RETIREE HEALTH BENEFIT PLAN OPTIONS Yosemite Community College
RETIREE HEALTH BENEFIT PLAN OPTIONS Yosemite Community College District November 15, 2016 Presented by: Lola Nickell & Bobbie Wellwood – SISC
2 Items for Discussion Section I: What’s Available? Section II: Overview of Plan Options • Brief summary of each plan, refer to Plan Benefit Summary for details Section III: Review of Plans & Differences Section IV: SISC Retiree Direct Bill Program Section V: Retirees Turning 65 – Medicare Enrollment Timing & Process Section VI: Review
3 Section I: What’s Available? There are three types of plans available through YCCD: 1. Blue Shield PPO - Medicare Coordination of Benefits (COB) Plans • Most expensive: Single $506 to $538 (varies by plan) 2. Kaiser Permanente Senior Advantage (KPSA) Plan (HMO) • Less expensive than PPO: Single $329 • May enroll mid year. Contact Benefits Department at least 60 days in advance. 3. Companion Care Medicare Supplement Plan • Less expensive than PPO: Single $419 • May enroll mid year. Contact Benefits Department at least 60 days in advance.
4 Section II: Overview of Plan Options Blue Shield PPO - Medicare Coordination of Benefits Plans Enrollment in Medicare Part A & B is required to avoid expensive premium surcharges for missing Medicare. • Member retains original Medicare A & B • Member may access medical services with any U. S. provider who accepts Medicare assignment. To maximize Plan benefits and minimize potential out of pocket cost, use providers in the Blue Shield PPO network. • Members enrolled on the Blue Shield PPO plan are not enrolled in Medicare Part D drug coverage. The Prescription Drug Plan, administered by Navitus Health Solutions, mirrors the Active Employee benefit. • 2016 -17 Monthly Single Rates: $506 to $538 (varies by plan)
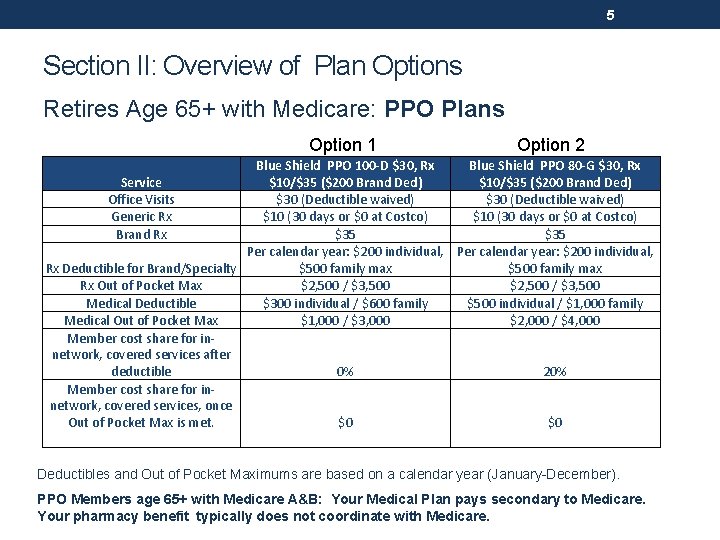
5 Section II: Overview of Plan Options Retires Age 65+ with Medicare: PPO Plans Option 1 Option 2 Blue Shield PPO 100 -D $30, Rx Blue Shield PPO 80 -G $30, Rx Service $10/$35 ($200 Brand Ded) Office Visits $30 (Deductible waived) Generic Rx $10 (30 days or $0 at Costco) Brand Rx $35 Per calendar year: $200 individual, Rx Deductible for Brand/Specialty $500 family max Rx Out of Pocket Max $2, 500 / $3, 500 Medical Deductible $300 individual / $600 family $500 individual / $1, 000 family Medical Out of Pocket Max $1, 000 / $3, 000 $2, 000 / $4, 000 Member cost share for innetwork, covered services after 0% 20% deductible Member cost share for innetwork, covered services, once Out of Pocket Max is met. $0 $0 Deductibles and Out of Pocket Maximums are based on a calendar year (January-December). PPO Members age 65+ with Medicare A&B: Your Medical Plan pays secondary to Medicare. Your pharmacy benefit typically does not coordinate with Medicare.

6 Section II: Overview of Plan Options Retires Age 65+ with Medicare: PPO Plans (Continued) Option 3 Blue Shield PPO 80 -C $20, Rx Service $10/$35 ($200 Brand Ded) Office Visits $20 (Deductible waived) Generic Rx $10 (30 days or $0 at Costco) Brand Rx $35 Per calendar year: $200 individual, Rx Deductible for Brand/Specialty $500 family max Rx Out of Pocket Max $2, 500 / $3, 500 Medical Deductible $200 individual / $500 family Medical Out of Pocket Max $1, 000 / $3, 000 Member cost share for innetwork, covered services after 20% deductible Member cost share for innetwork, covered services, once Out of Pocket Max is met. $0 Option 4 Blue Shield PPO 90 -G $30, Rx $9/$35 $30 (Deductible waived) $9 (30 days or $0 at Costco) $35 None $2, 500 / $3, 500 $500 individual / $1, 000 family $1, 000 / $3, 000 10% $0 Deductibles and Out of Pocket Maximums are based on a calendar year (January-December). PPO Members age 65+ with Medicare A&B: Your Medical Plan pays secondary to Medicare. Your pharmacy benefit typically does not coordinate with Medicare.
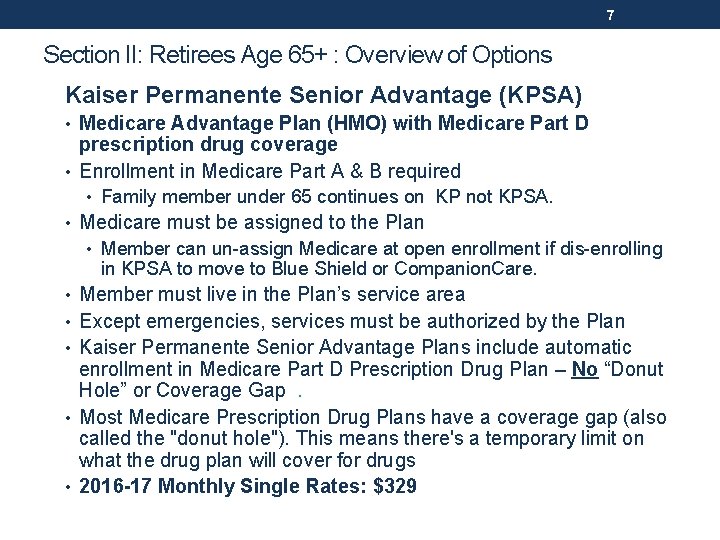
7 Section II: Retirees Age 65+ : Overview of Options Kaiser Permanente Senior Advantage (KPSA) • Medicare Advantage Plan (HMO) with Medicare Part D prescription drug coverage • Enrollment in Medicare Part A & B required • Family member under 65 continues on KP not KPSA. • Medicare must be assigned to the Plan • Member can un-assign Medicare at open enrollment if dis-enrolling in KPSA to move to Blue Shield or Companion. Care. • Member must live in the Plan’s service area • Except emergencies, services must be authorized by the Plan • Kaiser Permanente Senior Advantage Plans include automatic enrollment in Medicare Part D Prescription Drug Plan – No “Donut Hole” or Coverage Gap . • Most Medicare Prescription Drug Plans have a coverage gap (also called the "donut hole"). This means there's a temporary limit on what the drug plan will cover for drugs • 2016 -17 Monthly Single Rates: $329

8 Section II Benefit Overview: Kaiser Permanente Senior Advantage Plans – Retirees age 65+ with Medicare A&B SERVICES KAISER PERMANENTE SENIOR ADVANTAGE $10 OV, $10 -20 RX Ambulance (Ground or Air) $50/Trip Annual Physical Examination and Medicare approved No charge immunizations Acupuncture/Chiropractic $10 co-pay 30 combined visits DME - Durable Medical Equipment 100% (Kaiser DME formulary guidelines apply) Hospitalization Inpatient $0 admission Emergency Room $50 co-pay/waived if admitted Laboratory Services No charge $10 co-pay per individual visit; Mental Health - Outpatient unlimited visits $5 co-pay per group visit Physician Services/Basic Health Services Office visits $10 co-pay per visit Consultation, diagnosis & treatment by a specialist $10 co-pay per visit Prescription Drugs Generic: $10 co-pay a 100 day supply Using Kaiser pharmacies. Not subject to donut hole. Brand: $20 co-pay for a 100 day supply Vision Care Examination for eyeglasses $10 co-pay per visit Glaucoma testing $10 co-pay per visit Standard frame/lenses every 24 months $150 frame and lens allowance every 24 months Retiree plans with Medicare A&B Retirees must live in an approved zip code of the Kaiser Permanente California Service Area and Centers for Medicare and Medicaid (CMS)

9 Kaiser Permanente Senior Advantage • New Feature: Silver & Fit Exercise and Healthy Aging Program • Available only to KPSA members • Benefits include: • Gym Membership at participating clubs • Home Fitness Program • Healthy Aging Resource Library To learn more about Silver & Fit, including how to register and fitness facilities near you, visit Silverand. Fit. com.
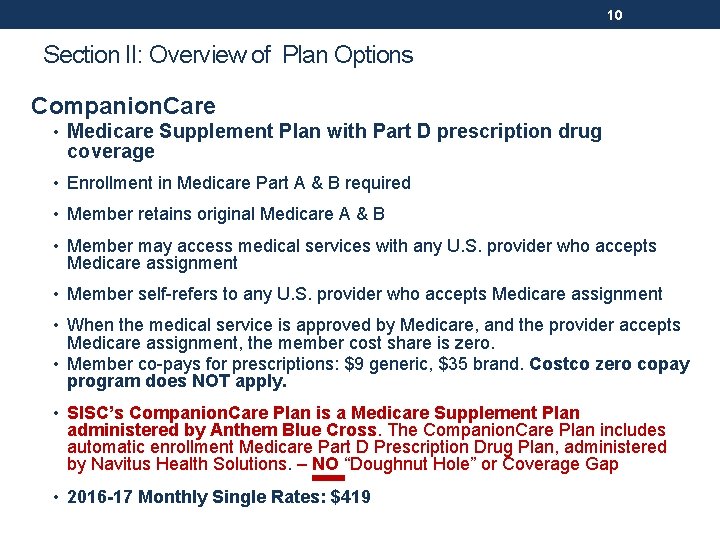
10 Section II: Overview of Plan Options Companion. Care • Medicare Supplement Plan with Part D prescription drug coverage • Enrollment in Medicare Part A & B required • Member retains original Medicare A & B • Member may access medical services with any U. S. provider who accepts Medicare assignment • Member self-refers to any U. S. provider who accepts Medicare assignment • When the medical service is approved by Medicare, and the provider accepts Medicare assignment, the member cost share is zero. • Member co-pays for prescriptions: $9 generic, $35 brand. Costco zero copay program does NOT apply. • SISC’s Companion. Care Plan is a Medicare Supplement Plan administered by Anthem Blue Cross. The Companion. Care Plan includes automatic enrollment Medicare Part D Prescription Drug Plan, administered by Navitus Health Solutions. – NO “Doughnut Hole” or Coverage Gap • 2016 -17 Monthly Single Rates: $419
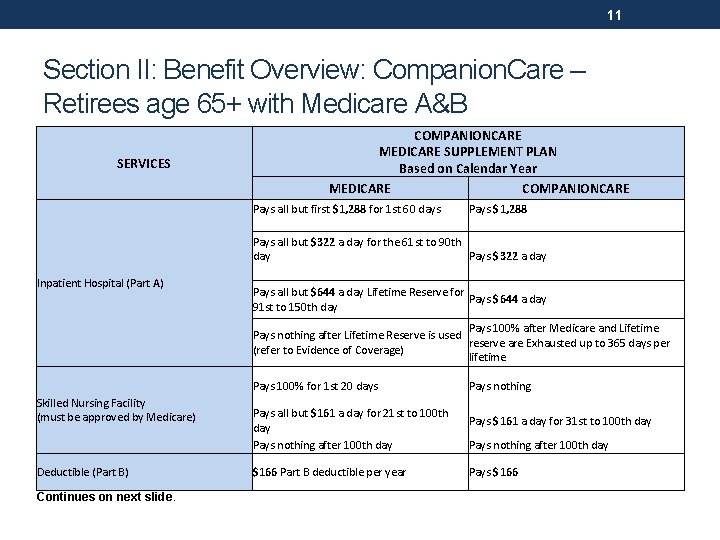
11 Section II: Benefit Overview: Companion. Care – Retirees age 65+ with Medicare A&B SERVICES COMPANIONCARE MEDICARE SUPPLEMENT PLAN Based on Calendar Year MEDICARE COMPANIONCARE Pays all but first $1, 288 for 1 st 60 days Pays $1, 288 Pays all but $322 a day for the 61 st to 90 th Pays $322 a day Inpatient Hospital (Part A) Pays all but $644 a day Lifetime Reserve for Pays $644 a day 91 st to 150 th day Pays 100% after Medicare and Lifetime Pays nothing after Lifetime Reserve is used reserve are Exhausted up to 365 days per (refer to Evidence of Coverage) lifetime Pays 100% for 1 st 20 days Skilled Nursing Facility (must be approved by Medicare) Deductible (Part B) Continues on next slide. Pays all but $161 a day for 21 st to 100 th day Pays nothing after 100 th day $166 Part B deductible per year Pays nothing Pays $161 a day for 31 st to 100 th day Pays nothing after 100 th day Pays $166
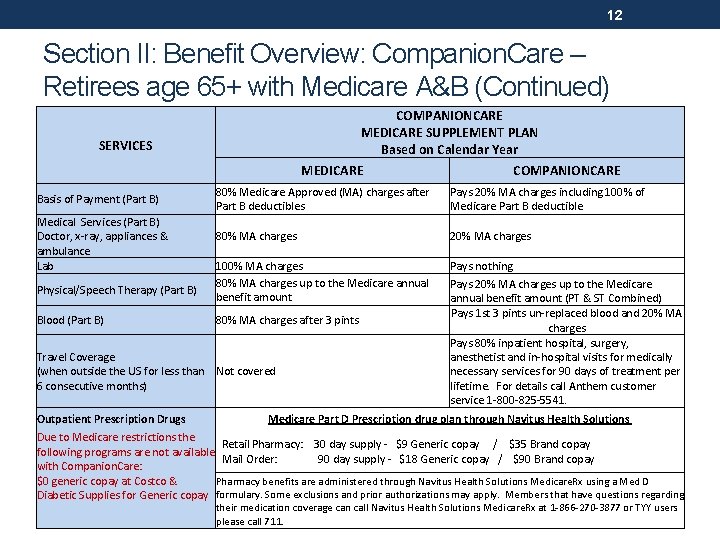
12 Section II: Benefit Overview: Companion. Care – Retirees age 65+ with Medicare A&B (Continued) COMPANIONCARE MEDICARE SUPPLEMENT PLAN Based on Calendar Year SERVICES MEDICARE Basis of Payment (Part B) Medical Services (Part B) Doctor, x-ray, appliances & ambulance Lab Physical/Speech Therapy (Part B) Blood (Part B) 80% Medicare Approved (MA) charges after Part B deductibles Pays 20% MA charges including 100% of Medicare Part B deductible 80% MA charges 20% MA charges 100% MA charges 80% MA charges up to the Medicare annual benefit amount Pays nothing Pays 20% MA charges up to the Medicare annual benefit amount (PT & ST Combined) Pays 1 st 3 pints un-replaced blood and 20% MA charges Pays 80% inpatient hospital, surgery, anesthetist and in-hospital visits for medically necessary services for 90 days of treatment per lifetime. For details call Anthem customer service 1 -800 -825 -5541. 80% MA charges after 3 pints Travel Coverage (when outside the US for less than Not covered 6 consecutive months) Outpatient Prescription Drugs COMPANIONCARE Medicare Part D Prescription drug plan through Navitus Health Solutions Due to Medicare restrictions the Retail Pharmacy: 30 day supply - $9 Generic copay / $35 Brand copay following programs are not available Mail Order: 90 day supply - $18 Generic copay / $90 Brand copay with Companion. Care: $0 generic copay at Costco & Pharmacy benefits are administered through Navitus Health Solutions Medicare. Rx using a Med D Diabetic Supplies for Generic copay formulary. Some exclusions and prior authorizations may apply. Members that have questions regarding their medication coverage can call Navitus Health Solutions Medicare. Rx at 1 -866 -270 -3877 or TYY users please call 711.

13 Section III : Review of Plan Types & Differences Important Details Providers Must live in plan service area Must receive non-emergency services in service area Medicare A & B required for enrollment Medicare assigned to Plan Retain Original Medicare Auto-Enrollment in Medicare Part D Prescription Drug Plan May enroll outside of annual open enrollment per SISC process (minimum 60 days in advance) Kaiser Permanente Senior Advantage (KPSA) Companion. Care Medicare Supplement KPSA U. S. Providers who Accept Medicare Assignment No (U. S. only) Yes No (U. S. only) Not mandatory, but expensive surcharges will apply No Yes No (U. S. only) Yes No, Assigned to Plan Yes No Yes Blue Shield PPO COB U. S. Providers who Accept Medicare Assignment; Use Blue Shield PPO providers to maximize benefits and minimize potential member cost share
14 Section IV: Retiree Direct Billing Program Overview • Self-pay retirees are billed directly by SISC • SISC has a team dedicated to managing monthly billing for District retiree medical plans. • The SISC team can assist you with all questions about: • Direct Bill Program billing and premium payment • Enrollment in SISC Direct Bill Plan Options • Your medical plan benefits will be administered entirely by the SISC Office. All communication regarding benefits and payments will be coming from and directed to the SISC office. • Upon receipt of your enrollment, SISC will send you a Welcome Letter with an explanation of the payment process.
Section IV : Retiree Program Overview, Continued • You will receive a monthly statement from SISC at the beginning of each month. The payment is for that coverage month and is due to SISC by the 20 th. US Mail: SISC III Health Benefits • SISC can accept advance payments for multiple months. Advance payments will be reflected on the monthly statement. • You may pay by check or an automatic PO Box 1591 electronic funds transfer. Bakersfield, CA 93302 -1591 15
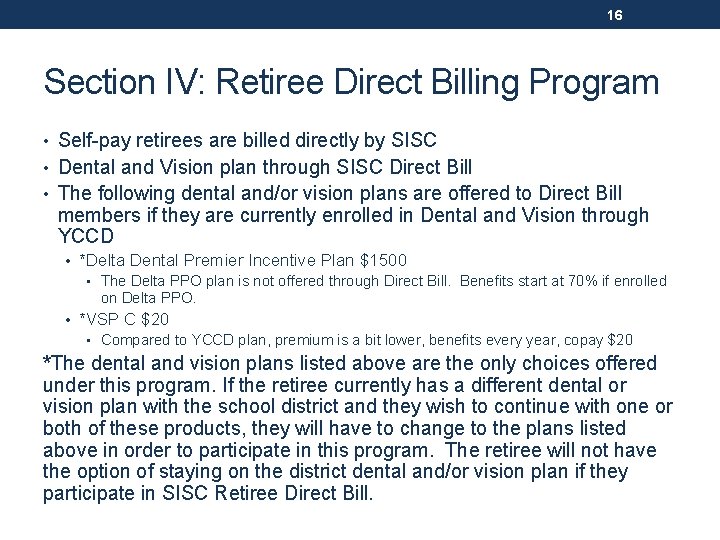
16 Section IV: Retiree Direct Billing Program • Self-pay retirees are billed directly by SISC • Dental and Vision plan through SISC Direct Bill • The following dental and/or vision plans are offered to Direct Bill members if they are currently enrolled in Dental and Vision through YCCD • *Delta Dental Premier Incentive Plan $1500 • The Delta PPO plan is not offered through Direct Bill. Benefits start at 70% if enrolled on Delta PPO. • *VSP C $20 • Compared to YCCD plan, premium is a bit lower, benefits every year, copay $20 *The dental and vision plans listed above are the only choices offered under this program. If the retiree currently has a different dental or vision plan with the school district and they wish to continue with one or both of these products, they will have to change to the plans listed above in order to participate in this program. The retiree will not have the option of staying on the district dental and/or vision plan if they participate in SISC Retiree Direct Bill.
17 Section V: General Information Retirees Turning 65 – Medicare Enrollment Timing and Process • SISC will send retirees/spouses turning 65 a letter approximately 90 days prior to their birthday as a reminder to apply for Medicare Parts A &B. • Contact the SISC office 90 days prior to your 65 th birthday if you would like to continue your SISC coverage after age 65. SISC can then send you the necessary enrollment forms or information required to move to an over 65 plan. • You must enroll and remain enrolled in Medicare Part A and Part B on the first date of Medicare eligibility, otherwise, non-refundable premium surcharges will be applied from the first date of Medicare eligibility. You are eligible for Medicare the first day of the month before your 65 th birthday.
18 Section V: General Information – Medicare Plans When considering other options (outside of SISC)… • Keep your annual Notice of Creditable Coverage • Compare plans carefully (example: KPSA SISC vs. individual) • Understand the Medicare Part D Coverage Gap (“Donut Hole”) • https: //www. medicare. gov/part-d/costs/coverage-gap/part-d-coverage- gap. html • Not everyone will enter the coverage gap. The coverage gap begins after you and your drug plan have spent a certain amount for covered drugs. In 2016, once you and your plan have spent $3, 310 ($3, 700 in 2017) on covered drugs, you're in the coverage gap. This amount may change each year. • SISC plans do NOT have a Part D coverage gap • Plan ahead so that you maintain continuous coverage • Notify SISC/YCCD if you plan to terminate coverage • Terminate coverage with YCCD only after you have a new plan in place • Avoid Medicare late enrollment penalties
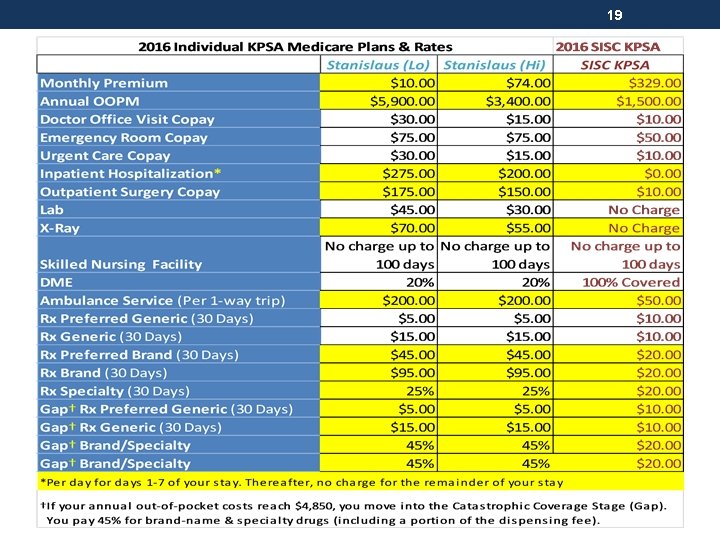
19
20 Resources • Medicare & You Handbook - published annually www. medicare. gov/medicare-and-you/medicare-andyou. html • Stanislaus County HICAP office http: //cahealthadvocates. org/hicap/stanislaus/ (209) 558 -4540 • Toulumne County HICAP office http: //cahealthadvocates. org/hicap/toulumne/ (209) 532 -6272 ext. 226
21 Section VI: Review • Multiple plan options available through YCCD • The Companion. Care and KPSA options are less expensive than PPO • You may change mid-year to Companion. Care or KPSA with at least 60 days notice to the YCCD Benefits Department • If you want to change back to PPO, you will need to wait until the annual Open Enrollment (October 1 st effective date) • KPSA • KP Enrollment form and KPSA election form + Medicare card copies for each covered member • Companion. Care Enrollment Form + Medicare card copies for each covered member
22 Questions? Thank you for your attendance.
- Slides: 22