Respiratory History and Physical Exam 1 RESPIRATORY SYSTEM
- Slides: 18
Respiratory History and Physical Exam 1
RESPIRATORY SYSTEM HISTORY & PHYSICAL EXAMINATION 2
Presenting Complaints • Patients with lung disease often complain of the following symptoms: – dyspnea/shortness of breath – cough – sputum production – Fatigue – exercise intolerance – chest tightness or chest pain. A thorough history and physical exam is required to identify other signs and symptoms to lead to a diagnosis. 3
History • The respiratory history draws on standard components of the history • • Identifying Data…. Name , age , sex etc. Chief Concern History of Presenting Illness Past Medical History Social History Occupational History Family History Functional Inquiry 4
History of Presenting Illness Along with standard HPI questions, ask about: • COUGH - time of day, severity, dry and hacking or productive • SPUTUM - quantity, colour, consistency, time of day • HEMOPTYSIS - source, colour, quantity • DYSPNEA - orthopnea, PND, severity • PAIN • WHEEZING 5
• • • SPUTUM EVALUATION ask about it, regardless of cough quantity - teaspoons, tablespoons, 1/2 cup clear, thin sputum - early or mild tracheo broncial inflammation yellow/green - results from myelo peroxidase action during cellular breakdown of WBCs during infection green - can also be from eosinophils in asthma (noninfectious) brownish or grayish - tar and nicotine from cigarettes, especially after quitting thick, sticky sputum - from cystic fibrosis thin, frothy, pinkish sputum - pulmonary edema bad-tasting sputum - anaerobic infection 6
Past Medical History ASK ESPECIALLY ABOUT PRIOR ILLNESSES, INCLUDING: • • • childhood respiratory illnesses asthma pneumonia TB other 7
• SOCIAL HISTORY • • • ask about travels environmental history: home - animals, humidifiers, heating occupation - exposure to chemicals or other agents personal - smoking, alcohol, drugs, hobbies • ENVIRONMENTAL FACTORS • CH 2 OPD 2 mnemonic (Community, Home, Hobbies, Occupation, Personal habits, Diet and Drugs) • OCCUPATIONAL HISTORY • • chronological listing of all jobs precise job activities all materials used in job, with MSDS if possible duration and intensity of exposure protective measures used, or breached ventilation of workplace timing relationship of symptoms with shift or vacation other workers similarly affected 8
PHYSICAL EXAMINATION • • • • To examine the back, have the person sitting, with arms crossed to move the scapulae out of the way. The front of the chest can be examined with the person sitting or lying down. Respiratory rates decrease with age. The are most accurately measured with the patient asleep. Infants and young children can be evaluated abdominally; older children and adults with direct measurement of chest movement. Normal rates are as follows (breaths/min): newborns: 30 -50 toddlers: 20 -40 school-aged children: 15 -25 adolescents and adults: 12 -20 Other aspects of the respiratory exam are as follows: respiratory rate (normal adult: 14 -20); note expiratory length. pulse blood pressure pulsus paradoxus Sp. O 2 temperature 9
INSPECTION • • • • General Inspection height, weight, BMI development nutrition edema position Chest shape barrel shaped: asthma, COPD in adults, cystic fibrosis in children pectus excavatum pectus carinatum symmetry, integrity respiratory distress tachypnea 10
• • • • use of accessory muscles during inspiration intercostal indrawing, supraclavicular indrawing diaphoresis nasal flaring, grunting in infants and children pursed lip breathing in adults audible sounds: snore, stridor, wheeze, ease of speech respiratory rhythm - regular, Kussmaul, Biot, Cheyne-stokes colour - pigmented, jaundiced, pale, plethoric, cyanosis nicotine stains clubbing skin - lesions, scars thoraco-abdominal motion - normal, paradoxical bony thorax and AP diameter expansion on deep inspiration position of trachea 11
PERCUSSION • Percussion is one of the most important techniques, establishing whether tissues are fluid-filled, air-filled, or solid. • pleural effusion will sound flat • lobar pneumonia will sound dull • unilateral hyper resonance suggests pneumothorax or COPD • Measure descent of diaphragm, normally 5 -6 cm in adults. • Dullness is heard over the scapula, liver, heart, and diapragm. It can also be caused by consolidation, fluid, pleural effusion, or pleural thickening. • Hyperresonance can be heard with a hyper inflated chest, ie with astma or COPD. 12
PALPATION • AREAS OF TENDERNESS: fractured rib, inflamed pleura. give a squeeze AP and laterally to elicit. • CHEST EXPANSION: place thumbs at level of 10 th ribs. placing the hands on the sides is most sensitive. • TACTILE FREMITUS: palpable vibrations transmitted to chest wall. check front and back may be decreased due to obstruction, COPD, pleural effusion, fibrosis, pneumothorax, or tumour may be increased due to pneumonia 13
AUSCULTATION • Warm the stethoscope. • Sound travels better through solid tissue than air; broncophony, egophony, or whispered pectoriloquy all represent solid or liquid is present. • listen to bare skin • breathe through open mouth • aim for between the ribs • dlp: Make a diagram of the chest wall, of where to listen • get people to pull arms forward to get scapulae out of the way when listening to back 14
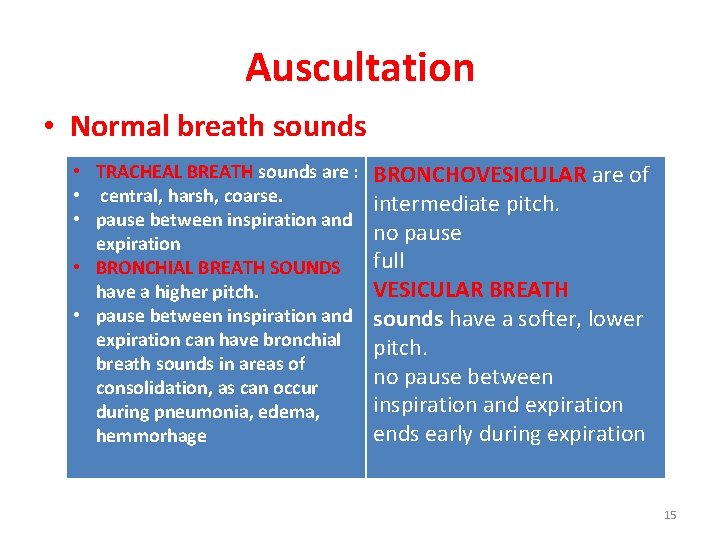
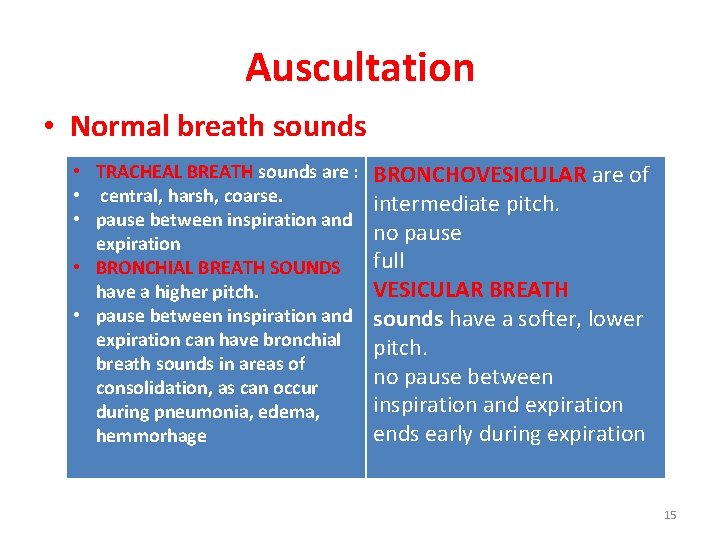
Auscultation • Normal breath sounds • TRACHEAL BREATH sounds are : • central, harsh, coarse. • pause between inspiration and expiration • BRONCHIAL BREATH SOUNDS have a higher pitch. • pause between inspiration and expiration can have bronchial breath sounds in areas of consolidation, as can occur during pneumonia, edema, hemmorhage BRONCHOVESICULAR are of intermediate pitch. no pause full VESICULAR BREATH sounds have a softer, lower pitch. no pause between inspiration and expiration ends early during expiration 15
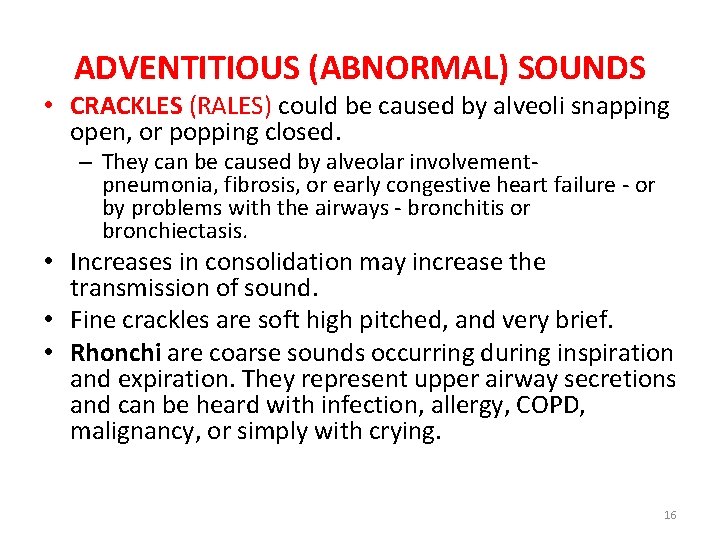
ADVENTITIOUS (ABNORMAL) SOUNDS • CRACKLES (RALES) could be caused by alveoli snapping open, or popping closed. – They can be caused by alveolar involvementpneumonia, fibrosis, or early congestive heart failure - or by problems with the airways - bronchitis or bronchiectasis. • Increases in consolidation may increase the transmission of sound. • Fine crackles are soft high pitched, and very brief. • Rhonchi are coarse sounds occurring during inspiration and expiration. They represent upper airway secretions and can be heard with infection, allergy, COPD, malignancy, or simply with crying. 16
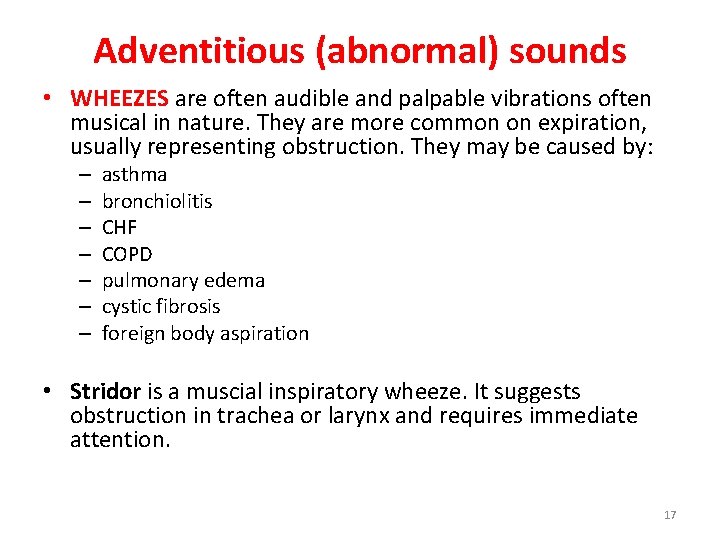
Adventitious (abnormal) sounds • WHEEZES are often audible and palpable vibrations often musical in nature. They are more common on expiration, usually representing obstruction. They may be caused by: – – – – asthma bronchiolitis CHF COPD pulmonary edema cystic fibrosis foreign body aspiration • Stridor is a muscial inspiratory wheeze. It suggests obstruction in trachea or larynx and requires immediate attention. 17
Pediatrics • A smaller stethoscope is better to use in infants. Ensure the head is midline. • A crying baby can still provide much information, and in fact inspiration can be well evaluated. 18