REVASCULARIZATION OF IMMATURE PERMANENT TEETH WITH APICAL PERIODONTITIS




- Slides: 38
REVASCULARIZATION OF IMMATURE PERMANENT TEETH WITH APICAL PERIODONTITIS: NEW TREATMENT PROTOCOL? Banchs F. , Trope M. Journal of Endodontics 2004; 30, 196 -200.
Revascularization of necrotic tooth Avulsion of immature tooth Success rate of revascularization: 18 -41% (Ohman 1965, Kling et al. 1986, Cvek et al 1990, Andreason et al 1995) Depending on Stage of root development (Opening > 1. 1 mm) Duration of extraoral time (within 45 min) Storage medium Presence/absence of bacteria
Revascularization of necrotic infected tooth Possible or Impossible? ? IDEA Effectively disinfected the canal Effectively sealed the coronal access
Three-Mix Antibiotic (Hoshino et al. , Int Endod J. 1996) Metronidazole Minocycline Ciprofloxacine
Metronidazole is a prodrug. It is converted in anaerobic organisms by the redox enzyme pyruvate-ferredoxin oxidoreductase. The nitro group of metronidazole is chemically reduced by ferredoxin and the products are responsible for disrupting the DNA helical structure , thus inhibiting nucleic acid synthesis.
Minocycline a member of the broad spectrum tetracycline antibiotics (which inhibit bacterial protein synthesis), and has a broader spectrum than the other members. It is a bacteriostatic antibiotic. As a result of its long half-life it generally has serum levels 2 -4 times that of most other tetracyclines.
Ciprofloxacin Belonging to a group called fluoroquinolones. Ciprofloxacin is bactericidal. Its mode of action depends upon blocking bacterial DNA replication by binding itself to an enzyme called DNA gyrase, thereby inhibiting the unwinding of bacterial chromosomal DNA during and after the replication.
Case Report An 11 -year-old boy of Japanese descent was referred to the endodontic clinic of the University of North Carolina by the pediatric dentistry department for evaluation on the lower right second premolar. Hx: The child had a lingual swelling of the right mandibular area 1 month previously with reported slight discomfort.
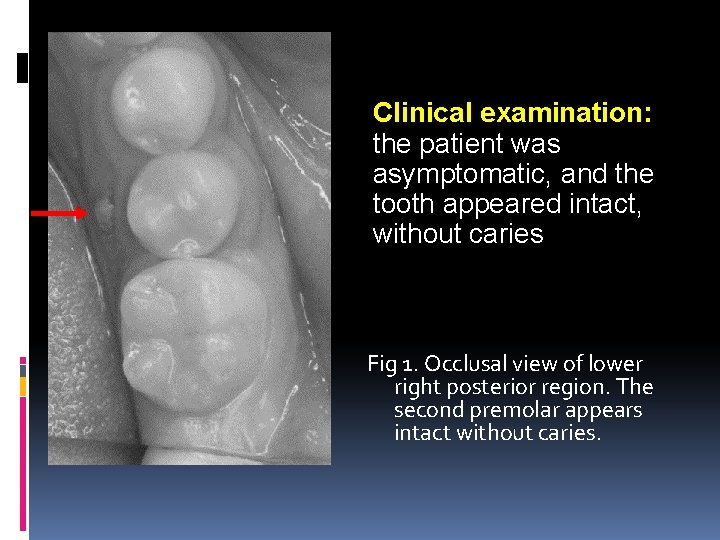
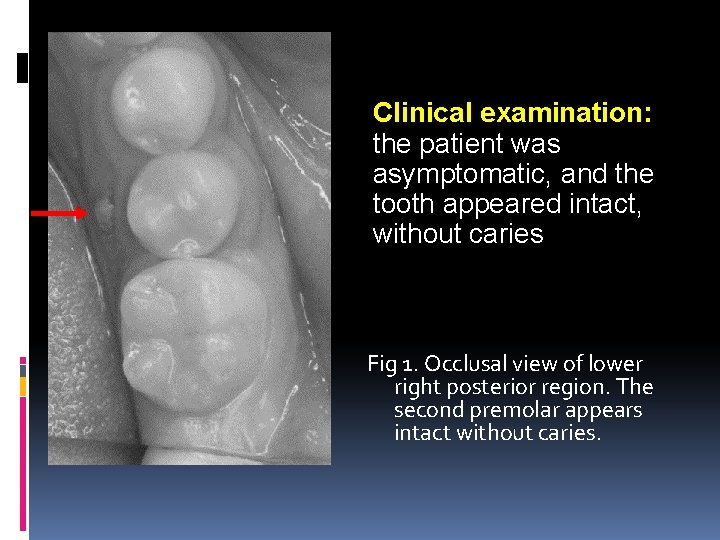
Clinical examination: the patient was asymptomatic, and the tooth appeared intact, without caries Fig 1. Occlusal view of lower right posterior region. The second premolar appears intact without caries.
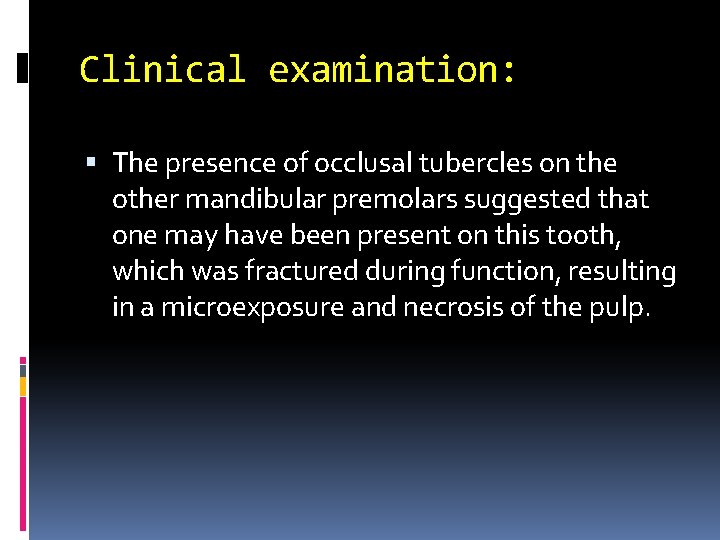
Clinical examination: The presence of occlusal tubercles on the other mandibular premolars suggested that one may have been present on this tooth, which was fractured during function, resulting in a microexposure and necrosis of the pulp.
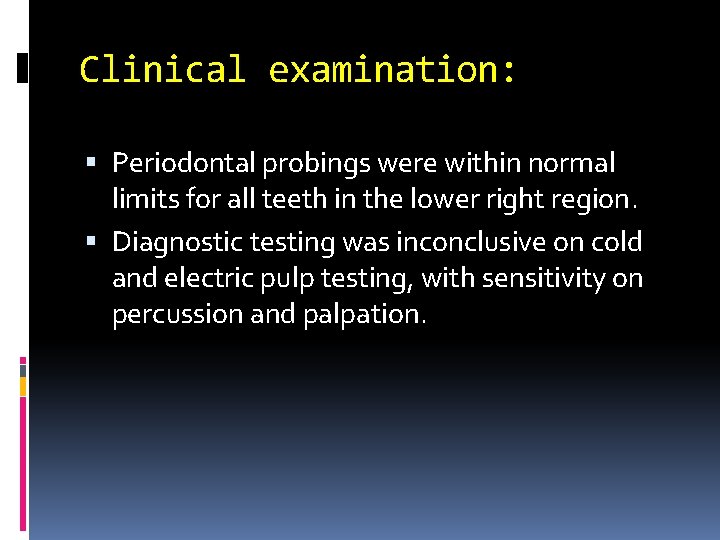
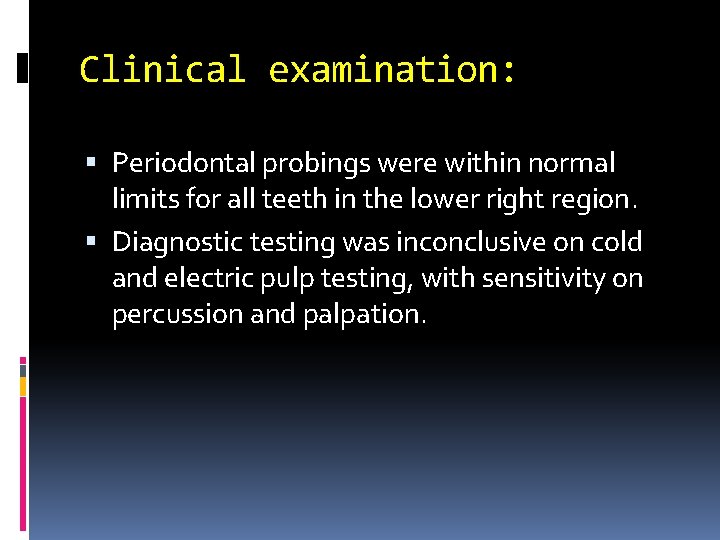
Clinical examination: Periodontal probings were within normal limits for all teeth in the lower right region. Diagnostic testing was inconclusive on cold and electric pulp testing, with sensitivity on percussion and palpation.
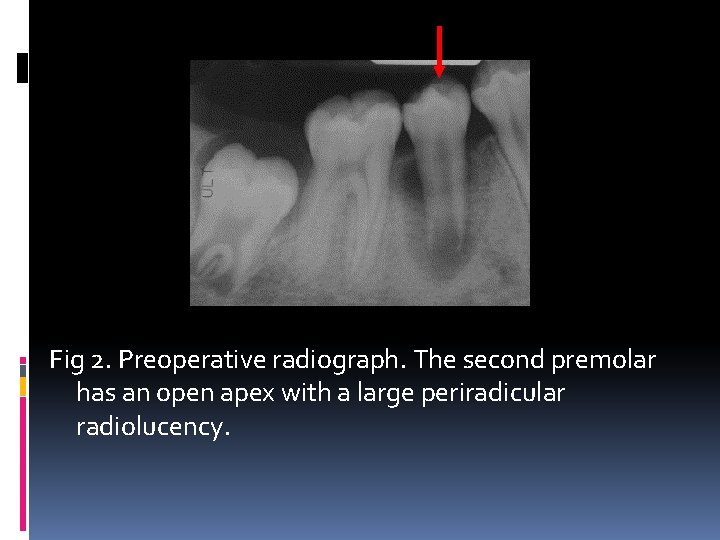
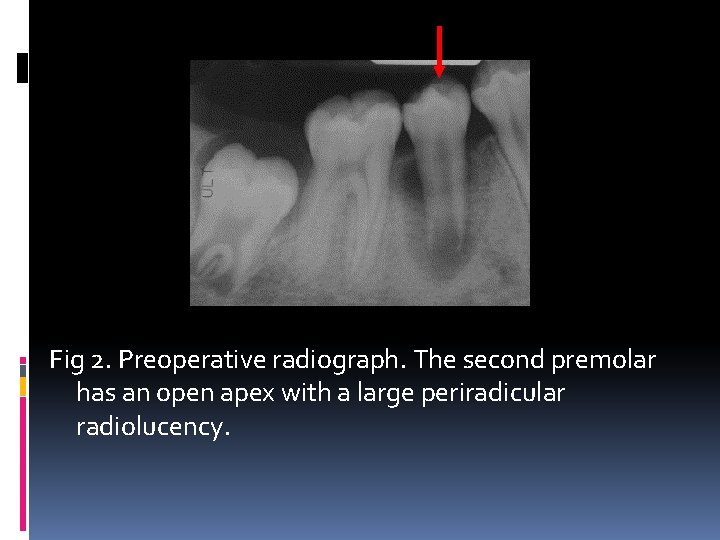
Fig 2. Preoperative radiograph. The second premolar has an open apex with a large periradicular radiolucency.
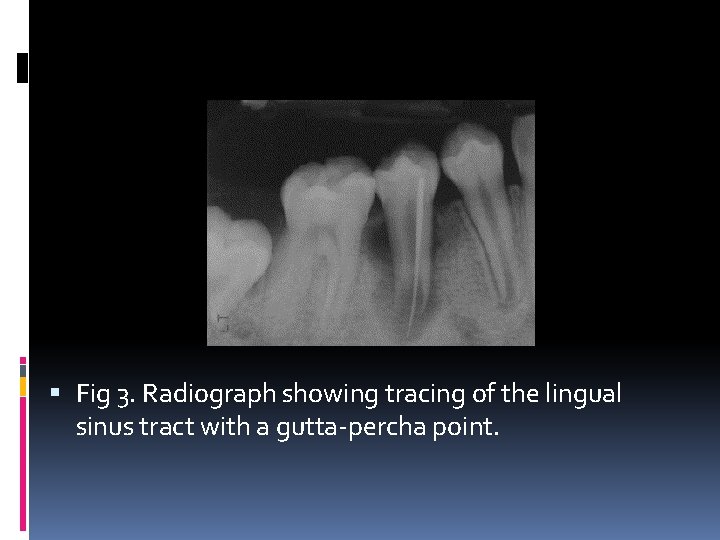
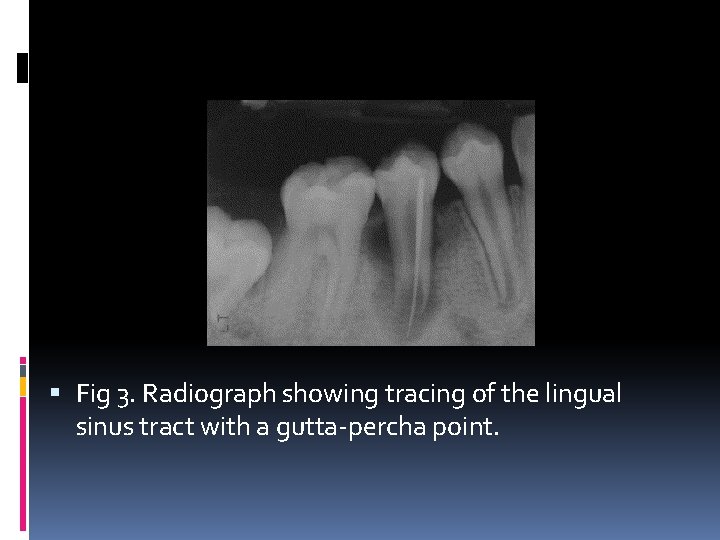
Fig 3. Radiograph showing tracing of the lingual sinus tract with a gutta-percha point.
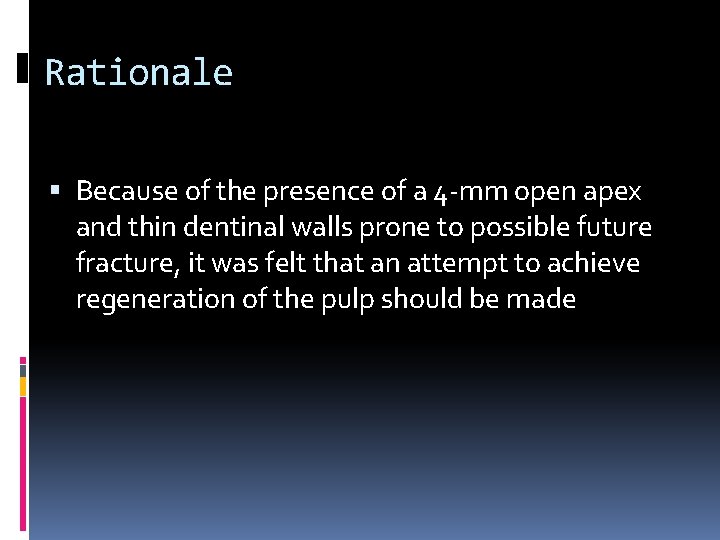
Rationale Because of the presence of a 4 -mm open apex and thin dentinal walls prone to possible future fracture, it was felt that an attempt to achieve regeneration of the pulp should be made
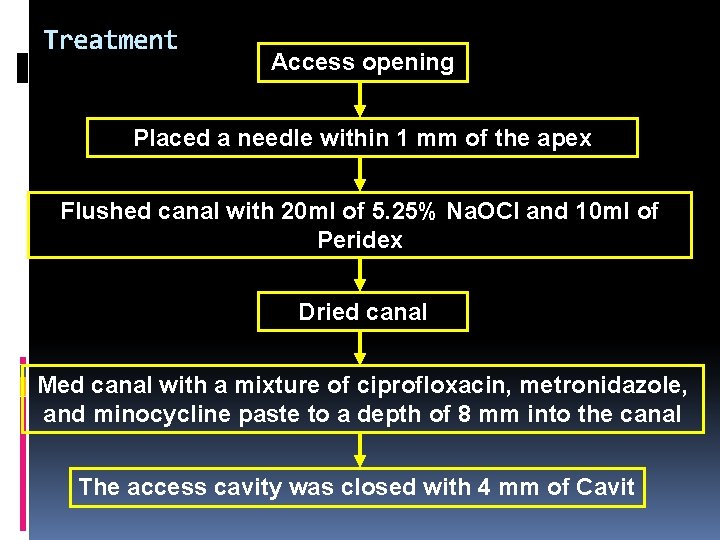
Treatment Access opening Placed a needle within 1 mm of the apex Flushed canal with 20 ml of 5. 25% Na. OCl and 10 ml of Peridex Dried canal Med canal with a mixture of ciprofloxacin, metronidazole, and minocycline paste to a depth of 8 mm into the canal The access cavity was closed with 4 mm of Cavit
26 DAYS LATER……
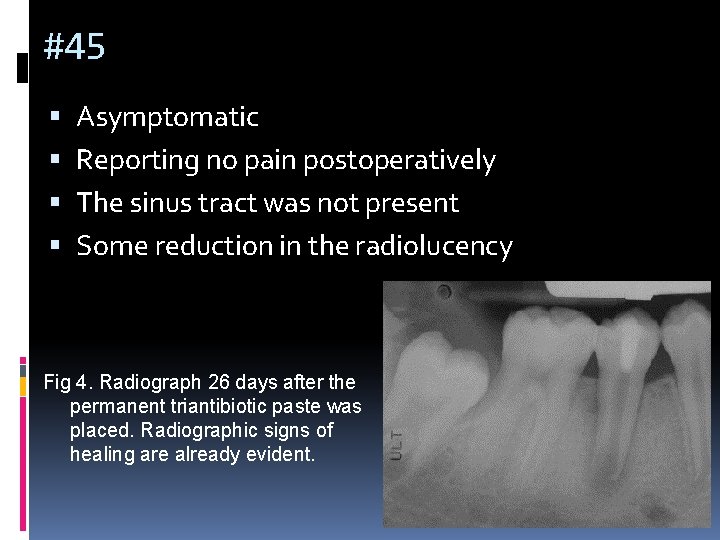
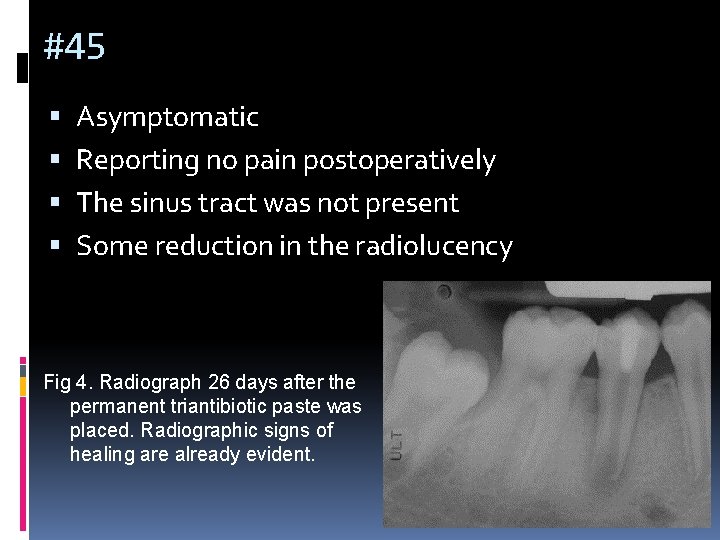
#45 Asymptomatic Reporting no pain postoperatively The sinus tract was not present Some reduction in the radiolucency Fig 4. Radiograph 26 days after the permanent triantibiotic paste was placed. Radiographic signs of healing are already evident.
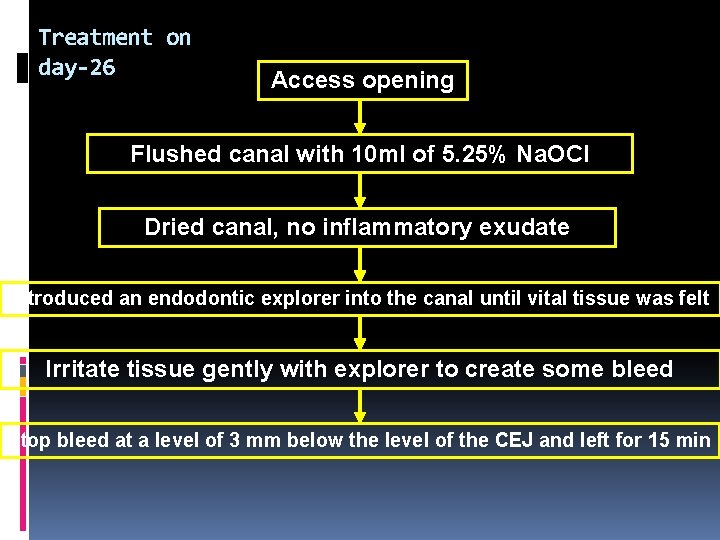
Treatment on day-26 Access opening Flushed canal with 10 ml of 5. 25% Na. OCl Dried canal, no inflammatory exudate Introduced an endodontic explorer into the canal until vital tissue was felt Irritate tissue gently with explorer to create some bleed Stop bleed at a level of 3 mm below the level of the CEJ and left for 15 min
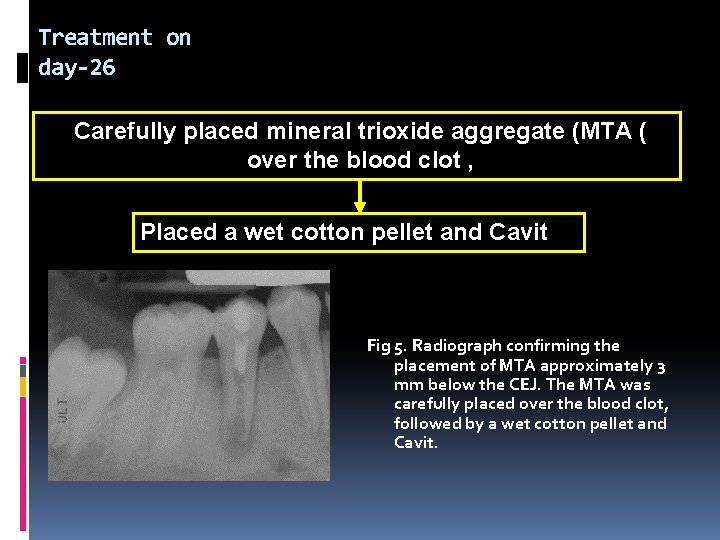
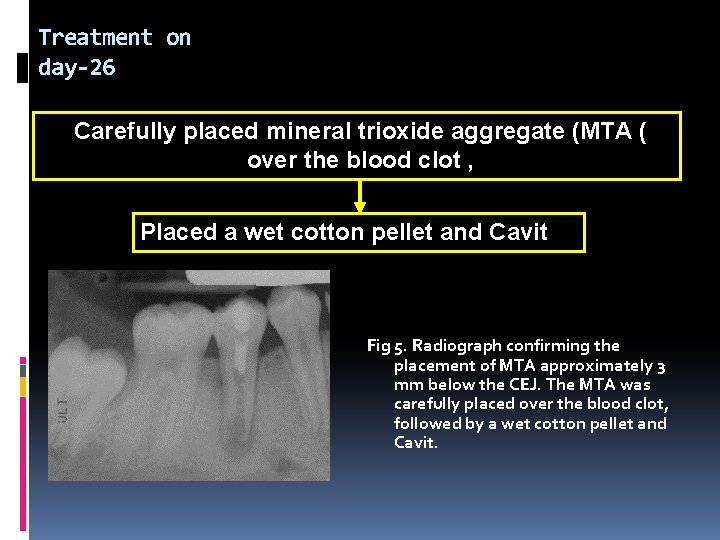
Treatment on day-26 Carefully placed mineral trioxide aggregate (MTA ( over the blood clot , Placed a wet cotton pellet and Cavit Fig 5. Radiograph confirming the placement of MTA approximately 3 mm below the CEJ. The MTA was carefully placed over the blood clot, followed by a wet cotton pellet and Cavit.
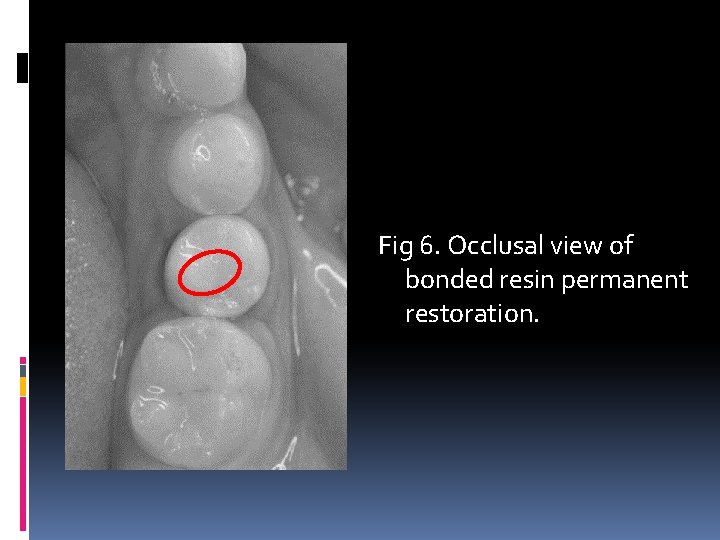
2 Weeks later…… #45 asymptomatic Replaced cavit and cotton pellet with a bonded resin restoration The patient was scheduled for recall examination and advised to call if he was in pain or if swelling or a recurrence of the sinus tract developed.
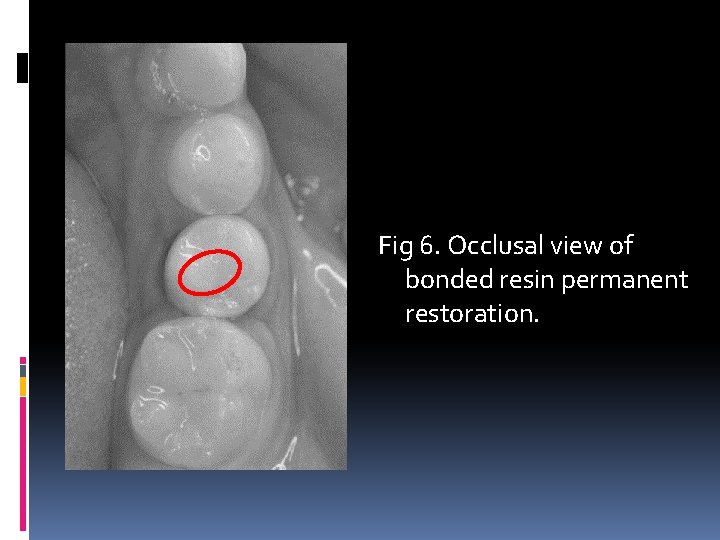
Fig 6. Occlusal view of bonded resin permanent restoration.

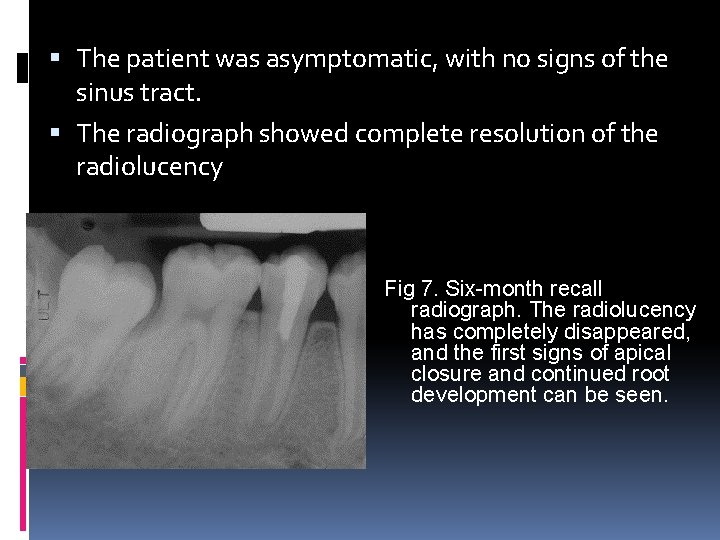
6 -MONTH RECALL
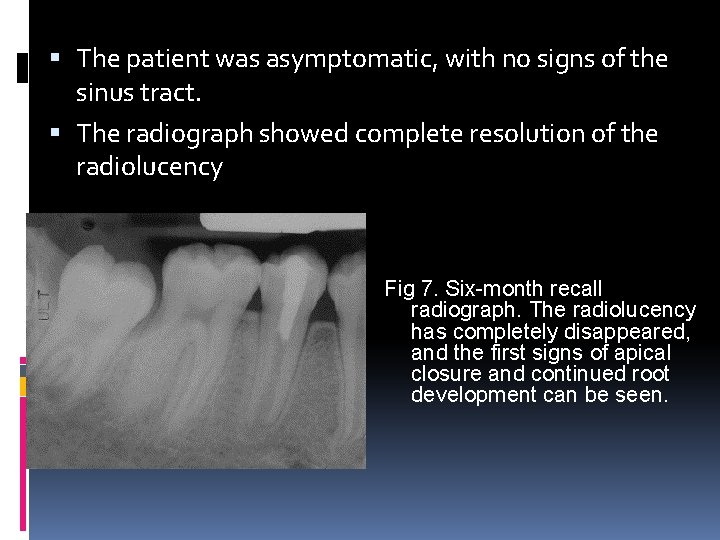
The patient was asymptomatic, with no signs of the sinus tract. The radiograph showed complete resolution of the radiolucency Fig 7. Six-month recall radiograph. The radiolucency has completely disappeared, and the first signs of apical closure and continued root development can be seen.
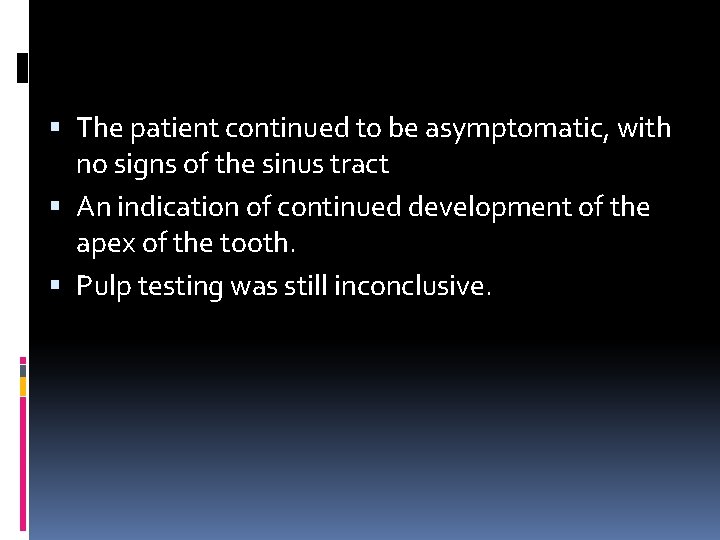
1 -YEAR AND 18 -MONTH RECALL
The patient continued to be asymptomatic, with no signs of the sinus tract An indication of continued development of the apex of the tooth. Pulp testing was still inconclusive.

Fig 8. Twelve-month radiograph showing continued root development Fig 9. Eighteen-month radiograph showing continued root development.
2 -YEAR RECALL
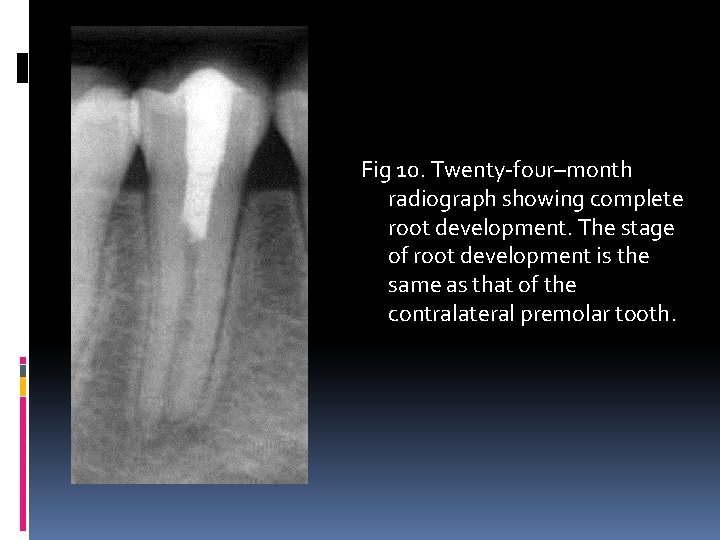
The patient continued to be asymptomatic, Closure of the apex and thickening of the dentinal walls was obvious. The tooth responded positively to the cold test.
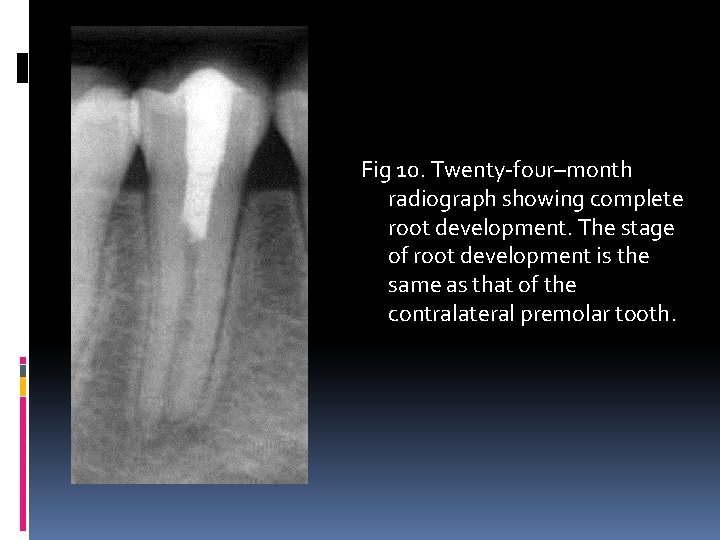
Fig 10. Twenty-four–month radiograph showing complete root development. The stage of root development is the same as that of the contralateral premolar tooth.

Before 2 years later
Discussion MI, cannot be performed in this case because the walls are so thin. Disinfection relies solely on irrigants and intracanal medication.
Ca(OH)2 necrose tissue in immediate contact Destroy tissues with the potential to differentiate into new pulp The canal walls will not be thickened or strengthened In fact, it will weaken the tooth (Andreasen et al. , 2002)
MTA If place MTA in the apical third of the immature tooth also not allow new tissue to grow into the root canal The root remain thin and weak
Blood Clot Acts as a matrix for the growth of new tissue in to the pulp space Similar to the necrotic pulp in a traumatized tooth
Is it really a pulp tissue? ? Root continued to grow Wall of the root appeared to thicken in a conventional manner
Origin of the tissue Some pulp tissue and Hertwig’s epithelial root sheath may have survived apically After disinfection and recovering of inflammation, these survived tissue can proliferate
Further studies Long-term outcome of the procedure Predictability of the procedure The type of tissue the develops in these cases

HAPPY ENDING