Respiratory System Chapter 13 1 Topics Respiratory Structures
![Steps of Respiration Airflow in the lungs is called ventilation. [AIR] EXCHANGE [BLOOD] Gases Steps of Respiration Airflow in the lungs is called ventilation. [AIR] EXCHANGE [BLOOD] Gases](https://slidetodoc.com/presentation_image_h2/adc24f557e52ae13bfbe75992fac7835/image-14.jpg)

![Effect of Plasma [H+] on Ventilation Regardless of the source, increases in the acidity Effect of Plasma [H+] on Ventilation Regardless of the source, increases in the acidity](https://slidetodoc.com/presentation_image_h2/adc24f557e52ae13bfbe75992fac7835/image-59.jpg)
![e. g. due to lactic acid Effect of Plasma [H+] on Ventilation Regardless of e. g. due to lactic acid Effect of Plasma [H+] on Ventilation Regardless of](https://slidetodoc.com/presentation_image_h2/adc24f557e52ae13bfbe75992fac7835/image-60.jpg)
![Hypoxia Deficiency of oxygen at the tissue level [there are 4 types of hypoxia] Hypoxia Deficiency of oxygen at the tissue level [there are 4 types of hypoxia]](https://slidetodoc.com/presentation_image_h2/adc24f557e52ae13bfbe75992fac7835/image-65.jpg)
- Slides: 67
Respiratory System Chapter 13 1
Topics • • • Respiratory Structures Ventilation & Lung Mechanics Gas Exchange in Alveoli & Tissues O 2, CO 2, and H+ Transport in Blood Control of Respiration Hypoxia 2
Respiratory System • Oral and nasal cavities, lungs, tubes that lead to lungs, and chest structures that move air into and out of lungs during breathing • Intakes oxygen and delivers it to the blood • Eliminates carbon dioxide (end product of metabolism) from the blood • Respiration: 1. Cellular Respiration = Utilization of oxygen in metabolism of organic molecules by cells; supplies energy to cells 2. *Pulmonary Physiology = Exchange of oxygen and carbon dioxide between organism and external environment 3
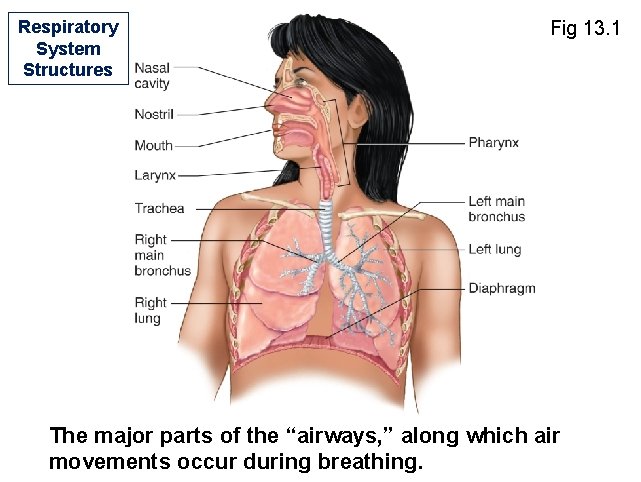
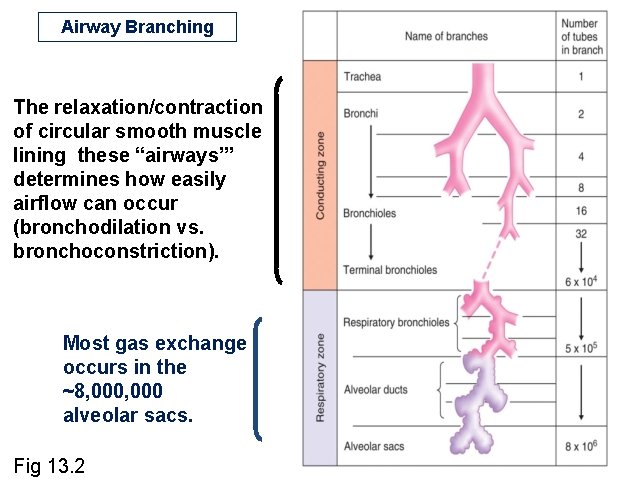
Inspiration/Inhalation • Movement of air from external environment through airways into alveoli of lungs during breathing Nose/Mouth→Pharynx→Larynx→Trachea →Bronchus→Lung • In lungs, bronchi undergo extensive branching → bronchioles → terminal bronchioles → respiratory bronchioles (some alveoli attached) → alveolar ducts → alveolar sacs §Alveolar sacs consist of alveoli (small, air-containing pockets; plural for alveolus), site of gas exchange with blood • Upper airways = nose/mouth, pharynx, larynx • Conducting zone = trachea to terminal bronchioles • Respiratory zone = respiratory bronchioles onward • Trachea and bronchi contain rings of cartilage. • Bronchioles are surrounded by smooth muscle, not cartilage. 4
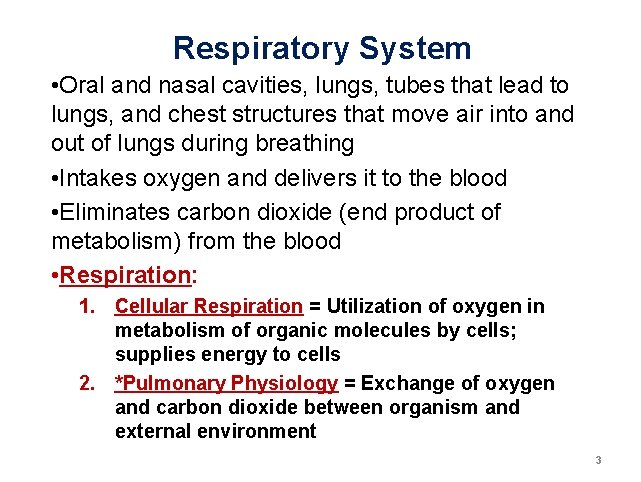
Respiratory System Structures Fig 13. 1 The major parts of the “airways, ” along which air movements occur during breathing.
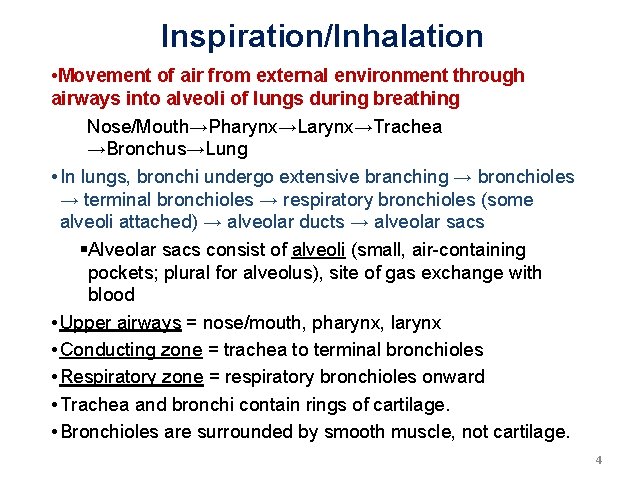
Airway Branching The relaxation/contraction of circular smooth muscle lining these “airways’” determines how easily airflow can occur (bronchodilation vs. bronchoconstriction). Most gas exchange occurs in the ~8, 000 alveolar sacs. Fig 13. 2
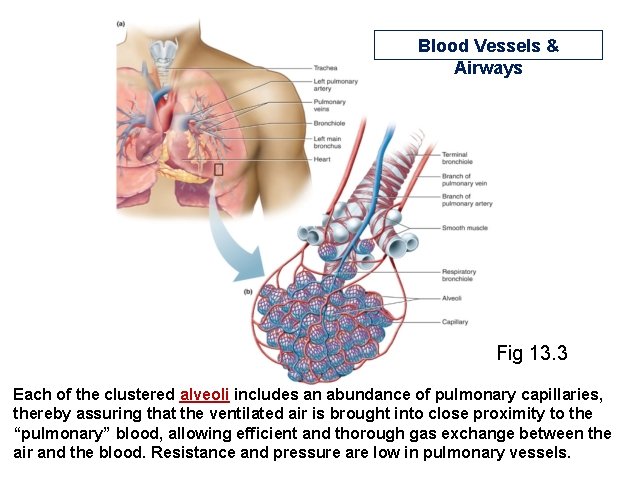
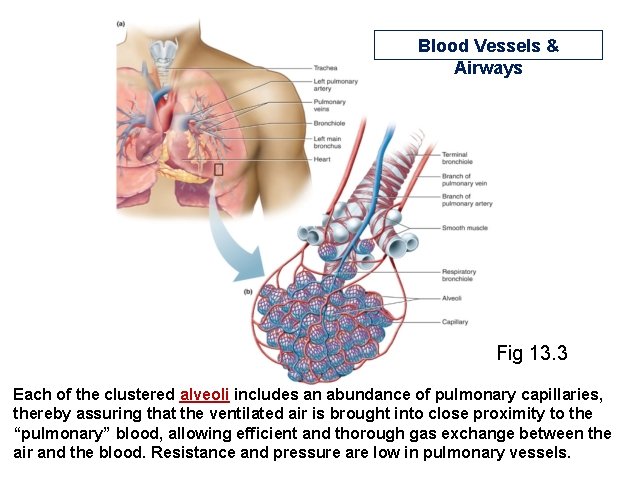
Blood Vessels & Airways Fig 13. 3 Each of the clustered alveoli includes an abundance of pulmonary capillaries, thereby assuring that the ventilated air is brought into close proximity to the “pulmonary” blood, allowing efficient and thorough gas exchange between the air and the blood. Resistance and pressure are low in pulmonary vessels.
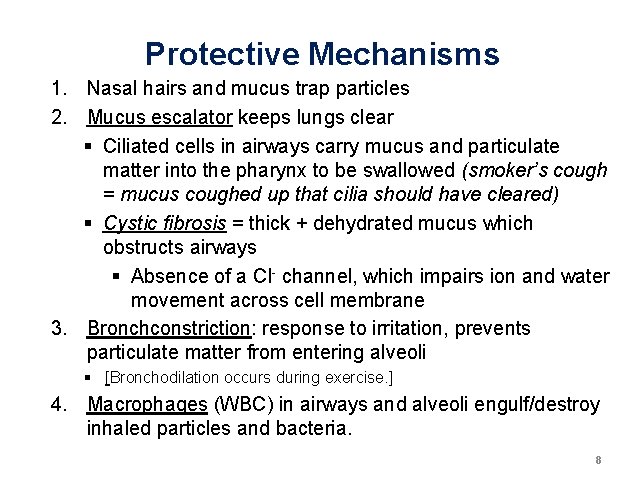
Protective Mechanisms 1. Nasal hairs and mucus trap particles 2. Mucus escalator keeps lungs clear § Ciliated cells in airways carry mucus and particulate matter into the pharynx to be swallowed (smoker’s cough = mucus coughed up that cilia should have cleared) § Cystic fibrosis = thick + dehydrated mucus which obstructs airways § Absence of a Cl- channel, which impairs ion and water movement across cell membrane 3. Bronchconstriction: response to irritation, prevents particulate matter from entering alveoli § [Bronchodilation occurs during exercise. ] 4. Macrophages (WBC) in airways and alveoli engulf/destroy inhaled particles and bacteria. 8
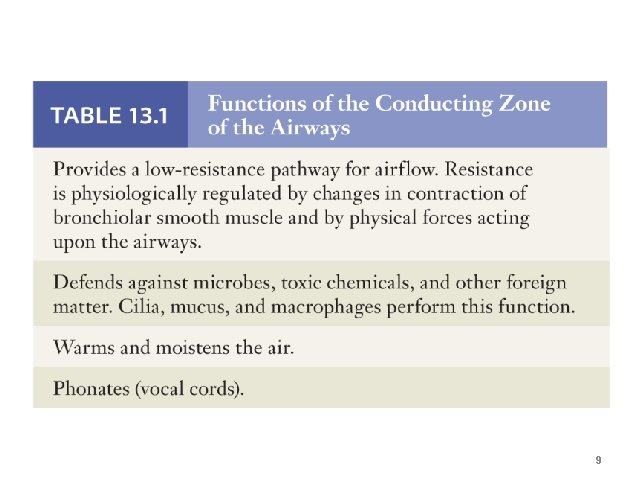
9
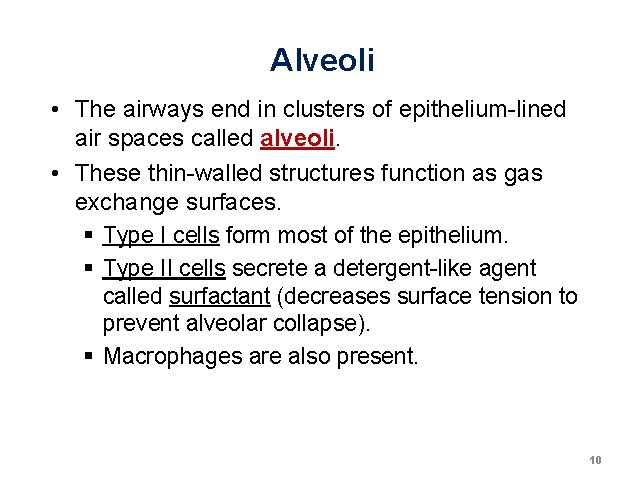
Alveoli • The airways end in clusters of epithelium-lined air spaces called alveoli. • These thin-walled structures function as gas exchange surfaces. § Type I cells form most of the epithelium. § Type II cells secrete a detergent-like agent called surfactant (decreases surface tension to prevent alveolar collapse). § Macrophages are also present. 10
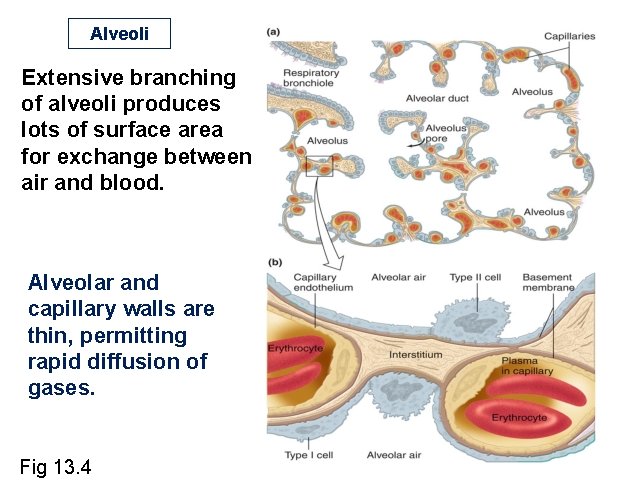
Alveoli Extensive branching of alveoli produces lots of surface area for exchange between air and blood. Alveolar and capillary walls are thin, permitting rapid diffusion of gases. Fig 13. 4
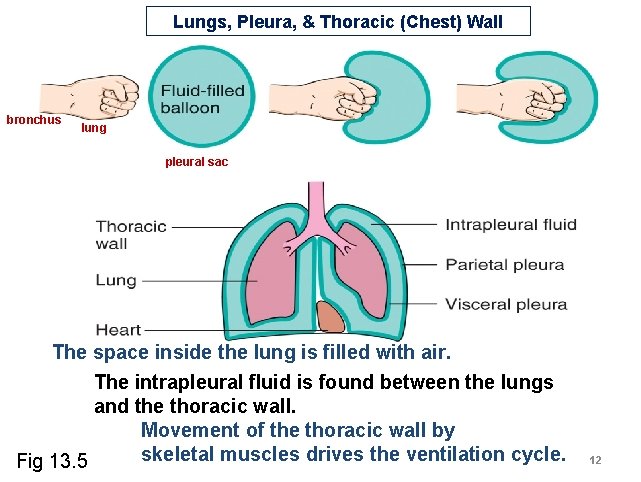
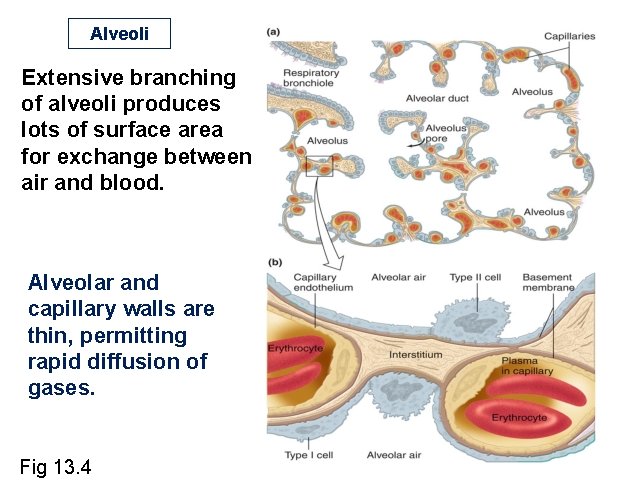
Lungs, Pleura, & Thoracic (Chest) Wall bronchus lung pleural sac The space inside the lung is filled with air. The intrapleural fluid is found between the lungs and the thoracic wall. Movement of the thoracic wall by skeletal muscles drives the ventilation cycle. Fig 13. 5 12
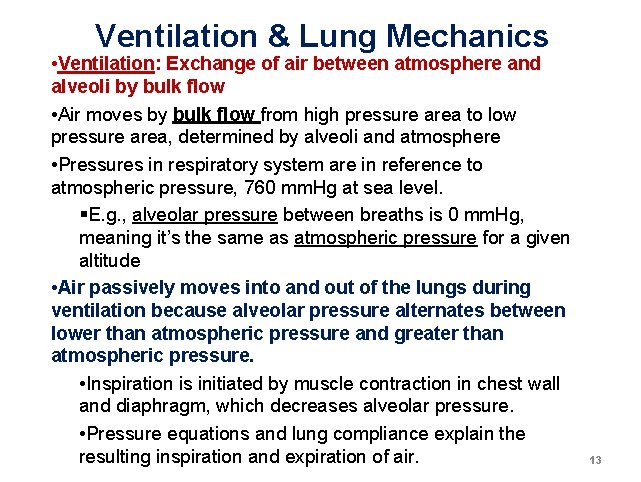
Ventilation & Lung Mechanics • Ventilation: Exchange of air between atmosphere and alveoli by bulk flow • Air moves by bulk flow from high pressure area to low pressure area, determined by alveoli and atmosphere • Pressures in respiratory system are in reference to atmospheric pressure, 760 mm. Hg at sea level. §E. g. , alveolar pressure between breaths is 0 mm. Hg, meaning it’s the same as atmospheric pressure for a given altitude • Air passively moves into and out of the lungs during ventilation because alveolar pressure alternates between lower than atmospheric pressure and greater than atmospheric pressure. • Inspiration is initiated by muscle contraction in chest wall and diaphragm, which decreases alveolar pressure. • Pressure equations and lung compliance explain the resulting inspiration and expiration of air. 13
![Steps of Respiration Airflow in the lungs is called ventilation AIR EXCHANGE BLOOD Gases Steps of Respiration Airflow in the lungs is called ventilation. [AIR] EXCHANGE [BLOOD] Gases](https://slidetodoc.com/presentation_image_h2/adc24f557e52ae13bfbe75992fac7835/image-14.jpg)
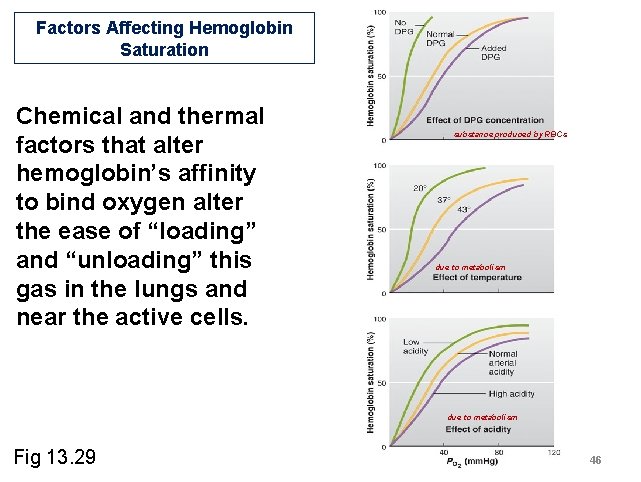
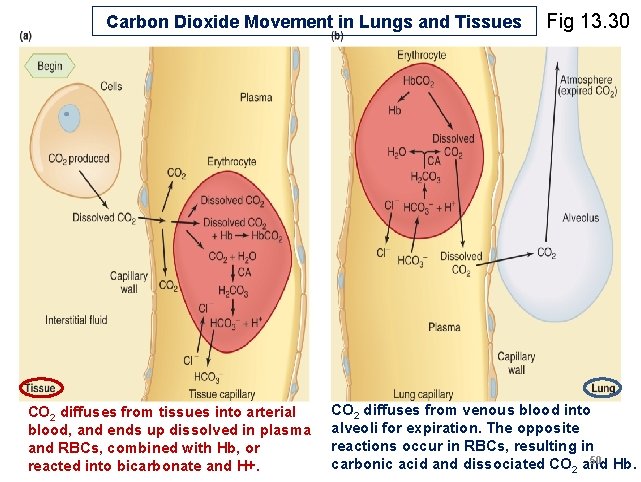
Steps of Respiration Airflow in the lungs is called ventilation. [AIR] EXCHANGE [BLOOD] Gases exchange by diffusion. Bloodflow through the pulmonary capillaries is driven by the contraction of the right ventricle. Fig 13. 6 14
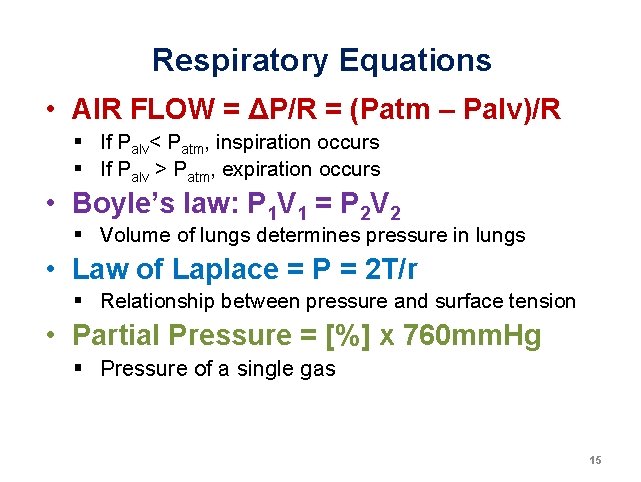
Respiratory Equations • AIR FLOW = ΔP/R = (Patm – Palv)/R § If Palv< Patm, inspiration occurs § If Palv > Patm, expiration occurs • Boyle’s law: P 1 V 1 = P 2 V 2 § Volume of lungs determines pressure in lungs • Law of Laplace = P = 2 T/r § Relationship between pressure and surface tension • Partial Pressure = [%] x 760 mm. Hg § Pressure of a single gas 15
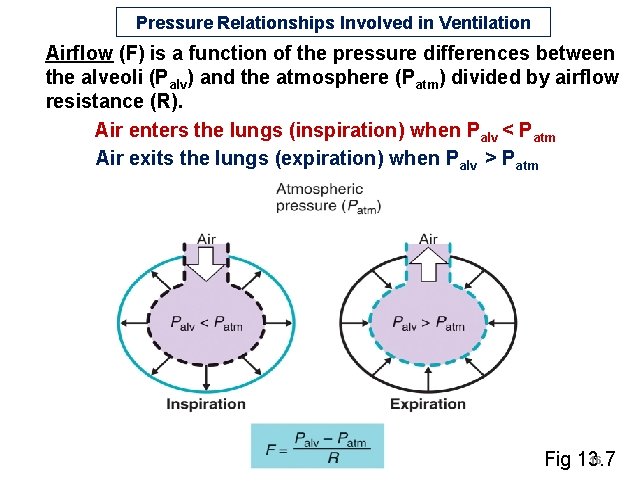
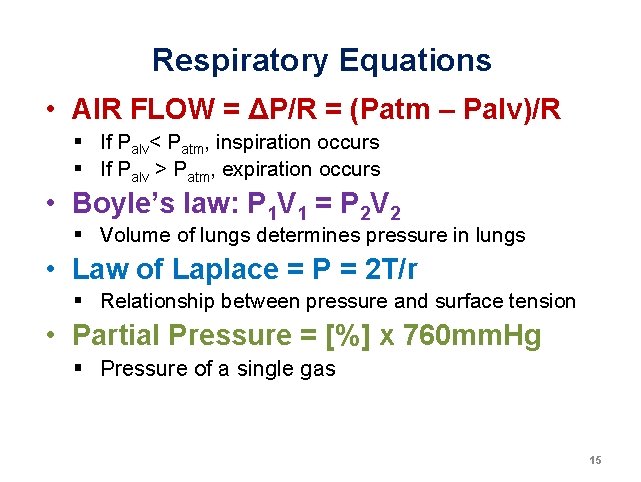
Pressure Relationships Involved in Ventilation Airflow (F) is a function of the pressure differences between the alveoli (Palv) and the atmosphere (Patm) divided by airflow resistance (R). Air enters the lungs (inspiration) when Palv < Patm Air exits the lungs (expiration) when Palv > Patm 1 16 Fig 13. 7
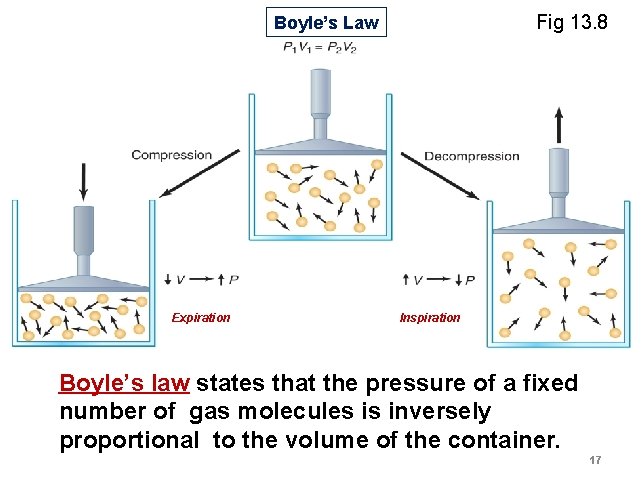
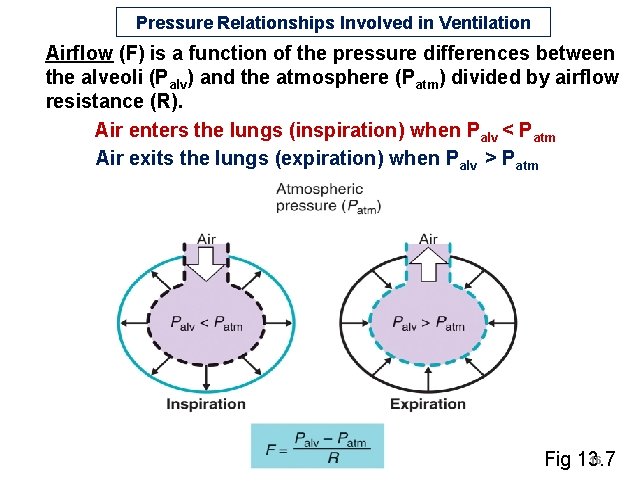
Fig 13. 8 Boyle’s Law Expiration Inspiration Boyle’s law states that the pressure of a fixed number of gas molecules is inversely proportional to the volume of the container. 17
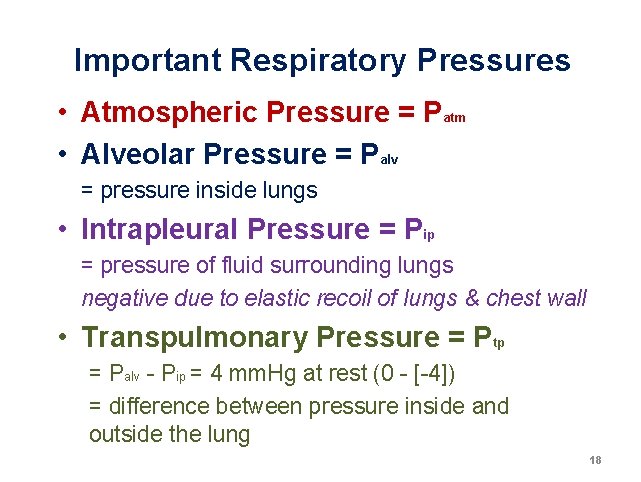
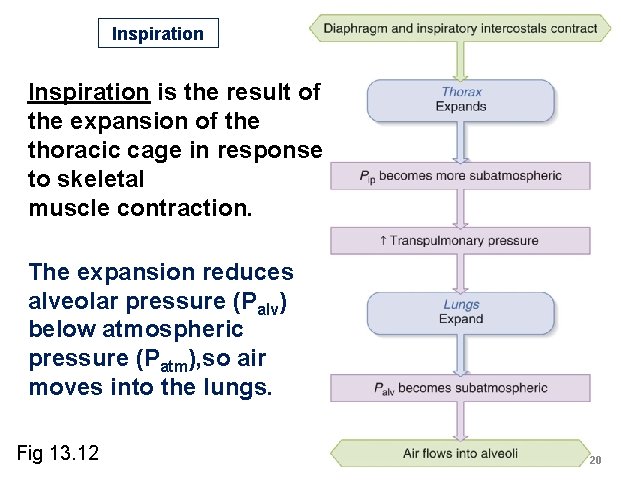
Important Respiratory Pressures • Atmospheric Pressure = Patm • Alveolar Pressure = Palv = pressure inside lungs • Intrapleural Pressure = Pip = pressure of fluid surrounding lungs negative due to elastic recoil of lungs & chest wall • Transpulmonary Pressure = Ptp = Palv - Pip = 4 mm. Hg at rest (0 - [-4]) = difference between pressure inside and outside the lung 18
Inspiration • Motor neuron signals initiate contraction of external intercostal muscles in chest wall (between ribs), resulting in expansion of thorax • Diaphragm also contracts downward to further expand thoracic cavity • Expansion of thorax results in passive enlargement of lungs, and decrease in Palv, which causes air to flow into alveoli • Degree of lung expansion and Ptp are directly proportional (due to change in Pip, which decreases with inspiration) • Lung compliance, or stretchability, also affects lung expansion 19
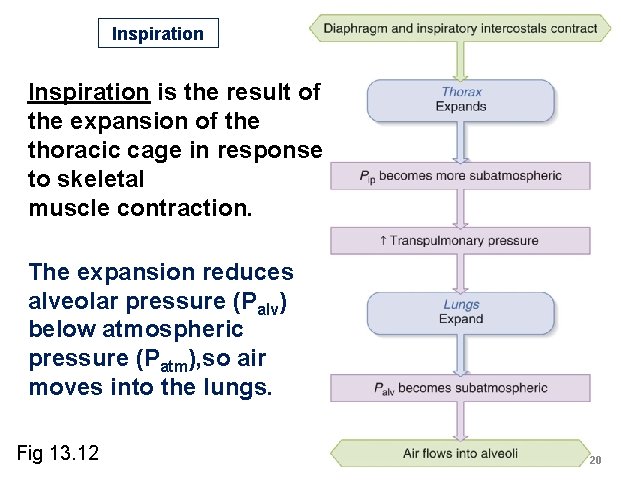
Inspiration is the result of the expansion of the thoracic cage in response to skeletal muscle contraction. The expansion reduces alveolar pressure (Palv) below atmospheric pressure (Patm), so air moves into the lungs. Fig 13. 12 20
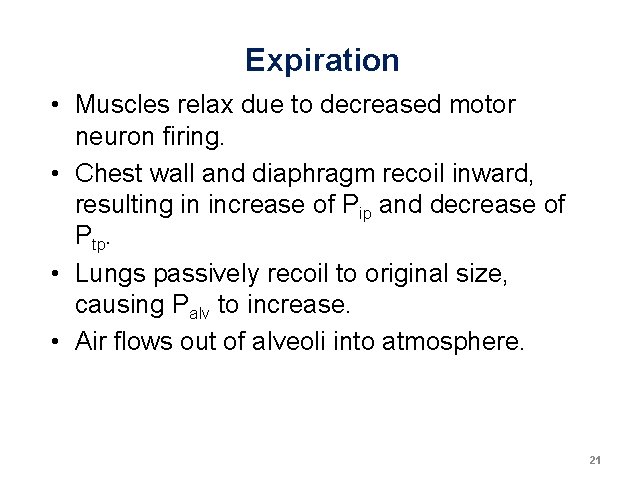
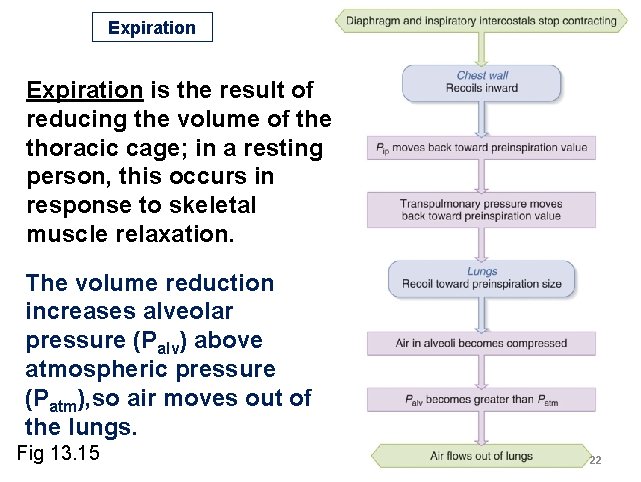
Expiration • Muscles relax due to decreased motor neuron firing. • Chest wall and diaphragm recoil inward, resulting in increase of Pip and decrease of Ptp. • Lungs passively recoil to original size, causing Palv to increase. • Air flows out of alveoli into atmosphere. 21
Expiration is the result of reducing the volume of the thoracic cage; in a resting person, this occurs in response to skeletal muscle relaxation. The volume reduction increases alveolar pressure (Palv) above atmospheric pressure (Patm), so air moves out of the lungs. Fig 13. 15 22
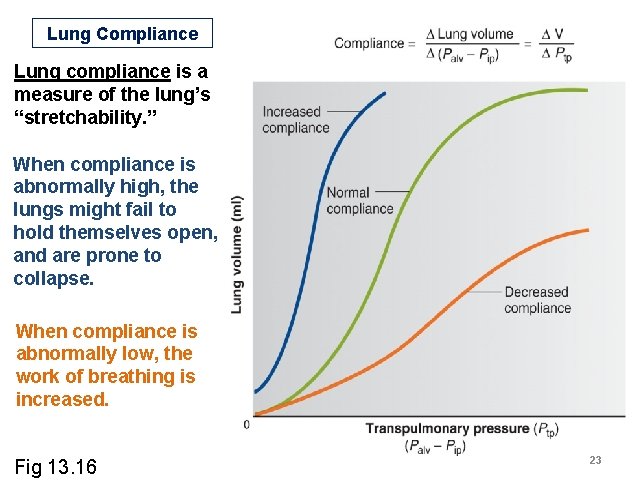
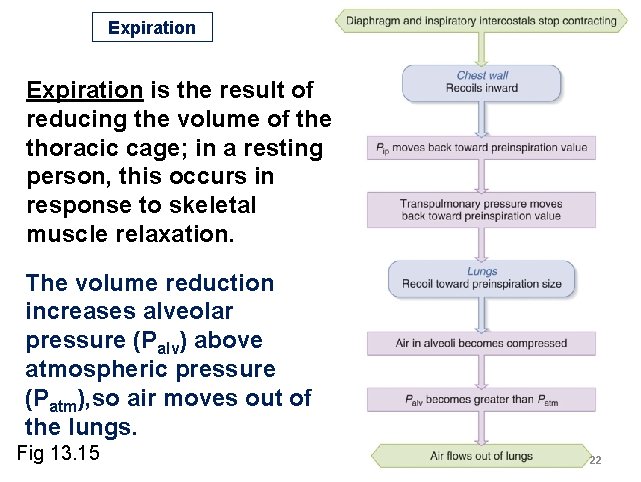
Lung Compliance Lung compliance is a measure of the lung’s “stretchability. ” When compliance is abnormally high, the lungs might fail to hold themselves open, and are prone to collapse. When compliance is abnormally low, the work of breathing is increased. Fig 13. 16 23
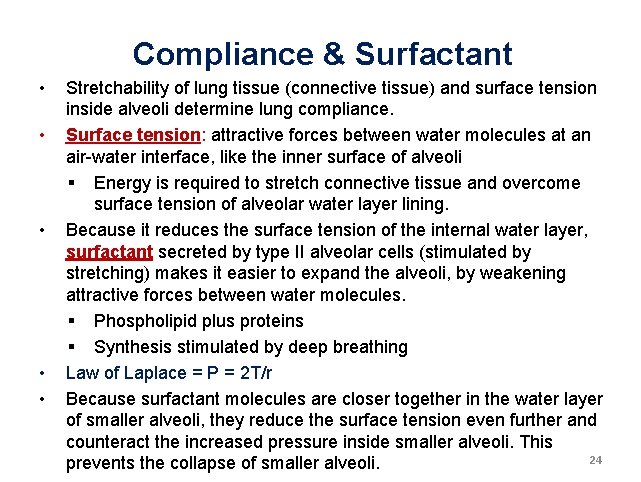
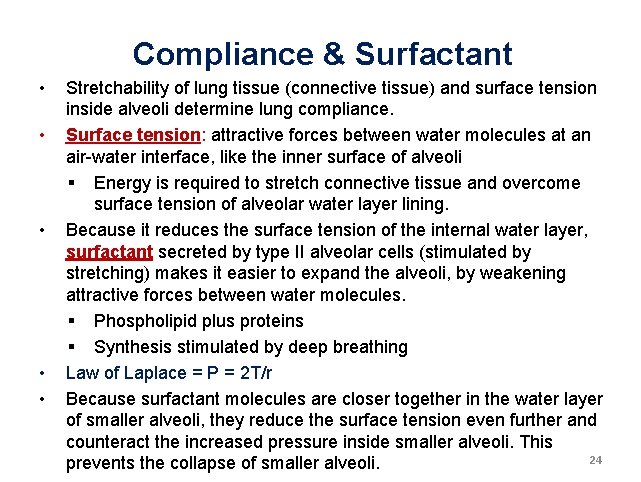
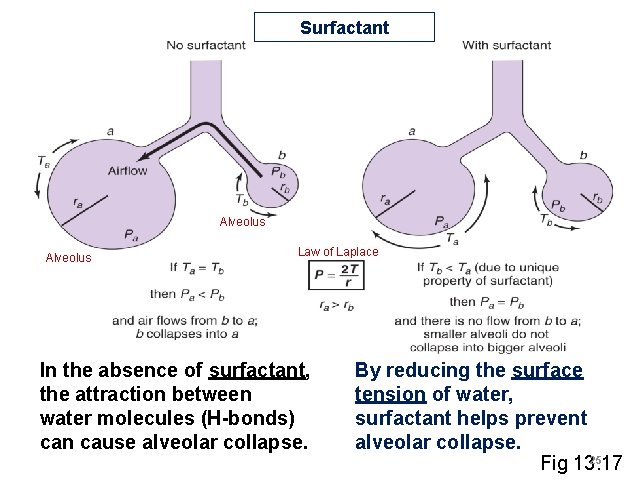
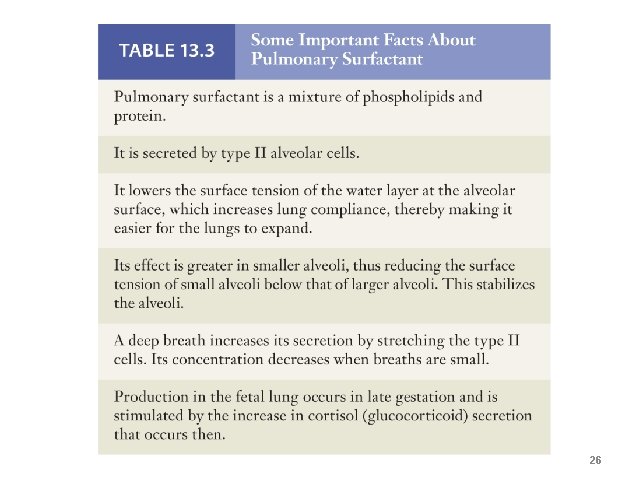
Compliance & Surfactant • • • Stretchability of lung tissue (connective tissue) and surface tension inside alveoli determine lung compliance. Surface tension: attractive forces between water molecules at an air-water interface, like the inner surface of alveoli § Energy is required to stretch connective tissue and overcome surface tension of alveolar water layer lining. Because it reduces the surface tension of the internal water layer, surfactant secreted by type II alveolar cells (stimulated by stretching) makes it easier to expand the alveoli, by weakening attractive forces between water molecules. § Phospholipid plus proteins § Synthesis stimulated by deep breathing Law of Laplace = P = 2 T/r Because surfactant molecules are closer together in the water layer of smaller alveoli, they reduce the surface tension even further and counteract the increased pressure inside smaller alveoli. This 24 prevents the collapse of smaller alveoli.
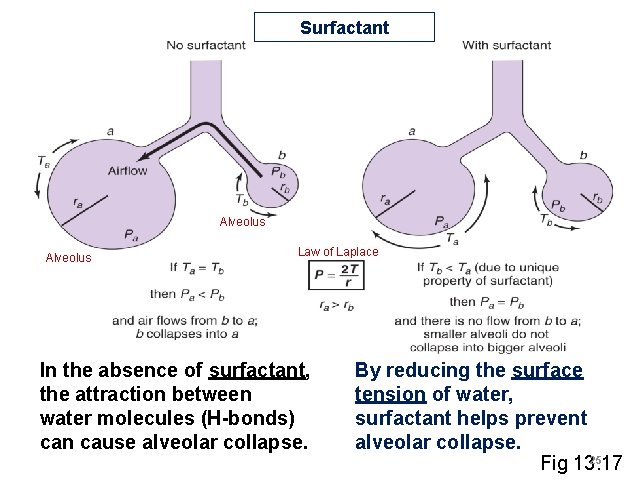
Surfactant Alveolus Law of Laplace In the absence of surfactant, the attraction between water molecules (H-bonds) can cause alveolar collapse. By reducing the surface tension of water, surfactant helps prevent alveolar collapse. 25 Fig 13. 17
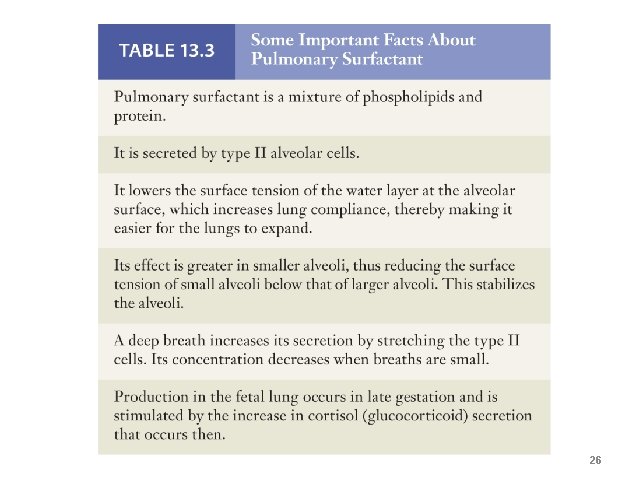
26
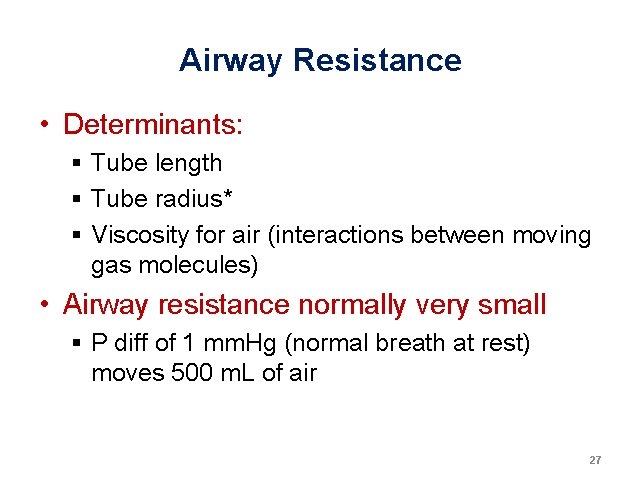
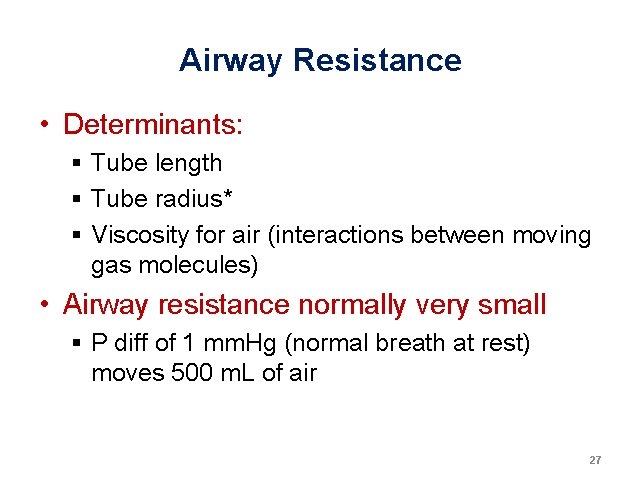
Airway Resistance • Determinants: § Tube length § Tube radius* § Viscosity for air (interactions between moving gas molecules) • Airway resistance normally very small § P diff of 1 mm. Hg (normal breath at rest) moves 500 m. L of air 27
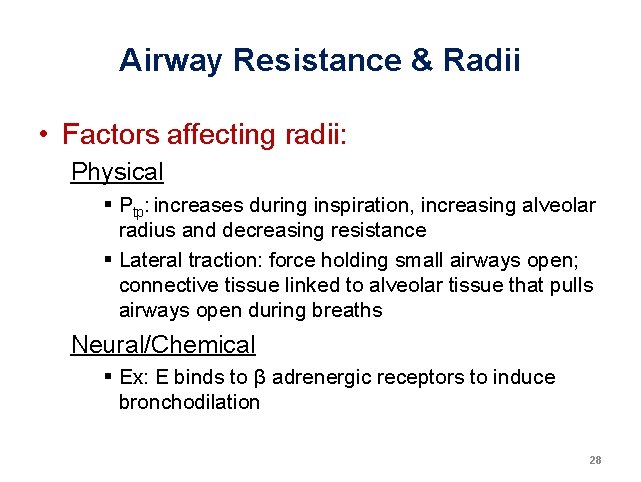
Airway Resistance & Radii • Factors affecting radii: Physical § Ptp: increases during inspiration, increasing alveolar radius and decreasing resistance § Lateral traction: force holding small airways open; connective tissue linked to alveolar tissue that pulls airways open during breaths Neural/Chemical § Ex: E binds to β adrenergic receptors to induce bronchodilation 28
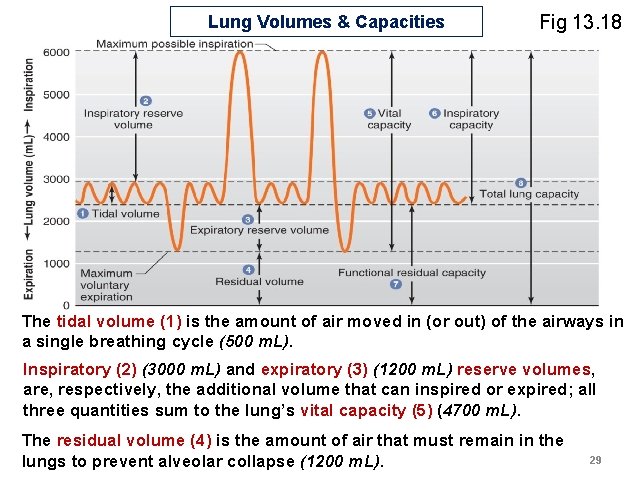
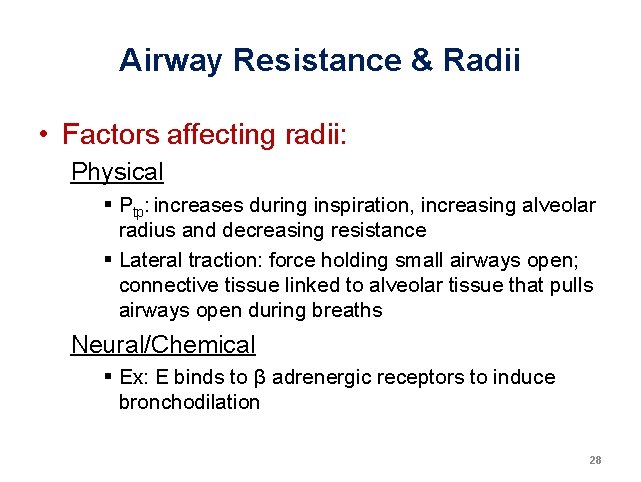
Lung Volumes & Capacities Fig 13. 18 The tidal volume (1) is the amount of air moved in (or out) of the airways in a single breathing cycle (500 m. L). Inspiratory (2) (3000 m. L) and expiratory (3) (1200 m. L) reserve volumes, are, respectively, the additional volume that can inspired or expired; all three quantities sum to the lung’s vital capacity (5) (4700 m. L). The residual volume (4) is the amount of air that must remain in the lungs to prevent alveolar collapse (1200 m. L). 29
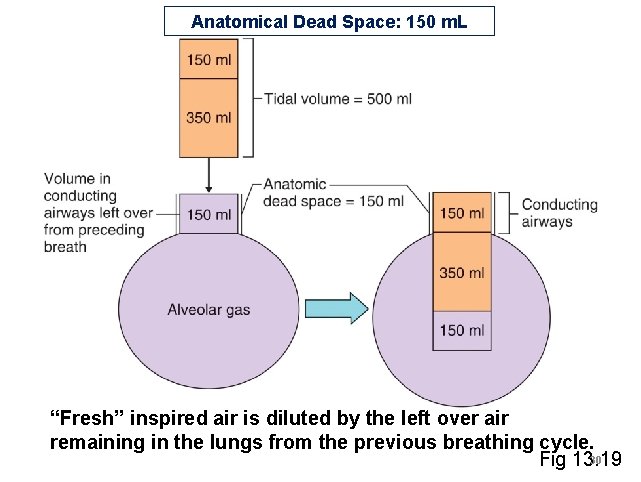
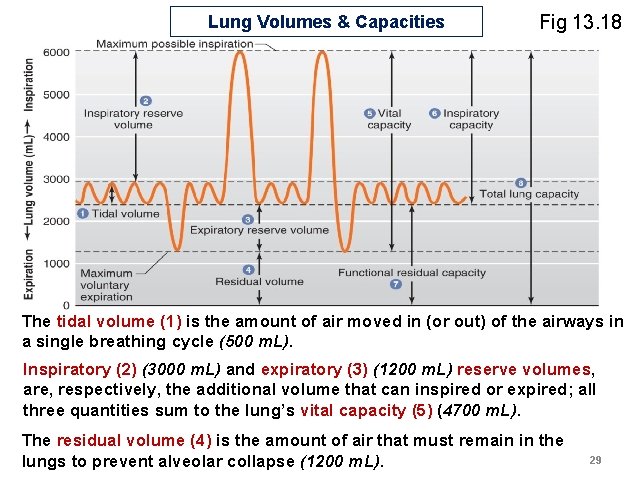
Anatomical Dead Space: 150 m. L “Fresh” inspired air is diluted by the left over air remaining in the lungs from the previous breathing cycle. 30 Fig 13. 19
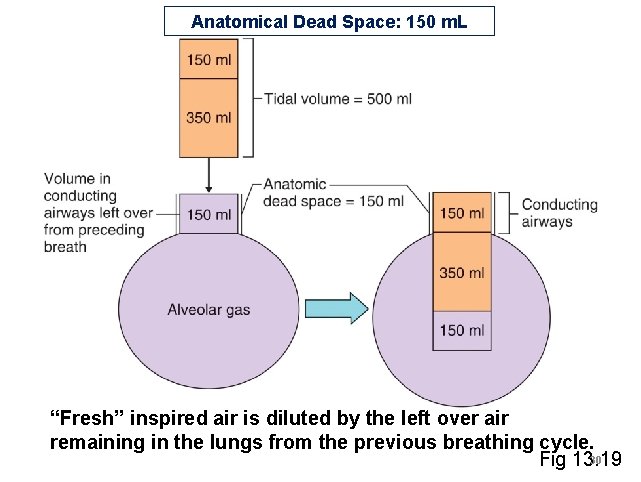
normal breathing 31
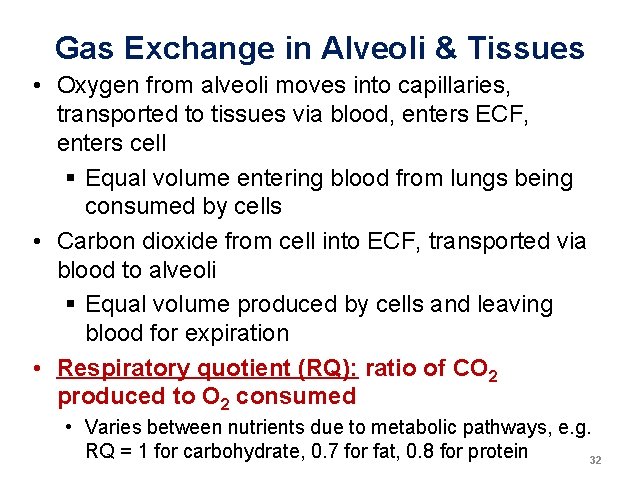
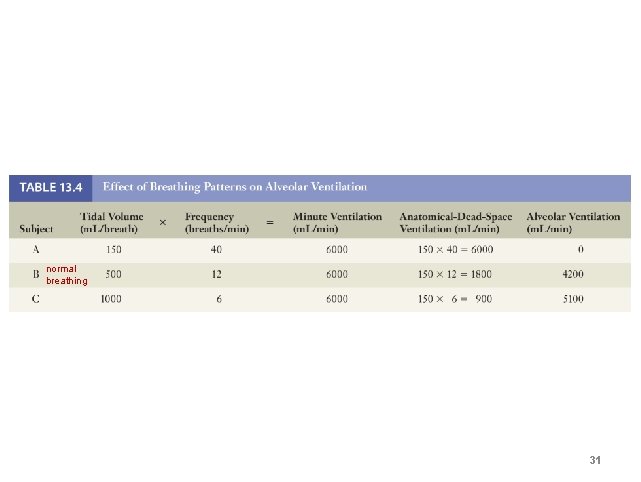
Gas Exchange in Alveoli & Tissues • Oxygen from alveoli moves into capillaries, transported to tissues via blood, enters ECF, enters cell § Equal volume entering blood from lungs being consumed by cells • Carbon dioxide from cell into ECF, transported via blood to alveoli § Equal volume produced by cells and leaving blood for expiration • Respiratory quotient (RQ): ratio of CO 2 produced to O 2 consumed • Varies between nutrients due to metabolic pathways, e. g. RQ = 1 for carbohydrate, 0. 7 for fat, 0. 8 for protein 32
Exchange of Gases In 1 Minute For RQ = 0. 8 21% of 4000 m. L inspired In the lungs, the concentration gradients favor the inward (toward the blood) diffusion of oxygen and the outward (toward the alveolar air) diffusion of carbon dioxide; owing to the metabolic activities of cells, these gradients are reversed 33 Fig 13. 20 at the interface of the blood and the active cells.
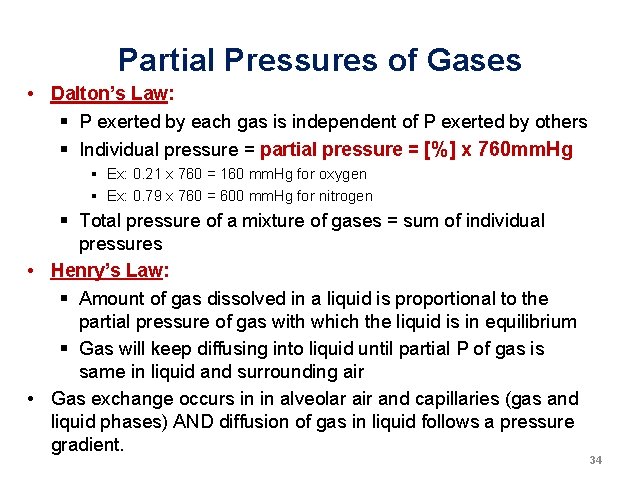
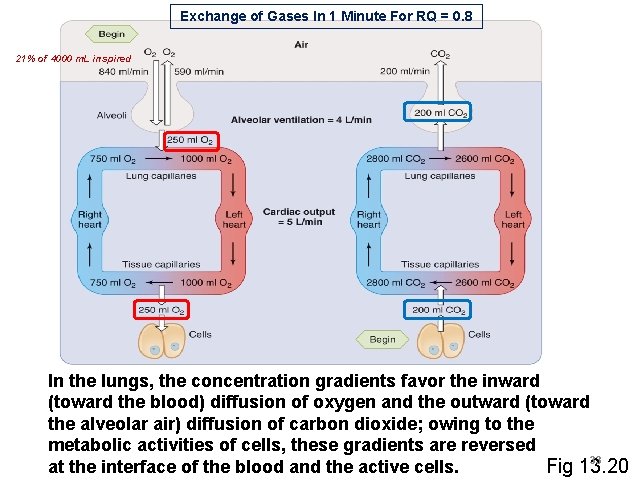
Partial Pressures of Gases • Dalton’s Law: § P exerted by each gas is independent of P exerted by others § Individual pressure = partial pressure = [%] x 760 mm. Hg § Ex: 0. 21 x 760 = 160 mm. Hg for oxygen § Ex: 0. 79 x 760 = 600 mm. Hg for nitrogen § Total pressure of a mixture of gases = sum of individual pressures • Henry’s Law: § Amount of gas dissolved in a liquid is proportional to the partial pressure of gas with which the liquid is in equilibrium § Gas will keep diffusing into liquid until partial P of gas is same in liquid and surrounding air • Gas exchange occurs in in alveolar air and capillaries (gas and liquid phases) AND diffusion of gas in liquid follows a pressure gradient. 34
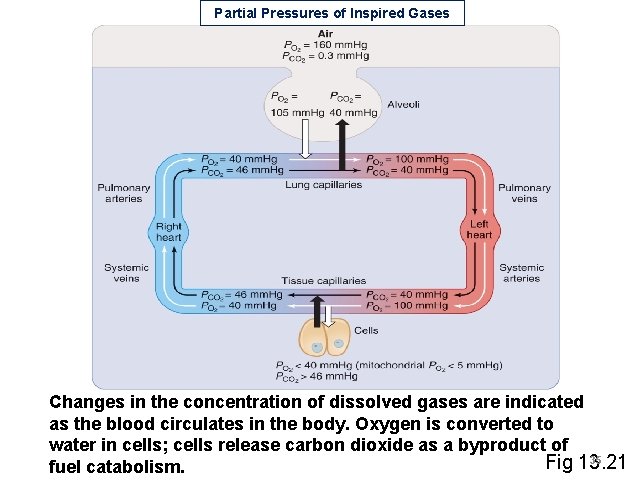
Partial Pressures of Inspired Gases Changes in the concentration of dissolved gases are indicated as the blood circulates in the body. Oxygen is converted to water in cells; cells release carbon dioxide as a byproduct of 35 Fig 13. 21 fuel catabolism.
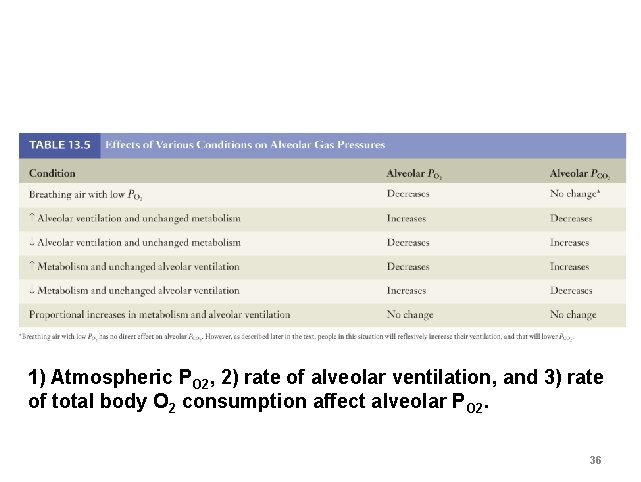
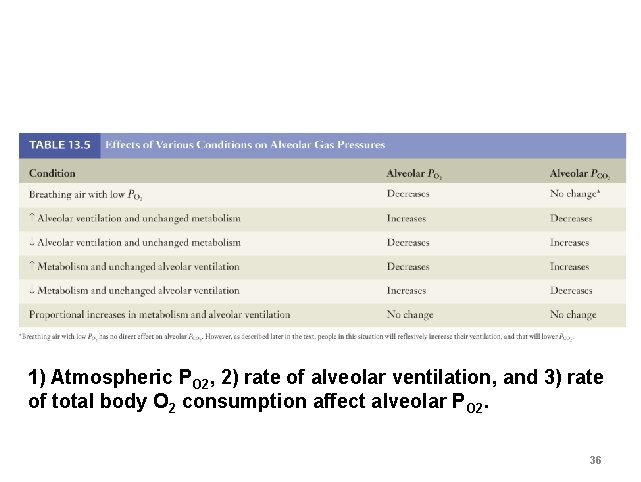
1) Atmospheric PO 2, 2) rate of alveolar ventilation, and 3) rate of total body O 2 consumption affect alveolar PO 2. 36
Relationship Between Alveolar Ventilation & Alveolar Partial Pressures Changes in the rate of ventilation alter the concentration of gases in the alveolar air. Hypoventilation and hyperventilation are in relation to the ratio of CO 2 production to ventilation. Fig 13. 22 37
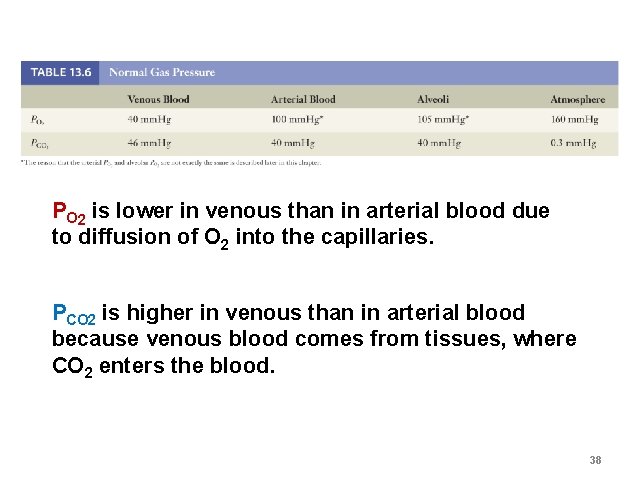
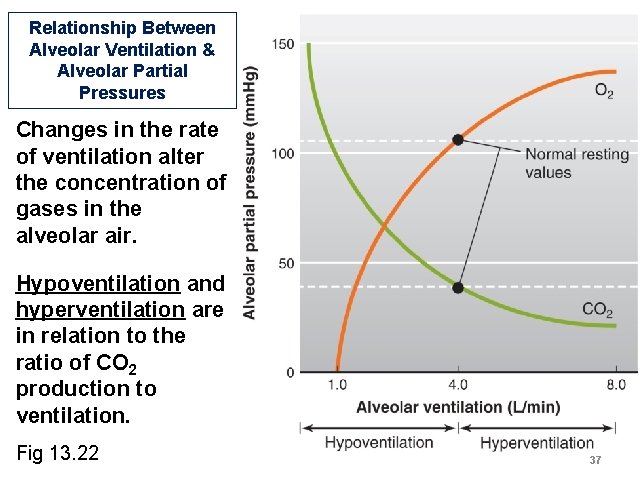
PO 2 is lower in venous than in arterial blood due to diffusion of O 2 into the capillaries. PCO 2 is higher in venous than in arterial blood because venous blood comes from tissues, where CO 2 enters the blood. 38
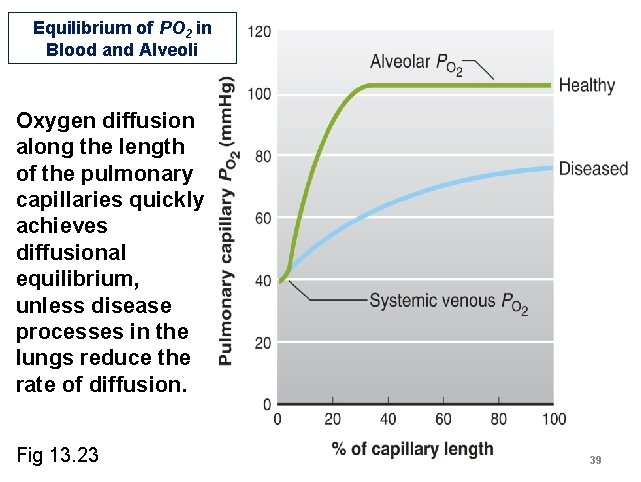
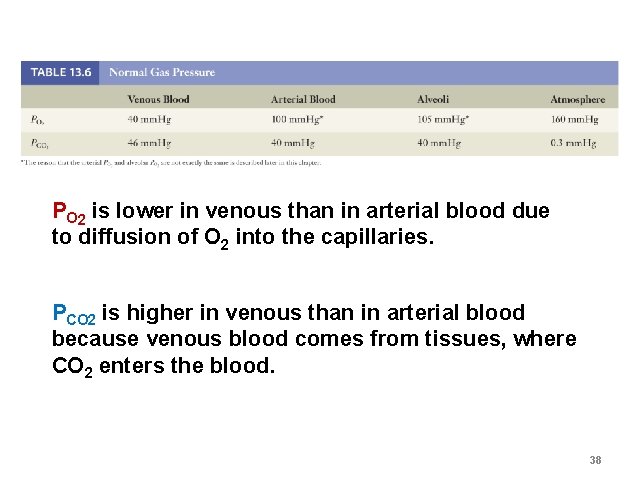
Equilibrium of PO 2 in Blood and Alveoli Oxygen diffusion along the length of the pulmonary capillaries quickly achieves diffusional equilibrium, unless disease processes in the lungs reduce the rate of diffusion. Fig 13. 23 39
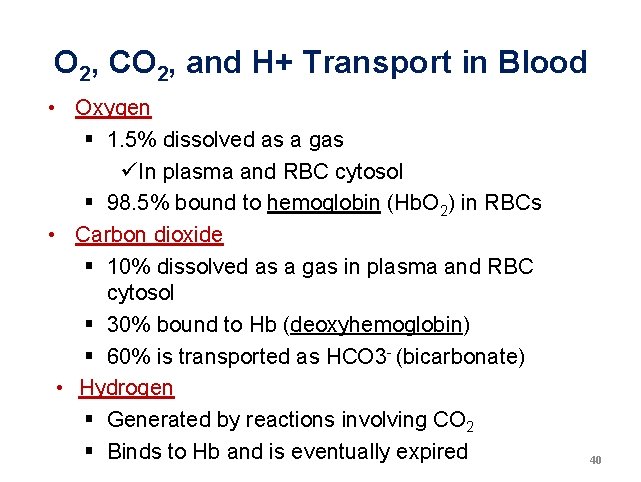
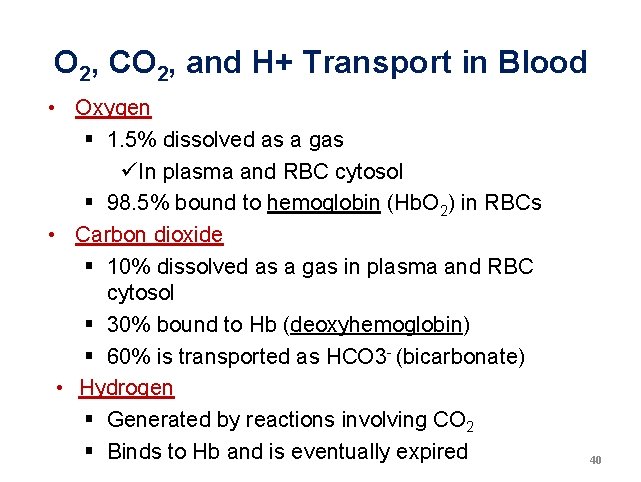
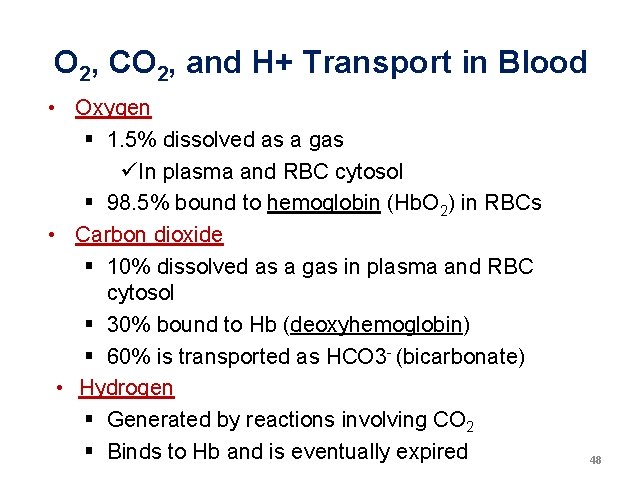
O 2, CO 2, and H+ Transport in Blood • Oxygen § 1. 5% dissolved as a gas üIn plasma and RBC cytosol § 98. 5% bound to hemoglobin (Hb. O 2) in RBCs • Carbon dioxide § 10% dissolved as a gas in plasma and RBC cytosol § 30% bound to Hb (deoxyhemoglobin) § 60% is transported as HCO 3 - (bicarbonate) • Hydrogen § Generated by reactions involving CO 2 § Binds to Hb and is eventually expired 40
in plasma and RBC cytosol in RBCs 41
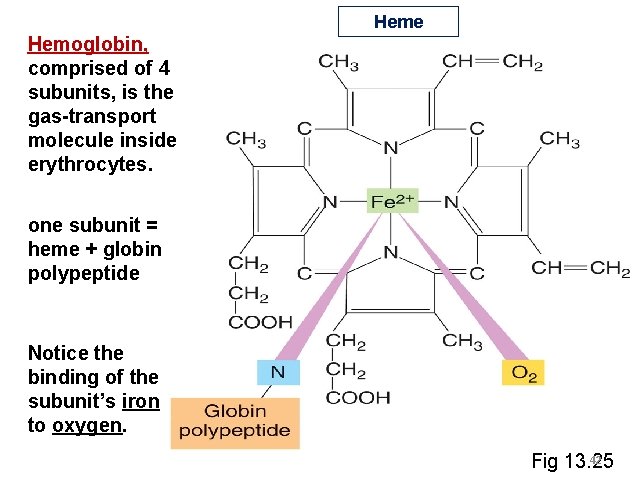
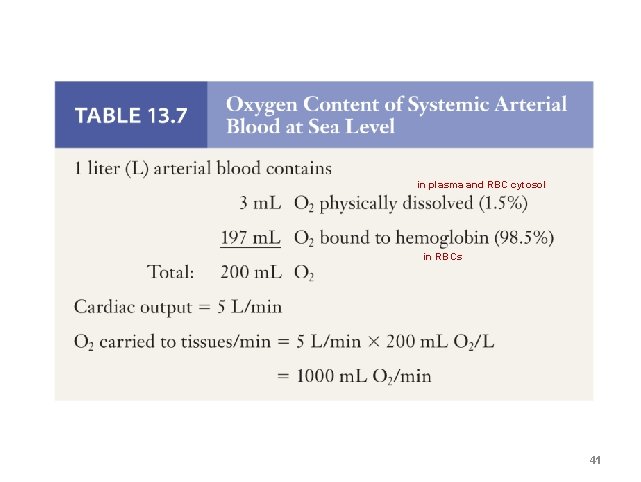
Heme Hemoglobin, comprised of 4 subunits, is the gas-transport molecule inside erythrocytes. one subunit = heme + globin polypeptide Notice the binding of the subunit’s iron to oxygen. 42 Fig 13. 25
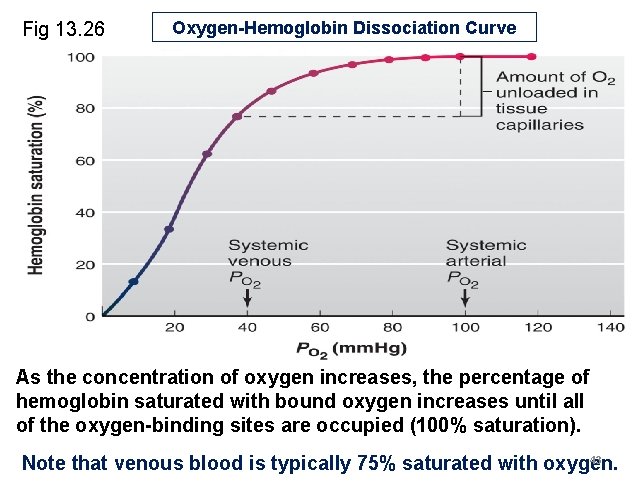
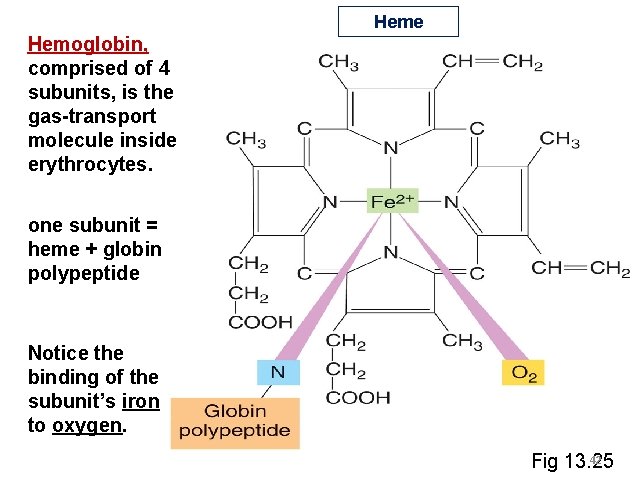
Fig 13. 26 Oxygen-Hemoglobin Dissociation Curve As the concentration of oxygen increases, the percentage of hemoglobin saturated with bound oxygen increases until all of the oxygen-binding sites are occupied (100% saturation). 43 Note that venous blood is typically 75% saturated with oxygen.
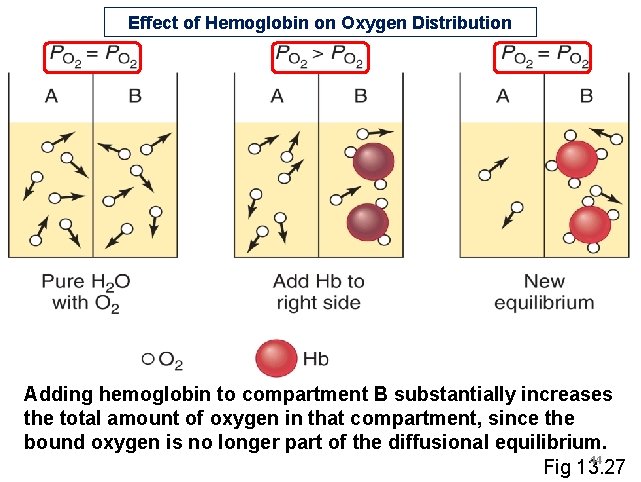
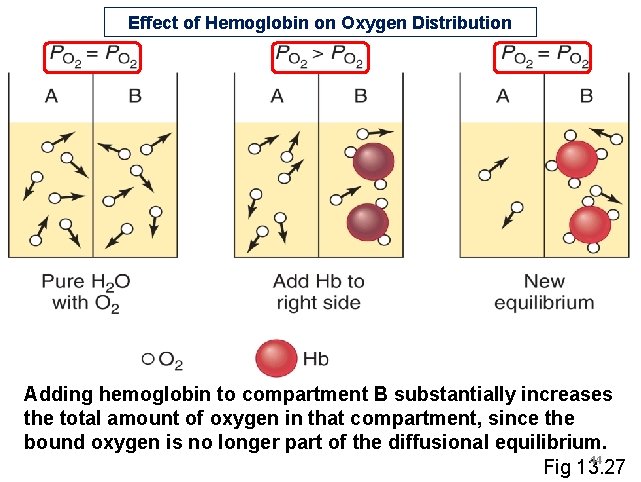
Effect of Hemoglobin on Oxygen Distribution Adding hemoglobin to compartment B substantially increases the total amount of oxygen in that compartment, since the bound oxygen is no longer part of the diffusional equilibrium. 44 Fig 13. 27
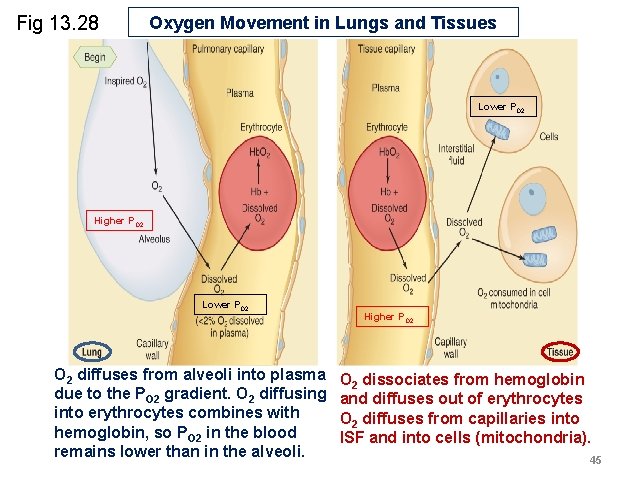
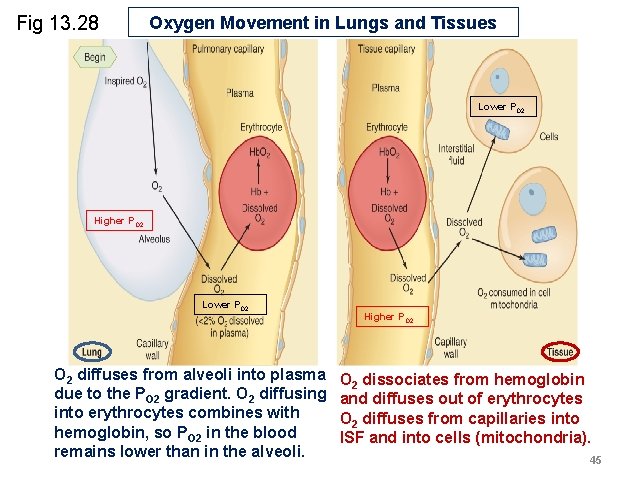
Fig 13. 28 Oxygen Movement in Lungs and Tissues Lower PO 2 Higher PO 2 Lower PO 2 diffuses from alveoli into plasma due to the PO 2 gradient. O 2 diffusing into erythrocytes combines with hemoglobin, so PO 2 in the blood remains lower than in the alveoli. Higher PO 2 dissociates from hemoglobin and diffuses out of erythrocytes O 2 diffuses from capillaries into ISF and into cells (mitochondria). 45
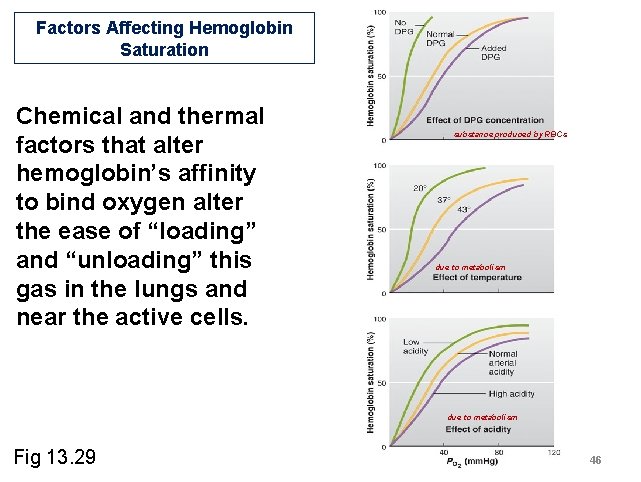
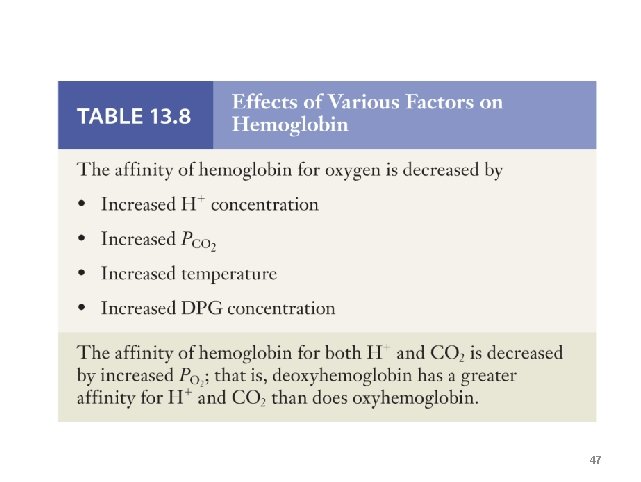
Factors Affecting Hemoglobin Saturation Chemical and thermal factors that alter hemoglobin’s affinity to bind oxygen alter the ease of “loading” and “unloading” this gas in the lungs and near the active cells. substance produced by RBCs due to metabolism Fig 13. 29 46
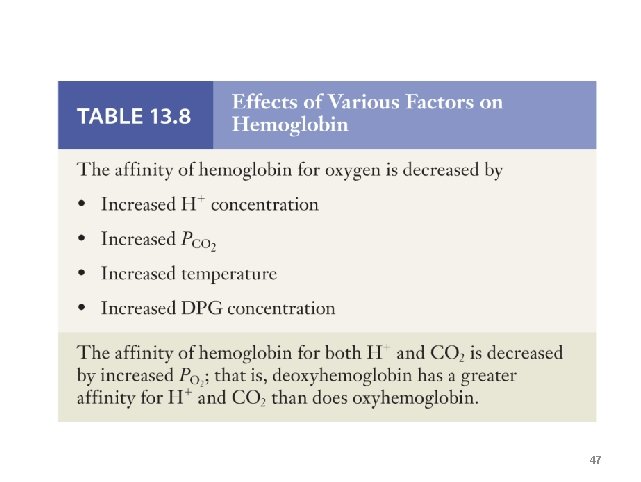
47
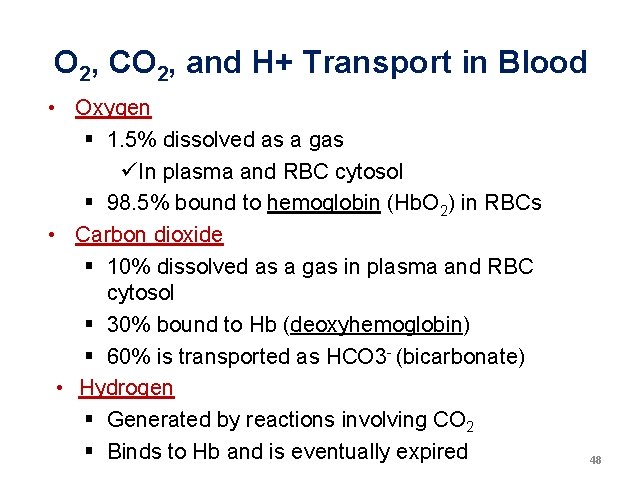
O 2, CO 2, and H+ Transport in Blood • Oxygen § 1. 5% dissolved as a gas üIn plasma and RBC cytosol § 98. 5% bound to hemoglobin (Hb. O 2) in RBCs • Carbon dioxide § 10% dissolved as a gas in plasma and RBC cytosol § 30% bound to Hb (deoxyhemoglobin) § 60% is transported as HCO 3 - (bicarbonate) • Hydrogen § Generated by reactions involving CO 2 § Binds to Hb and is eventually expired 48
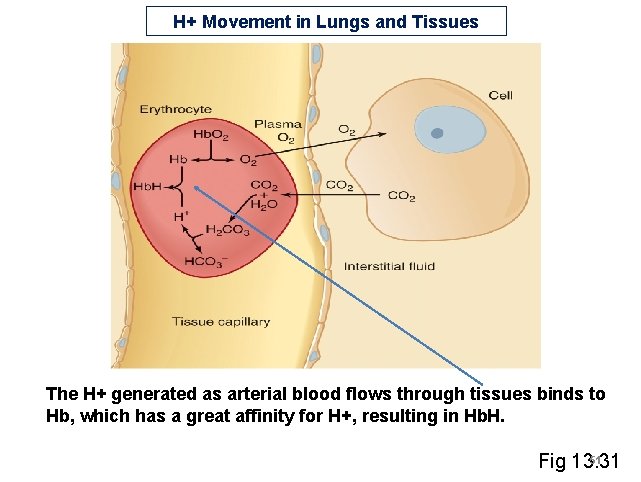
CO 2 Chemistry CO 2(g) + H 2 O Carbon Dioxide Water H 2 CO 3 Carbonic Acid H+ + HCO 3 Hydrogen Ion Bicarbonate • Carbonic anhydrase in RBCs catalyzes this reaction • Controlling [CO 2] means controlling p. H 49
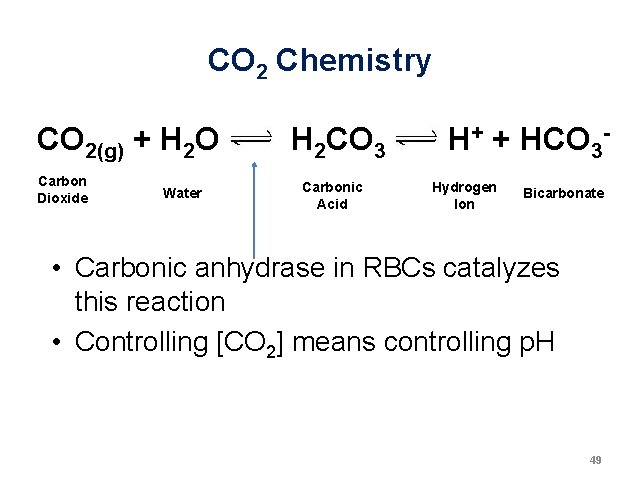
Carbon Dioxide Movement in Lungs and Tissues CO 2 diffuses from tissues into arterial blood, and ends up dissolved in plasma and RBCs, combined with Hb, or reacted into bicarbonate and H+. Fig 13. 30 CO 2 diffuses from venous blood into alveoli for expiration. The opposite reactions occur in RBCs, resulting in 50 Hb. carbonic acid and dissociated CO 2 and
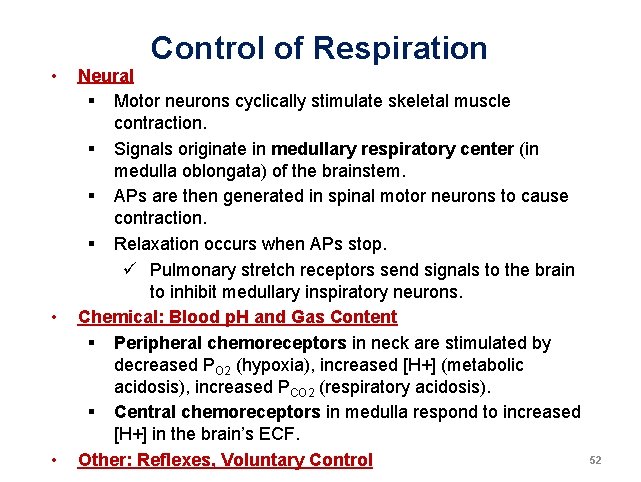
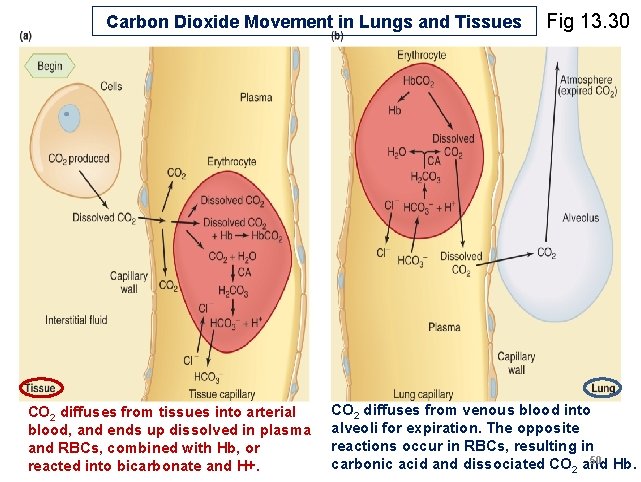
H+ Movement in Lungs and Tissues The H+ generated as arterial blood flows through tissues binds to Hb, which has a great affinity for H+, resulting in Hb. H. 51 Fig 13. 31
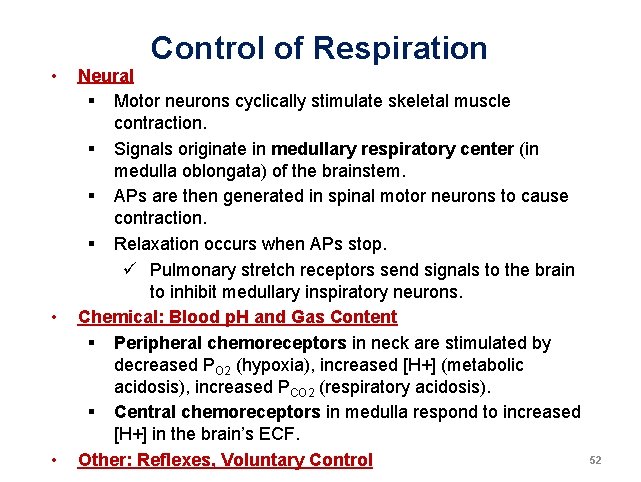
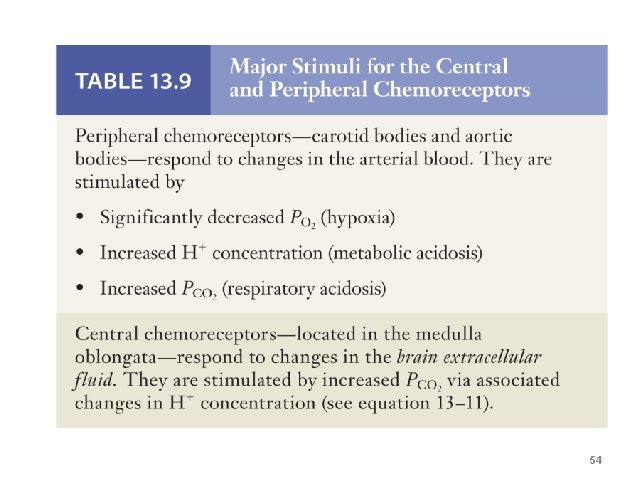
• • • Control of Respiration Neural § Motor neurons cyclically stimulate skeletal muscle contraction. § Signals originate in medullary respiratory center (in medulla oblongata) of the brainstem. § APs are then generated in spinal motor neurons to cause contraction. § Relaxation occurs when APs stop. ü Pulmonary stretch receptors send signals to the brain to inhibit medullary inspiratory neurons. Chemical: Blood p. H and Gas Content § Peripheral chemoreceptors in neck are stimulated by decreased PO 2 (hypoxia), increased [H+] (metabolic acidosis), increased PCO 2 (respiratory acidosis). § Central chemoreceptors in medulla respond to increased [H+] in the brain’s ECF. Other: Reflexes, Voluntary Control 52
Chemical Control of Respiration Chemosensory neurons (red circles) that respond to changes in blood p. H and gas content are located in the aorta and in the carotid sinuses, near the arterial baroreceptors. These sensory afferent neurons alter CNS regulation of the rate of ventilation. Fig 13. 33 53
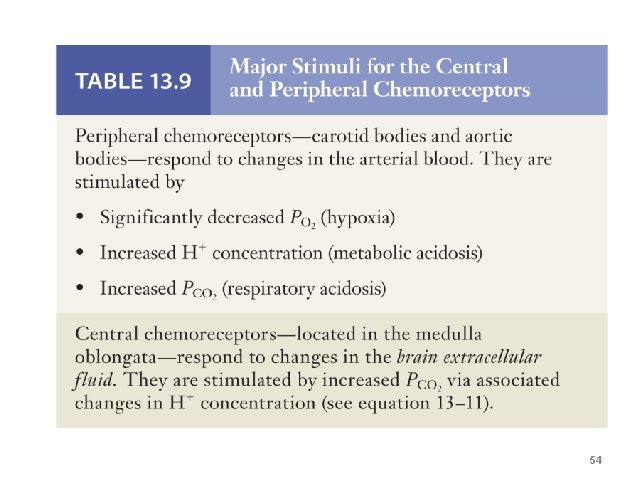
54

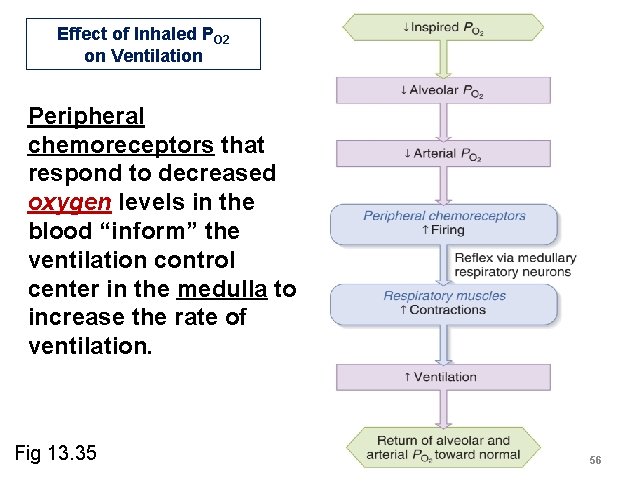
Effect of Inhaled PO 2 on Ventilation A severe reduction in the arterial concentration of oxygen in the blood can stimulate hyperventilation. 55 Fig 13. 34
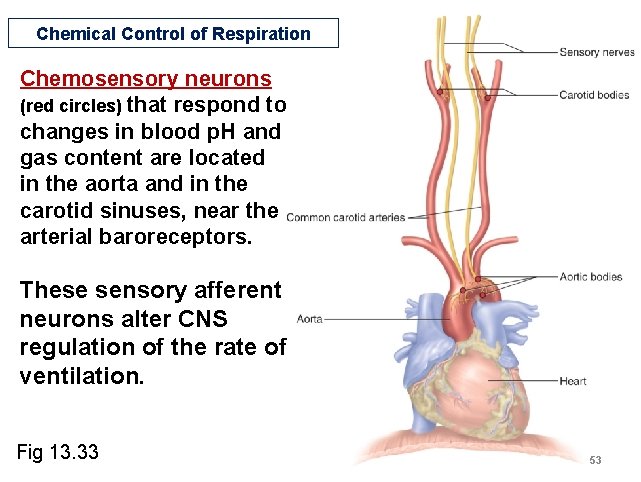
Effect of Inhaled PO 2 on Ventilation Peripheral chemoreceptors that respond to decreased oxygen levels in the blood “inform” the ventilation control center in the medulla to increase the rate of ventilation. Fig 13. 35 56
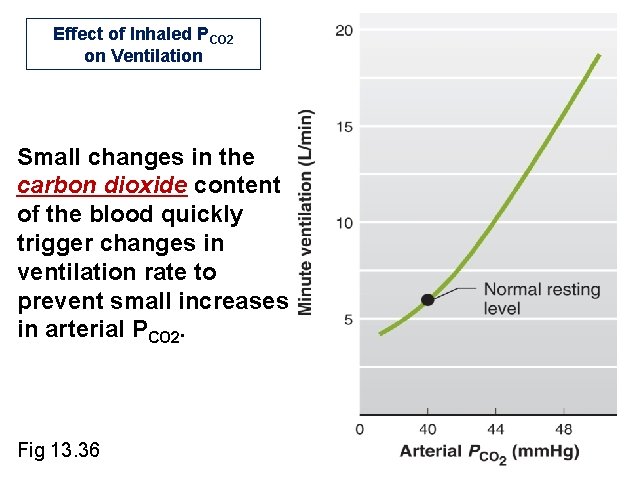
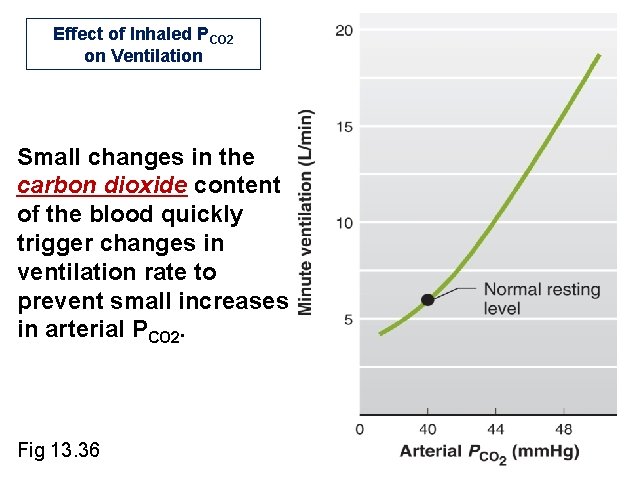
Effect of Inhaled PCO 2 on Ventilation Small changes in the carbon dioxide content of the blood quickly trigger changes in ventilation rate to prevent small increases in arterial PCO 2. Fig 13. 36
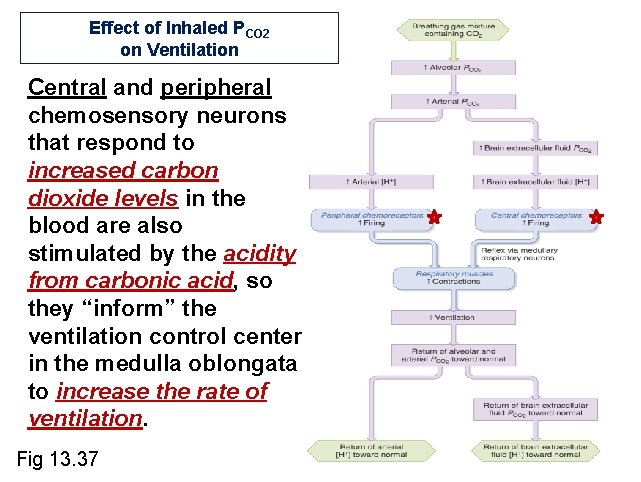
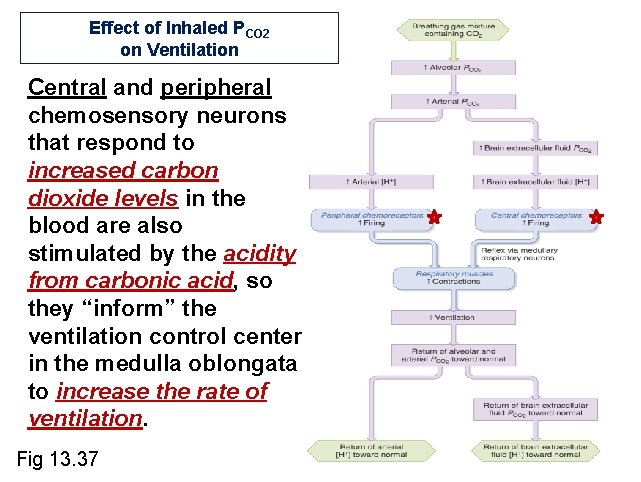
Effect of Inhaled PCO 2 on Ventilation Central and peripheral chemosensory neurons that respond to increased carbon dioxide levels in the blood are also stimulated by the acidity from carbonic acid, so they “inform” the ventilation control center in the medulla oblongata to increase the rate of ventilation. Fig 13. 37
![Effect of Plasma H on Ventilation Regardless of the source increases in the acidity Effect of Plasma [H+] on Ventilation Regardless of the source, increases in the acidity](https://slidetodoc.com/presentation_image_h2/adc24f557e52ae13bfbe75992fac7835/image-59.jpg)
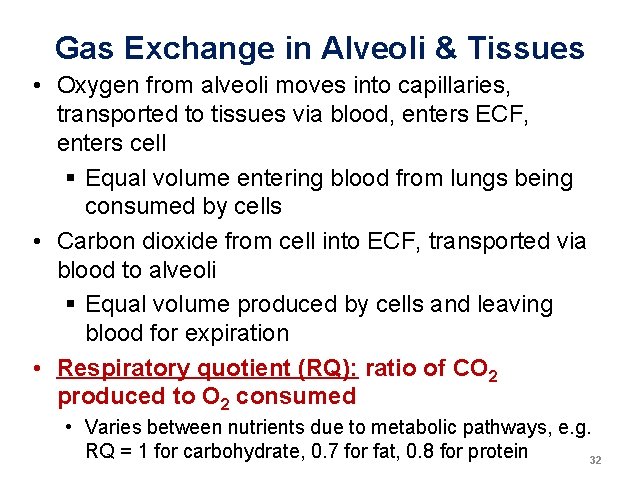
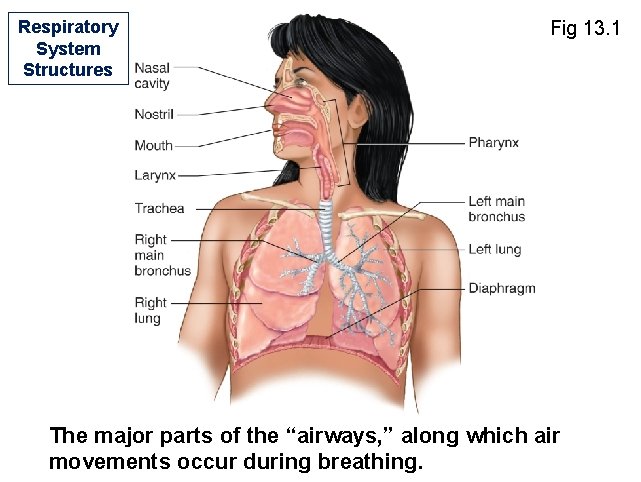
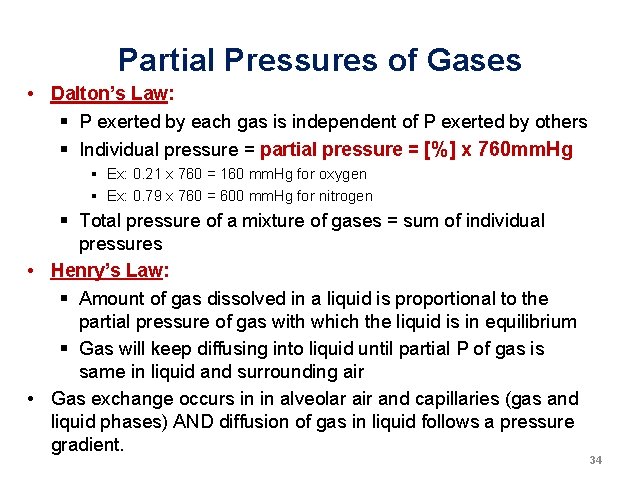
Effect of Plasma [H+] on Ventilation Regardless of the source, increases in the acidity of the blood cause hyperventilation. Causes of [H+] Change: Respiratory acidosis Respiratory alkalosis Metabolic acidosis Metabolic alkalosis Fig 13. 38 administration of lactic acid
![e g due to lactic acid Effect of Plasma H on Ventilation Regardless of e. g. due to lactic acid Effect of Plasma [H+] on Ventilation Regardless of](https://slidetodoc.com/presentation_image_h2/adc24f557e52ae13bfbe75992fac7835/image-60.jpg)
e. g. due to lactic acid Effect of Plasma [H+] on Ventilation Regardless of the source, increases in the acidity of the blood cause hyperventilation, even if carbon dioxide levels are driven to abnormally low levels. Fig 13. 39 60
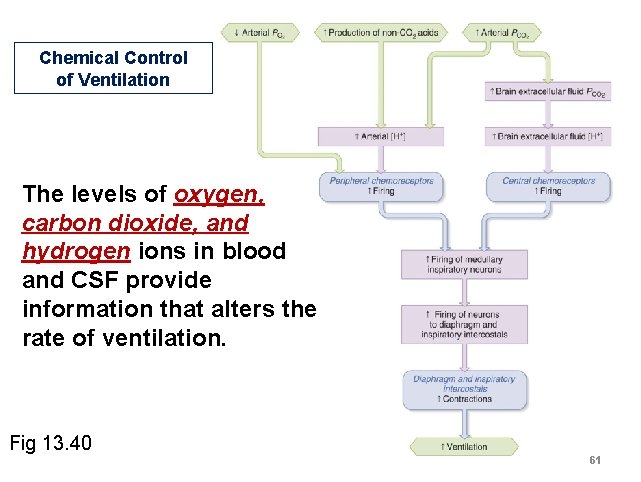
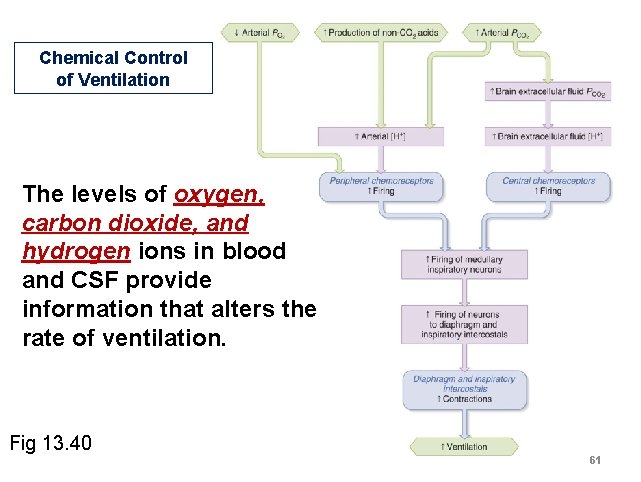
Chemical Control of Ventilation The levels of oxygen, carbon dioxide, and hydrogen ions in blood and CSF provide information that alters the rate of ventilation. Fig 13. 40 61
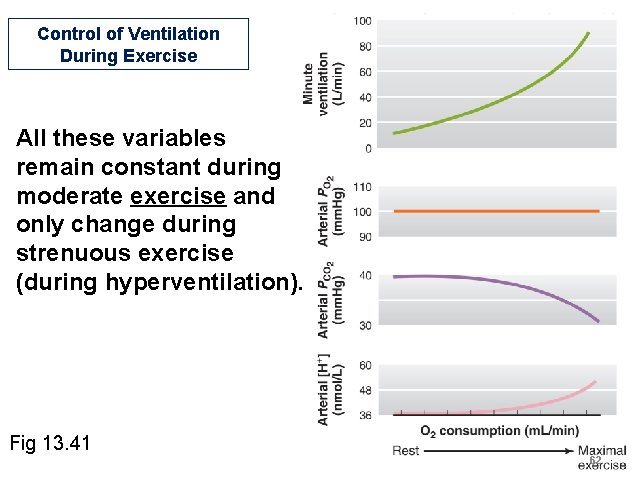
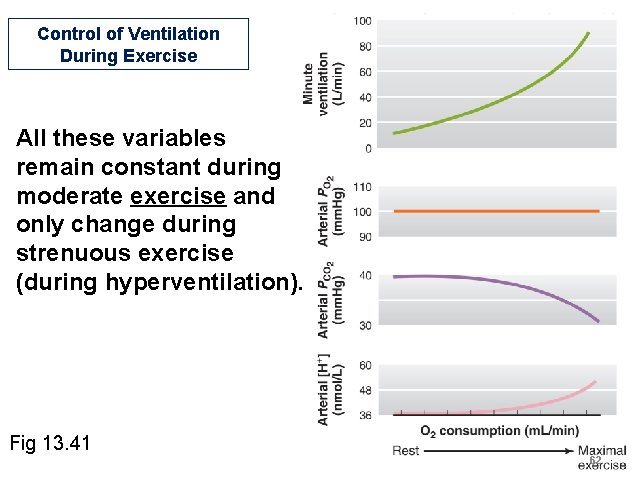
Control of Ventilation During Exercise All these variables remain constant during moderate exercise and only change during strenuous exercise (during hyperventilation). Fig 13. 41 62
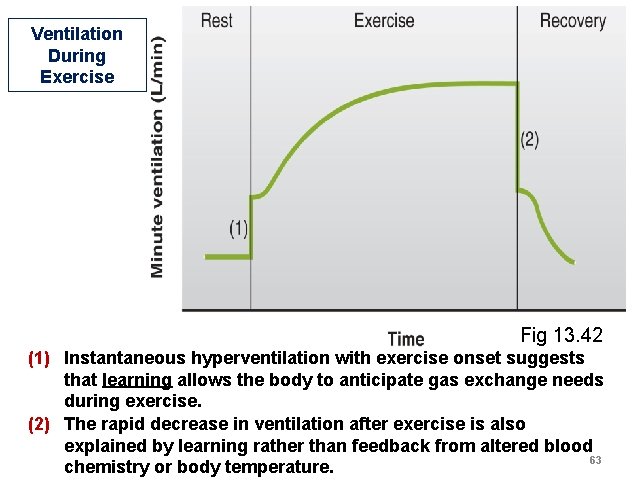
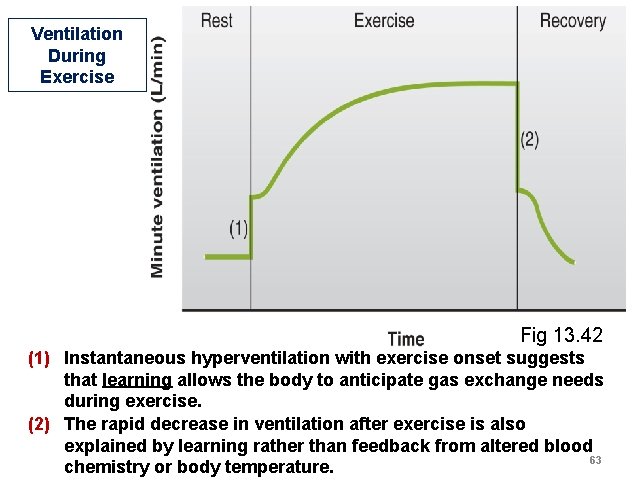
Ventilation During Exercise Fig 13. 42 (1) Instantaneous hyperventilation with exercise onset suggests that learning allows the body to anticipate gas exchange needs during exercise. (2) The rapid decrease in ventilation after exercise is also explained by learning rather than feedback from altered blood 63 chemistry or body temperature.
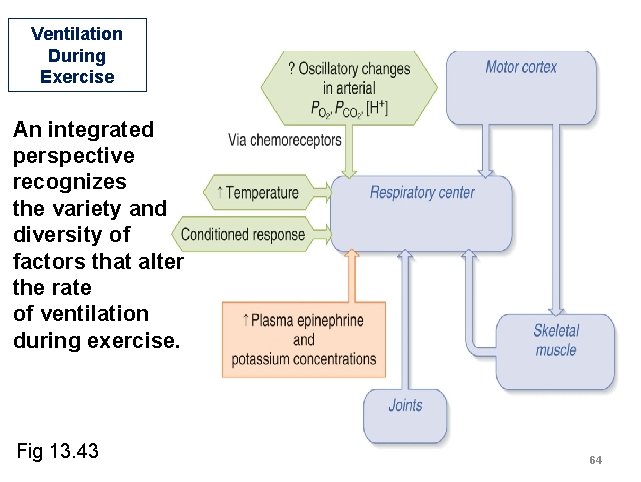
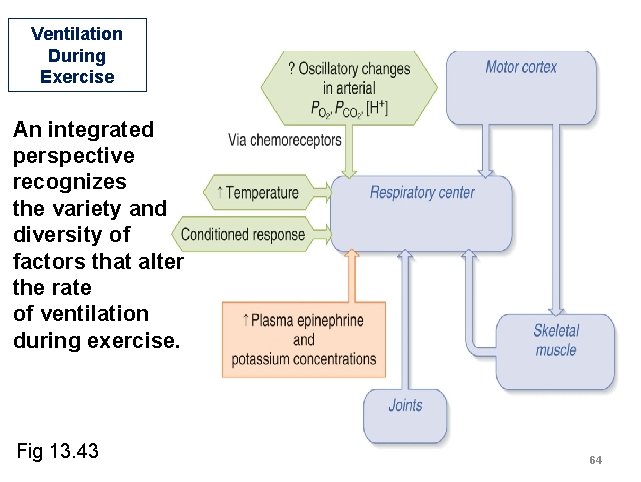
Ventilation During Exercise An integrated perspective recognizes the variety and diversity of factors that alter the rate of ventilation during exercise. Fig 13. 43 64
![Hypoxia Deficiency of oxygen at the tissue level there are 4 types of hypoxia Hypoxia Deficiency of oxygen at the tissue level [there are 4 types of hypoxia]](https://slidetodoc.com/presentation_image_h2/adc24f557e52ae13bfbe75992fac7835/image-65.jpg)
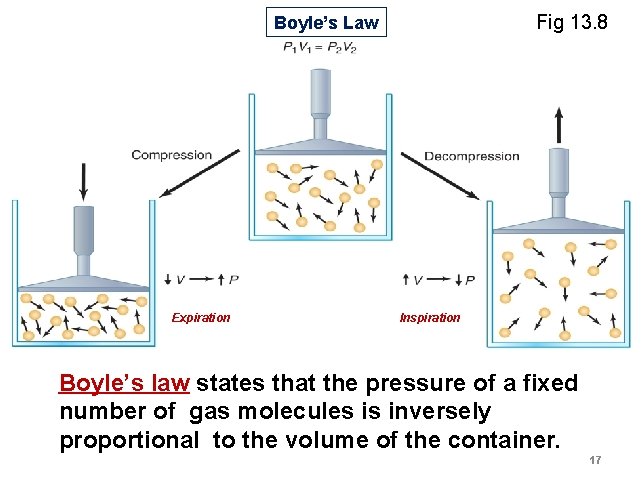
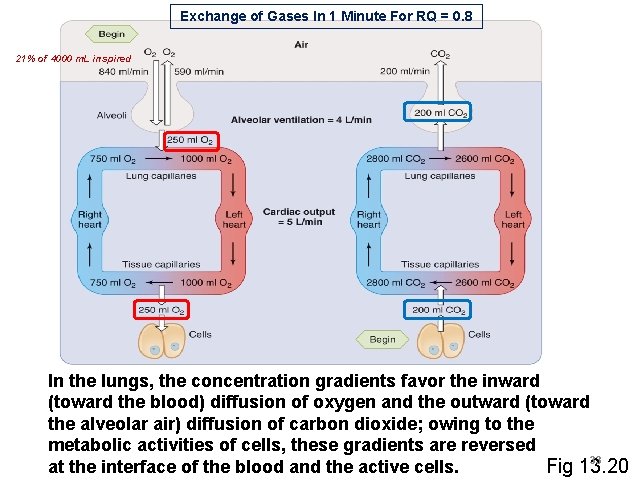
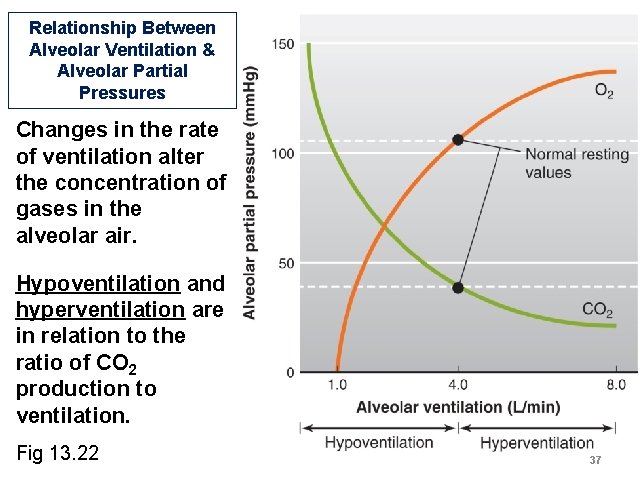
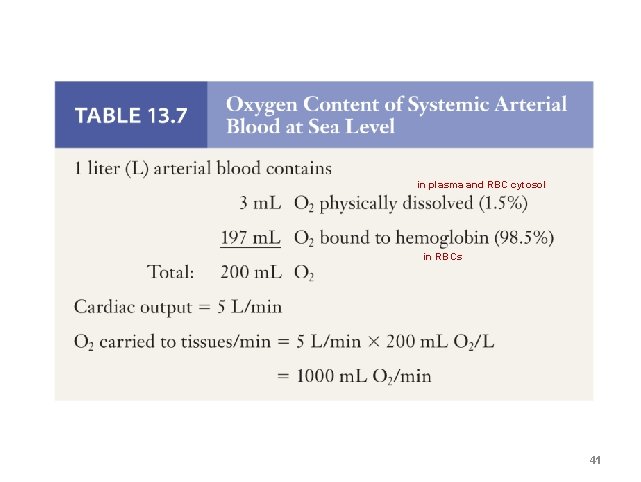
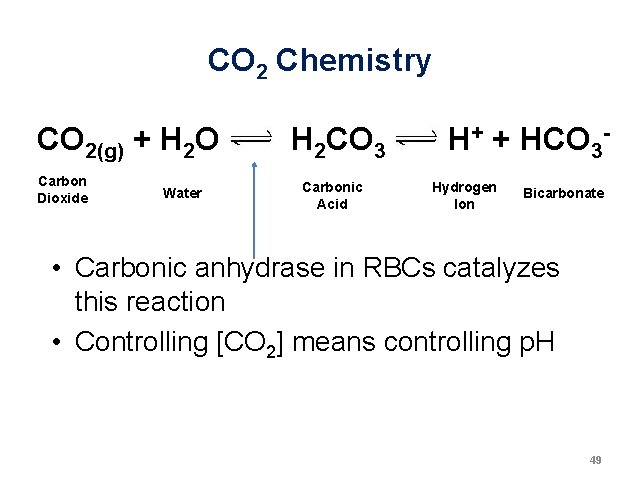
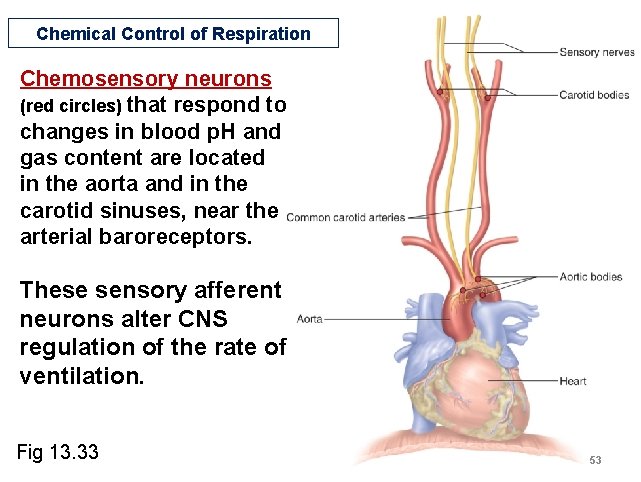
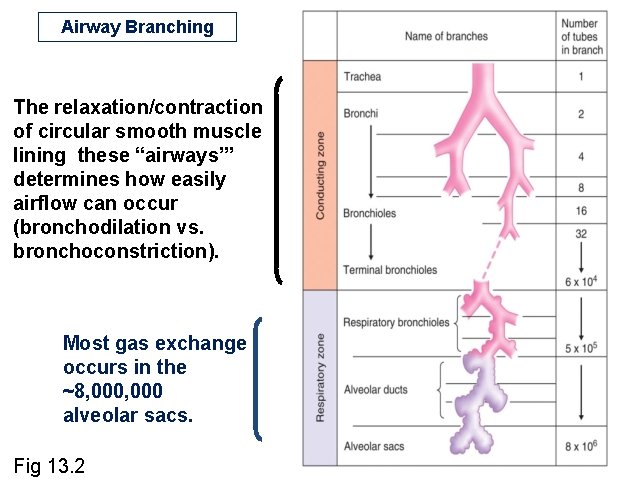
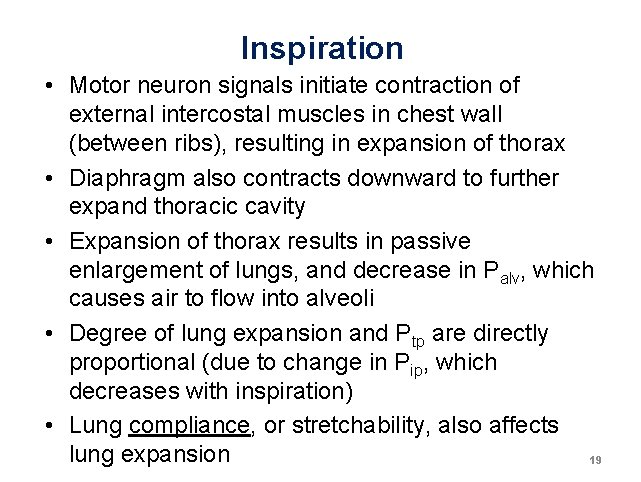
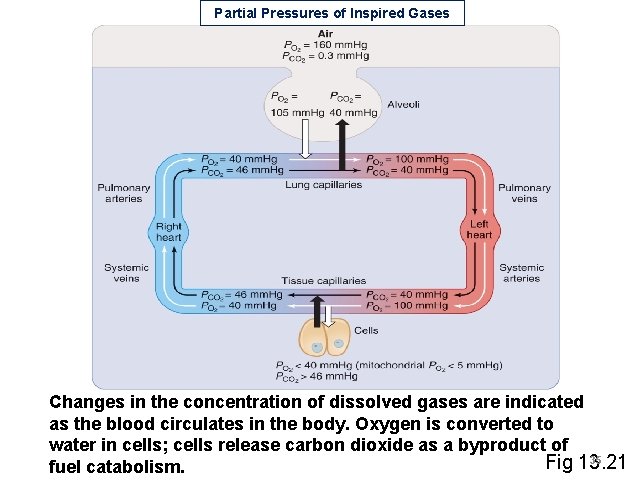
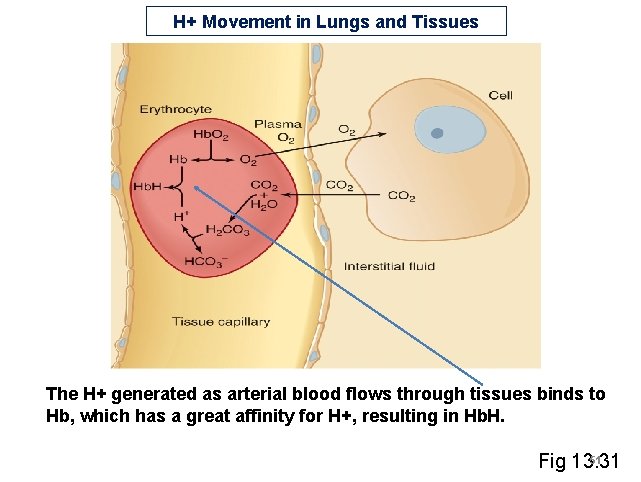
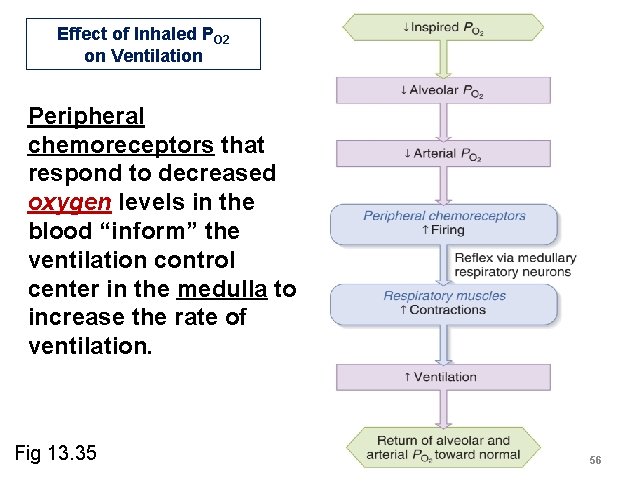
Hypoxia Deficiency of oxygen at the tissue level [there are 4 types of hypoxia] Hypoxic hypoxia: most common type, due to a reduction in arterial PO 2 • Several disease-related causes (Table 13. 10) • Occurs at high altitude due to decreased atmospheric pressure, and acclimatization can occur (Table 13. 11) 65
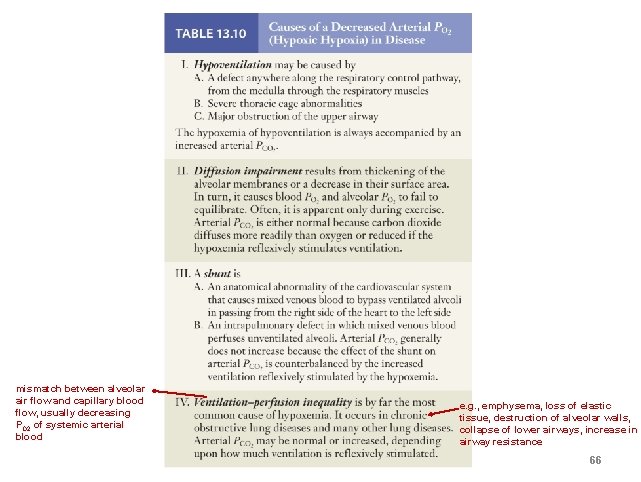
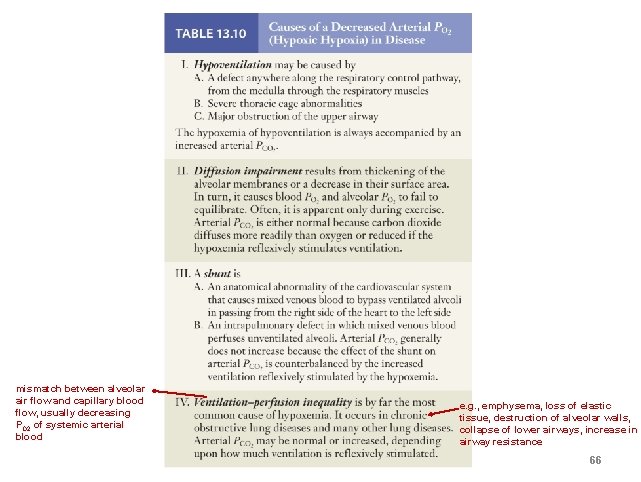
mismatch between alveolar air flow and capillary blood flow, usually decreasing PO 2 of systemic arterial blood e. g. , emphysema, loss of elastic tissue, destruction of alveolar walls, collapse of lower airways, increase in airway resistance 66
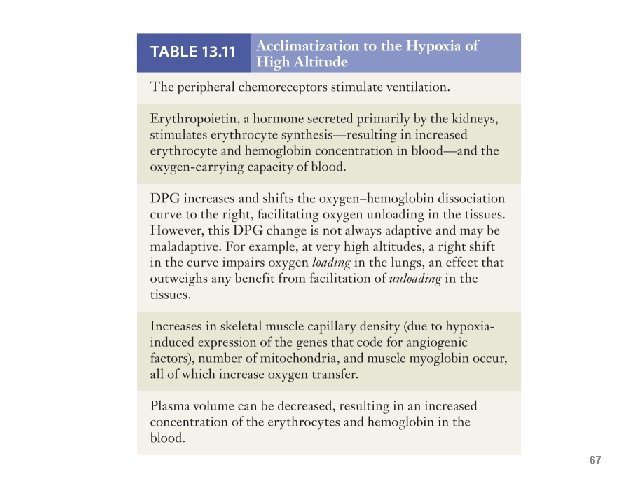
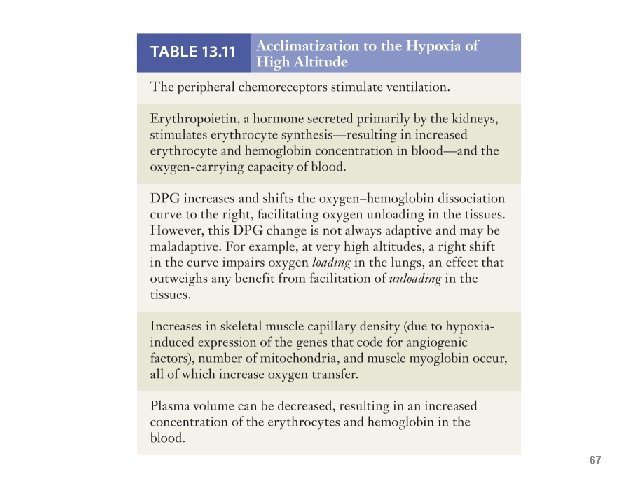
67