Respiratory System Respiratory Function What do cells need

- Slides: 47
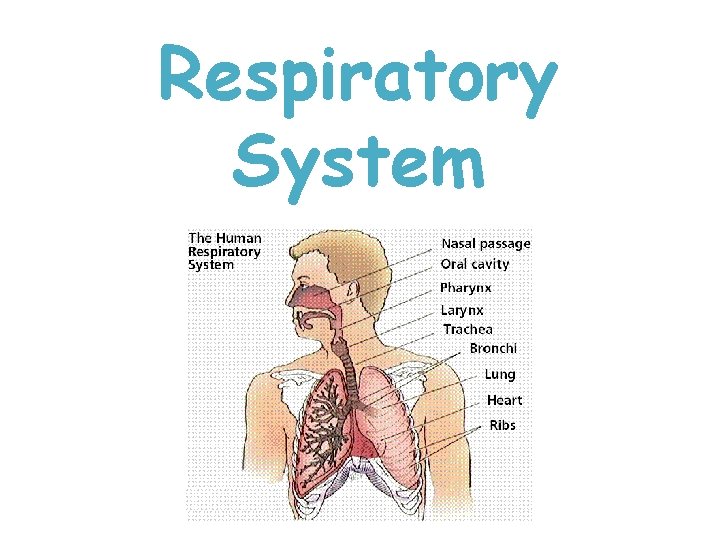
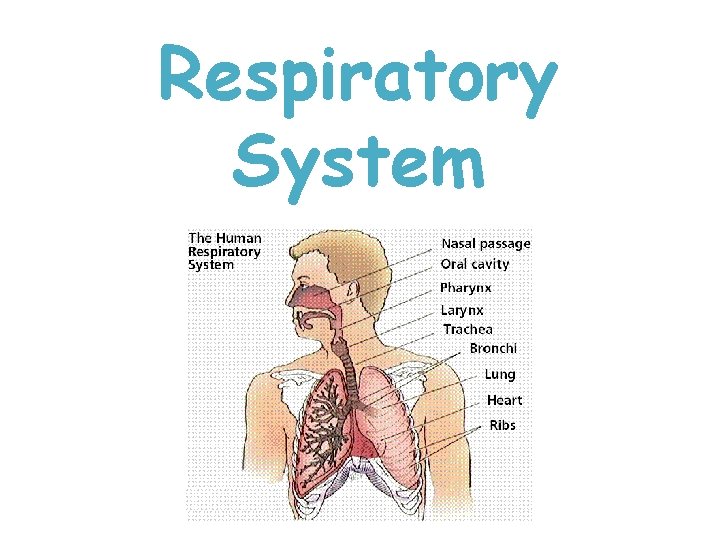
Respiratory System
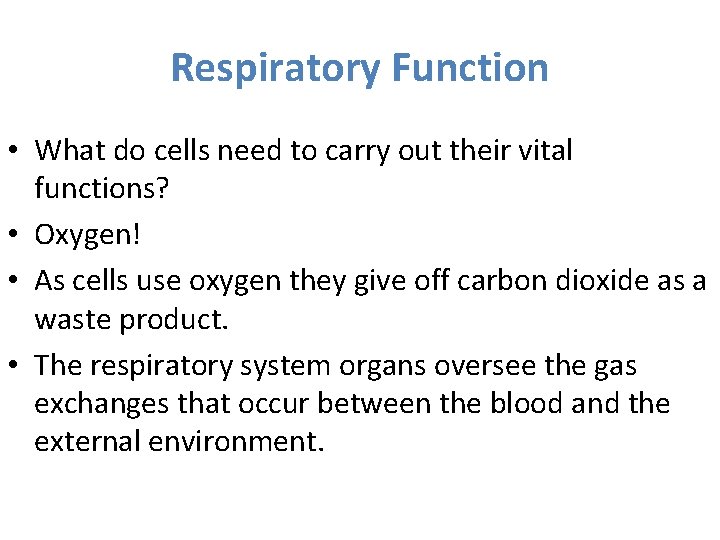
Respiratory Function • What do cells need to carry out their vital functions? • Oxygen! • As cells use oxygen they give off carbon dioxide as a waste product. • The respiratory system organs oversee the gas exchanges that occur between the blood and the external environment.

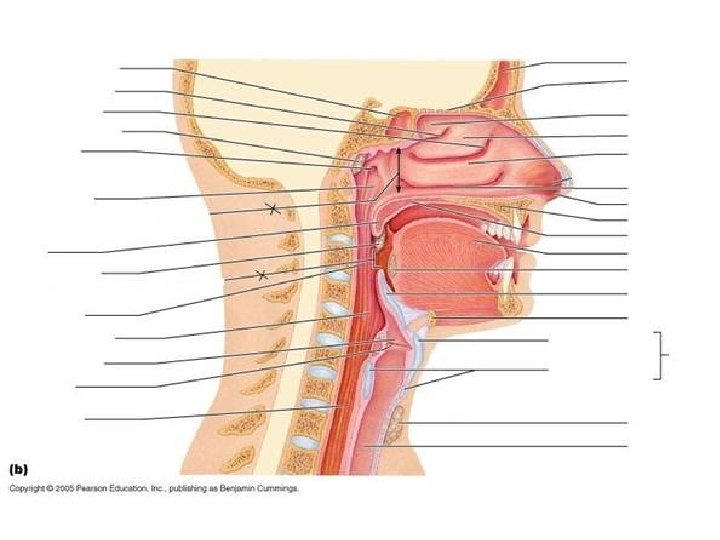
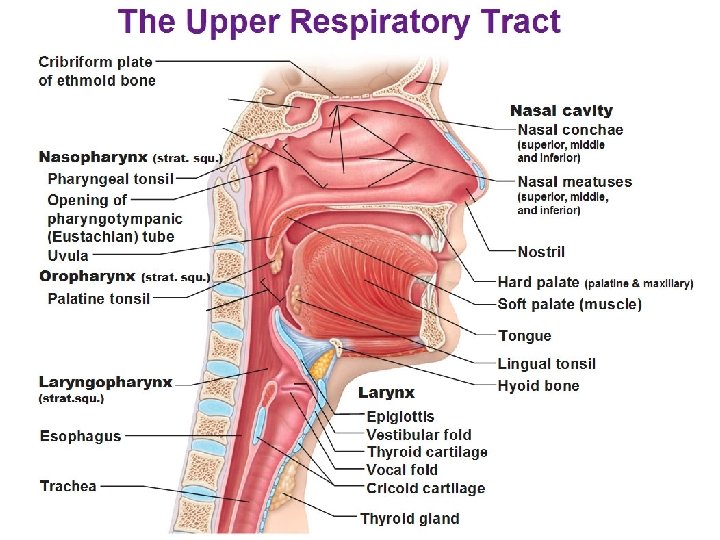
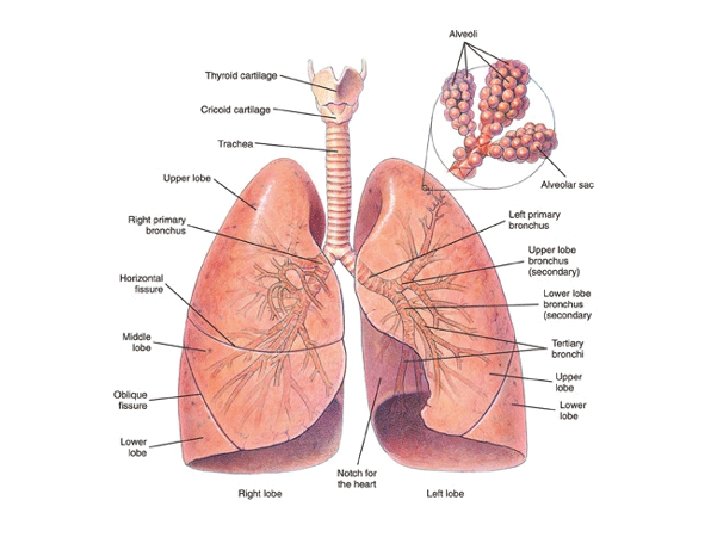
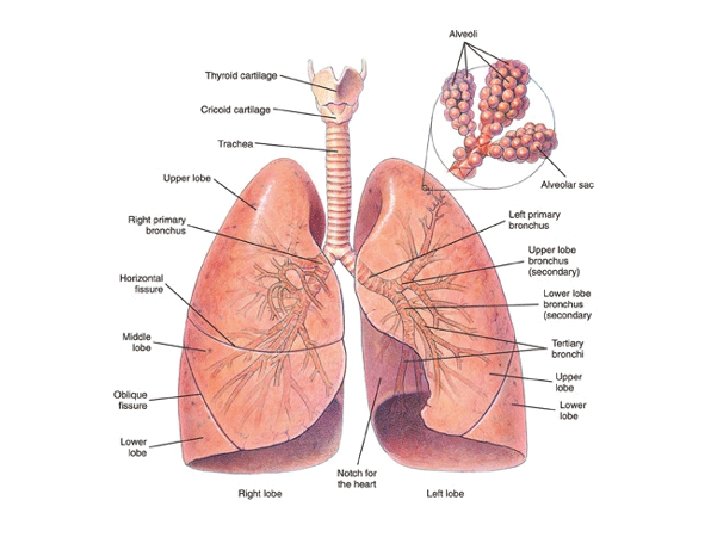
Respiratory Organs • • • Nose Pharynx Larynx Trachea Bronchi • All serve as conducting passageways that allow air to be purified, humidified, and warmed as the reach the lungs • The lungs contain tiny air sacs called alveoli where gas exchanges with the blood occur.
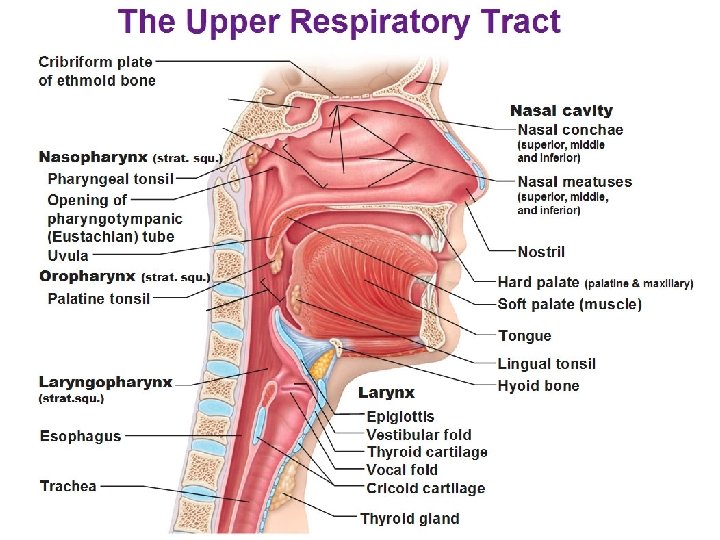
Nose • Also called nasal cavity • Interior is lined with the respiratory mucosa and a network of thin walled veins that warm the air as it flows past. • The sticky mucus also traps incoming bacteria and debris and moistens the air.
Nose • Conchae- located on lateral walls of nose – Increase the surface area exposed to air • The nasal cavity is separated from the oral cavity by the hard and soft palates.
Pharynx • Aka the throat • Muscular passageway • Food and air both pass through the pharynx. • Food is directed to the esophagus when the epiglottis closes. • Air is allowed through the epiglottis into the larynx.
Larynx • Formed by 8 rigid hyaline cartilages and the spoon shaped flap of elastic cartilage called the epiglottis. • When we swallow the larynx is pulled upward and epiglottis tips, forming a lid over the larynx.
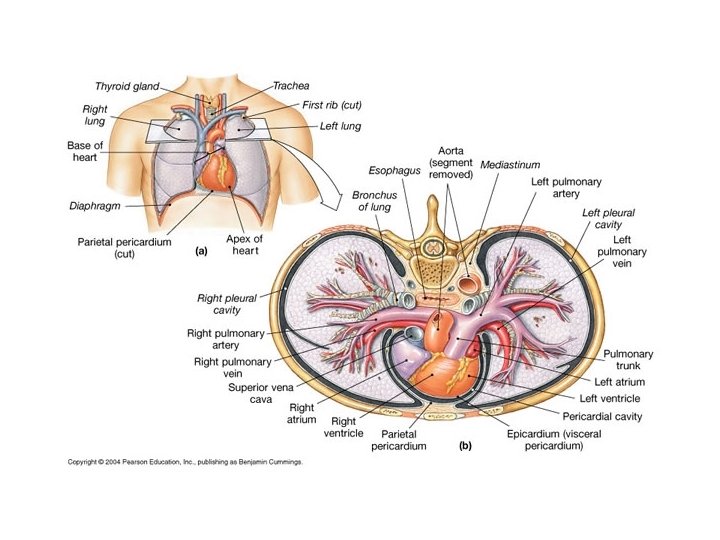
Trachea and Bronchi • The trachea, or windpipe is lined with ciliated mucosa that beat continuously in a direction opposite to the incoming air. • The right and left bronchi are formed by the division of the trachea and enter the medial depression of the lung.
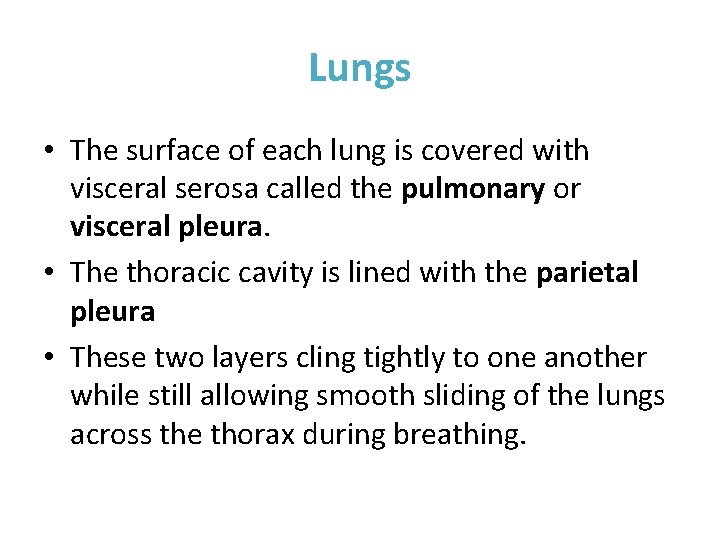
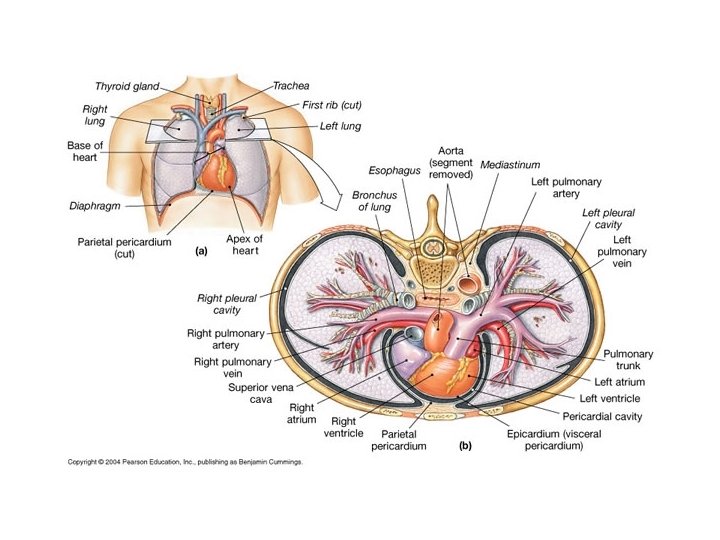
Lungs • The surface of each lung is covered with visceral serosa called the pulmonary or visceral pleura. • The thoracic cavity is lined with the parietal pleura • These two layers cling tightly to one another while still allowing smooth sliding of the lungs across the thorax during breathing.
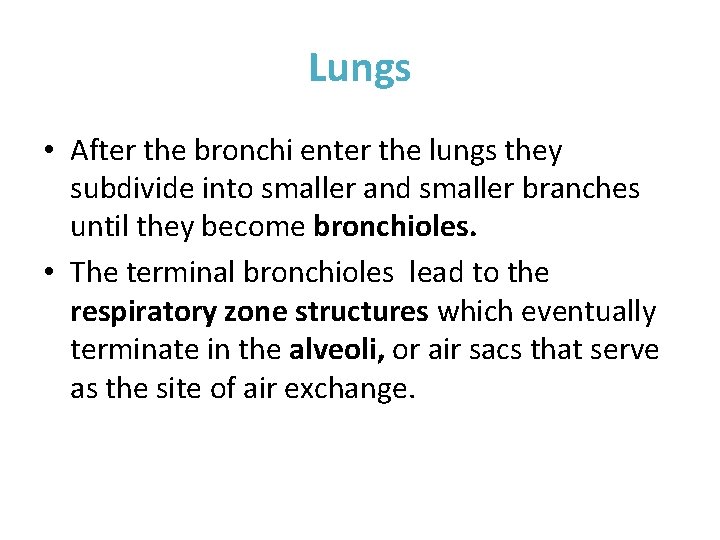
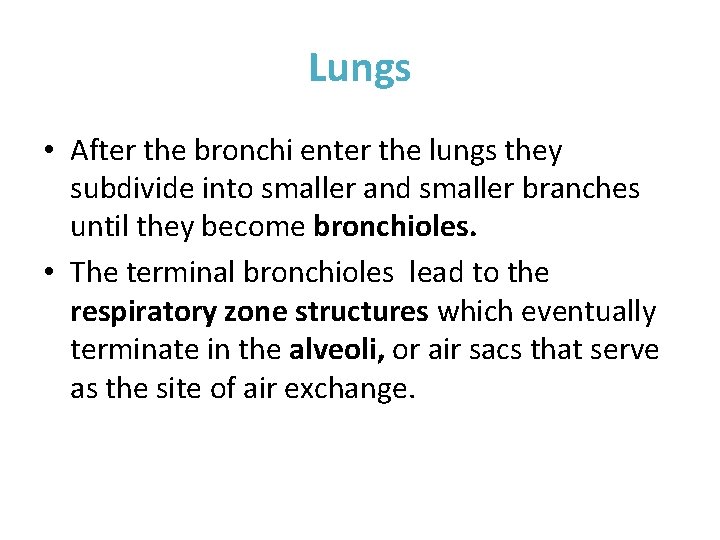
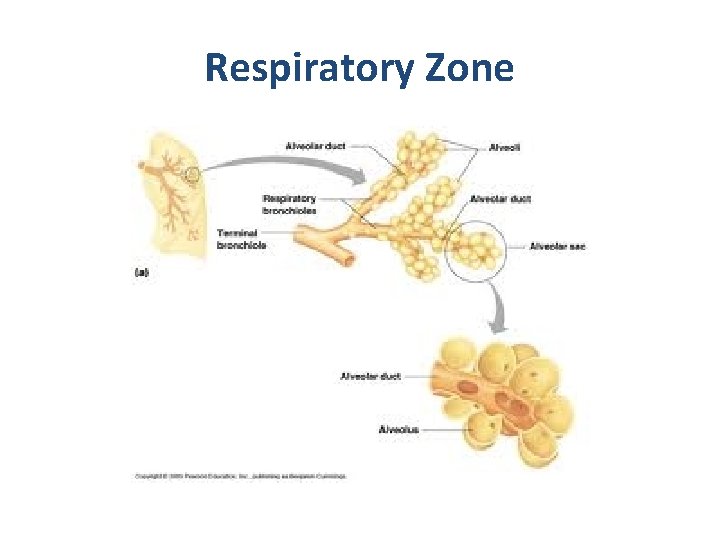
Lungs • After the bronchi enter the lungs they subdivide into smaller and smaller branches until they become bronchioles. • The terminal bronchioles lead to the respiratory zone structures which eventually terminate in the alveoli, or air sacs that serve as the site of air exchange.
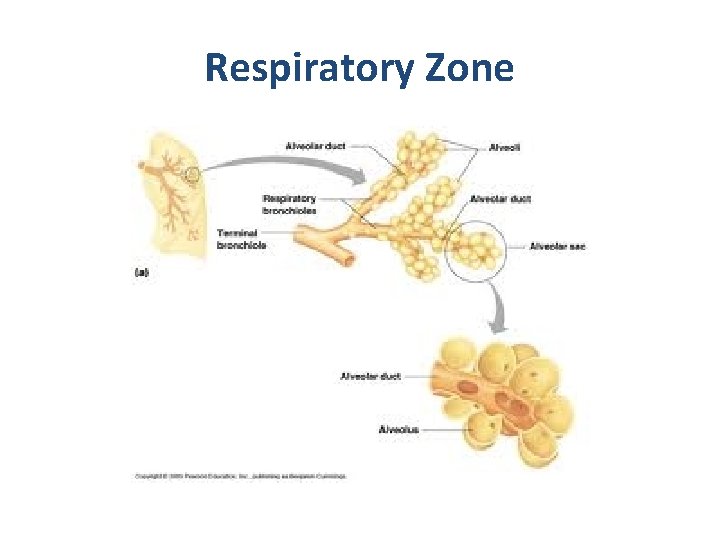
Respiratory Zone
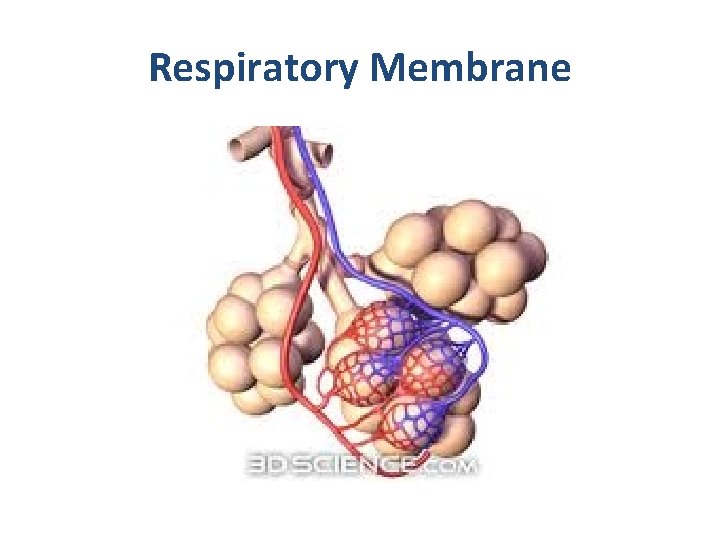
Respiratory Membrane • The external surfaces of the alveoli are covered in a cobweb of pulmonary capillaries. • Together these two structures make up the respiratory membrane (air-blood barrier)
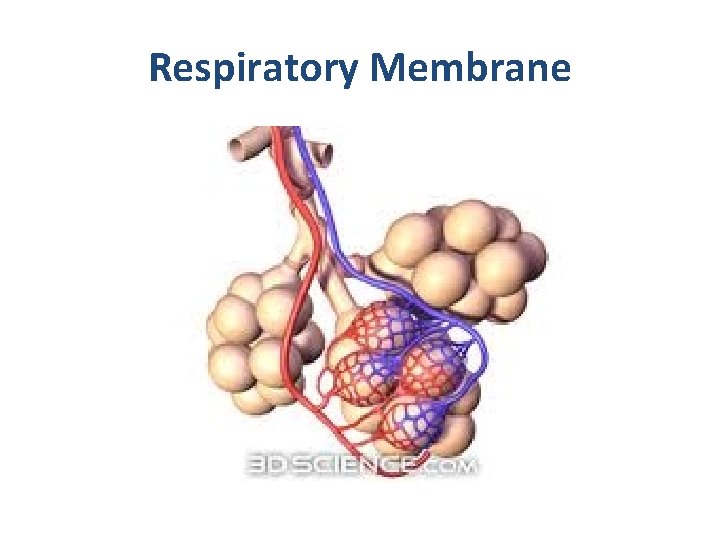
Respiratory Membrane
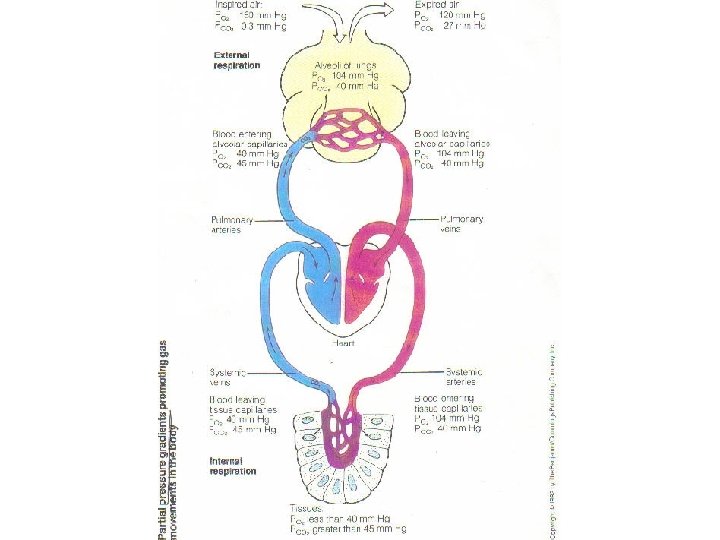
Respiratory Physiology • There are 4 distinct events collectively called respiration. 1. Pulmonary Ventilation (breathing)- air must move in and out of the lungs so that the gases in the air sacs of the lungs are continuously changed and refreshed.
Respiratory Physiology • There are 4 distinct events collectively called respiration. 2. External Respiration – gas exchange between the pulmonary blood and alveoli must take place
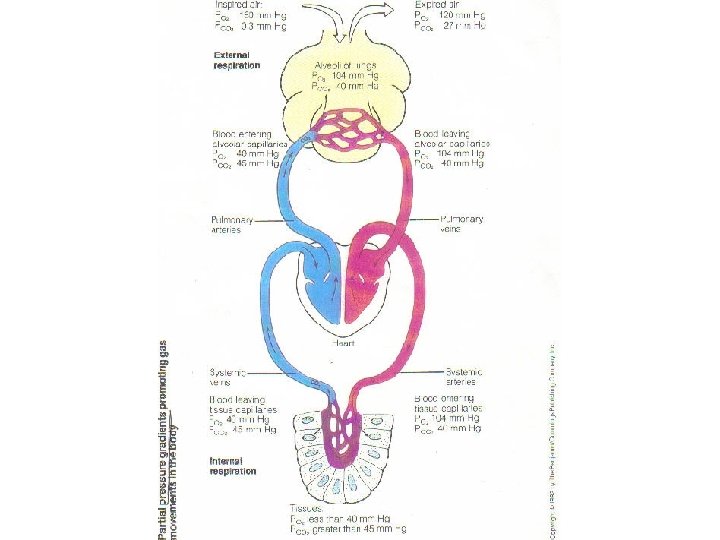
Respiratory Physiology • There are 4 distinct events collectively called respiration. 3. Respiratory Gas Exchange – oxygen and carbon dioxide must be transported to and from the lungs and tissue cells of the body via the blood stream.
Respiratory Physiology • There are 4 distinct events collectively called respiration. 4. Internal Gas Exchange – gas exchange at the systemic capillaries between the blood and tissue cells.
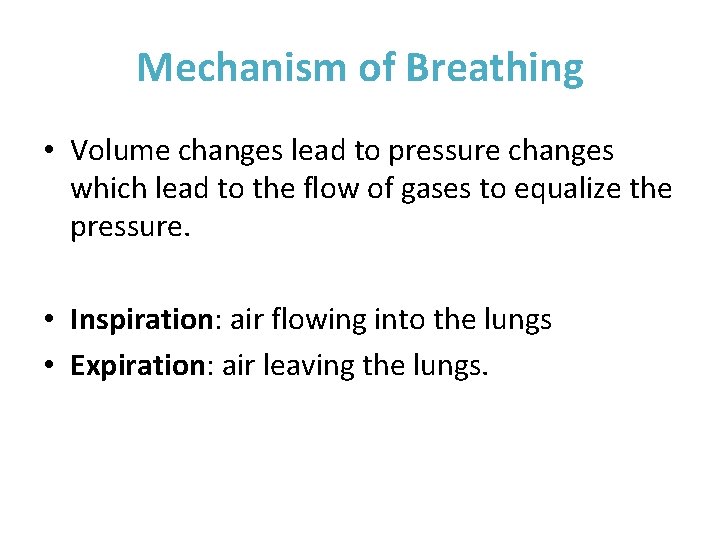
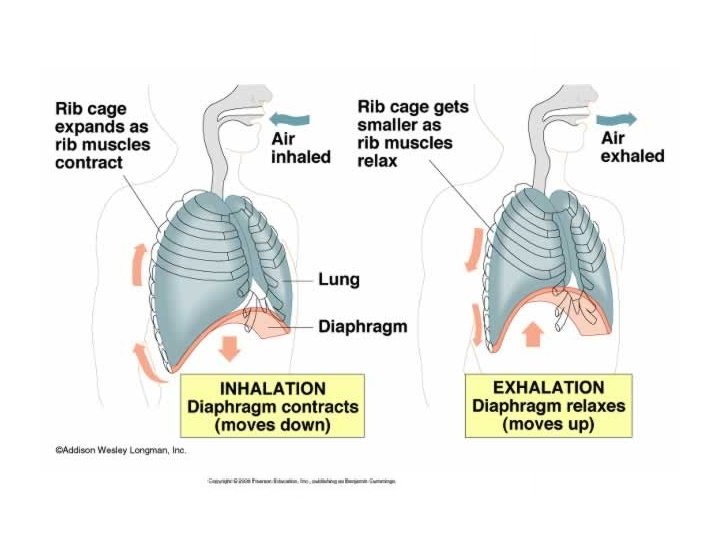
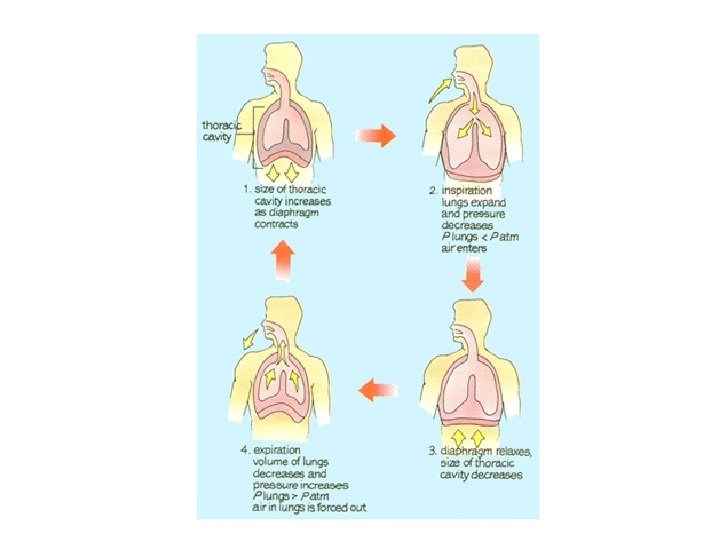
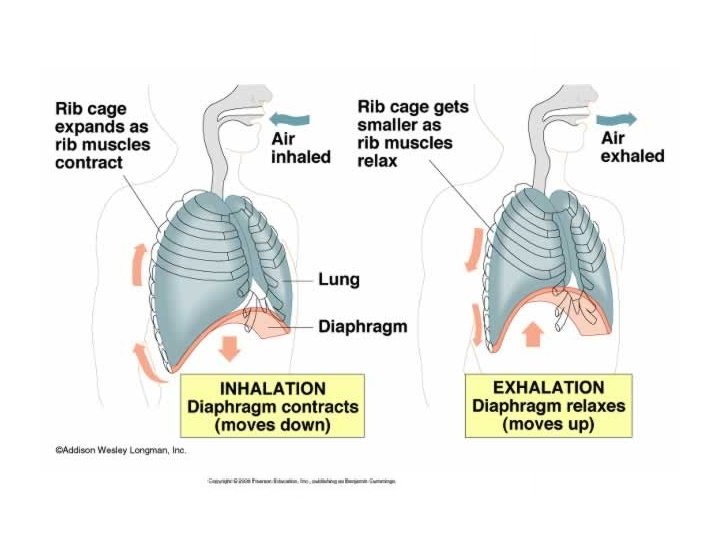
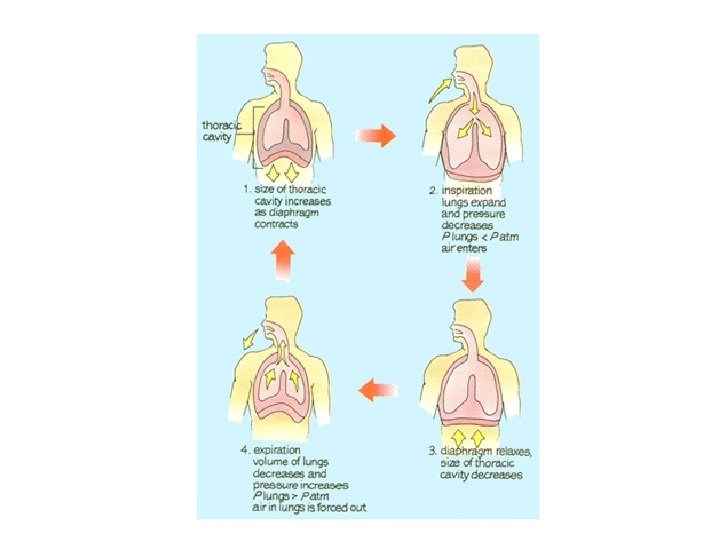
Mechanism of Breathing • Volume changes lead to pressure changes which lead to the flow of gases to equalize the pressure. • Inspiration: air flowing into the lungs • Expiration: air leaving the lungs.
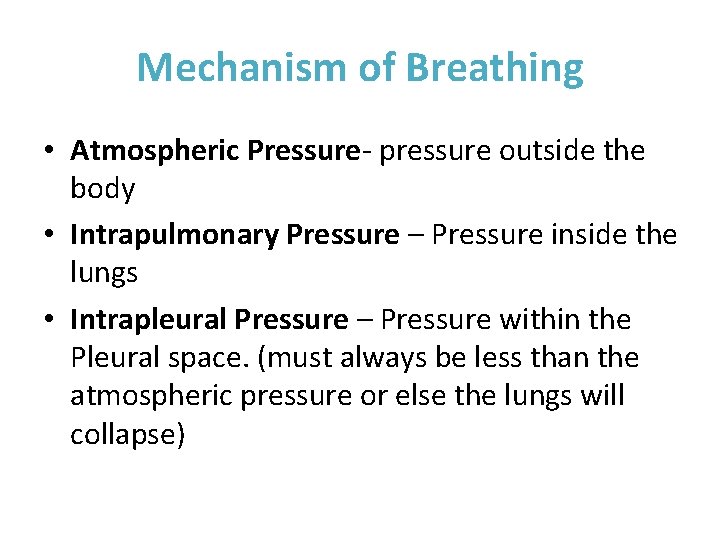
Mechanism of Breathing • Atmospheric Pressure- pressure outside the body • Intrapulmonary Pressure – Pressure inside the lungs • Intrapleural Pressure – Pressure within the Pleural space. (must always be less than the atmospheric pressure or else the lungs will collapse)
Gas Exchange • Because body cells continuously remove oxygen from the blood, there is always a higher concentration of oxygen in the alveoli than in the blood, thus oxygen moves from the alveoli, through the respiratory membrane into the more oxygen poor blood of the pulmonary capillaries.
Gas Exchange • On the other hand, as tissue cells remove oxygen from the blood, they release carbon dioxide into the blood. Because the concentration of carbon dioxide is much higher in the pulmonary capillaries than in the alveolar air, it will move from the blood into the alveoli and be flushed out of the lung on expiration.
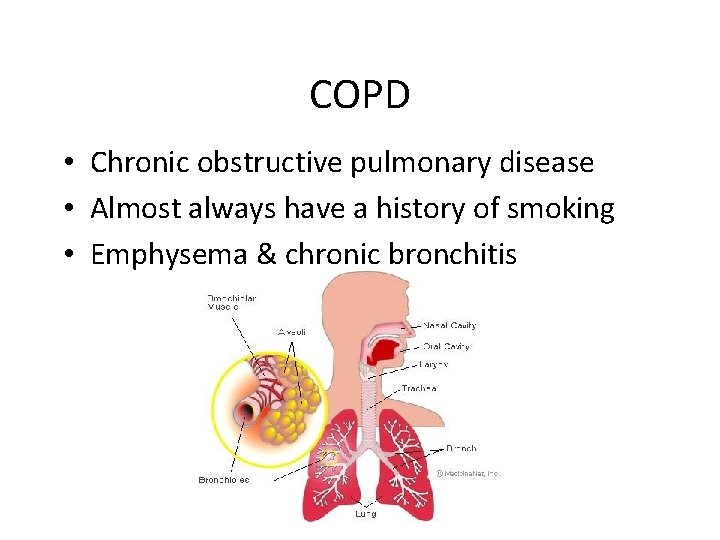
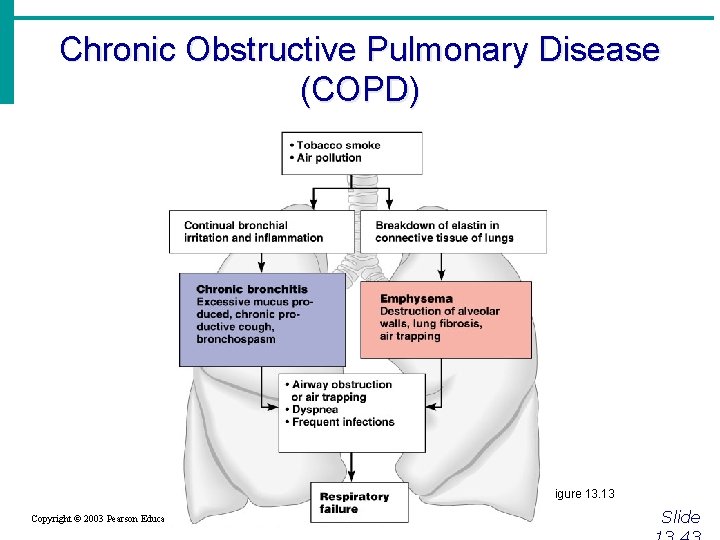
COPD • Chronic obstructive pulmonary disease • Almost always have a history of smoking • Emphysema & chronic bronchitis
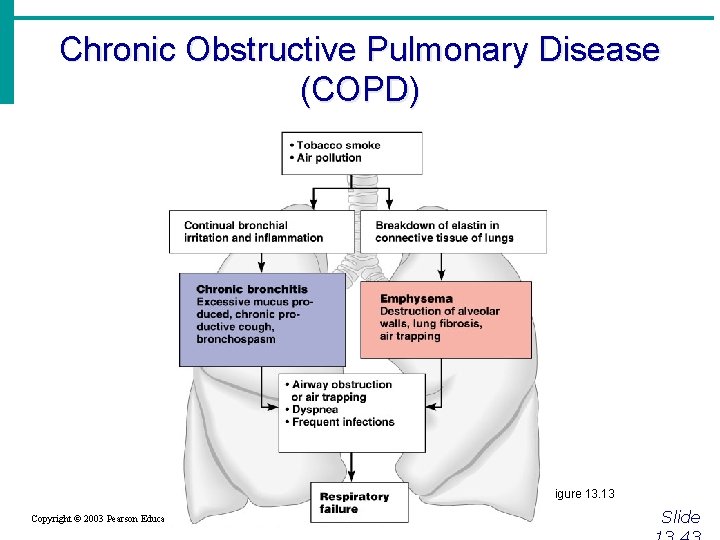
Chronic Obstructive Pulmonary Disease (COPD) Figure 13. 13 Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
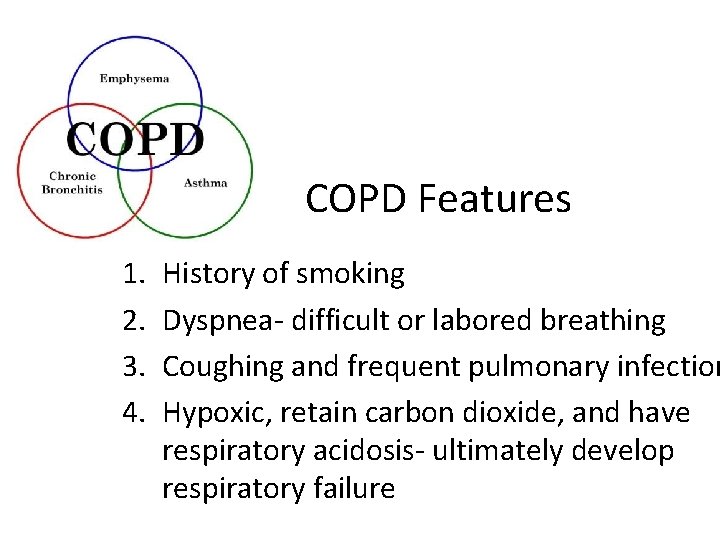
COPD Features 1. 2. 3. 4. History of smoking Dyspnea- difficult or labored breathing Coughing and frequent pulmonary infection Hypoxic, retain carbon dioxide, and have respiratory acidosis- ultimately develop respiratory failure
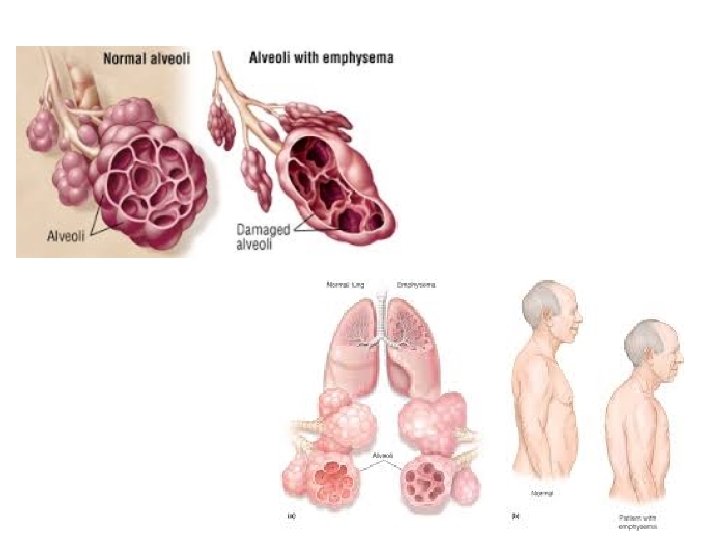
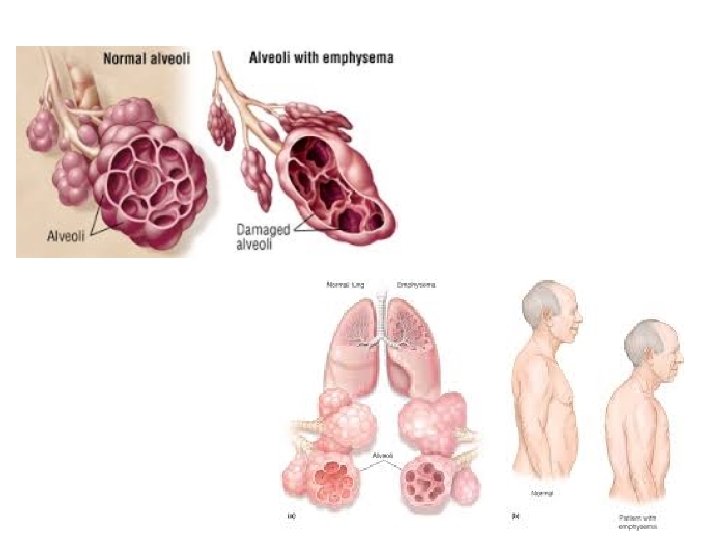
Emphysema • Alveoli enlarge • Chronic inflammation promotes fibrosis of the lungs • Lungs become less elastic • Airways collapse during expiration • Use a lot of energy to exhale • Always exhausted • Pink puffers
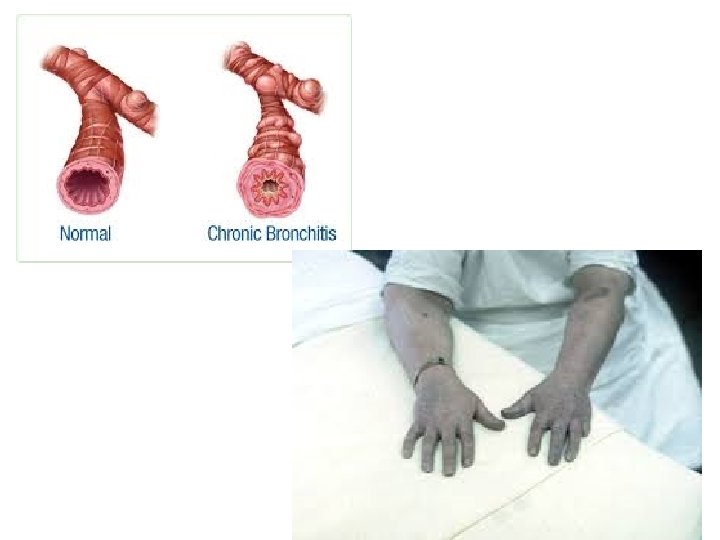
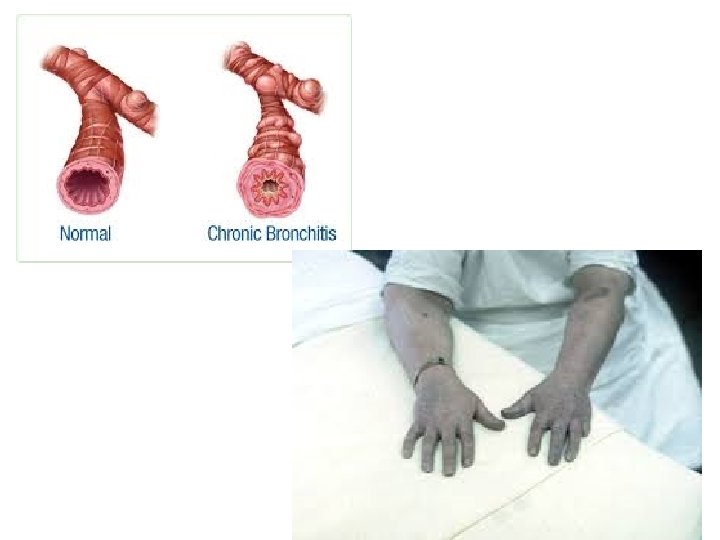
Chronic Bronchitis • Mucosa of the lower respiratory passages become severely inflamed and produce excessive amount of mucus • Pooled mucus impairs ventilation and gas exchange • Lung infections & pneumonias • Blue bloaters- due to cyanosis
Lung Cancer · Accounts for 1/3 of all cancer deaths in the United States · Increased incidence associated with smoking · Three common types · Squamous cell carcinoma · Adenocarcinoma · Small cell carcinoma Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
Sudden Infant Death syndrome (SIDS) · Apparently healthy infant stops breathing and dies during sleep · Some cases are thought to be a problem of the neural respiratory control center · One third of cases appear to be due to heart rhythm abnormalities Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
Asthma · Chronic inflamed hypersensitive bronchiole passages · Response to irritants with dyspnea, coughing, and wheezing Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
Developmental Aspects of the Respiratory System · Lungs are filled with fluid in the fetus · Lungs are not fully inflated with air until two weeks after birth · Surfactant that lowers alveolar surface tension is not present until late in fetal development and may not be present in premature babies Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
Developmental Aspects of the Respiratory System · Important birth defects · Cystic fibrosis – oversecretion of thick mucus clogs the respiratory system · Cleft palate Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
Aging Effects · Elasticity of lungs decreases · Vital capacity decreases · Blood oxygen levels decrease · Stimulating effects of carbon dioxide decreases · More risks of respiratory tract infection Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
Respiratory Rate Changes Throughout Life · Newborns – 40 to 80 respirations per minute · Infants – 30 respirations per minute · Age 5 – 25 respirations per minute · Adults – 12 to 18 respirations per minute · Rate often increases somewhat with old age Copyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings Slide
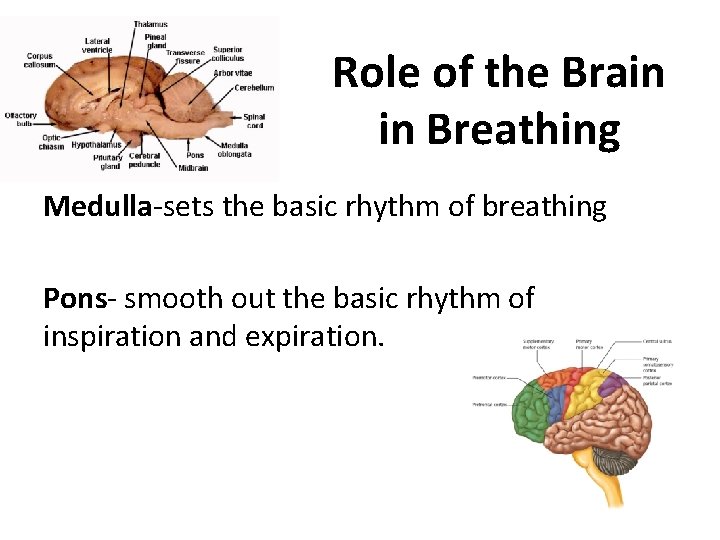
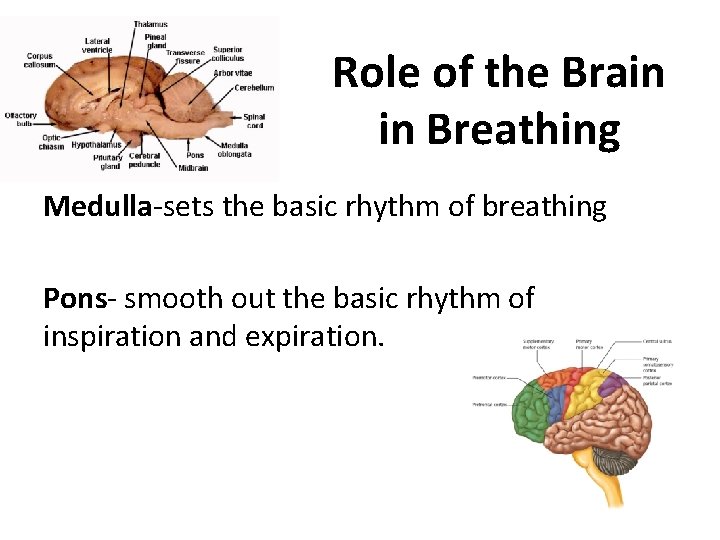
Role of the Brain in Breathing Medulla-sets the basic rhythm of breathing Pons- smooth out the basic rhythm of inspiration and expiration.
Volition • • Conscious control Singing Swallowing Swimming • Ex: toddler trying to hold their breath to deathwon’t happen because involuntary controls take over and normal respiration begins again.
Physical Factors • • Talking Coughing Exercise All can modify the rate and depth of breathing.
Emotional Factors • What type of emotional factors can affect breathing?
Chemical Factors • Most important factor that can modify respiratory rate and depth. • Levels of carbon dioxide and oxygen in the blood. • Increased carbon dioxide/decreased blood p. H will increase the rate and depth of breathing