Respiratory System and Gas Exchange Gas exchange intake
- Slides: 34
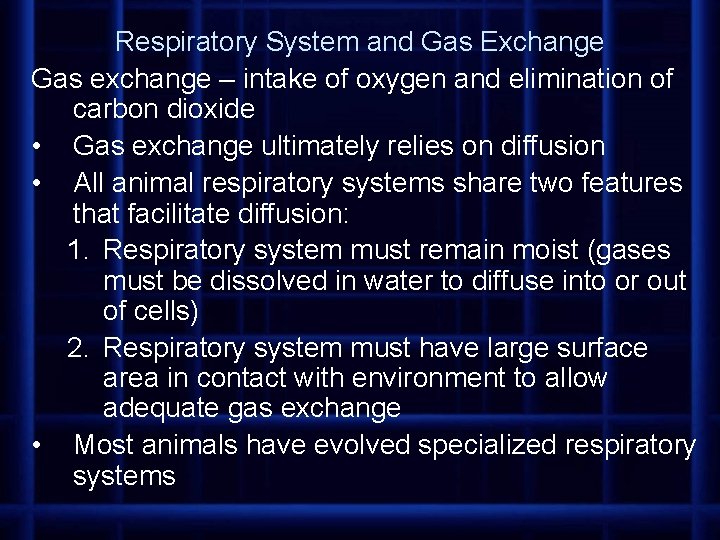
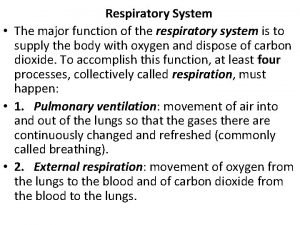
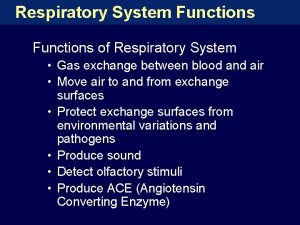
Respiratory System and Gas Exchange Gas exchange – intake of oxygen and elimination of carbon dioxide • Gas exchange ultimately relies on diffusion • All animal respiratory systems share two features that facilitate diffusion: 1. Respiratory system must remain moist (gases must be dissolved in water to diffuse into or out of cells) 2. Respiratory system must have large surface area in contact with environment to allow adequate gas exchange • Most animals have evolved specialized respiratory systems
In general, gas exchange in most respiratory systems occurs in the following stages: 1. air or water, containing oxygen, is moved past a respiratory system by bulk flow (fluids or gases move in bulk through relatively large spaces, from areas of higher pressure to areas of lower pressure) – commonly facilitated by muscular breathing movements 2. oxygen and carbon dioxide are exchanged through the respiratory surface by diffusion; oxygen is carried into capillaries of circulatory system and carbon dioxide is removed 3. Gases are transported between respiratory system and tissues by bulk flow of blood as it is pumped throughout body by heart 4. gases are exchanged between tissues and circulatory system by diffusion (oxygen diffuses out into tissue and carbon dioxide diffuses into capillaries based on concentration gradients)
Four types of surfaces have evolved for gas exchange – the animal’s own body surface, gills, tracheal tubes, and lungs 1. Small animals or those with low energy demands who live in a moist environment rely solely on simple diffusion • unicellular organisms, nematodes, flatworms, earthworms, jellyfish, sponges
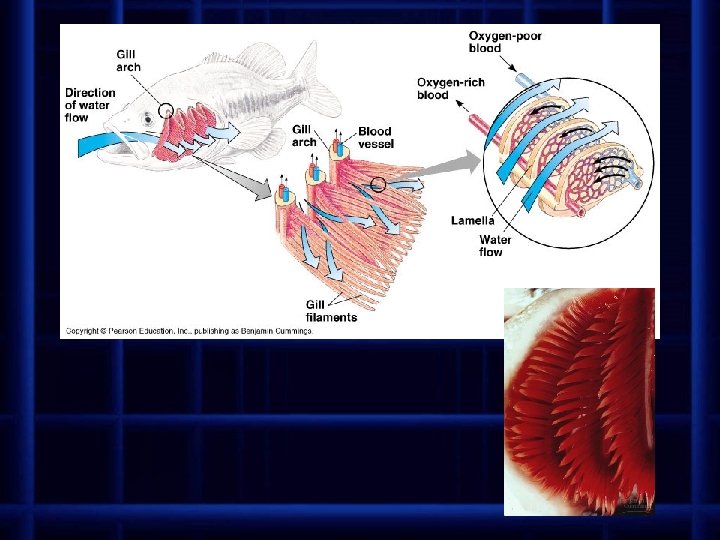
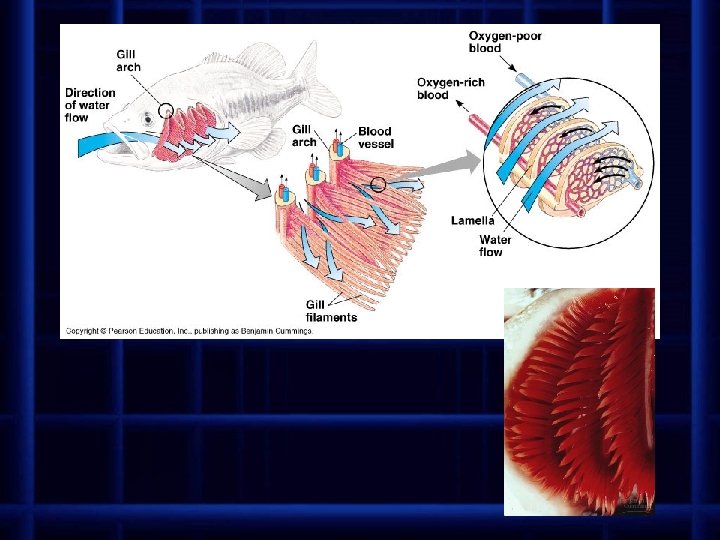
2. gills are the respiratory structures of many aquatic animals • elaborately branched or folded tissue for maximum surface area • have a dense profusion of capillaries just beneath outer membrane (bring blood close to surface for gas exchange) • gas exchange occurs as a result of a countercurrent exchange system • blood flows in capillaries of gills in the opposite direction as the water flowing over gills • maximizes difference in concentration of gases between blood and water
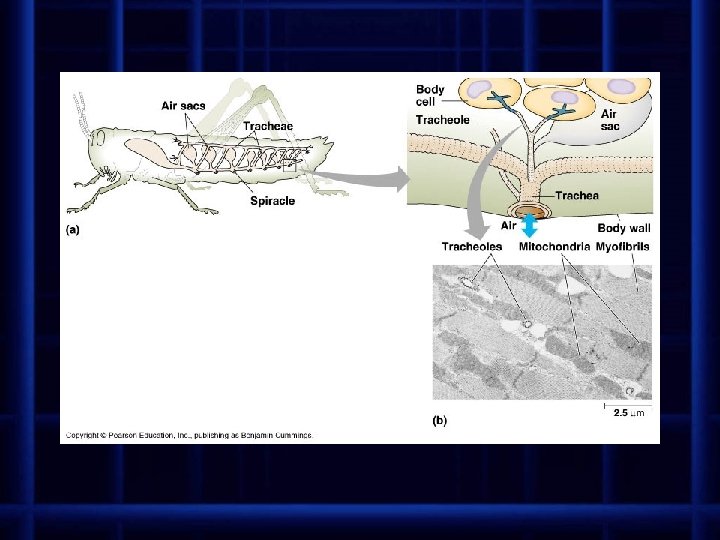
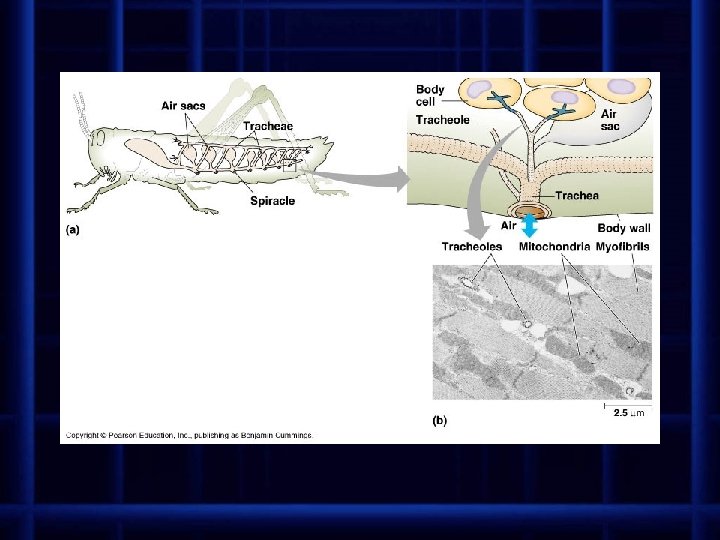
3. terrestrial animals have internal respiratory structures • air has more oxygen than water but presents problems with being dry • all respiratory surfaces must remain moist for diffusion of gases to occur • Insects use a system of elaborately branching internal tubes called tracheae (tracheal tubes) • air enters through tiny openings in body surface called spiracles • air is taken directly to cells through tubes
• • • Most terrestrial animals respire by means of lungs – chambers containing moist, delicate respiratory surfaces that are protected in body water loss is minimized (bathed in body fluids) and body wall provides support highly subdivided to increase surface area for gas exchange
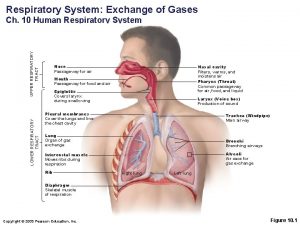
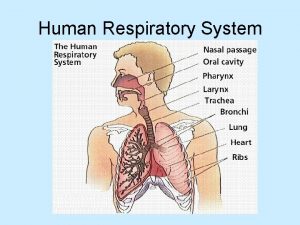
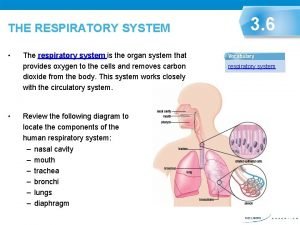
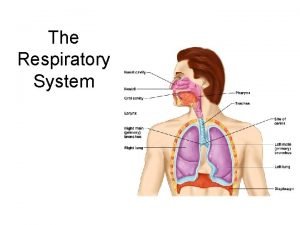
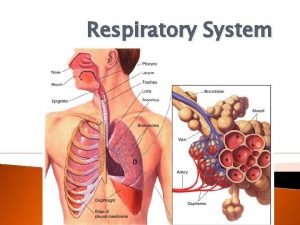
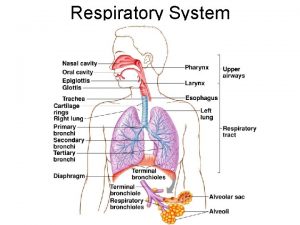
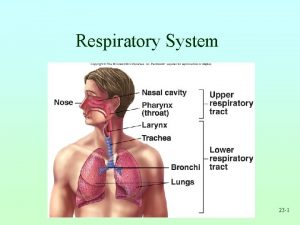
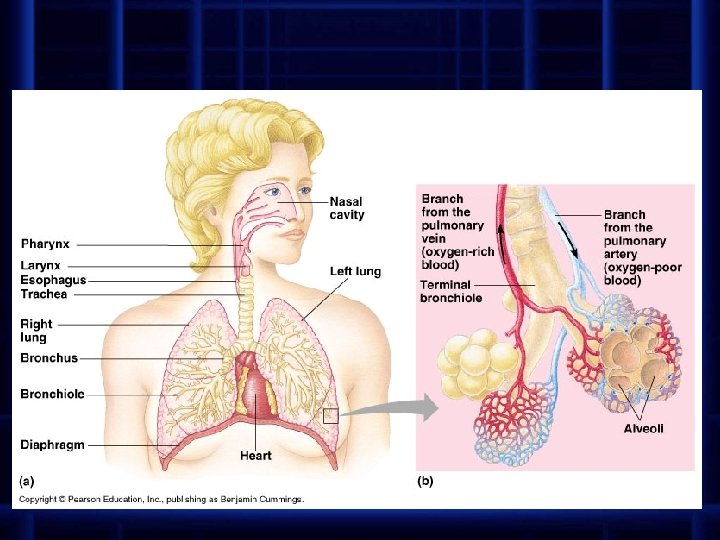
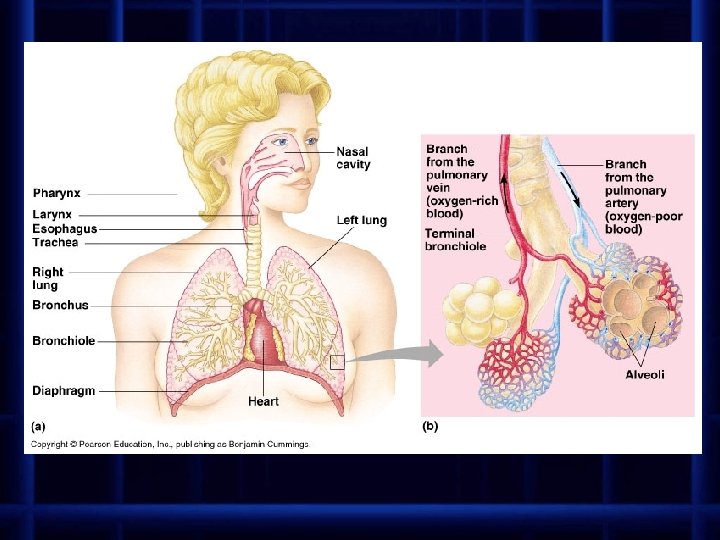
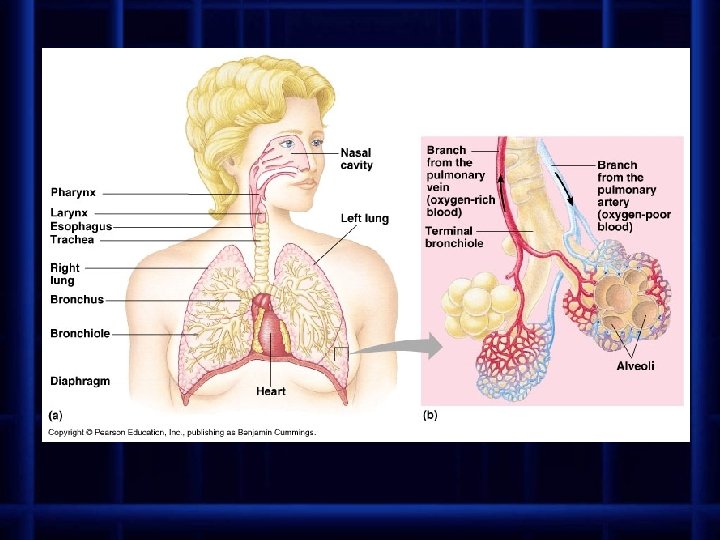
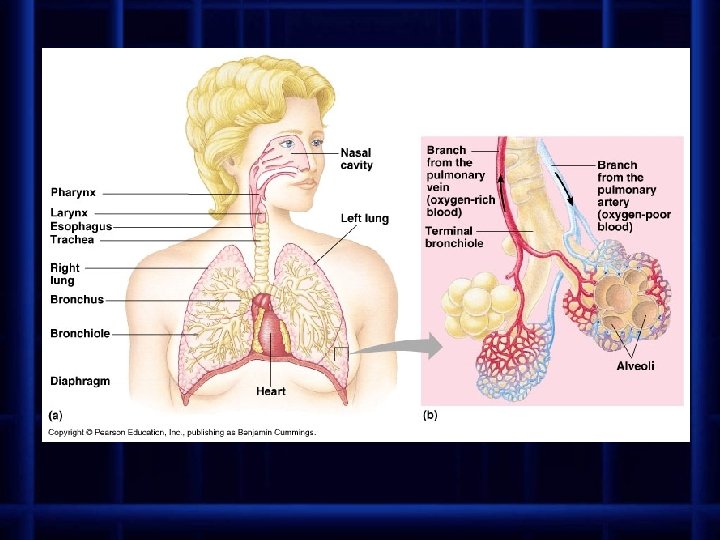
Human Respiratory System (and other vertebrates) is divided into two parts: the conducting portion (series of passageways that carry air to gas-exchange portion) and the gas exchange portion (gas is exchanged with the blood in tiny sacs in lungs) • nostrils – air enters body • nasal cavities – air is warmed, filtered and moistened – lined with ciliated epithelium that trap particles in mucus and move it to the throat to be swallowed
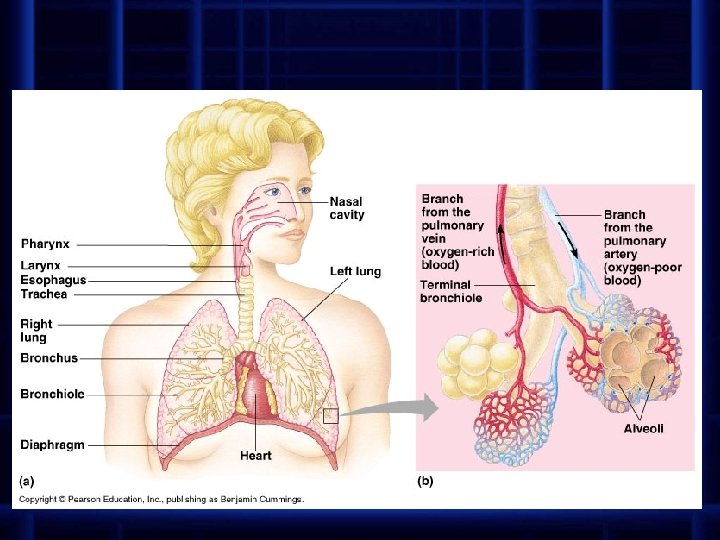
• • • pharynx – back of nasal cavities that is continuous with the throat larynx – opening in pharynx leads to larynx or “voice box” contains the vocal cords cartilage is embedded in walls to prevent collapse epiglottis – flap of tissue that automatically covers opening to larynx during swallowing – prevents food from entering lungs trachea (“windpipe”) – tube that carries air down to lungs – reinforced with cartilage to prevent collapse
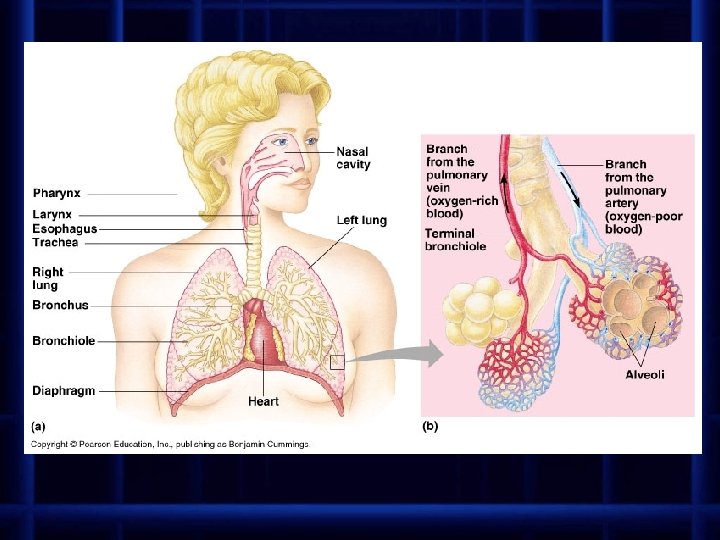
• • bronchi – trachea branches into two bronchi – each one leads to a lung bronchioles – bronchi branch into tiny tubes lungs – large, paired spongy organs – right lung is divided into three lobes – left lung divided into two lobes – each is covered by a pleural membrane – forms a sac and lines the thoracic cavity – secretes a fluid that provides lubrication between lungs and chest wall alveoli – each bronchiole ends in a cluster of tiny air sacs – walls of alveoli are extremely thin (one cell thick) and surrounded by capillaries – gases diffuse freely through the wall of the alveolus and capillary (oxygen diffuses into blood and carbon dioxide diffuses into alveoli)
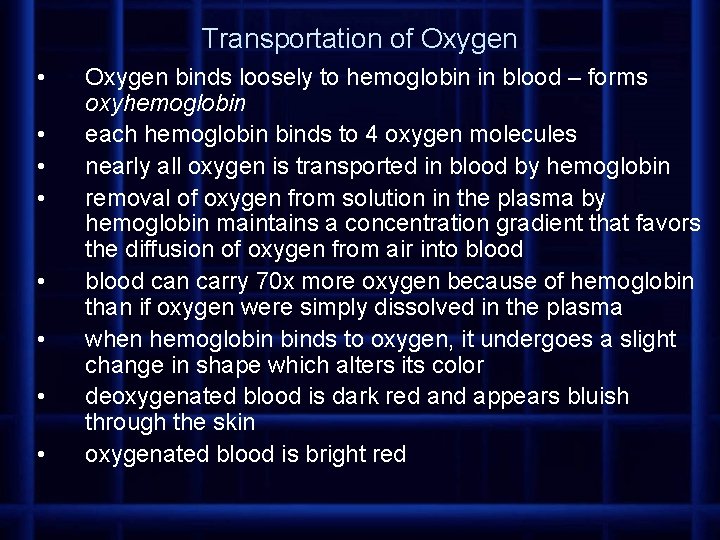
Transportation of Oxygen • • Oxygen binds loosely to hemoglobin in blood – forms oxyhemoglobin each hemoglobin binds to 4 oxygen molecules nearly all oxygen is transported in blood by hemoglobin removal of oxygen from solution in the plasma by hemoglobin maintains a concentration gradient that favors the diffusion of oxygen from air into blood can carry 70 x more oxygen because of hemoglobin than if oxygen were simply dissolved in the plasma when hemoglobin binds to oxygen, it undergoes a slight change in shape which alters its color deoxygenated blood is dark red and appears bluish through the skin oxygenated blood is bright red
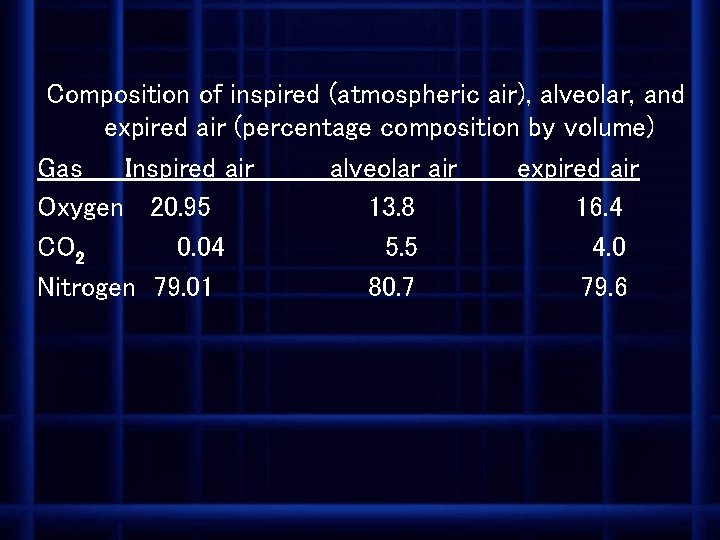
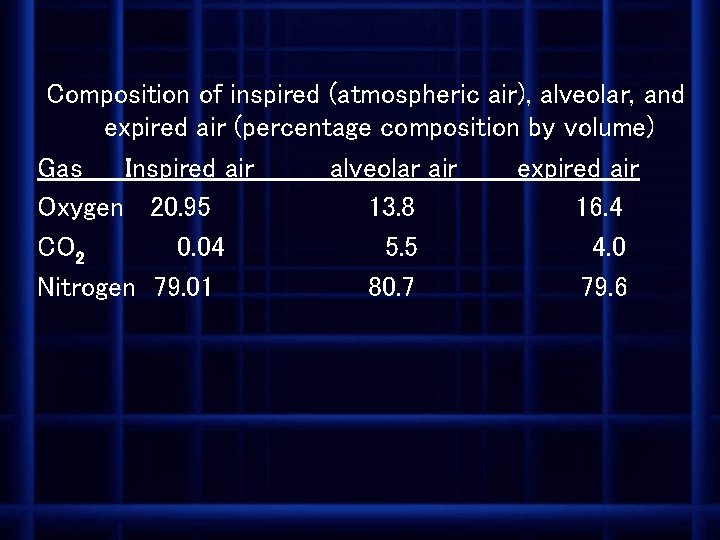
Composition of inspired (atmospheric air), alveolar, and expired air (percentage composition by volume) Gas Inspired air alveolar air expired air Oxygen 20. 95 13. 8 16. 4 CO 2 0. 04 5. 5 4. 0 Nitrogen 79. 01 80. 7 79. 6
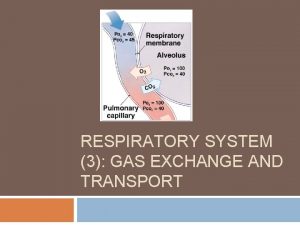
• Blood arriving in lungs has a relatively high concentration of carbon dioxide and relatively low concentration of oxygen – both gases diffuse down their concentration gradients to equalize between blood and air
Partial gas pressures • partial pressure is usually used to compare the proportion of gases in a mixture • the partial pressure of a gas in a mixture of gases is the pressure exerted by that gas (measured in kilopascals, k. Pa) • ex. at sea level, total atmospheric pressure is 101. 3 k. Pa • atmosphere contains 21% oxygen, therefore oxygen has a partial pressure of. 21 x 101. 3 k. Pa or 21. 3 k. Pa
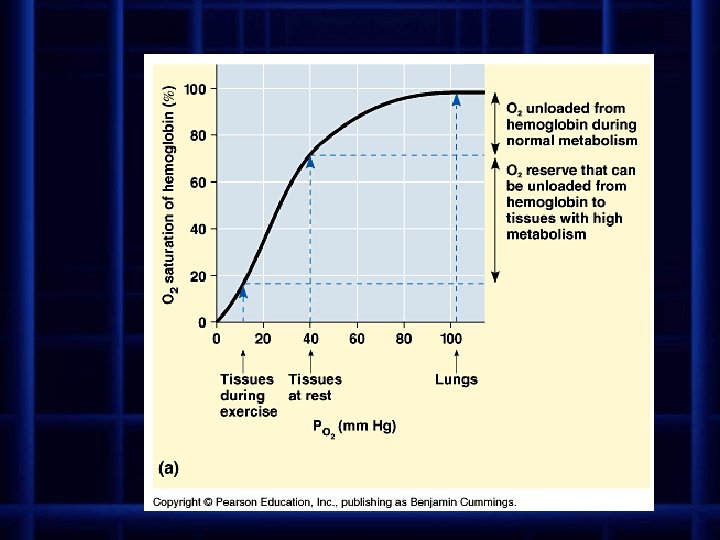
• • Hemoglobin and the transport of oxygen enters blood from alveoli and diffuses into red blood cells oxygen then combines with hemoglobin to form oxyhemoglobin (Hb. O 2) as hemoglobin picks up the first molecule of oxygen, it increases its affinity for oxygen and picks up the next molecule even faster, the third and fourth are picked up even faster the degree of oxygenation of hemoglobin is determined by the partial pressure of oxygen (p(O 2)) in the immediate surroundings
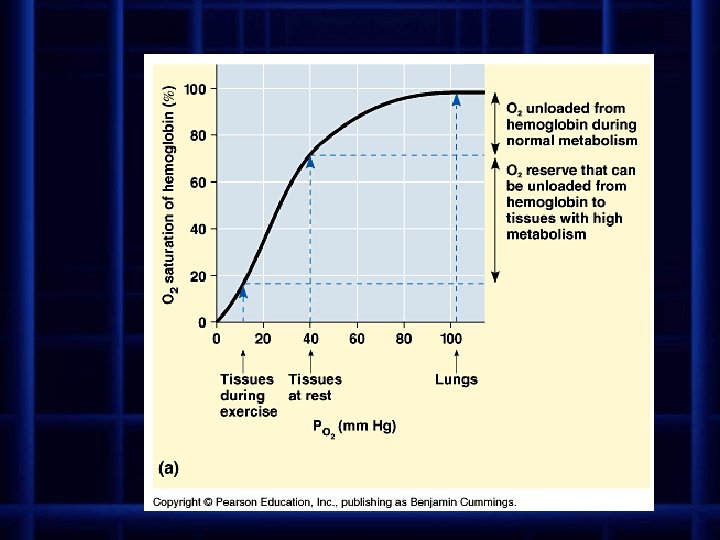
• If p(O 2) is low (as in the capillaries at the tissues needing oxygen) hemoglobin releases oxygen and carries relatively small amounts of oxygen • If p(O 2) is high (such as at the alveoli) hemoglobin becomes almost saturated with oxygen
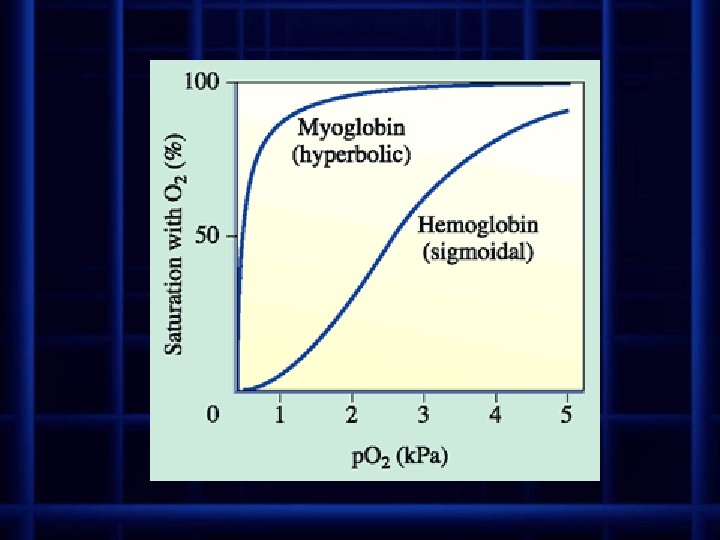
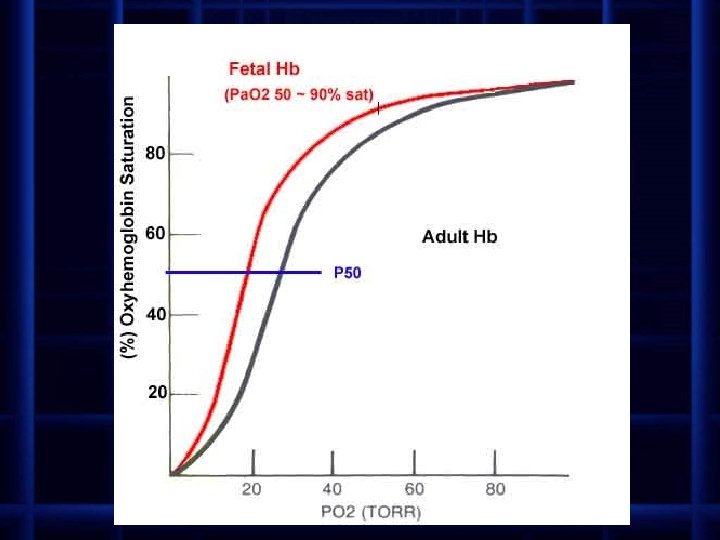
• an oxygen dissociation curve shows the degree of hemoglobin saturation with oxygen plotted against different values of p(O 2) – the curve is Sshaped • at p(O 2) close to zero there is no oxygen bound to the hemoglobin • at low p(O 2), the polypeptide chains are tightly bound together, making it difficult for an oxygen molecule to attach to iron in heme group • as one molecule of oxygen attaches, the polypeptide chain opens up exposing the other heme groups to oxygen and allowing oxygen to attach – the curves rises sharply • at very high p(O 2), the hemoglobin becomes saturated and the curve levels off
• oxygen at the muscles is taken over and stored by myoglobin – myoglobin has a much higher affinity for oxygen than hemoglobin – it binds with oxygen at a high rate and does not dissociate its oxygen unless the p(O 2) drops to very low levels – myoglobin stores oxygen in muscles until the demand becomes very great – during heavy exercise, muscles will get oxygen from hemoglobin first, then when supply oxygen from hemoglobin is exhausted, myoglobin will begin to release its oxygen
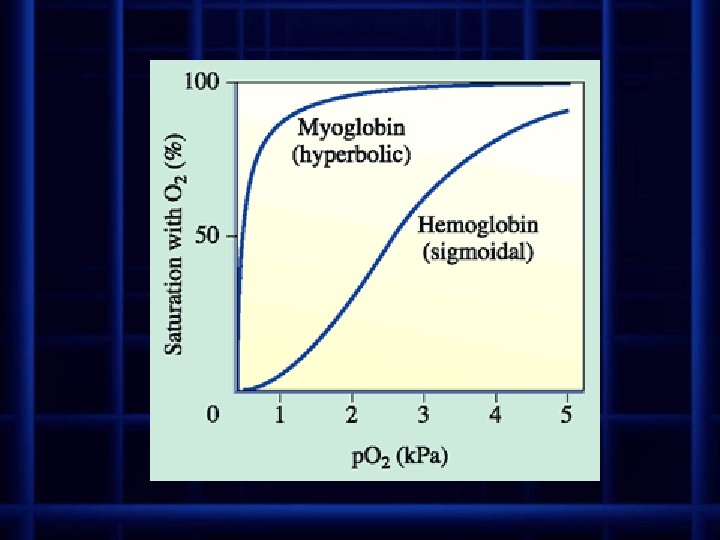
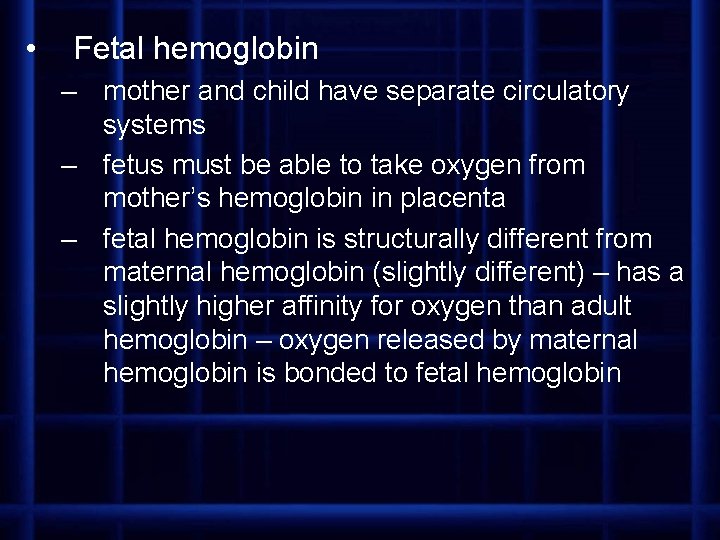
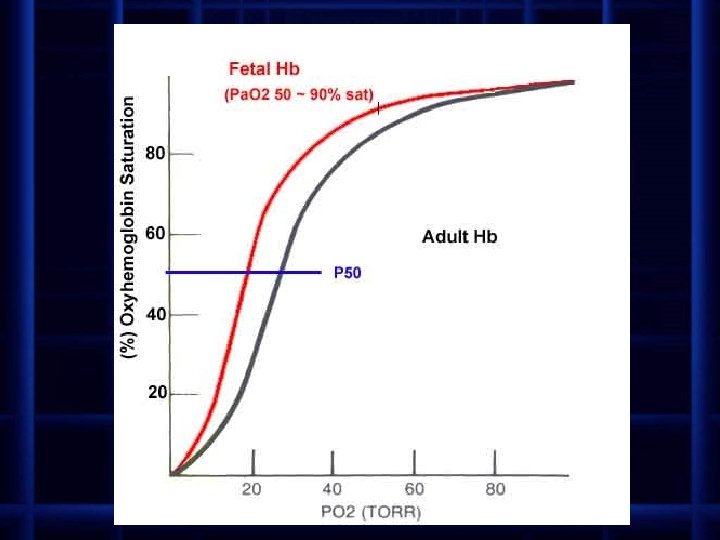
• Fetal hemoglobin – mother and child have separate circulatory systems – fetus must be able to take oxygen from mother’s hemoglobin in placenta – fetal hemoglobin is structurally different from maternal hemoglobin (slightly different) – has a slightly higher affinity for oxygen than adult hemoglobin – oxygen released by maternal hemoglobin is bonded to fetal hemoglobin
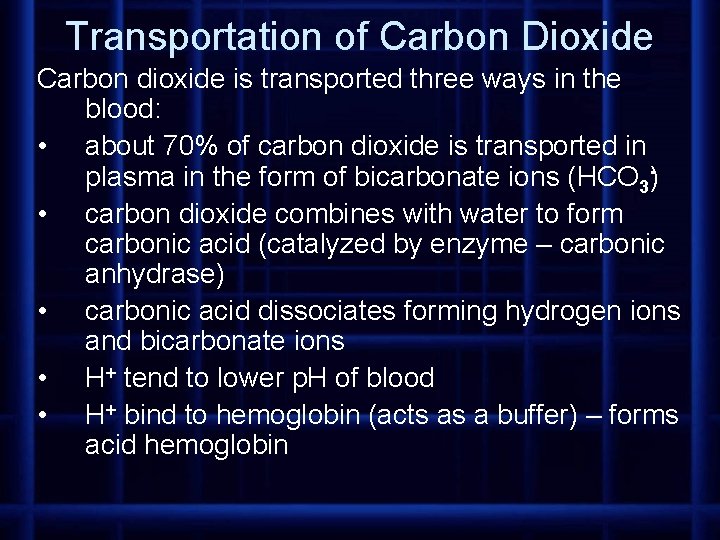
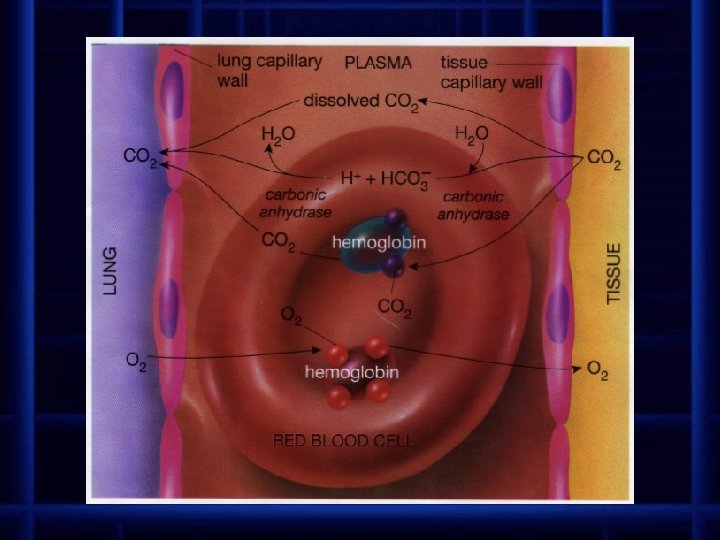
Transportation of Carbon Dioxide Carbon dioxide is transported three ways in the blood: • about 70% of carbon dioxide is transported in plasma in the form of bicarbonate ions (HCO 3 ) • carbon dioxide combines with water to form carbonic acid (catalyzed by enzyme – carbonic anhydrase) • carbonic acid dissociates forming hydrogen ions and bicarbonate ions • H+ tend to lower p. H of blood • H+ bind to hemoglobin (acts as a buffer) – forms acid hemoglobin
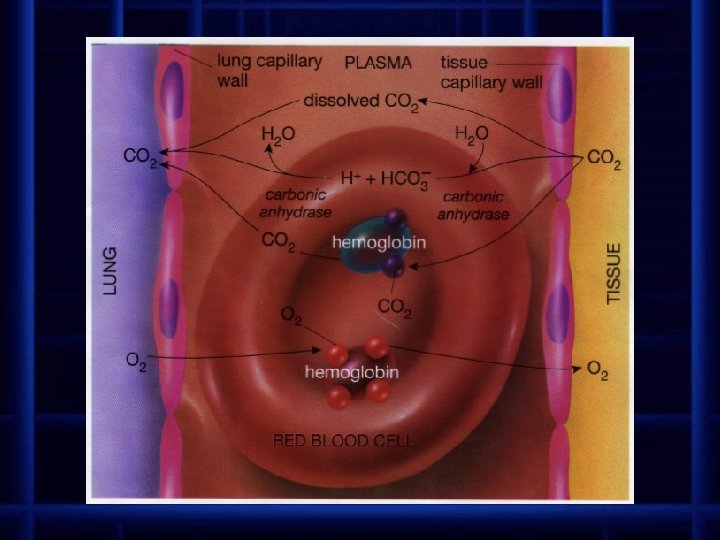
• • • about 20% of CO 2 binds to hemoglobin (has already released O 2 at tissues) to be carried back to lungs 10% remains dissolved in the plasma as CO 2 both the production of bicarbonate ion and the binding of CO 2 to hemoglobin reduces the concentration of CO 2 in blood to increase the gradient for CO 2 to flow out of body cells into blood
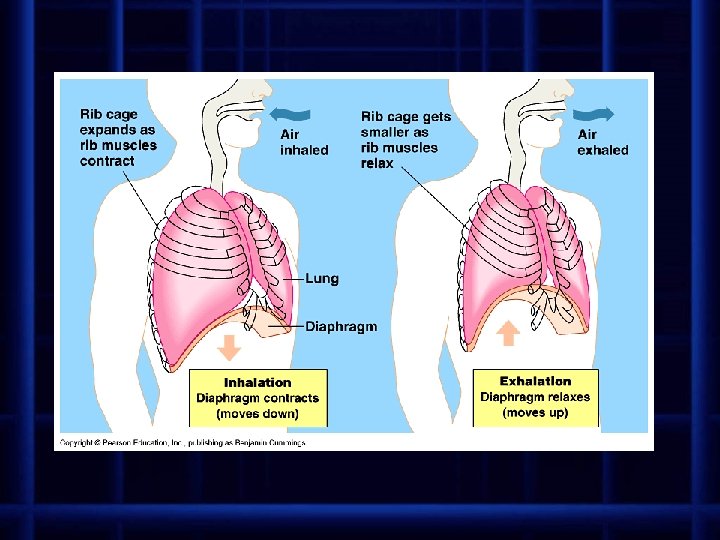
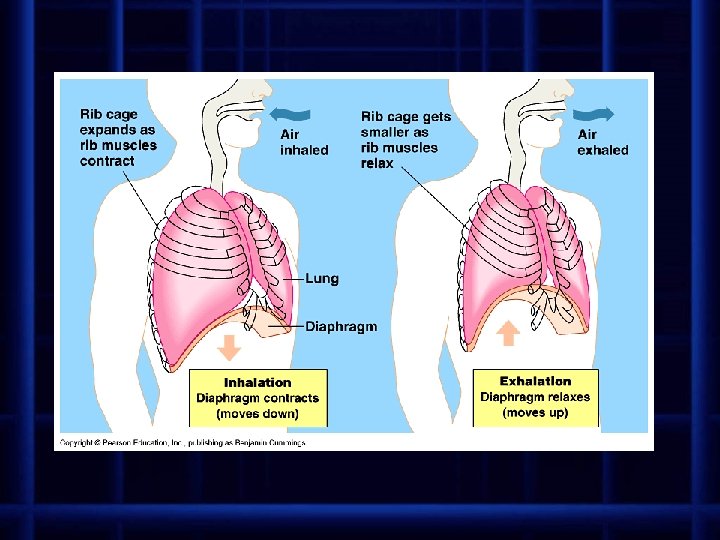
• • • Breathing (ventilation) is the mechanical process of moving air from the environment into the lungs and expelling air from the lungs Inspiration (inhalation) – volume of thoracic cavity is increased diaphragm (dome-shaped muscle forming floor of thoracic cavity) contracts and moves downward External intercostal rib muscles contract lifting ribs up and out (internal intercostal muscles relax) this increases volume of thoracic cavity which lowers air pressure air from outside rushes into lungs to equalize air pressure
• • • Expiration (exhalation) – volume of thoracic cavity is decreased diaphragm relaxes and returns to domeshape (moves up) Internal intercostal rib muscles contract (external intercostal muscles relax) causing ribs to drop back down this decreases the volume of thoracic cavity which increases air pressure air from inside lungs rushes out to equalize air pressure
• • • Breathing rate is controlled by the respiratory center in brain – located in medulla just above spinal cord muscles are stimulated to contract by impulses from respiratory center nerve cells in respiratory center generate cyclic bursts of impulses that cause the alternating contraction and relaxation of respiratory muscles
• • • respiratory center receives input from several sources and adjusts breathing rate and volume to meet body’s changing needs CO 2 concentration in blood is the most important chemical stimulus for regulating rate of respiration chemoreceptors in medulla, and in walls of the aorta and carotid arteries are sensitive to changes in arterial CO 2 concentration
 Gas exchange key events in gas exchange
Gas exchange key events in gas exchange Respiratory zone
Respiratory zone Site:slidetodoc.com
Site:slidetodoc.com Circulatory system and respiratory system work together
Circulatory system and respiratory system work together How respiratory system work with circulatory system
How respiratory system work with circulatory system Respiratory exchange ratio equation
Respiratory exchange ratio equation The actual exchange of gases occurs at the site of the *
The actual exchange of gases occurs at the site of the * Kemas intake system
Kemas intake system Upper and lower respiratory tract
Upper and lower respiratory tract Stress and respiratory system
Stress and respiratory system Structure of cell
Structure of cell Human.respiratory.system
Human.respiratory.system Bioflix activity: gas exchange -- inhaling and exhaling
Bioflix activity: gas exchange -- inhaling and exhaling Pulmonary gas exchange and transport diagram
Pulmonary gas exchange and transport diagram Gas exchange between tissues and capillaries
Gas exchange between tissues and capillaries Gas exchange in plants and animals venn diagram
Gas exchange in plants and animals venn diagram Chapter 42 circulation and gas exchange
Chapter 42 circulation and gas exchange Respiratory system bozeman
Respiratory system bozeman Unit 9 respiratory system
Unit 9 respiratory system Diagnostic test of respiratory system
Diagnostic test of respiratory system Respiratory system
Respiratory system Membranes of larynx
Membranes of larynx Respiratory system coloring page
Respiratory system coloring page Respiratory system purpose
Respiratory system purpose Conclusion about respiratory system
Conclusion about respiratory system The energy-releasing process that is fueled by oxygen
The energy-releasing process that is fueled by oxygen Chapter 7 cengage
Chapter 7 cengage Chapter 13 the respiratory system
Chapter 13 the respiratory system Perfusion respiratory
Perfusion respiratory Interesting facts about respiratory system
Interesting facts about respiratory system Lower respiratory structures
Lower respiratory structures How to draw the respiratory system
How to draw the respiratory system Upper respiratory tract
Upper respiratory tract Respiratory system diagram unlabeled
Respiratory system diagram unlabeled Respiratory system vocabulary
Respiratory system vocabulary