Respiratory Physiology Prof Omer Abdel Aziz Musa Faculty
Respiratory Physiology Prof. Omer Abdel Aziz Musa Faculty of medicine The National Ribat University
Respiratory Physiology • • Functions of respiratory system: 1. Gas exchange: O 2 uptake, CO 2 removal. 2. Regulation of acid-base balance. 3. Regulation of temperature. 4. Regulation of Body fluids. 5. Protection. 6. Endocrine & metabolic function. 7. Excretion e. g. Alcohol. • 8. Speech.

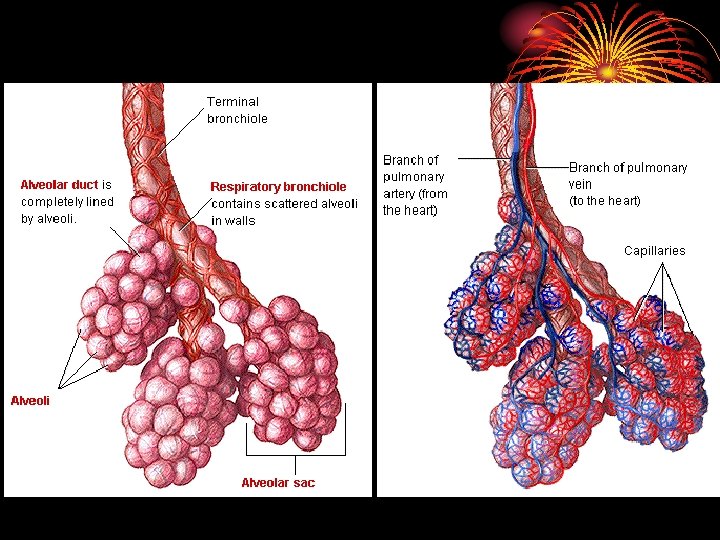
ANATOMY • Right lung three lobes and left two. • Each lobe divided into segments. • Trachea divides into main two bronchi then bronchioles, terminal b. and respiratory b. reaching the alveolar ducts to the alveoli. • Between the trachea and the alveoli airways divide 23 times, 16 conducting & 7 from resp. b. involved in gas exchange.
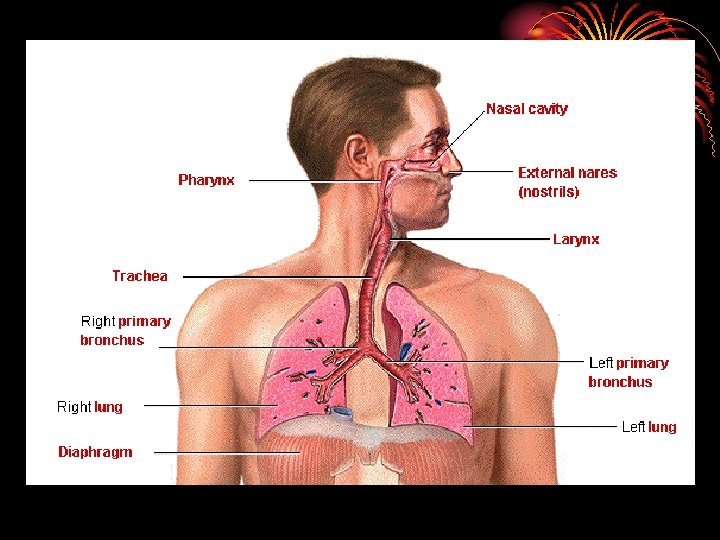
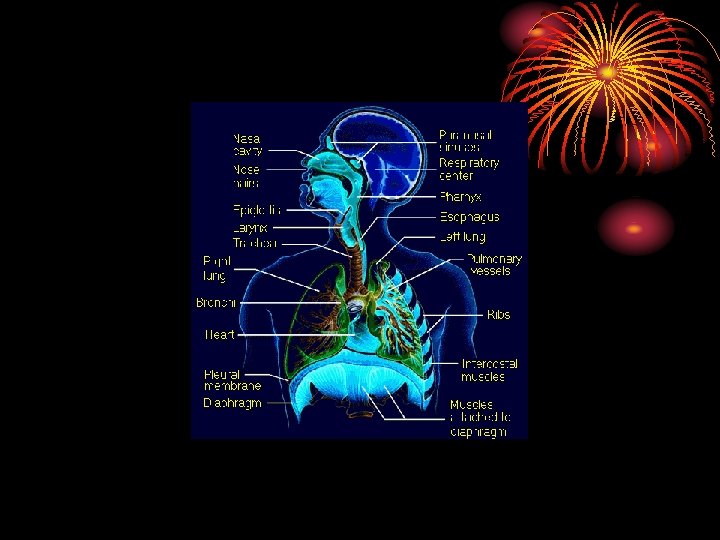
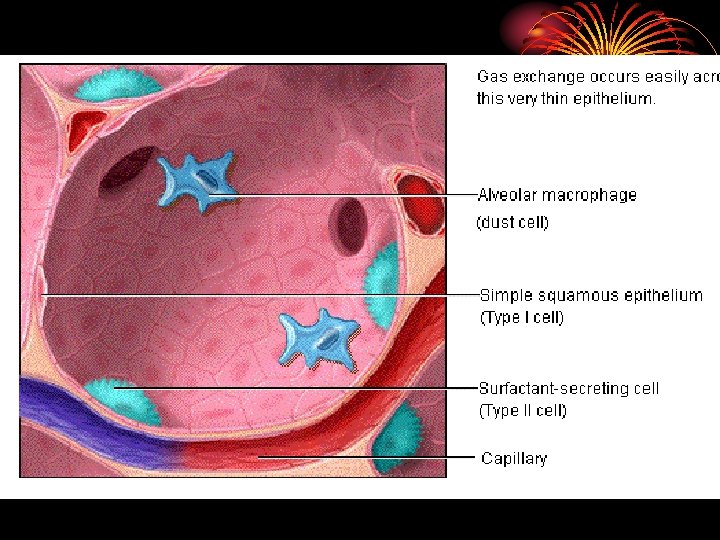
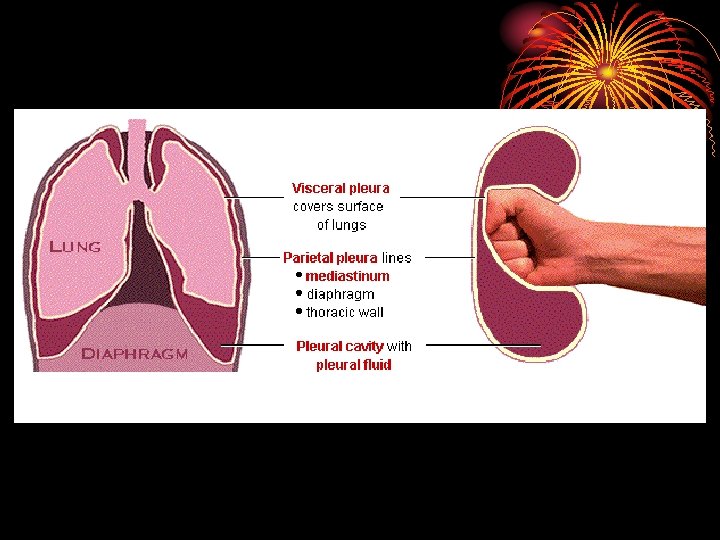
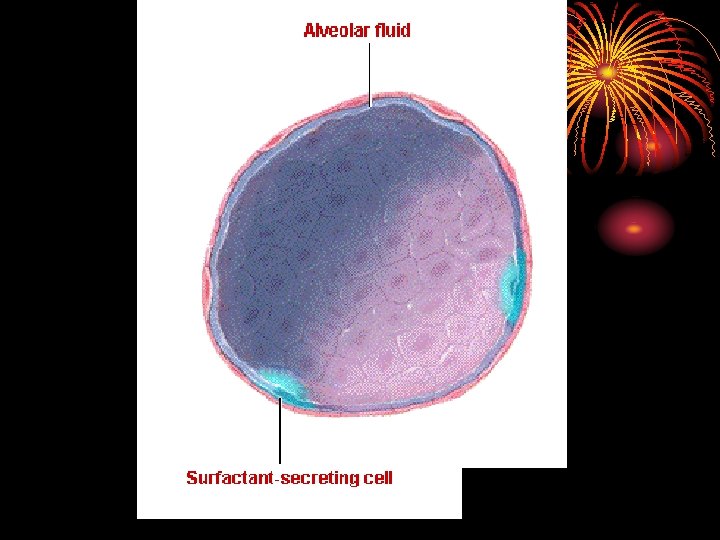
• area from 2. 5 cm 2 (trachea) to 11800 cm 2 in alveoli ? Air velocity. • 300 million alveoli, 70 m 2. • Alveoli lined by type 1 cells ( flat lining ) and type 11 cells ( granular pneumocytes secrete surfuctant ). • Pleura. • Respiratory muscles.
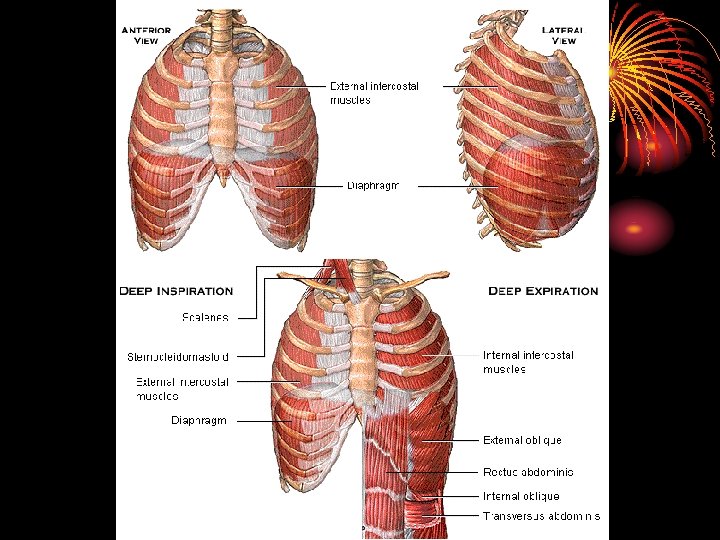
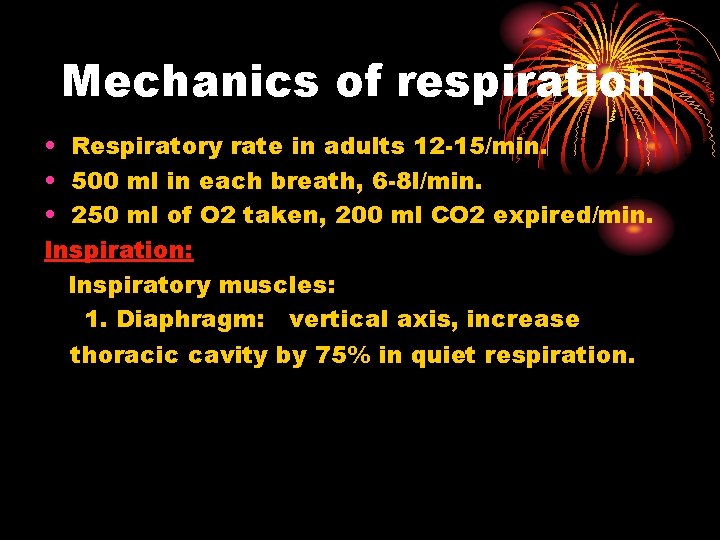
Mechanics of respiration • Respiratory rate in adults 12 -15/min. • 500 ml in each breath, 6 -8 l/min. • 250 ml of O 2 taken, 200 ml CO 2 expired/min. Inspiration: Inspiratory muscles: 1. Diaphragm: vertical axis, increase thoracic cavity by 75% in quiet respiration.
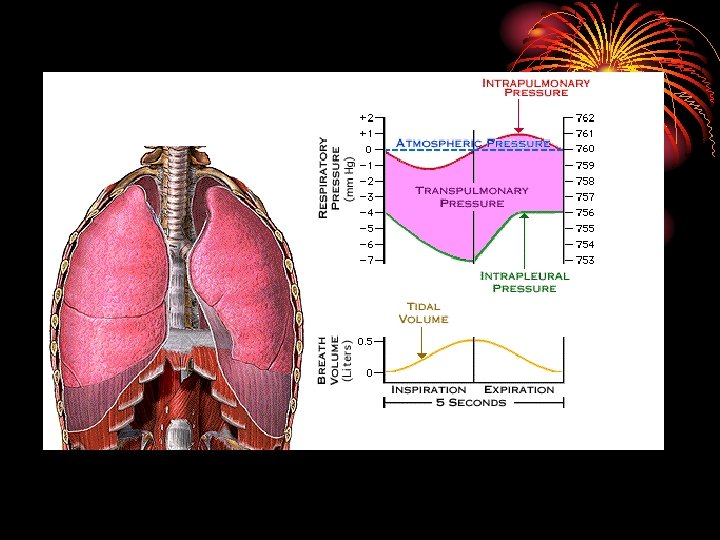
2. External intercostal muscles: anteroposterior diameter, 10% only. 3. Accessory inspiratory muscles: act in forcible respiration: scalene and sternocleidomastoid muscles. Mecahnics Contraction of insp. muscles decreases intrapleural pressure from – 2. 5 mm Hg to – 6 mm. Hg : by increasing the thoracic cavity the lungs will move with the thoracic cage as the parietal and visceral pleurae are in contact, the pressure in airways decreases, leading to entry of air from outside.
• In forcible insp. intrapleural pressure reaches – 30 mm Hg Expiration: • Passive process due to elastic recoil of insp. muscle and lungs leading to increased press. in airways and outflow of air. • Accessory expiratory muscles work in forced expiration: abdominal muscles and internal intercostal.
Q • Respiratory muscles do not fatigue due to alternation of contraction between: 1. inspiratory and expiratory muscles? • 2. Diaphragm and internal intercostals? • 3. the fibers of inspiratory muscles? • 4. internal and external intercostals? • 5. Diaphragm and external intercostals?
Q • Inspiration during quiet breathing is mainly produced by contraction of: • 1. Internal intercostal muscles? • 2. External intercostal m. ? • 3. Sternocleidomastoid m. ? • 4. Diaphragm? • 5. Abdominal m. ? • 4
Work of breathing • 1. Elastic work: work performed by the respiratory muscles in stretching the elastic tissues of the chest wall and lungs. During quiet inspiration represents 65% of the work. • 2. Non-elastic work: work performed by respiratory muscles in: • I. Moving non-elastic tissues (viscous resistance, 7%). • II. Moving air through air passages (airway resistance, 28%)
Compliance of the lung and chest wall • It is the change in lung volume per unit change in airway press. V/ P • Decreased: in pulmonary congestion and fibrosis. • Increased in emphysema.
Pulmonary circulation • Lungs receive the whole cardiac output (5 L). • Pulm. arterial press. 24/9 (av. 15). • Lt atrial press = 8 , oncotic press. 25 in drive to keep alveoli dry. • Base of lungs more perfused and more ventilated. ?
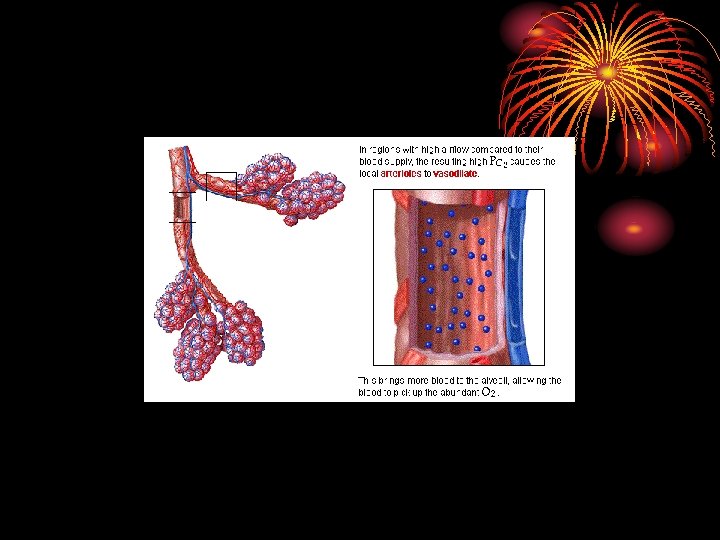
Ventilation-perfusion ratio V/Q • Pulm. alveolar ventilation / perfusion = 4. 2/5. 5 = 0. 8. • Both ventilation and perfusion decreases towards the apex, but the perfusion decreases more, so V/Q increases at the apex (more PO 2 T. B) at apex.
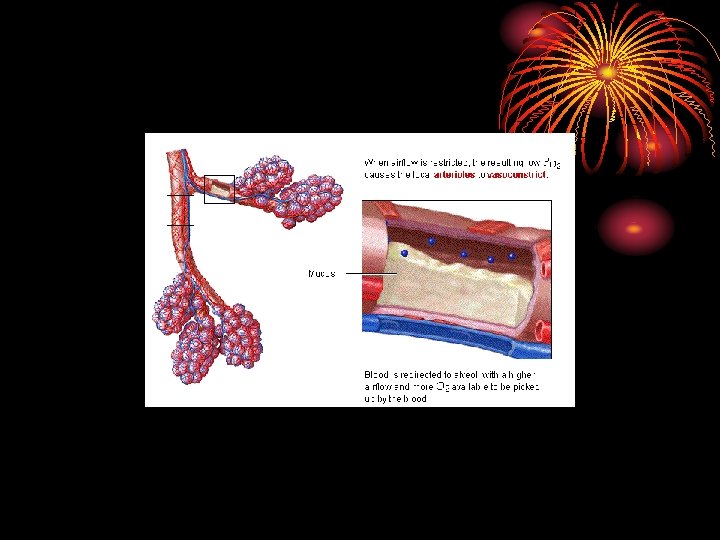
Physiological dead space • It is the area where no gas exchange takes place. It includes the anatomical dead space and any area either not ventilated or not perfused.
Anatomical dead space • It is the airways which conduct air without gas exchange. Its volume is 150 ml. • Alveolar ventilation /min = (500 – 150) x 12 = 4200 cm 3.
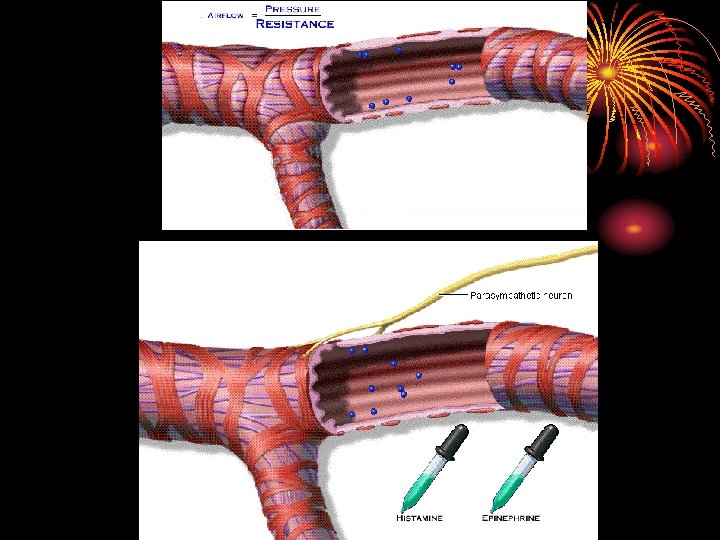
Bronchial tone • Bronchioles have no cartilage and more smooth muscles. • Bonchio. dilate during inspiration by sympathetic discharge. B 2 receptors. salbutamol. • Broichio. constrict during expiration by parasympathetic- muscaranic receptors. ipratropium.
• Non cholinergic – nonadrenergic innervation produces bronchodilation VIP? • Irritants, cool air, exercise lead to bronchoconstriction. • Circadian rhythm: Max. constriction at about 6 a. m. and max. dilation at 6 p. m. • Substance P , adenosine ( A 1 receptor ), & leukotrienes cause bronchoconst.
Quiz • Bronchoconstriction is produced by • 1. Sympathetic stimulation. • 2. Substance P. • 3. VIP. • 4. Surfactant. • 5. Normal saline. • 2
Surfactant • Lipid surface tension lowering agent. • Produced by type II alveolar epithelial cell. • Composed of phospholipids, neutral lipids, proteins and CHO. • Functions: 1. Lower surface tension in alveoli. 2. Helps to prevent pulmonary edema.
• Maturation of surfactant is accelerated by glucocorticoid (cortisol). • Surfactant decreases in smokers. • Cardiac surgery with interruption of pulm circulation, pulm, artery occlusion, main bronchus occlusion and long term 100% 02 can decrease surfactant.
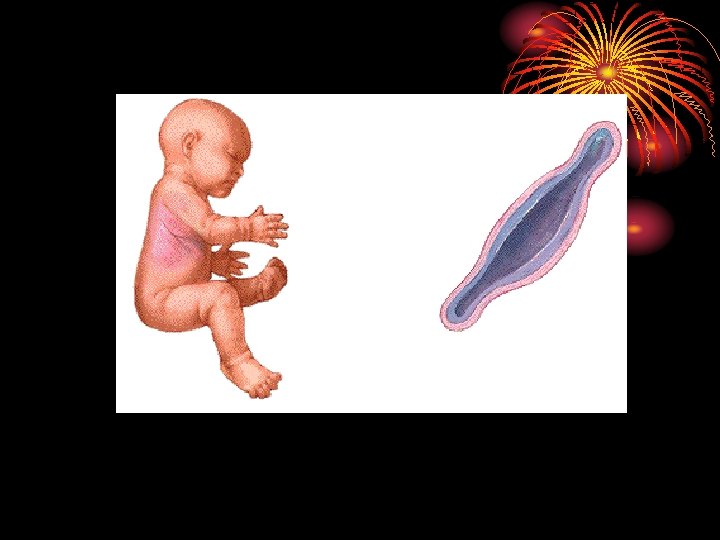
• Surfactant deficiency can cause infant respiratory distress syndrome (IRDS, hyaline membrane disease) in premature babies. • Surfactant (Synthetic and bovine) can be given by inhalation.
Summary • Inspiration is an active process due to contraction of respiratory muscles: diaphragm & external intercostal muscles. • Intapleural pressure at end of quiet expiration is -2. 5 mm. Hg and goes down to 6 during inspiration. • V/Q is normally 0. 8 • Compliance of the lung is the change in volume due to the change in pressure.
• Dead spaces are anatomical or physiological: no gas exchange. • Work of breathing is either elastic or non-elastic. • Bronchial tone can be affected by many factors which are related to asthma. • Surfactant? def. can cause IRDS.

Gas Laws
Gas laws • • • O 2 20. 98% CO 2 0. 04% N 2 78. 06% Inert 0. 092% Gases expand to fill available volume. The volume occupied by a specific no. of gases molecules at a constant temp. and press. is constant.
Laws The pressure of a gas in a mixture is directly proportional to the temp. and no. of moles and inversely proportional to the volume. P. Pressure. N. no. Moles. P = n. RT R. gas constant. V T. temp. V. volume.
Barometric press. at sea level is 760 mm Hg (pa). Then PO 2 = 20. 94 x 760 = 160 mm Hg. 100 Gas diffuses from areas of high pressure to areas of low pressure depending on. 1. Concentration gradient and surface area (directly). 2. Nature of barrier between the zones.
Thickness of membrane (inversely). Gases dissolve in liquids depending on their solubility and their partial press. in the mix. Partial press. of water vapor affect the partial press. of gases.
Measurement As gas volume vary with temp. and press and amount of water vapor in them varies it is imp. to correct its measurement to a set of standards. - Recording spirometors. - N 2 emits light in electric field in vacuo. - O 2 + Co 2 electrodes. - infrared absorption spectroscopy. - chromatography and mass spectrometry.
• STDP O C, 760 mm Hg, dry (Standard temp. and press. dry). • BTPS Body temp. and press. , saturated with water vapor. • ATPS Ambient temp. , press. Saturated with water vapor.
Partial pressure of a gas • Partial pressure of a gas in a mix. of gases is equal to the total press. multiplied by the fraction or % the gas in the mixture. (P). • Diffusion of a gas is affected by: 1. Solubility 2. Molecular weight as it increase when Mwt is low Co 2 diffusion >O 2
Thanks

Lung Volumes & Capacities
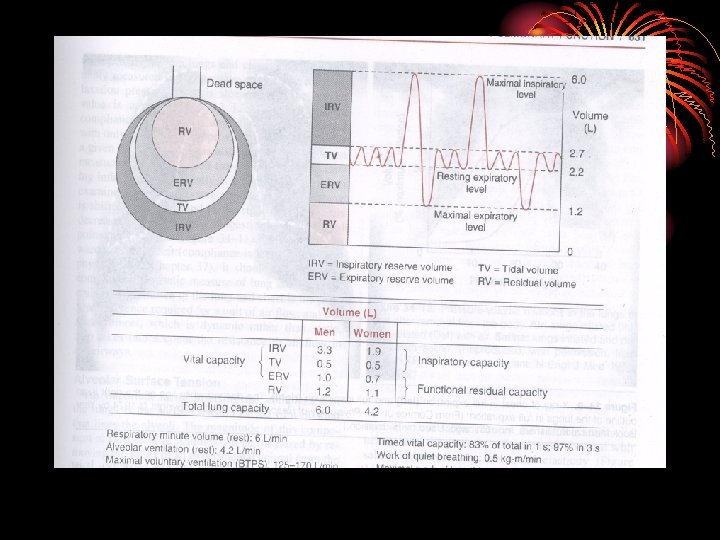
Lung volumes • Tidal volume: is the amount of air that moves into the lung with each normal inspiration. • Inspiratory reserve volume: amount of air inspired by a max. insp. after a normal insp. • Residual volume: amount of air left in the lungs after max. exp.
• Expiratory reserve volume: amount of air expired by a max. exp. After a normal exp. • Respiratory minute volume: (Pulmonary ventilation) amount of air inspired per min.
Capacities • Vital capacity: amount of air expired by a max exp. after a max. insp. • Inspiratory capacity: amount of air inspired by a max. insp. after a normal exp. • Expiratory capacity: max exp. after normal insp. • Total lung capacity: amount of air present in lungs after max. insp.
Pulmonary function tests • Function: 1. Diagnosis. 2. Follow up. 3. Compensation. 4. Preoperative assessment.
PFT 1. Spirometry: pocket, microlab, computerized. - FEV 1: forced expiratory volume in the first second. - FVC : forced vital capicity. - Peak expiratory flow rate PEFR. - Maximum expiratory flow loop. 1. Peak flow meter: PEFR. 2. Blood gases. 3. Transfer factor. 4. Static lung volumes.
Quiz • A patient with nocturnal cough showed the following findings in PFT: FEV 1 2 L, FVC=4 L, FEV 1 after salbutamol inhaler=2. 5 L, his diagnosis is: • 1. Chronic bronchitis. • 2. Emphysema. • 3. Obstructive lung disease. • 4. Asthma. • 5. Restrictive lung disease.
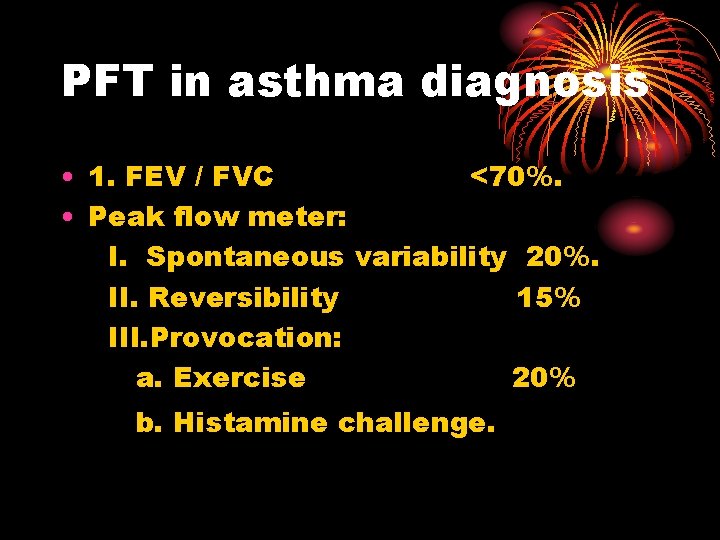
PFT in asthma diagnosis • 1. FEV / FVC <70%. • Peak flow meter: I. Spontaneous variability 20%. II. Reversibility 15% III. Provocation: a. Exercise 20% b. Histamine challenge.

Gas exchange
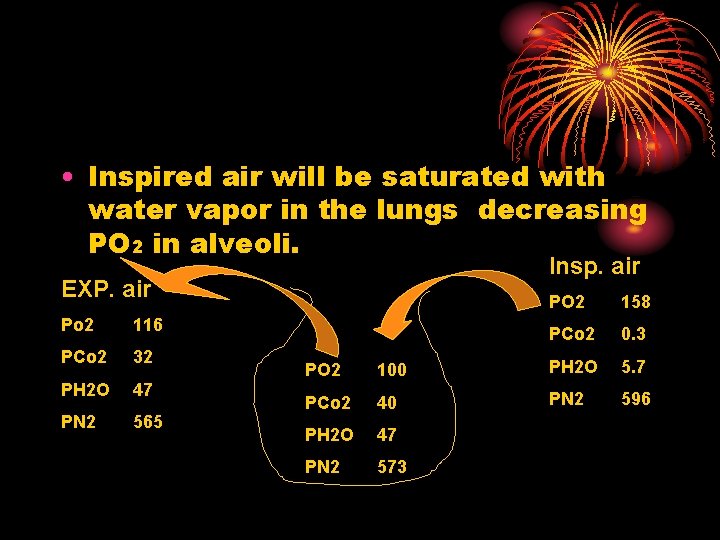
• Inspired air will be saturated with water vapor in the lungs decreasing PO 2 in alveoli. Insp. air EXP. air Po 2 116 PCo 2 32 PH 2 O 47 PN 2 565 PO 2 158 PCo 2 0. 3 PO 2 100 PH 2 O 5. 7 PCo 2 40 PN 2 596 PH 2 O 47 PN 2 573
Oxygen transport
Oxygen transport: • O 2 delivery to the tissues depend on: • 1. O 2 entering the lungs. (PO 2) • 2. Adequacy of gas exchange. • 3. Blood flow to the tissues. • 4. Capacity of the lungs to carry O 2.
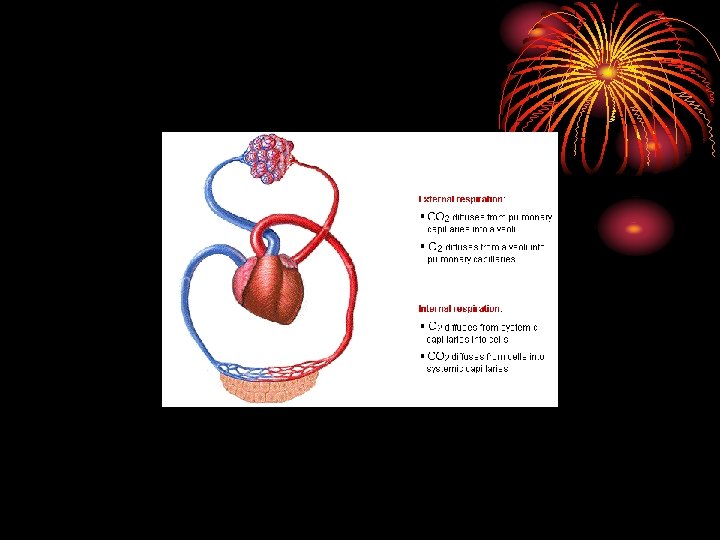
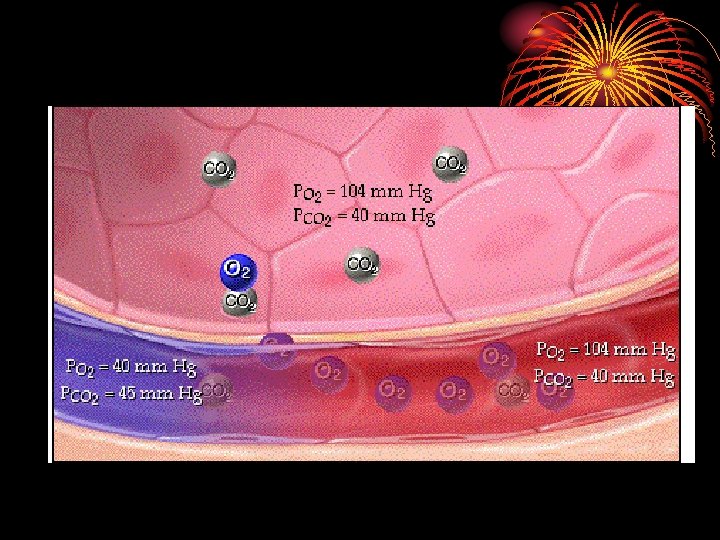
Gas transport between lungs and tissues: • Oxygen diffuses out of alveolar gas into the blood stream and CO 2 diffuses from the blood into the alveoli down their partial press. gradients. • Diffusion capacity of the lungs for a given gas is directly proportional to the alveolocapillary membrane (pulm. epithelium, capillary endothelium & their basement membranes) and inversely proportional to its thickness.
Carriage of O 2: • 1. Dissolved in plasma: 2%, amount dissolved depend on O 2 tension, at PO 2 (100), 0. 3 ml dissolved/100 ml while at PO 2 40 only 0. 12 ml/100 ml blood (venous). • Dissolved O 2 reaches the tissues, imp. For cornea & cartilage. It can be increased by increasing inhaled O 2. • 2. Combined with Hb: 98%, each Hb molecule carries 4 O 2 molecules? and each combination enhances the next?
Oxygen dissociation curve

- Slides: 64