Respiratory System Anatomy and Physiology Review Part II
- Slides: 18
Respiratory System Anatomy and Physiology Review Part II Diana Jones Paramedic
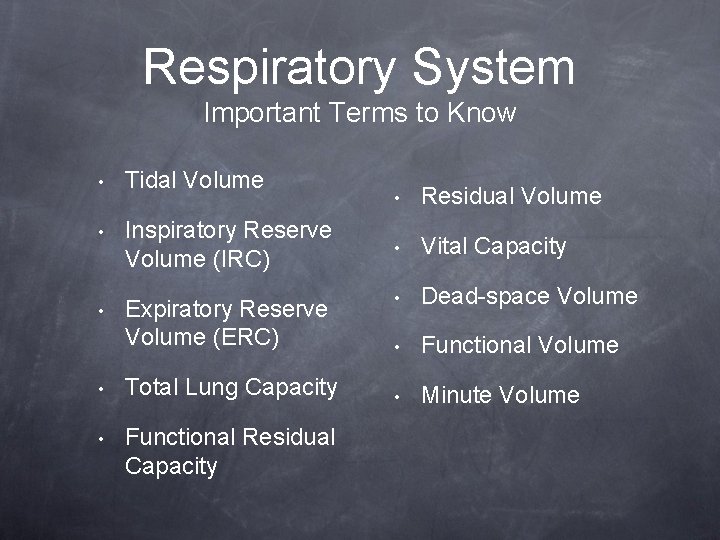
Respiratory System Important Terms to Know • Tidal Volume • Inspiratory Reserve Volume (IRC) • Expiratory Reserve Volume (ERC) • Total Lung Capacity • Functional Residual Capacity • Residual Volume • Vital Capacity • Dead-space Volume • Functional Volume • Minute Volume
What Drives the Respiratory System? • Carbon Dioxide • Detected by chemoreceptors • Increase in CO 2 • • Decrease in CO 2 • • Increase in ventilation Decrease in ventilation So what happens with COPD patients? ? ?
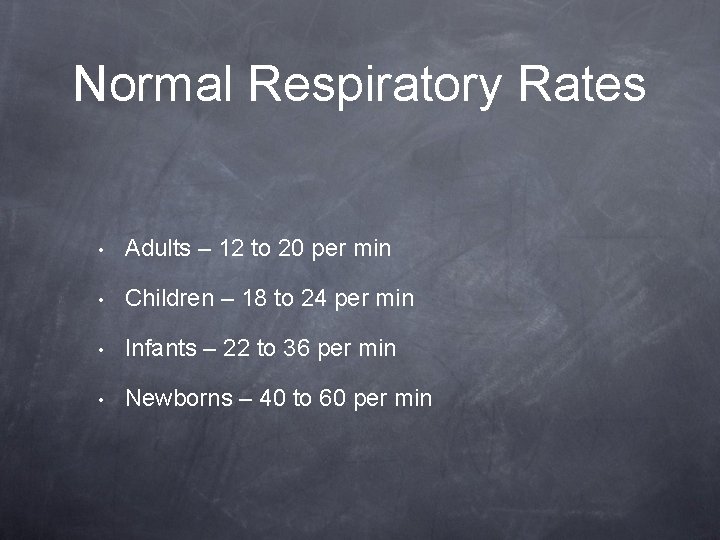
Normal Respiratory Rates • Adults – 12 to 20 per min • Children – 18 to 24 per min • Infants – 22 to 36 per min • Newborns – 40 to 60 per min
Factors Influencing Respiratory Rate • Fever • Drugs – depressants and stimulants • Anxiety • Sleep • Oxygen/CO 2 level • Disease
Tidal Volume • Tidal Volume (VT) – when at rest, the volume of air in 1 respiratory cycle (inspired and expired) • Normal adult is 500 m. L of air
Inspiratory Reserve Volume • Inspiratory Reserve Volume (IRV) – amount of additional air forcibly inhaled after inspiration of normal tidal volume • Varies by sex • Up to 3100 m. L
Expiratory Reserve Volume • Expiratory Reserve Volume (ERV) – amount of additional air forcibly exhaled after expiration of normal tidal volume • Approximately 1200 m. L
Residual Volume • Residual Volume – volume of air remaining the most forcible expiration • Approximately 1200 m. L
Vital Capacity • Vital Capacity (VC) – total amount of air that can be expired after a full inhalation • Can be affected by age and body size • Approximately 4800 m. L
Dead-space • Dead-space Volume – volume that remains in the airways (ex. Trachea, bronchi) and never reaches site for gas exchange • Approximately 150 m. L of tidal volume
Functional Volume • Functional Volume – air that reaches the alveoli and participates in gas exchange • Approximately 350 m. L of tidal volume
Functional Residual Capacity • Functional Residual Capacity (FRC) – amount of air remaining in the lungs after a normal expiration • Approximately 2400 m. L
Total Lung Capacity • Total Lung Capacity – maximum amount of air that can fill the lungs • Approximately 6 L
Minute Volume • Minute Volume (VE) – total volume of air exhaled per minute • Product of RATE x VOLUME; f x VT = VE • Approximately 6 L/min
Minute Volume • Homeostatic mechanism • Maintenance of Pa. CO 2 (blood carbon dioxide) • Critical significance in the mechanically ventilated patient • How would hyper or hypoventilation cause a shift in minute volume (remember the formula)
Important Measures Pulse Oximetry • Measures the amount of oxygen in the blood • Given as percent of hemoglobin saturated • • Detects carbon dioxide in a gas sample using infra-red light • Commonly recognized as “gold standard” for intubation confirmation • Provides wealth of additional information Used only as a tool • • End-tidal CO 2 What could be wrong the reading Normal is 95 to 100% • Be on the lookout for separate lecture
Questions?