RETINOPATHY OF PREMATURITY MEDICAL AND EDUCATIONAL PERSPECTIVES Preterm
- Slides: 52
RETINOPATHY OF PREMATURITY MEDICAL AND EDUCATIONAL PERSPECTIVES
Preterm Birth ■ 15 million babies are born too soon every year ■ 1. 1 million babies die from preterm birth complications ■ Over 1 million children die each year due to complications of preterm birth ■ Many survivors face a lifetime of disability, including learning disabilities and visual and hearing problems http: //www. marchofdimes. org
Preterm Birth ■ Preterm birth is defined as babies born alive before 37 weeks of pregnancy ■ Moderate to late preterm (32 to <37 weeks) ■ Very preterm (28 to <32 weeks) ■ Extremely preterm (<28 weeks) http: //www. marchofdimes. org
Socio-economic impact of Premature Birth on Vision: Development of Retinopathy of Prematurity Leading to blindness/poor vision in early infancy (ROP) Long-lasting burden, both in terms of social dependency and lost productivity
Steve Wonder, the singer we all love was born Premature and is Blind from Retinopathy of Prematurity (ROP)
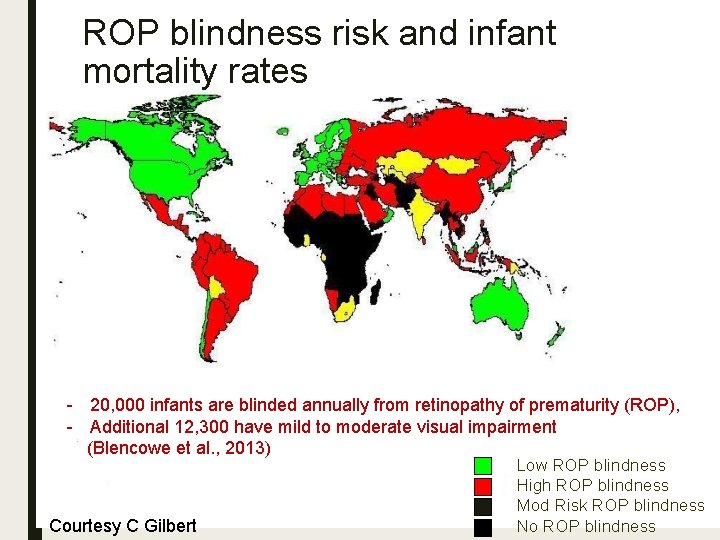
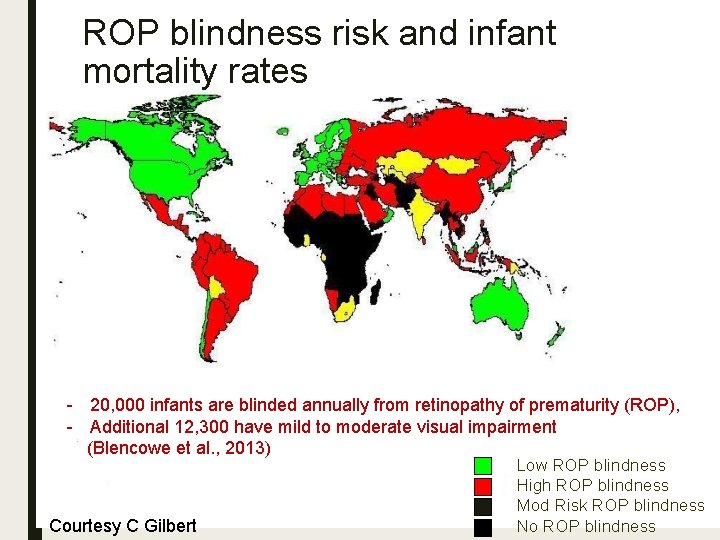
ROP blindness risk and infant mortality rates - 20, 000 infants are blinded annually from retinopathy of prematurity (ROP), - Additional 12, 300 have mild to moderate visual impairment (Blencowe et al. , 2013) Courtesy C Gilbert Low ROP blindness High ROP blindness Mod Risk ROP blindness No ROP blindness
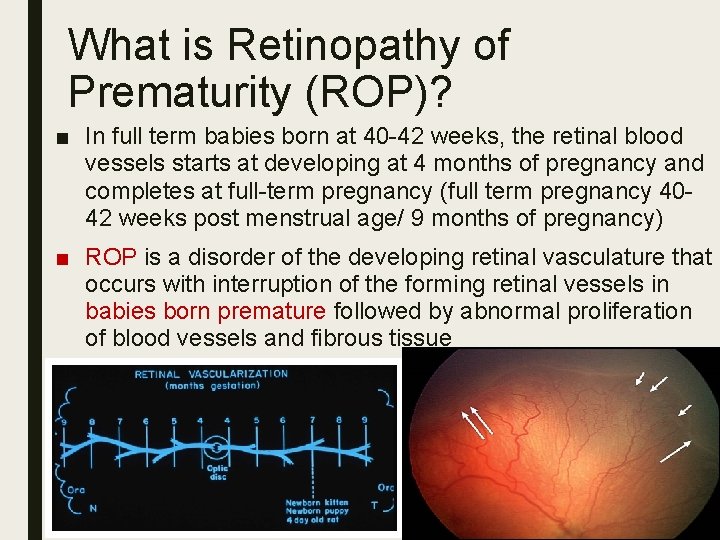
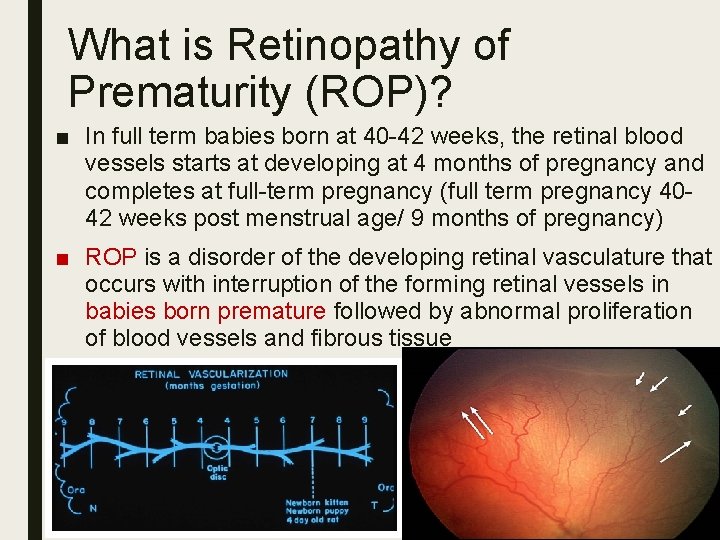
What is Retinopathy of Prematurity (ROP)? ■ In full term babies born at 40 -42 weeks, the retinal blood vessels starts at developing at 4 months of pregnancy and completes at full-term pregnancy (full term pregnancy 4042 weeks post menstrual age/ 9 months of pregnancy) ■ ROP is a disorder of the developing retinal vasculature that occurs with interruption of the forming retinal vessels in babies born premature followed by abnormal proliferation of blood vessels and fibrous tissue
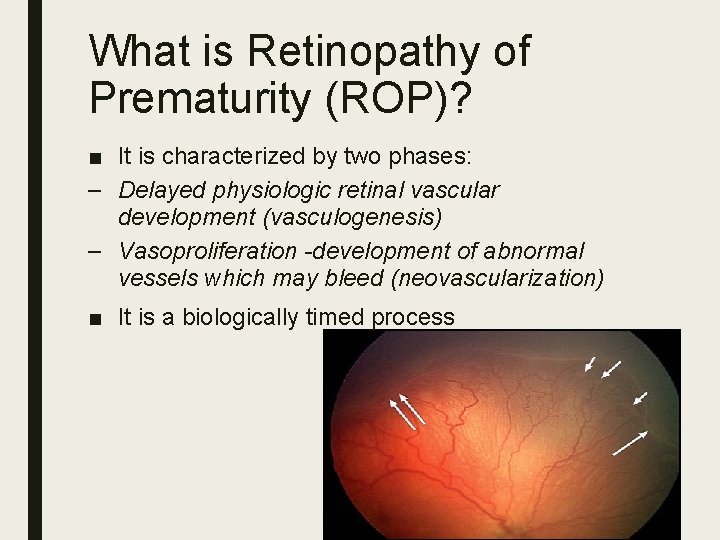
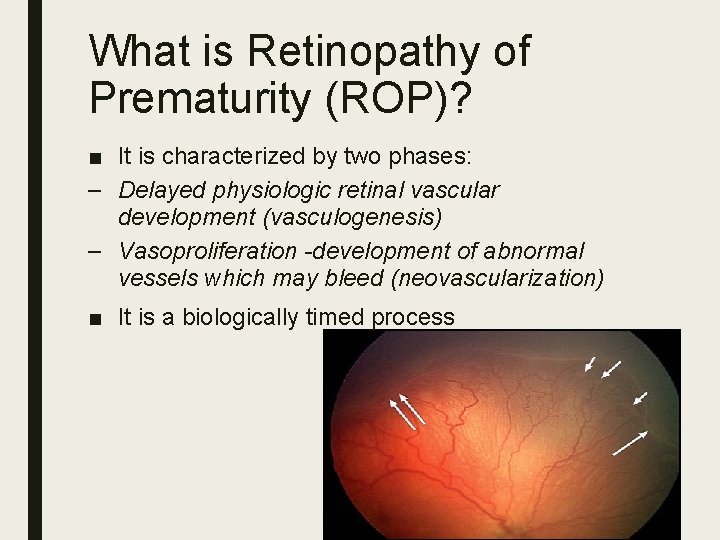
What is Retinopathy of Prematurity (ROP)? ■ It is characterized by two phases: – Delayed physiologic retinal vascular development (vasculogenesis) – Vasoproliferation -development of abnormal vessels which may bleed (neovascularization) ■ It is a biologically timed process
Risk Factors in the development of ROP ■ Premature birth (the lower the gestational age at birth higher the risk) ■ Low birth weight (the lower the weight at birth, higher the risk) ■ Multiple births ■ high levels of oxygen, fluctuations in oxygen delivery- severe ROP ■ Blood transfusions ■ Drugs/medicines (steroids) ■ Other associated illnesses (infection (sepsis), decrease blood pressure (hypotension), brain bleed (intraventricular hemorrhage) Some factors can be ameliorated by improved neonatal care
Major risk factors ■ High levels of oxygen supplementation was considered to be sole cause in early studies (50’s & 60’s) (Patz, Cross, Kinsey) ■ Both high oxygen (hyperoxia) and low oxygen (hypoxia) played role in the development of ROP ■ Low birth weight and lower gestational age are considered as the main prognostic factors in the development of ROP. Birth Year 1950
ROP and Oxygen ■ Restrictions in OXYGEN supplementation in 1950’s led to less blinding disease, but an estimated 16 deaths for every blindness prevented ■ Better monitoring capabilities and improved neonatal care have gradually decreased morbidity due to ROP – Continuous monitoring – Greater awareness
Three Epidemics of ROP ■ 1 st – affluent nurseries well stocked with oxygen ■ 2 nd – increased survival of smaller, more premature babies in high income countries ■ 3 rd – increase in the incidence of ROP in middle income and newly industrialized countries, which is occurring at the same time as the increasing survival of very immature infants,
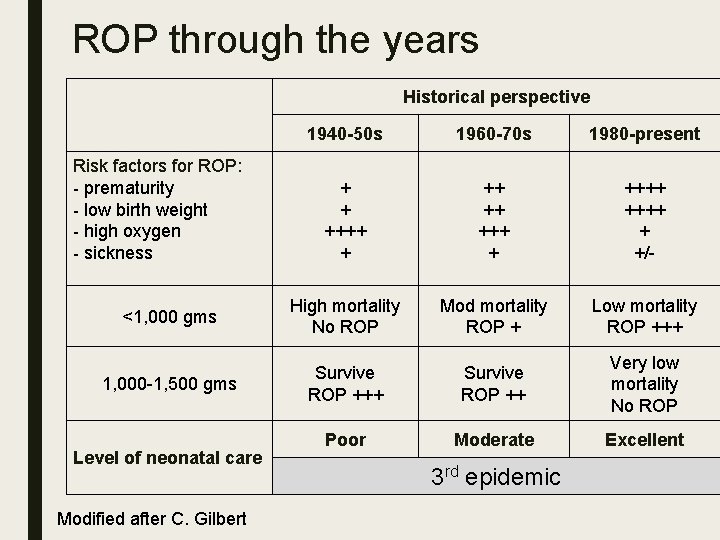
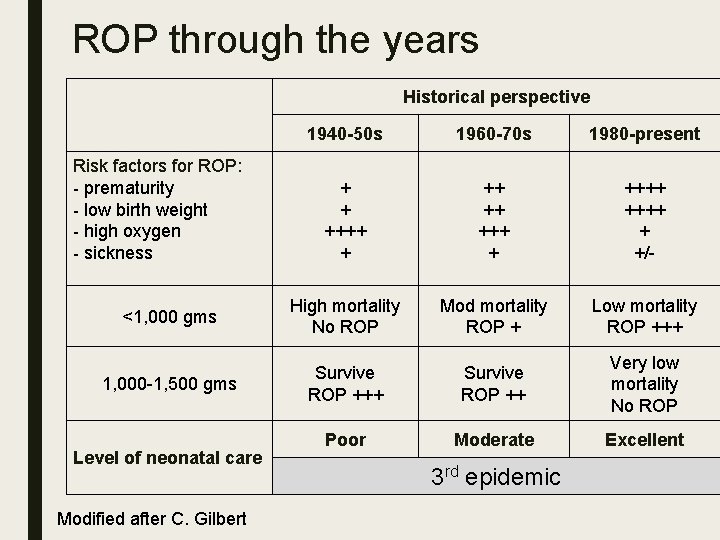
ROP through the years Historical perspective 1940 -50 s 1960 -70 s 1980 -present + + ++++ + ++++ + +/- <1, 000 gms High mortality No ROP Mod mortality ROP + Low mortality ROP +++ 1, 000 -1, 500 gms Survive ROP +++ Survive ROP ++ Very low mortality No ROP Poor Moderate Excellent Risk factors for ROP: - prematurity - low birth weight - high oxygen - sickness Level of neonatal care Modified after C. Gilbert 3 rd epidemic
How have advances in detection and treatment of ROP been possible? ■ Classification of acute phases of retinopathy ■ Randomized controlled clinical trials ■ Population-based natural history studies ■ Increased awareness and cooperation among neonatologists, ophthalmologists, and basic scientists
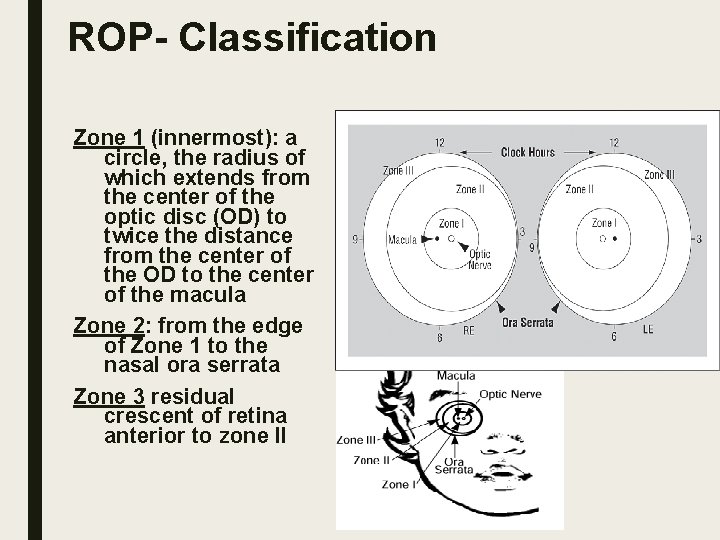
Basic Principle of International Classification of ROP (ICROP) The more posterior the disease and the greater the amount of involved retina, the more serious the ROP disease
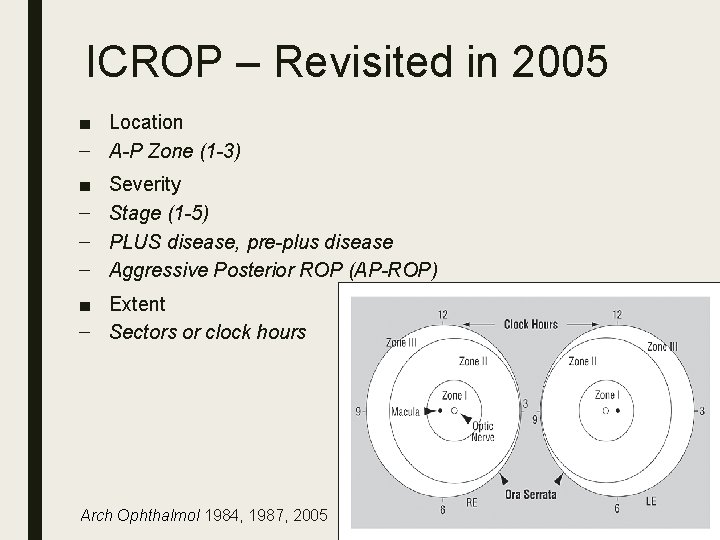
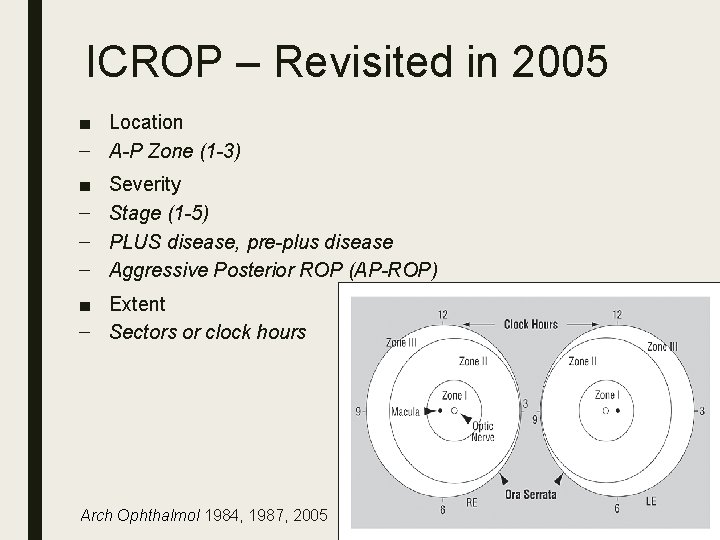
ICROP – Revisited in 2005 ■ Location – A-P Zone (1 -3) ■ – – – Severity Stage (1 -5) PLUS disease, pre-plus disease Aggressive Posterior ROP (AP-ROP) ■ Extent – Sectors or clock hours Arch Ophthalmol 1984, 1987, 2005
ROP eye examination by ophthalmologist in NICU and clinic
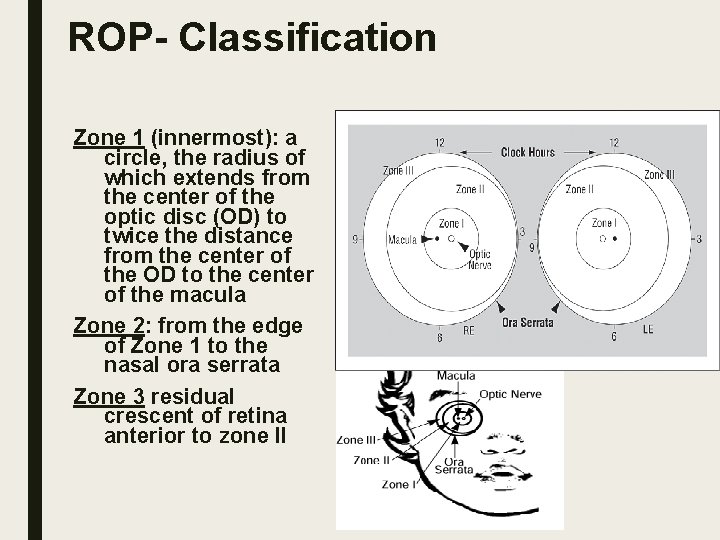
ROP- Classification Zone 1 (innermost): a circle, the radius of which extends from the center of the optic disc (OD) to twice the distance from the center of the OD to the center of the macula Zone 2: from the edge of Zone 1 to the nasal ora serrata Zone 3 residual crescent of retina anterior to zone II
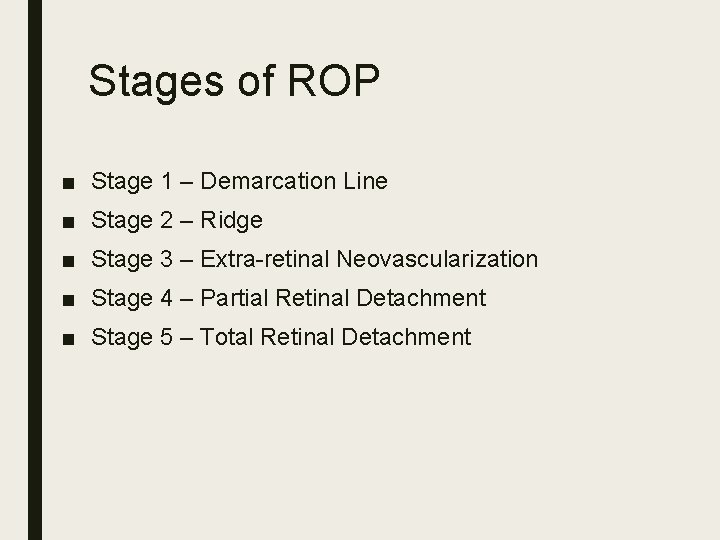
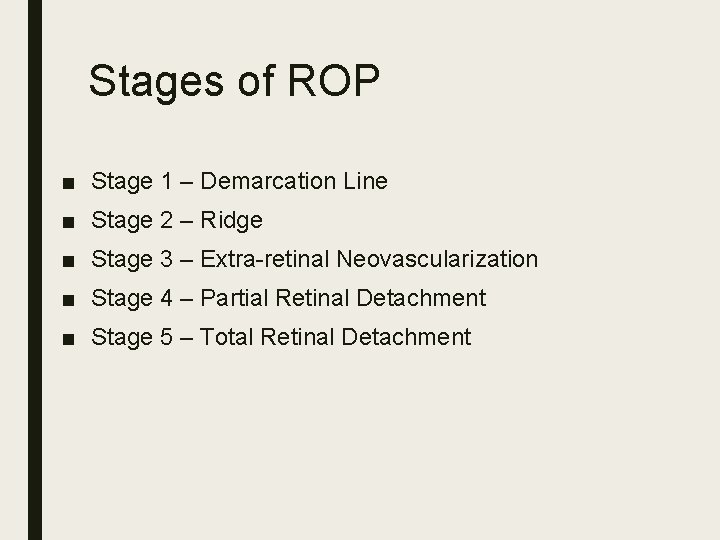
Stages of ROP ■ Stage 1 – Demarcation Line ■ Stage 2 – Ridge ■ Stage 3 – Extra-retinal Neovascularization ■ Stage 4 – Partial Retinal Detachment ■ Stage 5 – Total Retinal Detachment
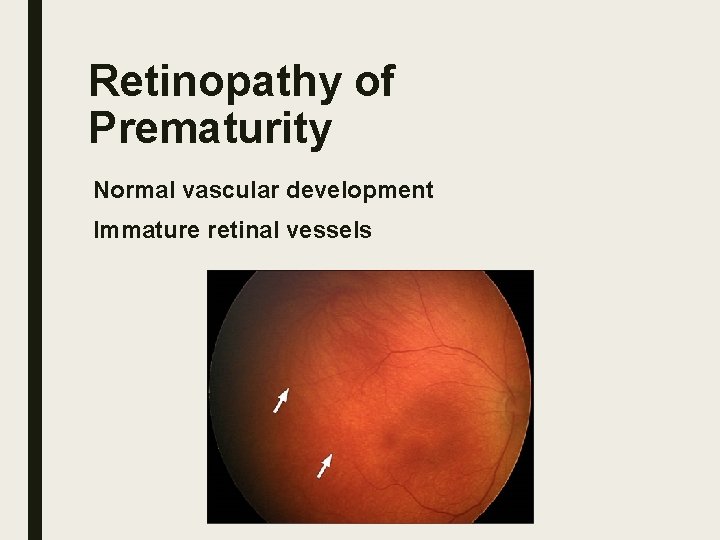
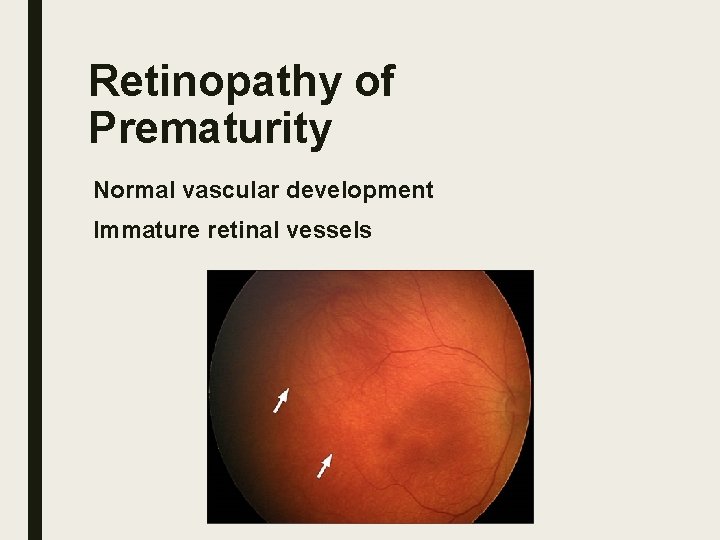
Retinopathy of Prematurity Normal vascular development Immature retinal vessels
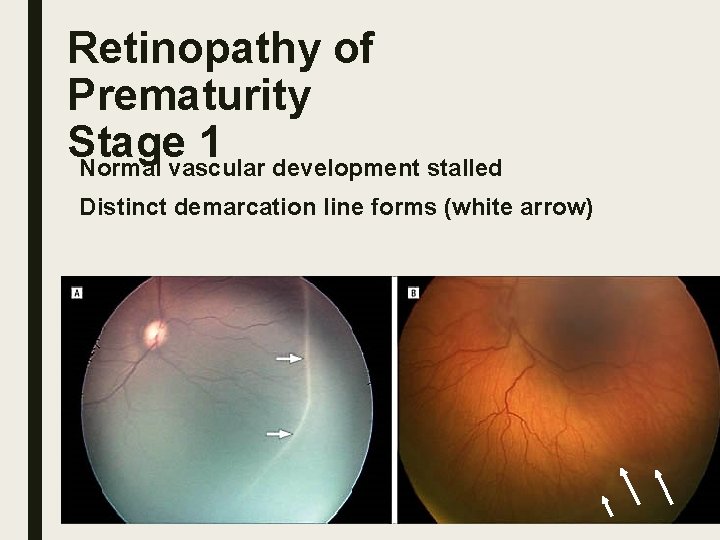
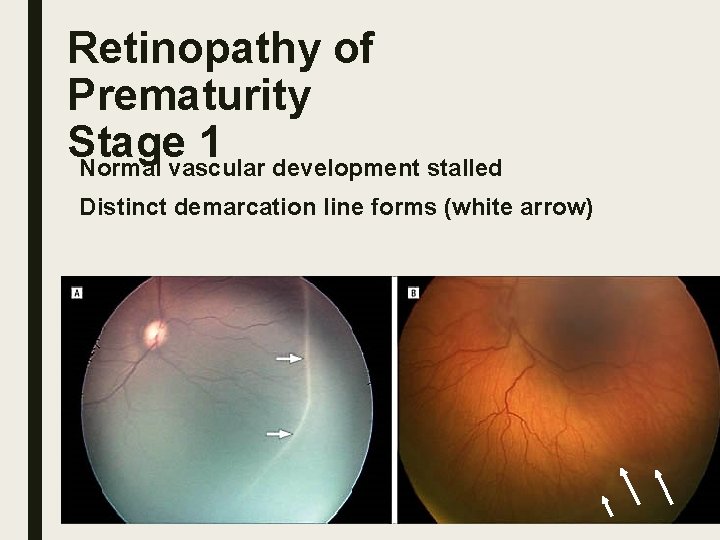
Retinopathy of Prematurity Stage 1 Normal vascular development stalled Distinct demarcation line forms (white arrow)
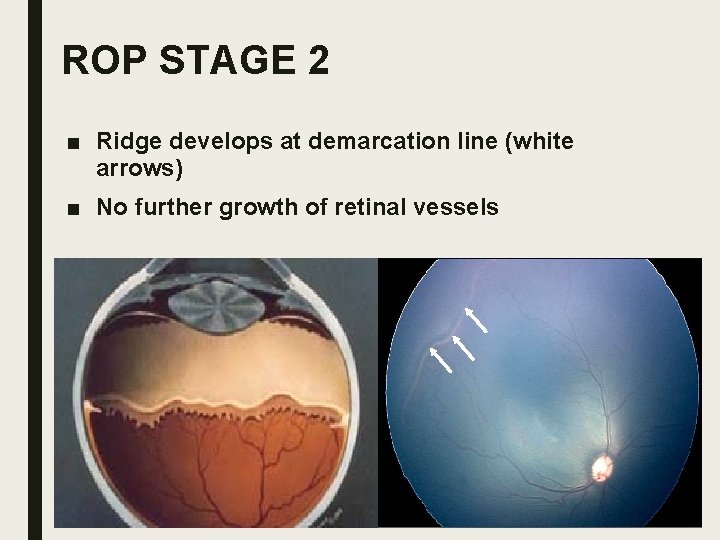
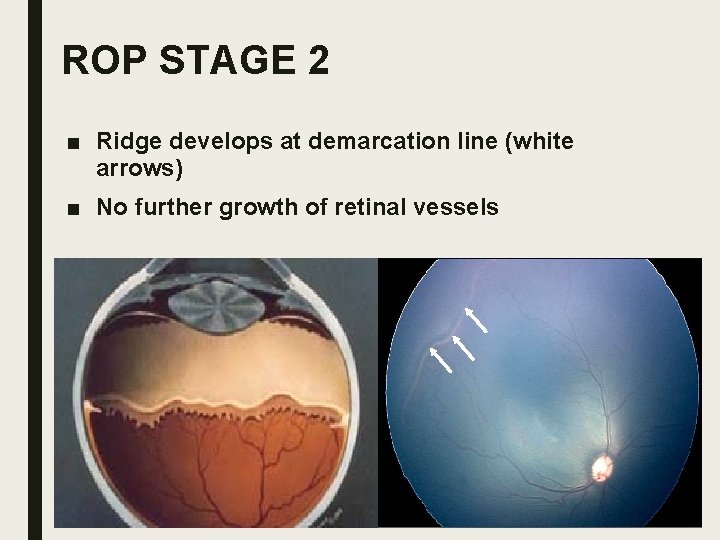
ROP STAGE 2 ■ Ridge develops at demarcation line (white arrows) ■ No further growth of retinal vessels
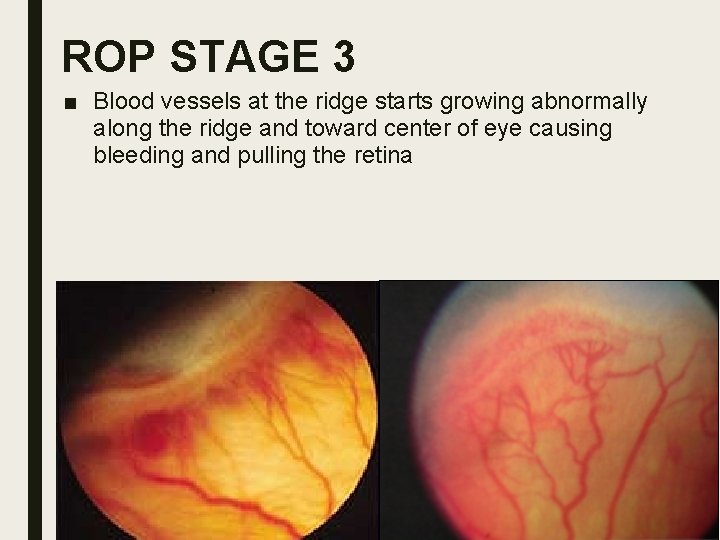
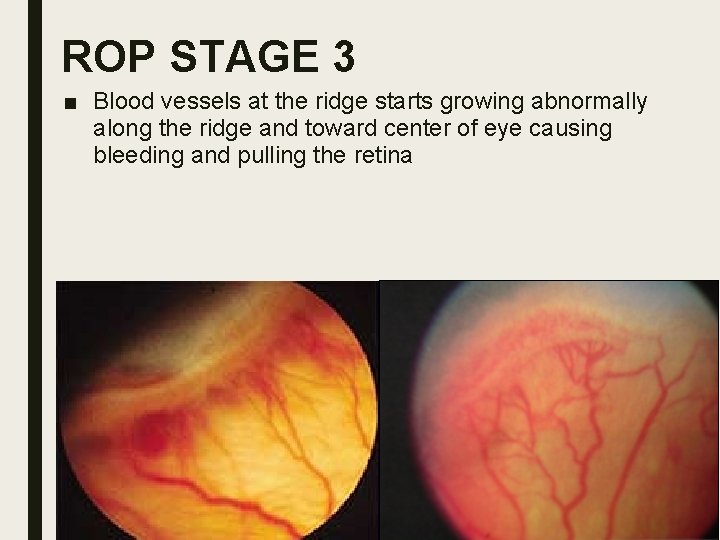
ROP STAGE 3 ■ Blood vessels at the ridge starts growing abnormally along the ridge and toward center of eye causing bleeding and pulling the retina
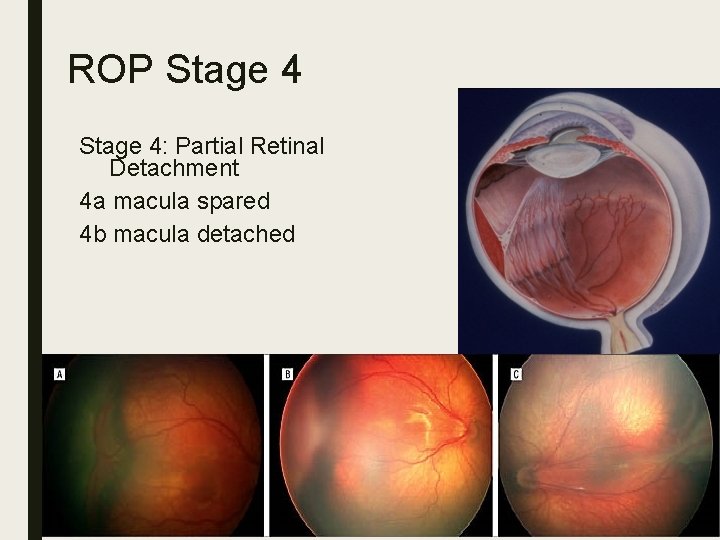
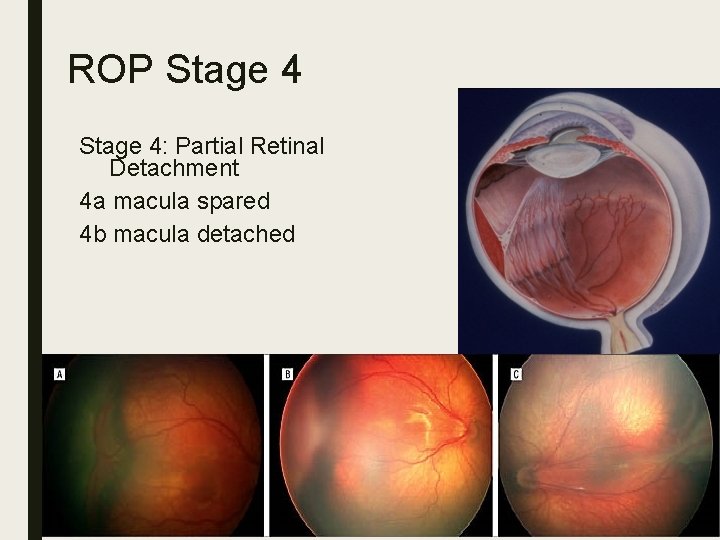
ROP Stage 4: Partial Retinal Detachment 4 a macula spared 4 b macula detached
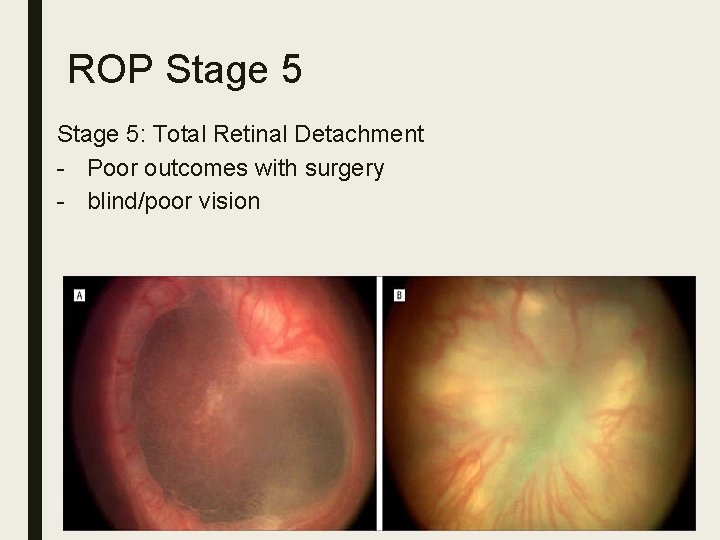
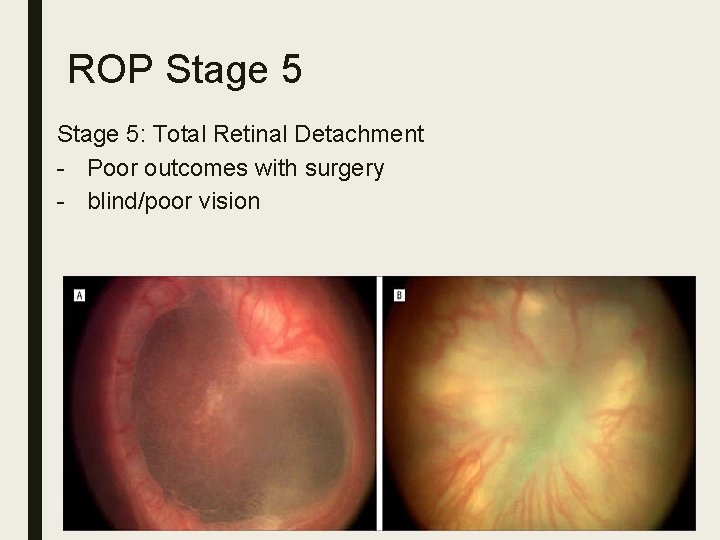
ROP Stage 5: Total Retinal Detachment - Poor outcomes with surgery - blind/poor vision
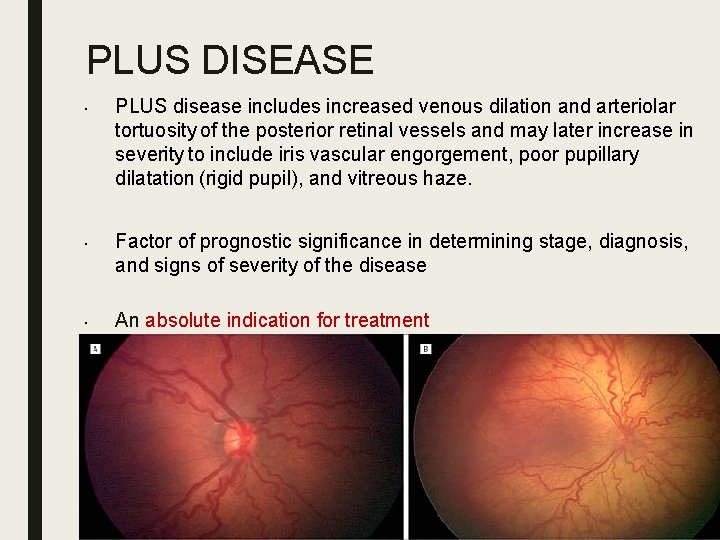
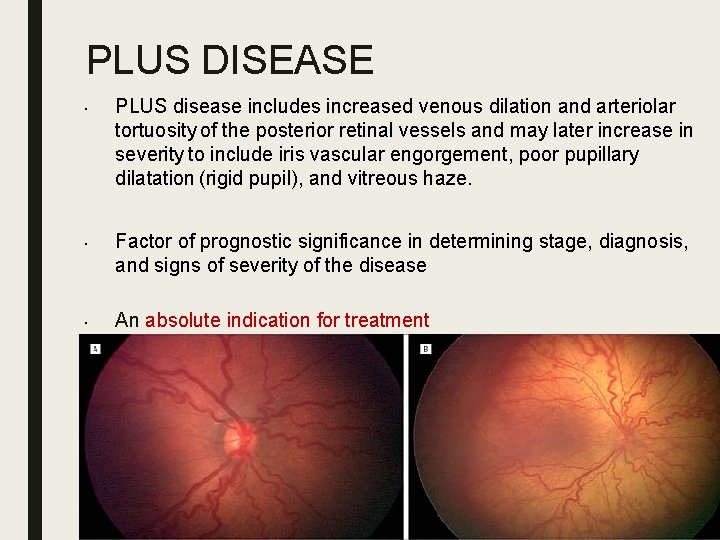
PLUS DISEASE • • • PLUS disease includes increased venous dilation and arteriolar tortuosity of the posterior retinal vessels and may later increase in severity to include iris vascular engorgement, poor pupillary dilatation (rigid pupil), and vitreous haze. Factor of prognostic significance in determining stage, diagnosis, and signs of severity of the disease An absolute indication for treatment
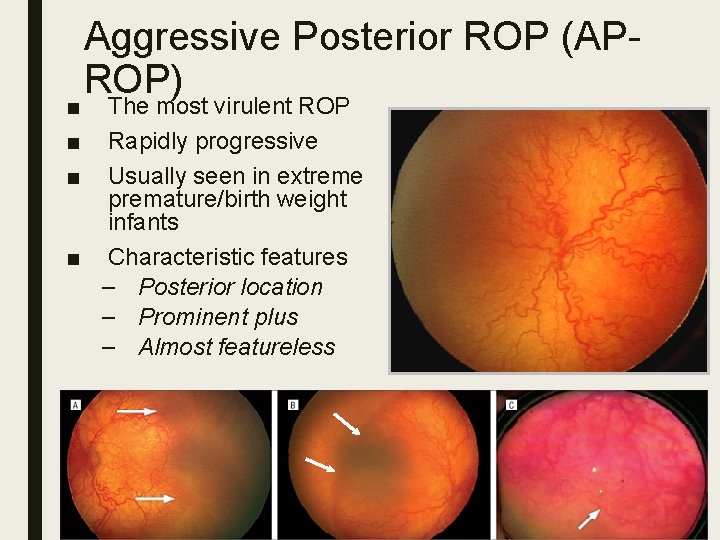
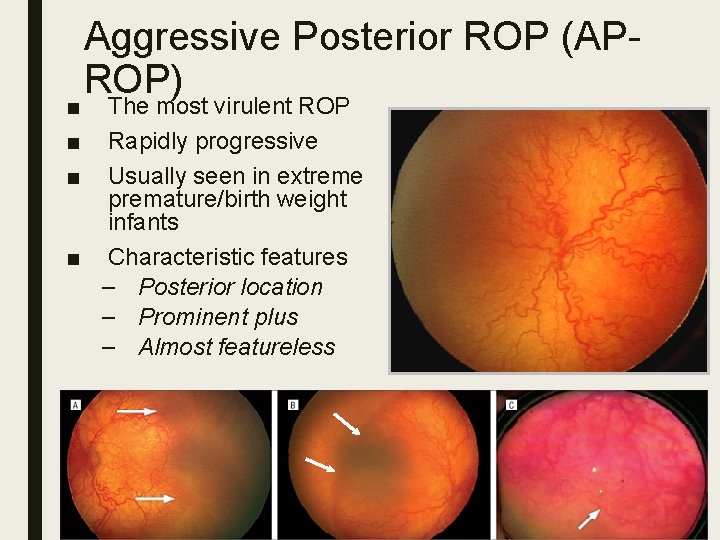
■ ■ ■ Aggressive Posterior ROP (APROP) The most virulent ROP Rapidly progressive Usually seen in extreme premature/birth weight infants ■ Characteristic features – Posterior location – Prominent plus – Almost featureless
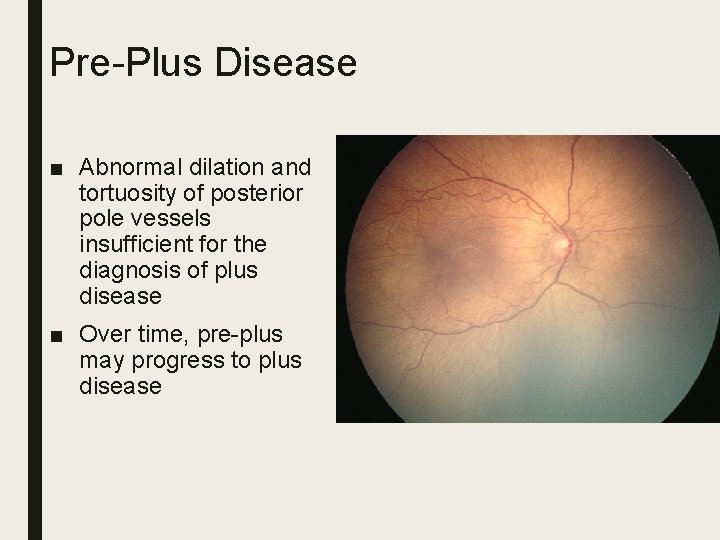
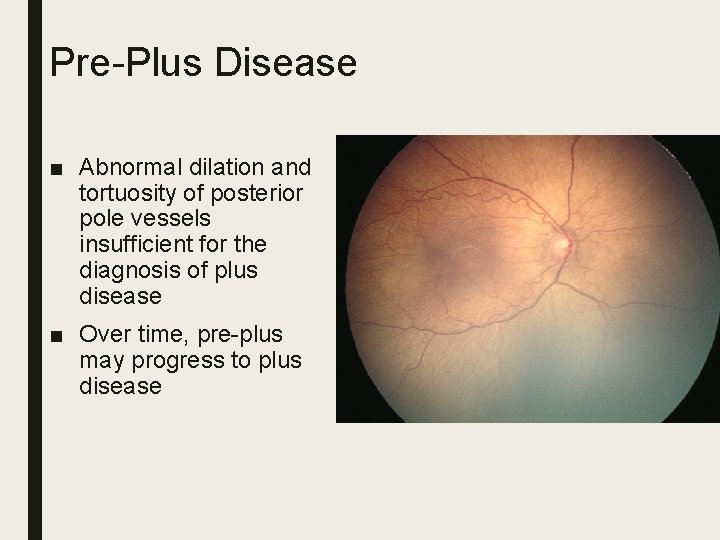
Pre-Plus Disease ■ Abnormal dilation and tortuosity of posterior pole vessels insufficient for the diagnosis of plus disease ■ Over time, pre-plus may progress to plus disease
Treatment Options: Primary Prevention – Decrease preterm birth – Modify or treat risk factors – Excellent neonatal care facilities
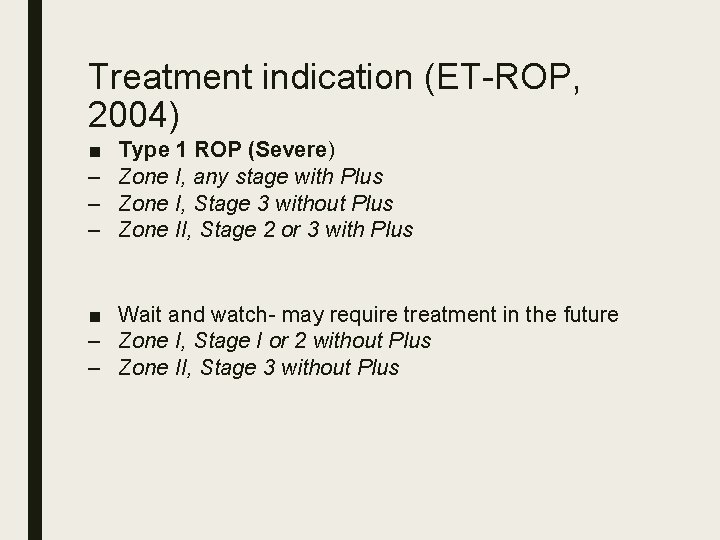
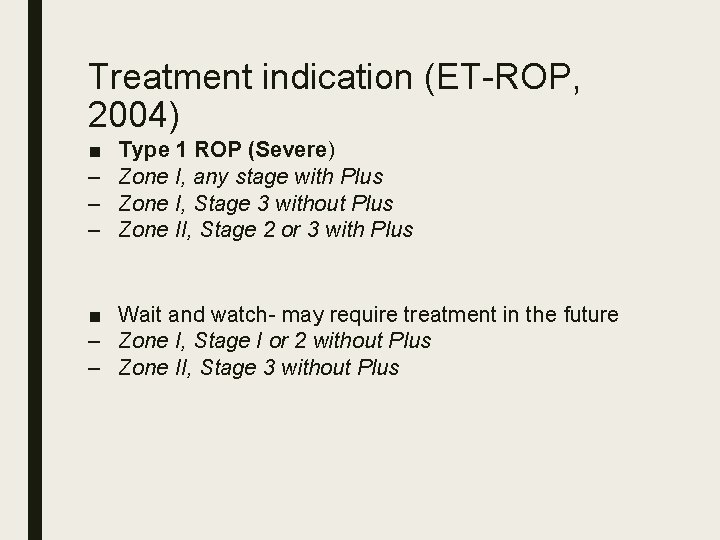
Treatment indication (ET-ROP, 2004) ■ – – – Type 1 ROP (Severe) Zone I, any stage with Plus Zone I, Stage 3 without Plus Zone II, Stage 2 or 3 with Plus ■ Wait and watch- may require treatment in the future – Zone I, Stage I or 2 without Plus – Zone II, Stage 3 without Plus
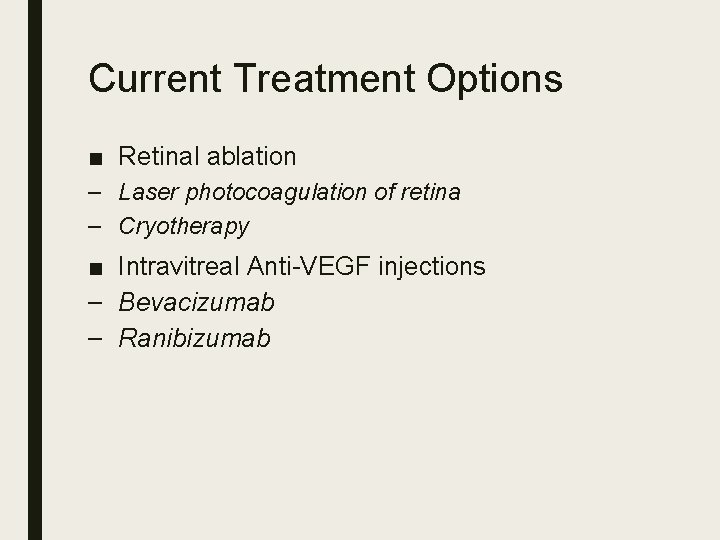
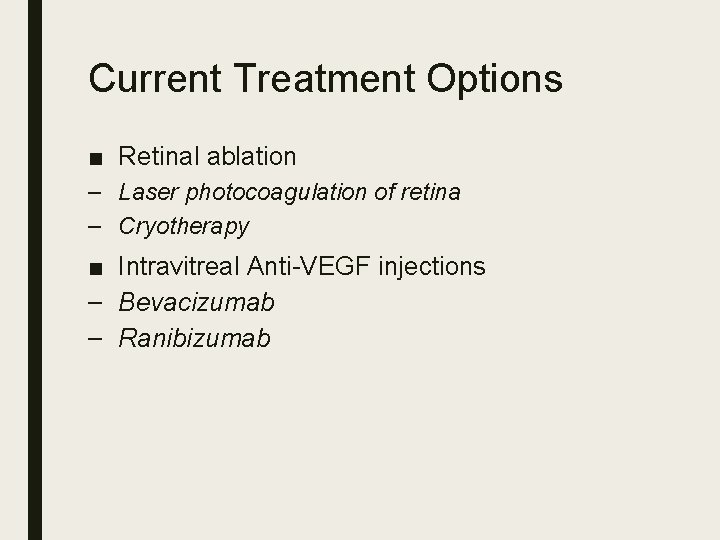
Current Treatment Options ■ Retinal ablation – Laser photocoagulation of retina – Cryotherapy ■ Intravitreal Anti-VEGF injections – Bevacizumab – Ranibizumab
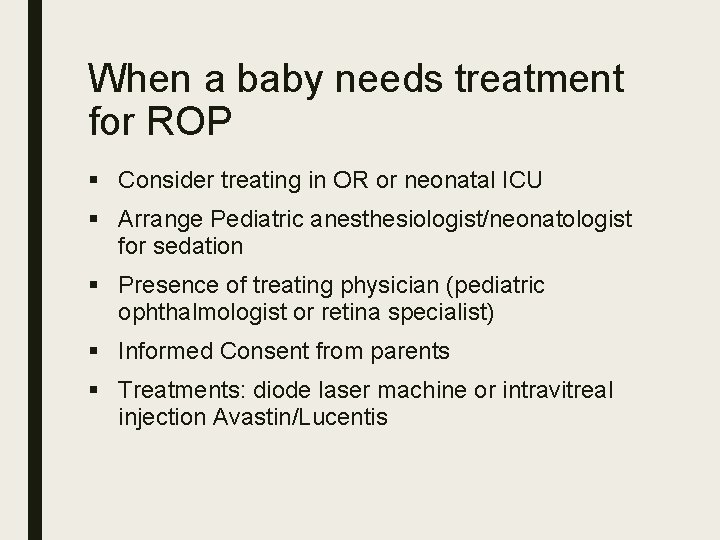
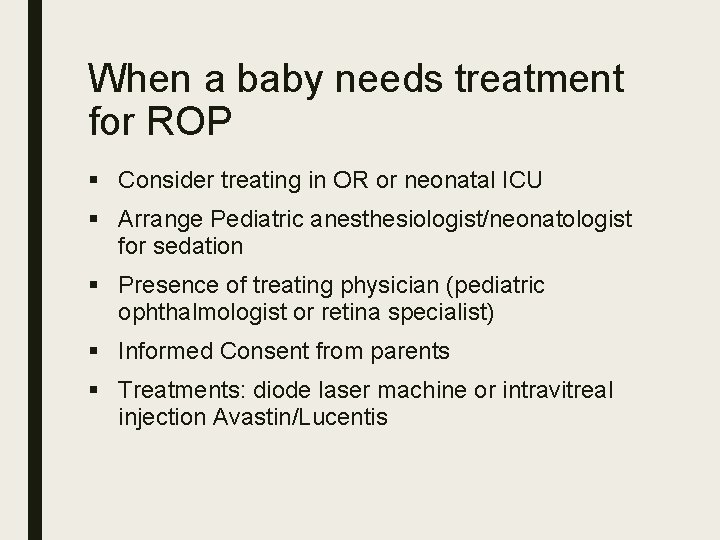
When a baby needs treatment for ROP § Consider treating in OR or neonatal ICU § Arrange Pediatric anesthesiologist/neonatologist for sedation § Presence of treating physician (pediatric ophthalmologist or retina specialist) § Informed Consent from parents § Treatments: diode laser machine or intravitreal injection Avastin/Lucentis
Treatment: ROP laser photocoagulation
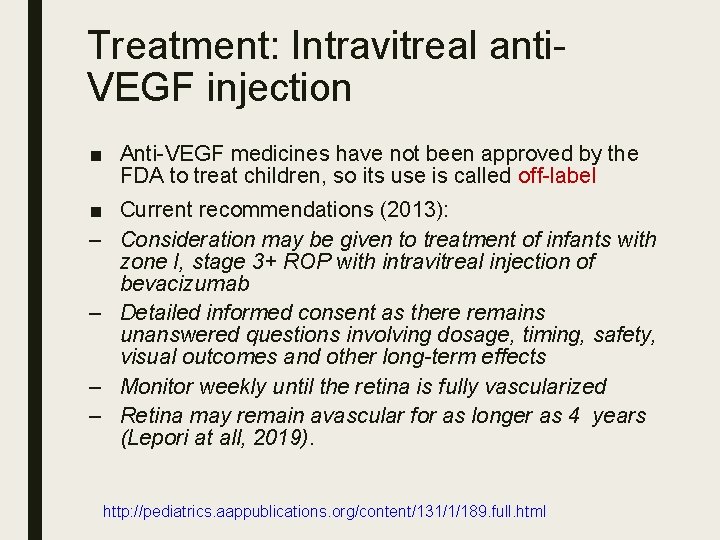
Treatment: Intravitreal anti. VEGF injection ■ Anti-VEGF medicines have not been approved by the FDA to treat children, so its use is called off-label ■ Current recommendations (2013): – Consideration may be given to treatment of infants with zone I, stage 3+ ROP with intravitreal injection of bevacizumab – Detailed informed consent as there remains unanswered questions involving dosage, timing, safety, visual outcomes and other long-term effects – Monitor weekly until the retina is fully vascularized – Retina may remain avascular for as longer as 4 years (Lepori at all, 2019). http: //pediatrics. aappublications. org/content/131/1/189. full. html
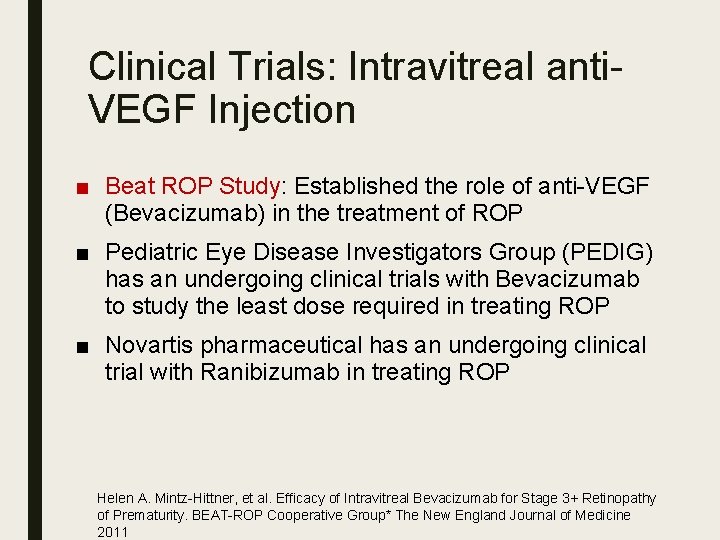
Clinical Trials: Intravitreal anti. VEGF Injection ■ Beat ROP Study: Established the role of anti-VEGF (Bevacizumab) in the treatment of ROP ■ Pediatric Eye Disease Investigators Group (PEDIG) has an undergoing clinical trials with Bevacizumab to study the least dose required in treating ROP ■ Novartis pharmaceutical has an undergoing clinical trial with Ranibizumab in treating ROP Helen A. Mintz-Hittner, et al. Efficacy of Intravitreal Bevacizumab for Stage 3+ Retinopathy of Prematurity. BEAT-ROP Cooperative Group* The New England Journal of Medicine 2011
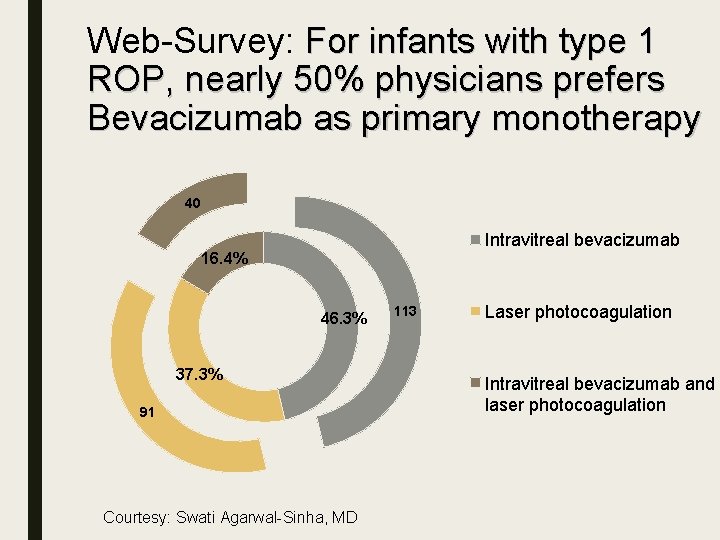
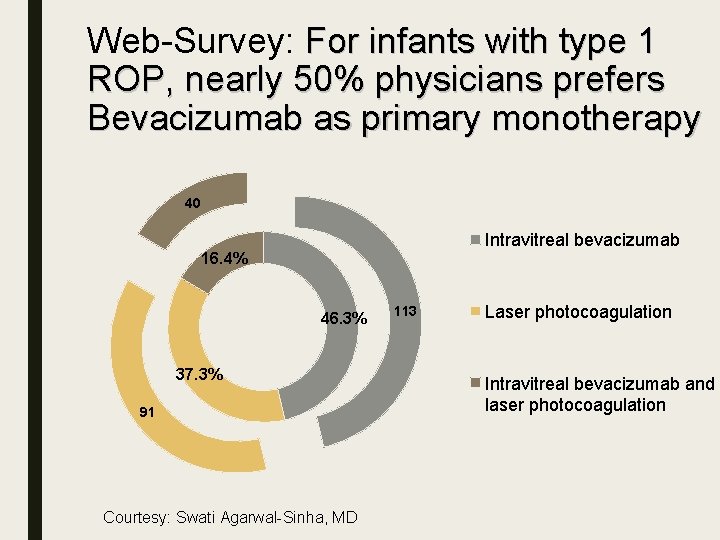
Web-Survey: For infants with type 1 ROP, nearly 50% physicians prefers Bevacizumab as primary monotherapy 40 Intravitreal bevacizumab 16. 4% 46. 3% 37. 3% 91 Courtesy: Swati Agarwal-Sinha, MD 113 Laser photocoagulation Intravitreal bevacizumab and laser photocoagulation
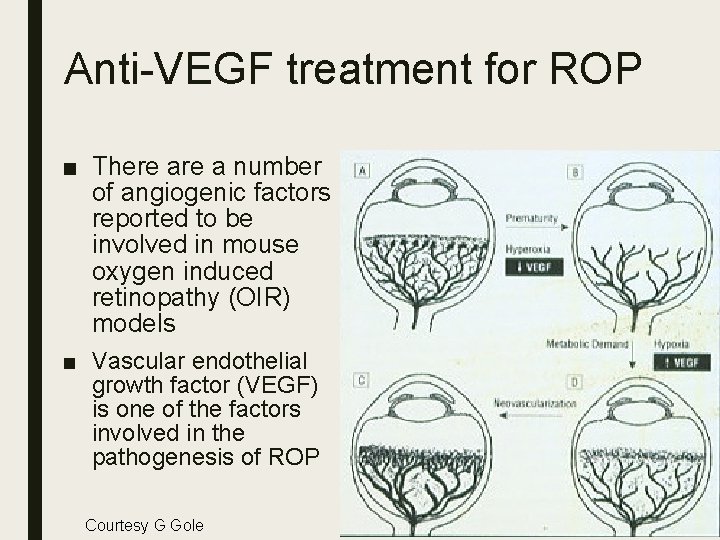
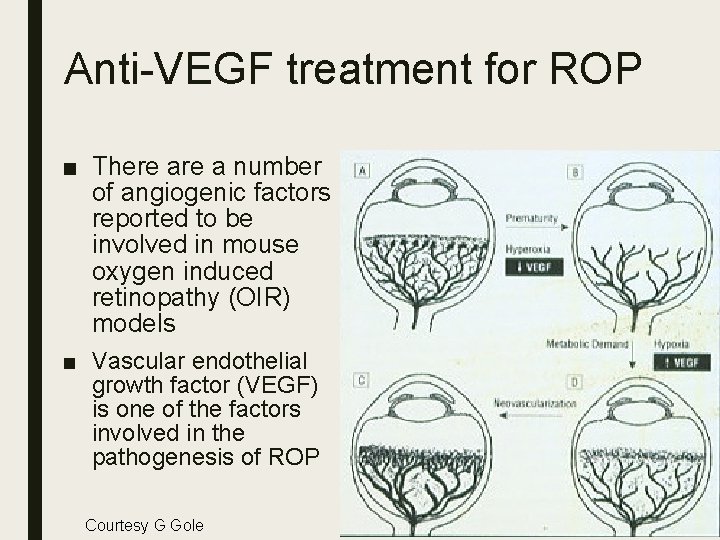
Anti-VEGF treatment for ROP ■ There a number of angiogenic factors reported to be involved in mouse oxygen induced retinopathy (OIR) models ■ Vascular endothelial growth factor (VEGF) is one of the factors involved in the pathogenesis of ROP Courtesy G Gole
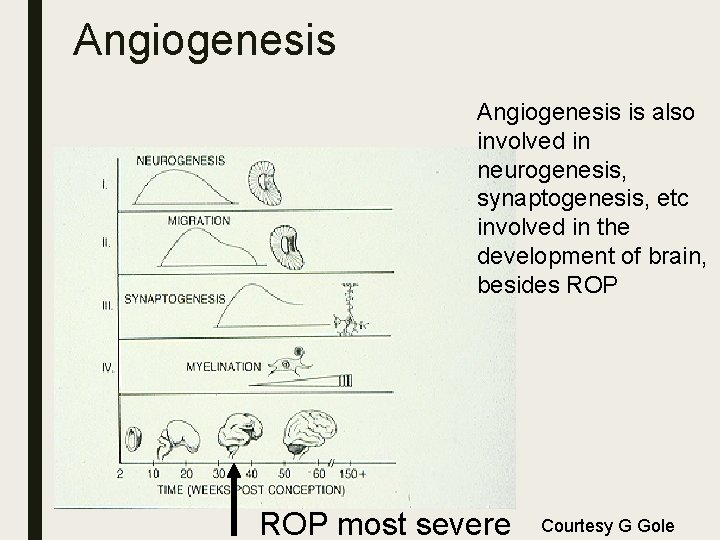
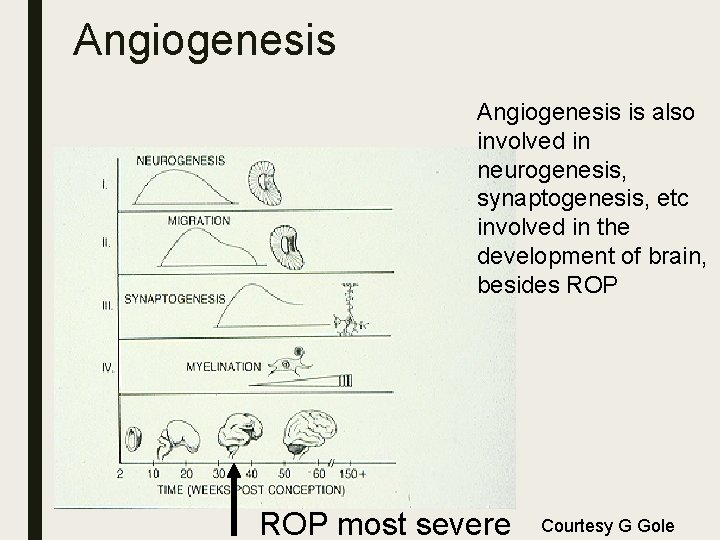
Angiogenesis is also involved in neurogenesis, synaptogenesis, etc involved in the development of brain, besides ROP most severe Courtesy G Gole
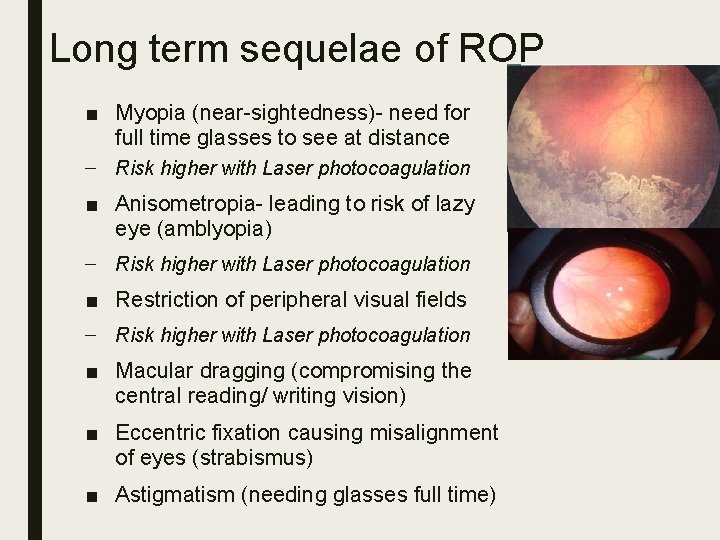
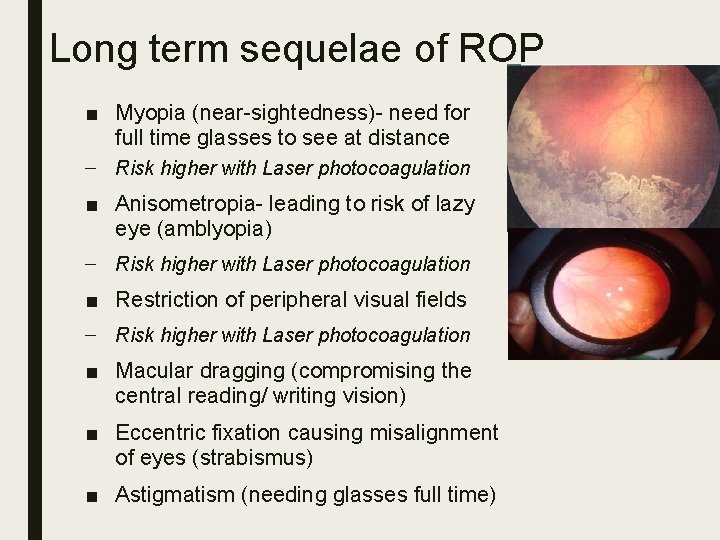
Long term sequelae of ROP ■ Myopia (near-sightedness)- need for full time glasses to see at distance – Risk higher with Laser photocoagulation ■ Anisometropia- leading to risk of lazy eye (amblyopia) – Risk higher with Laser photocoagulation ■ Restriction of peripheral visual fields – Risk higher with Laser photocoagulation ■ Macular dragging (compromising the central reading/ writing vision) ■ Eccentric fixation causing misalignment of eyes (strabismus) ■ Astigmatism (needing glasses full time)
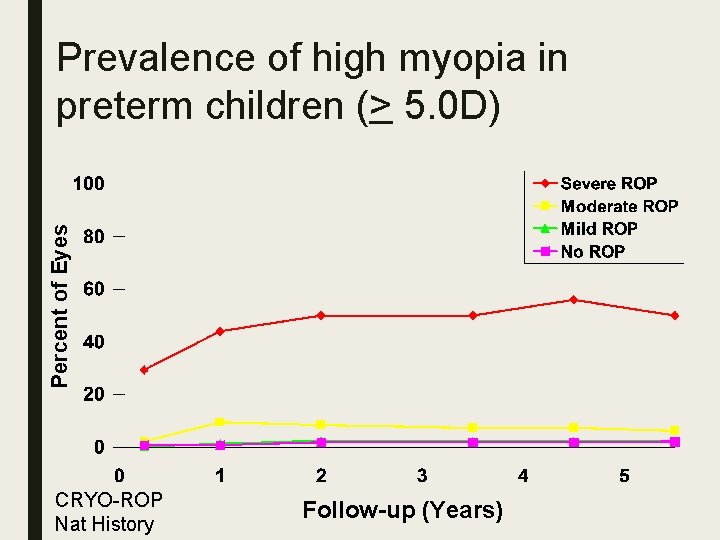
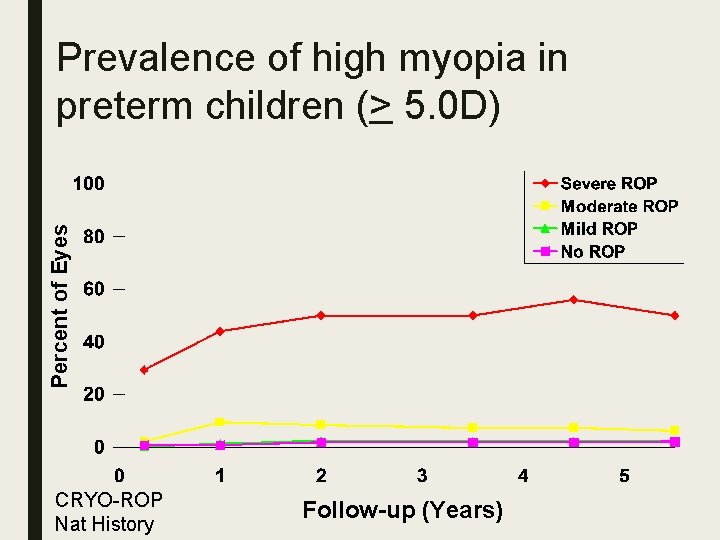
Percent of Eyes Prevalence of high myopia in preterm children (> 5. 0 D) CRYO-ROP Nat History Follow-up (Years)
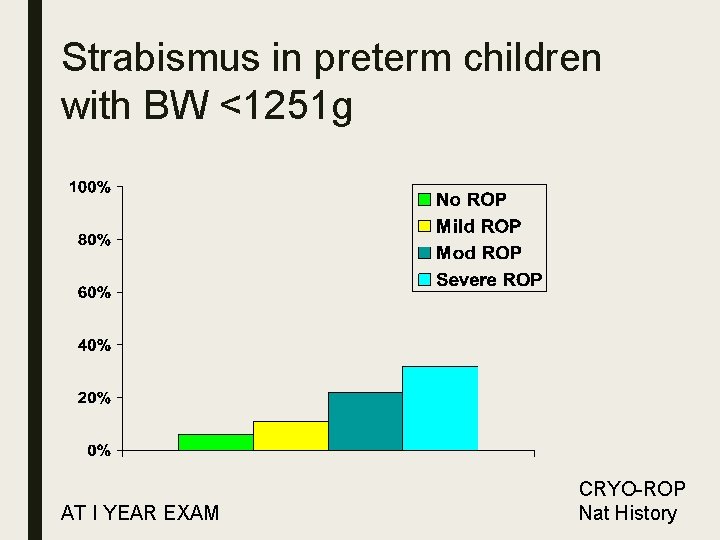
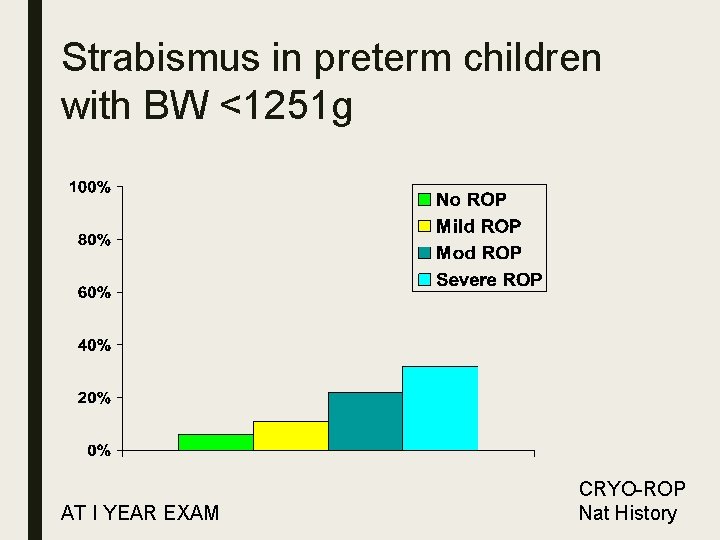
Strabismus in preterm children with BW <1251 g AT I YEAR EXAM CRYO-ROP Nat History
Neurologic Complications Associated with Prematurity Global delays Motor disability: cerebral palsy 7 -30% Cognitive disability Autism spectrum Neurological visual impairment (CVI)
Children with visual impairment often have other disabilities and there are not programs to support the child nor their families ■ Little data on outcomes of interventions for preverbal and nonverbal children with visual impairment before school age
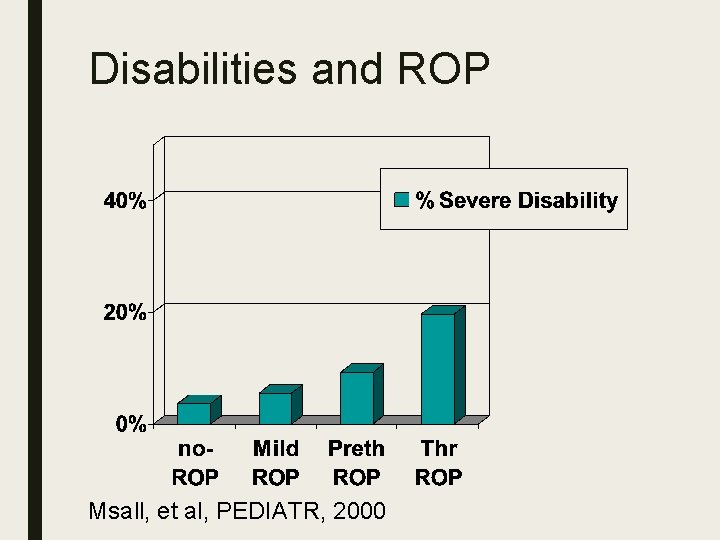
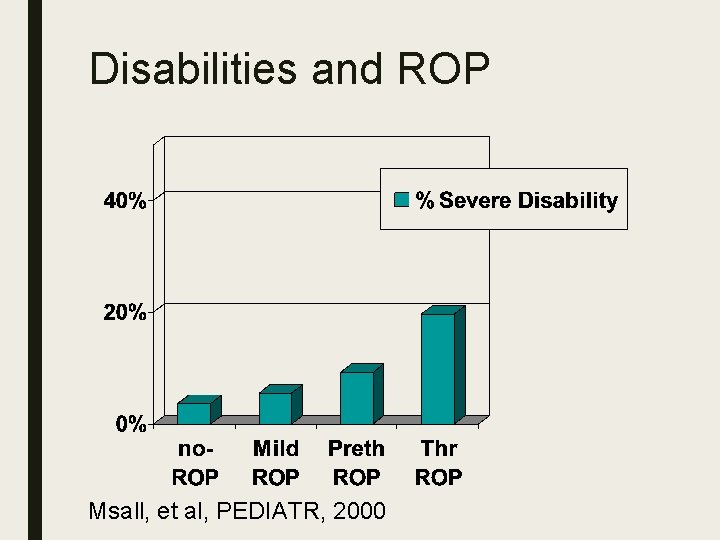
Disabilities and ROP Msall, et al, PEDIATR, 2000
Advocacy ■ Local, Regional, National plans ■ Should be established by National Societies (Ophthalmology and Pediatrics) ■ Governmental support ■ National Prevention of Blindness Committees
Interventions ■ Optical: correct refractive errors patching (amblyopia) spectacles (strabismus, anisometropia) magnification, poor accommodation ■ Surgical: retinal detachment surgery , strabismus surgery ■ Medical: glaucoma, strabismus, amblyopia
Interventions Trans-disciplinary: ■ child with multiple impairments ■ delayed visual maturation ■ low vision from structural defects
Conclusion ■ Children born prematurely should have ophthalmologic evaluation and intervention at frequent intervals during first 3 years of life regardless of presence of ROP and amount of prematurity.
Message for Parents/Teachers ■ ROP is caused by prematurity – It’s not the fault of doctors, nurses or ventilators ■ Everyone is stressed out by ROP exams – “for parents ROP examinations are gross” ■ ROP examinations can prevent blindness – Same anesthetic and lid speculum are used as for cataract surgery or LASIK ■ Parents need to follow up after discharge as recommended by the physician
Goal is to optimize child’s development ■ to perform daily activities ■ integrate with classmates ■ better quality of life, and education ■ Enter the job market like any other person
Recommendations ■ Look, you won’t see anything if you are not looking for it! ■ Develop local and regional screening criteria and intervention plans including early intervention
Suggested reads ■ Screening Examination of Premature Infants for Retinopathy of Prematurity. Pediatrics 2013; 131; 189 ■ International Classification for Retinopathy of prematurity Revisited. Arch Ophthalmol. 2005; 123: 991 -999 ■ Efficacy of Intravitreal Bevacizumab for Stage 3+Retinopathy of Prematurity. N Engl J Med 2011; 364: 603 -15.