Rethinking Obesity Anna Cowell James OConnell Aintree Weight
Rethinking Obesity Anna Cowell James O’Connell Aintree Weight Management Team
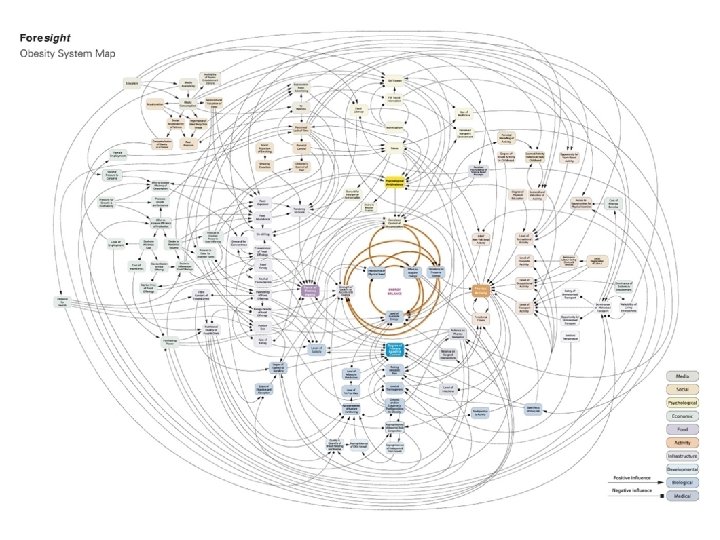
Aims & Objectives • To Provide an update on current obesity statistics. • To consider reasons for obesity epidemic. • To consider what works and what doesn’t at primary care level. • To provide an update on Bariatric surgery as a treatment option for obesity.
Obesity statistics (2015/16) • 58% of women and 68% of men were overweight or obese. • Obesity prevalence increased from 15% in 1993 to 27% in 2015. • Over 1 in 5 children in Reception, and over 1 in 3 children in Year 6 were measured as obese or overweight. • 525, 000 admissions in NHS hospitals where obesity was recorded as a factor. • Obesity costs the NHS £ 6, 000, 000 per year.

How Do We Treat Obesity?
Weight Stigma • • • Children with obesity experience a 63% higher chance of being bullied. 54% of adults stigmatised by colleagues. 69% of adults experiences of stigmatisation from health care professionals. All party parliamentary group report May 2018 • 88% of people with obesity have been stigmatised, criticised or abused as a result of their obesity. • 94% believe that there is not enough understanding about the causes of obesity amongst the public, politicians and other stakeholders. • More than one third of people with obesity have not accessed any lifestyle or prevention services. • 42% of people with obesity did not feel comfortable talking to their GP about their obesity.
Current Approach Obesity Eat Less Move More

Student Population • • • Body image, new relationships? First time away from home New city Isolated Stress – assessments exams, Job vs study balance
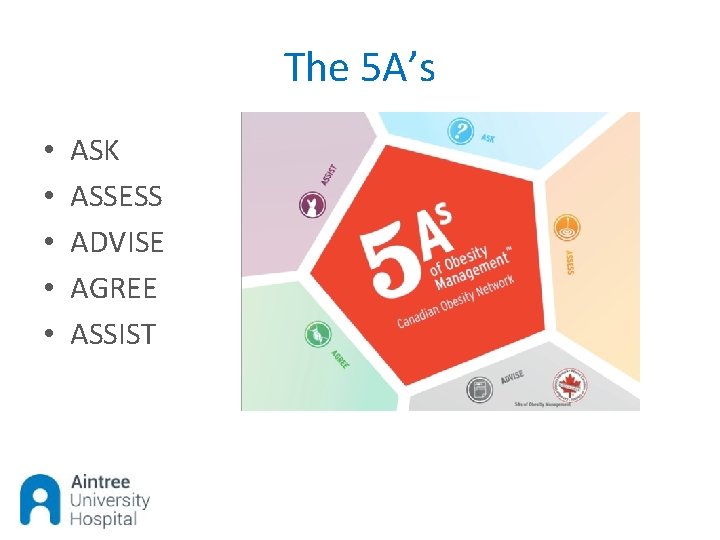
The 5 A’s • • • ASK ASSESS ADVISE AGREE ASSIST

Resources
Summary • • Challenge weight stigma Try to be non judgemental when dealing with weight issues Eat less move more advice doesn’t work Weight is a complex issue Use compassion and empathy Set goals away from weight Know your local services Refer to specialist services when appropriate ‘if you want things to change, you first have to change YOU’

BARIATRIC SURGERY
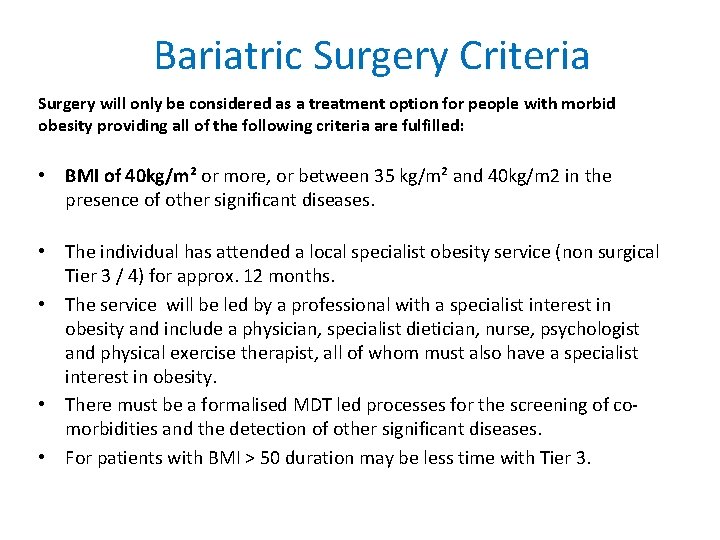
Bariatric Surgery Criteria Surgery will only be considered as a treatment option for people with morbid obesity providing all of the following criteria are fulfilled: • BMI of 40 kg/m² or more, or between 35 kg/m² and 40 kg/m 2 in the presence of other significant diseases. • The individual has attended a local specialist obesity service (non surgical Tier 3 / 4) for approx. 12 months. • The service will be led by a professional with a specialist interest in obesity and include a physician, specialist dietician, nurse, psychologist and physical exercise therapist, all of whom must also have a specialist interest in obesity. • There must be a formalised MDT led processes for the screening of comorbidities and the detection of other significant diseases. • For patients with BMI > 50 duration may be less time with Tier 3.
NHS Surgical Options
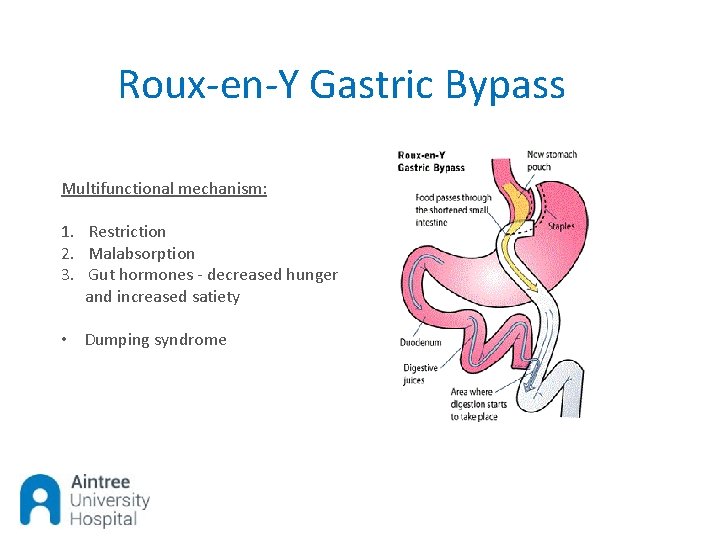
Roux-en-Y Gastric Bypass Multifunctional mechanism: 1. Restriction 2. Malabsorption 3. Gut hormones - decreased hunger and increased satiety • Dumping syndrome
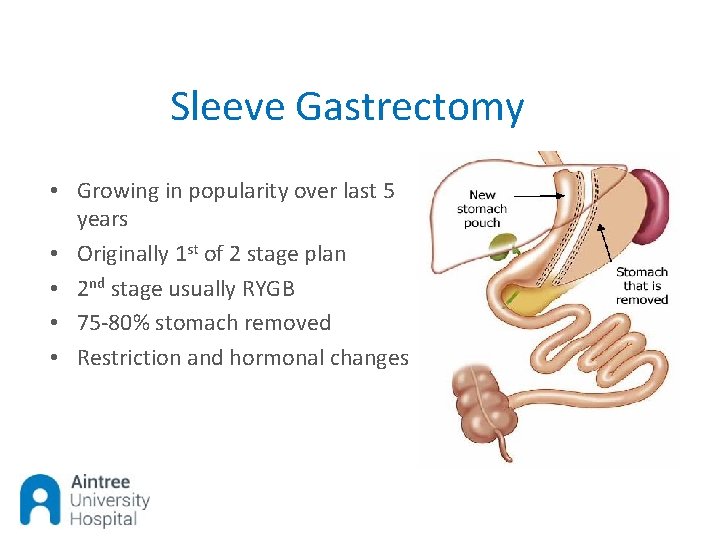
Sleeve Gastrectomy • Growing in popularity over last 5 years • Originally 1 st of 2 stage plan • 2 nd stage usually RYGB • 75 -80% stomach removed • Restriction and hormonal changes
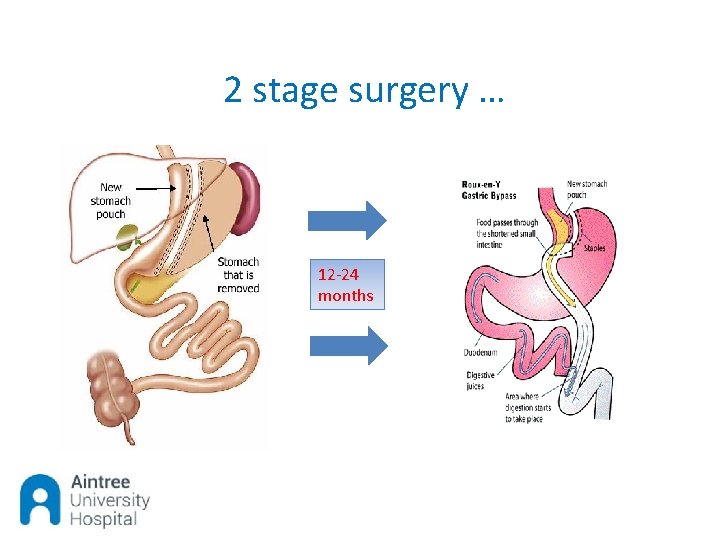
2 stage surgery … 12 -24 months
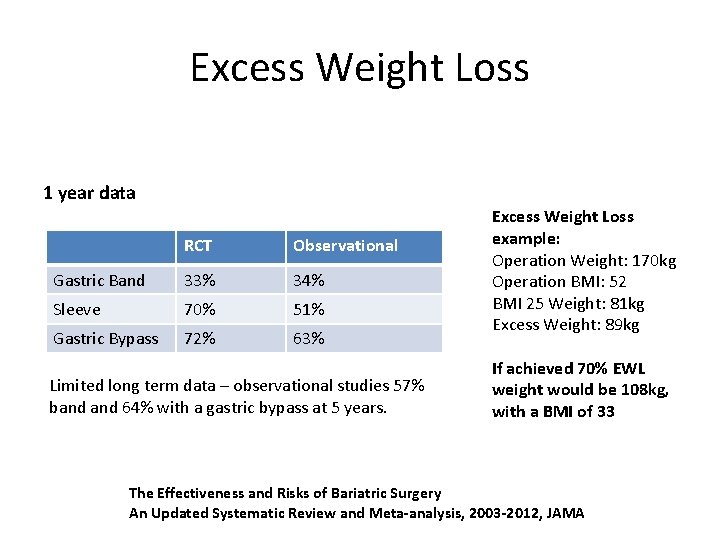
Excess Weight Loss 1 year data RCT Observational Gastric Band 33% 34% Sleeve 70% 51% Gastric Bypass 72% 63% Limited long term data – observational studies 57% band 64% with a gastric bypass at 5 years. Excess Weight Loss example: Operation Weight: 170 kg Operation BMI: 52 BMI 25 Weight: 81 kg Excess Weight: 89 kg If achieved 70% EWL weight would be 108 kg, with a BMI of 33 The Effectiveness and Risks of Bariatric Surgery An Updated Systematic Review and Meta-analysis, 2003 -2012, JAMA
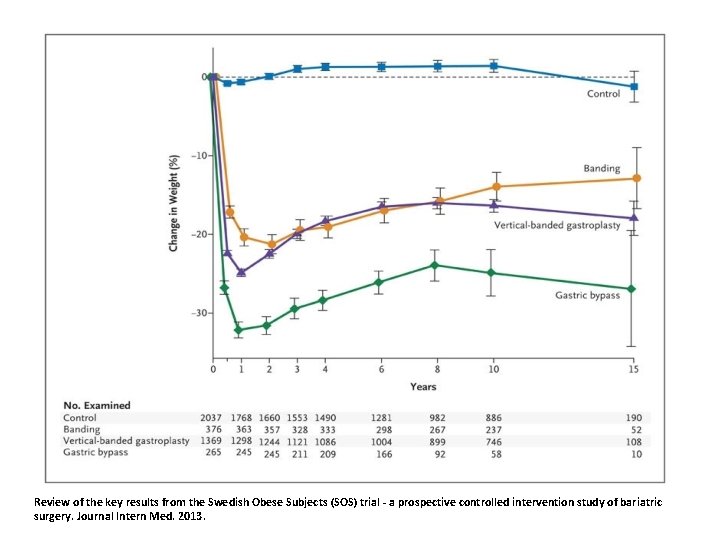
Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. Journal Intern Med. 2013.
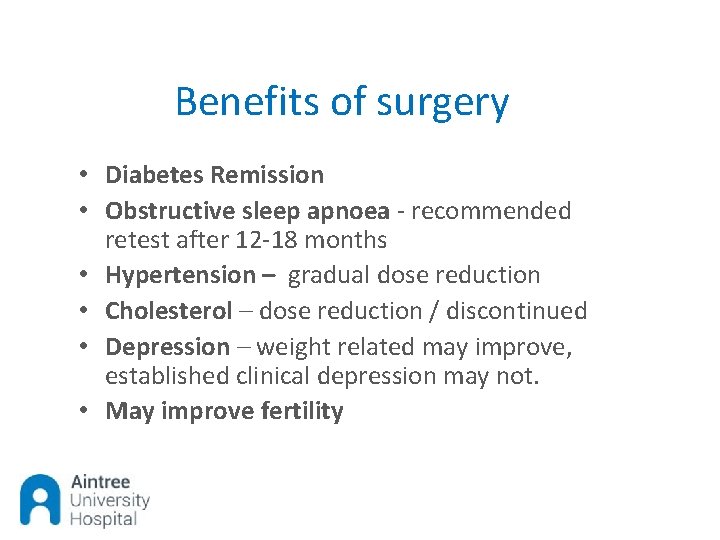
Benefits of surgery • Diabetes Remission • Obstructive sleep apnoea - recommended retest after 12 -18 months • Hypertension – gradual dose reduction • Cholesterol – dose reduction / discontinued • Depression – weight related may improve, established clinical depression may not. • May improve fertility
Common issues after surgery • • Hair thinning General dizziness Ulcers – risk increased further if smoking Gallstones Body dysmorphia Excess skin Vitamin and mineral deficiencies
References • • • http: //www. euro. who. int/__data/assets/pdf_file/0017/351026/Weight. Bias. pdf? ua=1 https: //www. obesityappg. com/inquiries https: //assets. publishing. service. gov. uk/government/uploads/system/uploads/attachme nt_data/file/287937/07 -1184 x-tackling-obesities-future-choices-report. pdf http: //www. obesitynetwork. ca/5 As https: //www. england. nhs. uk/wp-content/uploads/2016/05/appndx-7 -obesity-surgeryguid. pdf http: //www. by-band-sleeve. bristol. ac. uk/
Any Questions ?
- Slides: 23