Respiratory System Infections Respiratory System Divided into two


- Slides: 39

Respiratory System Infections
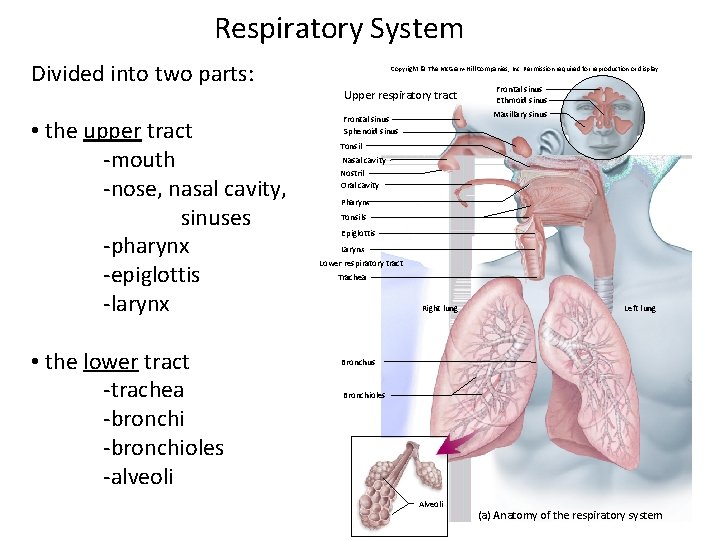
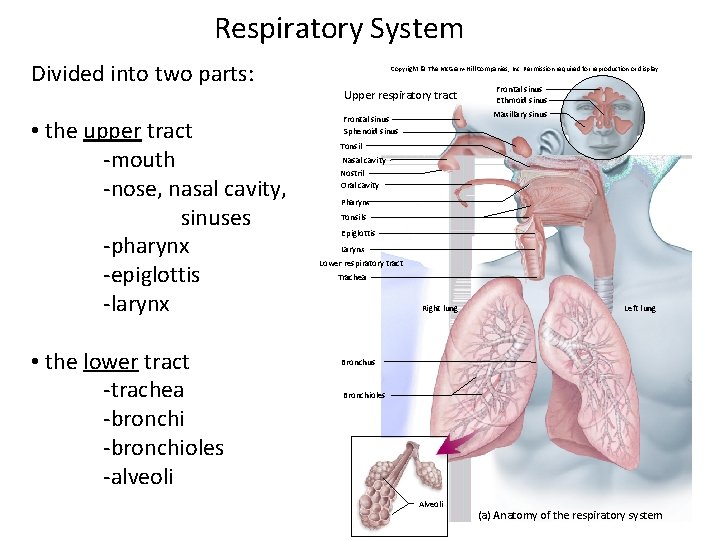
Respiratory System Divided into two parts: Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Upper respiratory tract • the upper tract -mouth -nose, nasal cavity, sinuses -pharynx -epiglottis -larynx • the lower tract -trachea -bronchioles -alveoli Frontal sinus Sphenoid sinus Frontal sinus Ethmoid sinus Maxillary sinus Tonsil Nasal cavity Nostril Oral cavity Pharynx Tonsils Epiglottis Larynx Lower respiratory tract Trachea Right lung Left lung Bronchus Bronchioles Alveoli (a) Anatomy of the respiratory system

Respiratory Defenses The respiratory tract is the most common portal of entry Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Protection from infection: Cilia • first line defenses: • nasal hairs • cilia • mucus Microvillus (5, 000×) Bacterium • second line defenses -macrophages • third line defenses -pathogen-specific secretory Ig. A (b) Ciliary defense of the tracheal mucosa © Ellen R. Dirksen/Visuals Unlimited
Normal Biota of the Respiratory Tract • This system harbors a large number of commensal microbes • Normal biota mainly found in the upper respiratory tract • Gram-positive bacteria are common in the normal biota -streptococci, staphylococci • Some can potentially be pathogenic: -Streptococcus pyogenes -Haemophilus influenzae -Streptococcus pneumoniae -Neisseria meningitidis -Staphylococcus aureus • Candida albicans (yeast) colonizes the oral mucosa
Respiratory System Infections • Encompass enormous variety of illnesses • • Trivial to fatal Divided into infections of • Upper respiratory • • • Head and neck Uncomfortable but generally not life threatening Lower respiratory • • • Chest More serious Can be life-threatening • Particularly in the immunocompromised
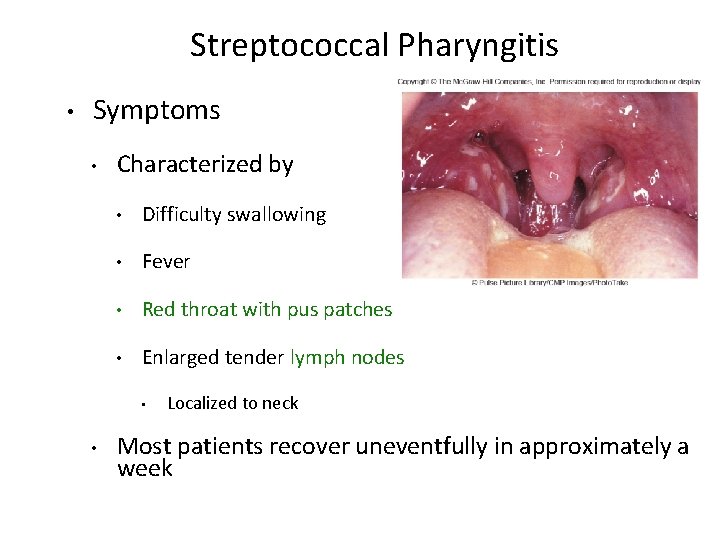
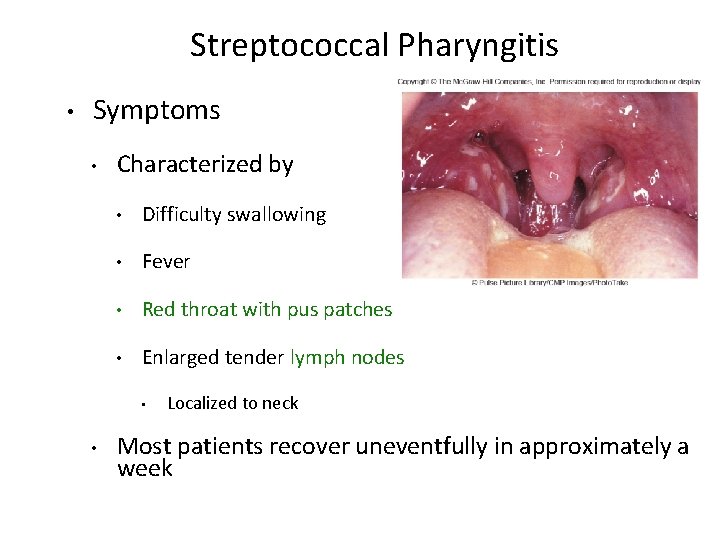
Streptococcal Pharyngitis • Symptoms • Characterized by • Difficulty swallowing • Fever • Red throat with pus patches • Enlarged tender lymph nodes • • Localized to neck Most patients recover uneventfully in approximately a week
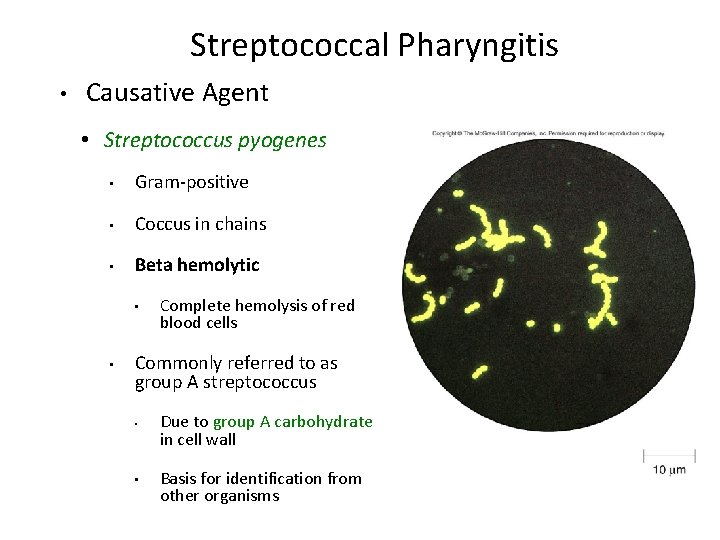
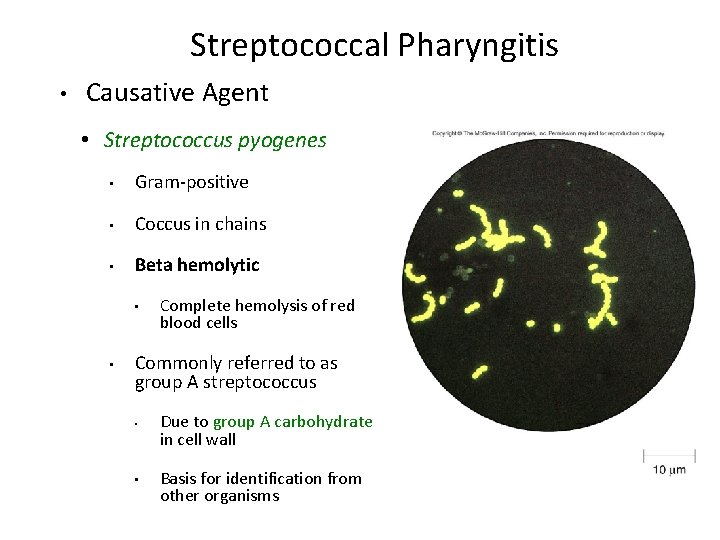
Streptococcal Pharyngitis • Causative Agent • Streptococcus pyogenes • Gram-positive • Coccus in chains • Beta hemolytic • • Complete hemolysis of red blood cells Commonly referred to as group A streptococcus • • Due to group A carbohydrate in cell wall Basis for identification from other organisms
Streptococcal Pharyngitis • Pathogenesis due to numerous virulence factors • Streptolysin O and S for hemolysis • Protein G used to inactivate antibody • More virulence factors used by S. pyogenes in other diseases – • Superantigens, etc. Complications of infection can occur during acute illness • Scarlet fever • Acute glomerulonephritis • Acute rheumatic fever
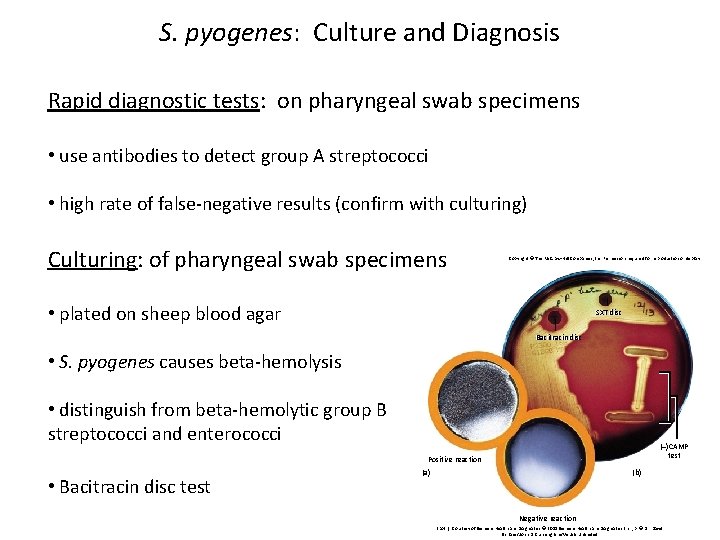
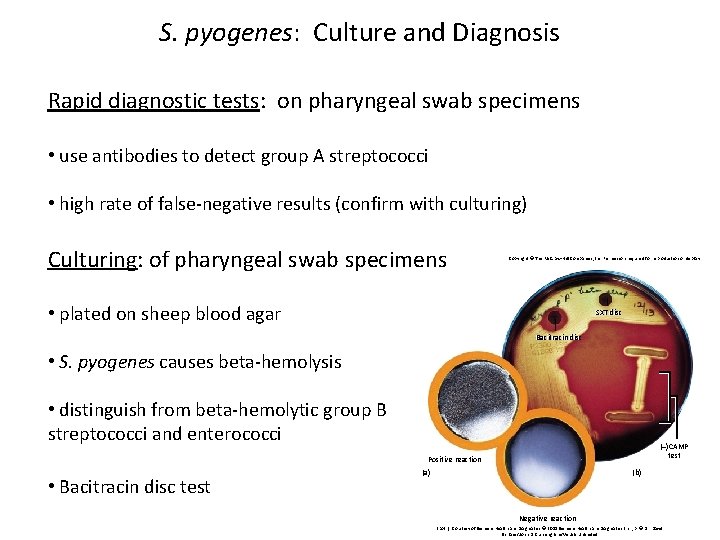
S. pyogenes: Culture and Diagnosis Rapid diagnostic tests: on pharyngeal swab specimens • use antibodies to detect group A streptococci Case File • high rate of false-negative results (confirm with culturing) Artwork Chapter 3 Culturing: of pharyngeal swab specimens Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. • plated on sheep blood agar SXT disc Bacitracin disc • S. pyogenes causes beta-hemolysis • distinguish from beta-hemolytic group B streptococci and enterococci (–)CAMP test Positive reaction • Bacitracin disc test (a) (b) Negative reaction (both): Courtesy of Siemens Healthcare Diagnostics © 2011 Siemens Healthcare Diagnostics Inc. ; b: © Dr. David Schlaes/John D. Cunningham/Visuals Unlimited
Treatment for Streptococcal pharyngitis: • Penicillin as many group A streptococci resistant to erythromycin • Use first-generation cephalosporin (cephalexin) for patients with penicillin allergies Prevention: • No vaccine • Prevention by good hand washing
Common Cold • Symptoms • • • Malaise Scratchy mild sore throat Runny nose Cough and hoarsness Nasal secretion • Initially profuse and watery • Later, thick and purulent • No fever • • Unless complicated with secondary infection Symptoms disappear in about a week
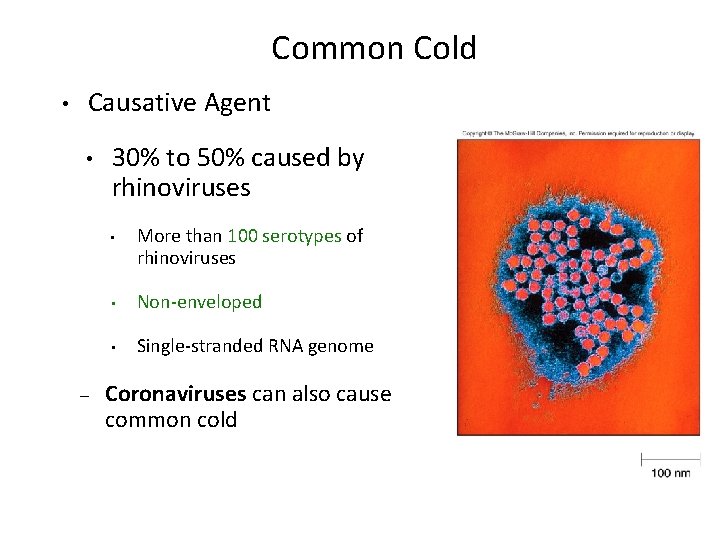
Common Cold • Causative Agent • 30% to 50% caused by rhinoviruses • – More than 100 serotypes of rhinoviruses • Non-enveloped • Single-stranded RNA genome Coronaviruses can also cause common cold
• Pathogenesis • Virus attach to specific receptors on respiratory epithelial cells and multiply in cells • • • Large number of viruses released from infected cells Injured cells cause inflammation which stimulates profuse nasal secretion, sneezing and tissue swelling Infection is halted by inflammatory response, interferon release, and immune response • • Common Cold Rhinovirus Infection can extend to ears, sinuses and lower respiratory tract before stopping Treatment is supportive with OTC medications
Whooping Cough • Aka: Pertussis • Symptoms • Runny nose followed by bouts of uncontrollable coughing • Termed paroxymal coughing • • Coughing spasm followed by characteristic “whoop” • • Severe cough can cause rupture of small blood vessels in the eyes Sound made by the forceful inspiration of air Vomiting and seizure may occur
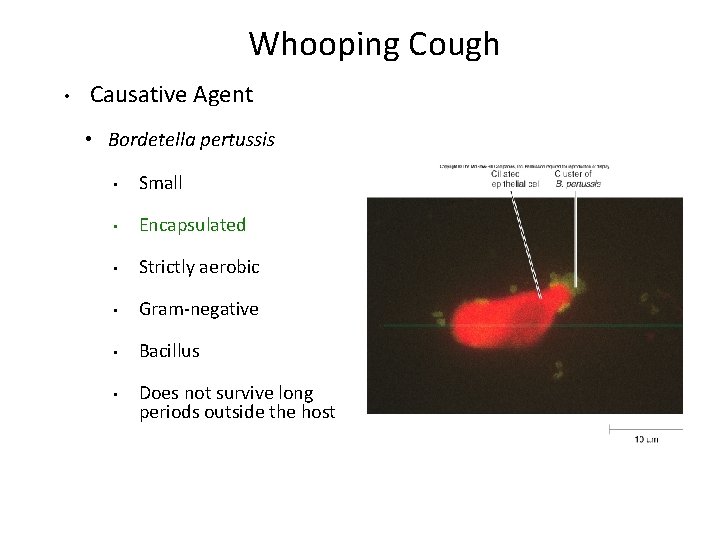
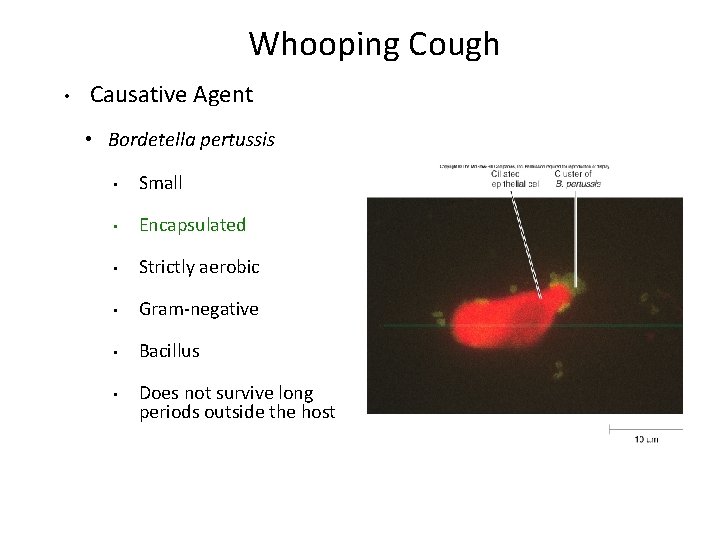
Whooping Cough • Causative Agent • Bordetella pertussis • Small • Encapsulated • Strictly aerobic • Gram-negative • Bacillus • Does not survive long periods outside the host
Whooping Cough • Pathogenesis • Enters respiratory tract with inspired air and attaches to ciliated cells • Organism colonizes structures of the upper and lower respiratory tract • Mucus secretion increases which causes ciliary action to decrease • Cough reflex is only mechanism for clearing secretions
Whooping Cough Video
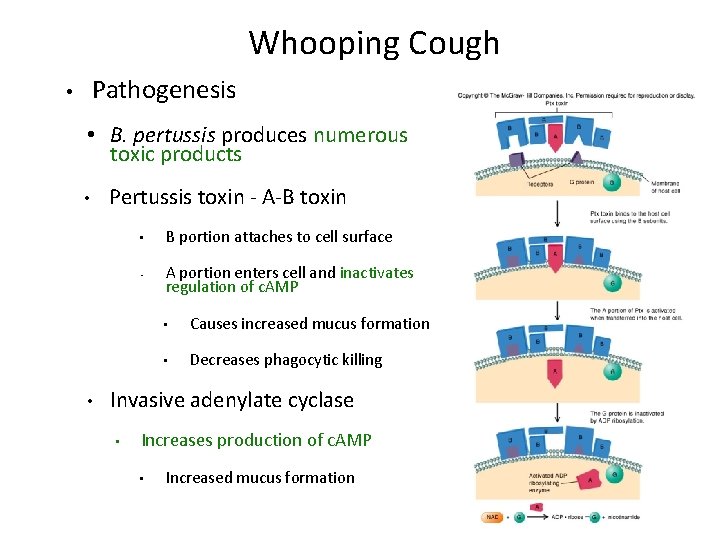
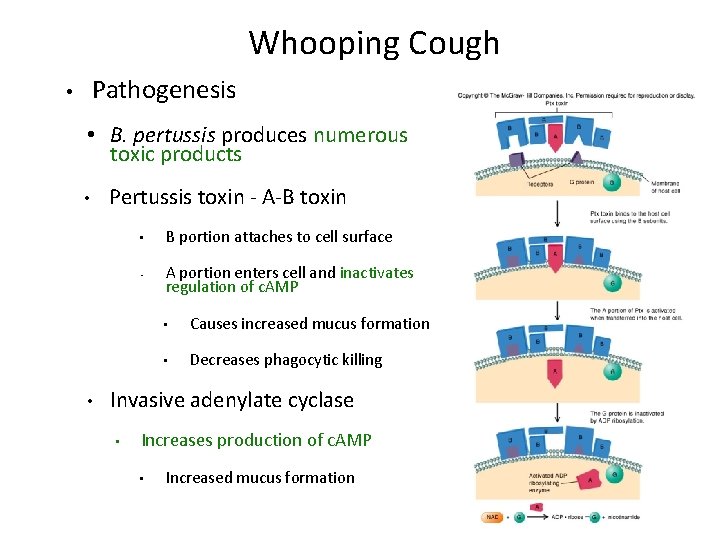
Whooping Cough Pathogenesis • • B. pertussis produces numerous toxic products • • Pertussis toxin - A-B toxin • B portion attaches to cell surface • A portion enters cell and inactivates regulation of c. AMP • Causes increased mucus formation • Decreases phagocytic killing Invasive adenylate cyclase • Increases production of c. AMP • Increased mucus formation
Whooping Cough • Epidemiology • Spreads via infected respiratory droplets • Most infectious during runny nose period • • Classically disease of infants • • Number of organisms decrease with onset of cough Milder forms are seen in older children and adults Often overlooked a persistent cold • Fosters transmission
Whooping Cough • Prevention • • Vaccine directed at protection of infants • Prevents disease in 70% of individuals • Pertussis vaccine combined with diphtheria and tetanus toxoids (DPT) • Injections given at 6 weeks, 4, 6, and 18 months, 5 years • now recommended for 12 year olds Treatment • Erythromycin is effective at reducing symptoms if given early
Tuberculosis • Symptoms • • Chronic illness Symptoms include • Slight fever with night sweats • Causative Agent • Mycobacterium tuberculosis (and M. bovis in AIDS) • Gram-positive cell wall • Slender bacillus • Acid fast due to mycolic acid in cell wall • Progressive weight loss • Slow growing • Chronic productive cough • Generation time 12 hours or more • Sputum often blood streaked • Resists most prevention methods of control
Tuberculosis • Pathogenesis • Usually contracted by inhalation of airborne organisms • Bacteria are taken up by pulmonary macrophages in the lungs • Resists destruction within phagocyte • Organism prevents the fusion of phagosome with lysosomes – allows multiplication in protected vacuole
Tuberculosis • Pathogenesis • Organisms are carried to lymph nodes • About 2 weeks post infection intense immune reaction occurs • Macrophages fuse together to make large multinucleated cell • Macrophages and lymphocytes surround large cell and form a tubercle of connective tissue • • This is an effort to wall off infected tissue Activated macrophages release into infected tissue • Causes death of tissue resulting in formation of “cheesy” material (biofilm)
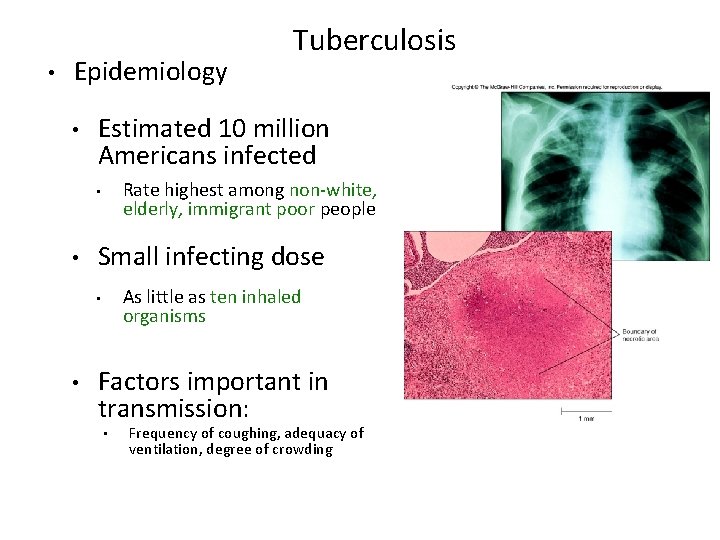
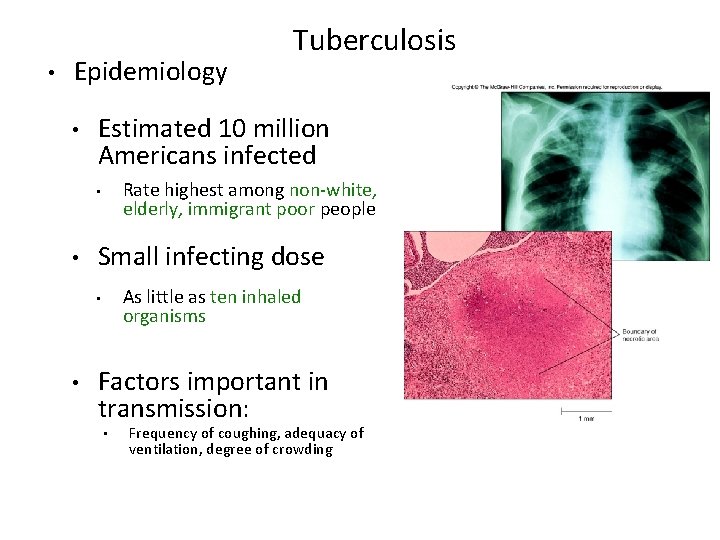
• Epidemiology • Estimated 10 million Americans infected Rate highest among non-white, elderly, immigrant poor people • • Small infecting dose As little as ten inhaled organisms • • Tuberculosis Factors important in transmission: • Frequency of coughing, adequacy of ventilation, degree of crowding
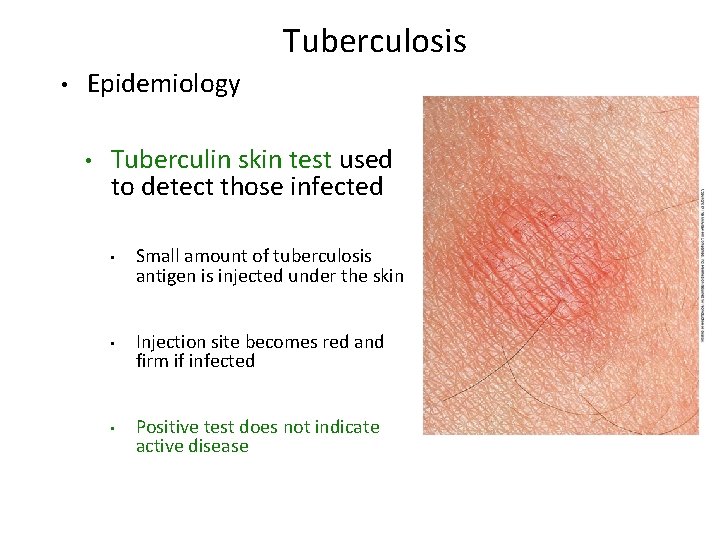
Tuberculosis • Epidemiology • Tuberculin skin test used to detect those infected • Small amount of tuberculosis antigen is injected under the skin • Injection site becomes red and firm if infected • Positive test does not indicate active disease
Tuberculosis • Prevention • Vaccination for tuberculosis widely used in many parts of the world • Vaccine known as Bacillus of Calmette and Guérin • • • BCG derived from Mycobacterium bovis Gives weak, partial immunity against tuberculosis Vaccine not given in United States because it eliminates use of tuberculin test as diagnostic tool • Treatment • Antibiotic treatment is given in cases of active tuberculosis • Two or more medications are given together to reduce potential antimicrobial resistance • Antimicrobials include Rifampin and Isoniazid (INH) • Both target actively growing organisms and metabolically inactive intracellular organisms • Therapy is pronged, lasting at least 6 months • Multi-drug resistant strains have arisen in the U. S. and Russia that have spread to other countries
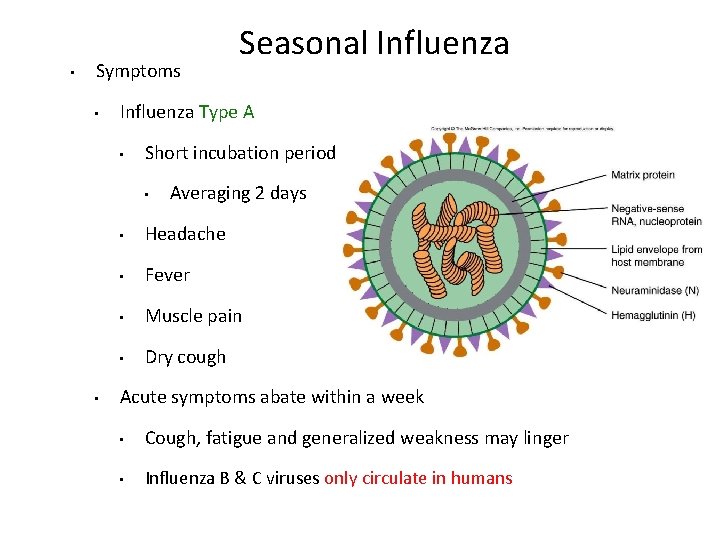
• Symptoms • Influenza Type A • Short incubation period • • Seasonal Influenza Averaging 2 days • Headache • Fever • Muscle pain • Dry cough Acute symptoms abate within a week • Cough, fatigue and generalized weakness may linger • Influenza B & C viruses only circulate in humans
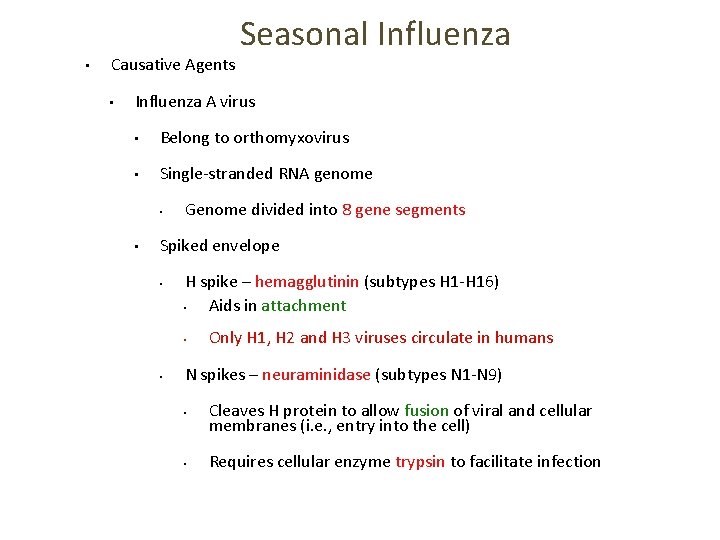
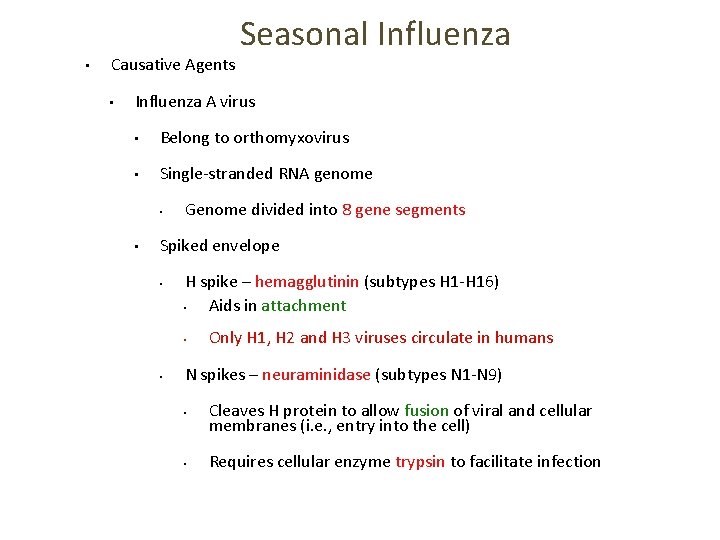
• Causative Agents • Seasonal Influenza A virus • Belong to orthomyxovirus • Single-stranded RNA genome • • Genome divided into 8 gene segments Spiked envelope • H spike – hemagglutinin (subtypes H 1 -H 16) • Aids in attachment • • Only H 1, H 2 and H 3 viruses circulate in humans N spikes – neuraminidase (subtypes N 1 -N 9) • Cleaves H protein to allow fusion of viral and cellular membranes (i. e. , entry into the cell) • Requires cellular enzyme trypsin to facilitate infection
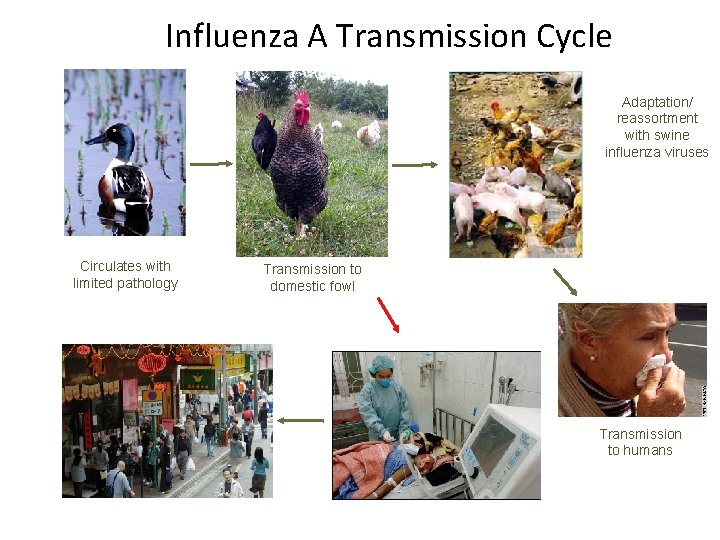
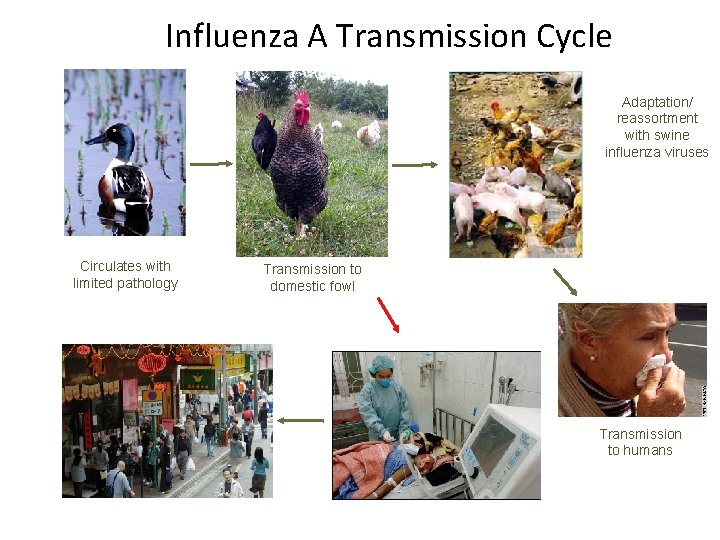
Influenza A Transmission Cycle Adaptation/ reassortment with swine influenza viruses Circulates with limited pathology Transmission to domestic fowl Transmission to humans
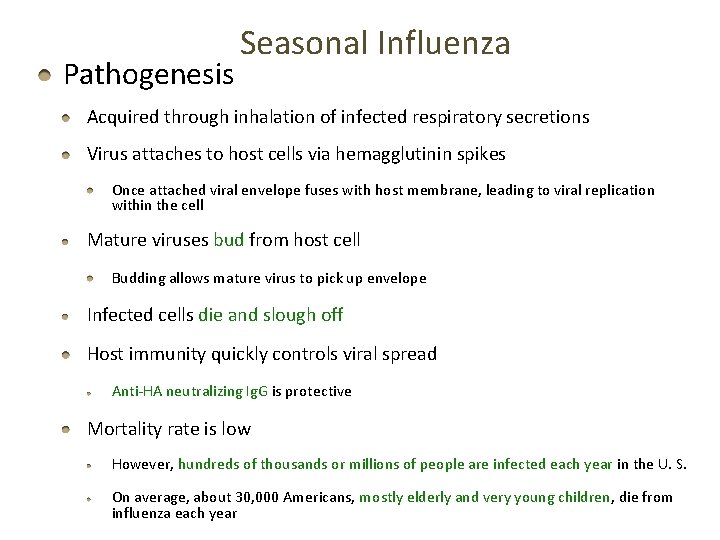
Pathogenesis Seasonal Influenza Acquired through inhalation of infected respiratory secretions Virus attaches to host cells via hemagglutinin spikes Once attached viral envelope fuses with host membrane, leading to viral replication within the cell Mature viruses bud from host cell Budding allows mature virus to pick up envelope Infected cells die and slough off Host immunity quickly controls viral spread Anti-HA neutralizing Ig. G is protective Mortality rate is low However, hundreds of thousands or millions of people are infected each year in the U. S. On average, about 30, 000 Americans, mostly elderly and very young children, die from influenza each year
Seasonal Influenza • Epidemiology • • Outbreaks occur in United States every year • Vaccines are formulated months in advance using prominent circulating strains • 2012 -2013 vaccine strains: Type / Geographic origin / Strain/ Year isolated (H & N genes) • A/California/7/2009 (H 1 N 1)-like virus • A/Victoria/361/2011 (H 3 N 2)-like virus • B/Wisconsin/1/2010 -like virus Pandemics occur periodically • Most famous pandemic of 1918 (Spanish flu) • • Spanned the globe in 9 months Pandemics have higher than normal morbidity
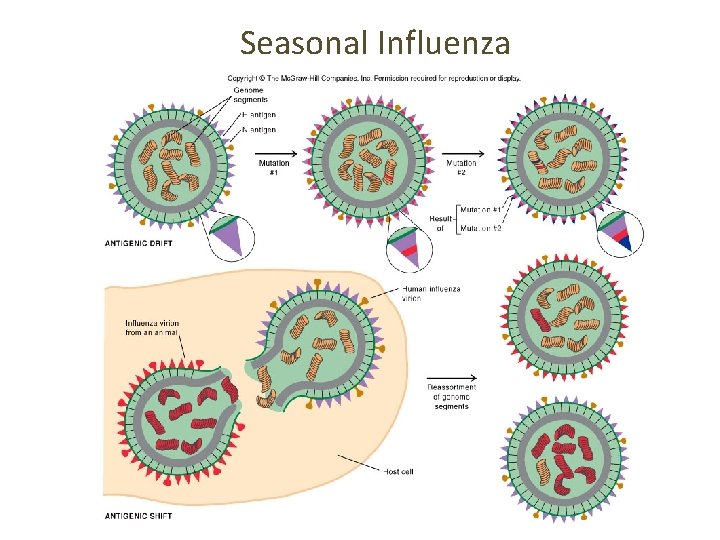
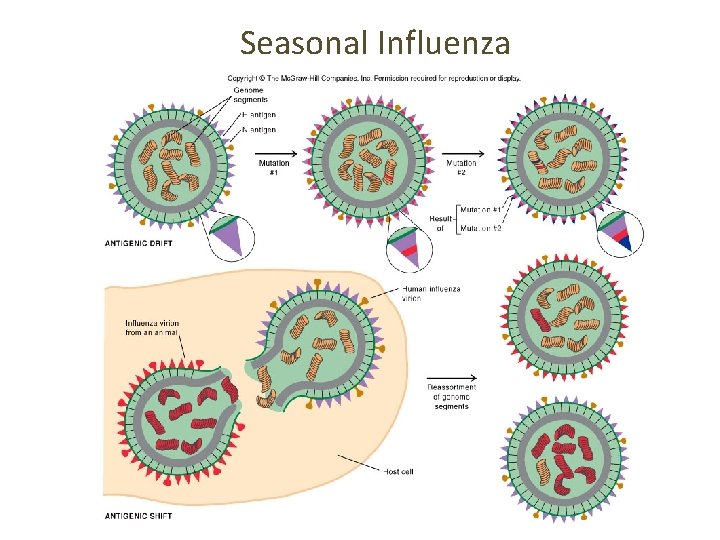
Seasonal Influenza • Epidemiology • Spread caused by major antigenic changes • Antigenic drift • Consists of amino acid changes in spikes (point mutations) • • Particularly hemagglutinin Changes minimize effectiveness of immunity to previous strains • Ensures enough susceptible people are available for continued virus survival • Antigenic shift • Represent more dramatic changes • Virus strains are drastically antigenically different from previous strains, importantly in the hemagglutinin • New virus comes from genetic re-assortment • Occurs when two different viruses infect a cell at the same time • Genetic mixing results in new virus that is often more virulent
Seasonal Influenza
Seasonal Influenza • Prevention and Treatment • Vaccine can be 80% to 90% effective • New vaccine required every year • • Due to antigenic drift Antiviral medications are 70% to 90% effective • Include amantadine, rimantadine, and Tamiflu • Must be taken early • Not a substitute for vaccine
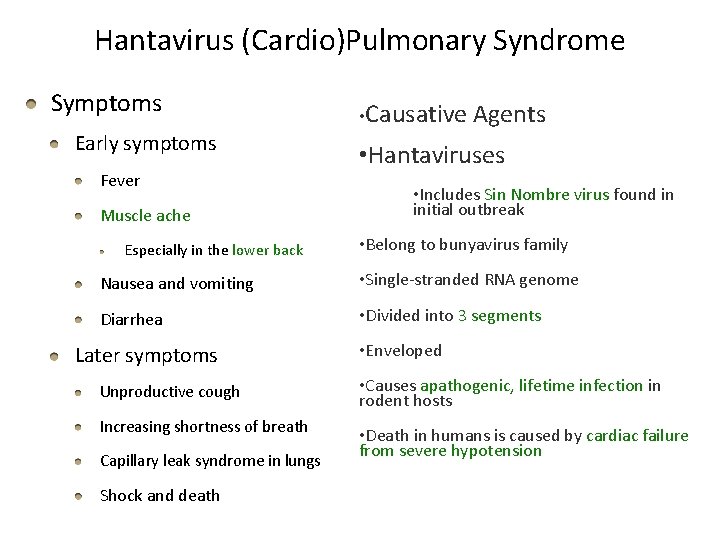
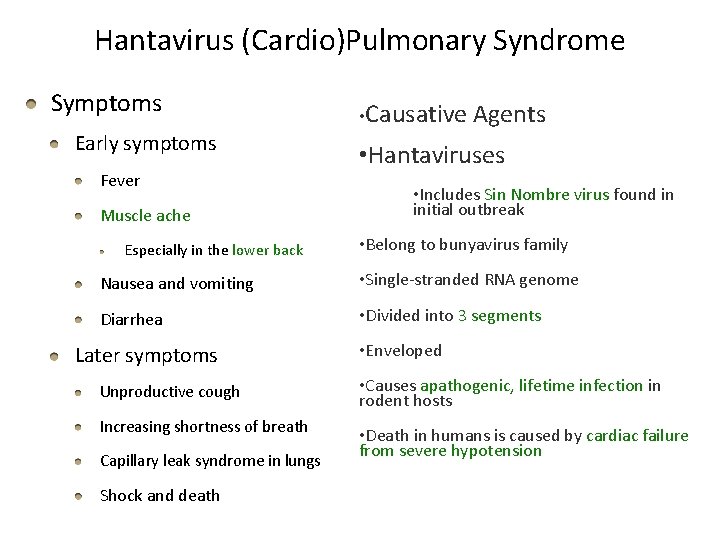
Hantavirus (Cardio)Pulmonary Syndrome Symptoms Early symptoms Fever Muscle ache Especially in the lower back • Causative Agents • Hantaviruses • Includes Sin Nombre virus found in initial outbreak • Belong to bunyavirus family Nausea and vomiting • Single-stranded RNA genome Diarrhea • Divided into 3 segments Later symptoms • Enveloped Unproductive cough • Causes apathogenic, lifetime infection in rodent hosts Increasing shortness of breath • Death in humans is caused by cardiac failure from severe hypotension Capillary leak syndrome in lungs Shock and death
Hantavirus Pulmonary Syndrome • Pathogenesis • Enters body via inhalation of dust contaminated with urine, feces and saliva of infected rodents • Viremia • Mechanism unknown • Carried throughout body • • Inflammation causes capillaries to leak fluid into lungs • • Infects capillary endothelial cells Causes hypoxia and hypotension Cardiac shock and death occurs in over 36% of patients
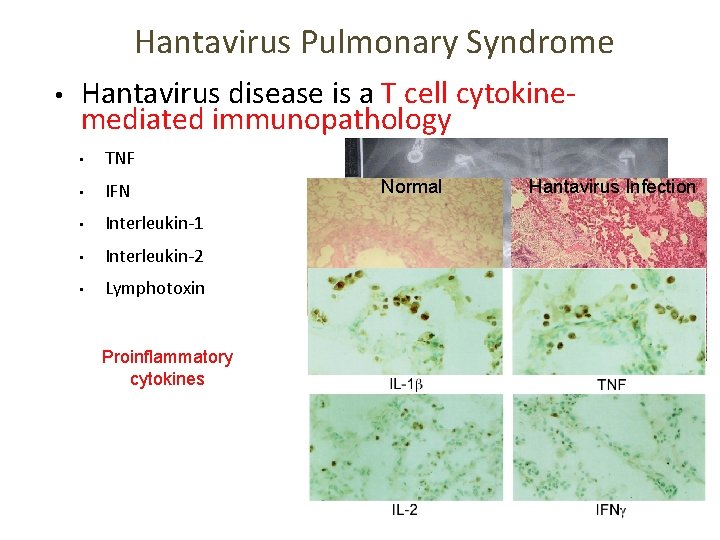
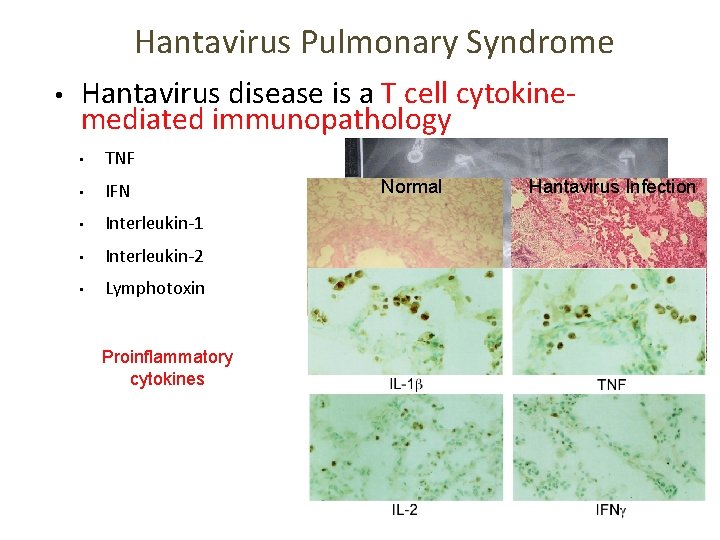
Hantavirus Pulmonary Syndrome • Hantavirus disease is a T cell cytokinemediated immunopathology • TNF • IFN • Interleukin-1 • Interleukin-2 • Lymphotoxin Proinflammatory cytokines Normal Hantavirus Infection • Immune cell infiltrates • No viral damage to the lung epithelium
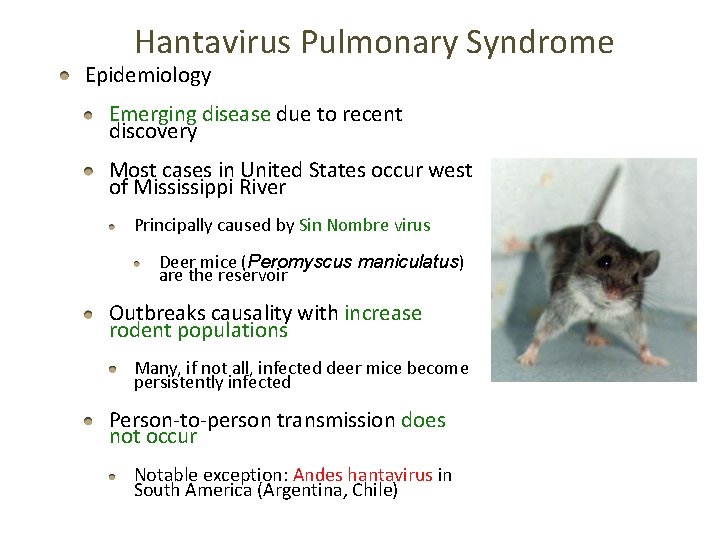
Hantavirus Pulmonary Syndrome Epidemiology Emerging disease due to recent discovery Most cases in United States occur west of Mississippi River Principally caused by Sin Nombre virus Deer mice (Peromyscus maniculatus) are the reservoir Outbreaks causality with increase rodent populations Many, if not all, infected deer mice become persistently infected Person-to-person transmission does not occur Notable exception: Andes hantavirus in South America (Argentina, Chile)
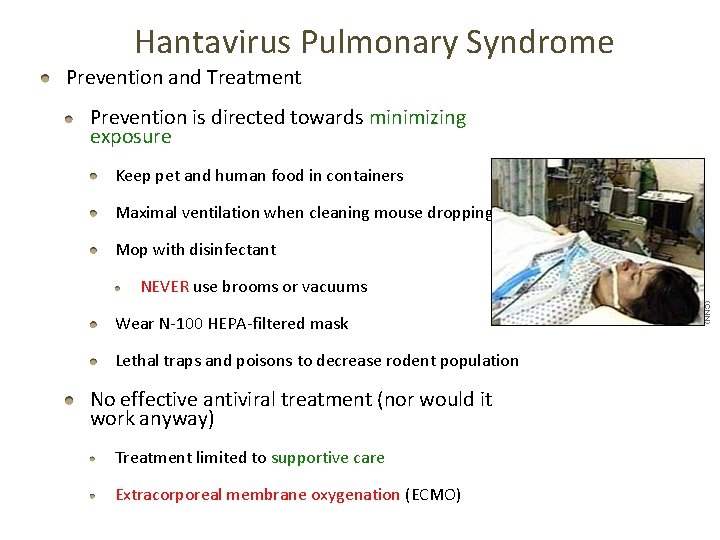
Hantavirus Pulmonary Syndrome Prevention and Treatment Prevention is directed towards minimizing exposure Keep pet and human food in containers Maximal ventilation when cleaning mouse droppings Mop with disinfectant NEVER use brooms or vacuums Wear N-100 HEPA-filtered mask Lethal traps and poisons to decrease rodent population No effective antiviral treatment (nor would it work anyway) Treatment limited to supportive care Extracorporeal membrane oxygenation (ECMO)