RESPIRATORY PHYSICAL ASSESSMENT AND PULMONARY TESTING BRUNNER STUDDARTHS
RESPIRATORY: PHYSICAL ASSESSMENT AND PULMONARY TESTING BRUNNER & STUDDARTH’S, 13 T H ED. CHAPTER 20
Management of Care (NCLEX-RN Test Plan §Initiate, evaluate, and update the plan of care and concept map §Assignment, Delegation and Supervision (LPN, VN, UAP, RNs) §Education to patients and staff §Advocacy for the patient’s rights and needs §Collaboration with Interdisciplinary team §Maintain patient confidentiality and privacy §Provide and receive hand off care report (e. g. use ISBAR) §Prioritize the delivery of care §Evaluate management outcomes

Review of Anatomy /Physiology Respiratory Assessment § Upper airway tract o nose, paranasal sinuses , tonsils, adenoids, pharynx § Lower respiratory tract o lungs, pleura, mediastinum o lobes, bronchioles o alveoli (Brunner p. 461 - 492) (Review the Glossary on page 463)
Ventilation/perfusion (V/Q) § Normal ventilation/perfusion § Low ventilation/perfusion (shunting) e. g. pneumonia, tumor, mucus plugs § High ventilation/perfusion (dead spaces) e. g. PE, cardiogenic shock § Absence of ventilation or perfusion (or limited) silent units – e. g. pneumothorax and severe acute respiratory distress syndrome (ARDs) § (Brunner p. 468 -470)
Airway Resistance Causes Alteration of the diameter of bronchioles, due to: §Contraction of bronchial smooth muscles (asthma) § Thickening of mucosa (chronic bronchitis) § Airway Resistance – determined by the radius §Obstruction of airway (tumor, mucus) §Loss of lung elasticity (emphysema) § Compliance - lungs losing elastic recoil and overdistention
Lung Volume and Lung Capacity § Tidal Volume (TV) (500 -1000 ml) – volume of inhaled and exhaled air per breath § Residual Volume (RV) (1, 200 ml) – volume of air in the lungs after max exhalation (increased with obstructive diseases) § Total Lung Capacity (TLC) (5, 800 ml) – Vol of air in the lungs after max inspiration (decreased with restrictive lung disease such as atelectasis and pneumonia, and increased in COPD) (Brunner, Table 20 -1 p. 468)
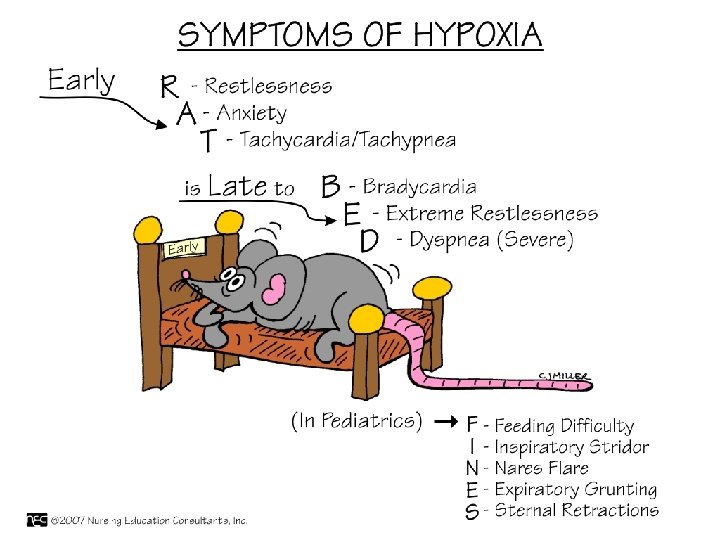
Hypoxia and Hypoxemia Hypoxia: § Inadequate cellular oxygenation (less O 2 to tissues) due to decrease blood supply § Cause: hypoventilation, ventilation-perfusion § Ventilation/perfusion problem – PE § Respiratory problem resulting in decrease in arterial oxygen § Results: Ischemia Hypoxemia: § Deficiency in the concentration of oxygen in arterial blood. § Symptoms include: cyanosis, restlessness, tachycardia
Symptoms of hypoxia § Changes in mental status § Restlessness § Anxiety § Agitation § Decreased LOC Physical signs of hypoxia § Tachycardia § Tachypnea § Dysrhythmias § Dyspnea § Cyanosis
Assessment: Acutely Ill Patient §Compare present findings with previous! §Requires expertise in physical assessment techniques §Analysis of findings: Labs, diagnostic results §Positioning of the patient o Head of bed up o LOC – agitation, restlessness §Vital signs – note changes
History Past Medical History § Childhood; infectious diseases; genetic considerations ex : alpha 1 antitrypsin deficiency § Immunizations (pneumonia or flu vaccines) § Major illnesses and hospitalizations § Medications; allergies § Family, health, and psychosocial history Psychosocial History § Occupation; geographic location; work and living environment § Habits: Smoking; alcohol; drugs; exercise; nutrition
Gerontological Changes and Oxygenation § Weakening of respiratory muscles and reduction in alveoli surface areas § Reduced ventilation and respiratory gas exchange § Decreased function of the cilia § Chest wall compliance is reduced – o increased chest rigidity, increased RR, decreased Pa. O 2
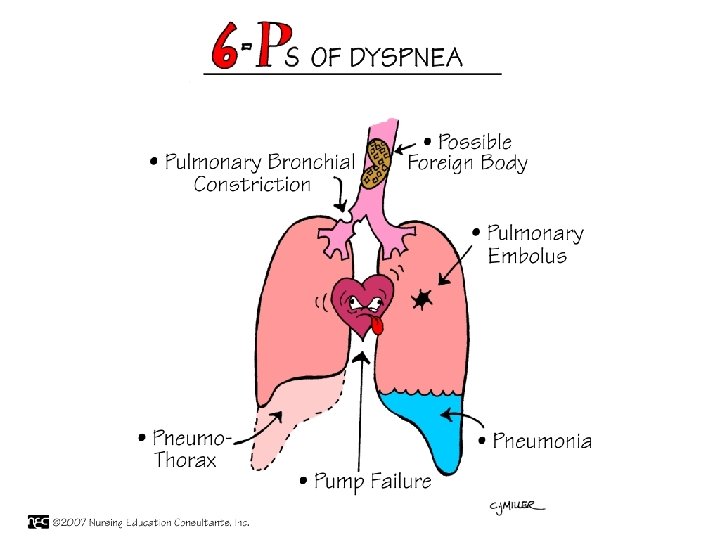

Dyspnea: Classifying § Acute versus chronic § Exertional § § More common for cardiac Activity tolerance § Orthopnea § § § Difficulty breathing unless sitting up Number of pillows Increasing severity of disease from exertional § Paroxysmal Nocturnal § § Asthma – Usually accompanied by coughing at nights Flash pulmonary edema

Dyspnea Document dyspnea according to Grade 1 - SOB with exertion Grade 2 - SOB while walking a short distance Grade 3 - SOB with mild daily activity Grade 4 - SOB at rest Grade 5 - Orthopnea (Grade 5 is the worse) What diagnoses will cause dyspnea?
Physical Assessment ◦ Inspection, palpation, percussion and auscultation ◦ Compare one side with the other § Use landmarks of anterior, lateral and posterior thorax § Brunner and ANGEL videos for sequence of palpation, tactile fremitus, percussion, etc. § Note respiratory excursion demo

Inspection § § § § § Rate Pattern of breathing Shallow Gasping Grunting Nasal flaring Accessory muscle use Altered patterns Skin color

Respiratory Effort Three basic levels 1. Increased work of breathing § Noticeable respiratory effort § No accessory muscle use § Mild dyspnea § Rate 22 - 26 2. Moderate dyspnea § Increased effort with mild accessory muscle use § Rate 28 – 34 3. Severe dyspnea § Multiple accessory muscle use § Rate high 30 s – 40 s

Palpation § From trachea down the chest wall § Tactile fremitus -Pt states “ 99” and vibrations felt on ulnar surfaces or fingers if there is an increase in solid tissue or consolidation as in pneumonia § Thoracic excursion – both hands at T 9 -T 10, pinch small skin fold between thumbs. Observe for symmetry and flattening of skin fold with deep expiration. (Brunner p. 500 -502)
Percussion § Resonant – low pitched, hollow over normal lung, chronic bronchitis § Hyperresonant – louder, lower pitched due to increased air, e. g. emphysema § Dull sounds – thud like, heard over dense tissue (tumor or consolidation) § Flat notes – soft and high pitched heard over airless tissue (bone) § Tympanic – loud, drum-like heard over a large air filled e. g. puffed out cheek or large pneumothorax
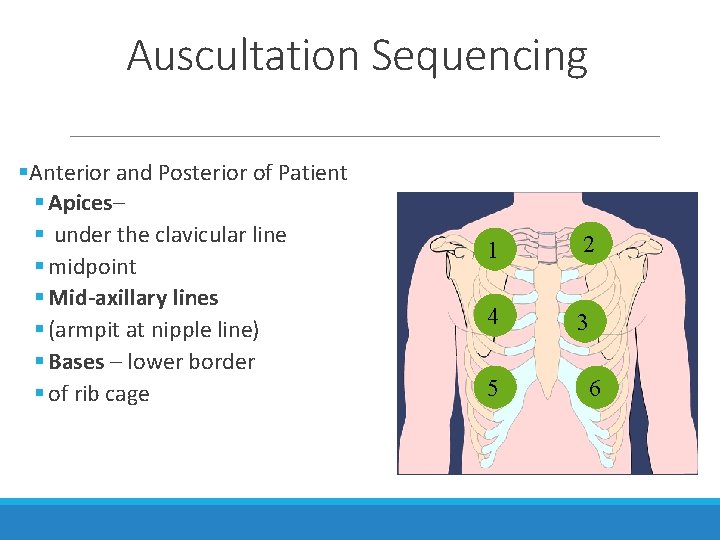
Auscultation Sequencing §Anterior and Posterior of Patient § Apices– § under the clavicular line § midpoint § Mid-axillary lines § (armpit at nipple line) § Bases – lower border § of rib cage 1 2 4 3 5 6
Auscultation § Note: Stethoscope over firmly against bare skin as the patient breathes slowly and deeply through the nose with pursed lips The nurse assesses for § Normal breath sounds § Adventitious breath sounds § Voice sounds

Auscultation §Normal Breath Sounds § Tracheal- over trachea (Inspiratory/Expiratory sounds are equal) § Bronchovesicular- over 1 st and 2 nd interspaces anteriorly and between the scapulae (I/E are equal) § Vesicular – heard over the thorax, lower pitched and softer than bronchial breathing (inspiratory BS 2 -3 times the length of expiratory) § Bronchial- over the manubrium (Expiratory sounds longer) §(NOTE: Listen to normal and abnormal breath sounds in Respiratory) §Brunner Table 20 -5 , p. 481

Auscultation § Adventitious/Abnornal Breath Sounds § Crackles (Rales) Fine crackles caused by sudden opening of airways filled with fluid (interstitial edema in and around the alveoli); begins at the end of inspiration Coarse crackles (Rhonchi) § Course/harsh crackles caused by exudate moving in large airways § Clears with coughing or suctioning

Auscultation Adventitious/Abnornal Breath Sounds § Wheezes § Sibilant - high pitched, musical from constriction/inflammation of smaller airways, eg. Asthma exacerbation § Pleural friction rub § (sounds like hand sliding over wet balloon) § Result of pleural inflammation § Creaking, grating sound § Audible on inspiration and expiration § Click on the link below or copy and paste to hear all the breath sounds lung sounds http: //www. easyauscultation. com/cases-listing-
Voice Sounds Bronchophony: §Vocal resonance more clearer or intense than normal, e. g. have pt repeat “ 99” and it sounds clearer than normal due to consolidation, atelectasis Egophony: §Voice sounds that are distorted – the distortion caused by consolidation transforms the sound into a clear “A” instead of “E” §E. g. in pneumonia or pleural effusion

Assessment Findings in Common Respiratory Disorders Disorder Tactile Fremitus Percussion Auscutation Pneumonia (consolidation) Increased Dull Bronchial breath sounds, crackles, bronchospasm egophony Emphysema Decreased Hyperresonant Absent/decreased BS crackles, wheezes or rhonchi Bronchitis Normal Resonant Normal/decreased BS, coarse crackles, rhonchi or wheezes Asthma Decreased Resonant to hyperresonant Wheezes, crackles Atelectases Absent Dull Decreased/absent BS, may be increased in Rt. Upper lobe atelectasis
Nursing Diagnoses: Respiratory Deviations § Risk for impaired gas exchange § Risk for aspiration § Ineffective airway clearance § Risk for ineffective management of therapeutic regimen §Ineffective breathing pattern §Knowledge deficit §Ineffective individual coping §Activity intolerance §Altered nutrition: less than body requirements
Capnography Used to monitor for the presence of CO 2 § Noninvasive method to determine carbon dioxide levels § Commonly used in critical care and procedural areas § Color changes from purple to yellow § Used to check endotracheal tube or gastric tube placement
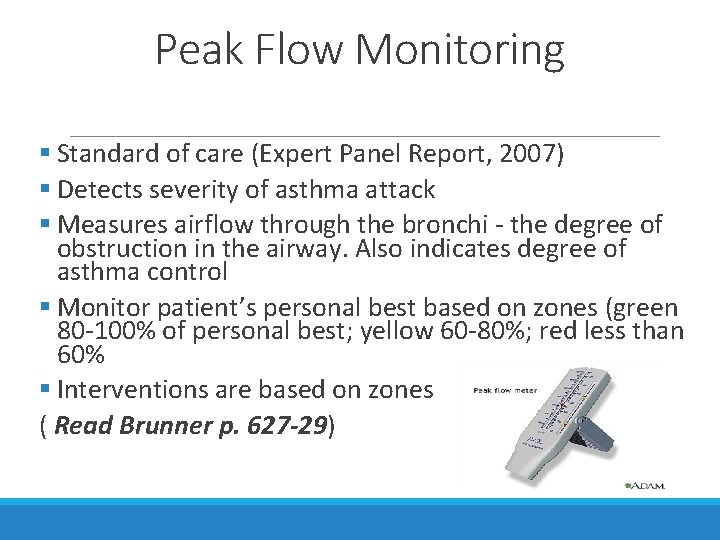
Peak Flow Monitoring § Standard of care (Expert Panel Report, 2007) § Detects severity of asthma attack § Measures airflow through the bronchi - the degree of obstruction in the airway. Also indicates degree of asthma control § Monitor patient’s personal best based on zones (green 80 -100% of personal best; yellow 60 -80%; red less than 60% § Interventions are based on zones ( Read Brunner p. 627 -29)

Peak Flow § Less than 300 indicates marked obstruction! § The indicator is set at zero before the patient blows into the device. § Best of 3 rapid forceful blows § Largest/highest of the two or three readings is considered the peak flow § Why patients monitor peak flow after taking medications?
Why Measure Pulmonary Function? § Perioperative evaluation before thoracic surgery § Evaluate response to bronchodilator therapy. May be done pre/post medication. § Routinely used to differentiate restrictive lung diseases (pneumonitis or sarcoidosis) from obstructive lung disorders (COPD) § Evaluate lung function for patients with allergies
Sputum Culture and Sensitivity (C&S) § Determine the presence and type of bacteria for antibiotic therapy § Collect sputum before antibiotic therapy started. Test effectiveness of therapy § Collect the specimen in a sterile container § Morning specimen preferred; best before eating and drinking
Sputum Studies: Microbiology §Gram Stain- what type of organism, needed to make diagnosis §Culture - identifies specific organism §Sensitivity- Identifies which antibiotics are most resistant or sensitive to the organism, assist in correct treatment §AFB or Acid Fast Bacilli- present in sputum cultures with TB §Cytology- detects cells shed by tumor
Bronchoscopy § Done with sedation § Signed consent needed § NPO 4 -6 hrs prior to procedure – prevent aspiration § Numbing solution sprayed in throat to prevent gag reflex § Post procedure standard care § Keep NPO until cough/gag reflex returns § Monitor VS, O 2 saturation level § Auscultate lungs bilaterally § Monitor for bleeding § Nursing Diagnoses: Risk for pneumothorax, perforation, aspiration, or hypoxemia
Bronchoscopy § Diagnosis of bronchogenic cancer and lung disease (TB, PCP Pneumonia, etc. ) § Visual exam helps determine abnormal structures, obstructions caused by abnormal tissue, foreign bodies, and allows for biopsy of structure § Allows direct visualization of trachea and bronchial tree (Click on the link to watch this video) bronchoscopy video
Thoracentesis § Contraindication: significant thrombocytopenia § Complications: Pneumothorax due to puncture of visceral pleura or air into pleural space § § § Interpleural bleeding due to punctured blood vessel Mediastinal shift- due to rapid fluid loss Labored breathing Cardiac arrhythmia Pulmonary edema § (Brunner, p. 489 Chart 20 -11 § Understand Nursing Care: Assisting the client undergoing thoracentesis – interventions and rationale
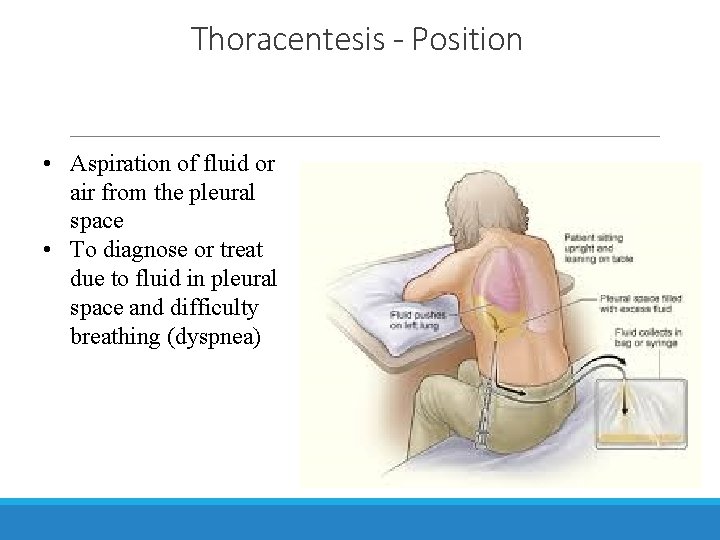
Thoracentesis - Position • Aspiration of fluid or air from the pleural space • To diagnose or treat due to fluid in pleural space and difficulty breathing (dyspnea)
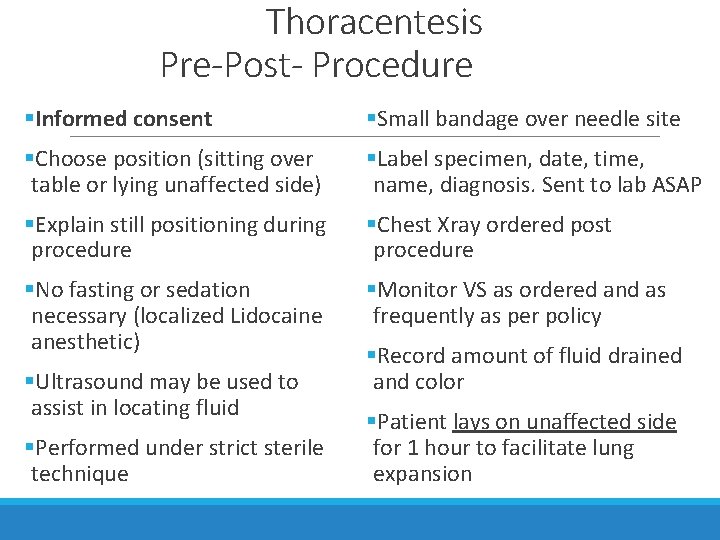
Thoracentesis Pre-Post- Procedure §Informed consent §Small bandage over needle site §Choose position (sitting over table or lying unaffected side) §Label specimen, date, time, name, diagnosis. Sent to lab ASAP §Explain still positioning during procedure §Chest Xray ordered post procedure §No fasting or sedation necessary (localized Lidocaine anesthetic) §Monitor VS as ordered and as frequently as per policy §Ultrasound may be used to assist in locating fluid §Performed under strict sterile technique §Record amount of fluid drained and color §Patient lays on unaffected side for 1 hour to facilitate lung expansion
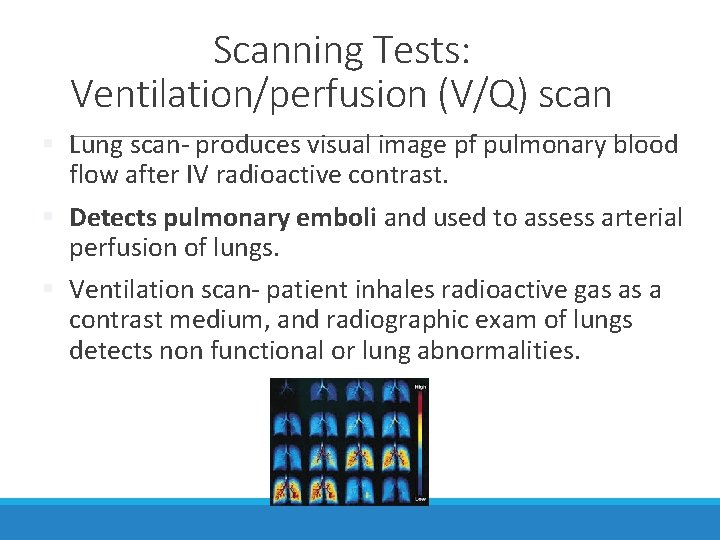
Scanning Tests: Ventilation/perfusion (V/Q) scan § Lung scan- produces visual image pf pulmonary blood flow after IV radioactive contrast. § Detects pulmonary emboli and used to assess arterial perfusion of lungs. § Ventilation scan- patient inhales radioactive gas as a contrast medium, and radiographic exam of lungs detects non functional or lung abnormalities.
Pulmonary Angiogram Invasive procedure – visualization of thromboembolic lung disease, e. g. pulmonary emboli Informed consent Dye injected into lung tissue thru catheter (jugular, subclavian, femoral vein) to visualize pulmonary vessels clot or embolus Pre- and Post-op: NPO; anticoagulation status, allergies to shellfish or iodine noted; assess for warm flushing sensation or chest pain during injection of dye Post-procedure care – VS, bleeding and hematoma, O 2 Sats, and assess neurovascular status (pulse, temp, edema, etc. )

Vignette/Case Study #1 66 y. o man presented to the primary care provider c/o h/a, fever, and cough for the past 3 days, and recent bouts of confusion History and Physical Exam: Vital Signs: T 100. 8°F, HR 110 beats/min; RR 28 breaths/min 1) What history questions would you ask the patient? 2) What additional physical assessments would you perform? Labs: WBC 20, 000 per mm 3; blood glucose 180 mg/d. L 3) What diagnostic procedures do you anticipate will be ordered?

Vignette #2 – Respiratory Depression A 24 y. o. male patient was admitted to the surgical unit after a successful repair of an inguinal hernia. He is 5 feet 10 inches tall; weighs 120 kg; neck circumference 21 inches. The pt has a morphine PCA; NKDA noted. VS: BP 122/70, RR 26, HR 88, and temp 98. 6°F. Patient c/o incision pain 7 of 10; family visiting. Nurse administers a bolus dose of morphine. Fifteen minutes after administering the pain medication, a family member enters the hallway and yells, “We need help in here! John is not breathing. ” The nurse finds the pt with periods of apnea lasting a few seconds followed by a short snorting gasp with RR 12 breaths per minute. His lips and nail beds are bluish. The patient is lying supine in the bed, awakens as the nurse enters, but is very lethargic and somnolent.

Vignette/Case Study #2 1. Which nursing assessment should be performed first? 2. Which nursing interventions must be provided immediately? 3. Explain the possible reasons for the patient’s sudden decline in the respiratory status.
Vignette/Case Study #3 - Bronchoscopy 2. Mr. Williams, a 72 -year-old man, is scheduled for a bronchoscopy, due to changes noted on a recent chest x-ray. A retired factory worker, Mr. Williams recently was notified that the buildings that he had worked in for over 25 years were destroyed due to asbestos. Additionally, the number of employees from this company with respiratory diseases or allergies is significantly above the national averages.

Answer 2 a. What is the rationale for the bronchoscopy in Mr. Williams? The bronchoscopy was ordered to determine the location and extent of the pathologic process seen on the chest x-ray, and to obtain a tissue sample for analysis and diagnosis. 2 b. List pre-procedure nursing interventions. Explain the procedure to the patient. Obtain informed consent prior to administration of any sedatives or narcotics. Ensure that patient is NPO status for at least 4 to 8 hours prior to the procedure. Ensure the patient removes dentures or any other oral prosthetics. Administer premedications as ordered.
2 c. What is the rationale for the administration of atropine and a sedative preprocedure? This medication inhibits vagal stimulation that protects the patient against bradycardia, dysrhythmias, and hypotension during the procedure. Atropine also suppresses the cough reflex, sedates the patient, and relieves anxiety. 2 d. For what postprocedure complications should the nurse assess Mr. Williams? Hypoxia Hypotension Tachycardia Hemoptysis Dyspnea Dysrhythmias
Question The nurse doing rounds at the beginning of a shift notices a sputum specimen in a container sitting on the bedside table in a patient's room. The nurse asks the patient when he produced the sputum specimen and he states that the specimen is about 4 hours old. What action should the nurse take? a) Immediately take the sputum specimen to the laboratory. b) Discard the specimen and assist the patient in obtaining another specimen. c) Refrigerate the sputum specimen and submit it once it is chilled. d) Add a small amount of normal saline to moisten the specimen.
Question NCLEX: Stress and Adaptation A patient has been placed on a ventilator, and the spouse is visiting for the first time. The spouse begins to cry. The best statement by the nurse is a) "If this upsets you, it may be better to not visit. ” b) "Tell me what you are feeling. ” c) "He is going to get better” d) "I know what you are going through. "
Question A patient has just undergone bronchoscopy. Which nursing assessment is most important at this time? a) Level of consciousness (LOC) b) Memory c) Personality changes d) Intellectual ability
Question The nurse at the clinic asks the patient about what brought him in to see the physician today. What is the purpose of asking the client about his primary health concern? a) To discover what the patient perceives as the health problem that needs treatment b) To triage the patient and determine if he really need to see the physician today c) To determine if the insurance company will pay for the visit d) To see if a prescription can be called in without having to see the physician
Question Normal vesicular breath sounds would be heard best over the: a) Lung fields b) Trachea c) Right and Left main bronchi d) Posterior area in between the scapula
Question A patient with an altered respiratory status is restless and slightly disoriented. A priority nursing action at this time would be to: a) b) c) d) Obtain a complete set of vital signs Evaluate a pulse oximetry reading Assess whether the patient is in pain Administer the ordered sedative
Question The nurse is completing a patient's health history with regard to potential risk factors for lung disease. What interview question addresses the most significant risk factor for respiratory diseases? a)“Have you ever been employed in a factory, smelter, or mill? ” b)“Does anyone in your family have any form of lung disease? ” c)“Do you currently smoke, or have you ever smoked? ” d)“Have you ever lived in an area that has high levels of air pollution? ”
Question The nurse is taking a respiratory history for a patient who has come into the clinic with a chronic cough. Which of following information should the nurse obtain from this patient? (Select all that apply. ) a) Financial ability to pay the bill b) Social support c) Previous history of lung disease in the patient or family d) Occupational and environmental influences e) Previous history of smoking
- Slides: 55