Retained Objects What we know what we are
Retained Objects: What we know, what we are learning Diane Rydrych Division of Health Policy MN Department of Health
Overview ¬ How common are RFO nationally? ¬ How common are RFO in MN? ¬ What does MN data show? ¬ Why do RFO happen?
RFO as a national issue ¬Rates difficult to come by – 1/19, 000? – 1/6, 000? ¬Mortality also unclear – Estimates range from 11% - 35%
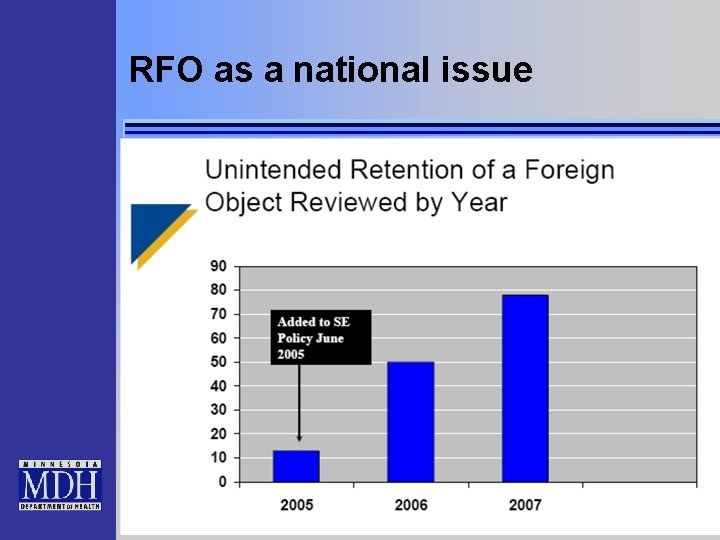
RFO as a national issue
RFO as a national issue ¬CT: 52 (3 years) ¬NJ: 58 (3 years) ¬NY: ~100/year ¬IN: 23 (2006) ¬MD: 6/year ¬PA: 60/year ¬ Note: not all include L&D
Risk Factors for RFO ¬NEJM 2003: – Emergency surgery – Unexpected change in procedure – Higher mean BMI – No sponge/ instrument counts
Risk Factors for RFO ¬Multiple changes in surgical team ¬Multiple procedures ¬Miscommunication ¬Incomplete wound explorations ¬Incorrect count unresolved
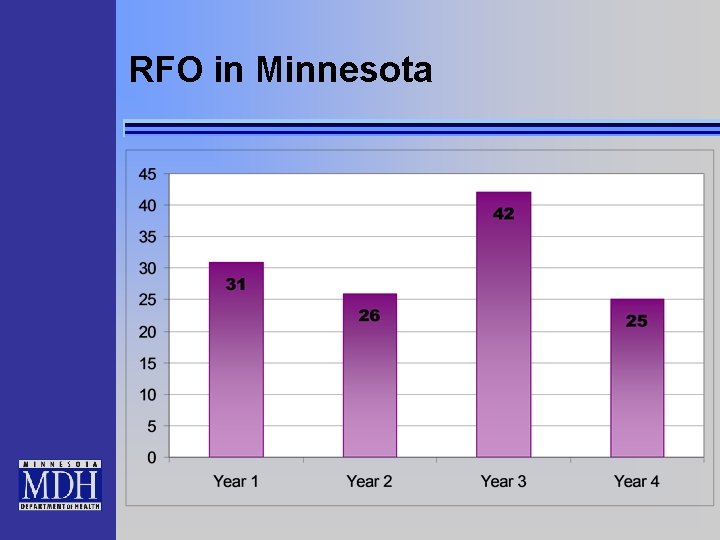
RFO in Minnesota
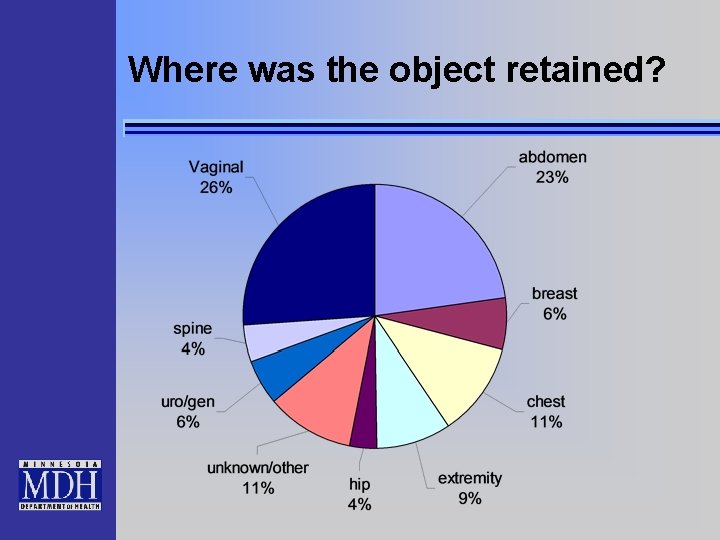
Where was the object retained?
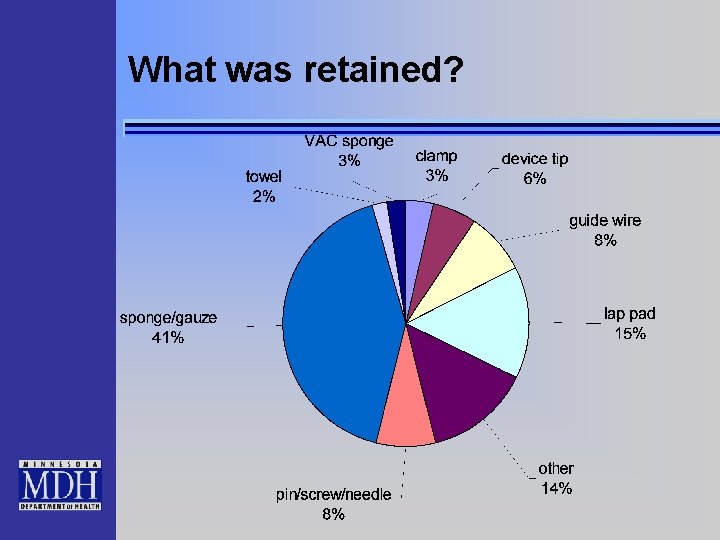
What was retained?
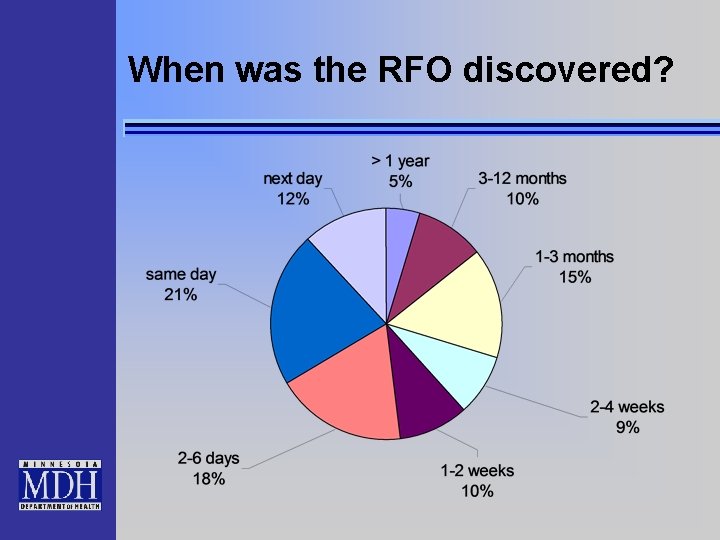
When was the RFO discovered?
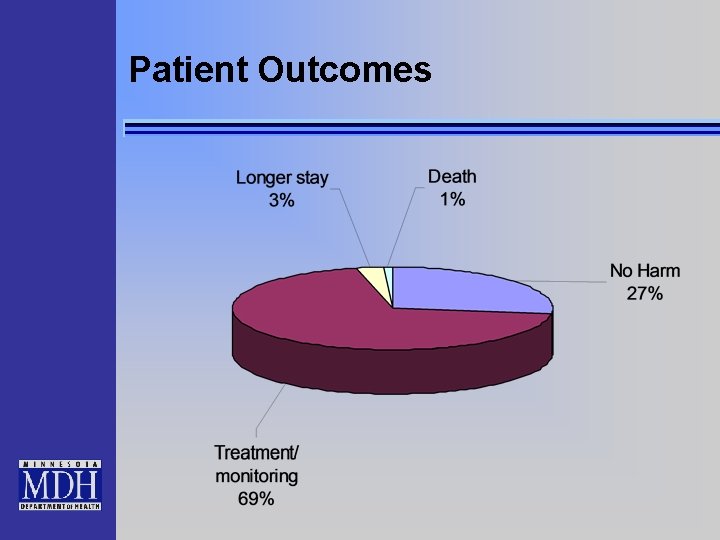
Patient Outcomes
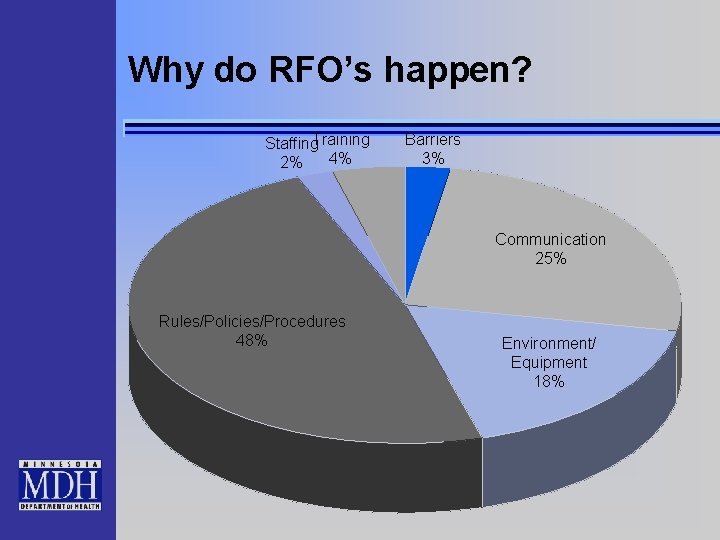
Why do RFO’s happen? Staffing. Training 4% 2% Barriers 3% Communication 25% Rules/Policies/Procedures 48% Environment/ Equipment 18%
Why do RFO’s happen? ¬Communication – Circulator believed counts were done in her absence – Number of VAC sponges in wound cavity not communicated – Circulator’s count was off; nurse didn’t communicate to MD until after a second count was also off – MD & rep knew of potential complication of pin retention; did not communicate to team
Why do RFO’s happen? ¬Communication – No visual cue in OR to indicate sponges placed or need to perform count – No prompt in EHR for sponge count completion – Some items not communicated/tallied when placed – Lack of clarity in x-ray requests
Why do RFO’s happen? ¬Rules/Policies/Procedures – “Sharp end” staff not involved in policy development – Not clear to nursing when to ask question about whether all sponges were removed – Policy not clear on process for counting; staff differ in approach – Unclear who should call for count – No policy to count VAC sponges placed or removed
Why do RFO’s happen? ¬Organizational Culture – many physicians do not take the pause seriously, therefore some staff are not taking the pause seriously – Staff acceptance of peers not following policy
Why do RFO’s happen? ¬Labor & Delivery – No policy for sponge counts – Reliance on provider vigilance – Inconsistent policy b/t surgery & OB – No one accountable for placement/removal of electrodes – Long tail sponges not used in L&D; 4 x 4’s harder to visualize – Many distractions after NSVD (family members, repair, etc)
What are we doing about it? ¬Training ¬Expand count policies to L&D ¬Improve count processes ¬Reconcile ALL objects ¬Improve documentation ¬New technology – Barcoding, scannable sponges, tailed sponges
- Slides: 20