RESTRAINTS Last Resort Not First Resort Competency for

- Slides: 46

RESTRAINTS Last Resort, Not First Resort Competency for RN’s Top 15 Health System
Definitions v v v Restraint: Any manual method, physical, or mechanical device, material, or equipment that immobilizes or reduces the ability of a patient to move his or her arms, legs, body or head freely. Restraint for Management of Violent Behavior: Used when patients display violent, aggressive or assaultive behavior to protect the patient against injury to self or others. Violent selfdestructive behavior jeopardizes the immediate physical safety of the patient, a staff member or others. Restraint for Management of Non-Violent Behavior: A restraint is the use of a physical device to restrict an individual’s movement, physical activity or normal access to his/her body, material or equipment attached or adjacent to the patient’s body. Top 15 Health System
Definitions v v Medication as a Restraint: A medication when it is used as a restriction to manage the patient’s behavior or restrict the patients’ freedom of movement is not a standard treatment or dosage for patient’s condition. Drugs that compromise a patient’s regular medication regimen are not considered a chemical restraint, even if their purpose is to control ongoing behavior. Adaptive/Supportive Device: Device used for postural support, to assist with, maintain, or enhance normal body functioning or to compensate for a specific physical deficit. The care of the patient and specific use of the device should follow customary care practices, patient plan of care or clinical pathway. Top 15 Health System
Examples of adaptive/supportive devices v v v v v Lap Belt (when the patient is able cognitively and physically to remove) Transfer belts (when the patient is able cognitively and physically to remove) Mitts – not pinned or tied down to the bed. The plastic buckle must be on the bottom side of the wrist. Orthopedic appliances or braces Wheelchairs (with or without seat belts) Bed side rails when used to assist in position changes Wedge cushion Kerlix rolls Geri-chairs that patient can release Bedside table Top 15 Health System
Medical Immobilization v v Mechanisms usually and customarily employed during medical, diagnostic or surgical purposes that are considered a regular part of such procedures. The purpose of medical immobilization is to prevent the patient from interrupting necessary medical, diagnostic or surgical procedures. Without medical immobilization, the patient may sustain greater harm. Examples of medical immobilization (but not limited to): Ø Ø Ø Body immobilization during surgery Arm board during IV therapy Papoose Cast Traction Adult protective sleeve Top 15 Health System Gait Belts are not considered a restraint when used to ambulate patients
Human Physical Restraint/Hold v Holding a patient in a manner that restricts his or her movement against the patients will is considered a restraint and the restraint policy will be followed to include the one hour face-to-face evaluation (i. e. physically holding a patient to give a forced psychotropic medication). Top 15 Health System
Should Alternatives to Restraints be Attempted? v Alternatives to restraints will be attempted and documented prior to initiation of restraints. Examples include: Ø Having a family member sit with the patient Ø Provide reality orientation when appropriate Ø Provide a quiet environment, change lighting, etc. Ø Comfort measures such as position changes or medication for pain Ø Patient attendant for continuous monitoring Ø Medication changes (example: if medications alter patients level of consciousness) Ø Assess bowel/bladder function Ø Does the patient have hearing aid and glasses? Top 15 Health System
Ø Ø Ø Diversional/physical activities such as folding linen, playing board/card games, etc. (activity box located on each nursing unit) Mitts (padded/unpadded) not pinned/tied down Posture belt Chair sitters View life sharing videos on TIGR: 13 videos available that provides songs, memories, and interaction for confused geriatric patients (Spanish and African American Heritage included) Top 15 Health System
What are the Restraint Devices Available at GCH? v v v v The least restrictive restraint device is to be utilized when a restraint is needed for patient safety. The following are restraint devices in order of restrictiveness: Side rail wedge and/or 3 -4 side rails up when specifically used as a restraint for the patient Transfer belt – if patient unable to remove on own Mitts – if pinned or tied down Soft restraints (wrist/ankle) 1: 1 Sitter (violent behavior restraint only) Lock and Key (violent behavior restraint only) If a patient falls do not consider using restraint and seclusion as routine part of fall prevention Top 15 Health System
Criteria for Utilizing Restraints v Violent Behavior Restraint: Ø Immediate serious risk of harm to self or others Ø Threat to safety of property or environment v Non-Violent Behavior Restraint: Ø Patient attempting to do something to his/her treatment site and/or interfering with clinically necessary medical surgical interventions/devices (i. e. pulling tubes, picking incision) Ø May include situation where the patient is unable to maintain balance or ambulate safely AND seek assistance Top 15 Health System
Policy Exclusions to Restraints? v v Medical Immobilization. Adaptive/Supportive Devices. Anesthetized patients regardless of location, during the acute recovery phase. “Acute recovery phase is defined as that period of time after completion of any invasive or surgical procedure requiring anesthesia, during which the patient is awaking from the sedating or anesthetizing medication and is unable to appropriately respond to commands/instruction. ” Forensic cases (police prisoners) who are restrained/shackled by law enforcement agency personnel although patient rights/dignity and safety must be respected and maintained. Top 15 Health System
v v v v Physical comforting of children or adolescents for a period of time less than 30 minutes. Side rails utilized for postural support or to assist patients with turning from side to side. Side rails utilized on stretchers or during transport. Side rails on specialty beds based on manufacturer’s recommendation as a patient safety component. Side rails in bassinets, warmers, or cribs. Side rails necessary to maintain safety of developmentally disabled or comatose patients. Padded side rails utilized for safety for patients on seizure precautions. Top 15 Health System
How is a Patient in Restraints to be Transported? v If a patient is in restraints and is transported off the floor, the RN will give report to an RN in the other department who will accept responsibility for the monitoring and documentation. If an RN is not available to monitor and document when the patient is in restraints, the assigned staff is to accompany the patient while the patient is off the unit. The RN is to monitor the patient and document on the appropriate restraint flowsheet (Non-Violent Behavior and Violent Behavior). Top 15 Health System
Patients in Restraints during Evacuation v If a patient is in restraints when a fire alarm sounds and/or internal disaster is announced: Ø The patient should be given an explanation regarding the situation in a calm and supportive manner. Ø The assigned staff member must remain with the patient who is restrained at all times, unless directed by administrative management. Ø The Clinical Nurse Manager/Nursing Supervisor/Designee RN must assess the patient and determine the number of additional staff needed if the patient must be removed from restraints and taken to a safe area. If the patient must be removed from restraints the patient must remain under 1: 1 supervision by the assigned staff unless the circumstances that justified the use of restraints no longer exist and the physician or RN discontinue the restraints. Top 15 Health System
Non-Violent Behavior Restraints v v For non-violent behavior restraints, the RN must contact the physician prior to application of the restraint for an order. In emergency situations, order can be obtained either during emergency application or immediately (without interval) after application. The physician is to perform a face-to-face evaluation within 24 hours for a new restraint order. The attending physician is notified of the non-violent restraint application within 12 hours by the nurse. The nurse will document that the physician was notified by checking the appropriate box on the restraint assessment flow sheet. If the clinical justification for the restraint continues, a physician re-order based on a face-to-face assessment is required at least every 24 hours to continue the non-violent restraint. Top 15 Health System
Required Documentation by RN for Non-Violent Behavior Restraints v The RN will assess the patient at application of the restraint and at least every 2 hours thereafter. Documentation of the restraint will be completed on the appropriate restraint flowsheet by completing the following sections: Ø Patient and/or family provided with information on reason for restraint and criteria for removal. Ø Date and time of restraint application Ø Alternatives used to modify behavior (check all that were attempted and found to be ineffective prior to application) • • • Companionship Comfort Environmental Diversionary Interference Other Top 15 Health System
Type of Restraints: Ø 3 -4 bed rails raised Ø Soft ankle or wrist Ø Mitt - if pinned or tied down Ø Posey Vest v Document attending physician notified of restraint within 12 hours. v Signs of injury associated with restraint application. v Documentation of patient assessment with initiation of restraint and every 2 hours by utilizing the key on the restraint flowsheet. v Top 15 Health System
v v v A care plan goal for patients with a restraint due to a nonviolent behavior reason is written on the restraint flowsheet. The care plan goal is to discontinue restraint as soon as possible when the patient behavior no longer interferes with medical treatment healing and is documented as such until alternative interventions are effective. Document the reason/continuation with each restraint reorder when the patient is in restraints. The nurse/physician is to discontinue the restraint order when the patients’ condition no longer warrants the restraint. Vital signs are taken on initiation or as soon as safety permits within 4 hours, then every 4 hours thereafter and with any acute change in patient condition. Top 15 Health System
Simultaneous use of Restraints and Seclusion v Simultaneous restraint and seclusion use is only permitted if the patient is continually monitored: Face-to-face by an assigned, trained staff member. Top 15 Health System
Policy on Violent Behavior Restraints v v The RN will contact the physician prior to the application of the restraint for an order. In emergency situations, an order can be obtained either during the emergency application or immediately (without interval) after application. The physician is to perform a face-to-face evaluation of the patient within 1 hour of application, even if the patient no longer needs restraints. The attending physician is immediately notified by the resident or intern to consult regarding the restraint order. The intern or resident documents the attending physician was contacted. If clinical justification for the restraint continues, the physician should be notified to receive a re-order (time limited) as follows: Top 15 Health System
v Adult: Order every 4 hours with physician face-to-face evaluation every 8 hours (every other order). v Adolescent: Order every 2 hours with face-to-face evaluation every 4 hours (every other order). v Child: Order every 1 hour with physician face-to-face evaluation every 2 hours (every other order). Top 15 Health System
Required documentation by RN for Violent Behavior Restraint v The RN will assess the patient at application of the restraint and ensure monitoring at least every 15 minutes thereafter. Documentation of the restraint will be completed on the “Restraint Flowsheet” by completing the following sections: Ø Patient and/or family provided with information on reason for restraint and criteria for removal. Ø Date and time of restraint application Ø Alternatives used to modify behavior (check all that were attempted and found to be ineffective prior to application) • • • Companionship Comfort Environmental Diversionary Interference Other Top 15 Health System
v v v Type of Restraints: Ø 3 -4 side rails raised Ø Soft ankle or wrist Ø Mitt if pinned or tied down Ø Lock and Key Ø Belt Ø 1: 1 continuous attendant Ø Physical Hold/Escort Signs of injury associated with restraint application (require documentation in the nursing notes). Documentation of patient assessment at least every 15 minutes by utilizing the key on the restraint flowsheet. Top 15 Health System
v v A care plan goal for patients with a restraint due to a violent behavior reason is written on the restraint flowsheet. The care plan goal is to discontinue restraint as soon as possible when the patient behavior no longer interferes with medical treatment healing and is documented as such until alternative interventions are effective. Document the reason the patient is in restraints. The nurse/physician is to discontinue the restraint order when the patients’ condition no longer warrants the restraint. The RN may assign a trained staff member to perform 15 minute monitoring. The RN must do the actual assessment with initial restraint and at least every 1 hour. Vital signs are taken on initiation or as soon as safety permits within 4 hours, then every 4 hours thereafter and with any acute change in patient condition. Top 15 Health System
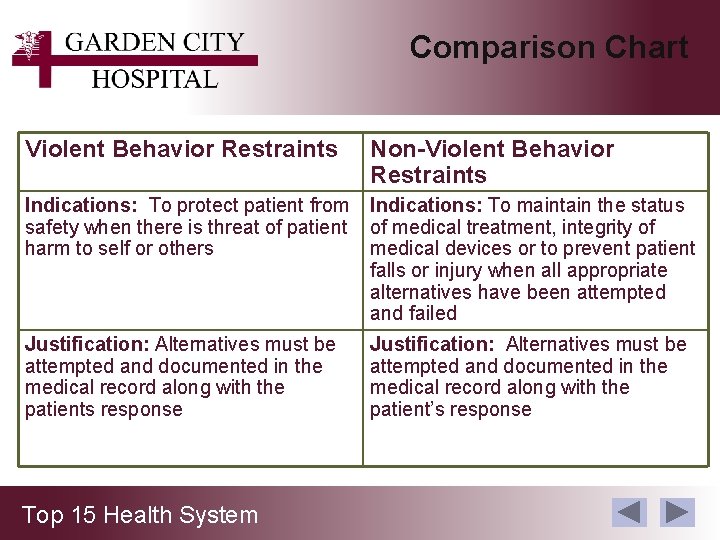
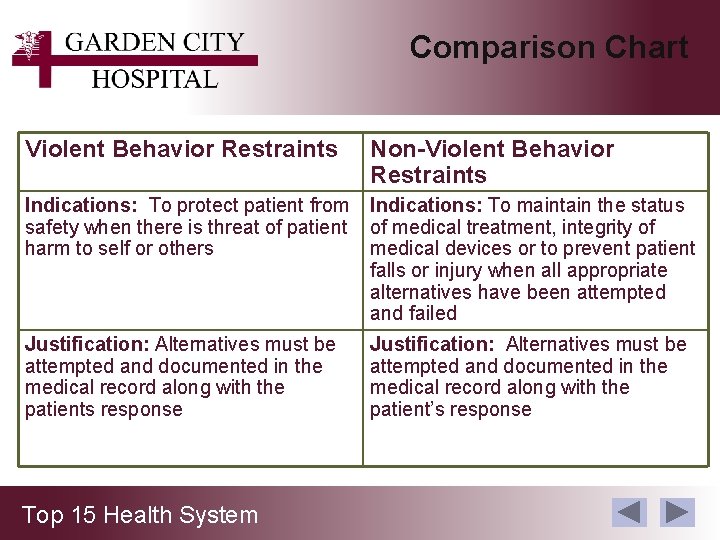
Comparison Chart Violent Behavior Restraints Non-Violent Behavior Restraints Indications: To protect patient from safety when there is threat of patient harm to self or others Indications: To maintain the status of medical treatment, integrity of medical devices or to prevent patient falls or injury when all appropriate alternatives have been attempted and failed Justification: Alternatives must be attempted and documented in the medical record along with the patients response Justification: Alternatives must be attempted and documented in the medical record along with the patient’s response Top 15 Health System
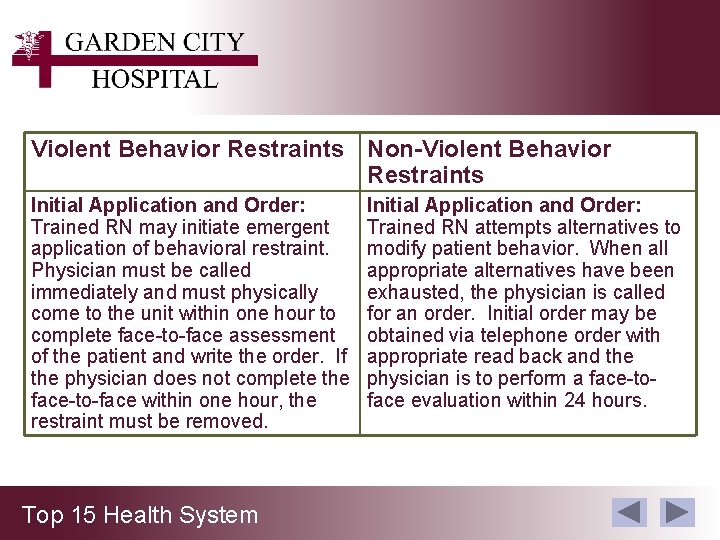
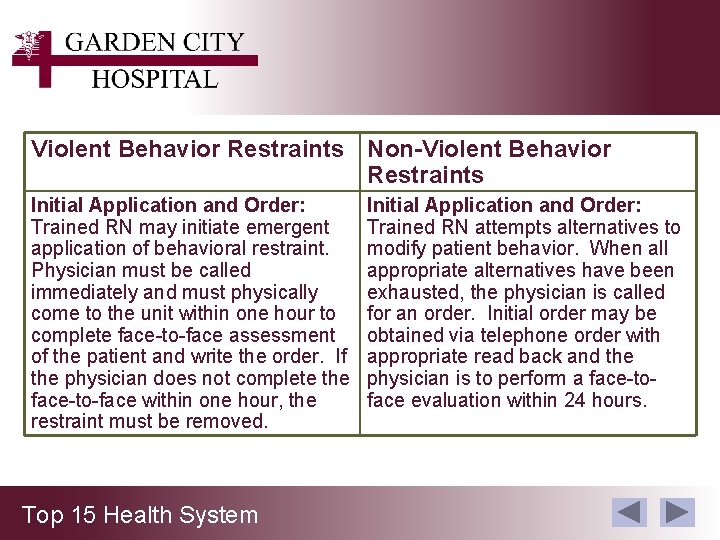
Violent Behavior Restraints Non-Violent Behavior Restraints Initial Application and Order: Trained RN may initiate emergent application of behavioral restraint. Physician must be called immediately and must physically come to the unit within one hour to complete face-to-face assessment of the patient and write the order. If the physician does not complete the face-to-face within one hour, the restraint must be removed. Top 15 Health System Initial Application and Order: Trained RN attempts alternatives to modify patient behavior. When all appropriate alternatives have been exhausted, the physician is called for an order. Initial order may be obtained via telephone order with appropriate read back and the physician is to perform a face-toface evaluation within 24 hours.
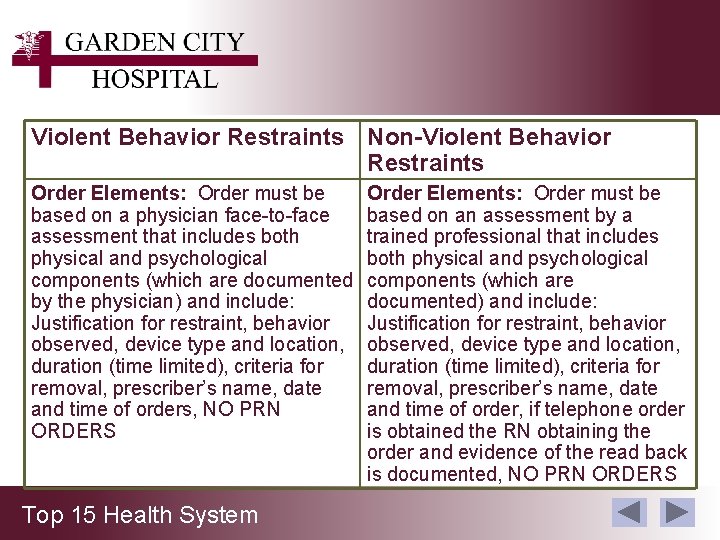
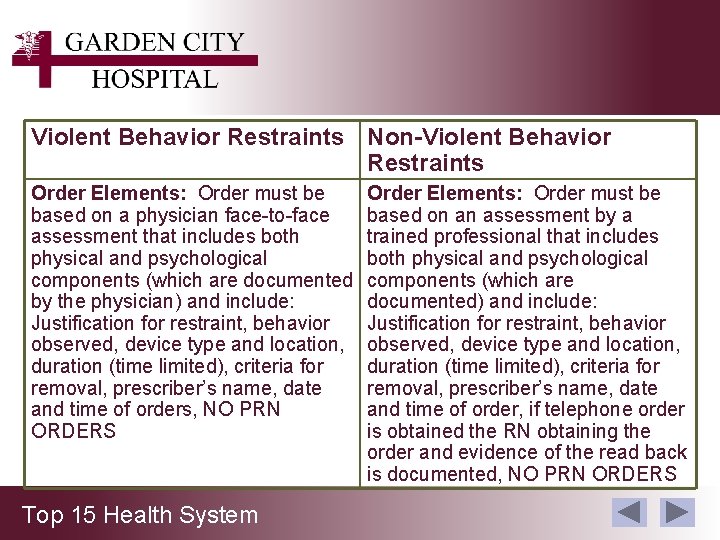
Violent Behavior Restraints Non-Violent Behavior Restraints Order Elements: Order must be based on a physician face-to-face assessment that includes both physical and psychological components (which are documented by the physician) and include: Justification for restraint, behavior observed, device type and location, duration (time limited), criteria for removal, prescriber’s name, date and time of orders, NO PRN ORDERS Top 15 Health System Order Elements: Order must be based on an assessment by a trained professional that includes both physical and psychological components (which are documented) and include: Justification for restraint, behavior observed, device type and location, duration (time limited), criteria for removal, prescriber’s name, date and time of order, if telephone order is obtained the RN obtaining the order and evidence of the read back is documented, NO PRN ORDERS
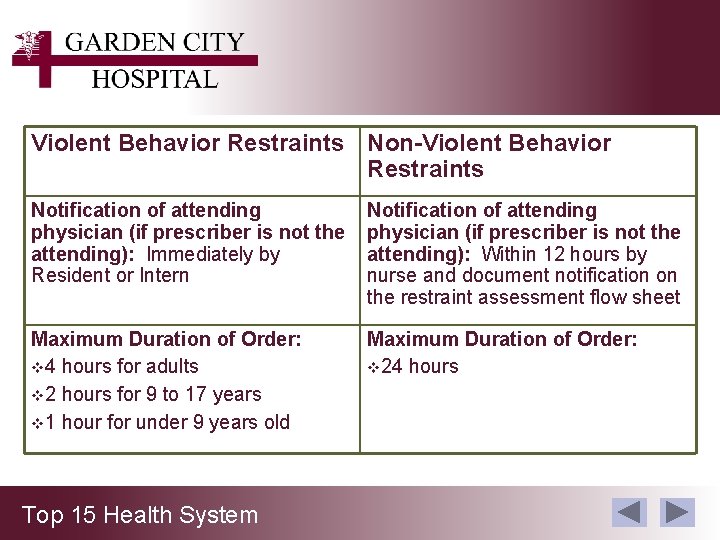
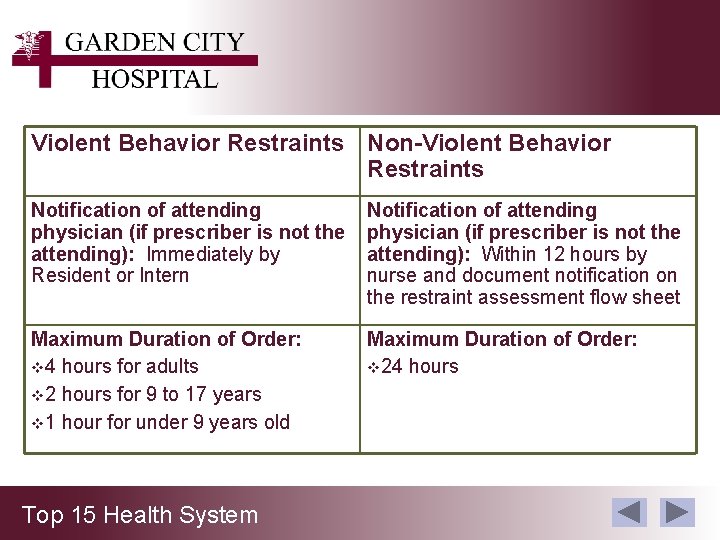
Violent Behavior Restraints Non-Violent Behavior Restraints Notification of attending physician (if prescriber is not the attending): Immediately by Resident or Intern Notification of attending physician (if prescriber is not the attending): Within 12 hours by nurse and document notification on the restraint assessment flow sheet Maximum Duration of Order: v 4 hours for adults v 2 hours for 9 to 17 years v 1 hour for under 9 years old Maximum Duration of Order: v 24 hours Top 15 Health System
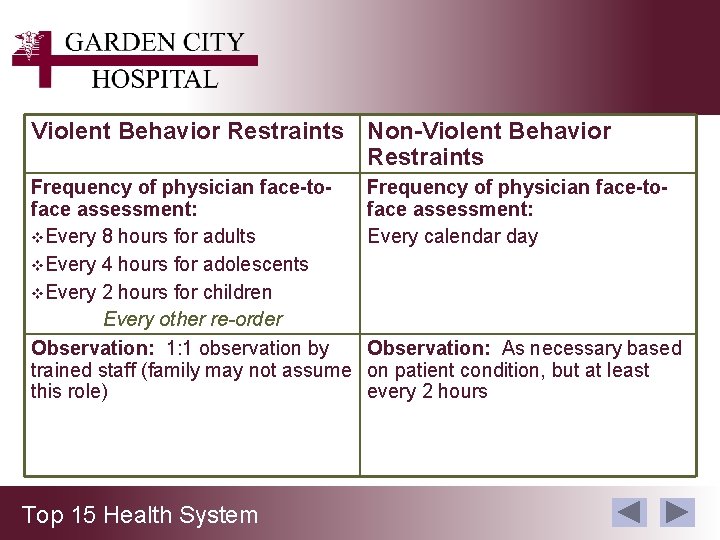
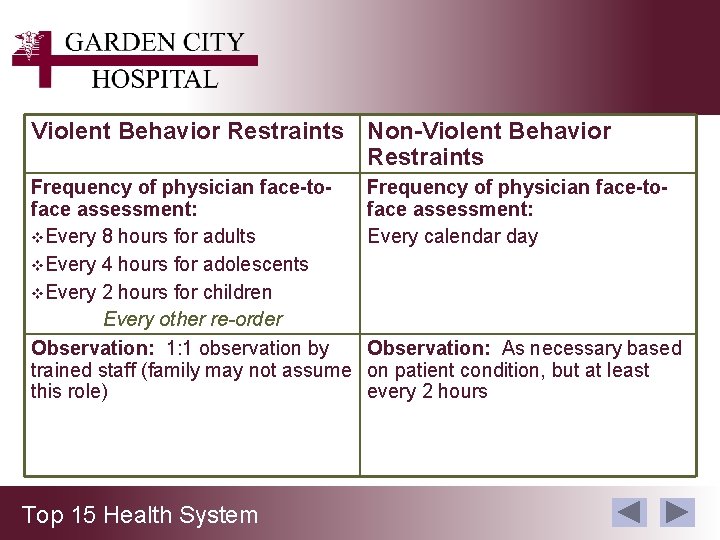
Violent Behavior Restraints Non-Violent Behavior Restraints Frequency of physician face-toface assessment: v. Every 8 hours for adults v. Every 4 hours for adolescents v. Every 2 hours for children Every other re-order Observation: 1: 1 observation by trained staff (family may not assume this role) Top 15 Health System Frequency of physician face-toface assessment: Every calendar day Observation: As necessary based on patient condition, but at least every 2 hours
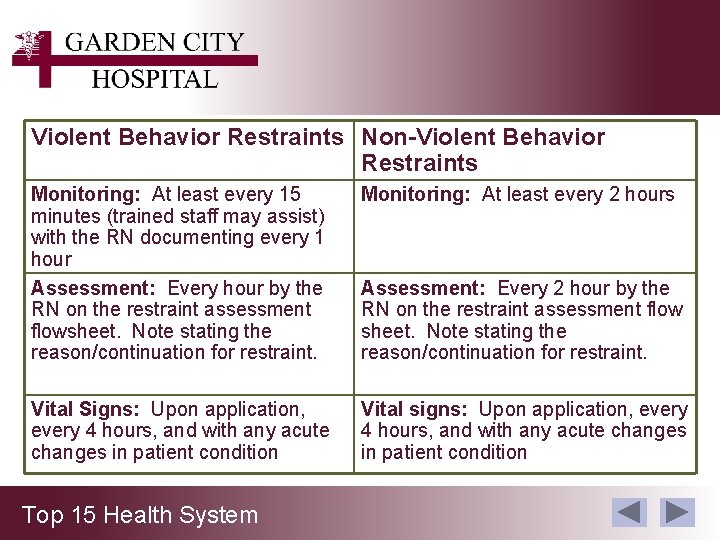
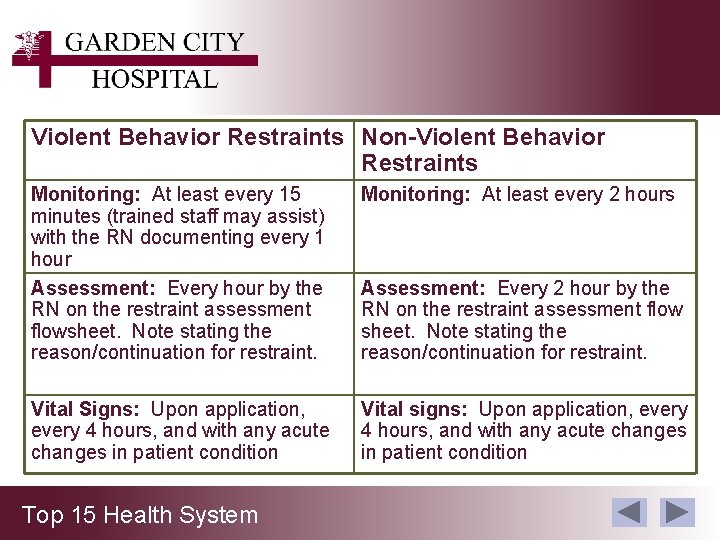
Violent Behavior Restraints Non-Violent Behavior Restraints Monitoring: At least every 15 minutes (trained staff may assist) with the RN documenting every 1 hour Assessment: Every hour by the RN on the restraint assessment flowsheet. Note stating the reason/continuation for restraint. Monitoring: At least every 2 hours Vital Signs: Upon application, every 4 hours, and with any acute changes in patient condition Vital signs: Upon application, every 4 hours, and with any acute changes in patient condition Top 15 Health System Assessment: Every 2 hour by the RN on the restraint assessment flow sheet. Note stating the reason/continuation for restraint.
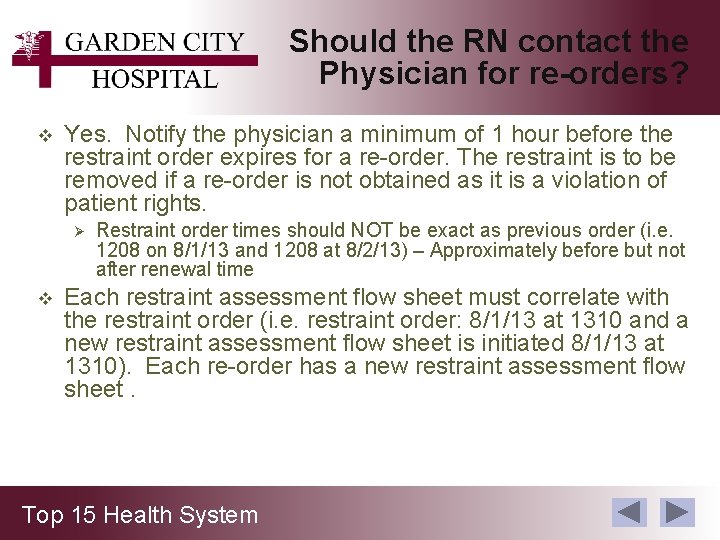
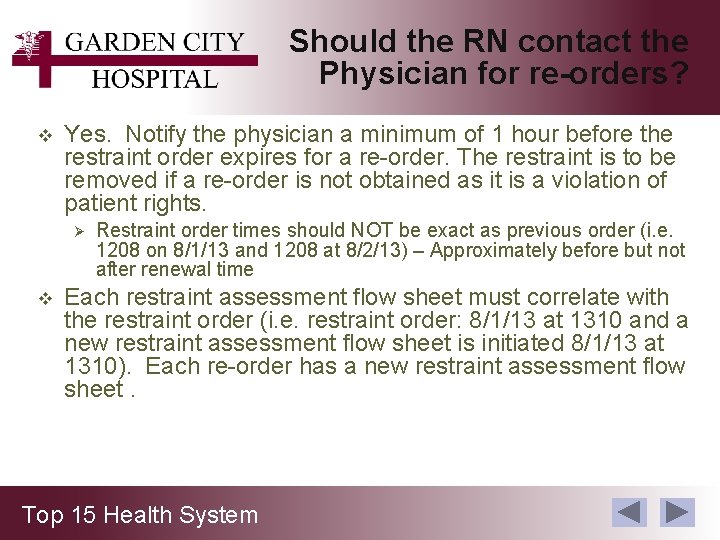
Should the RN contact the Physician for re-orders? v Yes. Notify the physician a minimum of 1 hour before the restraint order expires for a re-order. The restraint is to be removed if a re-order is not obtained as it is a violation of patient rights. Ø v Restraint order times should NOT be exact as previous order (i. e. 1208 on 8/1/13 and 1208 at 8/2/13) – Approximately before but not after renewal time Each restraint assessment flow sheet must correlate with the restraint order (i. e. restraint order: 8/1/13 at 1310 and a new restraint assessment flow sheet is initiated 8/1/13 at 1310). Each re-order has a new restraint assessment flow sheet. Top 15 Health System
Discontinued Restraints before the Order Expires v The nurse/physician is to discontinue the order when the patients’ condition no longer warrants the restraint. Top 15 Health System
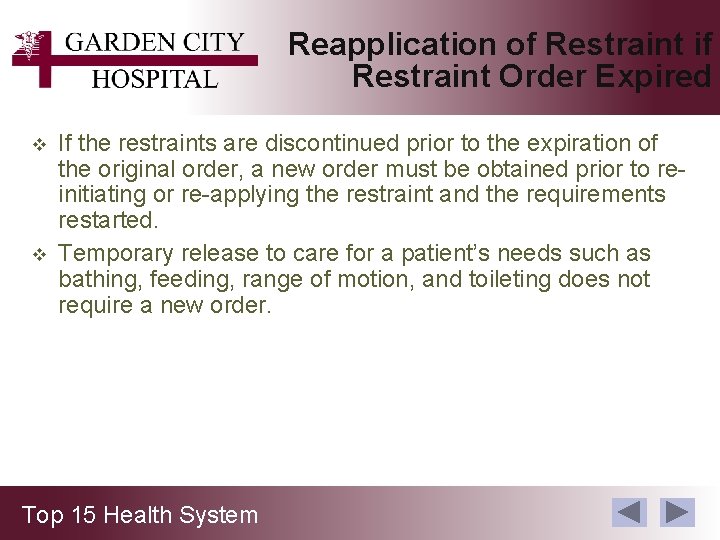
Reapplication of Restraint if Restraint Order Expired v v If the restraints are discontinued prior to the expiration of the original order, a new order must be obtained prior to reinitiating or re-applying the restraint and the requirements restarted. Temporary release to care for a patient’s needs such as bathing, feeding, range of motion, and toileting does not require a new order. Top 15 Health System
Educational Material Regarding Restraints for Patients and/or Families v v v Patient and/or family is to be provided with information regarding the reason for restraint and criteria for removal. A patient and family educational brochure is available on all nursing units. Documentation that restraint education was provided is to be completed on the restraint flowsheet. Top 15 Health System
Death Report Requirements Regarding Restraints v GCH will report deaths associated with the use of restraints to CMS. The following information will be reported: Ø Each death that occurs while the patient is in a restraint. Ø Each death that occurs within 24 hours after the patient has been removed from the restraint. Ø Each death known to the hospital that occurs within 1 week after restraint where it is reasonable to assume that use of restraint contributed directly or indirectly to the patient’s death. “Reasonable to assume” in this context includes, but is not limited to, deaths related to restrictions of movement for prolonged periods of time, or death related to chest compression, restriction of breathing or asphyxiation. Top 15 Health System
Roles for reporting to CMS v Staff role: Ø Identify if death occurred in the situations referenced above and notify Nursing Manager/Director or Nursing Supervisor v Nursing Managers/Directors during day shift and Nursing Supervisors role: Ø Complete the CMS restraint death notification form and fax it to Risk Management via the Hospital Restraint/Seclusion Death Report for CMS-Fax Sheet immediately following the patient’s death. Top 15 Health System
v Notify Risk Management of: Ø The patient’s name Ø Date of patient’s expiration Ø Time of patient’s expiration Ø Whether the death occurred: • While in Restraint/Seclusion • Within 24 hours of removal of Restraint/Seclusion • Within one week where Restraint/Seclusion contributed to the patient’s death Top 15 Health System
Nursing Required Document Regarding Restraints v v v v Each episode of Non-Violent Behavior Restraint or Violent Behavior Restraint use is documented in the patient’s medical record via Restraint flowsheet (as applicable) Document reason for restraint (minimally with each order and re-order) Document alternatives to restraints that were attempted and patient response Document the revision of the plan of care accordingly Discontinuation of restraint including the patient’s behavior reflecting improvement which supports the discontinuation shall be documented Initiatives to assist the patient meeting the criteria for discontinuation of restraints are documented Patient and/or family education regarding restraints Top 15 Health System
Criteria for Discontinuing Restraints v v v The patient will no longer interfere with medical therapy/healing The patient is not longer a threat to him/herself, staff, or others Document a note: Ø Date and time restraint was removed Ø Patient’s behavior reflecting improvement that supports the discontinuation Ø Initiatives used to assist the patient in meeting the criteria for discontinuation of restraints Top 15 Health System
Answers to FAQ’s v v v Justification for a restraint must match the restraint order (i. e. Soft wrist restraint order for patient pulling out lines – not a posey order) Patients with a restraint due to a violent reason are to be monitored every 15 minutes with documentation on the violent restraint flowsheet. The RN is to assess the patient and document on the violent restraint flowsheet at the initiation of the restraint and every 1 hour. The every 15 minute monitoring and documentation may be delegated to a trained PCA/TP 1: 1 sitter is not an alternative to a restraint. 1: 1 sitter is a form of restraint for violent behavior (i. e. Suicidal patient) Top 15 Health System
Answers to FAQ’s v v The RN is to assess the patient and document on the non -violent restraint flowsheet minimally every 2 hours. Confusion is not normal for an older adult. “Older adults are three times more likely to be restrained during an acute hospital admission than younger patients, even though this practice is associated with poor outcomes” (Said and Kautz, 2013). Restraints are not the best way to make sure a patient does not discontinue medical equipment. Alternatives should be implemented and documented. Restraints are not to be considered/utilized based on staff to patient ratios. Top 15 Health System
Answers to FAQ’s v v Confused patients should not be restrained so they won’t get hurt. Divers ional activities should be implemented. “Research over the past 20 years has repeatedly demonstrated that restraints don’t protect patients from falling, wandering, or removing tubes and other devices; in fact, they can exacerbate many problems, causing serious physical, emotional, and psychological problems” (Said and Kautz, 2013) Patient diagnosis does not indicate the need for restraints. Patient behavior should guide the consideration for restraints after alternatives to restraints are attempted and documented. Top 15 Health System
Are you Aware of the Adverse Effects of Physical Restraints? v Damaging consequence of using physical restraints include the following: Ø Ø Ø Functional decline Decreased peripheral circulation Cardiovascular stress Incontinence Muscle atrophy Pressure ulcers Infection Agitation Social isolation Confusion, depression, and fear Serious injuries, including fractures from falls Death from aspiration, restriction of breathing, and strangulation Top 15 Health System
Policy Regarding Non-Violent Behavior and Violent Behavior Restraints v Please refer to the GCH Clinical Practice Manual or policies on the GCWeb: Section Safety/Infection Control, for complete information regarding restraints. Top 15 Health System
References v v v Said, A. , and Kautz, D. (2013). “Reducing restraint use for older adults in acute care” Nursing 2013. Center for Medicare and Medicare (CMS) Healthcare Facilities Accreditation Program (HFAP) Top 15 Health System
v This completes the Restraint module. v Please take the post-test. Top 15 Health System