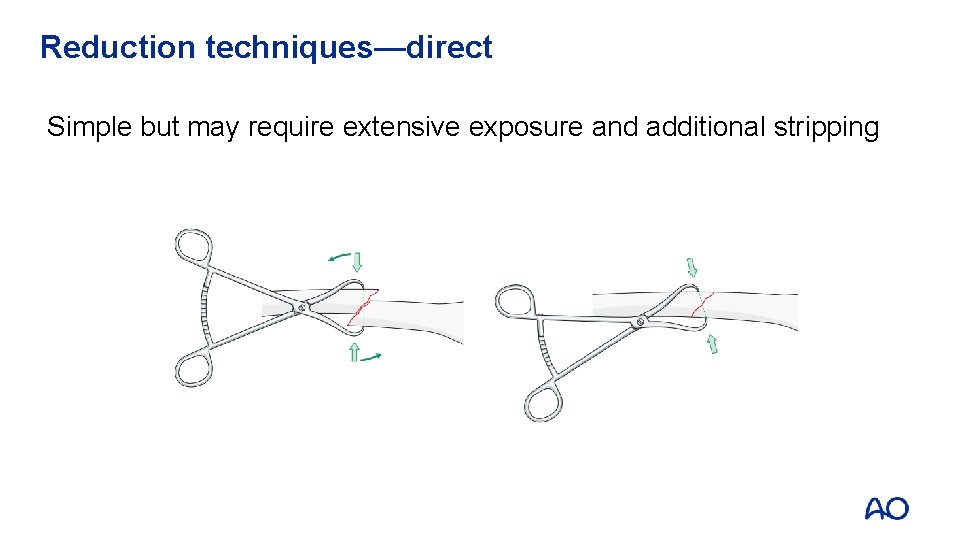
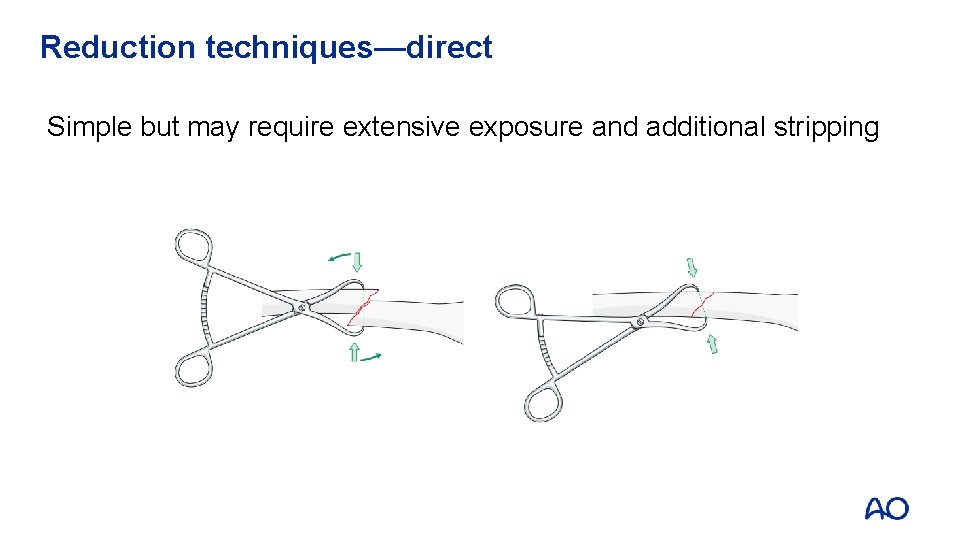
Reduction techniques—direct Simple but may require extensive exposure and additional stripping
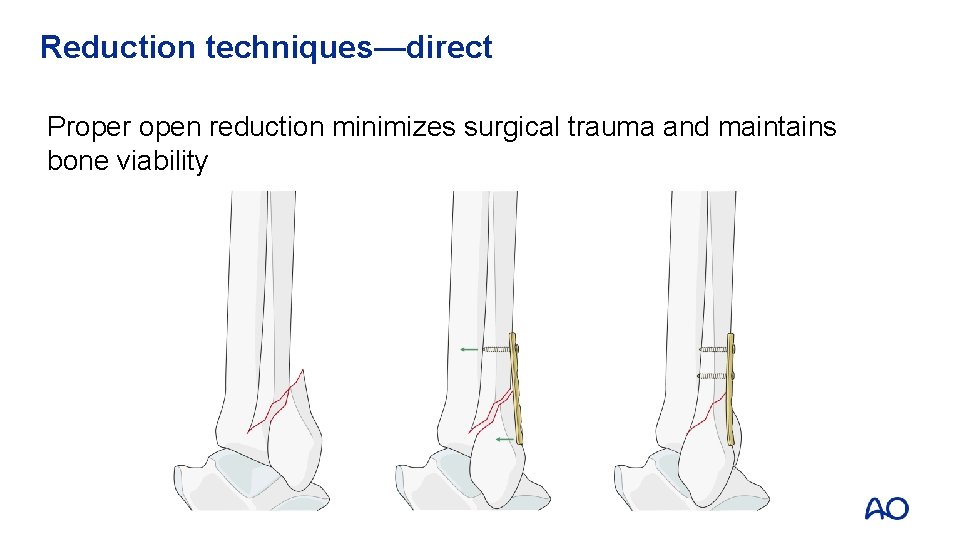
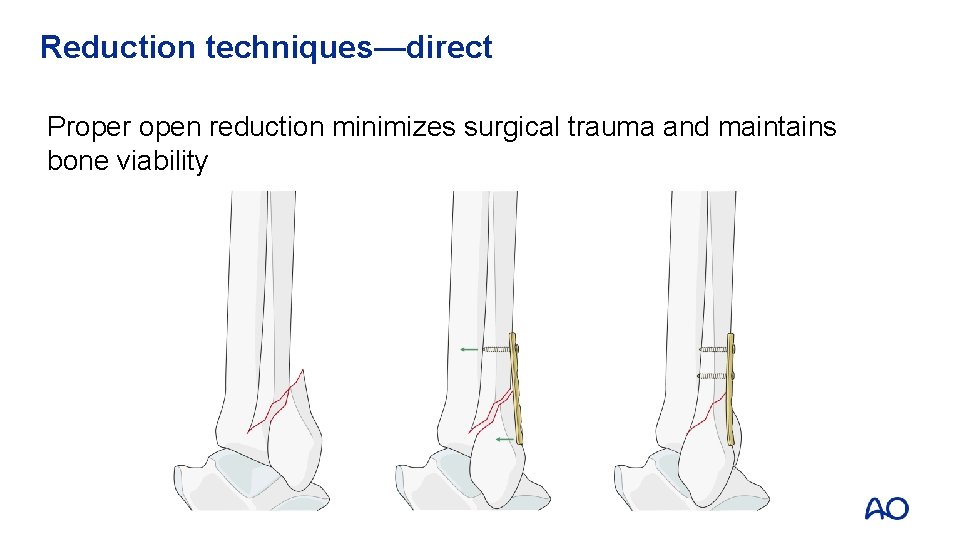
Reduction techniques—direct Proper open reduction minimizes surgical trauma and maintains bone viability
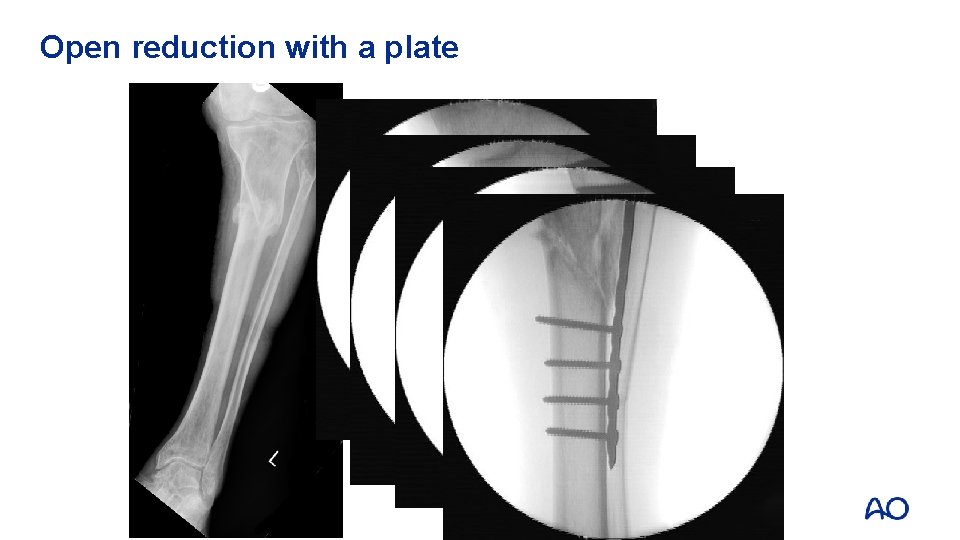
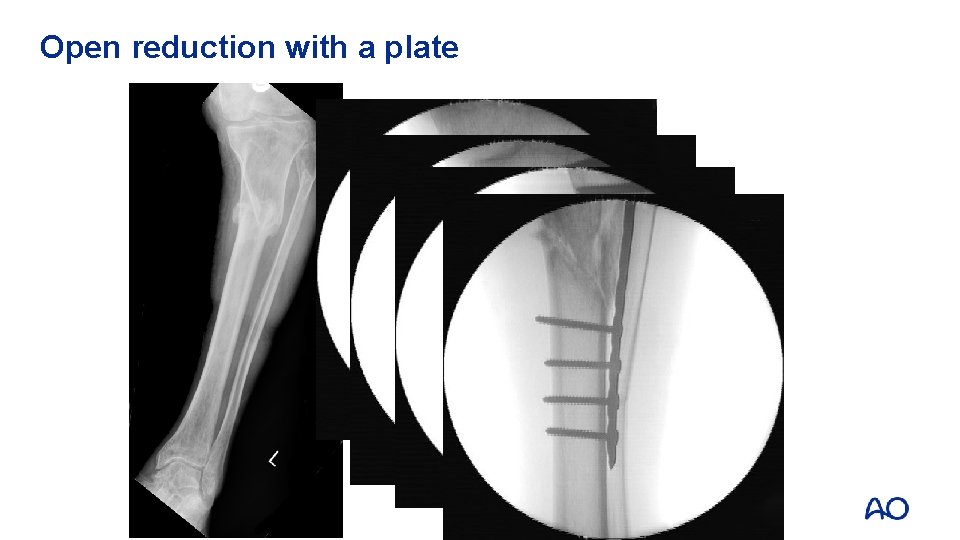
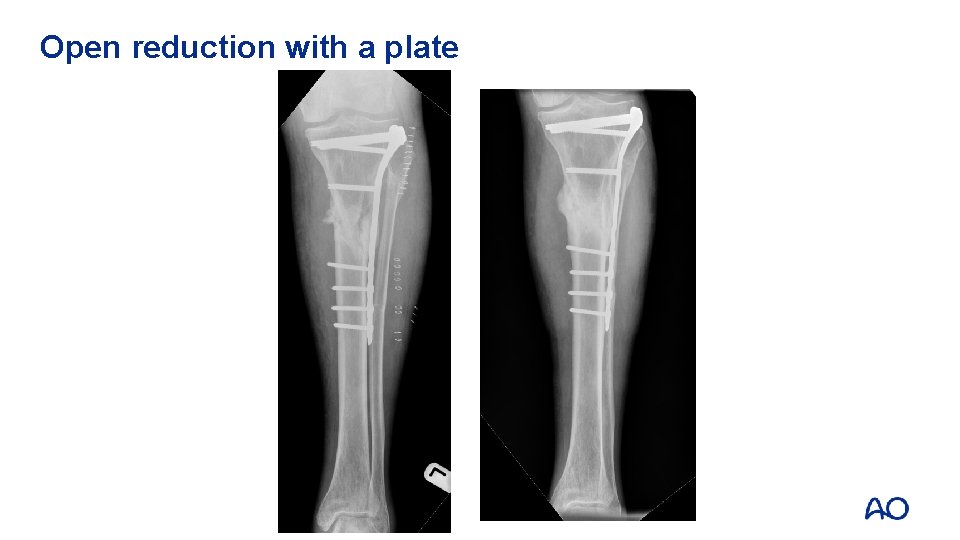
Open reduction with a plate
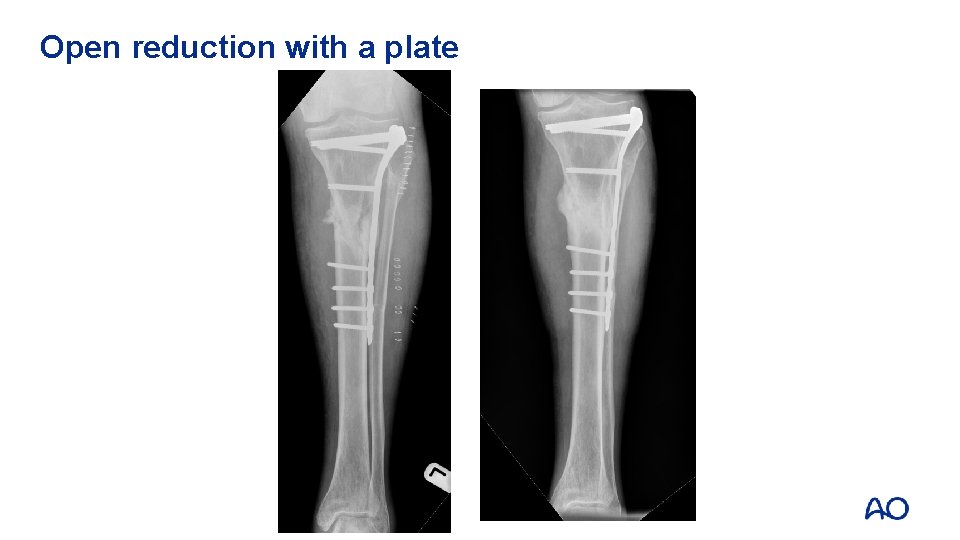
Open reduction with a plate
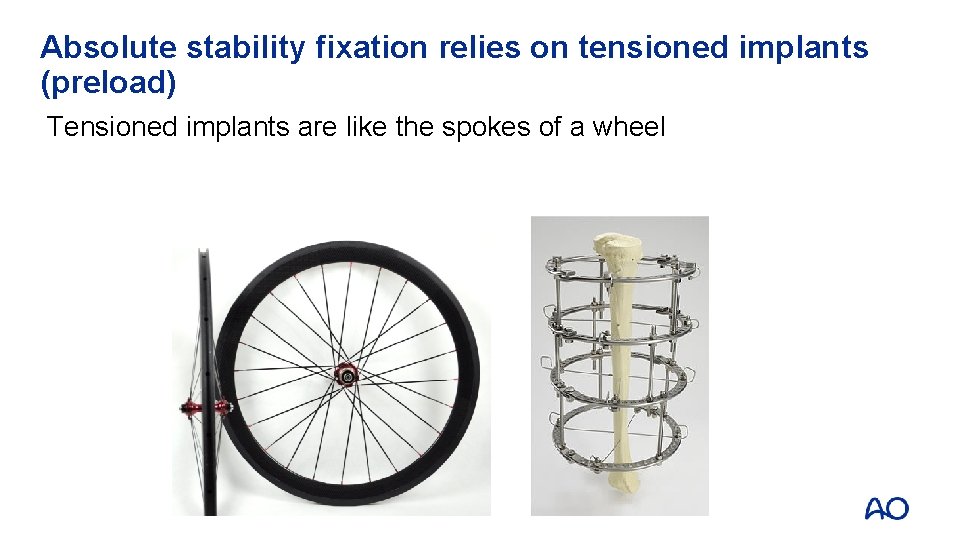
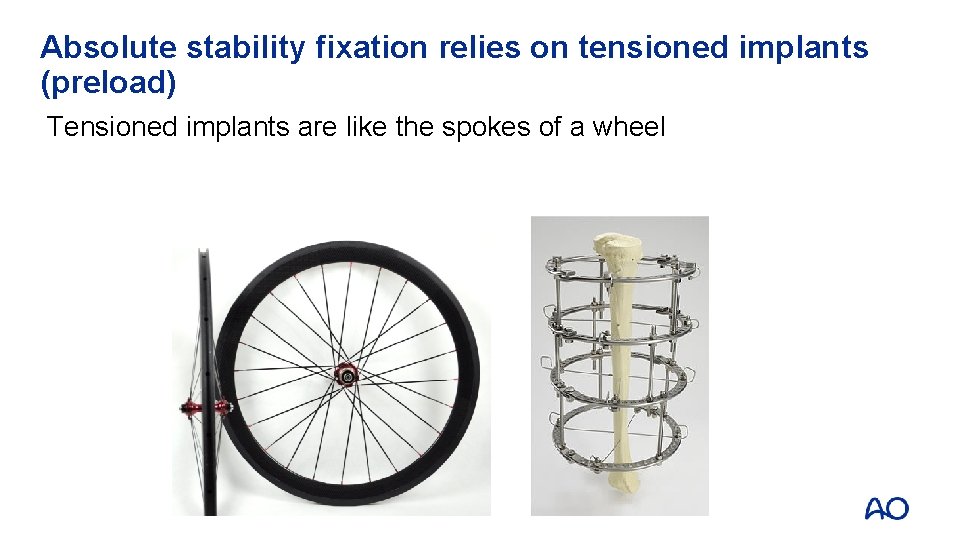
Absolute stability fixation relies on tensioned implants (preload) Tensioned implants are like the spokes of a wheel
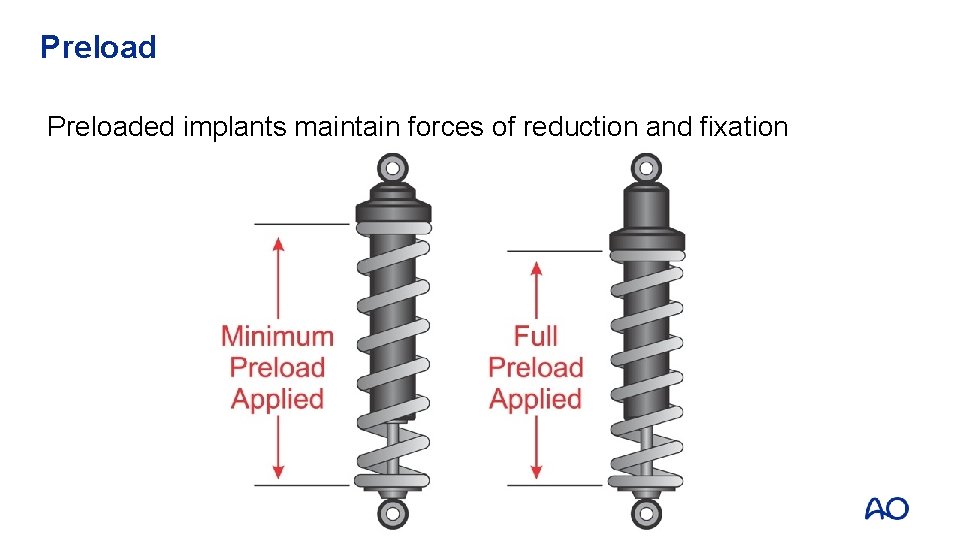
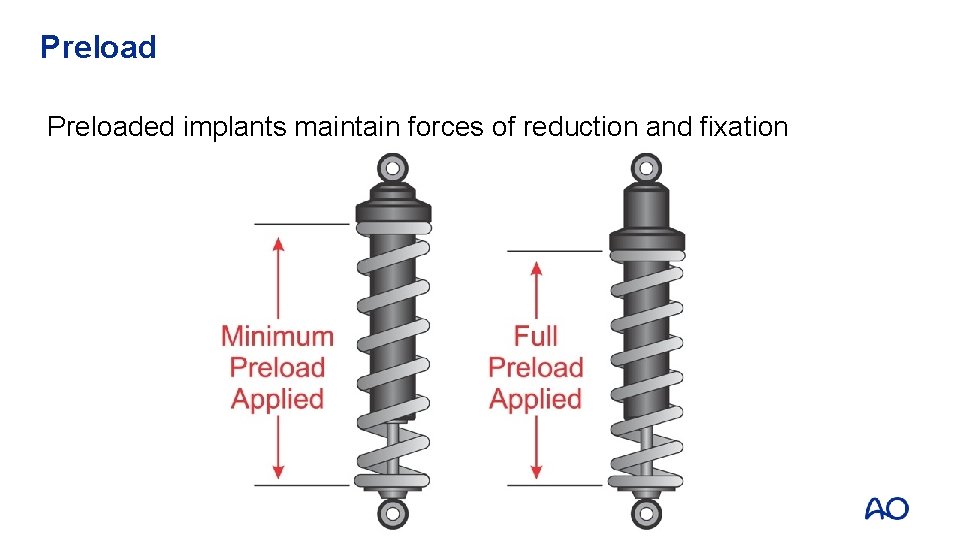
Preloaded implants maintain forces of reduction and fixation
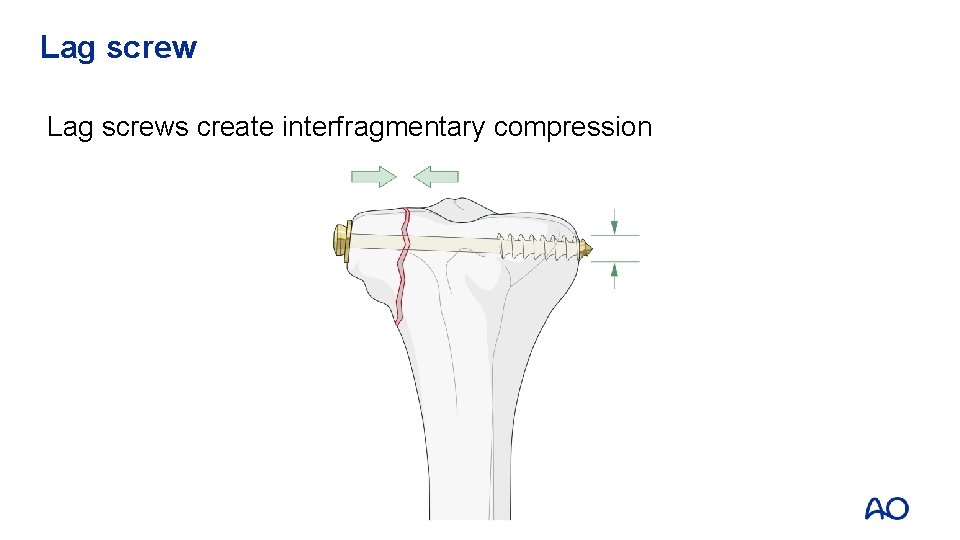
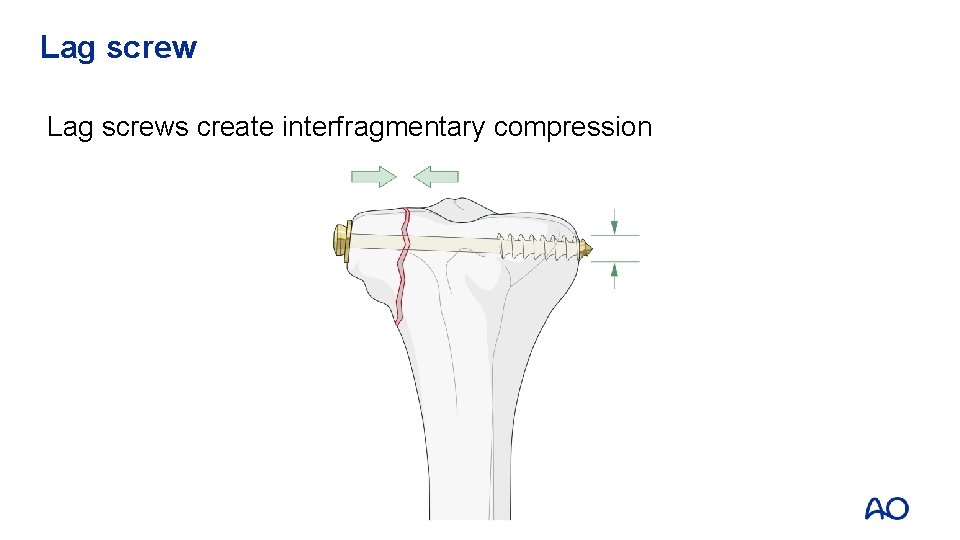
Lag screws create interfragmentary compression
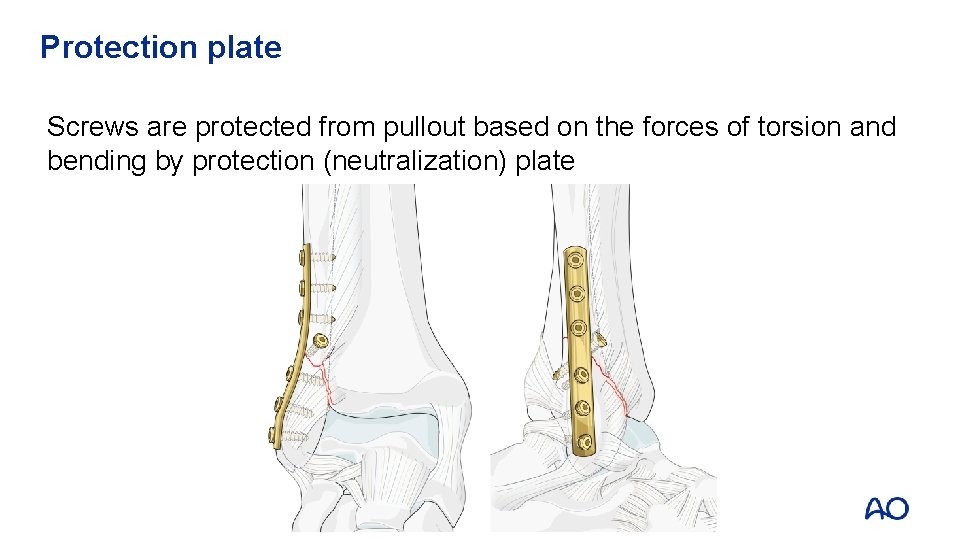
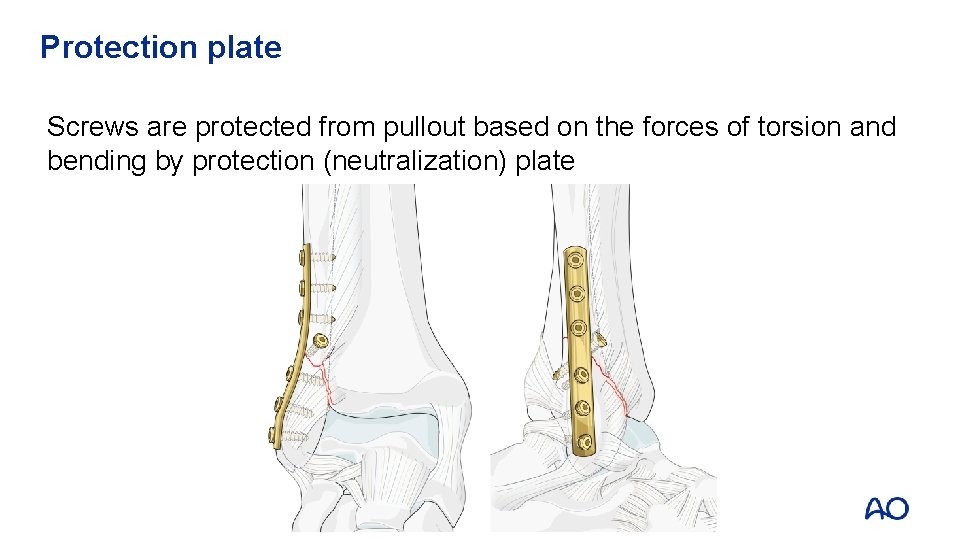
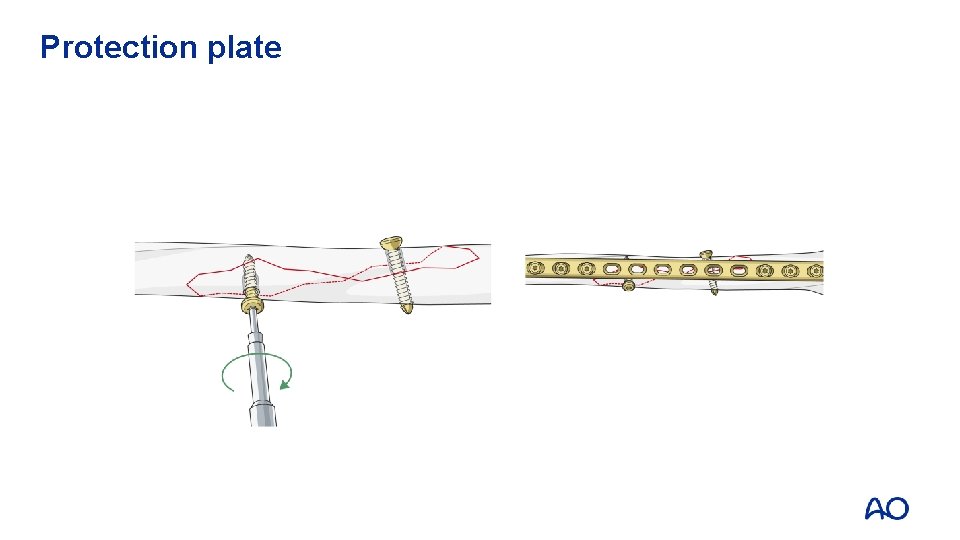
Protection plate Screws are protected from pullout based on the forces of torsion and bending by protection (neutralization) plate
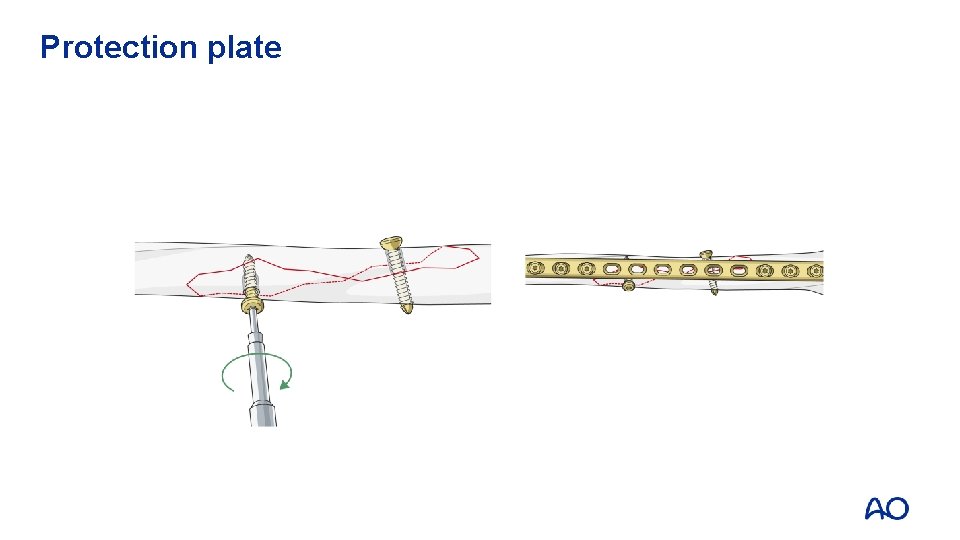
Protection plate
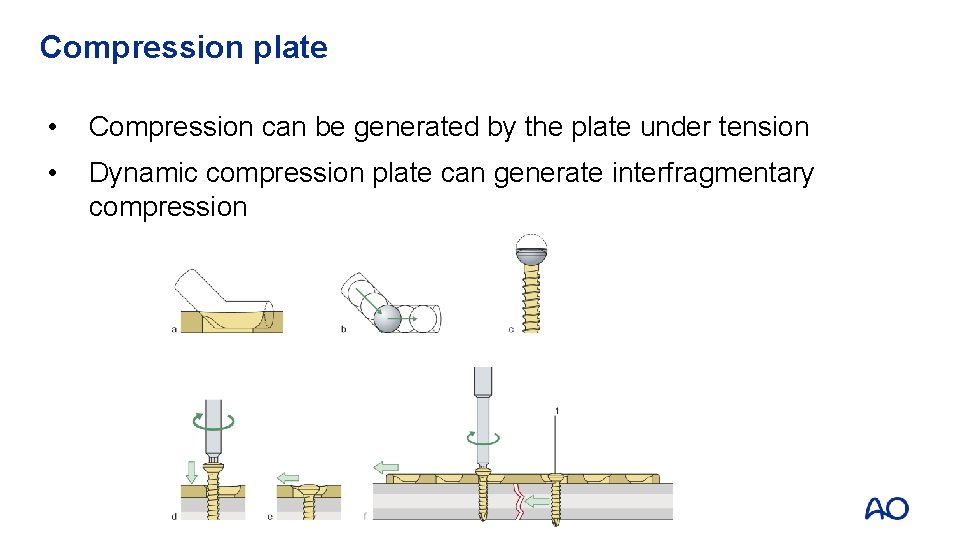
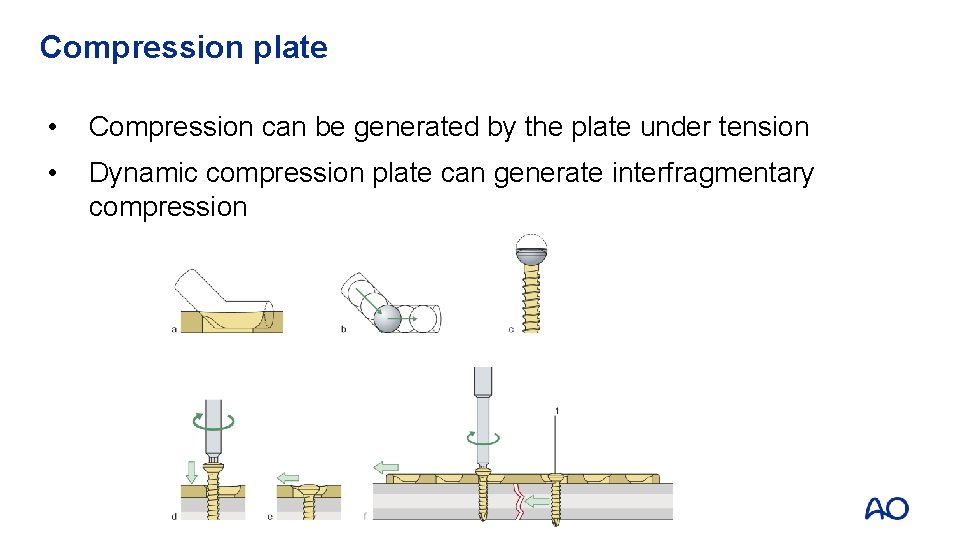
Compression plate • Compression can be generated by the plate under tension • Dynamic compression plate can generate interfragmentary compression
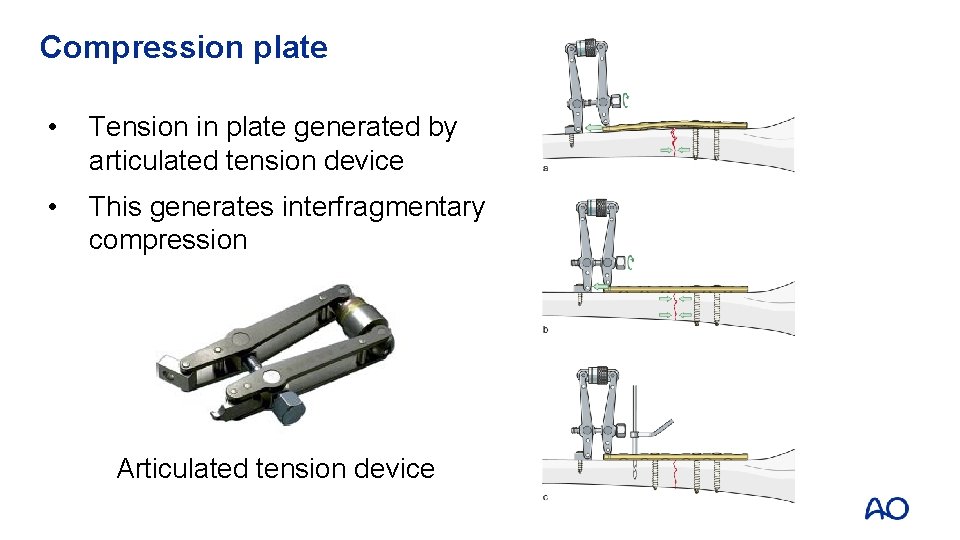
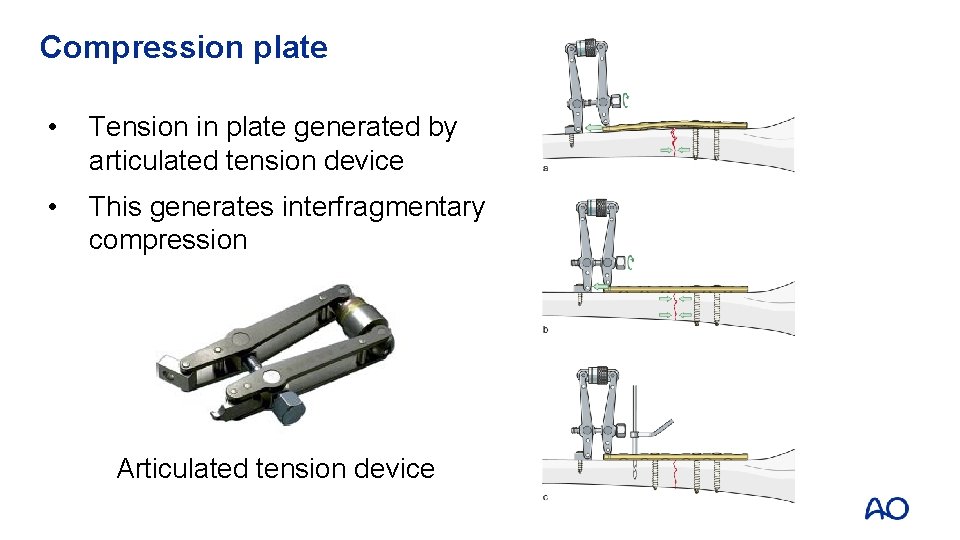
Compression plate • Tension in plate generated by articulated tension device • This generates interfragmentary compression Articulated tension device
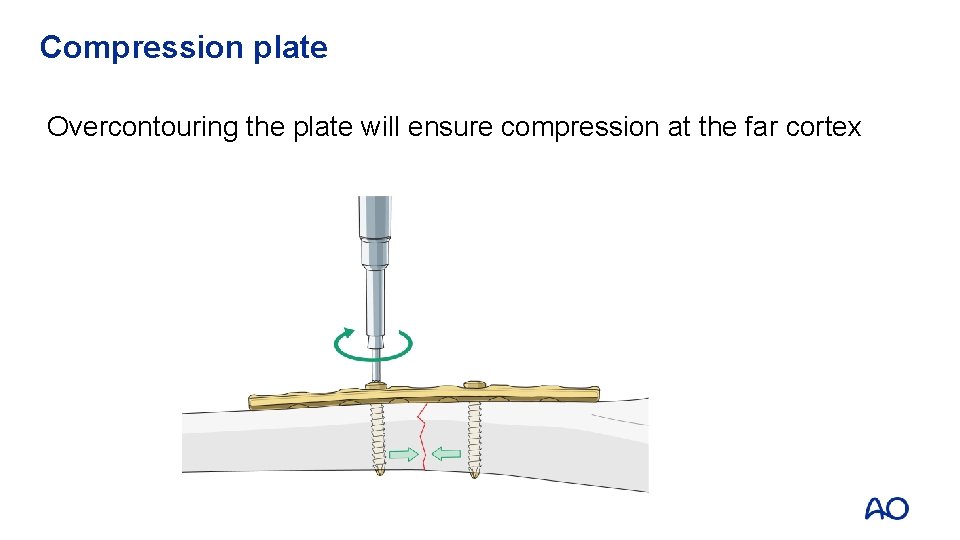
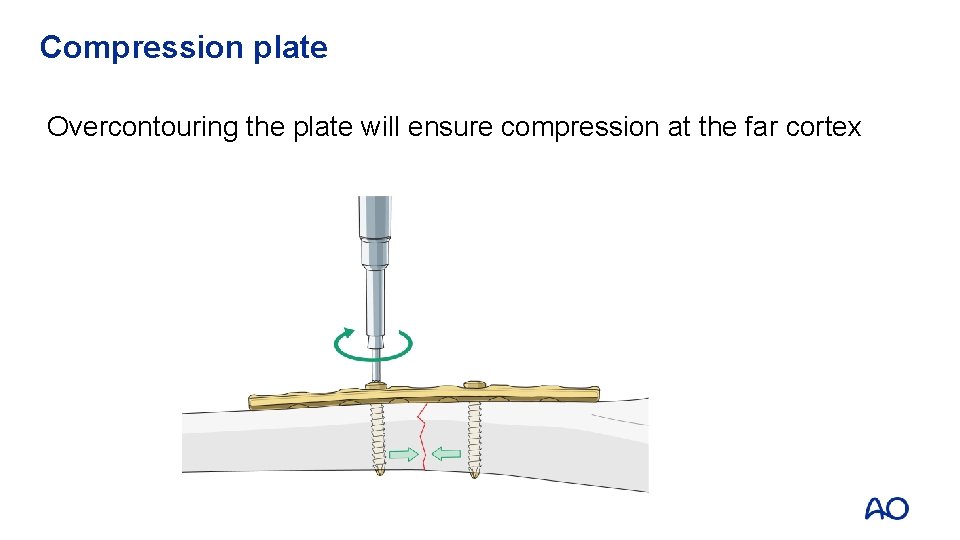
Compression plate Overcontouring the plate will ensure compression at the far cortex
Alignment is crucial Ideal implant will: • Hold the joint-bearing segments in their correct anatomical relationship until the bone in between heals with callus • Lie as close as possible to mechanical axis—line connecting centers of rotation of joints at each end
New design intramedullary nails
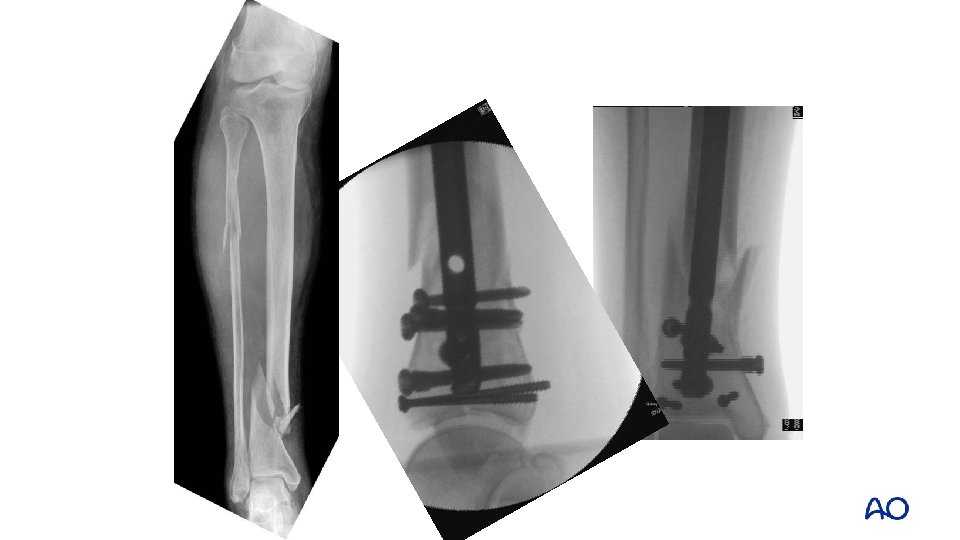
New design intramedullary nails • Extend the nailable zone into the metaphysis • Special techniques for reduction, particularly when the fracture is close to entry point

Entry point troubles
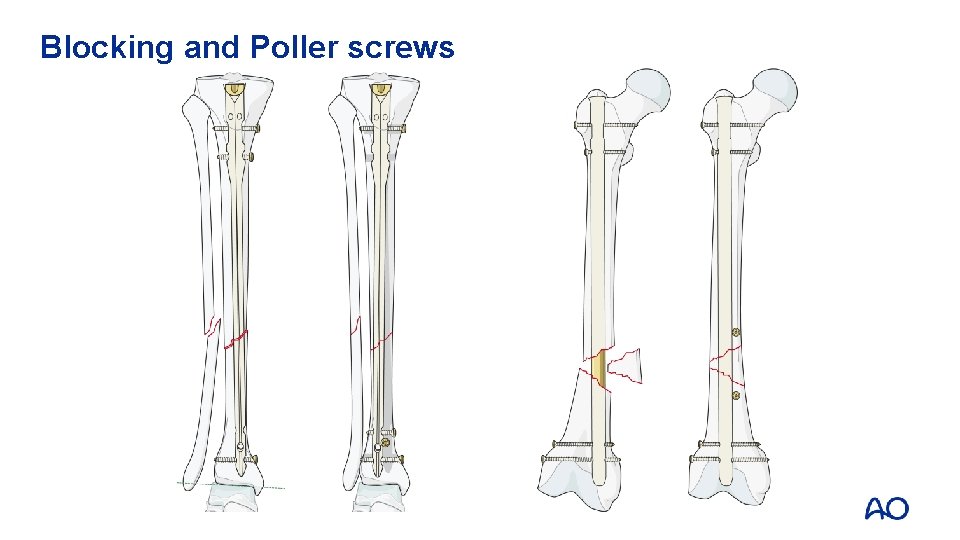
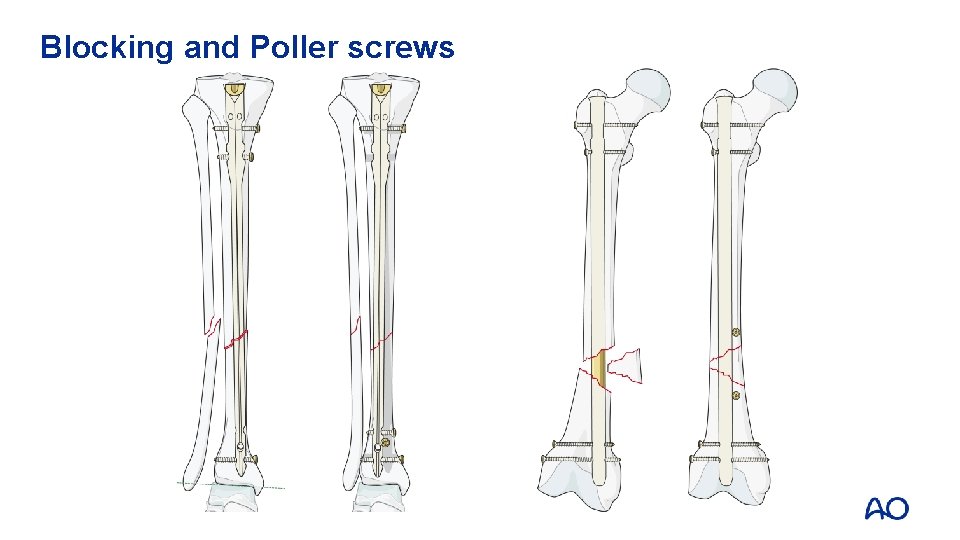
Blocking and Poller screws
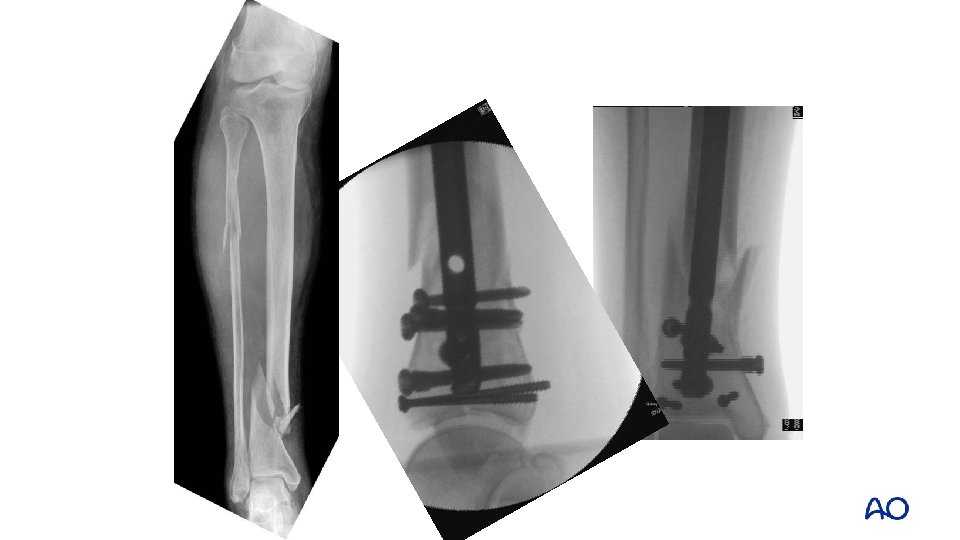

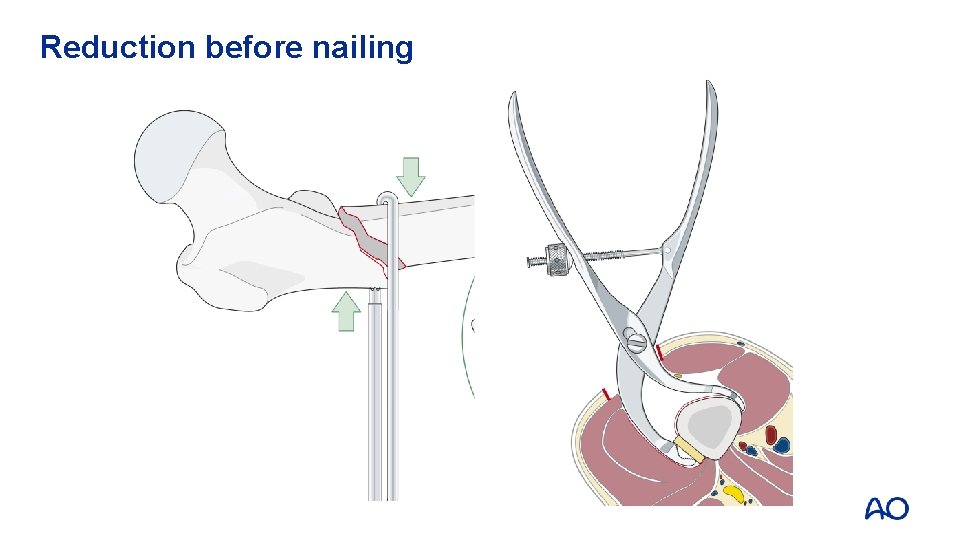
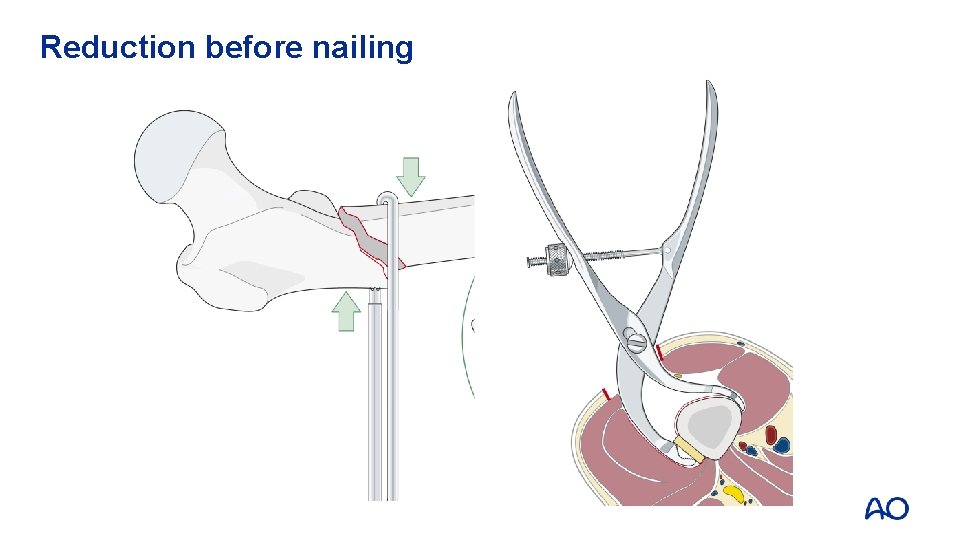
Reduction before nailing
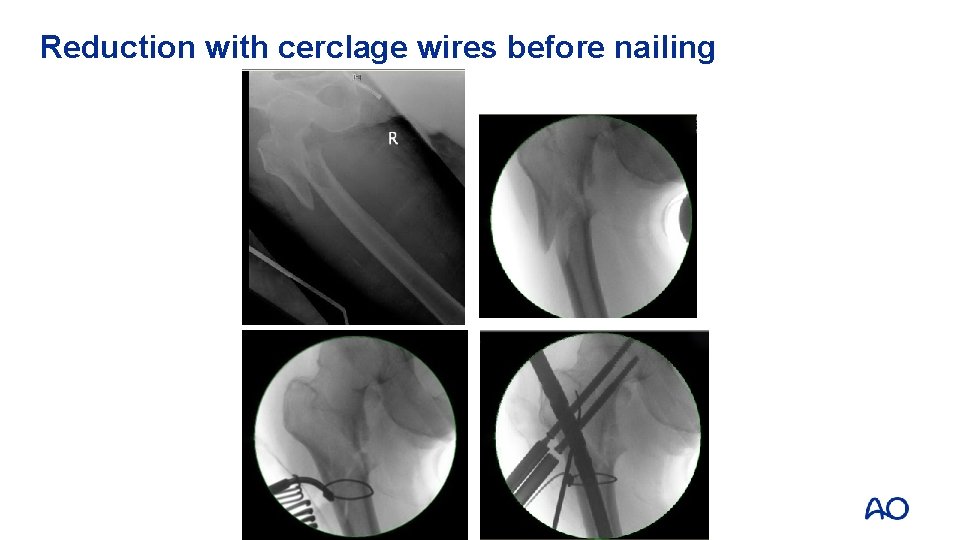
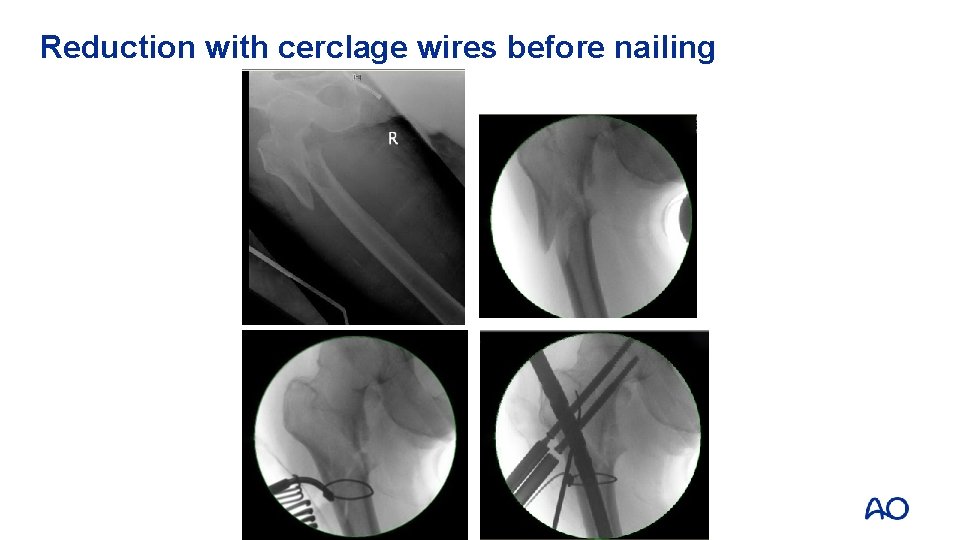
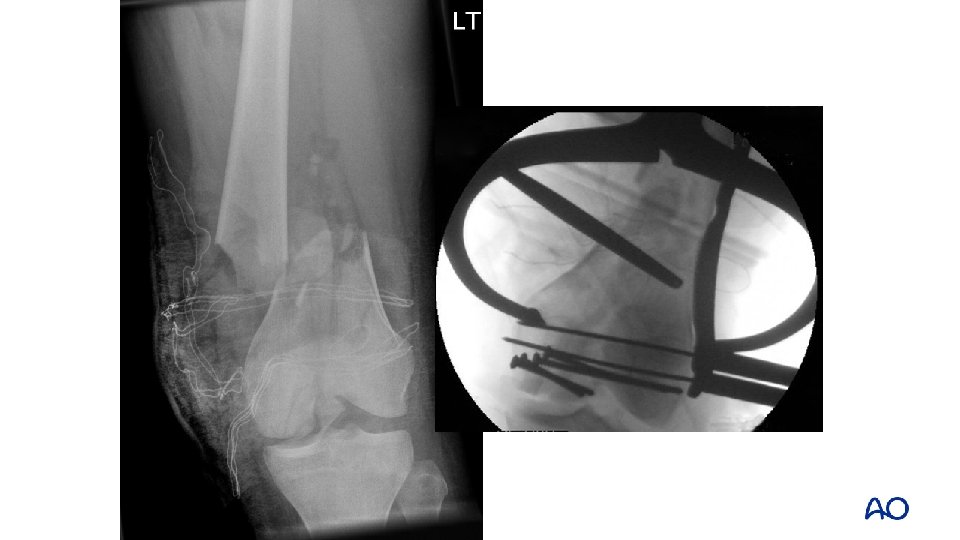
Reduction with cerclage wires before nailing
Bridging plate Hold the joint bearing segments in their correct anatomical relationship until the bone in between heals
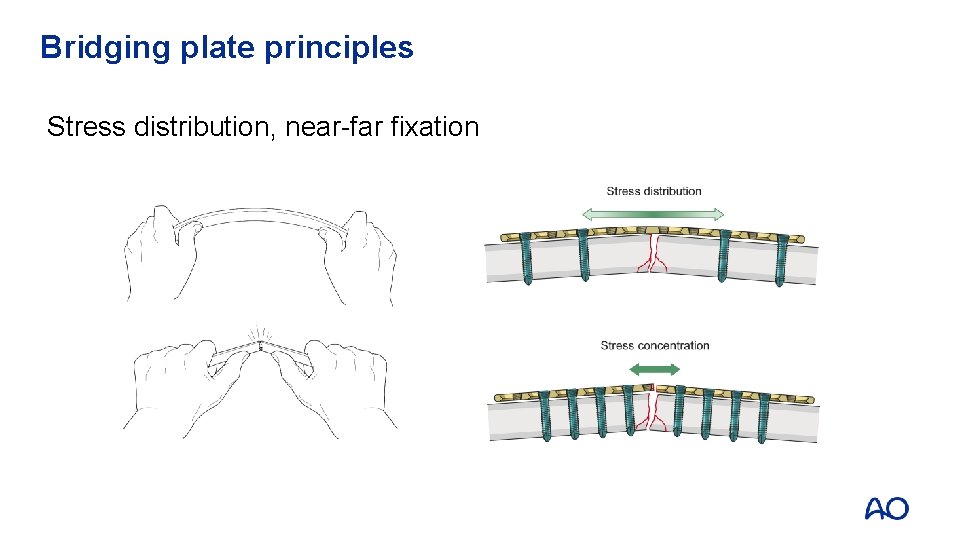
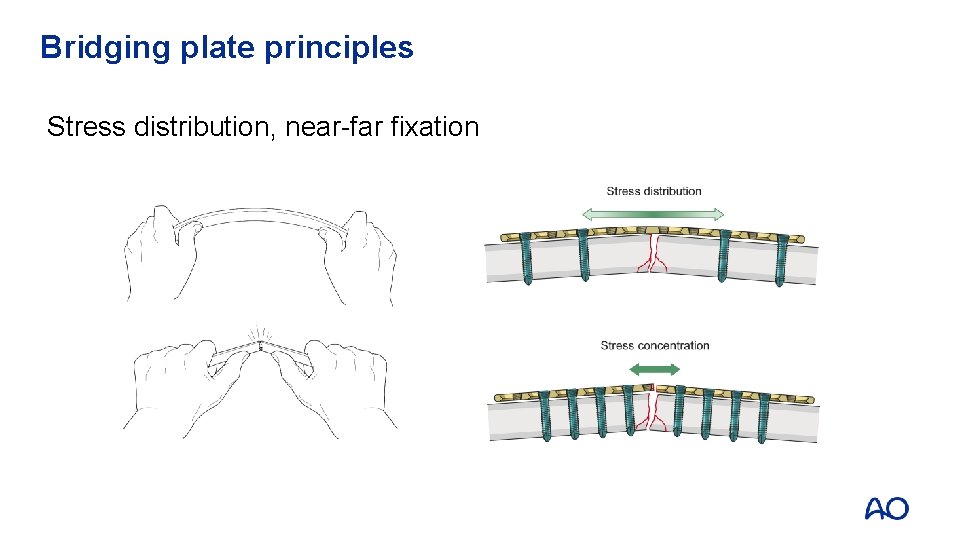
Bridging plate principles Stress distribution, near-far fixation
Minimal access techniques • Reduce surgical insult to traumatized soft tissues • Small incisions away from zone of injury • Less pain, faster rehabilitation • Technically demanding, requires sophisticated equipment
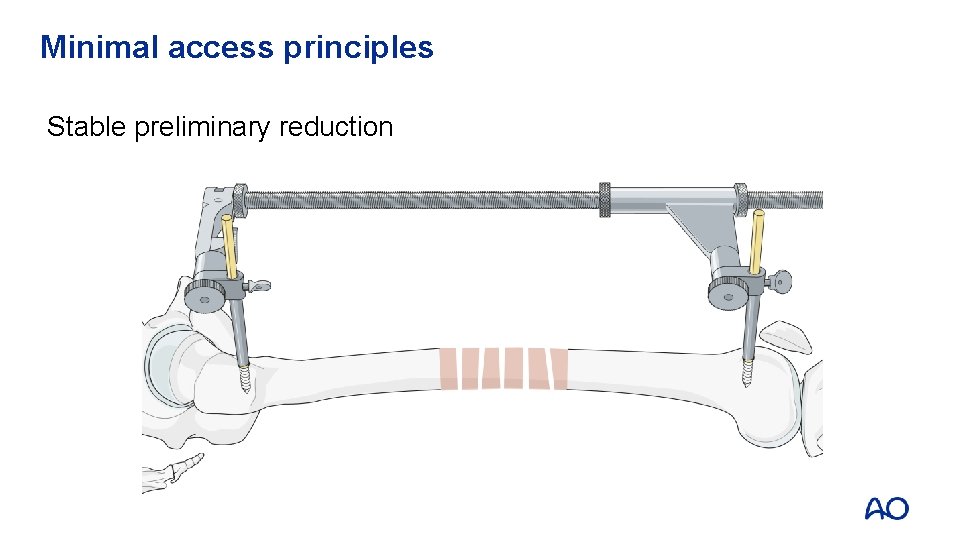
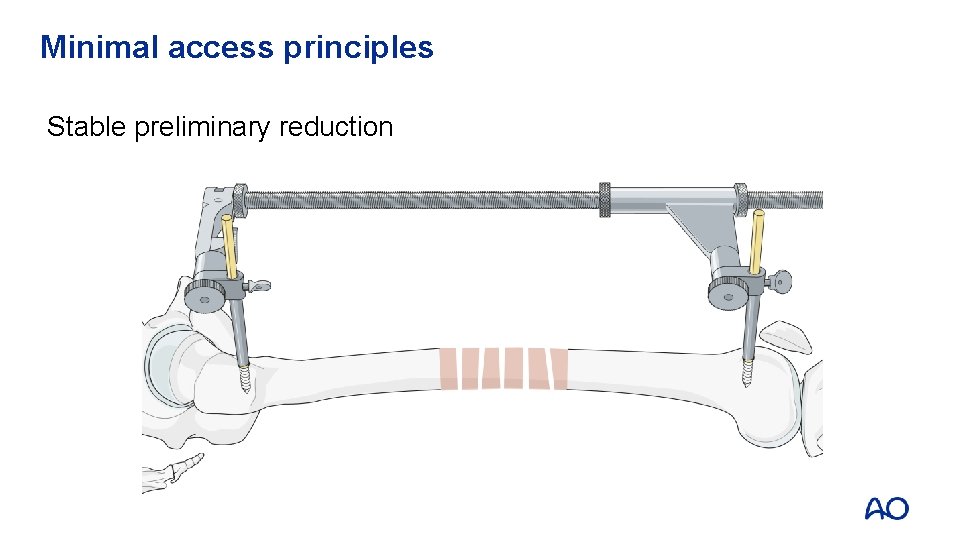
Minimal access principles Stable preliminary reduction
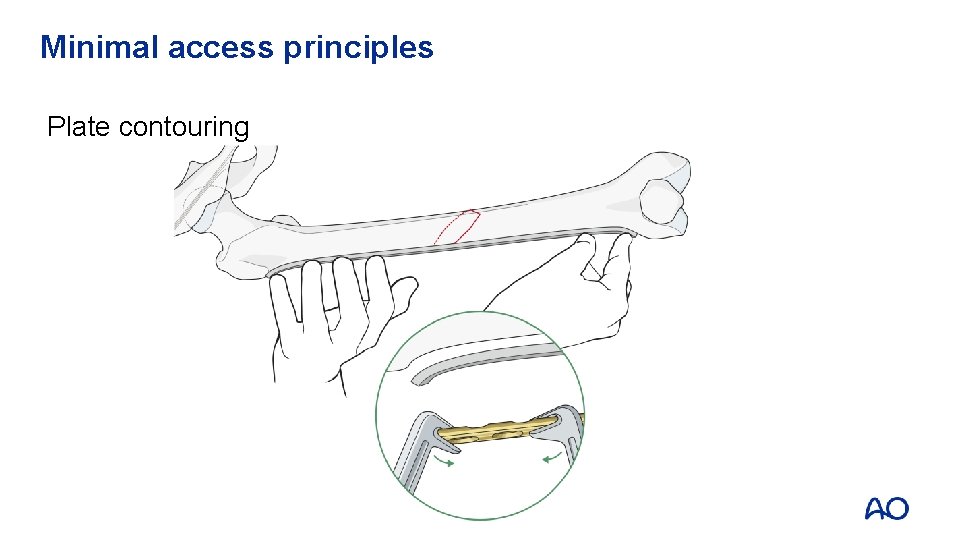
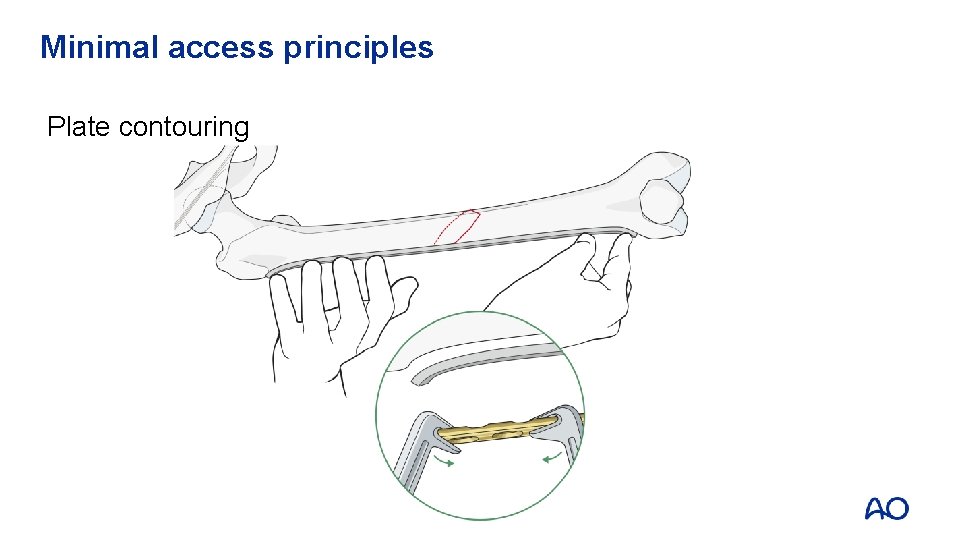
Minimal access principles Plate contouring
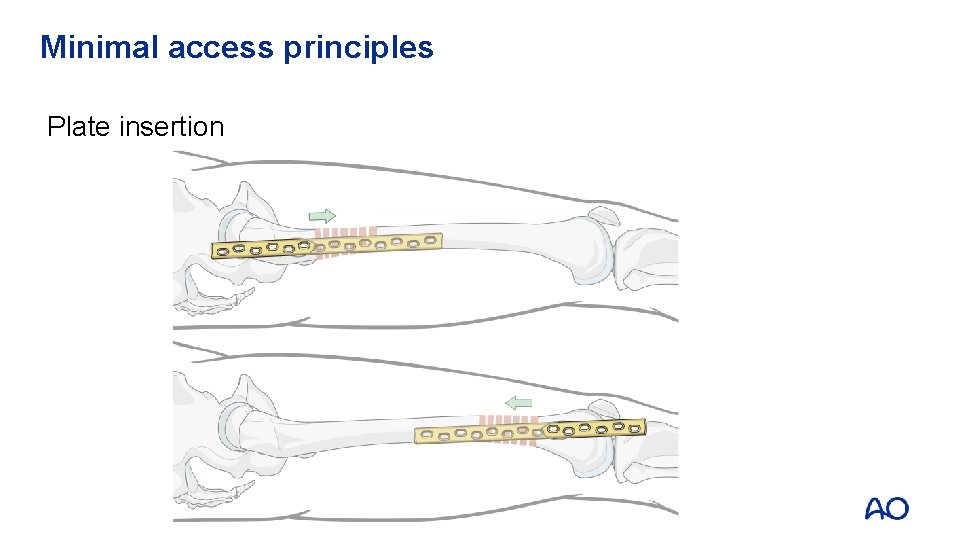
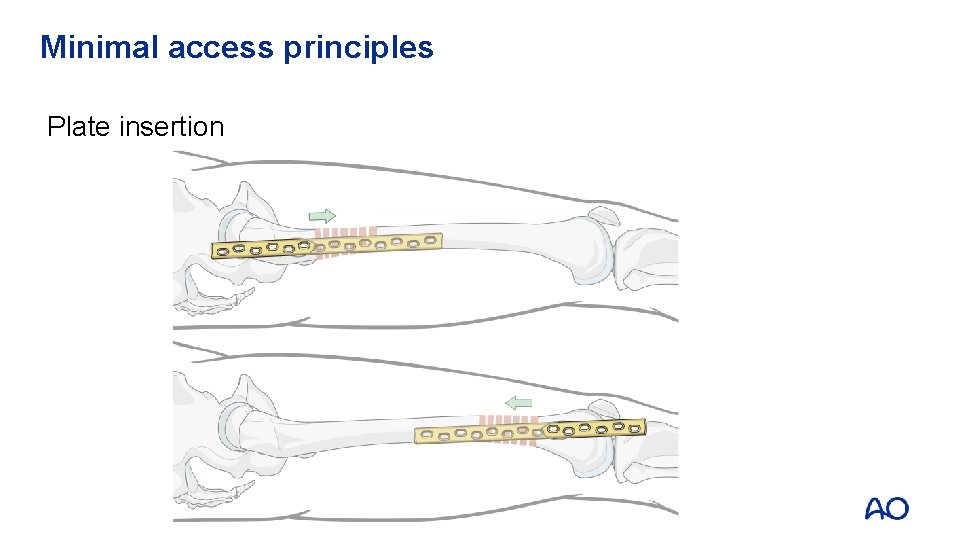
Minimal access principles Plate insertion
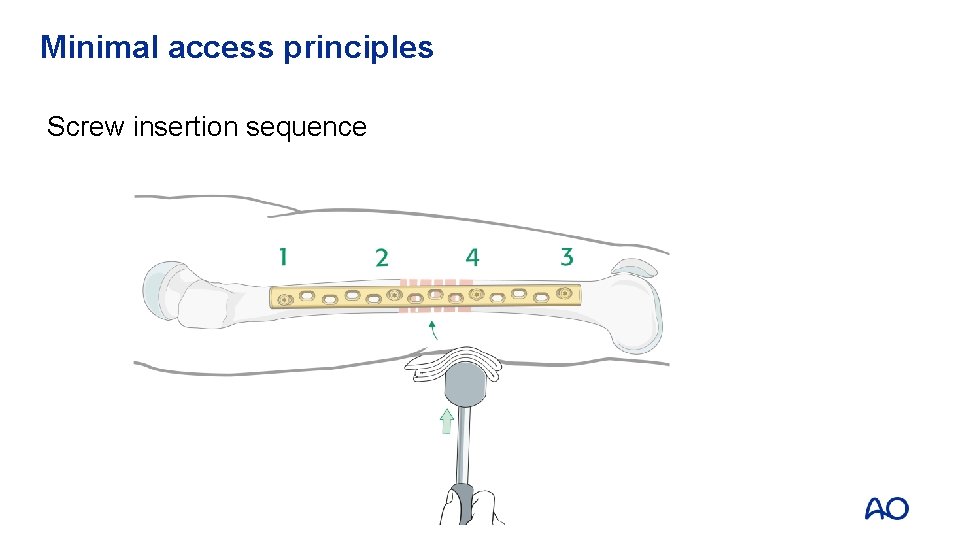
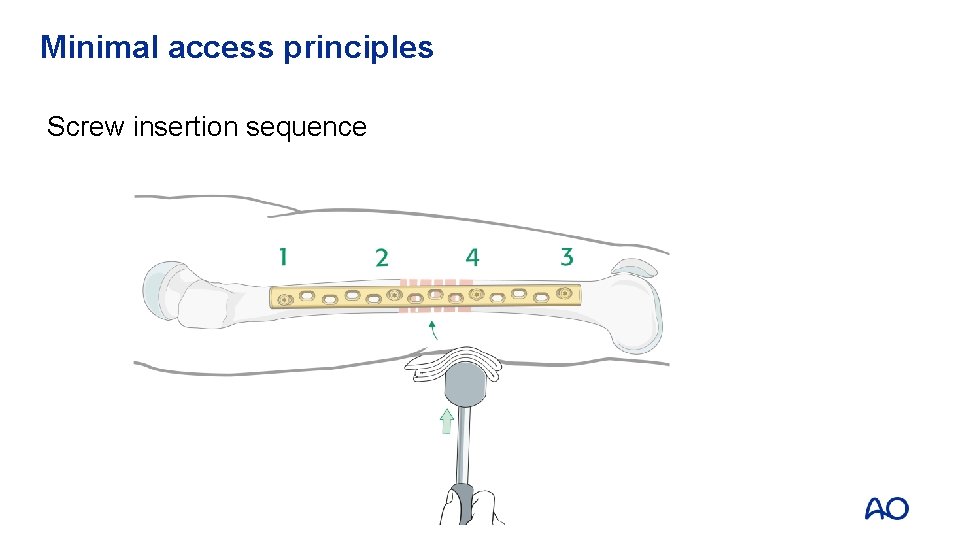
Minimal access principles Screw insertion sequence
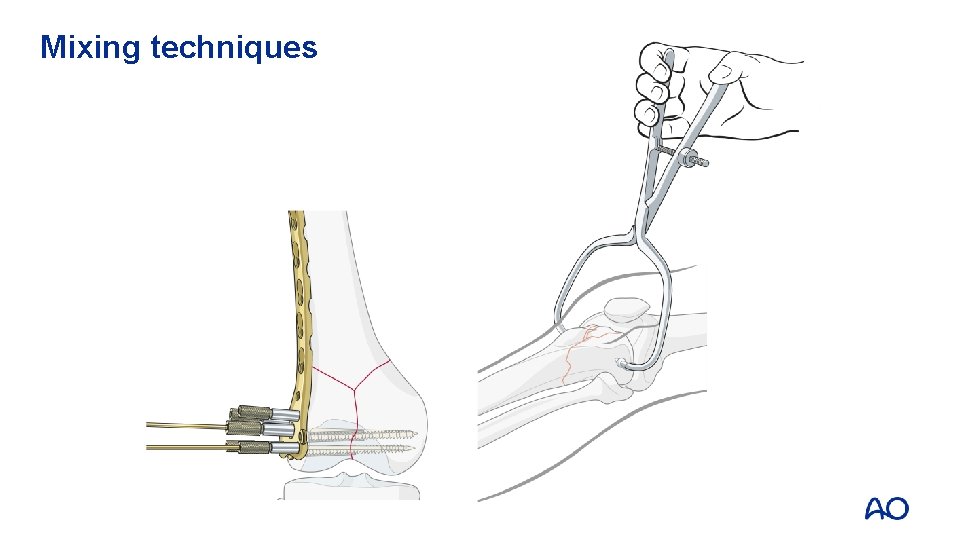
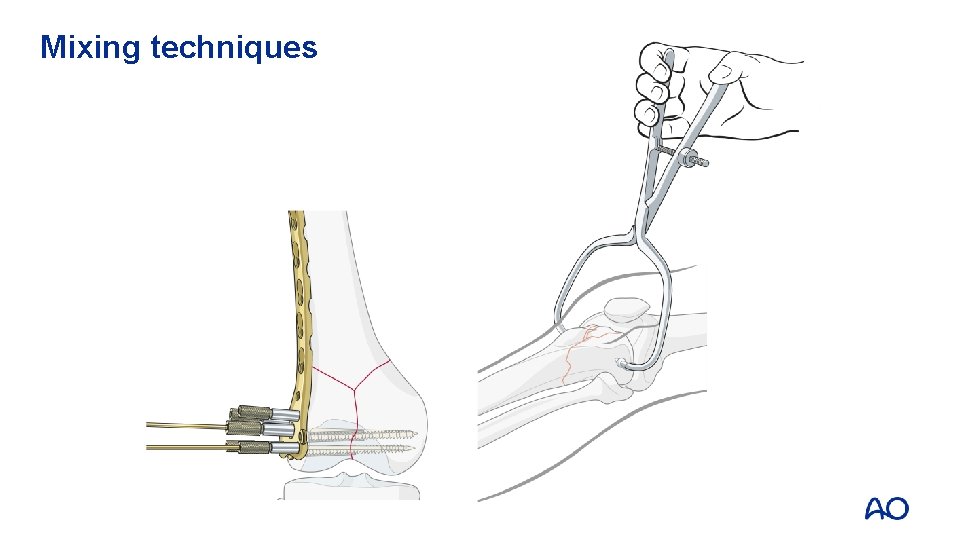
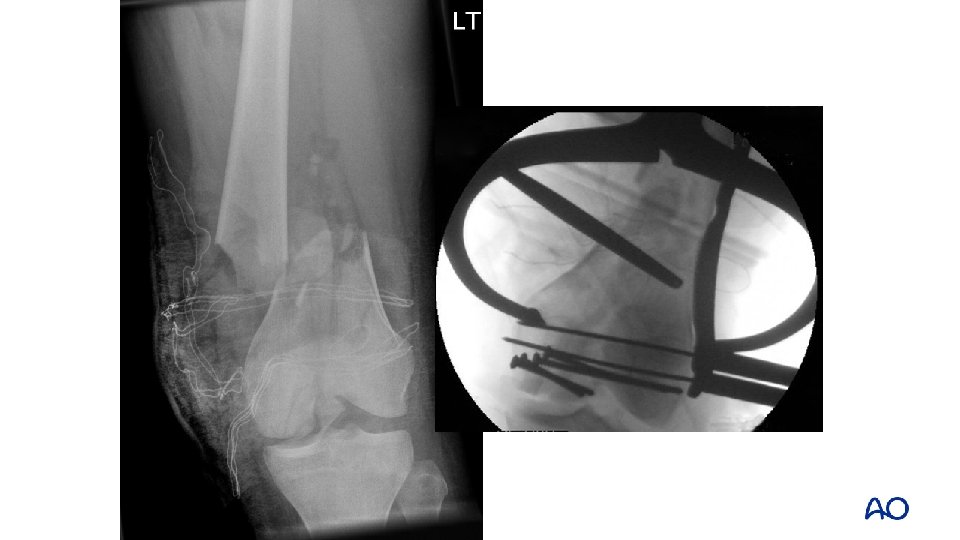
Mixing techniques

Take-home messages • Anatomy is crucial – absolute stability – low strain – implants under tension – no callus • Alignment only – choose nail or bridging plate – moderate strain – healing with callus • Important to have a plan that makes sense and to execute that plan appropriately