Respiratory illness in children Assessment and management of

- Slides: 27
Respiratory illness in children Assessment and management of acute episodes Jeremy Hull, CHOX Oxford Children’s Hospital
What are acute episodes? • Breathlessness • Cough • Noisy breathing Oxford Children’s Hospital
What are the likely causes? • • Asthma Croup Bronchiolitis Pneumonia • • • Pertussis Inhaled foreign body Anaphylaxis Pneumothorax Not respiratory – sepsis – diabetic ketoacidosis – heart failure likely rare Oxford Children’s Hospital
Assessment • History! – – – – previously well, or previous episodes coryza onset of symptoms – sudden, gradual, precipitant any history of choking eating and drinking exercise / general activity levels usual medication Oxford Children’s Hospital
Assessment • Examination – – – – – Global assessment – well or ill? ABC Conscious level Respiratory rate – COUNT don’t guess Heart rate Work of breathing – recession plus use of accessory muscles Oxygen saturation – use paediatric probe for < 2 yrs Breathing noises – stridor or audible wheeze Auscultate – wheeze and/or crackles Oxford Children’s Hospital
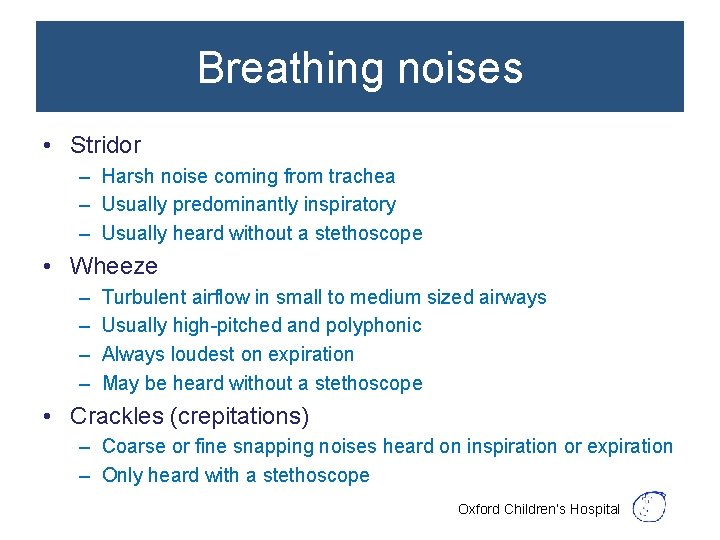
Breathing noises • Stridor – Harsh noise coming from trachea – Usually predominantly inspiratory – Usually heard without a stethoscope • Wheeze – – Turbulent airflow in small to medium sized airways Usually high-pitched and polyphonic Always loudest on expiration May be heard without a stethoscope • Crackles (crepitations) – Coarse or fine snapping noises heard on inspiration or expiration – Only heard with a stethoscope Oxford Children’s Hospital
Heart rate and respiratory rate • Heart rate – Will change with distress and anxiety – Higher in febrile children – Varies with age • Respiratory rate – May be the only abnormal sign – Varies with age Oxford Children’s Hospital
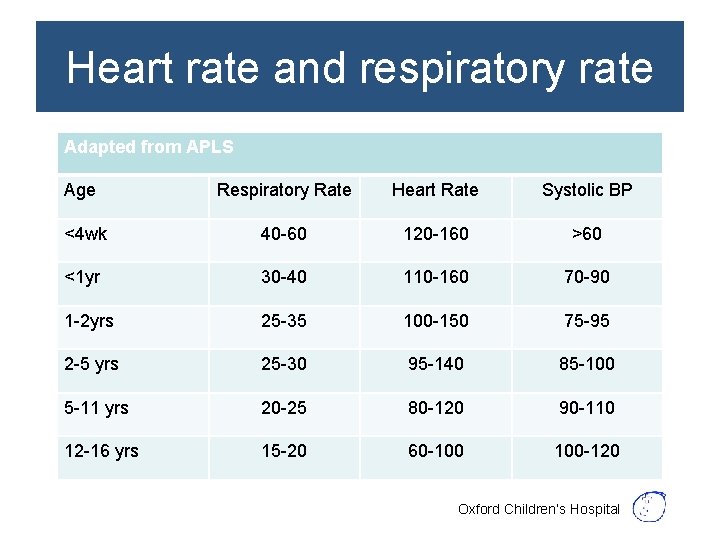
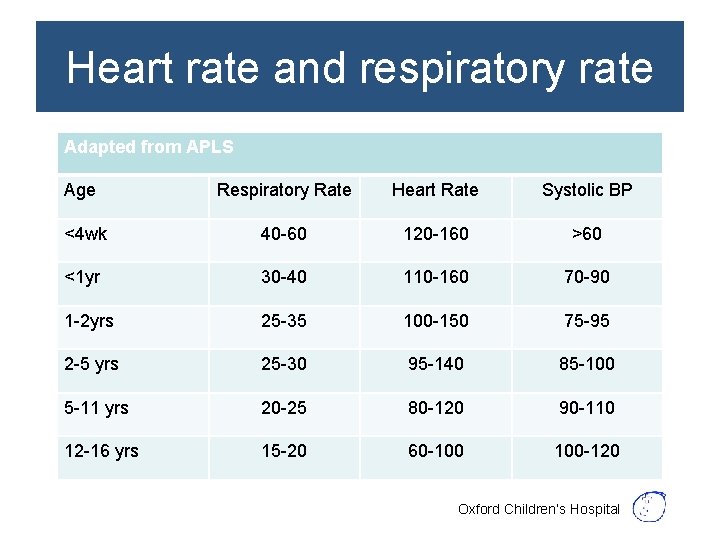
Heart rate and respiratory rate Adapted from APLS Age Respiratory Rate Heart Rate Systolic BP <4 wk 40 -60 120 -160 >60 <1 yr 30 -40 110 -160 70 -90 1 -2 yrs 25 -35 100 -150 75 -95 2 -5 yrs 25 -30 95 -140 85 -100 5 -11 yrs 20 -25 80 -120 90 -110 12 -16 yrs 15 -20 60 -100 100 -120 Oxford Children’s Hospital
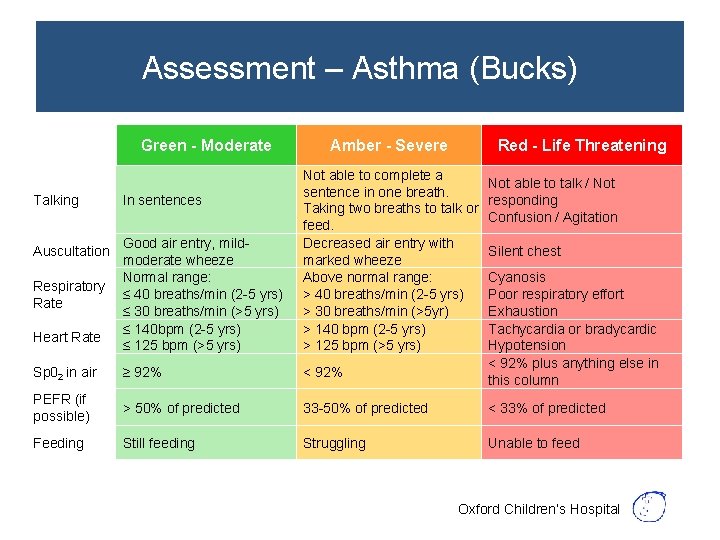
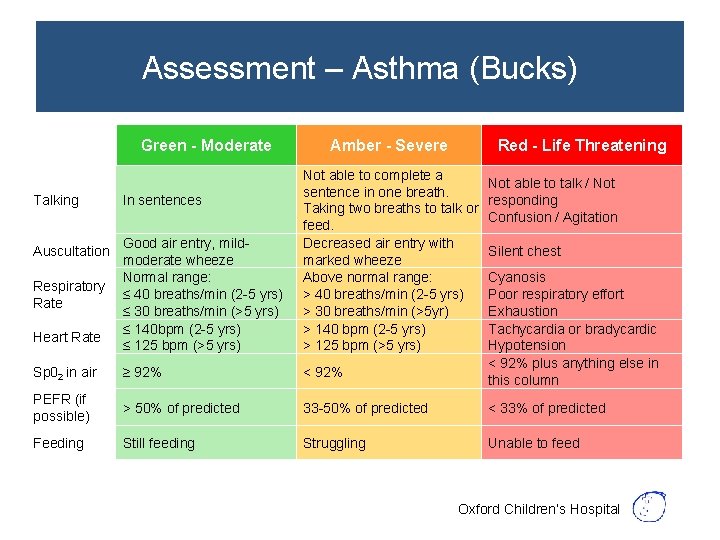
Assessment – Asthma (Bucks) Green - Moderate Amber - Severe Red - Life Threatening Good air entry, mildmoderate wheeze Normal range: ≤ 40 breaths/min (2 -5 yrs) ≤ 30 breaths/min (>5 yrs) ≤ 140 bpm (2 -5 yrs) ≤ 125 bpm (>5 yrs) Not able to complete a sentence in one breath. Taking two breaths to talk or feed. Decreased air entry with marked wheeze Above normal range: > 40 breaths/min (2 -5 yrs) > 30 breaths/min (>5 yr) > 140 bpm (2 -5 yrs) > 125 bpm (>5 yrs) Sp 02 in air ≥ 92% < 92% PEFR (if possible) > 50% of predicted 33 -50% of predicted < 33% of predicted Feeding Still feeding Struggling Unable to feed Talking Auscultation Respiratory Rate Heart Rate In sentences Not able to talk / Not responding Confusion / Agitation Silent chest Cyanosis Poor respiratory effort Exhaustion Tachycardia or bradycardic Hypotension < 92% plus anything else in this column Oxford Children’s Hospital
Assessment – Asthma (BTS) https: //www. brit-thoracic. org. uk/guidelines-and-quality-standards/asthma-guideline/ Oxford Children’s Hospital
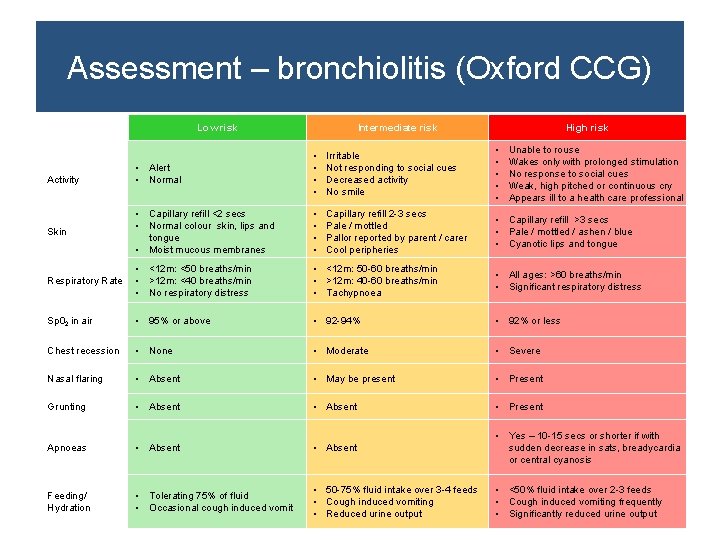
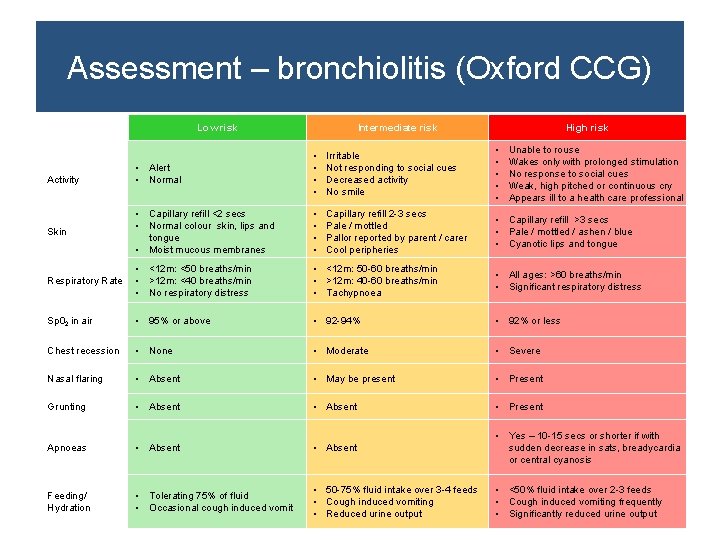
Assessment – bronchiolitis (Oxford CCG) Low risk Intermediate risk High risk • Alert • Normal • • Irritable Not responding to social cues Decreased activity No smile • • • Skin • Capillary refill <2 secs • Normal colour skin, lips and tongue • Moist mucous membranes • • Capillary refill 2 -3 secs Pale / mottled Pallor reported by parent / carer Cool peripheries • Capillary refill >3 secs • Pale / mottled / ashen / blue • Cyanotic lips and tongue Respiratory Rate • <12 m: <50 breaths/min • >12 m: <40 breaths/min • No respiratory distress • <12 m: 50 -60 breaths/min • >12 m: 40 -60 breaths/min • Tachypnoea • All ages: >60 breaths/min • Significant respiratory distress Sp 02 in air • 95% or above • 92 -94% • 92% or less Chest recession • None • Moderate • Severe Nasal flaring • Absent • May be present • Present Grunting • Absent • Present Apnoeas • Absent • Yes – 10 -15 secs or shorter if with sudden decrease in sats, breadycardia or central cyanosis Feeding/ Hydration • Tolerating 75% of fluid • Occasional cough induced vomit • 50 -75% fluid intake over 3 -4 feeds • Cough induced vomiting • Reduced urine output • <50% fluid intake over 2 -3 feeds • Cough induced vomiting frequently • Significantly reduced urine output Activity Unable to rouse Wakes only with prolonged stimulation No response to social cues Weak, high pitched or continuous cry Appears ill to a health care professional
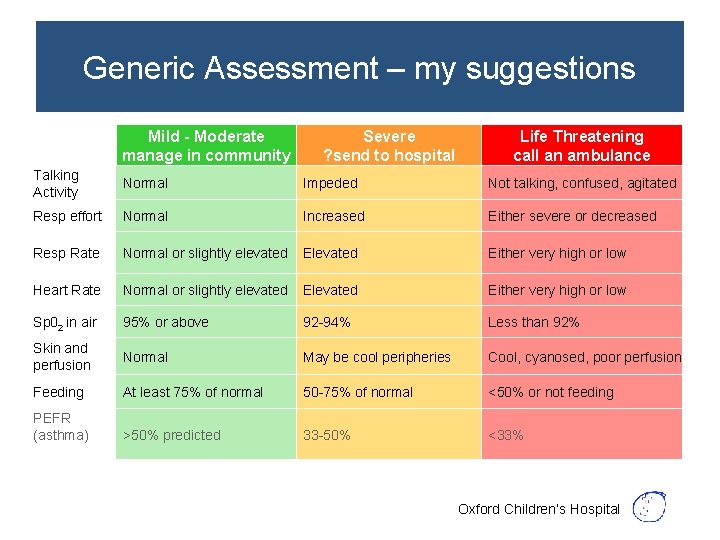
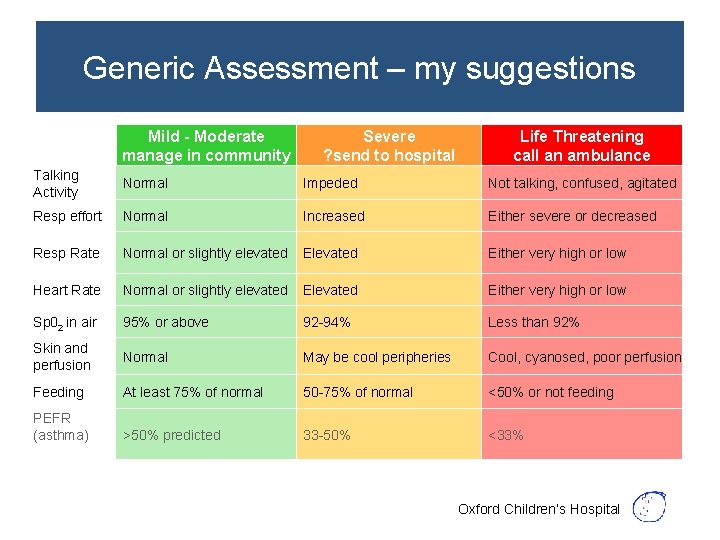
Generic Assessment – my suggestions Mild - Moderate manage in community Severe ? send to hospital Life Threatening call an ambulance Talking Activity Normal Impeded Not talking, confused, agitated Resp effort Normal Increased Either severe or decreased Resp Rate Normal or slightly elevated Either very high or low Heart Rate Normal or slightly elevated Either very high or low Sp 02 in air 95% or above 92 -94% Less than 92% Skin and perfusion Normal May be cool peripheries Cool, cyanosed, poor perfusion Feeding At least 75% of normal 50 -75% of normal <50% or not feeding PEFR (asthma) >50% predicted 33 -50% <33% Oxford Children’s Hospital
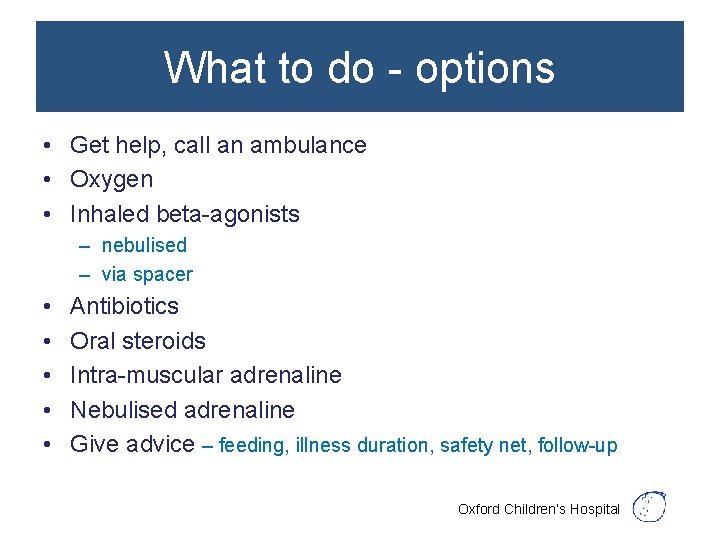
What to do - options • Get help, call an ambulance • Oxygen • Inhaled beta-agonists – nebulised – via spacer • • • Antibiotics Oral steroids Intra-muscular adrenaline Nebulised adrenaline Give advice – feeding, illness duration, safety net, follow-up Oxford Children’s Hospital
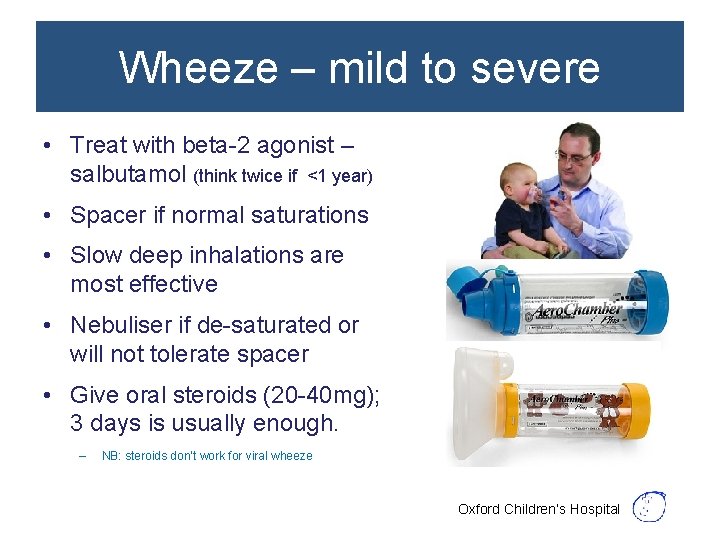
Wheeze – mild to severe • Treat with beta-2 agonist – salbutamol (think twice if <1 year) • Spacer if normal saturations • Slow deep inhalations are most effective • Nebuliser if de-saturated or will not tolerate spacer • Give oral steroids (20 -40 mg); 3 days is usually enough. – NB: steroids don’t work for viral wheeze Oxford Children’s Hospital
Wheeze • Mild to moderate wheeze can be treated at home – Can safely use upto 10 puffs (<5 yrs) or 20 puffs (<5 years) every 4 hours – Reduce frequency according to symptoms – Need to check on the child at least once during the night – Need to seek further help if wheeze worsens – Need review if not better in 3 days Oxford Children’s Hospital
Life-threatening wheeze • Give oxygen • Call an ambulance • Give salbutamol (2. 5 – 5 mg) nebuliser driven by oxygen • Continuous nebulisers if necessary (top-up every 10 minutes) • If you have it, add nebulised ipratropium (250 mcg) for 2 nebs • If the child can swallow, give a dose of prednisolone (20 -40 mg) Oxford Children’s Hospital
Croup • Symptoms and signs – – <5 years coryza for 24 hours barking cough, stridor low grade fever, not toxic • If intermittent stridor, give oral steroid – dexamethasone 0. 15 mg/kg or prednisolone 1 mg/kg 2 doses 12 hours apart • Need planned review if stridor present • Hospital review if – stridor at rest – recession at rest • If desaturated, severe stridor and recession – Give oxygen, call an ambulance, give nebulised adrenaline 5 ml of 1 in 1000 Oxford Children’s Hospital
Bronchiolitis • Symptoms and signs – – infants coryza, breathlessness, poor feeding cough, low grade fever tachypnoea, recession, crackles +/wheeze • Supportive treatment – frequent, smaller volume feeds – paracetamol • Hospital review if – – – recession at rest desaturated, taking <50% of feeds, history of apnoea low threshold for infants < 6 weeks old and ex-preterm infants. Oxford Children’s Hospital
Pneumonia • Symptoms and signs – – lethargy and fever cough, breathlessness, chest pain crackles or bronchial breathing not bilateral wheeze! • Give amoxycillin • Hospital review if – significant respiratory distress (see slide 11) – gets less well or remains febrile after 72 hours despite amoxycillin Oxford Children’s Hospital
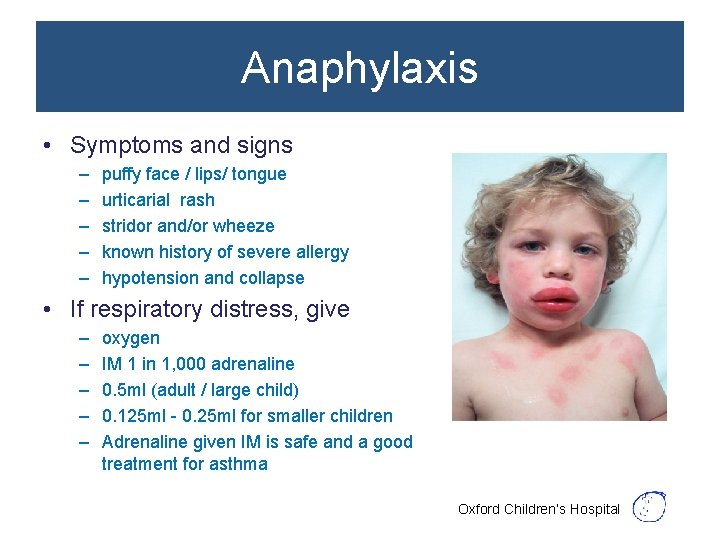
Anaphylaxis • Symptoms and signs – – – puffy face / lips/ tongue urticarial rash stridor and/or wheeze known history of severe allergy hypotension and collapse • If respiratory distress, give – – – oxygen IM 1 in 1, 000 adrenaline 0. 5 ml (adult / large child) 0. 125 ml - 0. 25 ml for smaller children Adrenaline given IM is safe and a good treatment for asthma Oxford Children’s Hospital
Be suspicious if • Very young infant (< 4 weeks) – Increases possibility of a congenital problem (heart or lungs) • There is tachypnoea but no recession, consider – – sepsis acidosis fever anxiety • The child has not been previously well Oxford Children’s Hospital
Follow-up after exacerbations • Follow up within 48 hours (NICE) or at the longest 7 days of discharge – certainly by phone, preferably face – to – face • Identify any avoidable factors and review PAAP – or provide if not already given • Review inhaler technique and adherence • Adjust management if necessary Oxford Children’s Hospital

Duncan’s slides on coding Oxford Children’s Hospital
Follow up after asthma exacerbations • Code and capture asthma admissions and ED attendances – key outcome measure of practice asthma care
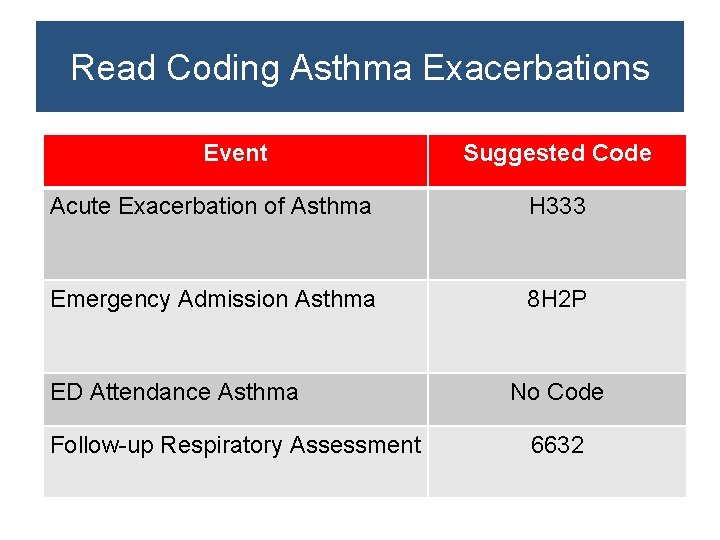
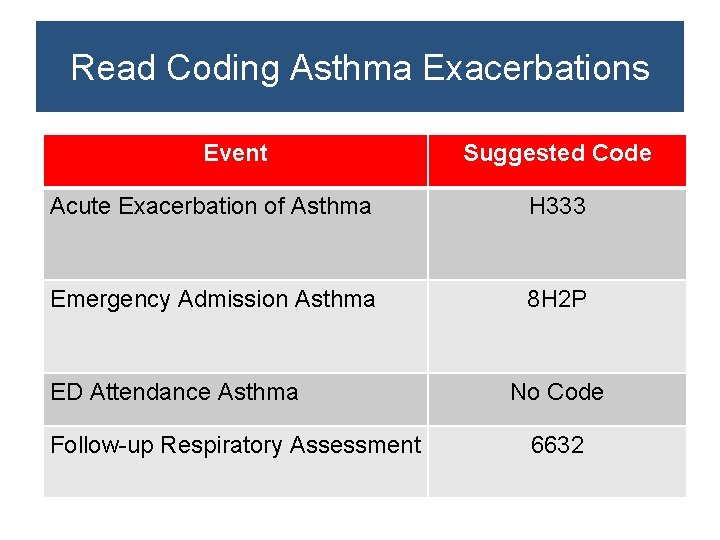
Read Coding Asthma Exacerbations Event Suggested Code Acute Exacerbation of Asthma H 333 Emergency Admission Asthma 8 H 2 P ED Attendance Asthma Follow-up Respiratory Assessment No Code 6632
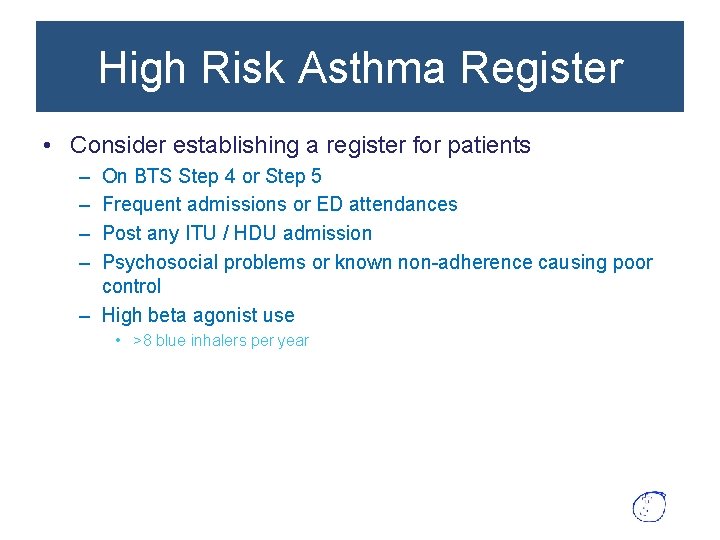
High Risk Asthma Register • Consider establishing a register for patients – – On BTS Step 4 or Step 5 Frequent admissions or ED attendances Post any ITU / HDU admission Psychosocial problems or known non-adherence causing poor control – High beta agonist use • >8 blue inhalers per year
Possible Coding for High Risk Asthma • 13 Zu – “At Risk of Emergency Hospital Admission” • Makes health professionals aware of their risk status, prompts rapid response to calls, notification of OOH service via special patient notes etc. • This code is used for the avoiding unplanned admissions DES and would involve provision of a care plan