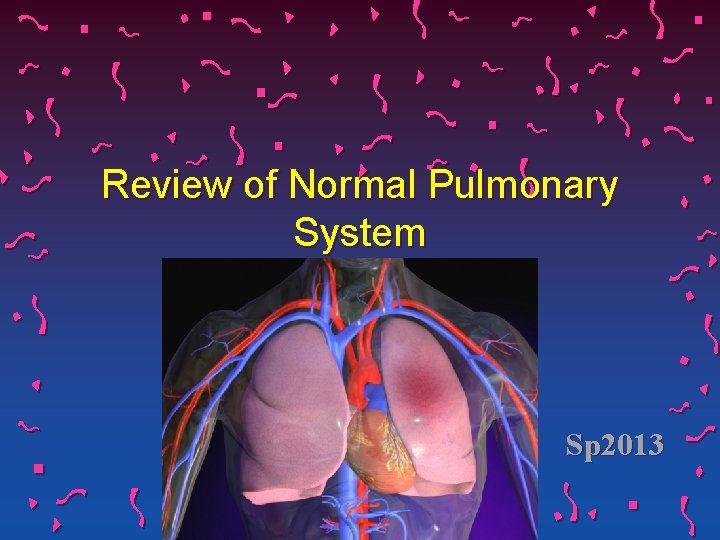
Review of Normal Pulmonary System Sp 2013 Respiratory




- Slides: 59
Review of Normal Pulmonary System Sp 2013
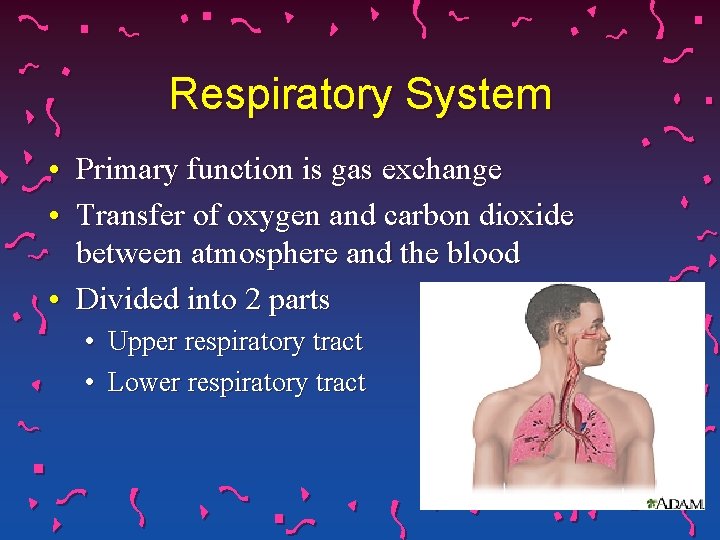
Respiratory System • Primary function is gas exchange • Transfer of oxygen and carbon dioxide between atmosphere and the blood • Divided into 2 parts • Upper respiratory tract • Lower respiratory tract
• Made up of : • Two lungs • Their airways • Blood vessels that serve them • Chest wall • Diaphragm • Thoracic gage
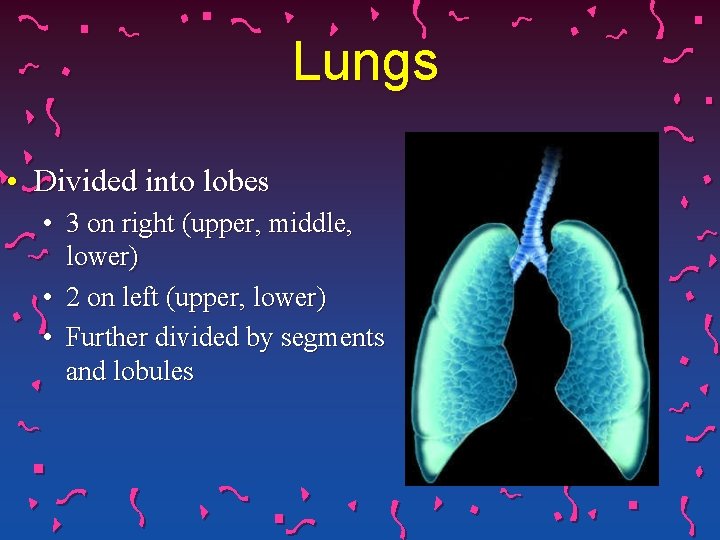
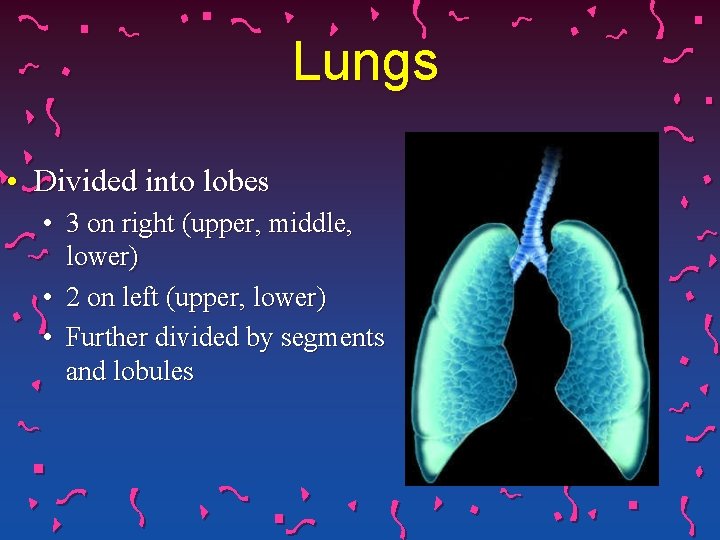
Lungs • Divided into lobes • 3 on right (upper, middle, lower) • 2 on left (upper, lower) • Further divided by segments and lobules
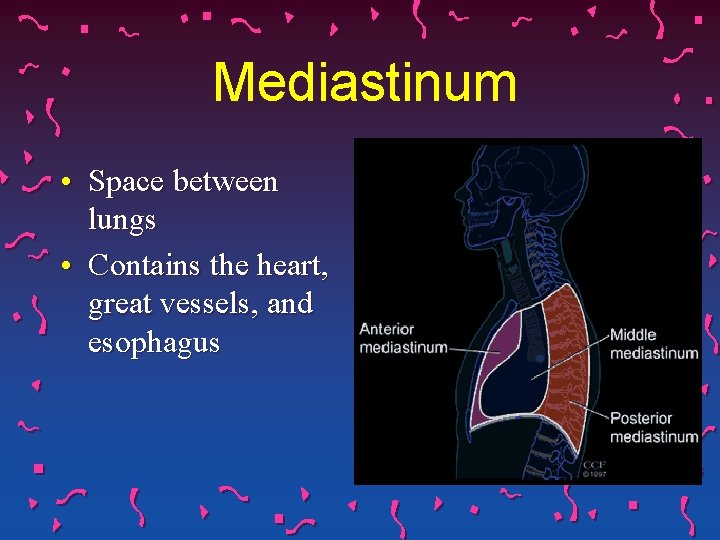
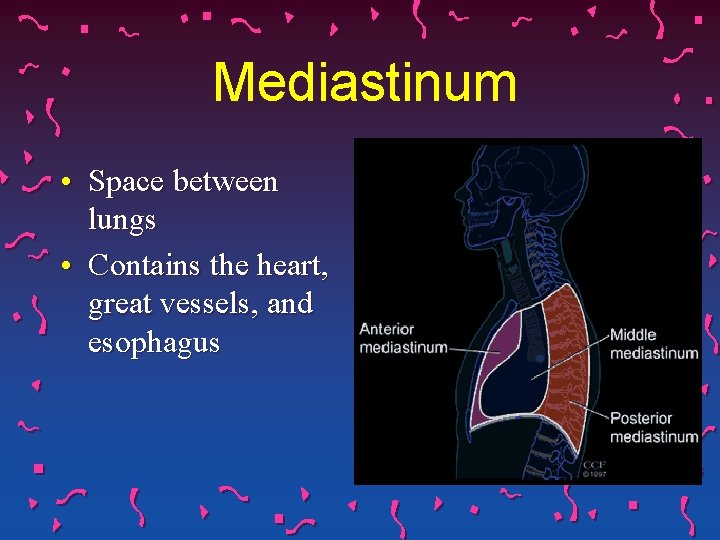
Mediastinum • Space between lungs • Contains the heart, great vessels, and esophagus
Chest Wall • Shaped, supported, and protected by 24 ribs (12 each side) • Ribs and sternum protect lungs and heart from injury • Rib Cage • Pleura • Respiratory muscles
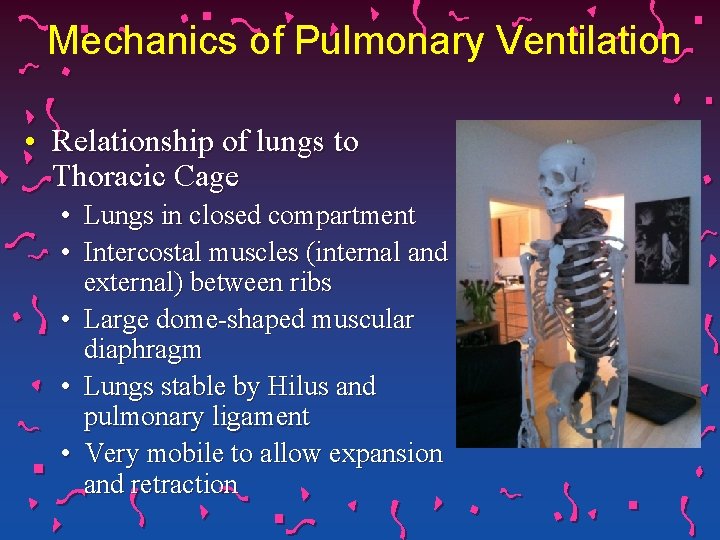
Mechanics of Pulmonary Ventilation • Relationship of lungs to Thoracic Cage • Lungs in closed compartment • Intercostal muscles (internal and external) between ribs • Large dome-shaped muscular diaphragm • Lungs stable by Hilus and pulmonary ligament • Very mobile to allow expansion and retraction

Mechanics of Pulmonary Ventilation • Parietal pleura • Interior surface of thoracic cavity • Visceral pleura • Surface of lung • Surfaces so closely apposed • Intrapleural space • Potential space • Filled with thin film of fluid produced by both layers • Acts as lubricant and adherent (glass slides with drop of water)
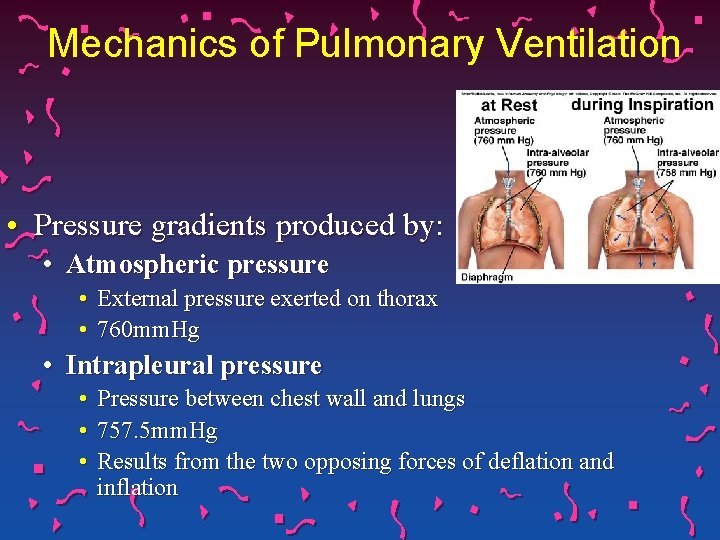
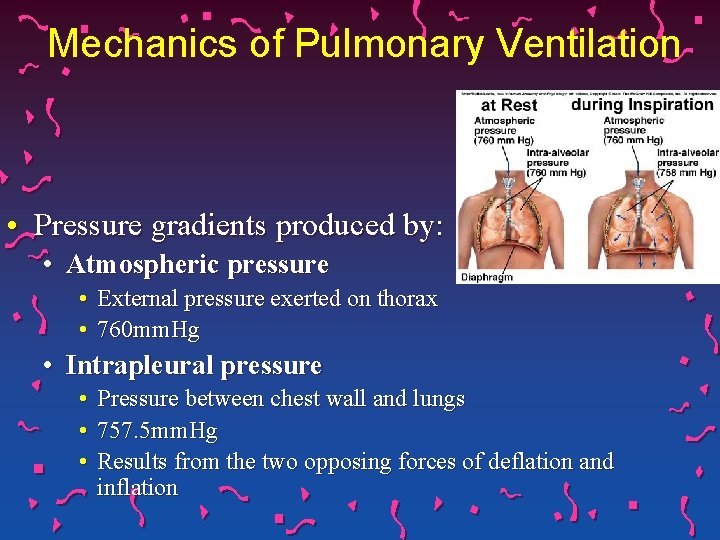
Mechanics of Pulmonary Ventilation • Pressure gradients produced by: • Atmospheric pressure • External pressure exerted on thorax • 760 mm. Hg • Intrapleural pressure • Pressure between chest wall and lungs • 757. 5 mm. Hg • Results from the two opposing forces of deflation and inflation
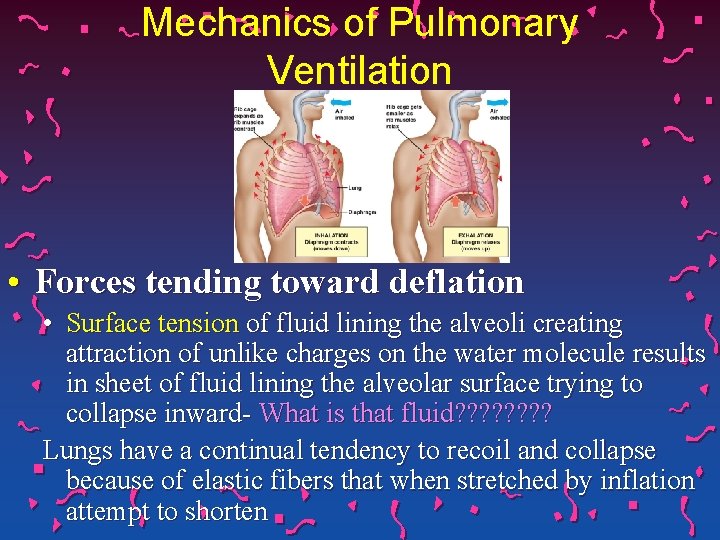
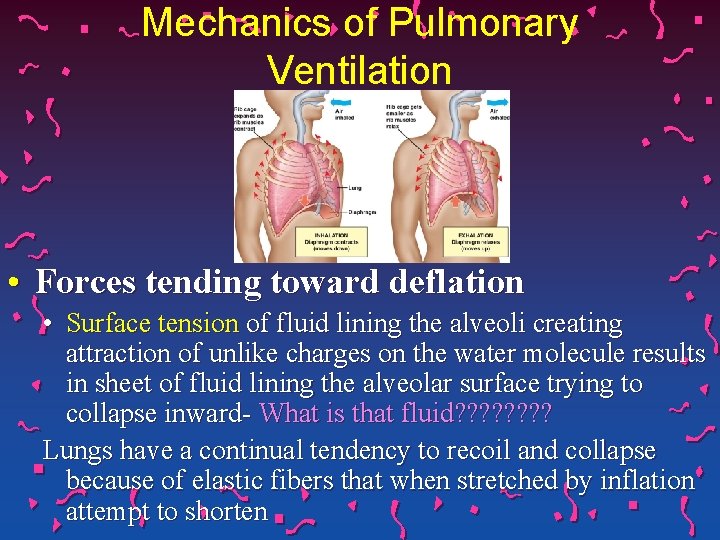
Mechanics of Pulmonary Ventilation • Forces tending toward deflation • Surface tension of fluid lining the alveoli creating attraction of unlike charges on the water molecule results in sheet of fluid lining the alveolar surface trying to collapse inward- What is that fluid? ? ? ? Lungs have a continual tendency to recoil and collapse because of elastic fibers that when stretched by inflation attempt to shorten
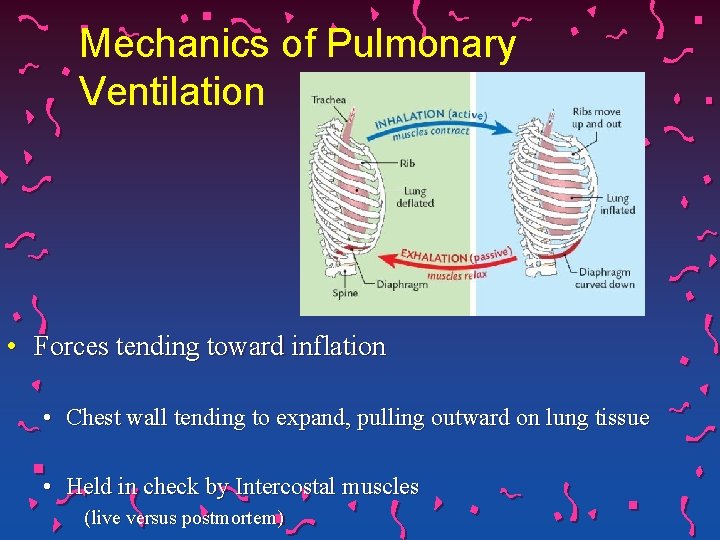
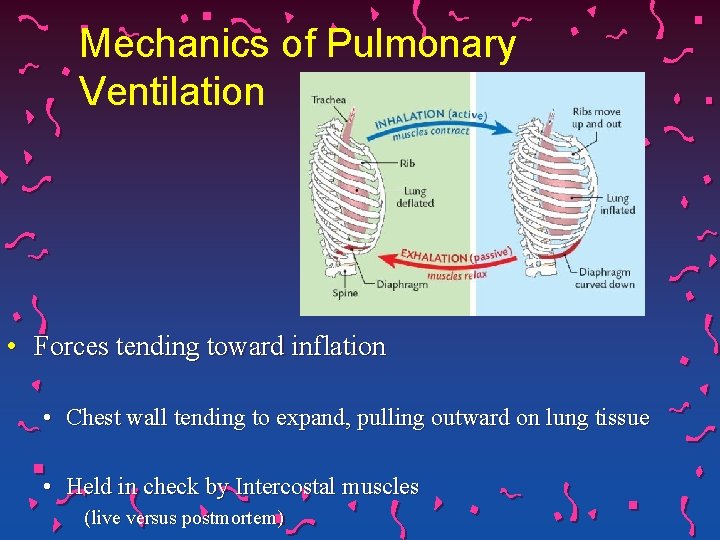
Mechanics of Pulmonary Ventilation • Forces tending toward inflation • Chest wall tending to expand, pulling outward on lung tissue • Held in check by Intercostal muscles (live versus postmortem)
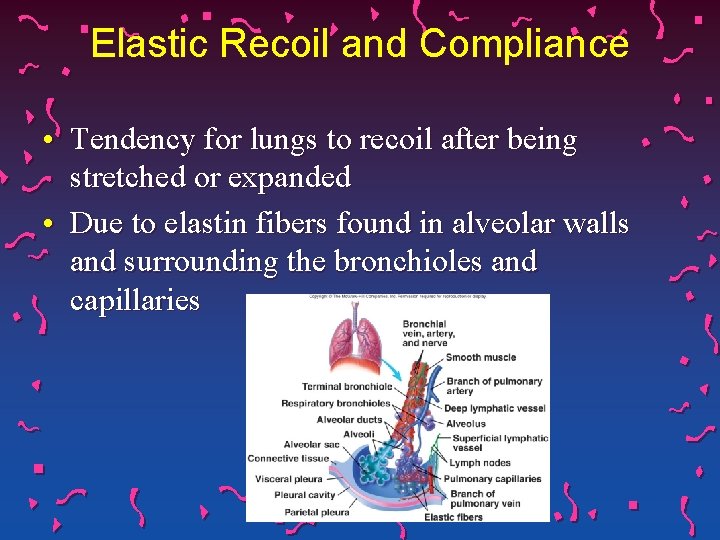
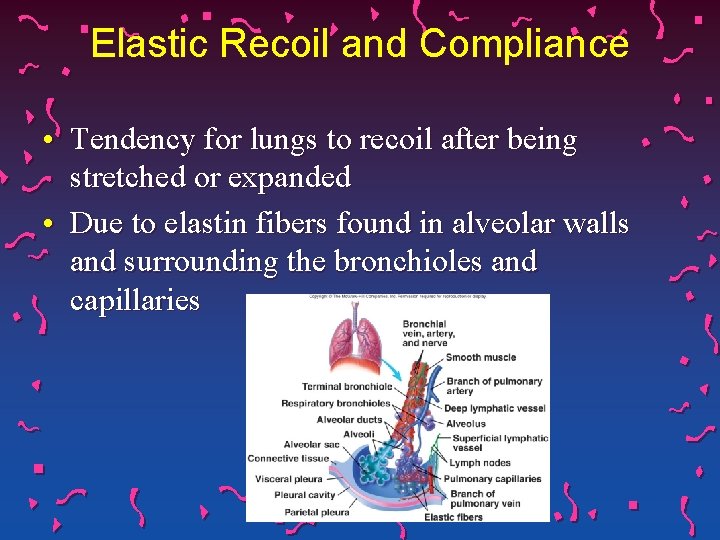
Elastic Recoil and Compliance • Tendency for lungs to recoil after being stretched or expanded • Due to elastin fibers found in alveolar walls and surrounding the bronchioles and capillaries
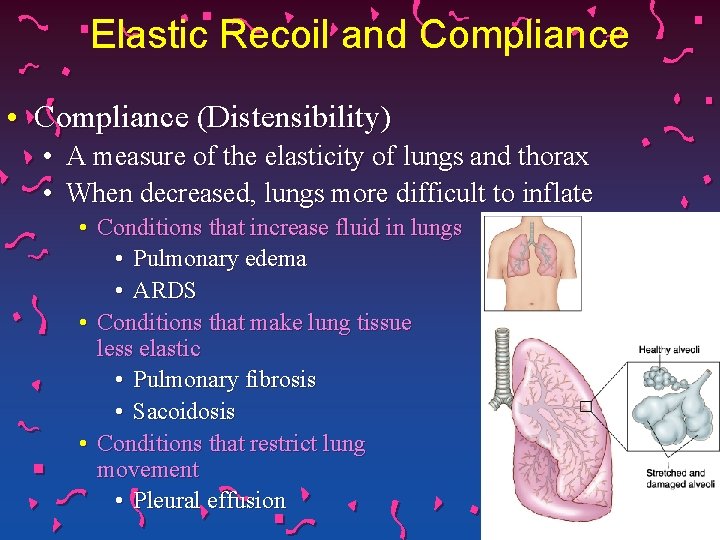
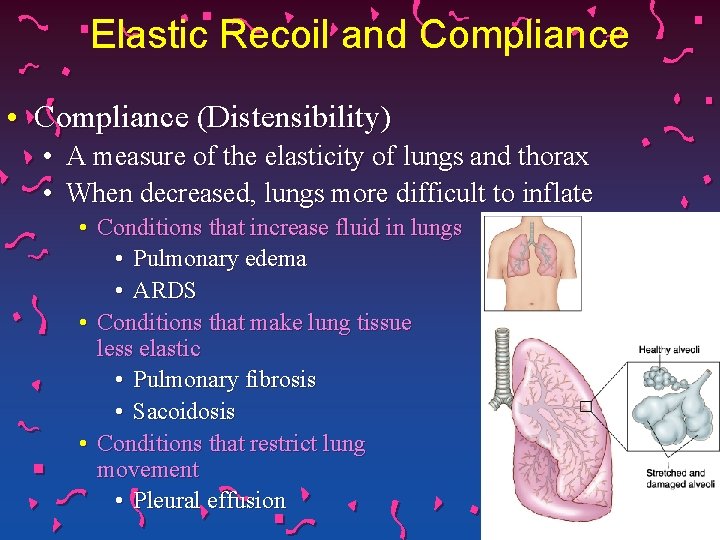
Elastic Recoil and Compliance • Compliance (Distensibility) • A measure of the elasticity of lungs and thorax • When decreased, lungs more difficult to inflate • Conditions that increase fluid in lungs • Pulmonary edema • ARDS • Conditions that make lung tissue less elastic • Pulmonary fibrosis • Sacoidosis • Conditions that restrict lung movement • Pleural effusion
Elastic Recoil and Compliance • Compliance is increased • as a result of aging • Destruction of alveolar walls • Loss of tissue elasticity • emphysema
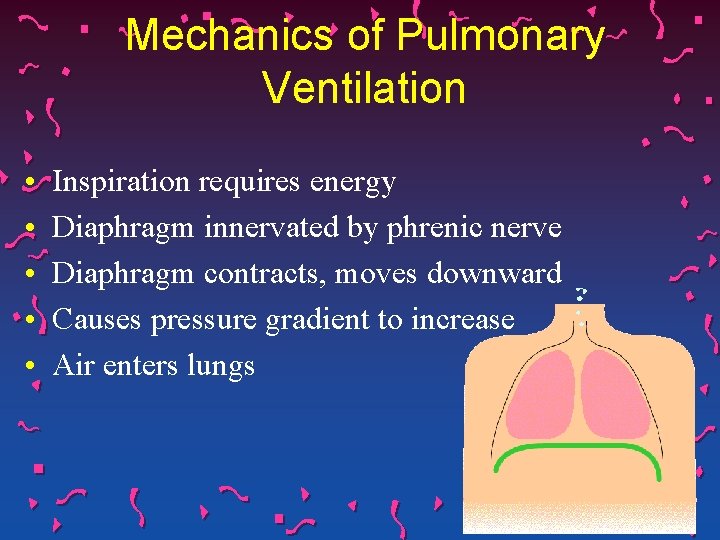
Mechanics of Pulmonary Ventilation • • • Inspiration requires energy Diaphragm innervated by phrenic nerve Diaphragm contracts, moves downward Causes pressure gradient to increase Air enters lungs
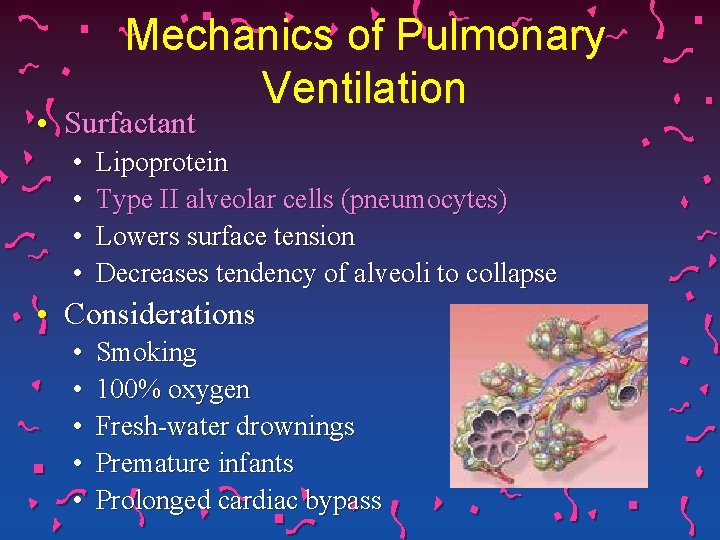
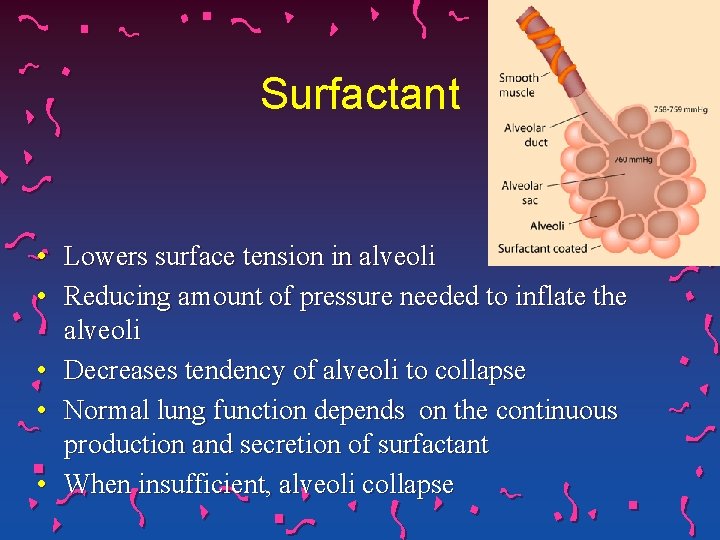
Mechanics of Pulmonary Ventilation • Surfactant • • Lipoprotein Type II alveolar cells (pneumocytes) Lowers surface tension Decreases tendency of alveoli to collapse • Considerations • • • Smoking 100% oxygen Fresh-water drownings Premature infants Prolonged cardiac bypass
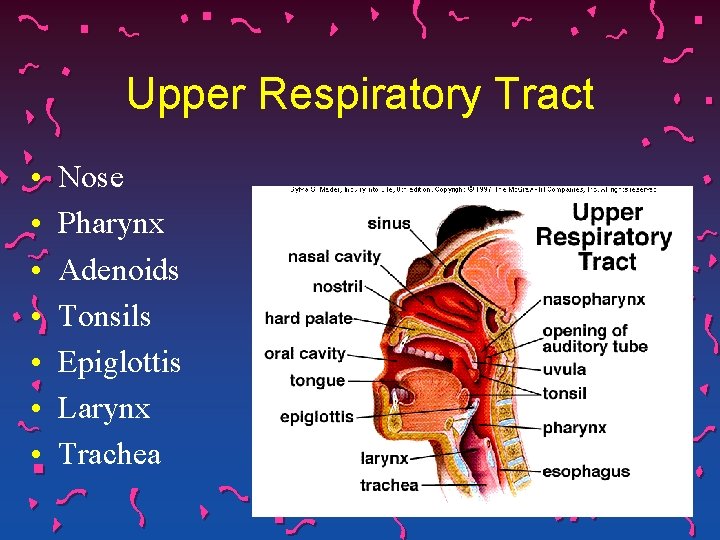
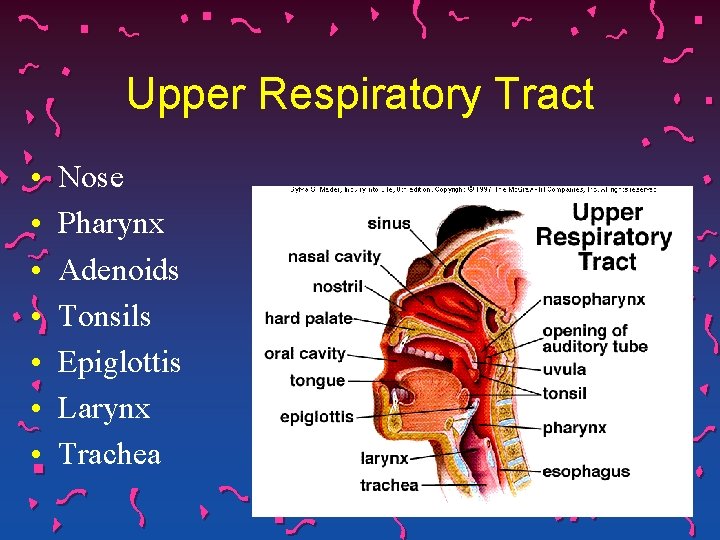
Upper Respiratory Tract • • Nose Pharynx Adenoids Tonsils Epiglottis Larynx Trachea
Remember… • The epiglottis (small flap of tissue at base of tongue) covers larynx during swallowing • Any condition that alters mental status or swallowing ability may impair this protective function • Decreased LOC • CVA • Presence of tracheostomy tube
Upper Respiratory Tract • Major functions • Filtration of dust, dirt, foreign materials, and bacteria larger than 5 -10 microns • Humidification and warming of air • Considerations • • • Olfactory nerve endings at roof of nose Laryngeal nerve is branch of Vagus (X) Trachea supported by U-shaped cartilages, connects larynx to bronchi (conducting airways)
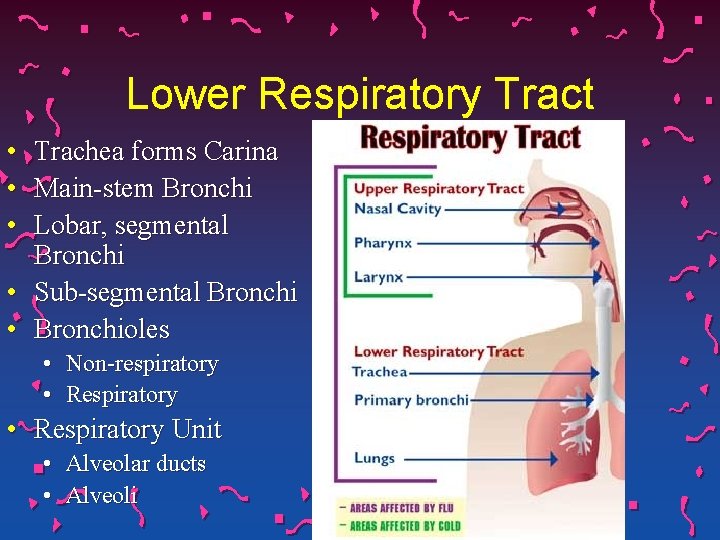
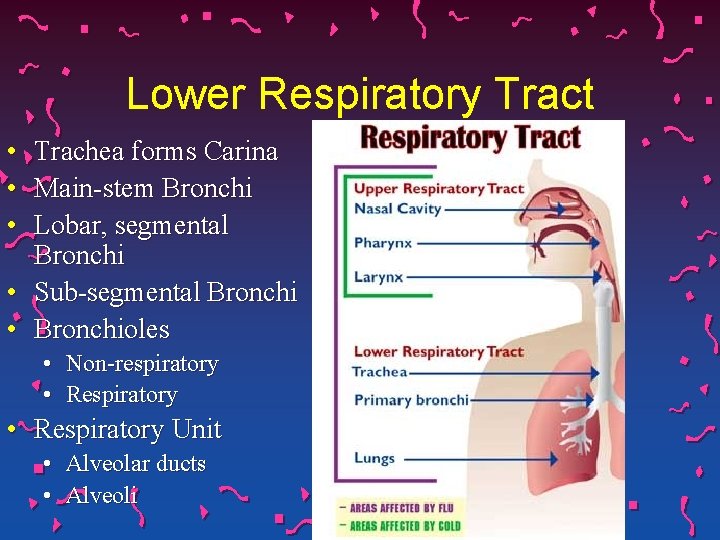
Lower Respiratory Tract • • • Trachea forms Carina Main-stem Bronchi Lobar, segmental Bronchi • Sub-segmental Bronchi • Bronchioles • Non-respiratory • Respiratory Unit • Alveolar ducts • Alveoli
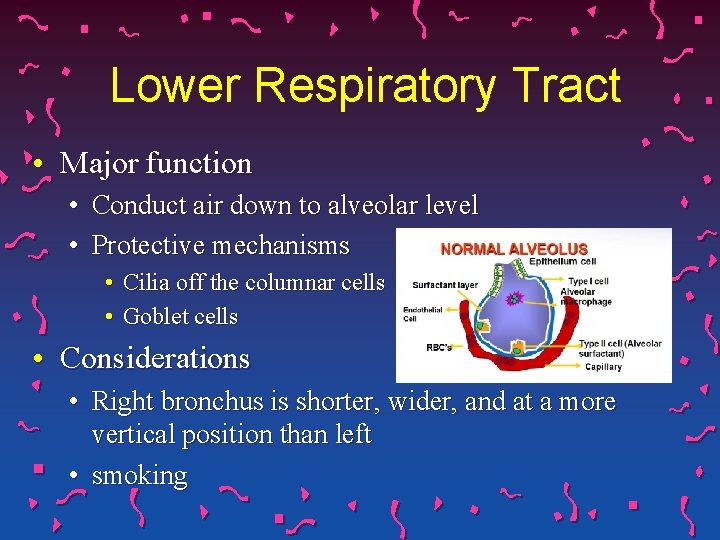
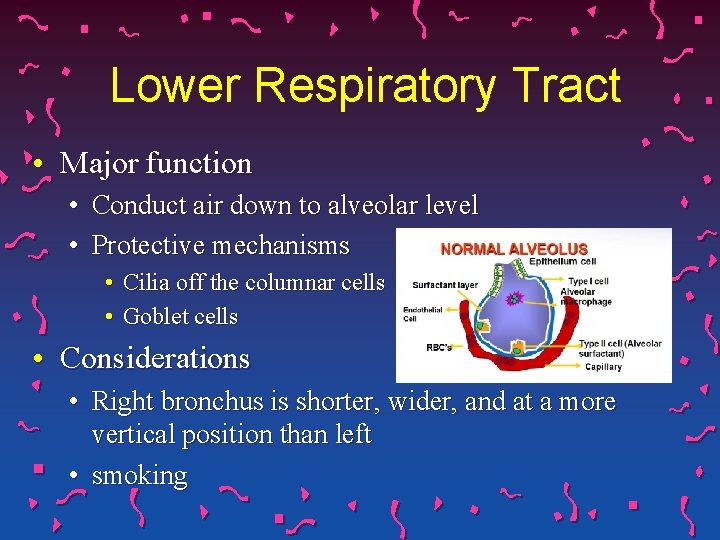
Lower Respiratory Tract • Major function • Conduct air down to alveolar level • Protective mechanisms • Cilia off the columnar cells • Goblet cells • Considerations • Right bronchus is shorter, wider, and at a more vertical position than left • smoking
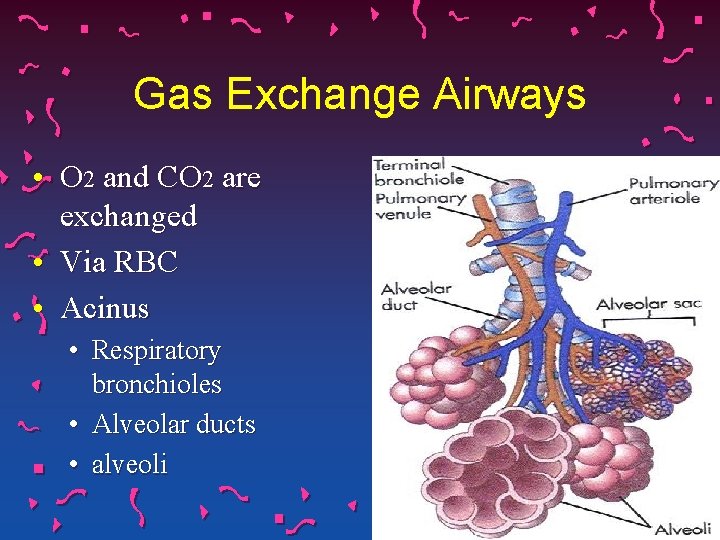
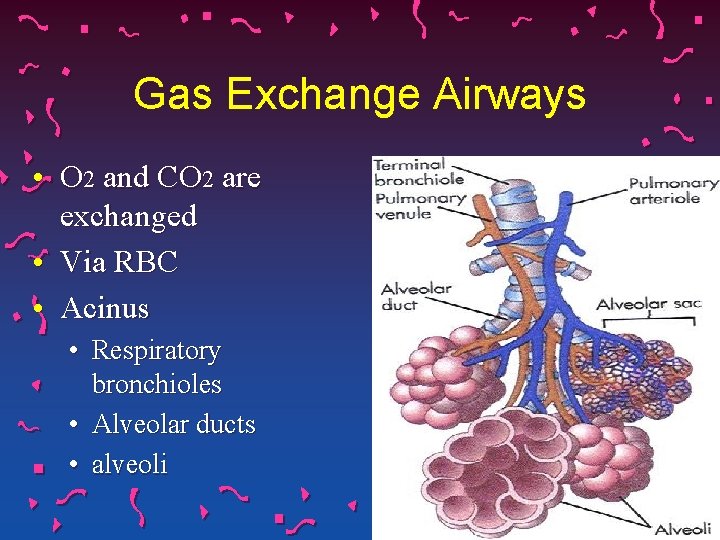
Gas Exchange Airways • O 2 and CO 2 are exchanged • Via RBC • Acinus • Respiratory bronchioles • Alveolar ducts • alveoli
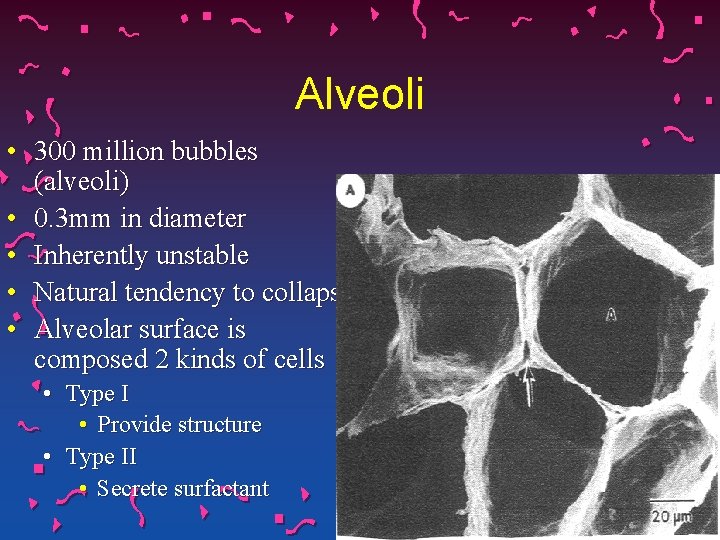
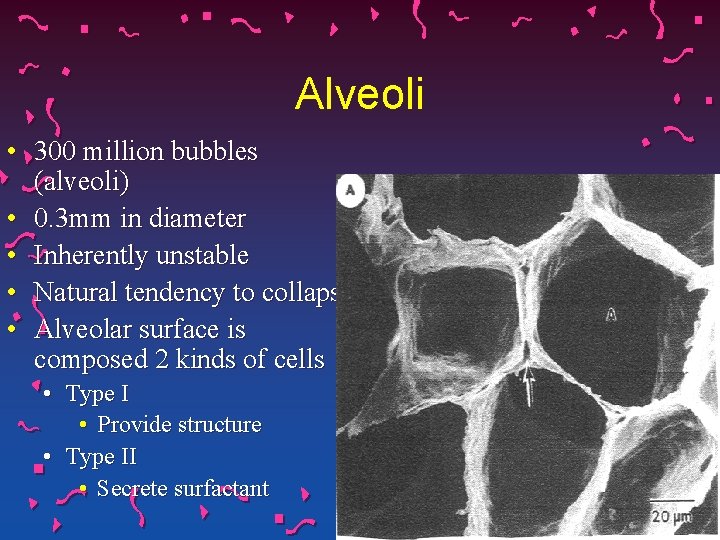
Alveoli • 300 million bubbles (alveoli) • 0. 3 mm in diameter • Inherently unstable • Natural tendency to collapse • Alveolar surface is composed 2 kinds of cells • Type I • Provide structure • Type II • Secrete surfactant
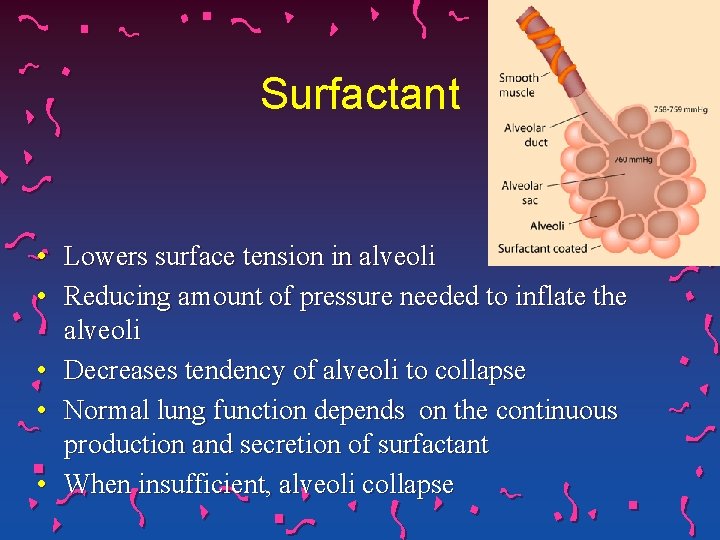
Surfactant • Lowers surface tension in alveoli • Reducing amount of pressure needed to inflate the alveoli • Decreases tendency of alveoli to collapse • Normal lung function depends on the continuous production and secretion of surfactant • When insufficient, alveoli collapse
Sighs • Normally, each person takes a slightly larger breath • After every five to six breaths • Stretches the alveoli • Causes surfactant to be secreted by type II cells

Atelectasis • Collapsed, airless alveoli Remember… • The postoperative patient is at risk for atelectasis • Pain • Tendency to resist taking deeper, sigh breaths
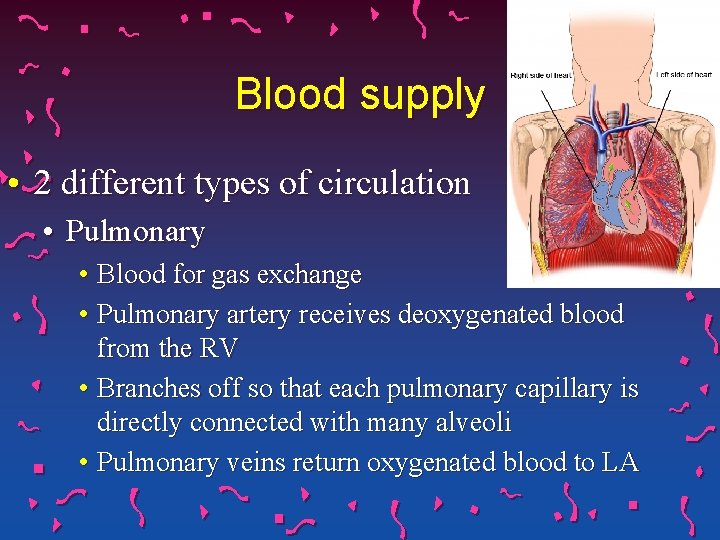
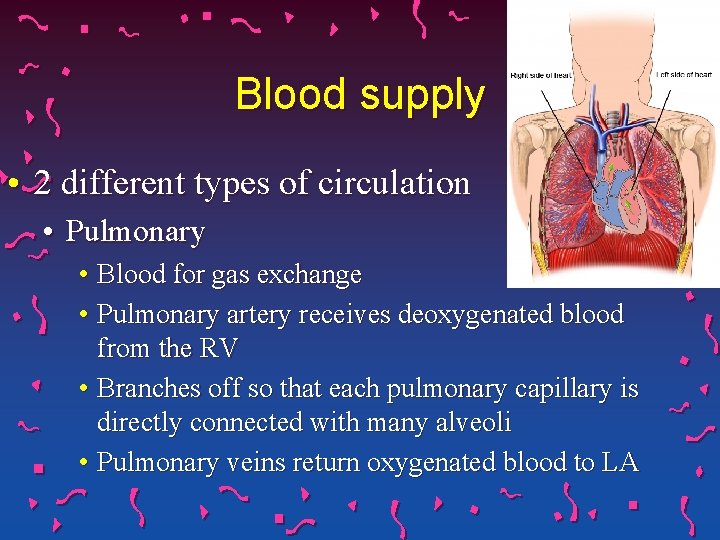
Blood supply • 2 different types of circulation • Pulmonary • Blood for gas exchange • Pulmonary artery receives deoxygenated blood from the RV • Branches off so that each pulmonary capillary is directly connected with many alveoli • Pulmonary veins return oxygenated blood to LA
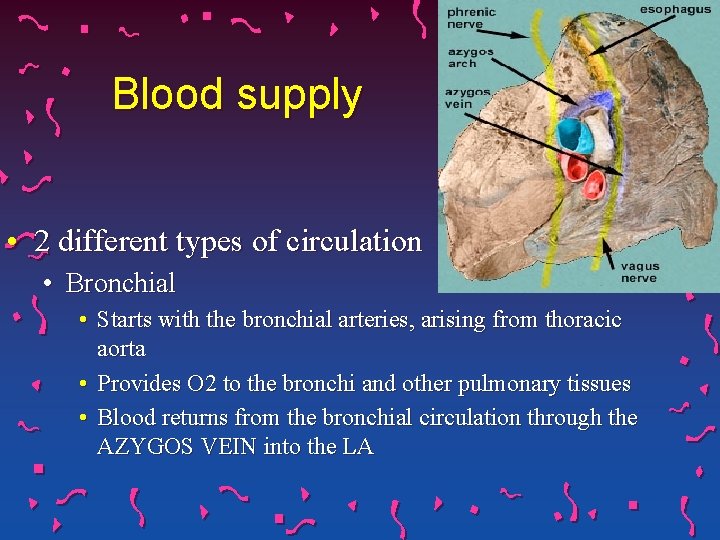
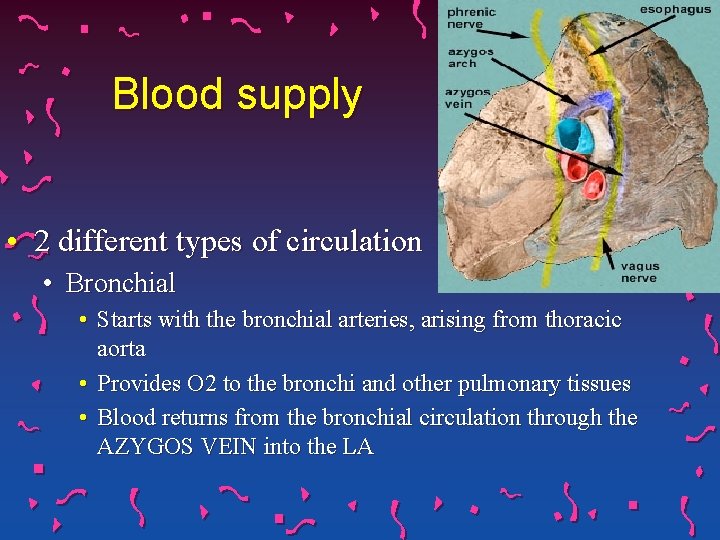
Blood supply • 2 different types of circulation • Bronchial • Starts with the bronchial arteries, arising from thoracic aorta • Provides O 2 to the bronchi and other pulmonary tissues • Blood returns from the bronchial circulation through the AZYGOS VEIN into the LA
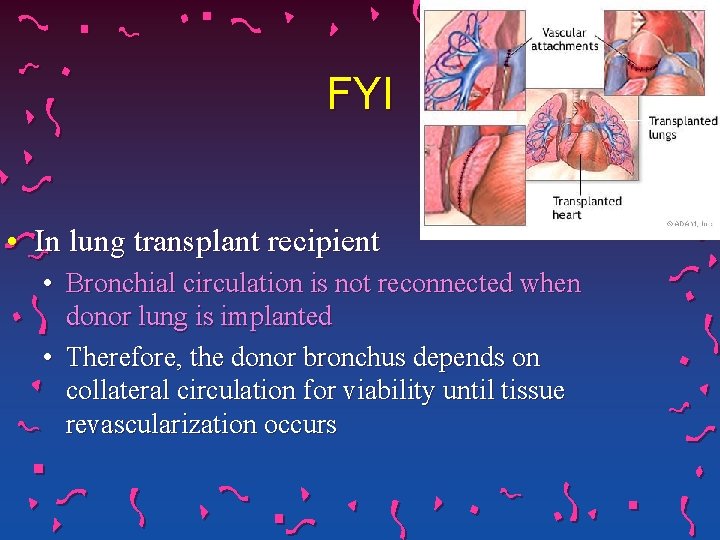
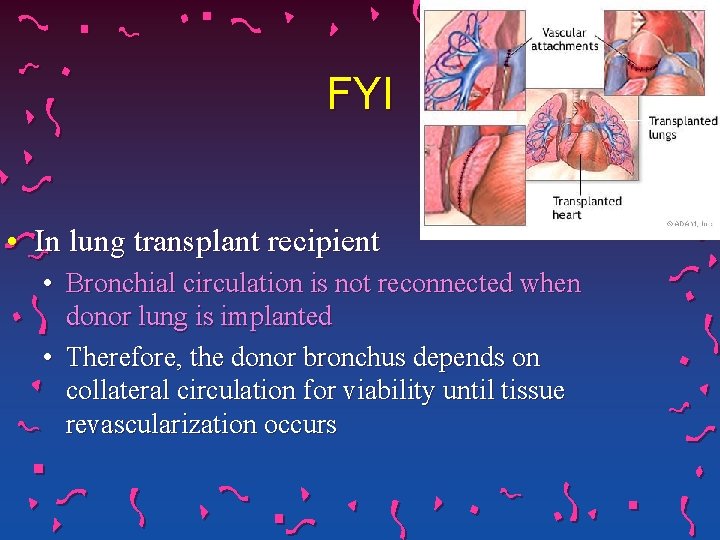
FYI • In lung transplant recipient • Bronchial circulation is not reconnected when donor lung is implanted • Therefore, the donor bronchus depends on collateral circulation for viability until tissue revascularization occurs
Diffusion • Gases moving back and forth across the alveolar capillary membrane • Higher concentration to lower concentration • Ability of lungs to oxygenate arterial blood adequately is determined by examination of the arterial oxygen tension (Pa. O 2) and arterial oxygen saturation (Sa. O 2)
Diffusion • Oxygen is carried in the blood in two forms • Dissolved oxygen in plasma (Pa. O 2) mm. Hg • Oxygen in chemical combination with hemoglobin (Sa. O 2) • Percentage – the amount of oxygen bound to hemoglobin in comparison (%) with the amount of oxygen the hemoglobin carry • (Example: if Sa. O 2 is 90%, then 90% of the hemoglobin attachments for oxygen have oxygen bound to them)

What is Partial Pressure. . . ? ? • Each gas has a pressure • That gas if alone, occupies a certain volume at a certain temperature. • The TOTAL partial pressure of a mixture of ideal gases • Vtot is the total volume in gas mixture • px is the partial pressure of gas X • ptot is the total pressure of gas mixture
Remember. . • Hypoxia • inadequate oxygen supply to the cells and tissues • High altitudes • Altitude sickness • Preterm birth • Anoxia • Complete deprivation • Hypoxemia • limited to low oxygen in the blood
Remember. . • Hypoxemic hypoxia • oxygen deficiency in which the arterial content of oxygen is low because the arterial partial pressure of oxygen is low • Hypoventilation • Heart shunts • V/Q mismatch (pulmonary embolism) • Low partial pressure of O 2 in the lungs when coming out of anesthesia
Remember. . • Anemic hypoxia • arterial partial pressure of oxygen is normal, but total oxygen content of the blood is reduced due to a decreased ability for hemoglobin to carry oxygen. • chronic anemia • carbon monoxide poisoning
Remember. . • Ischemic hypoxia • decreased blood flow • heart failure and vasodilatory shock. • Histotoxic hypoxia • quantity of oxygen reaching the cells is normal, but the cells are unable to use the oxygen effectively, due to disabled oxidative phosphorylation enzymes • Cyanide Toxicity
Signs and Symptoms • Gradual or sudden – depends • Gradual • H/A , fatigue, shortness of breath, a feeling of euphoria and nausea • Sudden /Rapid • • • changes in levels of consciousness Seizures Cyanosis Priapism Coma and death
Arterial Blood Gases • See Separate lecture!!
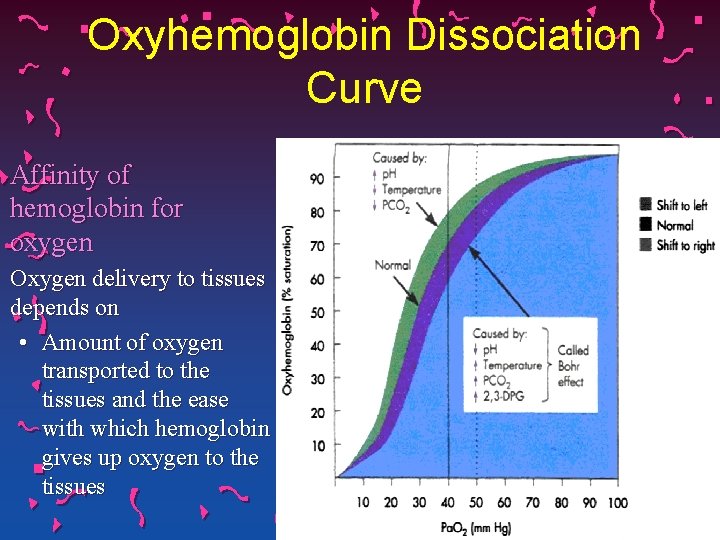
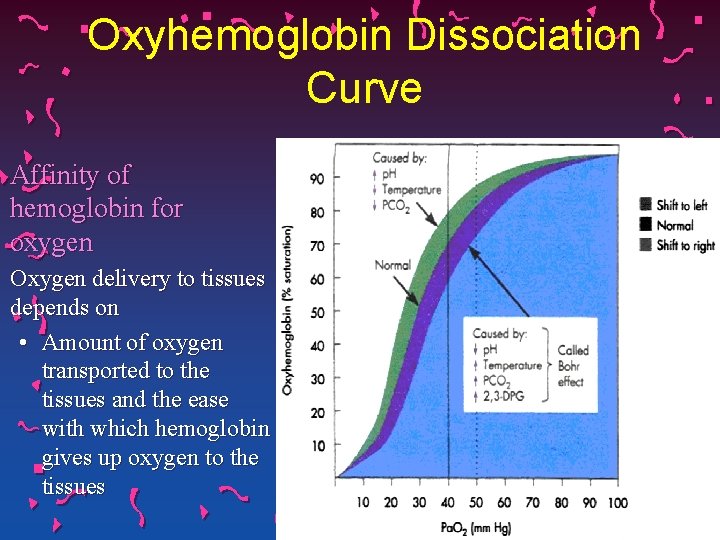
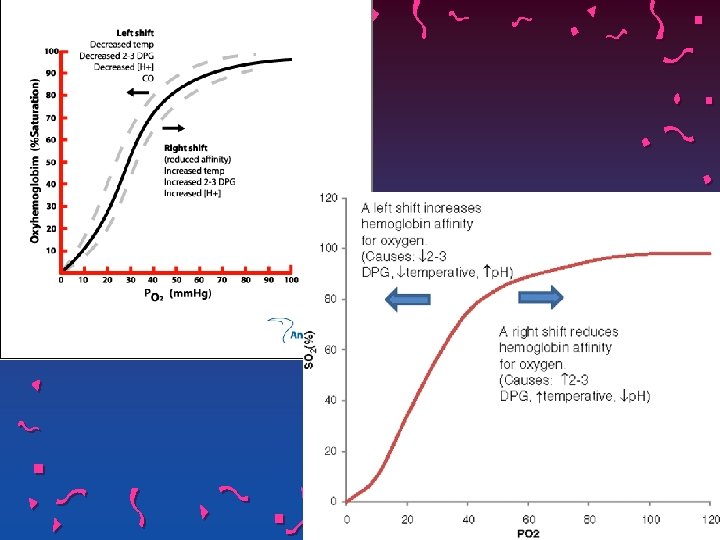
Oxyhemoglobin Dissociation Curve Affinity of hemoglobin for oxygen Oxygen delivery to tissues depends on • Amount of oxygen transported to the tissues and the ease with which hemoglobin gives up oxygen to the tissues
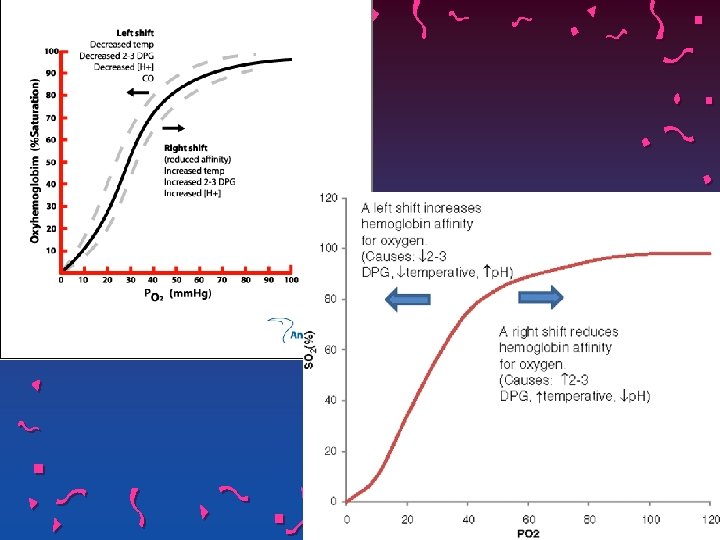
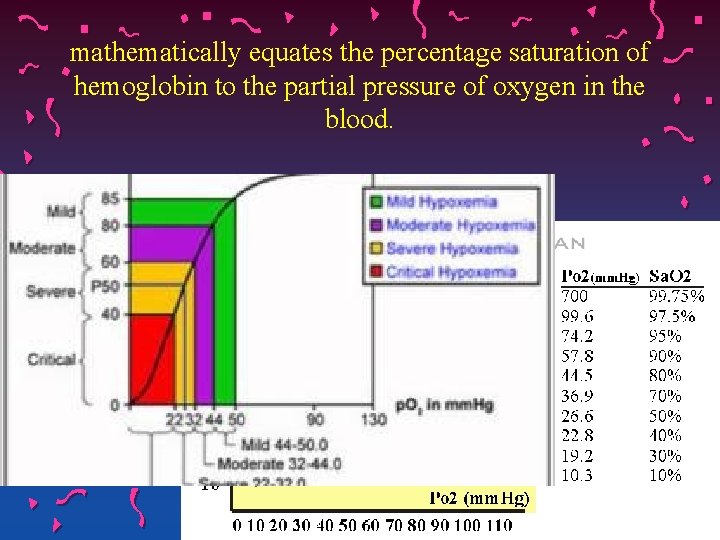
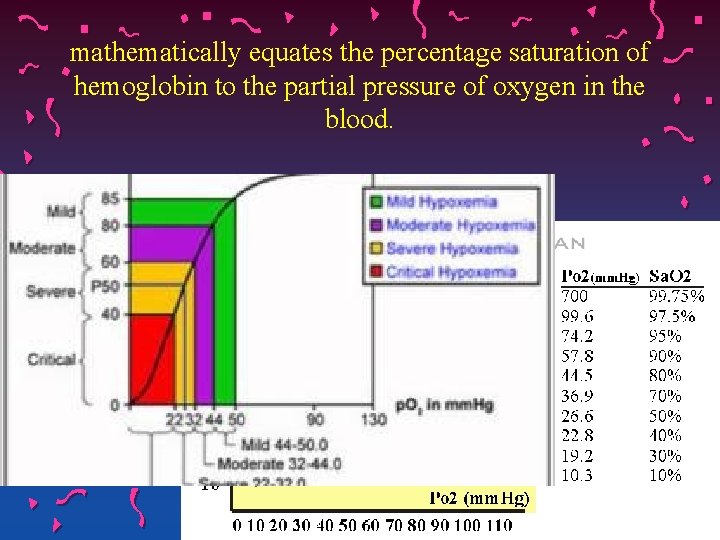
mathematically equates the percentage saturation of hemoglobin to the partial pressure of oxygen in the blood.
One simple rule is that hypoxemia becomes very serious • When decreased partial pressure of oxygen in blood is less than 60 mm Hg • At that point is the beginning of the steep portion of the hemoglobin dissociation curve, where a small decrease in the partial pressure of oxygen results in a large decrease in the oxygen content of the blood • or when hemoglobin oxygen saturation is less than 90%.
Mixed Venous Blood Gases • • Provides information about tissue oxygen demand Normal or near-normal cardiac status • Assessment of Pa. O 2 or Sa. O 2 is usually sufficient to determine adequate oxygenation • Not true for patient with impaired cardiac output or who is hemodynamically unstable • Calculating Pv. O 2 and Sv. O 2 to determine if tissues are receiving enough oxygen
Mixed Venous Blood Gases • PA Catheter • Consists of venous blood that has returned to the heart from all tissue beds and “mixed” in RV • When tissue oxygen delivery is inadequate or when inadequate oxygen is transported to the tissues by the hemoglobin, the Pv. O 2 and Sv. O 2 fall
Oximetry • Well-oxygenated blood absorbs light differently than deoxygenated blood • Oximeter determines the amount of light absorbed by the vascular bed and uses this information to calculate the saturation • Remember… • Oximeter will pick up any gas so as to be an unreliable tool for CO poisoning
Oxygen Delivery • Information from ABGs or pulse oximetry used to assess adequacy of oxygenation • Several questions must be asked to determine if oxygenation is adequate: #1 What is Sp. O 2 or Pa. O 2 compared with expected normal values #2 What is the degree of hypoxemia and what is the trend? #3 Has there been a rapid decline in Sp. O 2 or Pa. O 2
Oxygen Delivery Remember… A sudden drop in blood oxygen level can be life threatening, a gradual decline is tolerated with fewer symptoms • #5 Are there signs or symptoms of inadequate oxygenation? Remember… the brain is very sensitive to a decrease in tissue oxygen delivery, the very first evidence of hypoxemia may be apprehension, restlessness, or irritability
Oxygen Delivery • #6 What is the oxygenation status with activity or exercise? • Sp. O 2 levels during a standardized 6 minute walk distance test or with activities of daily living to assess for desaturation with activities • An Sp. O 2 of less than 88 during exertion indicates the need for supplemental oxygen
Control of Receptors • Cell clusters in the medulla on the brainstem is the respiratory center • Respond to chemical and mechanical signals from the body • Impulses are sent from medulla to respiratory muscles via spinal cord and phrenic nerves • Respiration is controlled by chemoreceptors and mechanical sensors
Control of Receptors • Chemoreceptors • Responds to change in chemical composition (Pa. CO 2 and p. H) of fluid around it • Central chemoreceptors in medulla respond to changes in H+ concentration • Decrease in H+ (alkalosis) causes medulla to decrease RR • Increase in H+ (acidosis) causes medulla to increase RR
Control of Receptors • Mechanical receptors • Located in lungs, upper airways, chest wall, and diaphragm • Stimulated by: • Irritants • Muscle stretching • Alveolar wall distortion • These receptors are stimulated by fluid entering the pulmonary interstitial space
Control of Receptors • As lungs inflate, pulmonary stretch receptors activate inspiratory center to inhibit further lung expansion • Prevents over-distention of lungs Impulses from mechanical sensors are sent through Vagus nerve to the brain Receptors are believed to cause rapid respiration seen in pulmonary edema
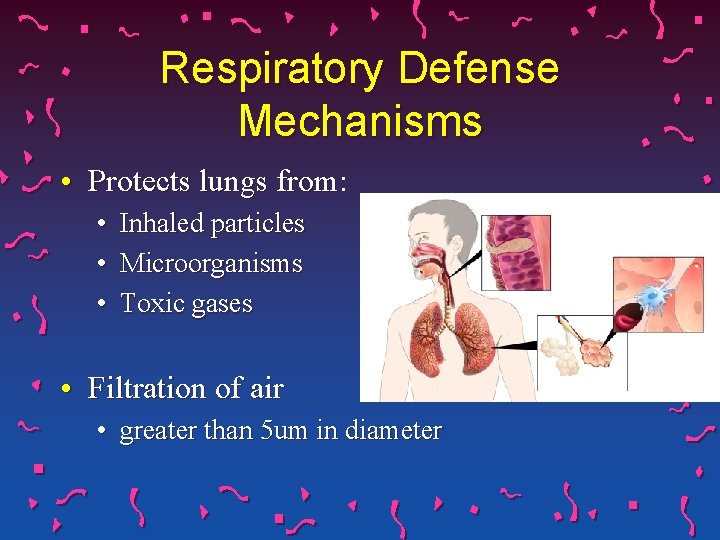
Respiratory Defense Mechanisms • Protects lungs from: • • • Inhaled particles Microorganisms Toxic gases • Filtration of air • greater than 5 um in diameter
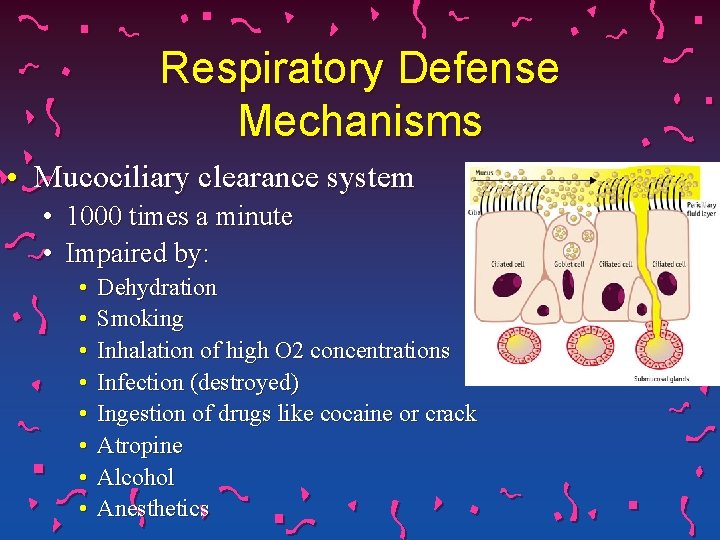
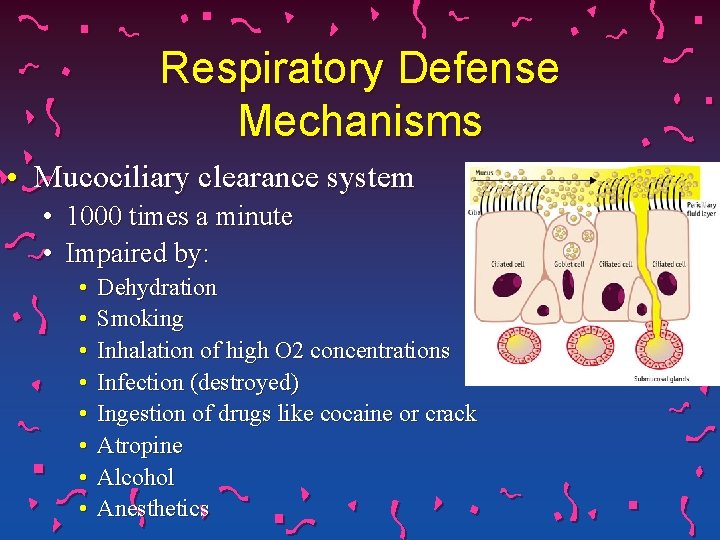
Respiratory Defense Mechanisms • Mucociliary clearance system • 1000 times a minute • Impaired by: • • Dehydration Smoking Inhalation of high O 2 concentrations Infection (destroyed) Ingestion of drugs like cocaine or crack Atropine Alcohol Anesthetics

Respiratory Defense Mechanisms • Cough reflex • Only effective in removing secretions above subsegmental level • Below it, mucociliary mechanism • Reflex bronchoconstriction • hypersensitivity
Respiratory Defense Mechanisms • Alveolar macrophages • Rapidly phagocytize inhaled foreign particles such as bacteria • Particles that cannot be adequately phagocytized tend to remain for indefinite time • Could stimulate the inflammatory or fibrogenic response • Impaired by inhaled tobacco products
Gerontologic Considerations • Structural alterations • • Decrease in elastic recoil of lung Decrease chest compliance AP diameter of thoracic cage increases Decrease in chest wall compliance Decrease number in functional alveoli Small airways in lung bases close earlier in expiration So. . More inspired air is distributed to lung apices and ventilation is less well matched to perfusion, causing a lowering of the Pa. O 2
Gerontologic Considerations • Defense Mechanisms • Less effective • Decline in cell-mediated immunity and formation of antibodies • Alveolar macrophages less effective at phagocytosis • Less forceful cough • Fewer and less functional cilia • Ig. A (neutralizing viruses) diminished • Respiratory controls altered
The END