Respiratory Physiology Charlie Hession Pulmonary Circulation Hypoxia Lung
- Slides: 67
Respiratory Physiology Charlie Hession
Pulmonary Circulation Hypoxia Lung Mechanics Control of Breathing (Awake) Topics Covered
Pulmonary Circulation
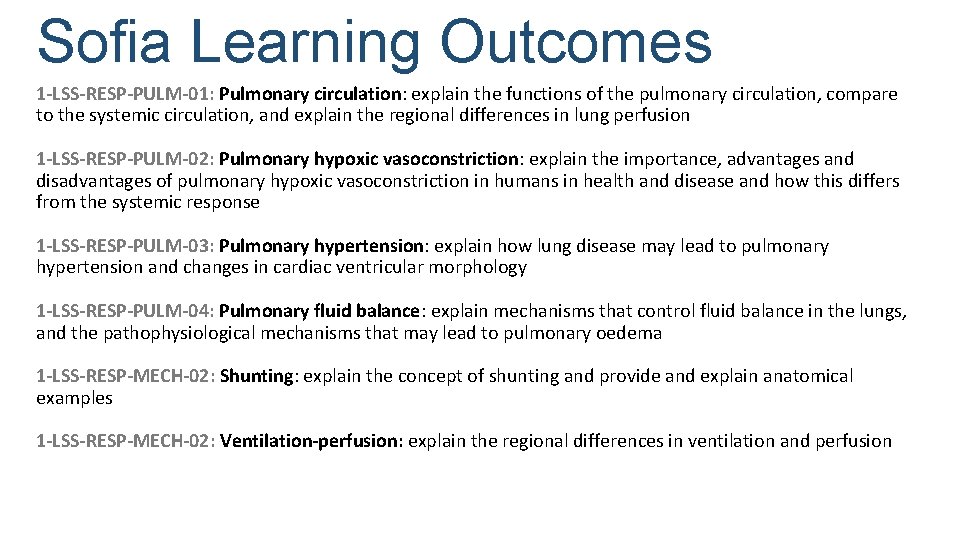
Sofia Learning Outcomes 1 -LSS-RESP-PULM-01: Pulmonary circulation: explain the functions of the pulmonary circulation, compare to the systemic circulation, and explain the regional differences in lung perfusion 1 -LSS-RESP-PULM-02: Pulmonary hypoxic vasoconstriction: explain the importance, advantages and disadvantages of pulmonary hypoxic vasoconstriction in humans in health and disease and how this differs from the systemic response 1 -LSS-RESP-PULM-03: Pulmonary hypertension: explain how lung disease may lead to pulmonary hypertension and changes in cardiac ventricular morphology 1 -LSS-RESP-PULM-04: Pulmonary fluid balance: explain mechanisms that control fluid balance in the lungs, and the pathophysiological mechanisms that may lead to pulmonary oedema 1 -LSS-RESP-MECH-02: Shunting: explain the concept of shunting and provide and explain anatomical examples 1 -LSS-RESP-MECH-02: Ventilation-perfusion: explain the regional differences in ventilation and perfusion
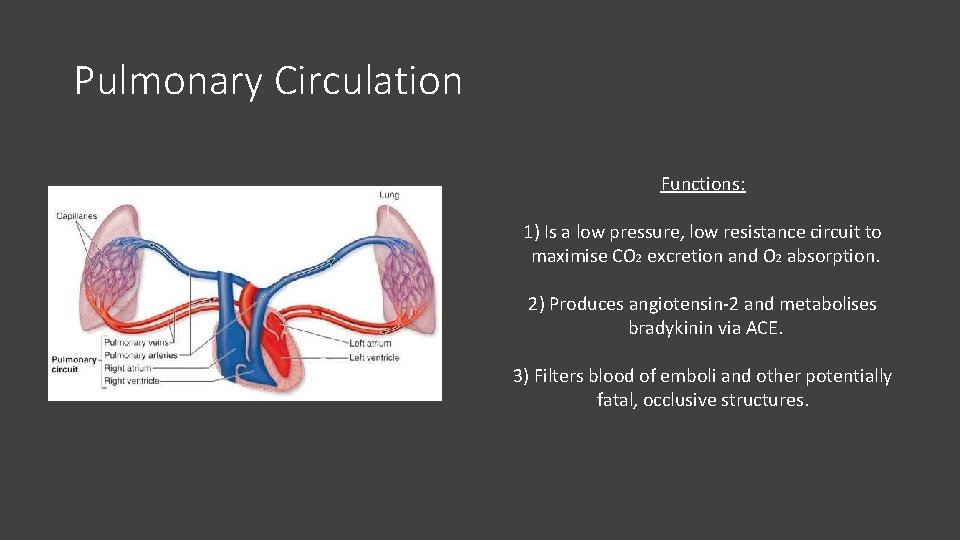
Pulmonary Circulation Functions: 1) Is a low pressure, low resistance circuit to maximise CO 2 excretion and O 2 absorption. 2) Produces angiotensin-2 and metabolises bradykinin via ACE. 3) Filters blood of emboli and other potentially fatal, occlusive structures.
SBA 1 What is the Mean Arterial Pressure (MAP) of the pulmonary circulation? a) 4 mm. Hg b) 7 mm. Hg c) 13 mm. Hg d) 25 mm. Hg e) 93 mm. Hg
SBA 1 What is the Mean Arterial Pressure (MAP) of the pulmonary circulation? a) 4 mm. Hg b) 7 mm. Hg c) 13 mm. Hg d) 25 mm. Hg e) 93 mm. Hg
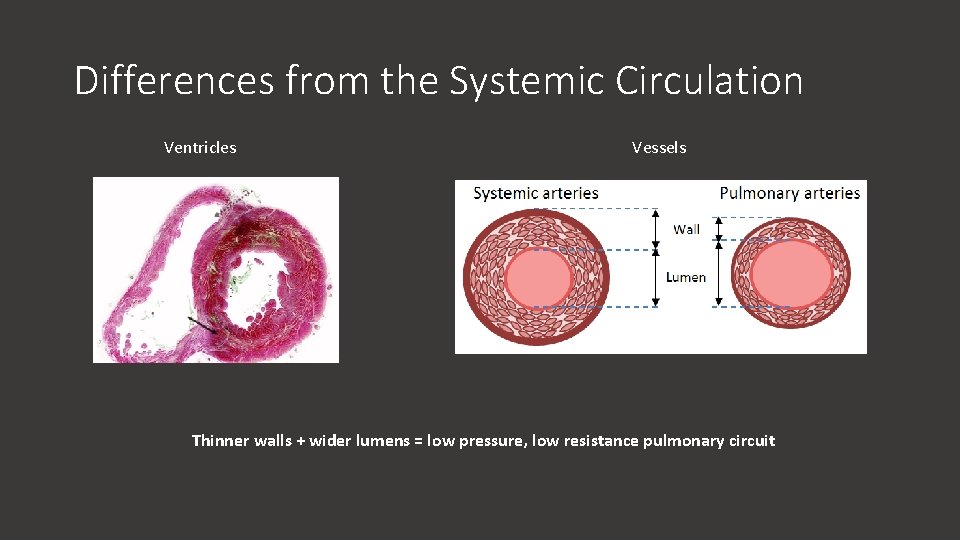
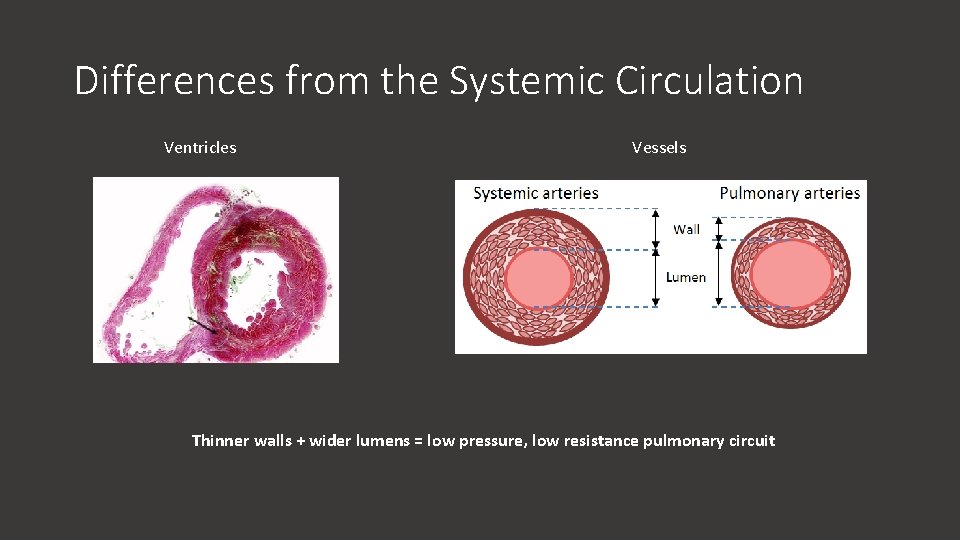
Differences from the Systemic Circulation Ventricles Vessels Thinner walls + wider lumens = low pressure, low resistance pulmonary circuit
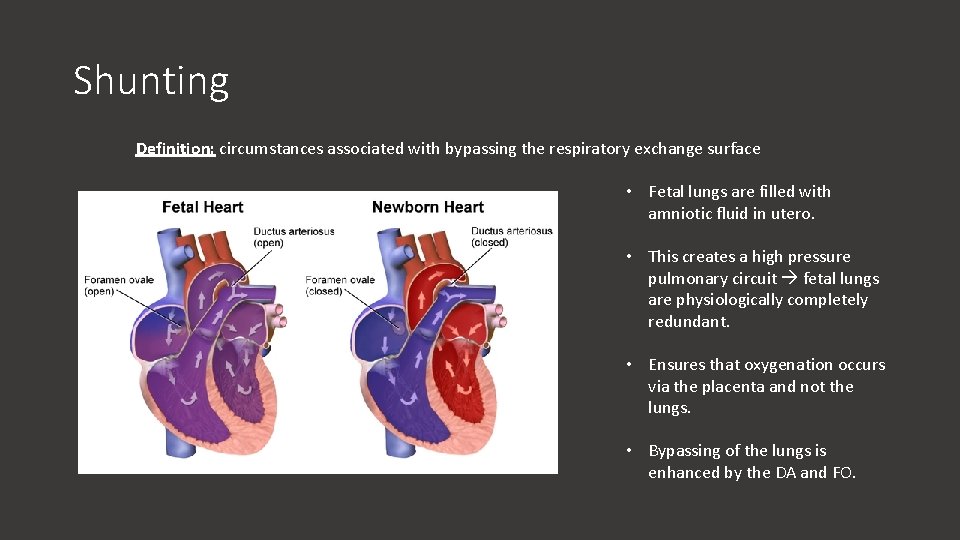
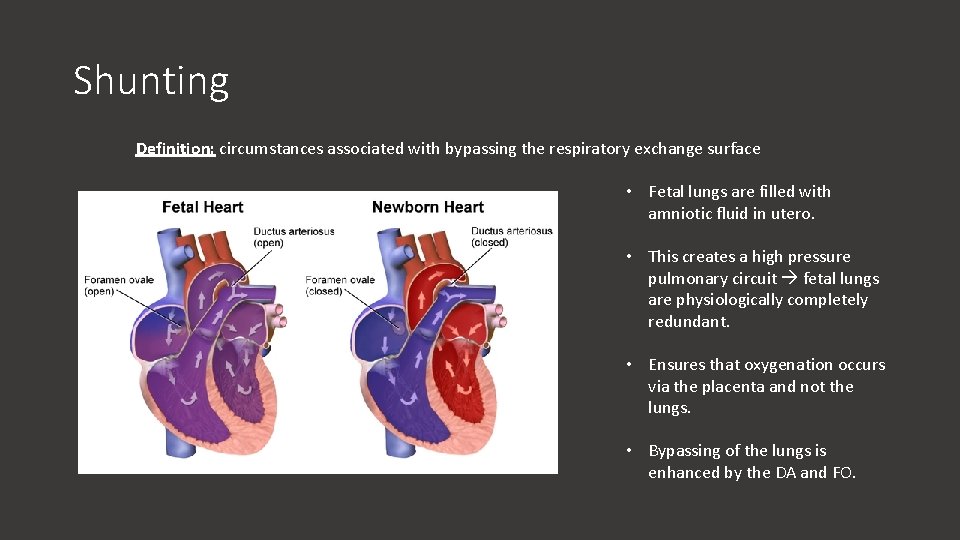
Shunting Definition: circumstances associated with bypassing the respiratory exchange surface • Fetal lungs are filled with amniotic fluid in utero. • This creates a high pressure pulmonary circuit fetal lungs are physiologically completely redundant. • Ensures that oxygenation occurs via the placenta and not the lungs. • Bypassing of the lungs is enhanced by the DA and FO.
ARQ 1 Assertion: The lung apex is better ventilated than the lung base at rest Reason: Basal alveoli are less compliant than apical alveoli at rest a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
ARQ 1 Assertion: The lung apex is better ventilated than the lung base at rest Reason: Basal alveoli are less compliant than apical alveoli at rest a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
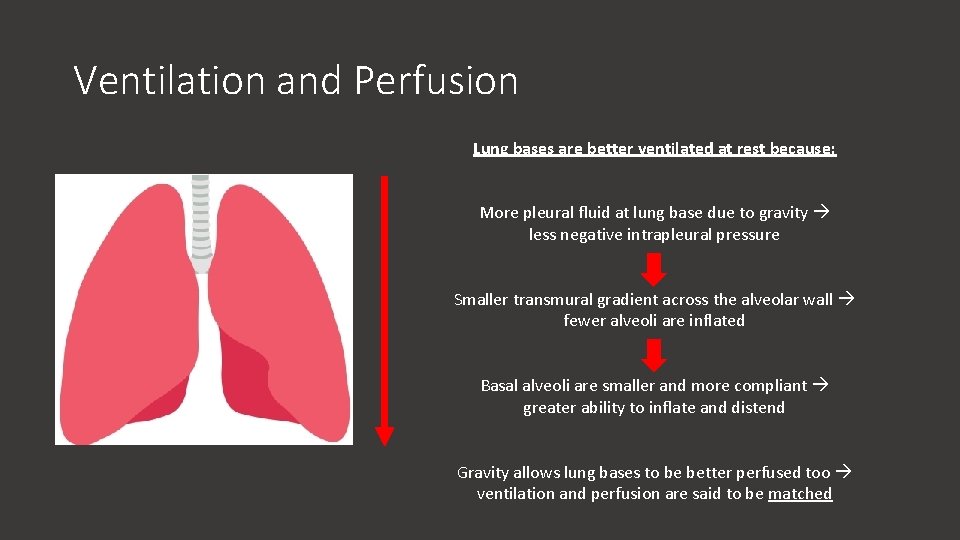
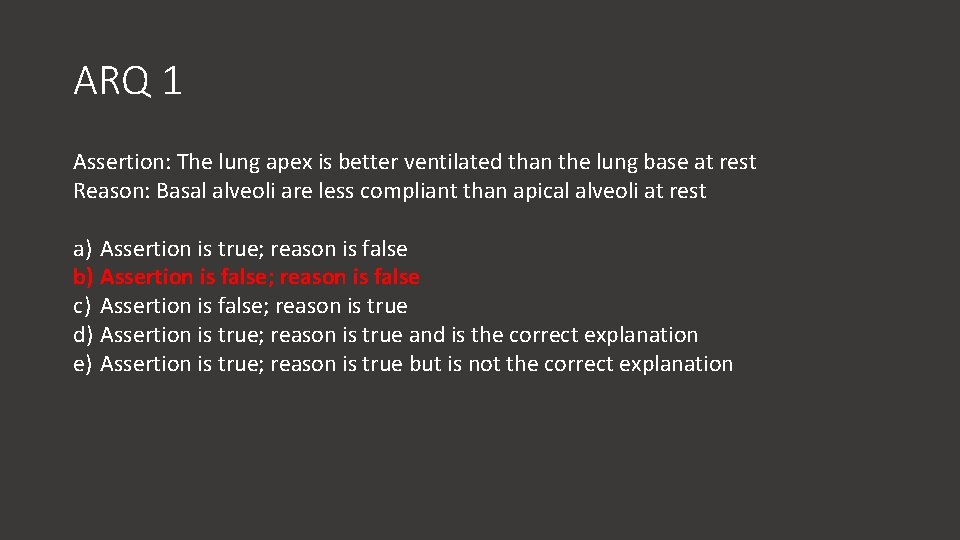
Ventilation and Perfusion Lung bases are better ventilated at rest because: More pleural fluid at lung base due to gravity less negative intrapleural pressure Smaller transmural gradient across the alveolar wall fewer alveoli are inflated Basal alveoli are smaller and more compliant greater ability to inflate and distend Gravity allows lung bases to be better perfused too ventilation and perfusion are said to be matched
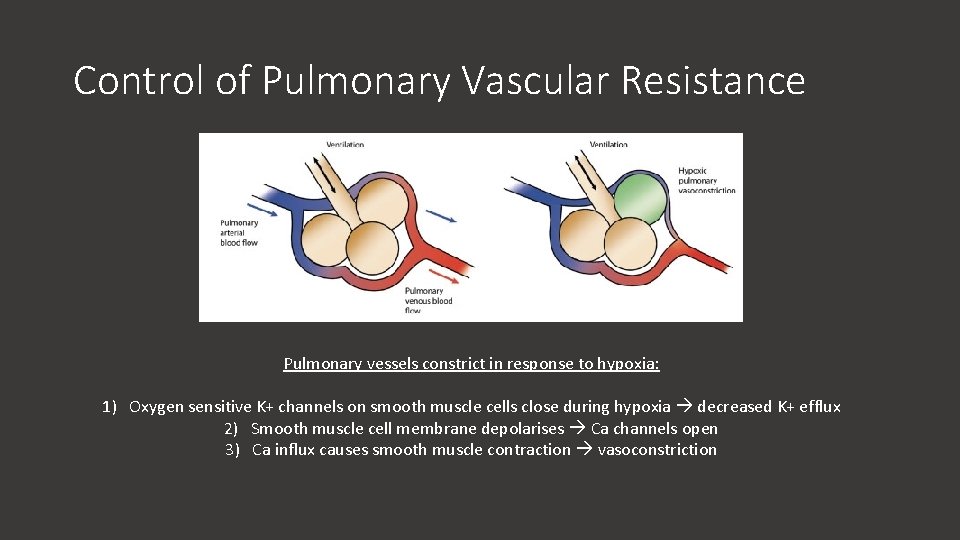
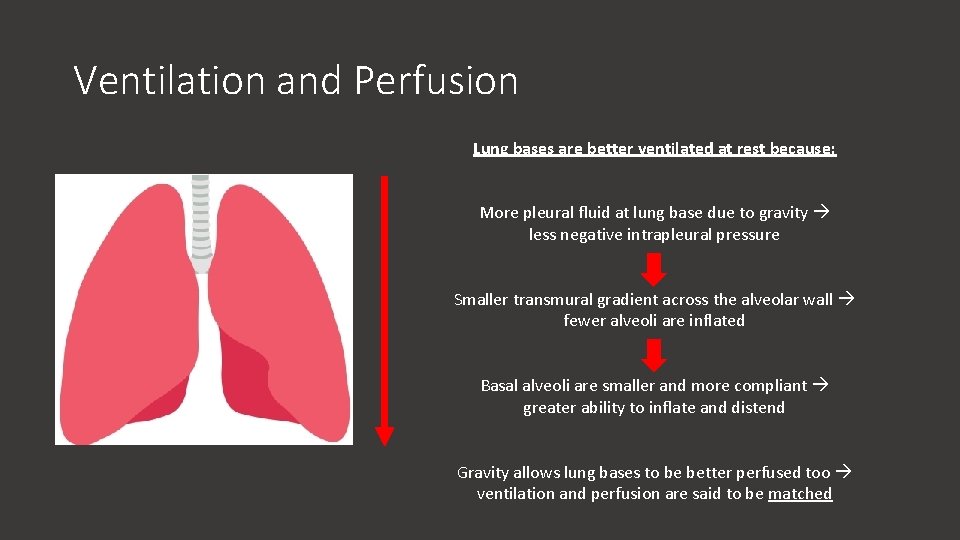
Control of Pulmonary Vascular Resistance Pulmonary vessels constrict in response to hypoxia: 1) Oxygen sensitive K+ channels on smooth muscle cells close during hypoxia decreased K+ efflux 2) Smooth muscle cell membrane depolarises Ca channels open 3) Ca influx causes smooth muscle contraction vasoconstriction
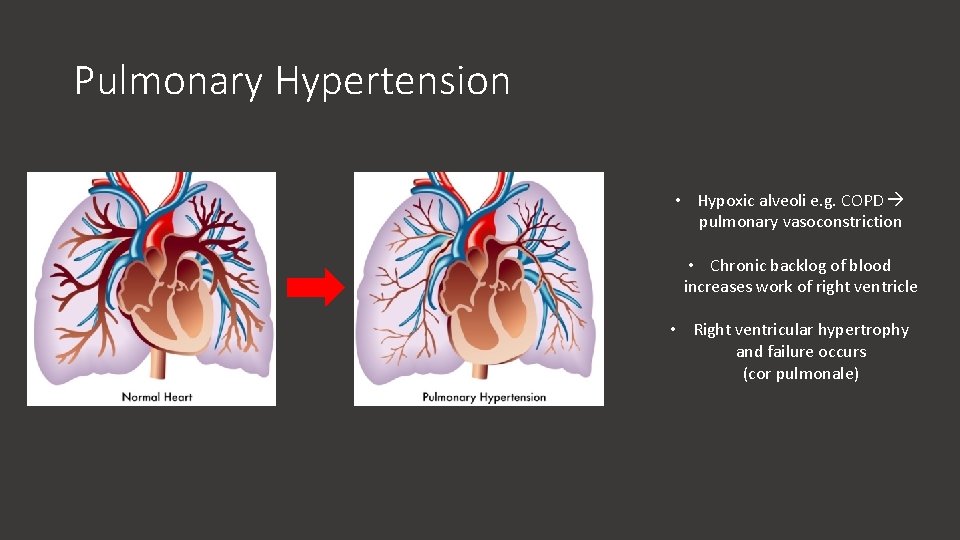
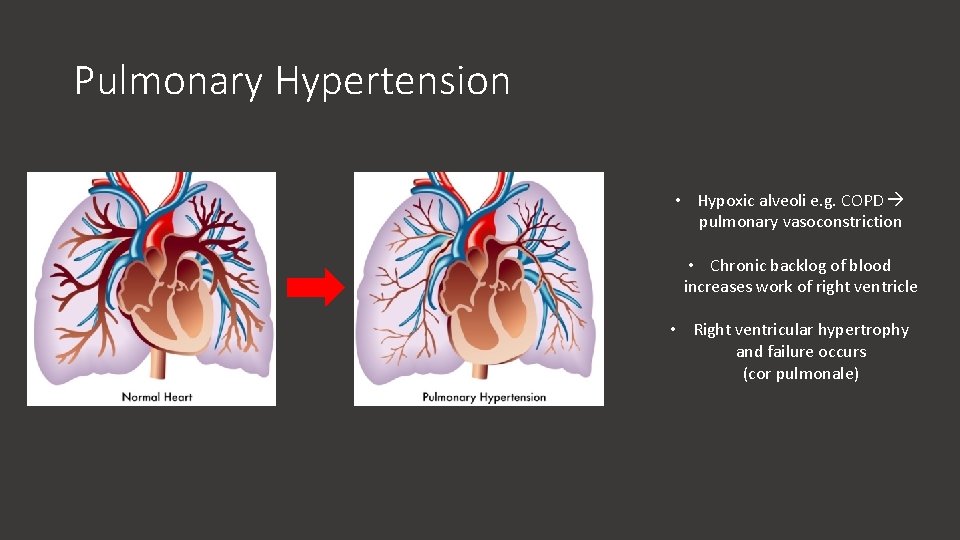
Pulmonary Hypertension • Hypoxic alveoli e. g. COPD pulmonary vasoconstriction • Chronic backlog of blood increases work of right ventricle • Right ventricular hypertrophy and failure occurs (cor pulmonale)
SBA 2 Which of these is not a cause of pulmonary oedema? a) Mitral stenosis b) Left heart failure c) Liver failure d) Pulmonary stenosis e) Lung metastases
SBA 2 Which of these is not a cause of pulmonary oedema? a) Mitral stenosis b) Left heart failure c) Liver failure d) Pulmonary stenosis e) Lung metastases
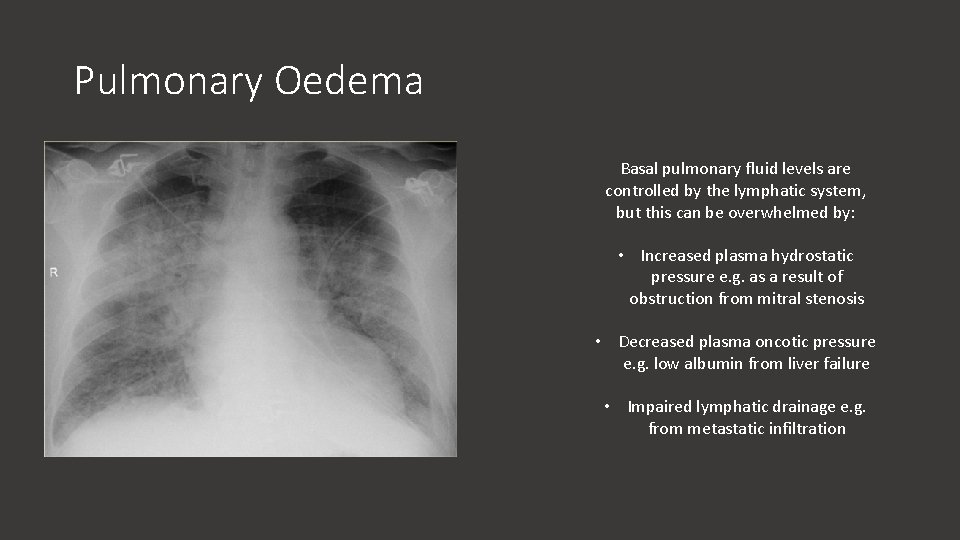
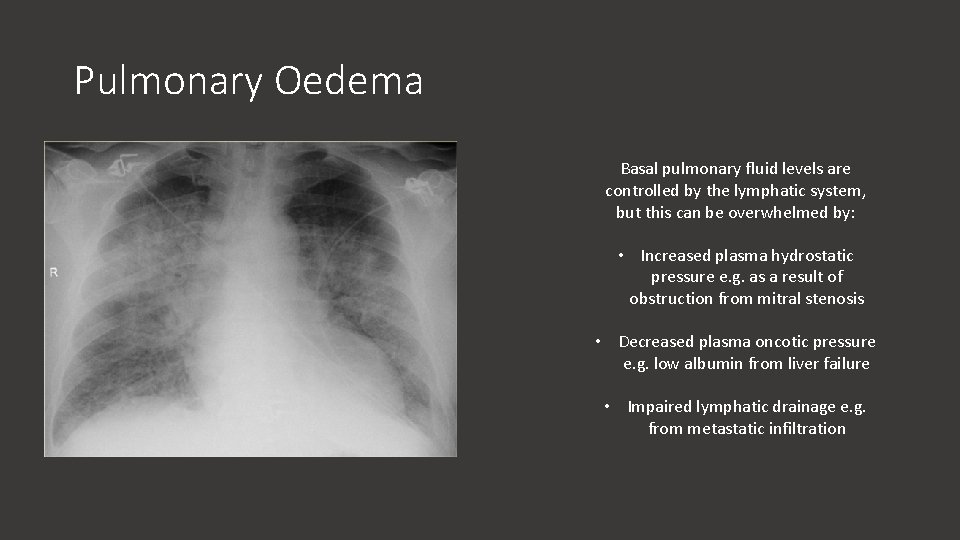
Pulmonary Oedema Basal pulmonary fluid levels are controlled by the lymphatic system, but this can be overwhelmed by: • Increased plasma hydrostatic pressure e. g. as a result of obstruction from mitral stenosis • Decreased plasma oncotic pressure e. g. low albumin from liver failure • Impaired lymphatic drainage e. g. from metastatic infiltration
SAQ 1 1) What are the functions of the pulmonary circulation? (3 marks) 2) Which enzyme degrades bradykinin? (1 mark) 3) Explain the mechanism by which pulmonary vessels constrict during hypoxia (3 marks) 4) Give 3 causes of pulmonary oedema (3 marks)
SAQ 1 1) What are the functions of the pulmonary circulation? (3 marks) • Low pressure, low resistance circuit to facilitate gas exchange • Synthesis of angiotensin-2 and degradation of bradykinin • Filters blood of emboli 2) Which enzyme degrades bradykinin? (1 mark) Angiotensin Converting Enzyme (ACE) 3) Explain the mechanism by which pulmonary vessels constrict during hypoxia (3 marks) • Oxygen sensitive K+ channels on smooth muscle cells close during hypoxia decreased K+ efflux • Smooth muscle cell membrane depolarises Ca channels open • Ca influx causes smooth muscle contraction vasoconstriction 4) Give 3 causes of pulmonary oedema (3 marks) • Mitral stenosis • Liver failure • Lung metastases • Left heart failure
Hypoxia
Sofia Learning Outcomes 1 -LSS-RESP-GAS-01: Oxygen cascade: summarise the oxygen cascade 1 -LSS-RESP-GAS-03: Gas transport: explain how respiratory gases are transported in the blood, explain key gas laws involved including Henry, Fick, Dalton, Boyle and Charles; explain how respiratory gas transport changes in exercise and at altitude 1 -LSS-RESP-GAS-04: Dissociation curves: explain respiratory gas dissociation curves and how these are affected by physiological and environmental changes 1 -LSS-RESP-GAS-07: Acid-base disturbance: explain the changes in blood gas measurements in acidosis (respiratory / metabolic), alkalosis (respiratory / metabolic) and respiratory failure (type 1 / type 2) 1 -LSS-RESP-GAS-10: Altitude sickness: explain the effects of altitude on oxygen availability, explain the acute and long term compensatory physiological mechanisms to high altitude, explain the pathophysiological cause of high-altitude pulmonary and cerebral oedema, and recall the first line interventions to treat altitude sickness
Definitions Hypoxic: describes a low oxygen environment Hypoxemic: describes low blood oxygen levels Hypoxia Systemic Pulmonary
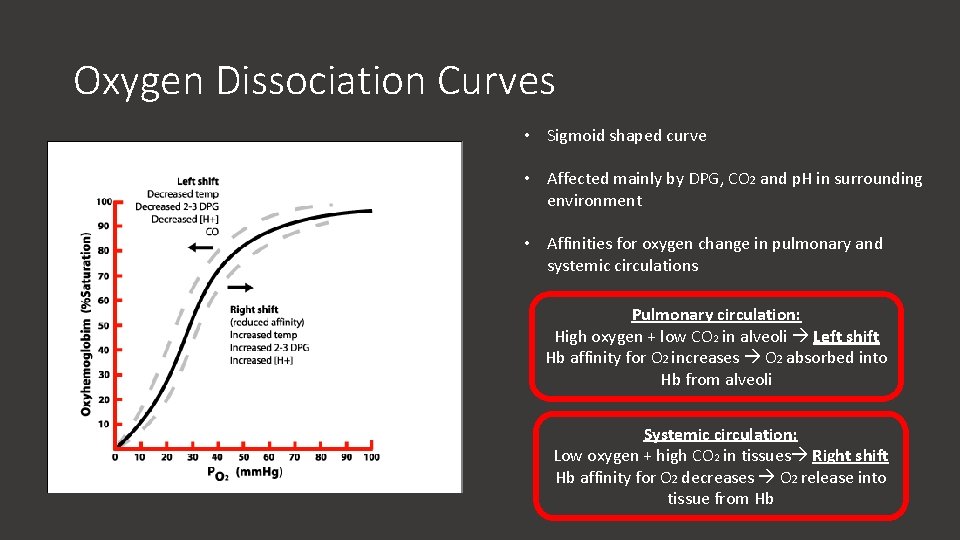
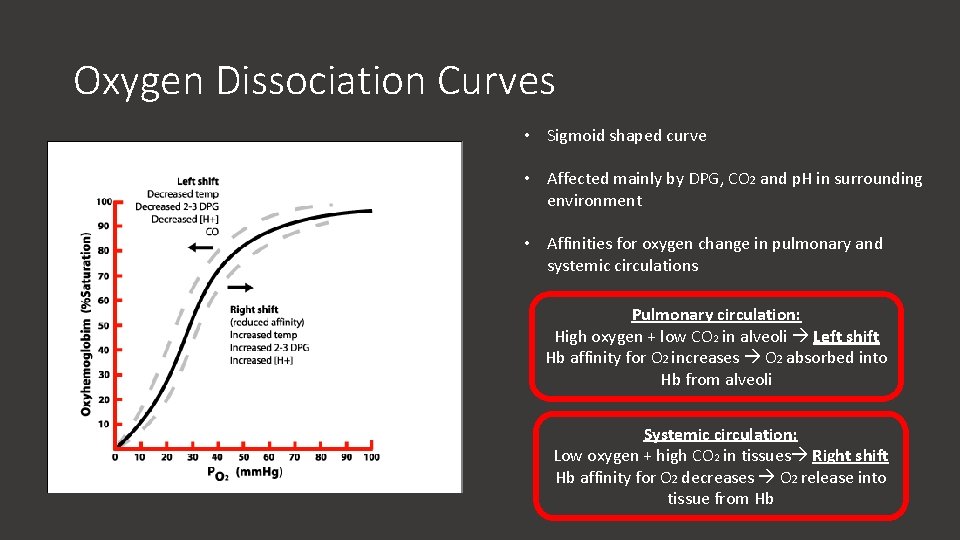
Oxygen Dissociation Curves • Sigmoid shaped curve • Affected mainly by DPG, CO 2 and p. H in surrounding environment • Affinities for oxygen change in pulmonary and systemic circulations Pulmonary circulation: High oxygen + low CO 2 in alveoli Left shift Hb affinity for O 2 increases O 2 absorbed into Hb from alveoli Systemic circulation: Low oxygen + high CO 2 in tissues Right shift Hb affinity for O 2 decreases O 2 release into tissue from Hb
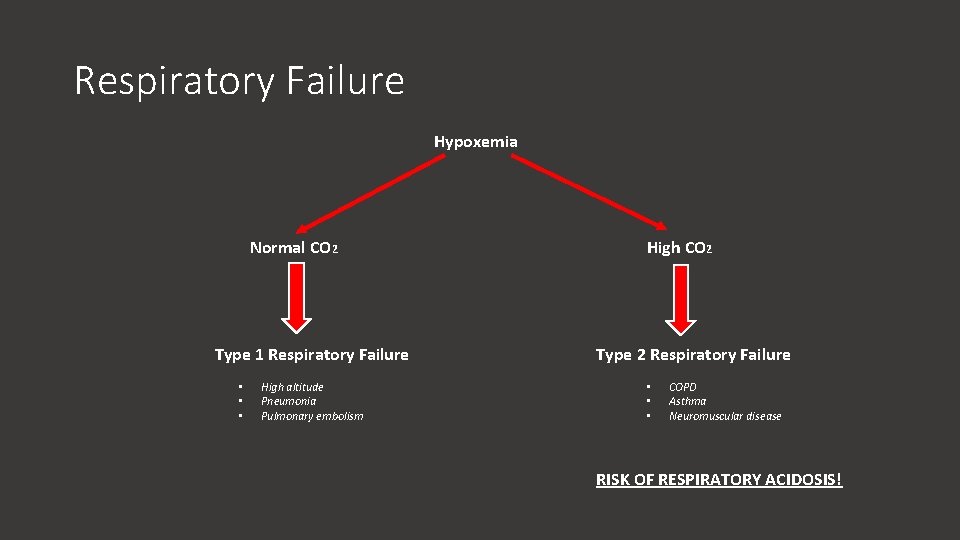
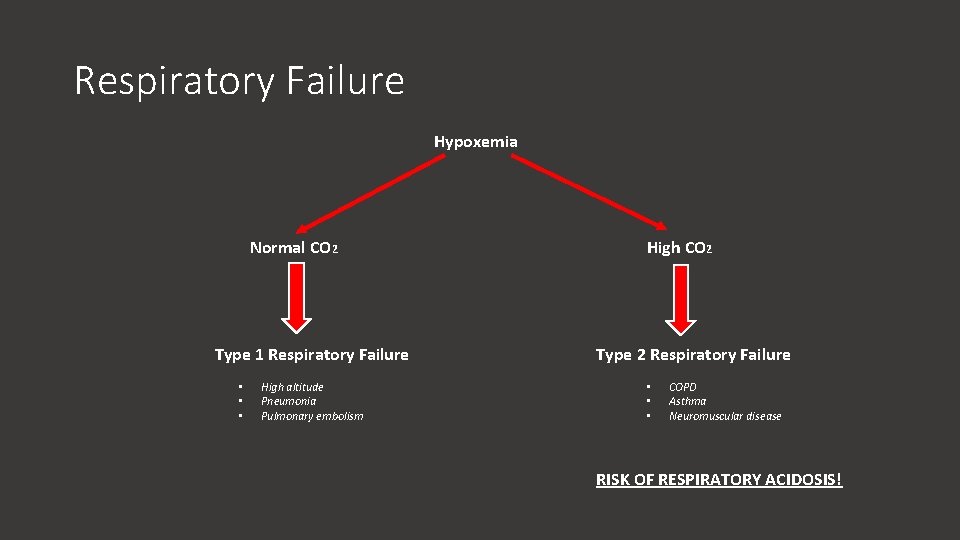
Respiratory Failure Hypoxemia Normal CO 2 Type 1 Respiratory Failure • • • High altitude Pneumonia Pulmonary embolism High CO 2 Type 2 Respiratory Failure • • • COPD Asthma Neuromuscular disease RISK OF RESPIRATORY ACIDOSIS!
SBA 3 Which of the following is the most likely acid-base abnormality found in altitude sickness? a) Respiratory alkalosis b) Respiratory acidosis c) Metabolic alkalosis d) Metabolic acidosis e) Mixed respiratory and metabolic acidosis
SBA 3 Which of the following is the most likely acid-base abnormality found in altitude sickness? a) Respiratory alkalosis b) Respiratory acidosis c) Metabolic alkalosis d) Metabolic acidosis e) Mixed respiratory and metabolic acidosis
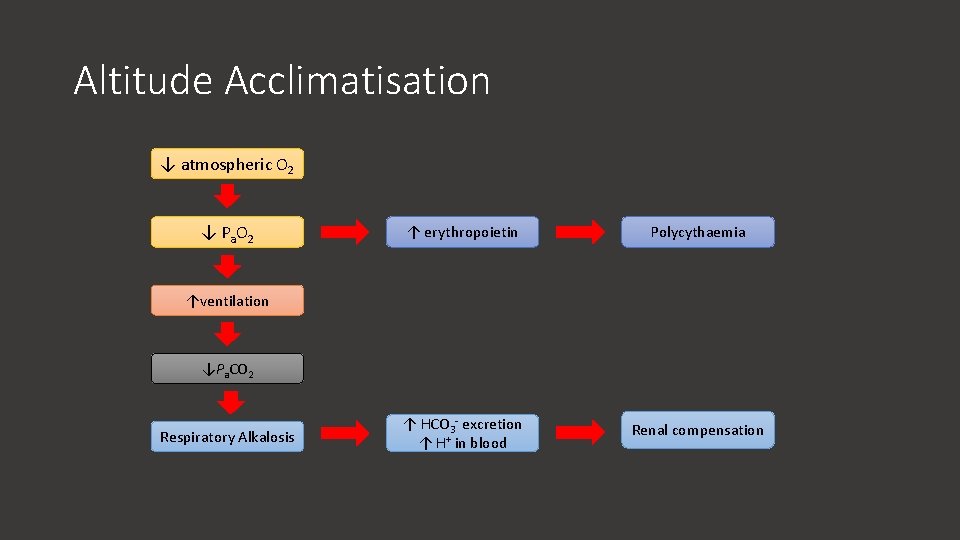
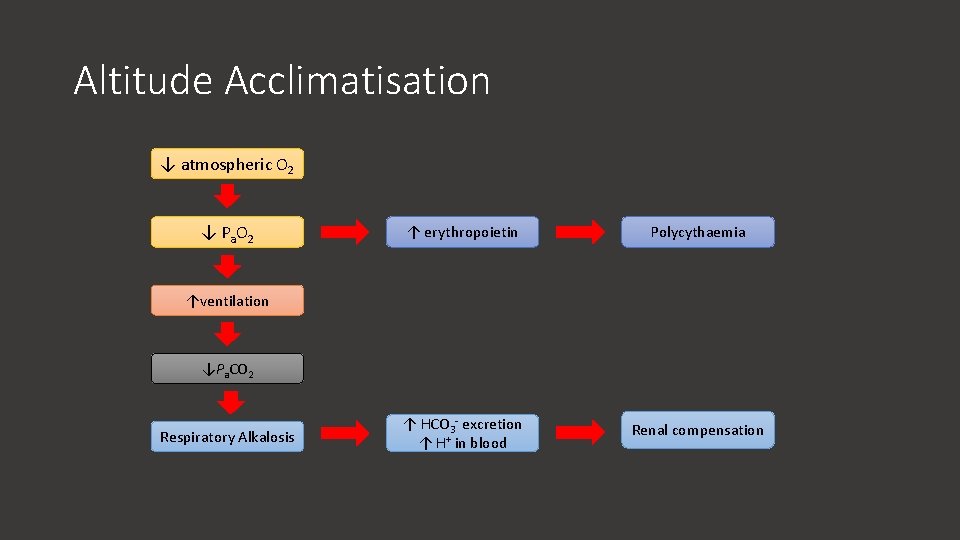
Altitude Acclimatisation ↓ atmospheric O 2 ↓ P a O 2 ↑ erythropoietin Polycythaemia ↑ HCO 3 - excretion ↑ H+ in blood Renal compensation ↑ventilation ↓Pa. CO 2 Respiratory Alkalosis
ARQ 2 Assertion: Cerebral oedema may occur at high altitude Reason: The systemic response to hypoxia is vasodilation a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
ARQ 2 Assertion: Cerebral oedema may occur at high altitude Reason: The systemic response to hypoxia is vasodilation a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
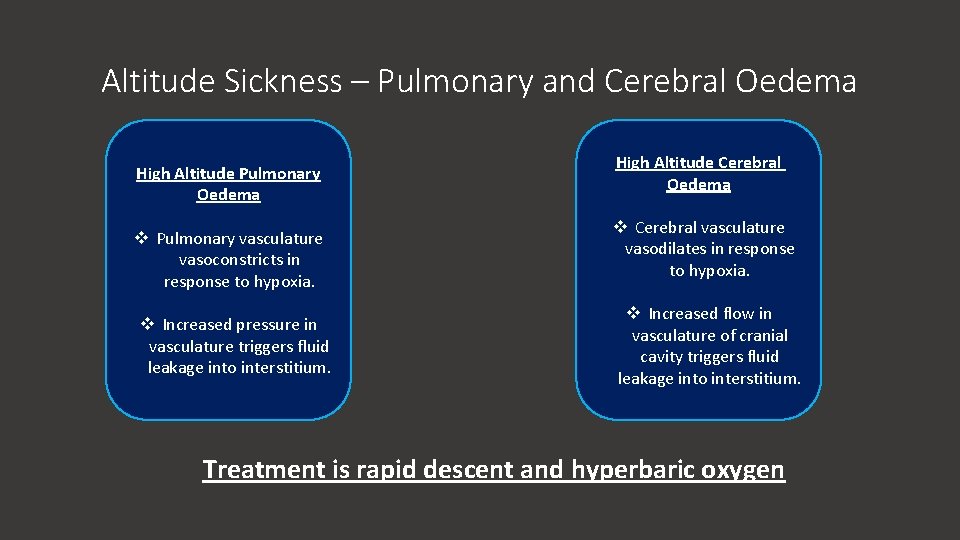
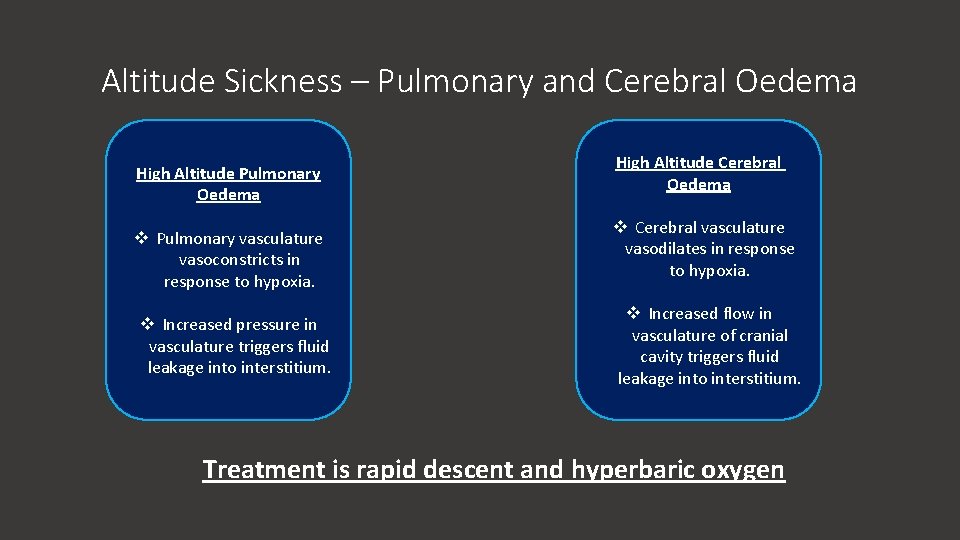
Altitude Sickness – Pulmonary and Cerebral Oedema High Altitude Pulmonary Oedema v Pulmonary vasculature vasoconstricts in response to hypoxia. v Increased pressure in vasculature triggers fluid leakage into interstitium. High Altitude Cerebral Oedema v Cerebral vasculature vasodilates in response to hypoxia. v Increased flow in vasculature of cranial cavity triggers fluid leakage into interstitium. Treatment is rapid descent and hyperbaric oxygen
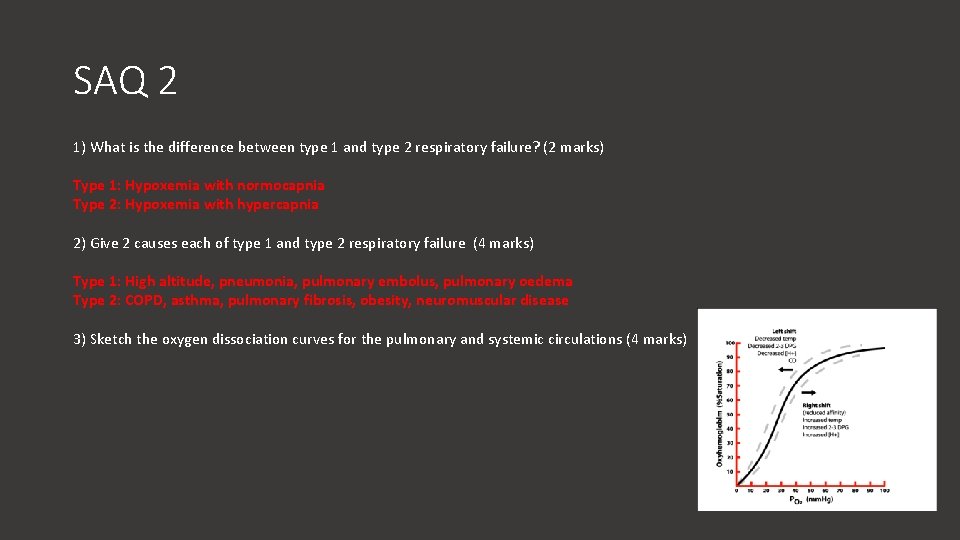
SAQ 2 1) What is the difference between type 1 and type 2 respiratory failure? (2 marks) 2) Give 2 causes each of type 1 and type 2 respiratory failure (4 marks) 3) Sketch the oxygen dissociation curves for the pulmonary and systemic circulations (4 marks)
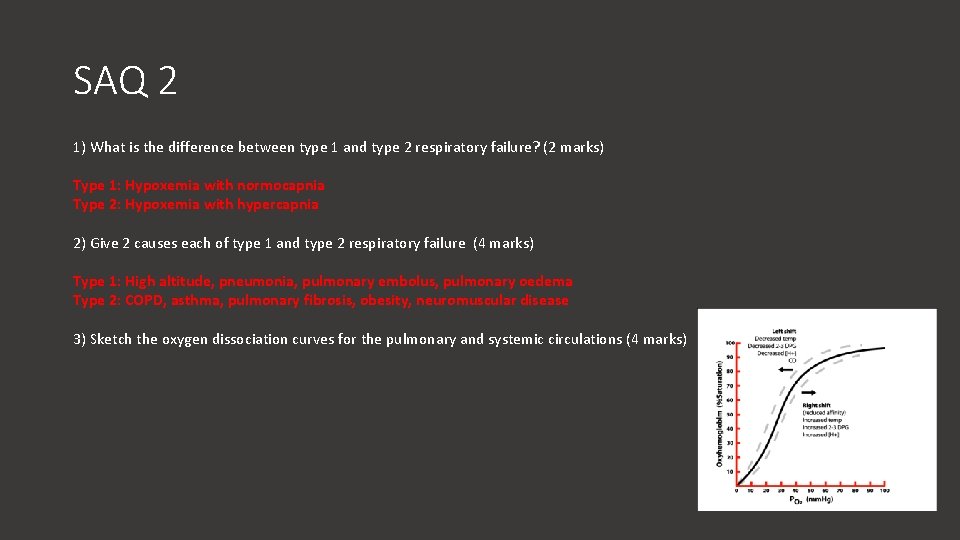
SAQ 2 1) What is the difference between type 1 and type 2 respiratory failure? (2 marks) Type 1: Hypoxemia with normocapnia Type 2: Hypoxemia with hypercapnia 2) Give 2 causes each of type 1 and type 2 respiratory failure (4 marks) Type 1: High altitude, pneumonia, pulmonary embolus, pulmonary oedema Type 2: COPD, asthma, pulmonary fibrosis, obesity, neuromuscular disease 3) Sketch the oxygen dissociation curves for the pulmonary and systemic circulations (4 marks)
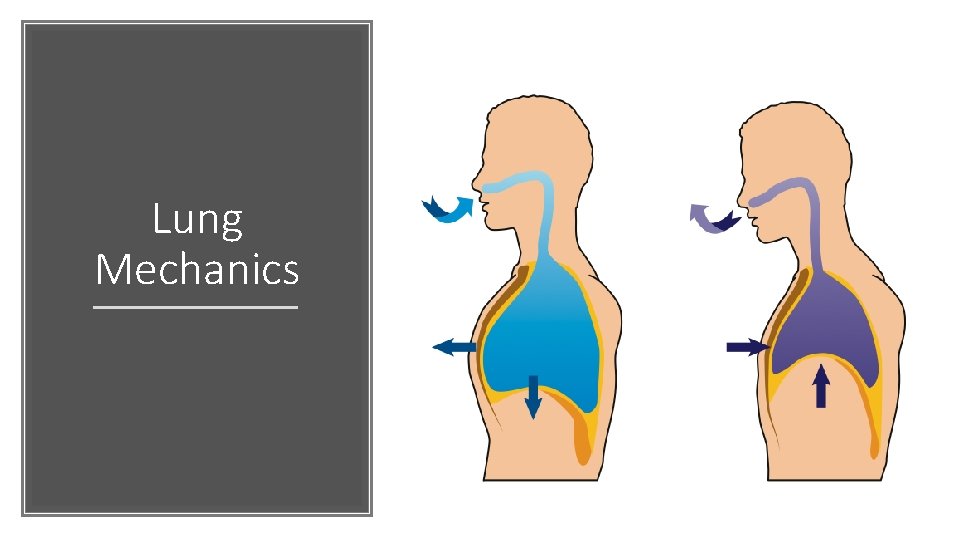
Lung Mechanics
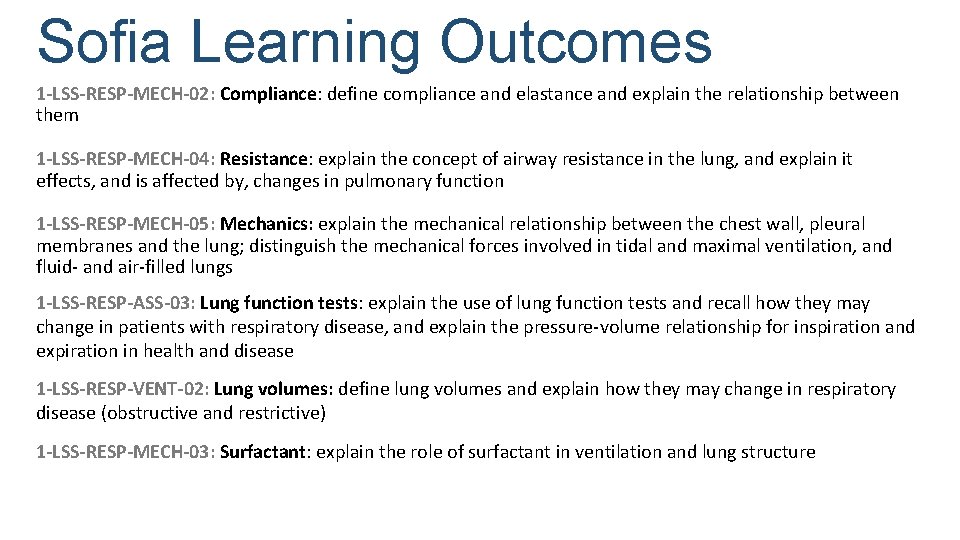
Sofia Learning Outcomes 1 -LSS-RESP-MECH-02: Compliance: define compliance and elastance and explain the relationship between them 1 -LSS-RESP-MECH-04: Resistance: explain the concept of airway resistance in the lung, and explain it effects, and is affected by, changes in pulmonary function 1 -LSS-RESP-MECH-05: Mechanics: explain the mechanical relationship between the chest wall, pleural membranes and the lung; distinguish the mechanical forces involved in tidal and maximal ventilation, and fluid- and air-filled lungs 1 -LSS-RESP-ASS-03: Lung function tests: explain the use of lung function tests and recall how they may change in patients with respiratory disease, and explain the pressure-volume relationship for inspiration and expiration in health and disease 1 -LSS-RESP-VENT-02: Lung volumes: define lung volumes and explain how they may change in respiratory disease (obstructive and restrictive) 1 -LSS-RESP-MECH-03: Surfactant: explain the role of surfactant in ventilation and lung structure
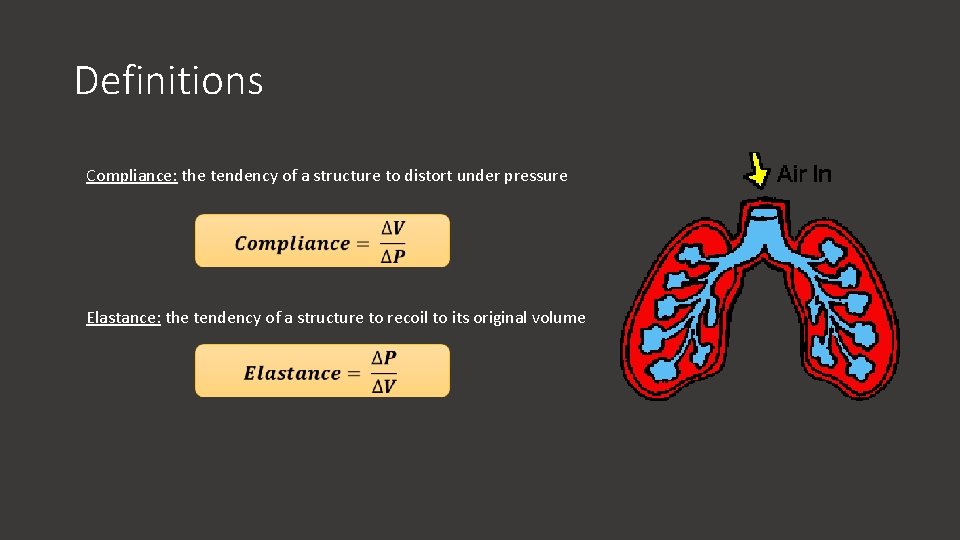
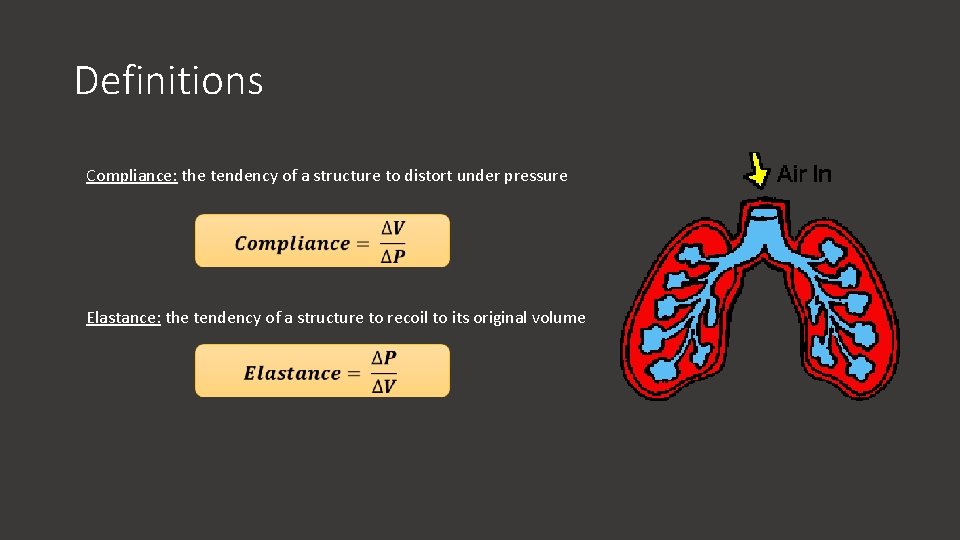
Definitions Compliance: the tendency of a structure to distort under pressure Elastance: the tendency of a structure to recoil to its original volume
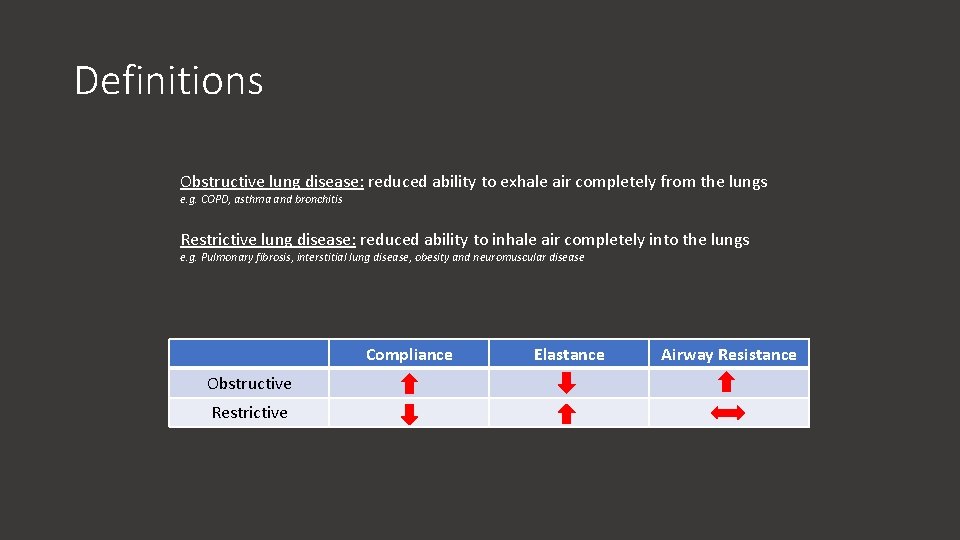
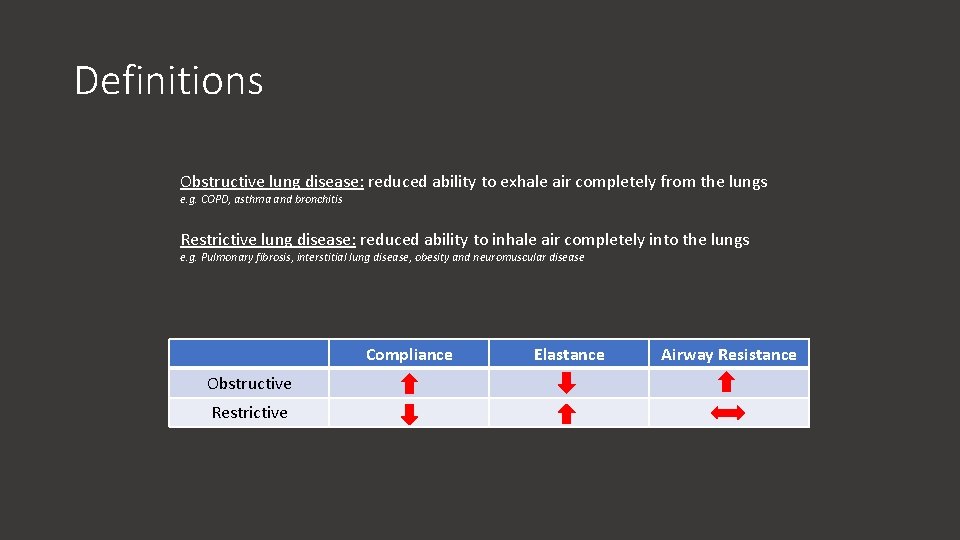
Definitions Obstructive lung disease: reduced ability to exhale air completely from the lungs e. g. COPD, asthma and bronchitis Restrictive lung disease: reduced ability to inhale air completely into the lungs e. g. Pulmonary fibrosis, interstitial lung disease, obesity and neuromuscular disease Compliance Obstructive Restrictive Elastance Airway Resistance
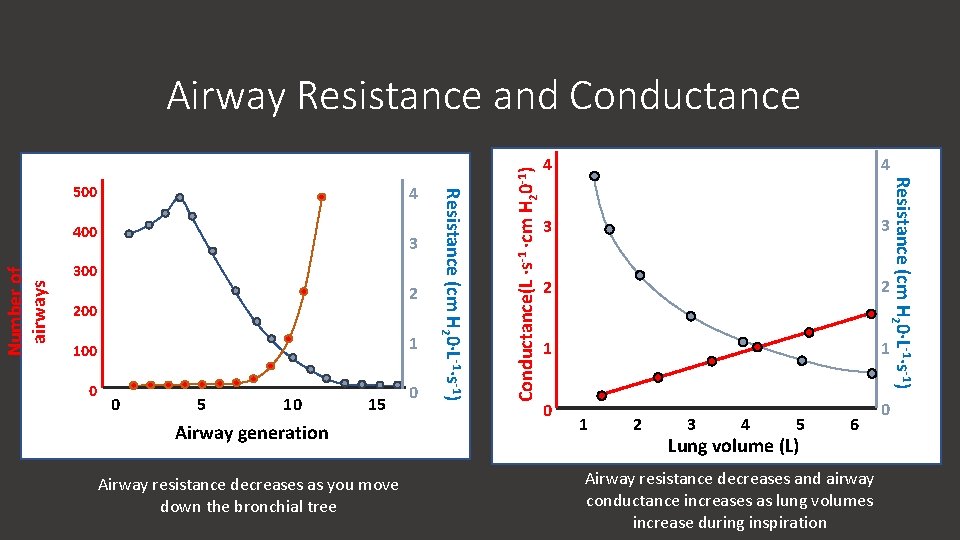
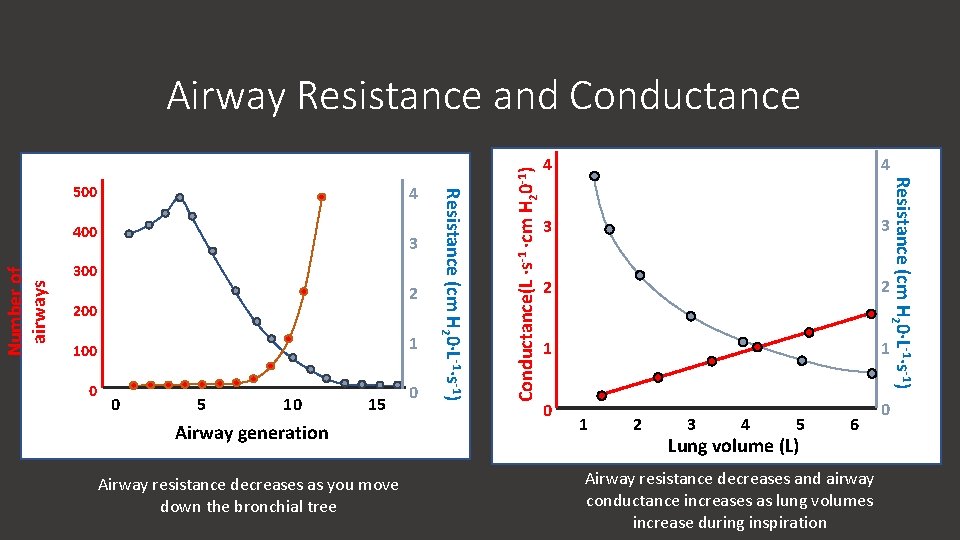
Number of airways 400 3 300 2 200 1 100 0 0 5 10 15 Airway generation Airway resistance decreases as you move down the bronchial tree 0 4 4 3 3 2 2 1 1 0 0 Resistance (cm H 20∙L-1∙s-1) 4 Resistance (cm H 20∙L-1∙s-1) 500 Conductance(L ∙s-1 ∙cm H 20 -1) Airway Resistance and Conductance 1 2 3 4 5 Lung volume (L) 6 Airway resistance decreases and airway conductance increases as lung volumes increase during inspiration
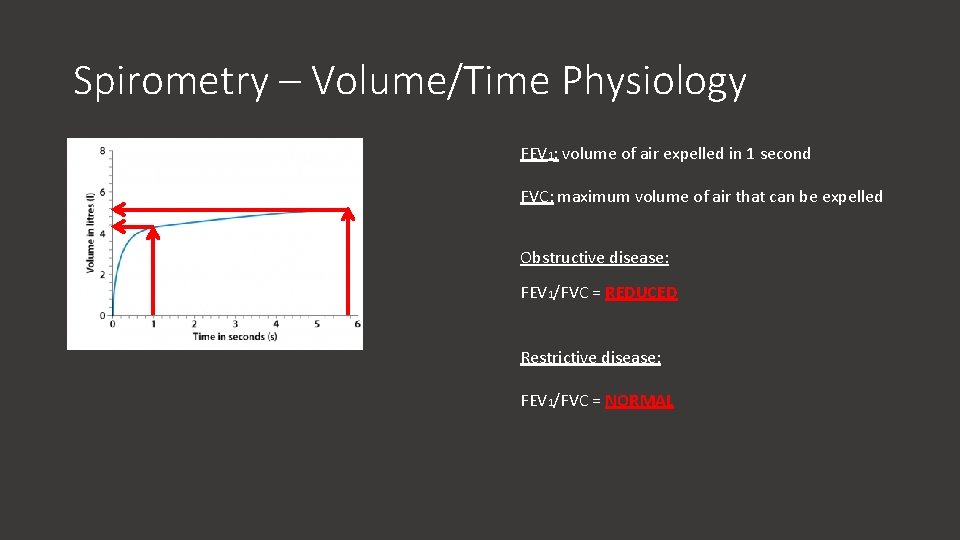
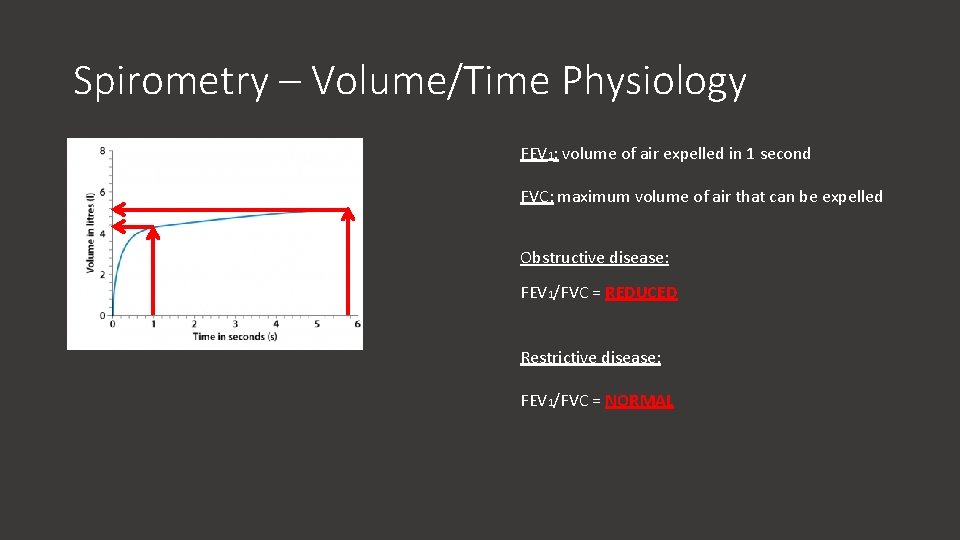
Spirometry – Volume/Time Physiology FEV 1: volume of air expelled in 1 second FVC: maximum volume of air that can be expelled Obstructive disease: FEV 1/FVC = REDUCED Restrictive disease: FEV 1/FVC = NORMAL
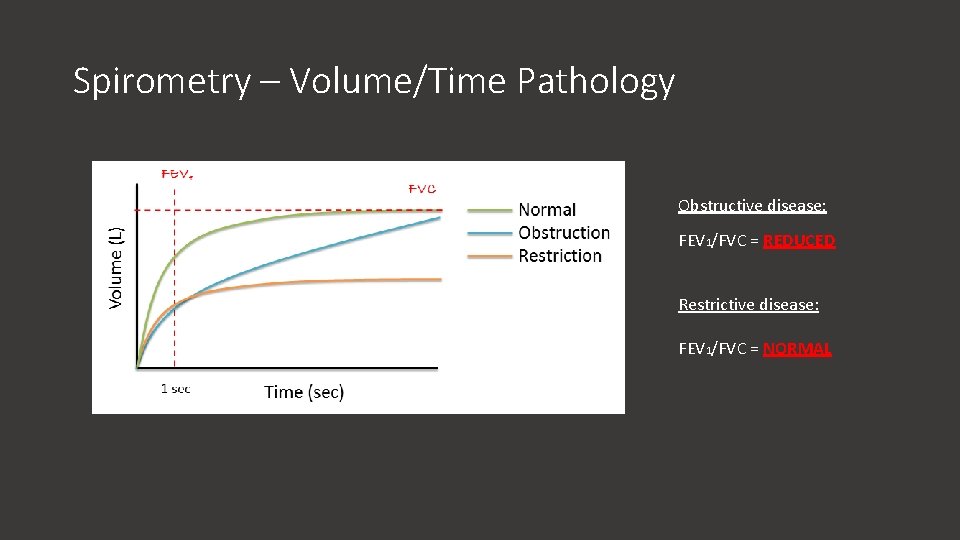
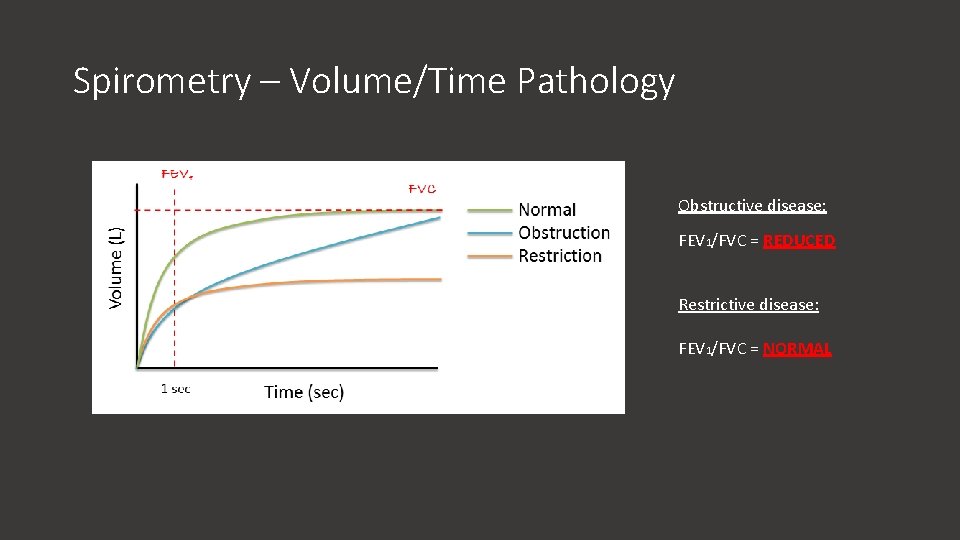
Spirometry – Volume/Time Pathology Obstructive disease: FEV 1/FVC = REDUCED Restrictive disease: FEV 1/FVC = NORMAL
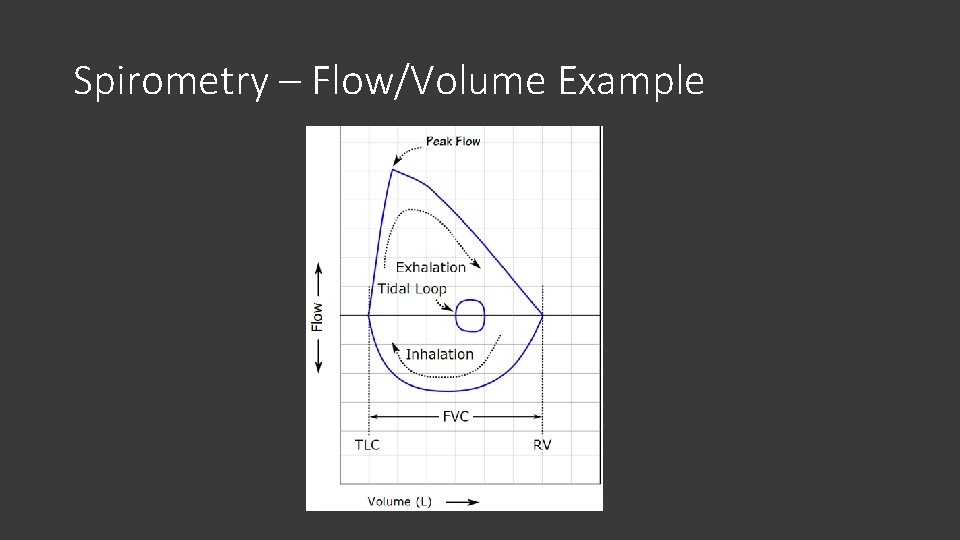
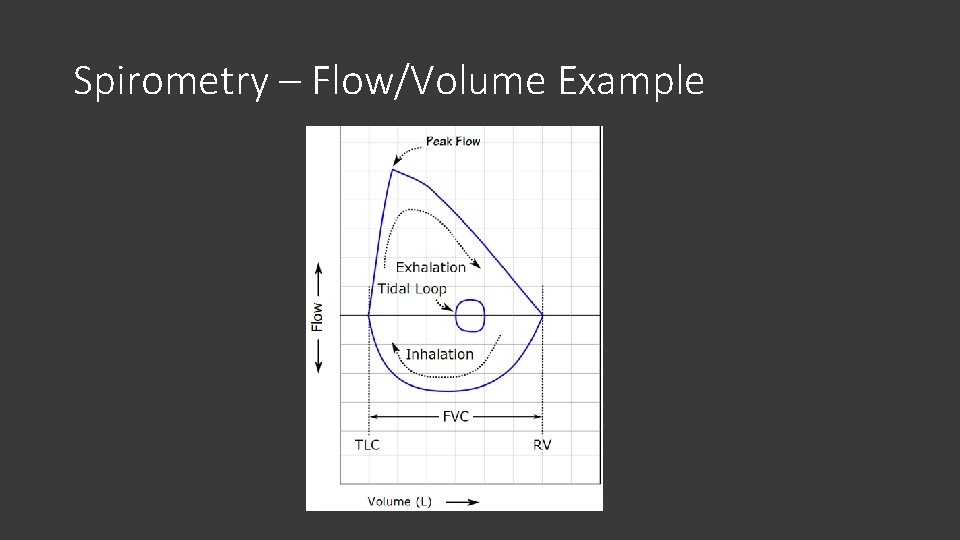
Spirometry – Flow/Volume Example
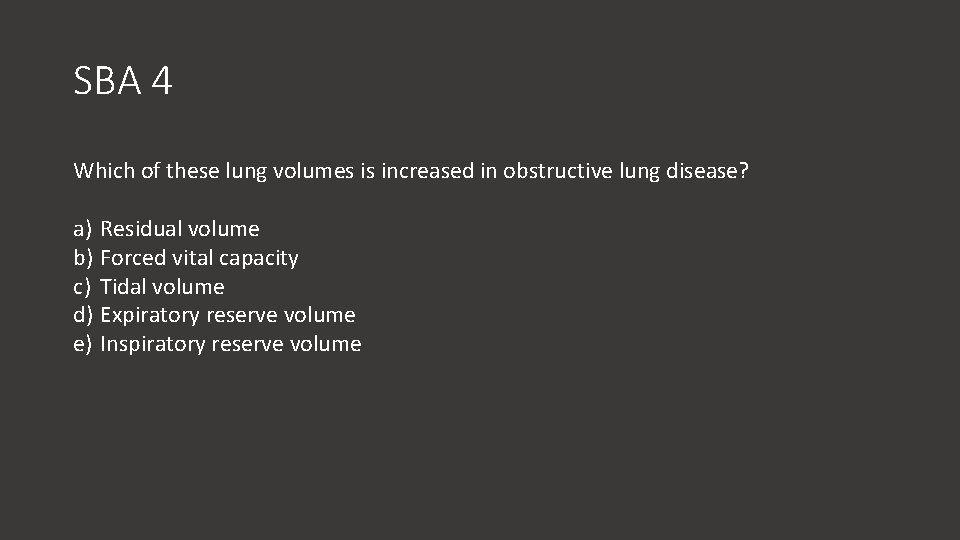
SBA 4 Which of these lung volumes is increased in obstructive lung disease? a) Residual volume b) Forced vital capacity c) Tidal volume d) Expiratory reserve volume e) Inspiratory reserve volume
SBA 4 Which of these lung volumes is increased in obstructive lung disease? a) Residual volume b) Forced vital capacity c) Tidal volume d) Expiratory reserve volume e) Inspiratory reserve volume
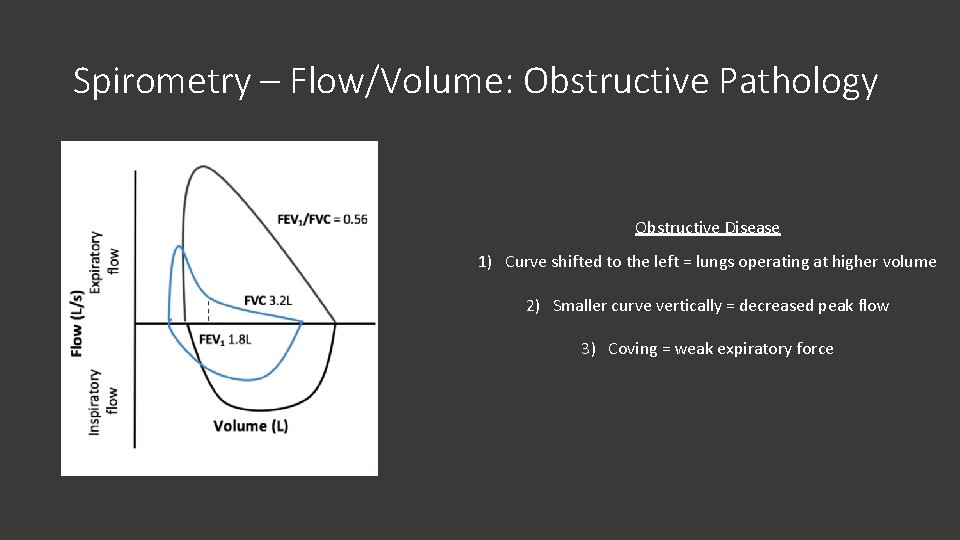
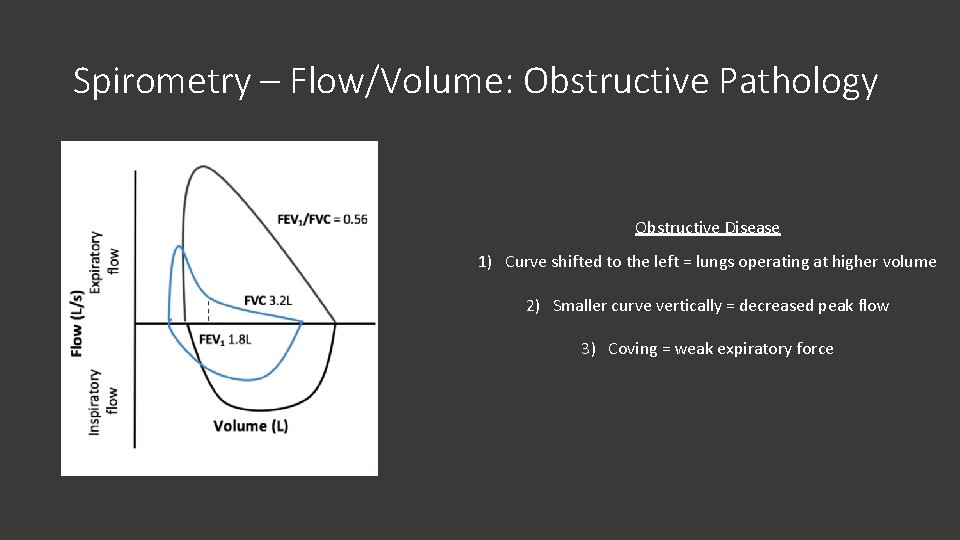
Spirometry – Flow/Volume: Obstructive Pathology Obstructive Disease 1) Curve shifted to the left = lungs operating at higher volume 2) Smaller curve vertically = decreased peak flow 3) Coving = weak expiratory force
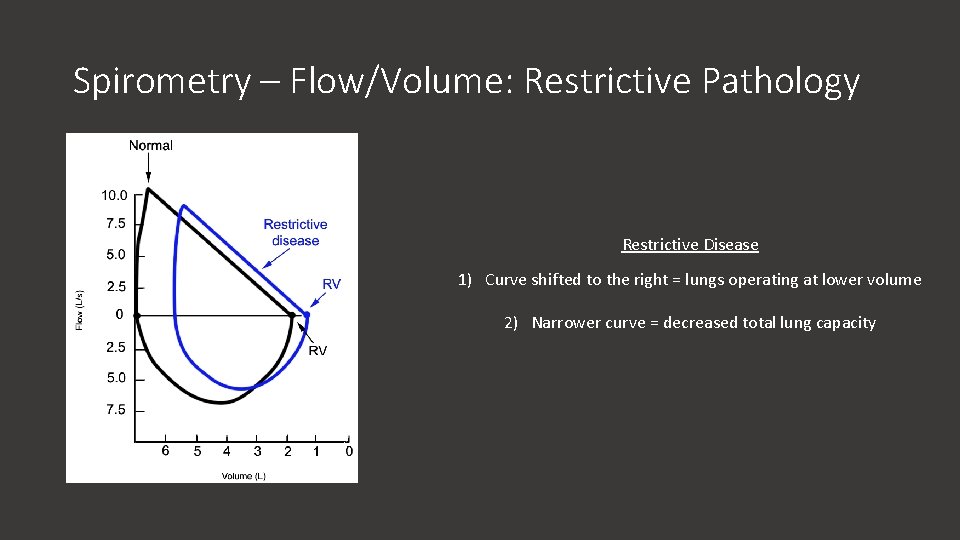
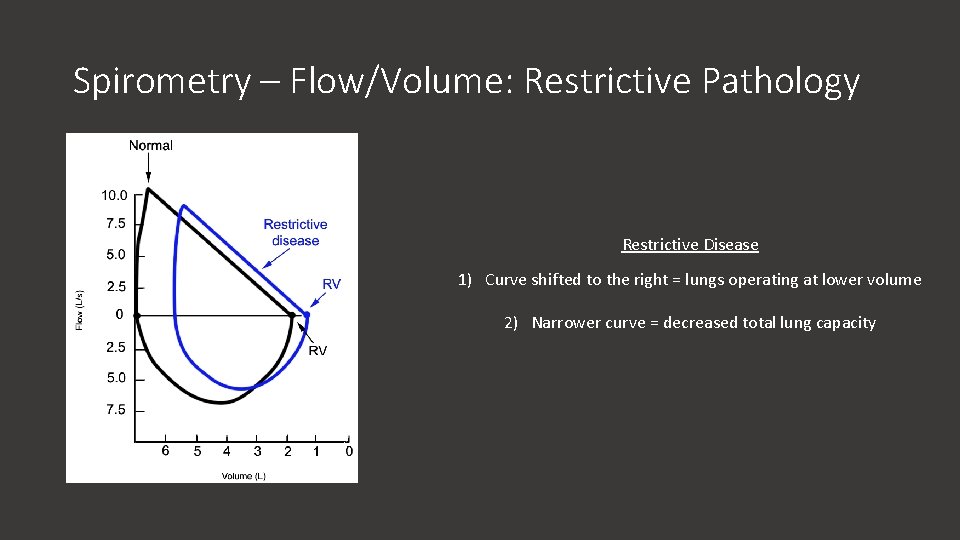
Spirometry – Flow/Volume: Restrictive Pathology Restrictive Disease 1) Curve shifted to the right = lungs operating at lower volume 2) Narrower curve = decreased total lung capacity
ARQ 3 Assertion: During inspiration, Palv becomes more negative Reason: During inspiration, Ppl becomes more positive a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
ARQ 3 Assertion: During inspiration, Palv becomes more negative Reason: During inspiration, Ppl becomes more positive a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
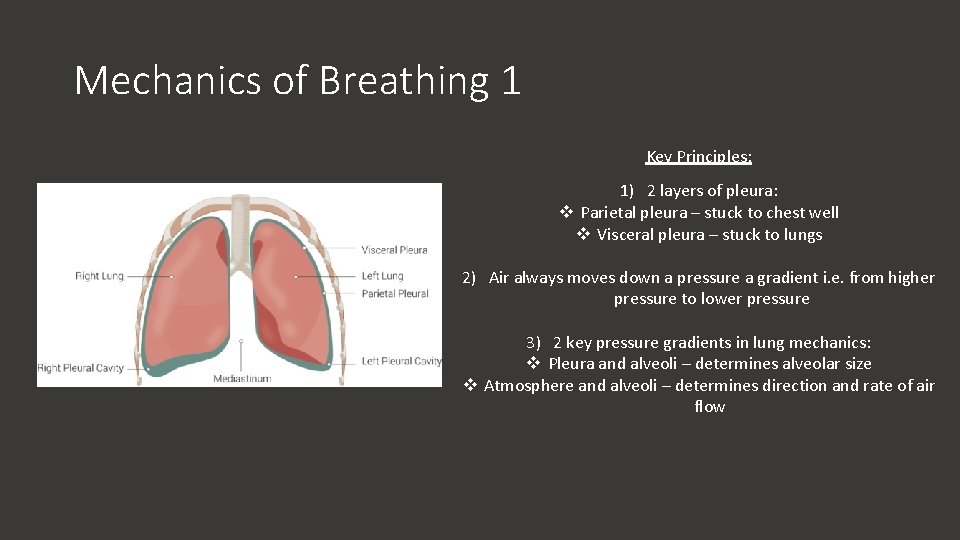
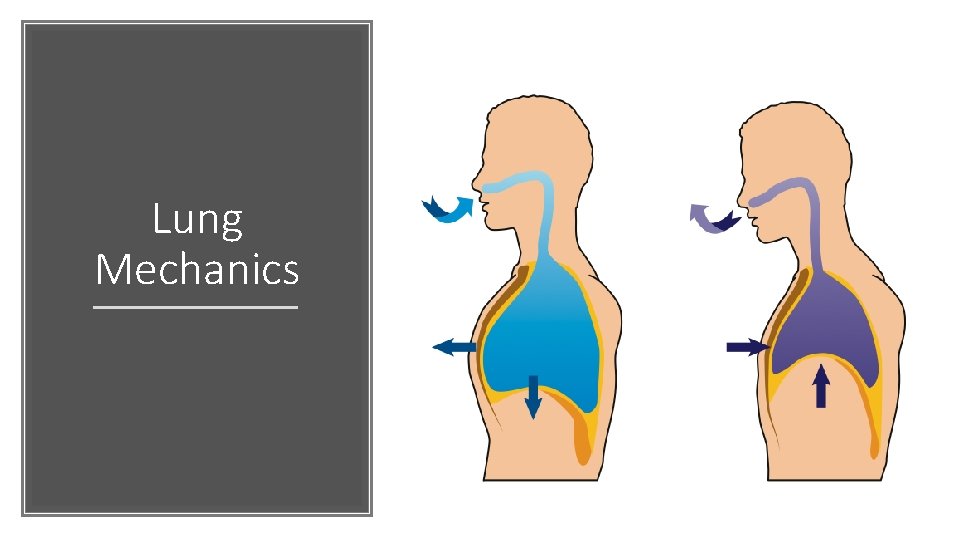
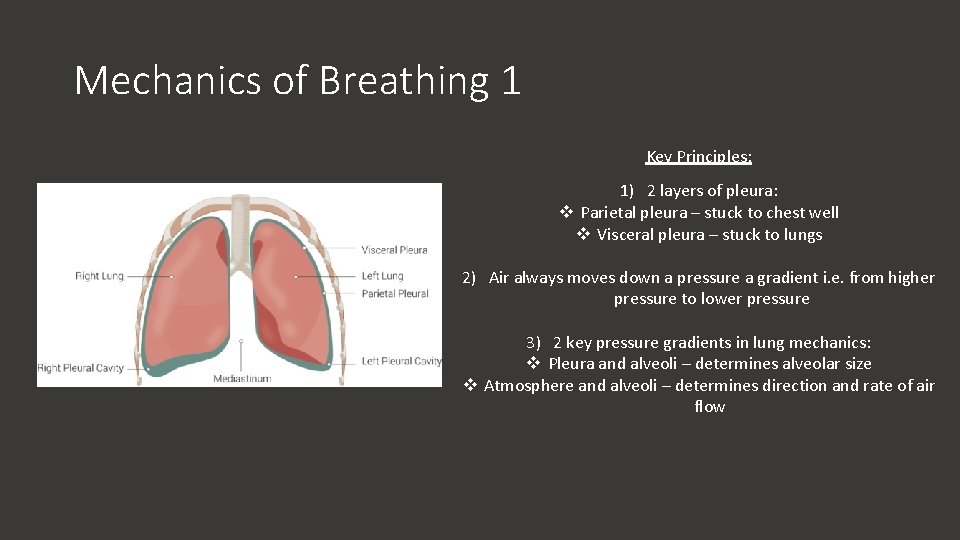
Mechanics of Breathing 1 Key Principles: 1) 2 layers of pleura: v Parietal pleura – stuck to chest well v Visceral pleura – stuck to lungs 2) Air always moves down a pressure a gradient i. e. from higher pressure to lower pressure 3) 2 key pressure gradients in lung mechanics: v Pleura and alveoli – determines alveolar size v Atmosphere and alveoli – determines direction and rate of air flow
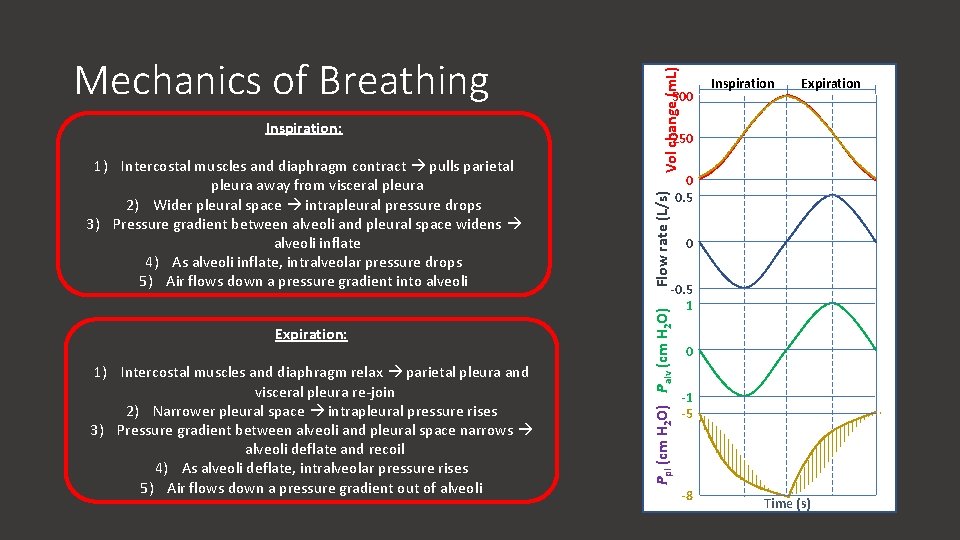
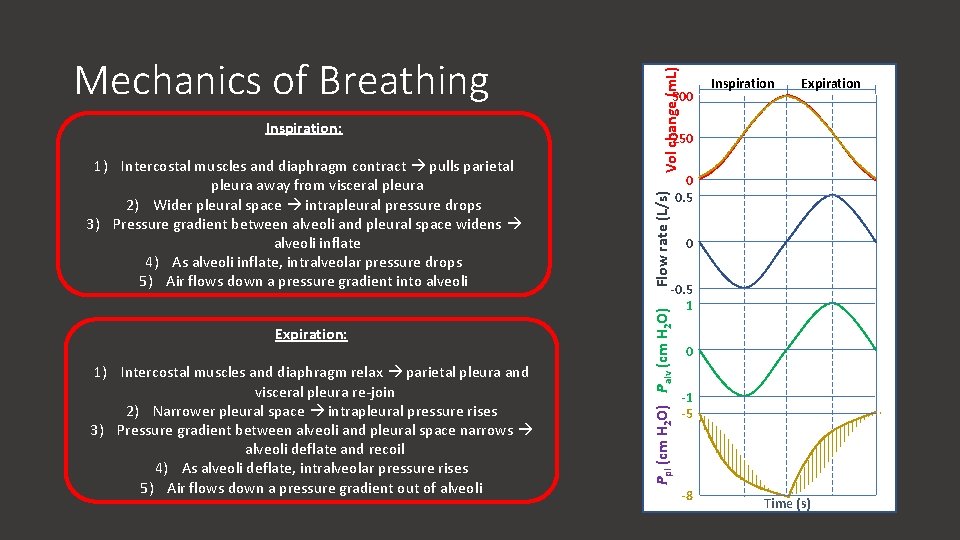
Expiration: 1) Intercostal muscles and diaphragm relax parietal pleura and visceral pleura re-join 2) Narrower pleural space intrapleural pressure rises 3) Pressure gradient between alveoli and pleural space narrows alveoli deflate and recoil 4) As alveoli deflate, intralveolar pressure rises 5) Air flows down a pressure gradient out of alveoli Vol change (m. L) 1) Intercostal muscles and diaphragm contract pulls parietal pleura away from visceral pleura 2) Wider pleural space intrapleural pressure drops 3) Pressure gradient between alveoli and pleural space widens alveoli inflate 4) As alveoli inflate, intralveolar pressure drops 5) Air flows down a pressure gradient into alveoli Inspiration Expiration 250 Flow rate (L/s) Inspiration: 500 0 0. 5 0 -0. 5 1 Ppl (cm H 2 O) Palv (cm H 2 O) Mechanics of Breathing 0 -1 -5 -8 Time (s)
ARQ 4 Assertion: Lung surfactant increases alveolar compliance Reason: Lung surfactant reduces alveolar surface tension a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
ARQ 4 Assertion: Lung surfactant increases alveolar compliance Reason: Lung surfactant reduces alveolar surface tension a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
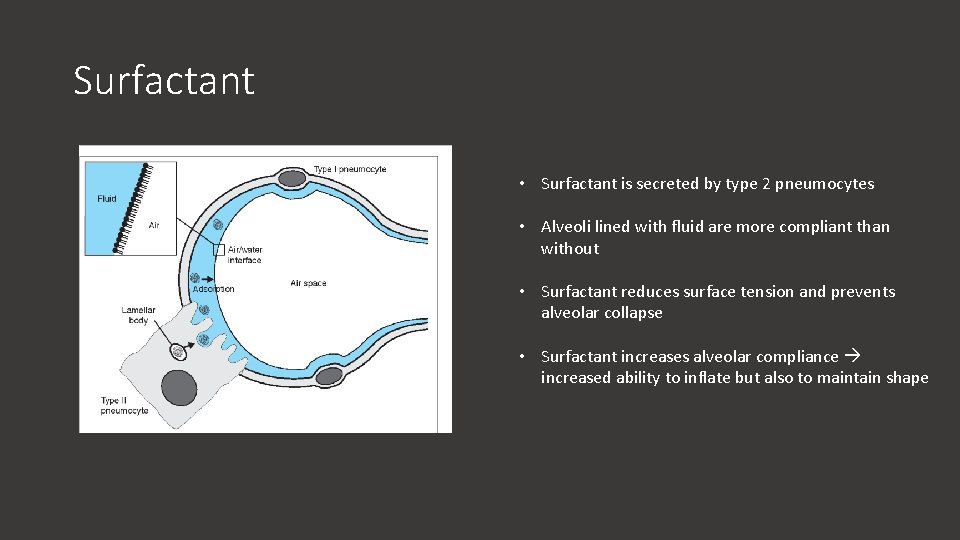
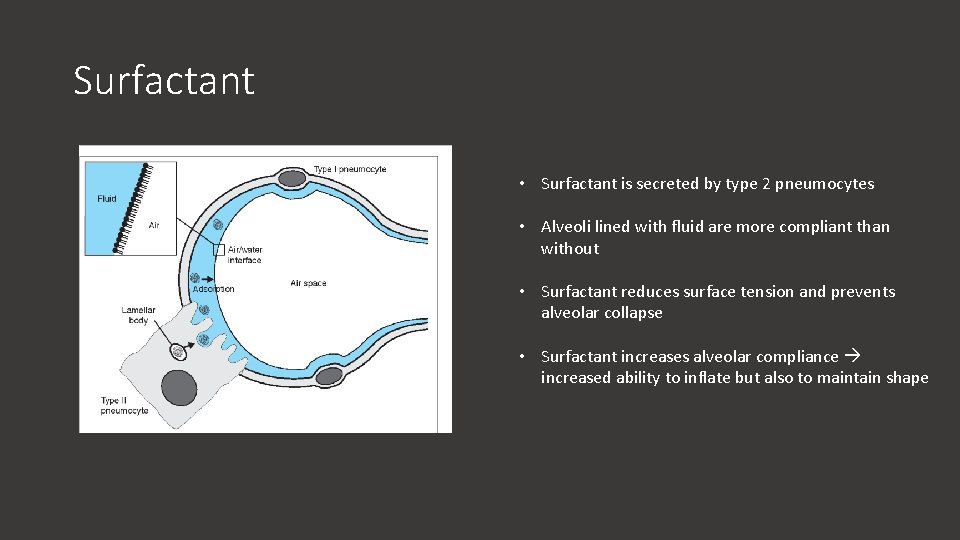
Surfactant • Surfactant is secreted by type 2 pneumocytes • Alveoli lined with fluid are more compliant than without • Surfactant reduces surface tension and prevents alveolar collapse • Surfactant increases alveolar compliance increased ability to inflate but also to maintain shape
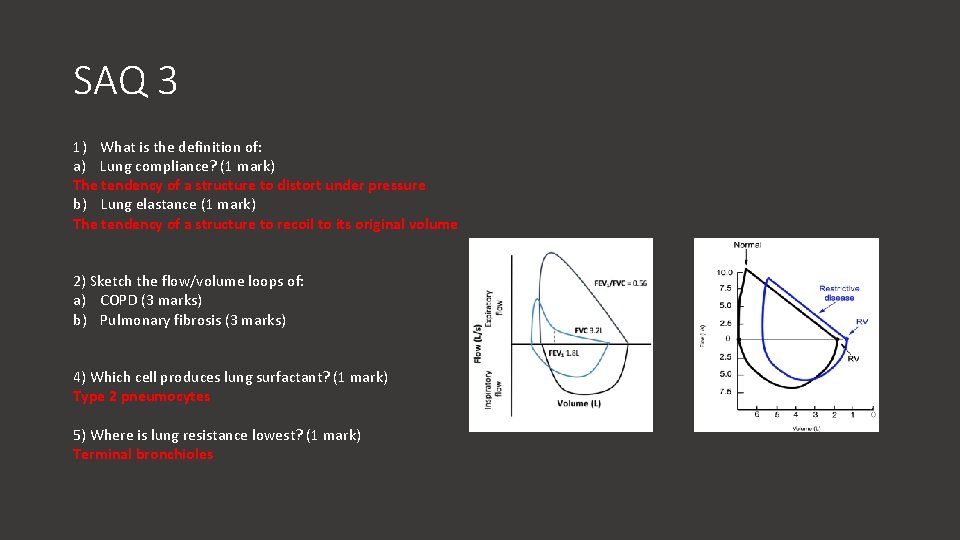
SAQ 3 1) What is the definition of: a) Lung compliance? (1 mark) b) Lung elastance (1 mark) 2) Sketch the flow/volume loops of: a) COPD (3 marks) b) Pulmonary fibrosis (3 marks) 4) Which cell produces lung surfactant? (1 mark) 5) Where is lung resistance lowest? (1 mark)
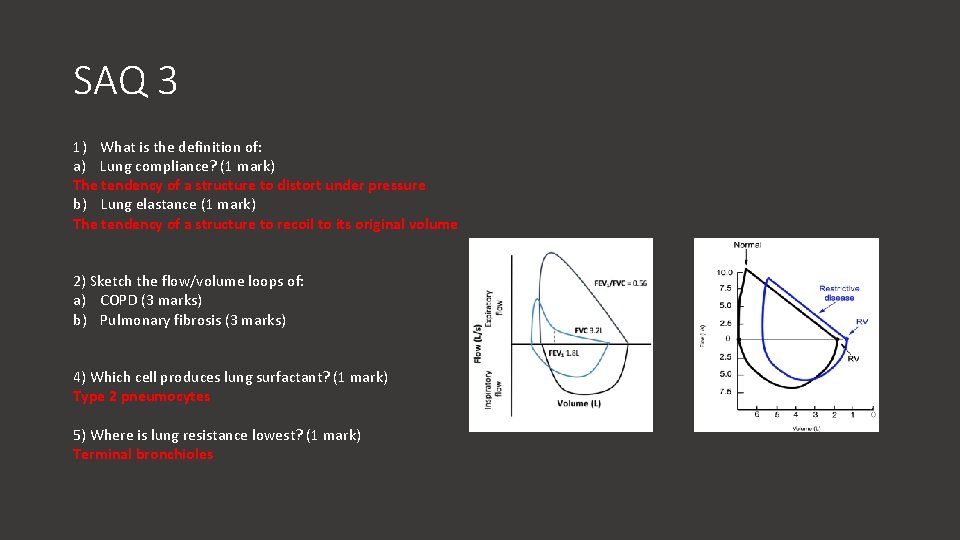
SAQ 3 1) What is the definition of: a) Lung compliance? (1 mark) The tendency of a structure to distort under pressure b) Lung elastance (1 mark) The tendency of a structure to recoil to its original volume 2) Sketch the flow/volume loops of: a) COPD (3 marks) b) Pulmonary fibrosis (3 marks) 4) Which cell produces lung surfactant? (1 mark) Type 2 pneumocytes 5) Where is lung resistance lowest? (1 mark) Terminal bronchioles
Control of Breathing (Awake)
Sofia Learning Outcomes 1 -LSS-RESP-CONT-01: Central control of breathing: explain the central organisation of breathing, and recall the principle inputs and outputs, including sensitivity to carbon dioxide and hypoxia
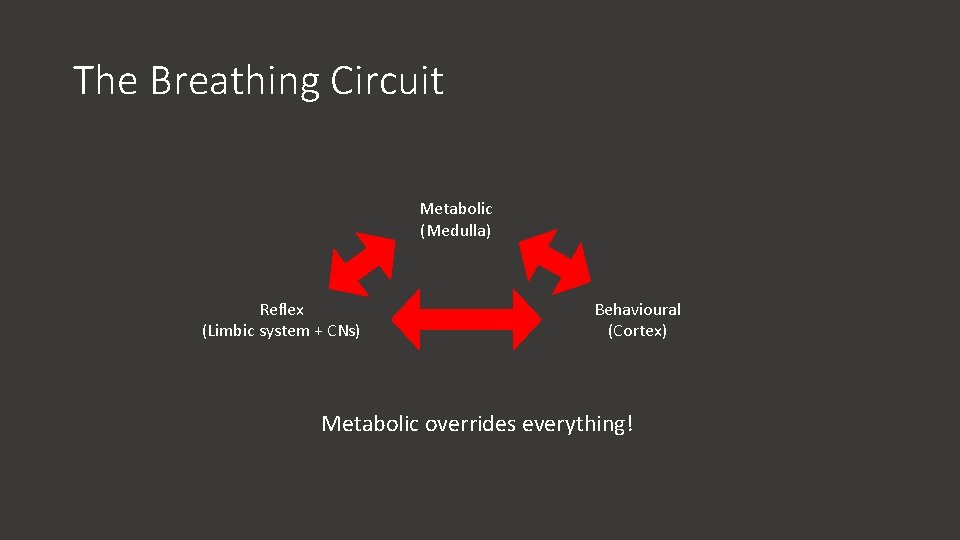
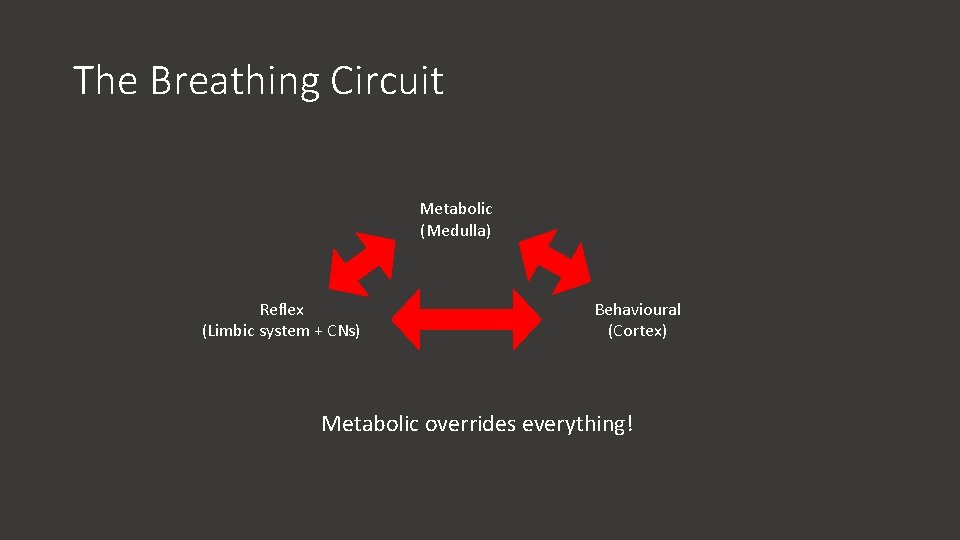
The Breathing Circuit Metabolic (Medulla) Reflex (Limbic system + CNs) Behavioural (Cortex) Metabolic overrides everything!
SBA 5 Which of these cranial nerves receives afferent fibres from the carotid body? a) Trigeminal nerve b) Facial nerve c) Glossopharyngeal nerve d) Vagus nerve e) Hypoglossal nerve
SBA 5 Which of these cranial nerves receives afferent fibres from the carotid body? a) Trigeminal nerve b) Facial nerve c) Glossopharyngeal nerve d) Vagus nerve e) Hypoglossal nerve
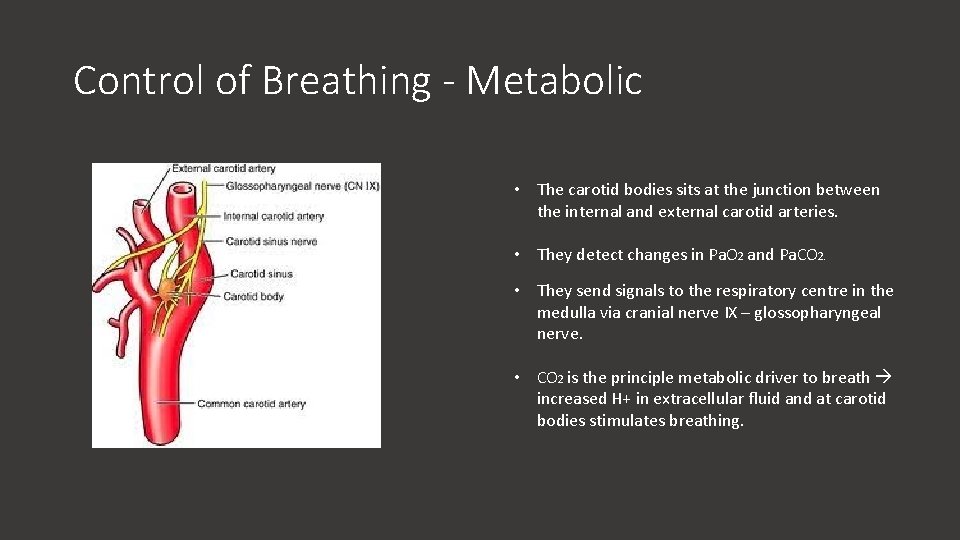
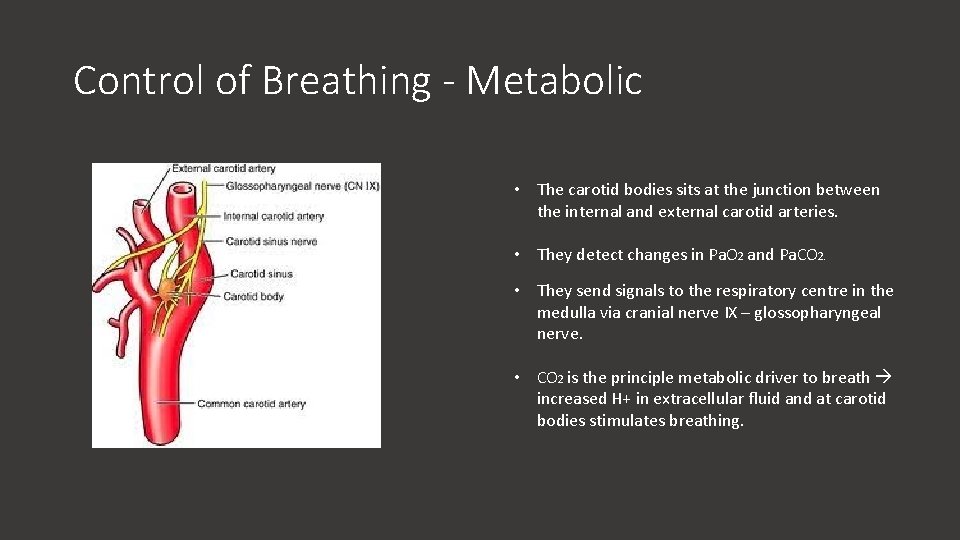
Control of Breathing - Metabolic • The carotid bodies sits at the junction between the internal and external carotid arteries. • They detect changes in Pa. O 2 and Pa. CO 2. • They send signals to the respiratory centre in the medulla via cranial nerve IX – glossopharyngeal nerve. • CO 2 is the principle metabolic driver to breath increased H+ in extracellular fluid and at carotid bodies stimulates breathing.
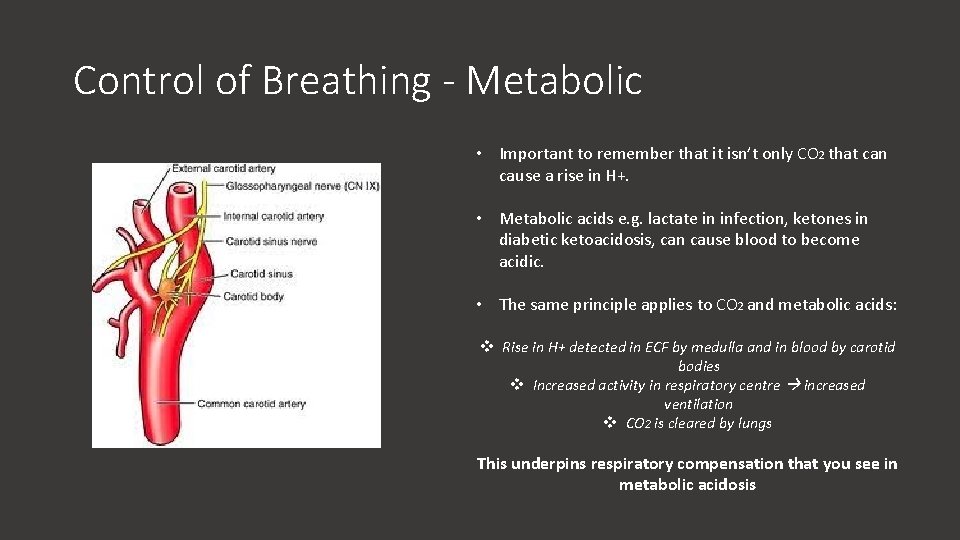
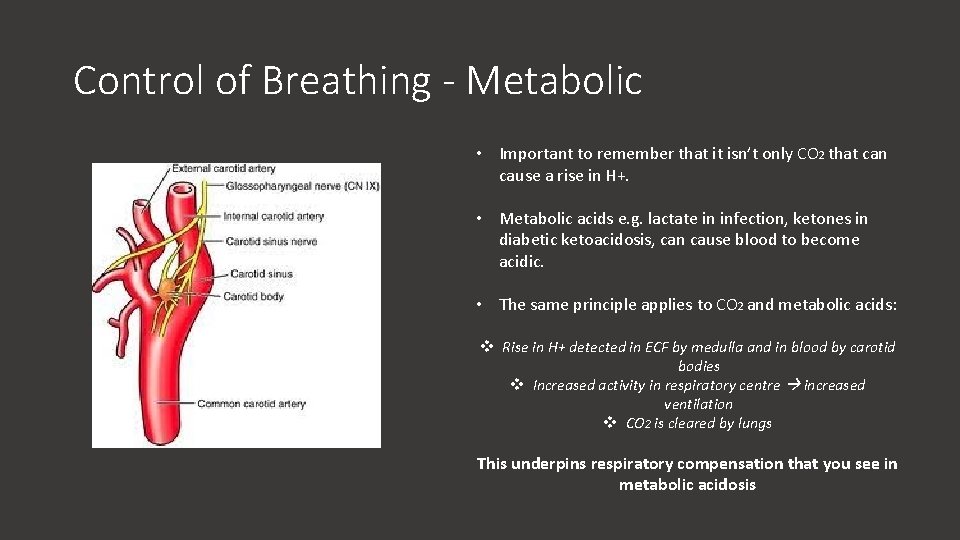
Control of Breathing - Metabolic • Important to remember that it isn’t only CO 2 that can cause a rise in H+. • Metabolic acids e. g. lactate in infection, ketones in diabetic ketoacidosis, can cause blood to become acidic. • The same principle applies to CO 2 and metabolic acids: v Rise in H+ detected in ECF by medulla and in blood by carotid bodies v Increased activity in respiratory centre increased ventilation v CO 2 is cleared by lungs This underpins respiratory compensation that you see in metabolic acidosis
ARQ 5 Assertion: Metabolic alkalosis may lead to hypoventilation Reason: A decrease in H+ stimulates renal excretion of bicarbonate a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
ARQ 5 Assertion: Metabolic alkalosis may lead to hypoventilation Reason: A decrease in H+ stimulates renal excretion of bicarbonate a) Assertion is true; reason is false b) Assertion is false; reason is false c) Assertion is false; reason is true d) Assertion is true; reason is true and is the correct explanation e) Assertion is true; reason is true but is not the correct explanation
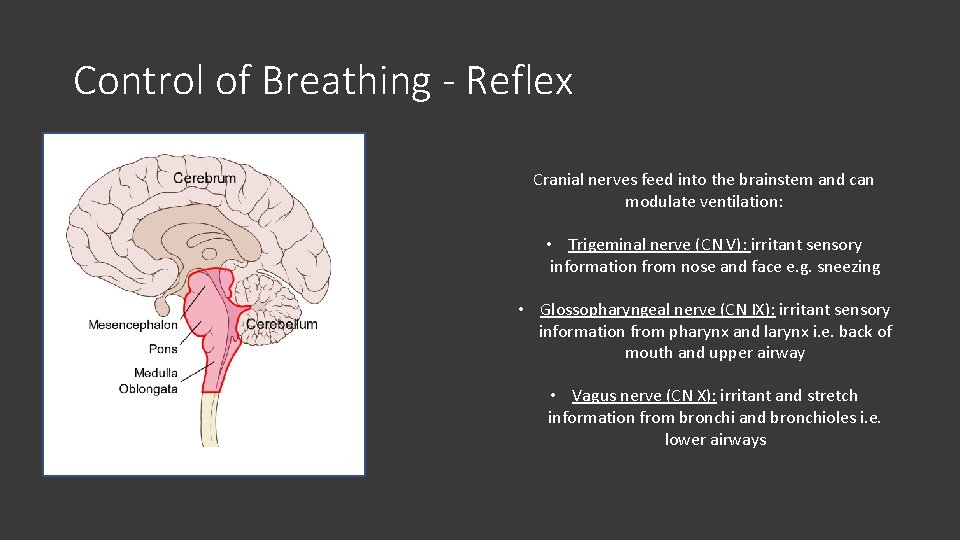
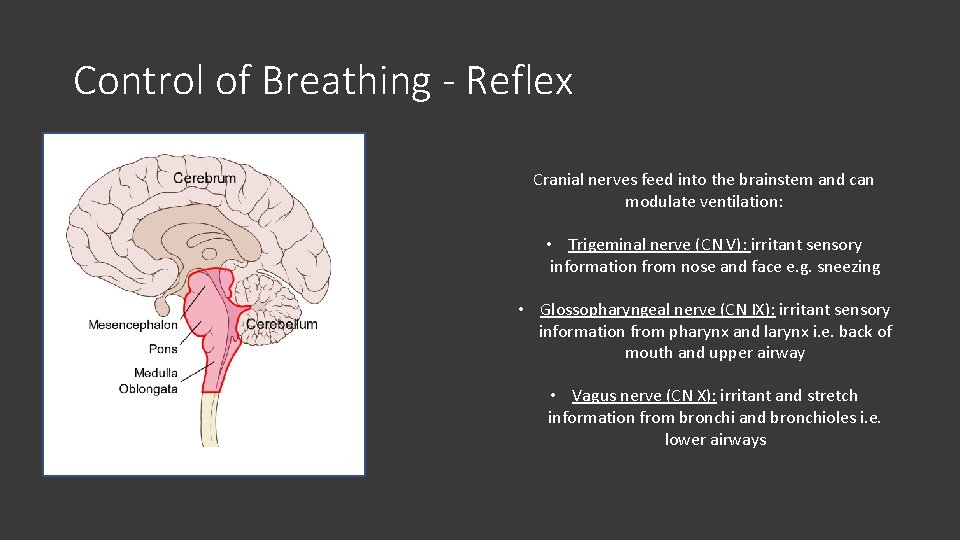
Control of Breathing - Reflex Cranial nerves feed into the brainstem and can modulate ventilation: • Trigeminal nerve (CN V): irritant sensory information from nose and face e. g. sneezing • Glossopharyngeal nerve (CN IX): irritant sensory information from pharynx and larynx i. e. back of mouth and upper airway • Vagus nerve (CN X): irritant and stretch information from bronchi and bronchioles i. e. lower airways
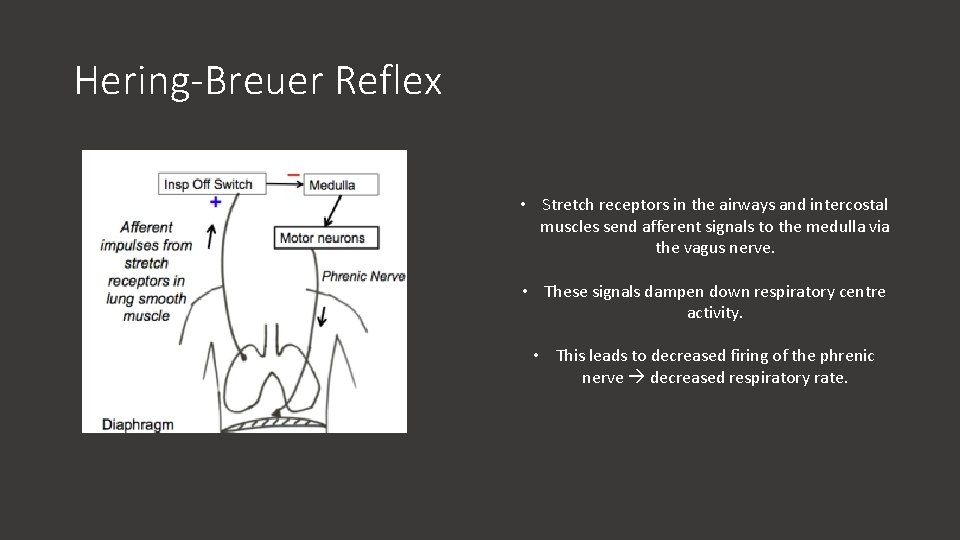
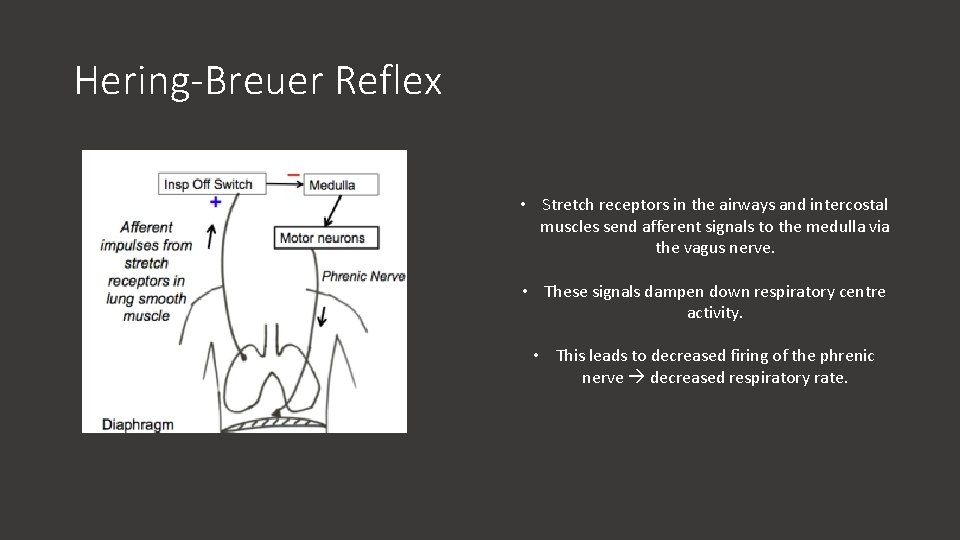
Hering-Breuer Reflex • Stretch receptors in the airways and intercostal muscles send afferent signals to the medulla via the vagus nerve. • These signals dampen down respiratory centre activity. • This leads to decreased firing of the phrenic nerve decreased respiratory rate.
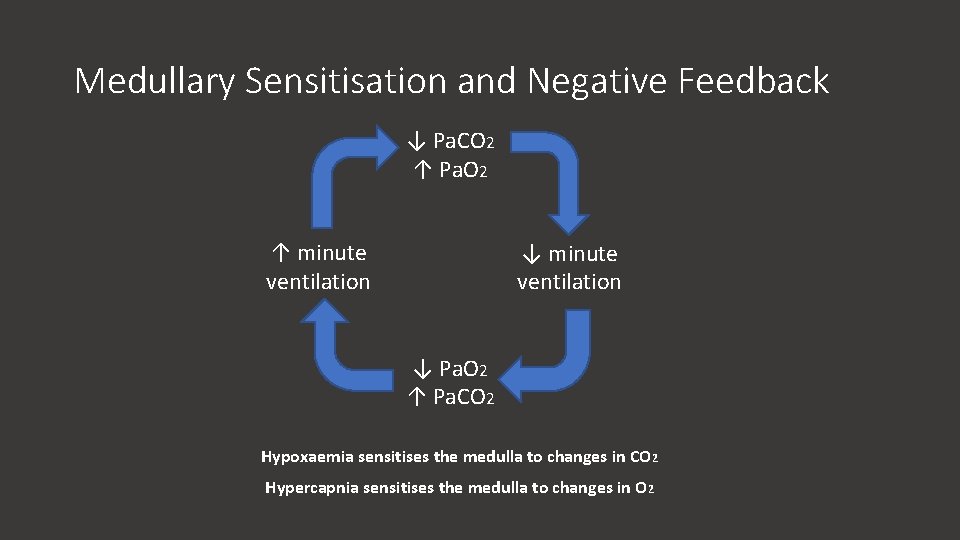
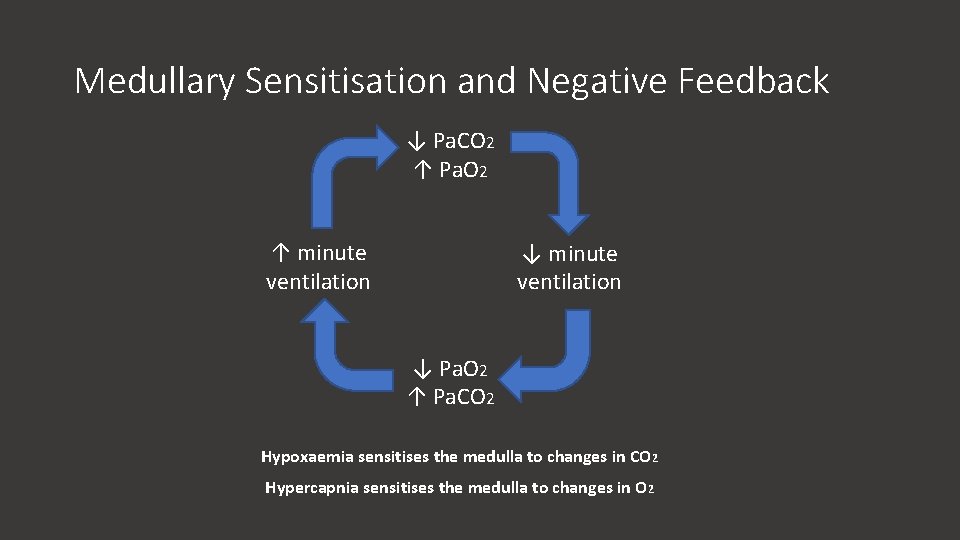
Medullary Sensitisation and Negative Feedback ↓ Pa. CO 2 ↑ Pa. O 2 ↑ minute ventilation ↓ Pa. O 2 ↑ Pa. CO 2 Hypoxaemia sensitises the medulla to changes in CO 2 Hypercapnia sensitises the medulla to changes in O 2
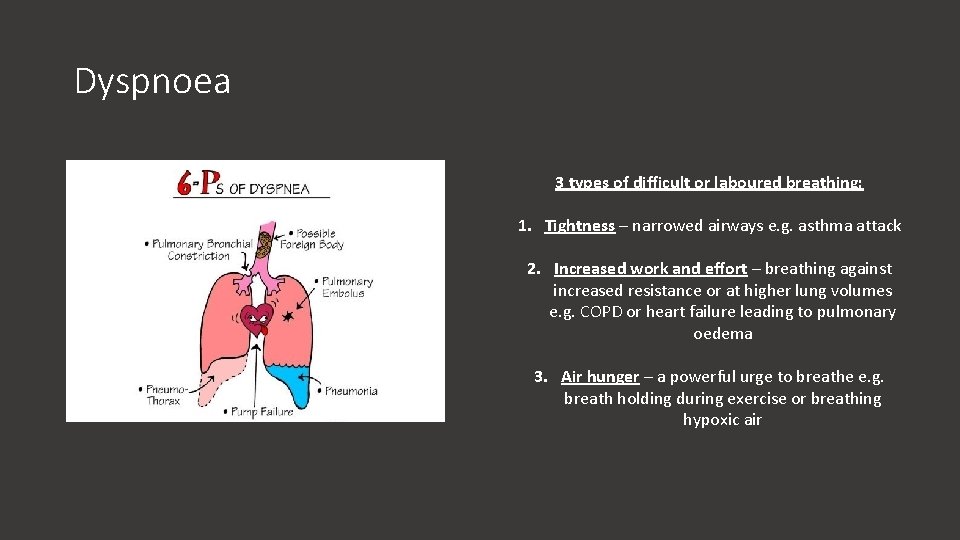
Dyspnoea 3 types of difficult or laboured breathing: 1. Tightness – narrowed airways e. g. asthma attack 2. Increased work and effort – breathing against increased resistance or at higher lung volumes e. g. COPD or heart failure leading to pulmonary oedema 3. Air hunger – a powerful urge to breathe e. g. breath holding during exercise or breathing hypoxic air
Thank You and Good Luck! Any Qs? : cmh 214@ic. ac. uk Feedback: bit. ly/muslimmedics