Retinal Haemorrhages in Infants Aetiology and Differential Diagnosis
- Slides: 29
Retinal Haemorrhages in Infants: Aetiology and Differential Diagnosis Chris Lloyd Paediatric Ophthalmologist Manchester Royal Eye Hospital, UK APIL Meeting 19 th June 2008
Retinal Haemorrhages in Infants • Long associated with inflicted neurotrauma (shaken-baby) • But…also associated with other conditions • Ophthalmologists and lawyers must be aware of the differential diagnosis
Types of Retinal (Fundus) Haemorrhages • • • Vitreous Preretinal Superficial intraretinal Deep intraretinal Sub-RPE/Choroidal Each has characteristic appearance, diagnostic and prognostic implications
Vitreous Haemorrhages • Uncommon (as ILM tough) • Due to breakthrough of large retinal or pre-retinal haemorrhages • Curls, streaks or diffuse patches • Usually clear spontaneously – timescale varies – can be prolonged • Severe haemorrhages may loculate/form ochre membranes - amblyogenic
Pre-retinal (Sub-Hyaloid) Haemorrhages • Blood just below ILM (from radial peripapillary or superficial capillaries) • Singular or in small groups at posterior pole • Initially round – over time develops fluid level (boat, crescent) – postural • Resolves from top to bottom (often leaving curved white line inferiorly)
Pre-retinal “thumbprint” haemorrhage • • • Found at posterior pole Often around 1 DD in size Usually several grouped together Glistening light reflex (not a Roth spot) Absorb quickly leaving no trace
Superficial intra-retinal haemorrhages • Arise from capillaries in superficial capillary bed (between NFL and ganglion cell layer) • Spread along NFL • Elongated, fanning in direction of NFL • Splinter or flame pattern near disc • More irregular in periphery • Clear quickly – bright red to rusty red colour change
Deep intra-retinal haemorrhages • Arise from deep capillary layer (usually in outer reticular layer but may also be in inner or outer nuclear layer) • Blood pools vertically between neural fibres and cell nuclei • Dot or blot appearance • Dots usually clear quickly – blots are domed, full thickness and may persist for weeks
Subretinal haemorrhages • Blood between photoreceptors and RPE • From retina or choroid • Large, retinal haem may break through ELM to cause subretinal haem (partic when neovasc-n) • Red blotches/elevated retina/usually extensive • Slow resorption – yellow exudate • Mottled damaged retina
Choroidal Haemorrhages • Arise from choriocapillaris through break in Bruch’s membrane into space below RPE • May also arise from neovascular tuftson inner side of Bruch’s • Dark blue-Gray colour • RPE stretched and often ruptures – ‘red corona’ • Vast majority traumatic in origin
Retinal Haemorrhages in infancy: Differential Diagnosis 1 Common causes • Normal vaginal/assisted delivery • Inflicted neurotrauma (NAI) • Retinopathy of prematurity
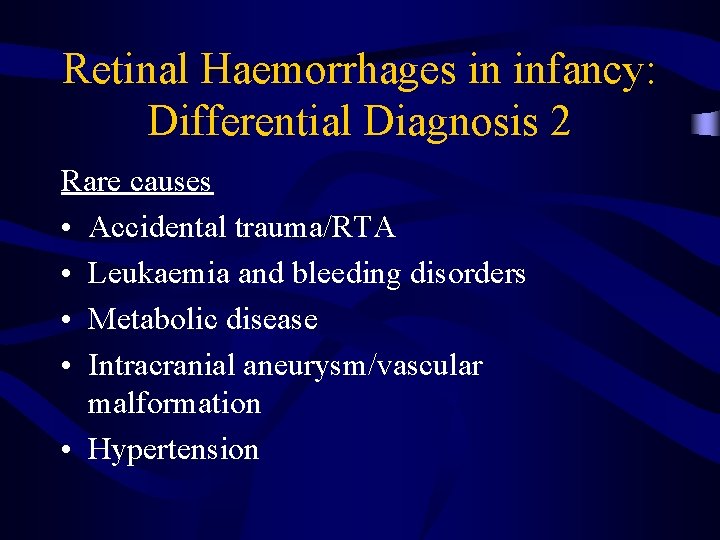
Retinal Haemorrhages in infancy: Differential Diagnosis 2 Rare causes • Accidental trauma/RTA • Leukaemia and bleeding disorders • Metabolic disease • Intracranial aneurysm/vascular malformation • Hypertension
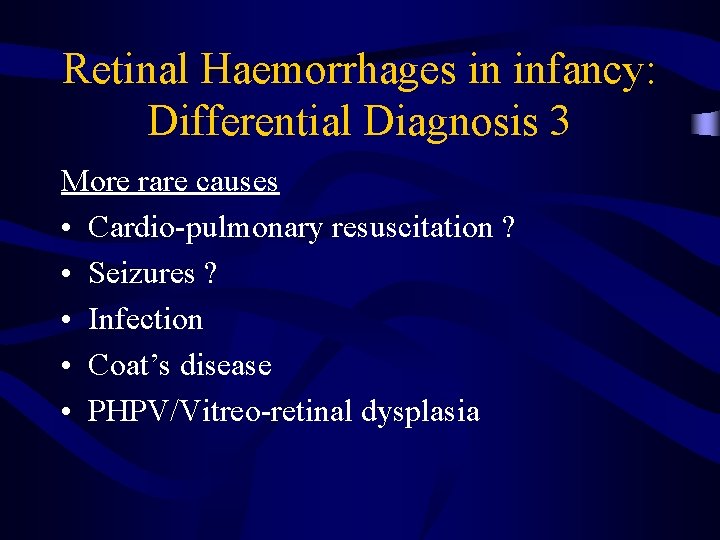
Retinal Haemorrhages in infancy: Differential Diagnosis 3 More rare causes • Cardio-pulmonary resuscitation ? • Seizures ? • Infection • Coat’s disease • PHPV/Vitreo-retinal dysplasia
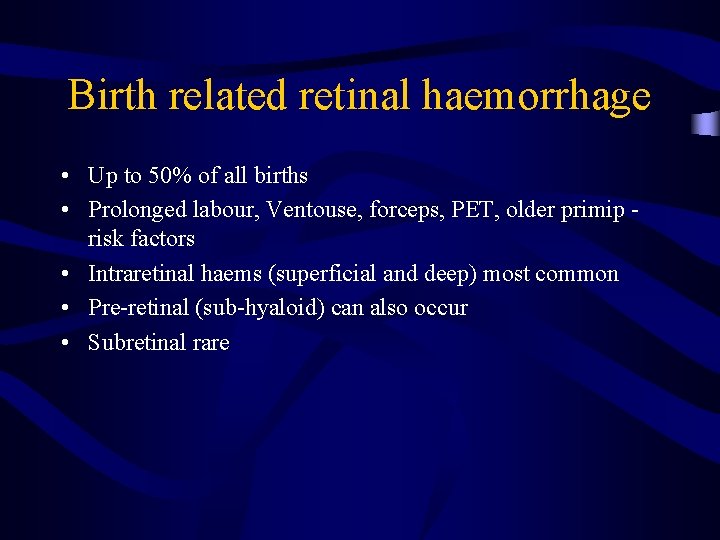
Birth related retinal haemorrhage • Up to 50% of all births • Prolonged labour, Ventouse, forceps, PET, older primip risk factors • Intraretinal haems (superficial and deep) most common • Pre-retinal (sub-hyaloid) can also occur • Subretinal rare
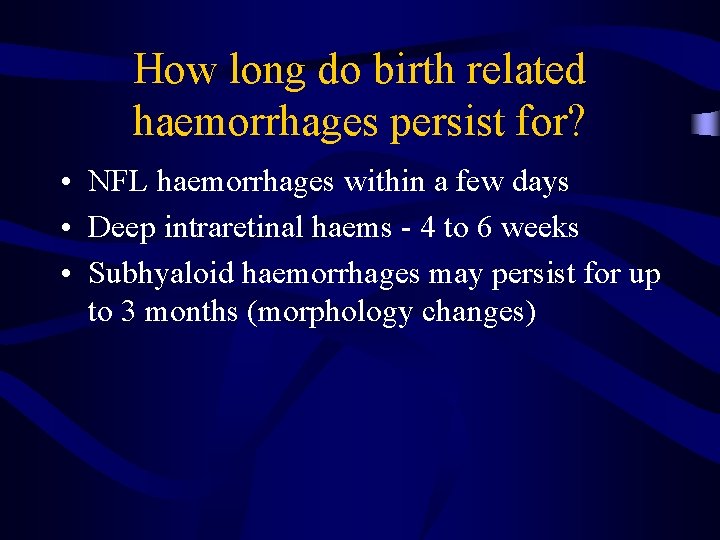
How long do birth related haemorrhages persist for? • NFL haemorrhages within a few days • Deep intraretinal haems - 4 to 6 weeks • Subhyaloid haemorrhages may persist for up to 3 months (morphology changes)
NAI : Eye Signs • Intraocular or periocular trauma occurs in approximately 40% of abused infants • Retinal haemorrhages are the most common ocular injury • Around 80% of infants with significant intracranial injuries will have retinal haemorrhages
NAI : Eye Injuries • • Nerve fibre layer haemorrhages Intraretinal haemorrhages Preretinal haemorrhages Vitreous haemorrhages Retinoschisis Perimacular folds Subretinal/Choroidal haemorrhage Optic nerve sheath haemorrhages
What is the typical pattern of retinal haemorrhages in NAI? • Posterior pole (? venous mechanism) • Peripheral retina (? tractional) • If exceed 20 -30% of retina – ? ? indicator of very violent shaking (Betz)
Can NAI cause unilateral retinal haemorrhages? • Yes – several papers confirm this • Haemorrhages in NAI often highly asymmetrical • But…unilateral posterior pole haemorrhages described after accidental head trauma
Are any ocular findings absolutely pathognomonic of child abuse? • NO! • But – extensive peripheral retinal haemorrhages, perimacular folds, haemorrhagic retinal cysts and traumatic retinoschisis point strongly to child abuse rather than accidental trauma
Accidental injury and retinal haemorrhages • Remains area of controversy • Rarely after severe accidental injury (which usually also causes skull fractures and adjacent intracranial damage) • Confined to posterior pole • Often unilateral and ipsilateral to side of intracranial bleed
Retinal haemorrhages and metabolic disease • Galactosaemia-vitreous haemorrhages described in severe cases • Glutaric aciduria – subdural and retinal haemorrhages described – infants present with neurodevelopmental delay, cerebral atrophy, dystonia and dyskinesia
Retinal haemorrhage and intracranial vascular malformation • Ruptured subarachnoid vascular malformations are very rare in children under 3 years old • Associated optic nerve sheath haemorrhage described in 7 week old (Weissgold et al Surv Ophthalmol 39(6)1995) • Little other evidence of Terson’s syndrome in infants
Retinal haemorrhages in leukaemia (AML, ALL) • • • Very common in leukaemic children Usually posterior pole Any layer Tortuous retinal veins/cotton wool spots Look for infiltration of eye/uveitis – ‘sanctuary site’ - sign of CNS disease
Retinal haemorrhages and blood disorders • • • Juvenile pernicious anaemia Aplastic anaemia Megaloblastic anaemia Malaria Protein C deficiency Hyperviscosity syndromes All extremely rare and unlikely to cause haemorrhages in infancy - involve specialist paediatric haematologist where doubt
Can Cardio-Pulmonary Resuscitation cause retinal haemorrhages? • Single case reports – NAI not adequately excluded • Larger studies (169 cases, 45 cases) suggest CPR alone is very unlikely to cause retinal haemorrhages even if carried out by unskilled individuals
Can Epileptic fits cause retinal haemorrhages? • 2 large studies ( 560 adults, 33 children) suggest not • 1 case report of premature infant at 23 days Conclusion • Very rarely if ever
Infection and retinal haemorrhage • • • Meningococcal meningitis CMV HSV VZV Toxoplasmosis Look for areas of retinal necrosis, systemic signs of infection, immunocompromise
Other aetiologies • Coats’ – rare, unilateral retinal telangiectasia • PHPV (PFV) – usually unilateral, microphthalmic/cataract – posterior form may present with retinal detachment/bleeding • Retinal dysplasia – retinal folds/gliosis/bleeding (Norrie’s, Trisomy 13 -15, Meckel-Gruber and other $)