RESPIRATORY FUNCTION Stacie Pigues MSN RN NWCC NUR



- Slides: 72
RESPIRATORY FUNCTION Stacie Pigues, MSN, RN NWCC NUR 1117 Foundations of Nursing
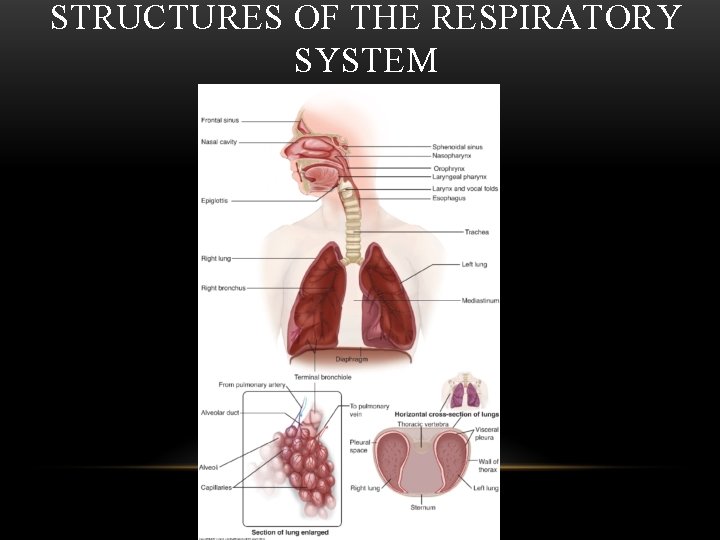
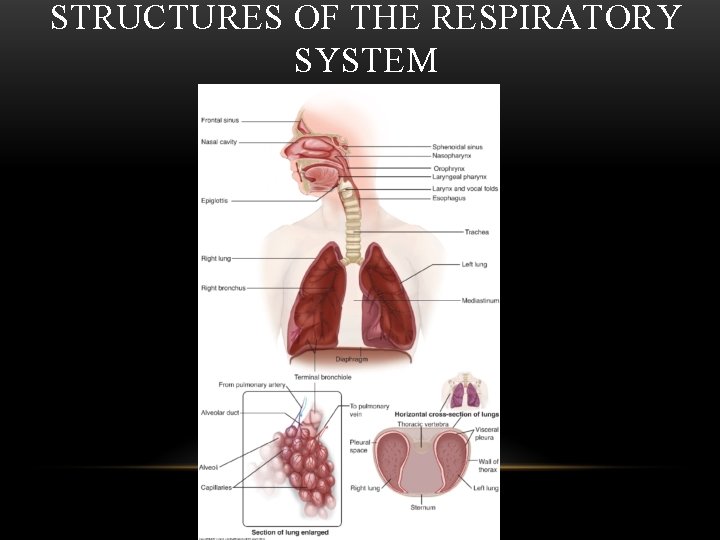
STRUCTURES OF THE RESPIRATORY SYSTEM
STRUCTURES OF THE RESPIRATORY SYSTEM Upper Airway: – Mouth – Nose – Pharynx
STRUCTURES OF THE RESPIRATORY SYSTEM Lower Airway: – Trachea – Bronchioles – Alveoli – Lungs
NORMAL RESPIRATORY FUNCTION – – – Ventilation Gas diffusion Gas transport Control of ventilation Defenses of the respiratory system Normal breathing pattern
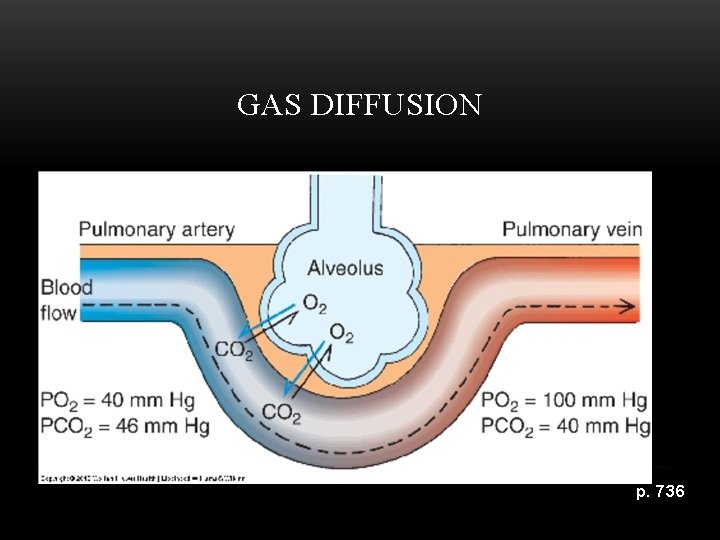
NORMAL RESPIRATORY FUNCTION • Ventilation, or breathing, is the process of moving air into and out of the lungs so that gas exchange can take place. • Gas Diffusion refers to the movement of oxygen between the alveoli and the blood.
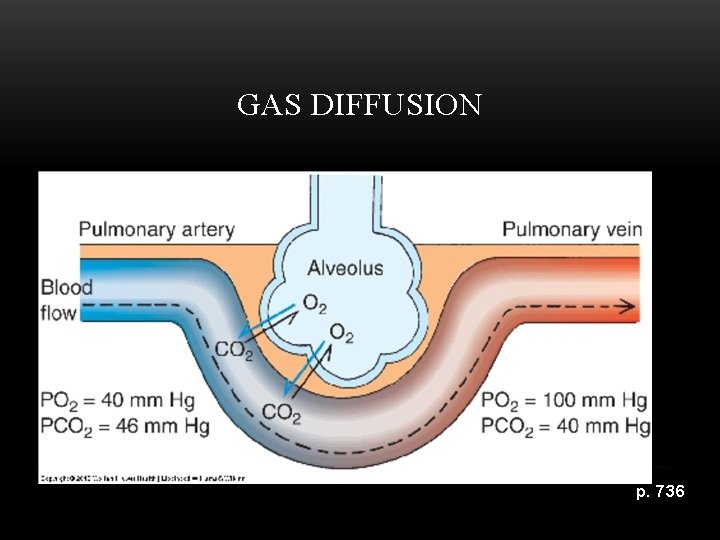
GAS DIFFUSION p. 736
NORMAL RESPIRATORY FUNCTION • Gas Transport occurs when oxygen crosses the alveolar-capillary membrane into the blood where blood transports it to the tissues. • Control of Ventilation, this process is controlled through neural pathways.
DEFENSES OF THE RESPIRATORY SYSTEM Upper Airway functions to: • Warm and humidify inspired air while maintaining the fluid character of the lower airway • Clean inspired air • Protect lower airway from infection and injury due to aspiration
DEFENSES OF THE RESPIRATORY SYSTEM Lower Airway functions to: • Further clean inspired air • “Mucus Blanket” –protects • “Mucociliary Elevator”- helps remove bacteria
PROTECTIVE REFLEXES • Coughing • Sneezing
FACTORS THAT AFFECT BREATHING • Age • Activity level • Life style
NORMAL BREATHING PATTERN Normal Parameters of Respiratory Rates • effortless, smooth, even and regular • average adult moves ½ L of air per breath
NORMAL BREATHING PATTERN Newborns and infants • Rapid breathers • Breathe 30 -60 times per minute • Surfactant replacement therapy
NORMAL BREATHING PATTERN Toddler and Preschooler • Breathing even and smoother • By age three, 20 -30 breaths per min. • Risk for aspiration
NORMAL BREATHING PATTERN Child and Adolescent • Breathing steadily slows • Breathe 12 -20 times per minute • Adolescence smoking and tobacco use
NORMAL BREATHING PATTERN Adults • Breathe 12 -20 times per minute • Structural and functional changes: ØThoracic wall is more rigid ØLungs do not stretch as well ØGas exchange is affected ØProtective functions are impaired ØCough is less effective
NORMAL BREATHING PATTERN Older Adults • Breathe 16 -25 times per minute • Factors that affect older adults respiratory changes contribute to: Ø Activity intolerance Ø Increased respiratory infections
HISTORY • Do you have a cough? • Common causes: üHistamines üBorderline heart failure üNervous habit ü“Common” cough-only concerned if it changes
HISTORY • Are you coughing up sputum? üHow much? Teaspoon, tablespoon or ½ cup üWhat is the color of the sputum? Clear, yellow, bloody (hemoptysis) üConsistency? Thick or thin
HISTORY • Are you experiencing shortness of breath (dyspnea)? • Possible causes: üLung disease üCHF üAnxiety
HISTORY • Are you having any chest pain? • Possible causes: üInfection üInflammation üPneumonia üBronchitis
HISTORY • What is your normal breathing pattern? • When and how often do the breathing problems occur? • Identify any exposures putting the patient at risk.
FACTORS AFFECTING RESPIRATORY FUNCTION • Environment • Lifestyle and habits • Body position • Increased work of breathing
ENVIRONMENT • • Weather Geographical location Air pollution Pollens and allergens
LIFESTYLE AND HABITS • Smoking: pack(per day/week) or years • Drugs and alcohol • Nutrition
INCREASED WORK OF BREATHING Restricted lung movement • Atelectasis • May be chronic or acute due to: • Smoke inhalation • Pulmonary fibrosis • Respiratory distress syndrome • Pneumonia
INCREASED WORK OF BREATHING Restricted lung movement • Obesity • Chest or abdominal binders • Abdominal distension caused by gas/fluid • Meds/anesthesia • Rib injuries • Musculoskeletal chest deformities • Severe weakness • Neuromuscular disorders
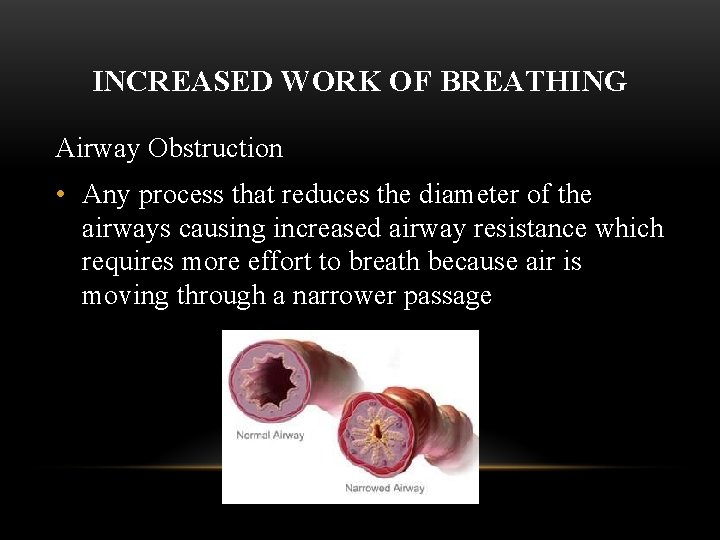
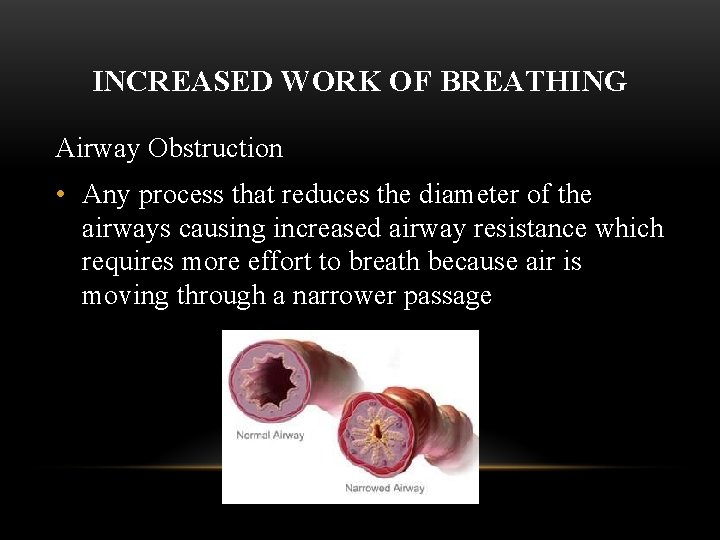
INCREASED WORK OF BREATHING Airway Obstruction • Any process that reduces the diameter of the airways causing increased airway resistance which requires more effort to breath because air is moving through a narrower passage
INCREASED WORK OF BREATHING Airway Obstruction • Possible causes of airway obstruction are: • Foreign body aspiration • Excessive mucus üChronic bronchitis üCystic Fibrosis üAsthma üCroup üEpiglottis • Abnormal growths in the airway
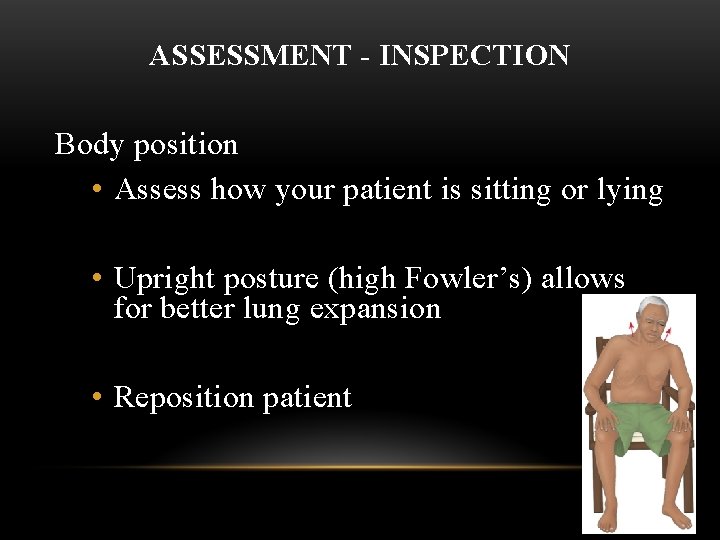
ASSESSMENT - INSPECTION Body position • Assess how your patient is sitting or lying • Upright posture (high Fowler’s) allows for better lung expansion • Reposition patient
ASSESSMENT - INSPECTION • What is the rate? • How hard are they working to breathe? • Describe breathing pattern. Ø Hypoxemia-low oxygen levels in the blood Ø Hypercapnia-abnormally high carbon dioxide in the blood Ø Hyperventilation- excessive elimination of carbon dioxide causing dizziness and respiratory alkalosis
ASSESSMENT - INSPECTION Assessing color: • Cyanosis- bluish skin discoloration caused by a desaturation of oxygen on the hemoglobin – Central cyanosis-mucus membranes blue around mouth and eyes - indicates SEVERE oxygenation problems
ASSESSMENT - INSPECTION • Clubbing- round and enlarged fingers and toes • Chest deformities- barrel chest • Wounds • Masses
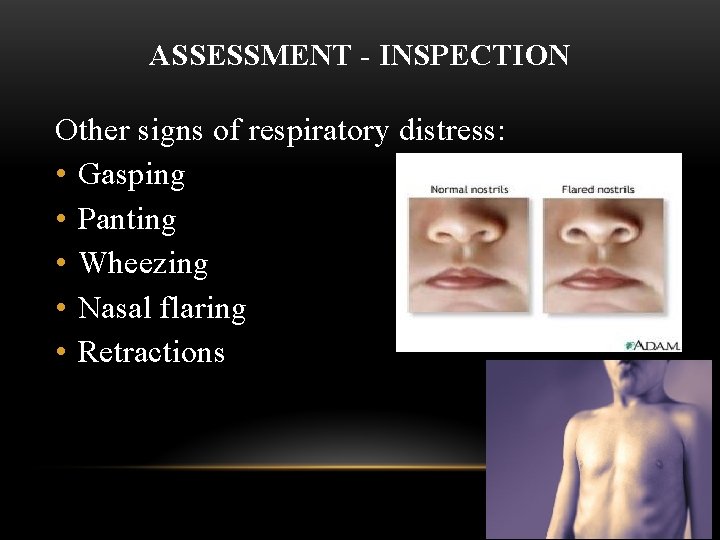
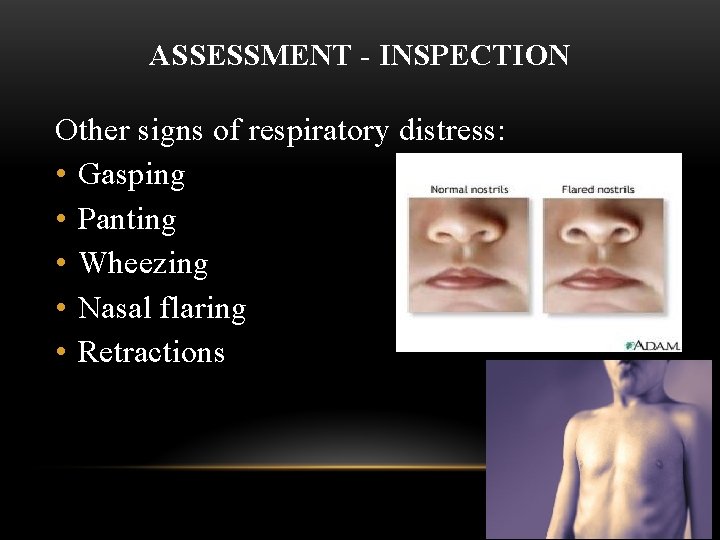
ASSESSMENT - INSPECTION Other signs of respiratory distress: • Gasping • Panting • Wheezing • Nasal flaring • Retractions
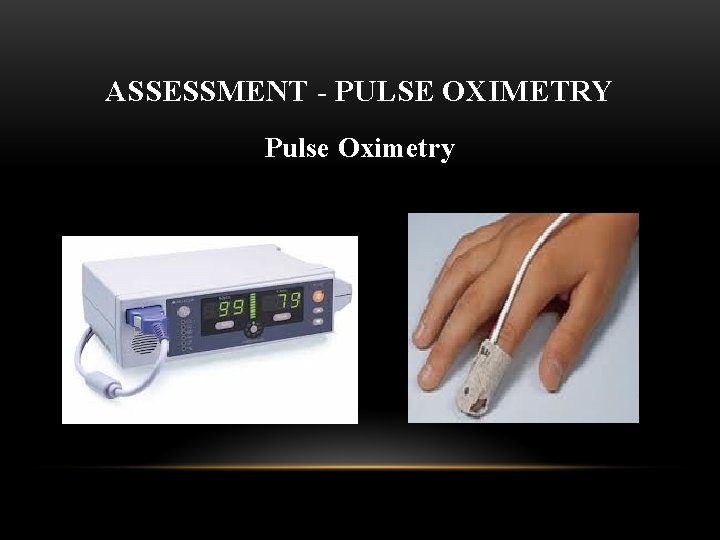
ASSESSMENT - PULSE OXIMETRY Pulse Oximetry
ASSESSMENT - PULSE OXIMETRY Pulse Oximetry - O 2 Saturation • Any changes in a patient’s level of consciousness, dizziness, restlessness, agitation, etc. —check pulse oximeter-may be due to hypoxia! If oxygen level normal—check glucose level. • Normal Oxygen sat 95 -100% with O 2 intervention generally required if < 93% • Patients with sleep apnea may need to bring their machines to the hospital. These patients are at high risk for hypoxia and respiratory arrest especially post-op. • Higher altitudes= less oxygen available for gas diffusion = SOB & activity intolerance (p. 738)
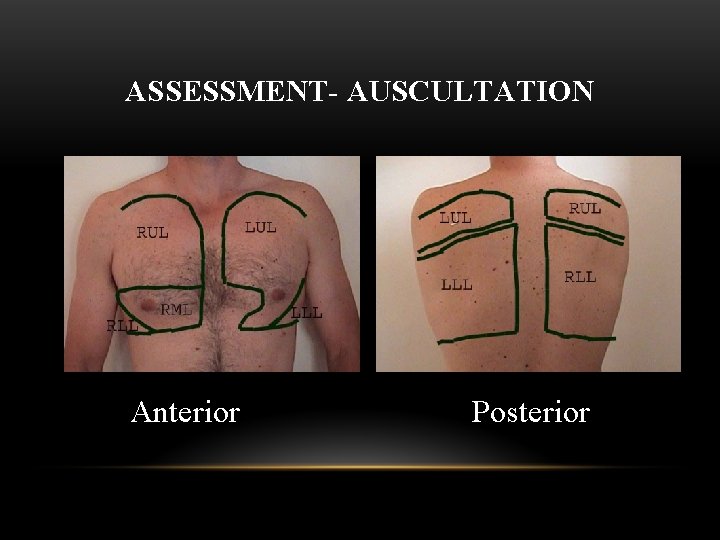
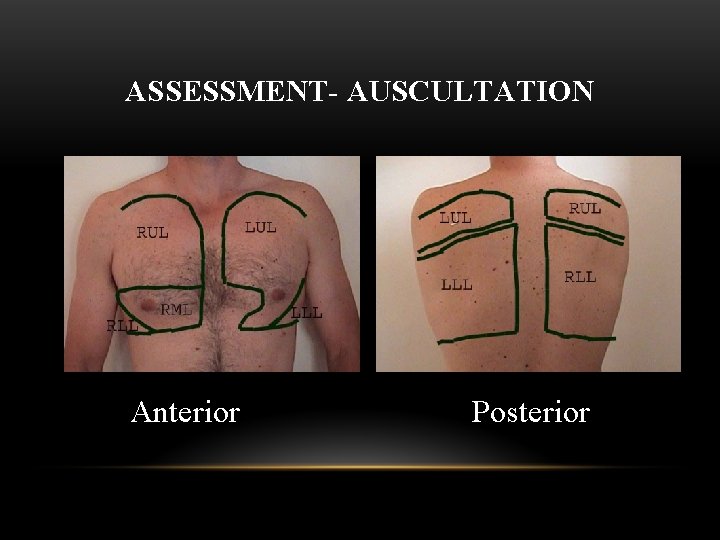
ASSESSMENT- AUSCULTATION Anterior Posterior
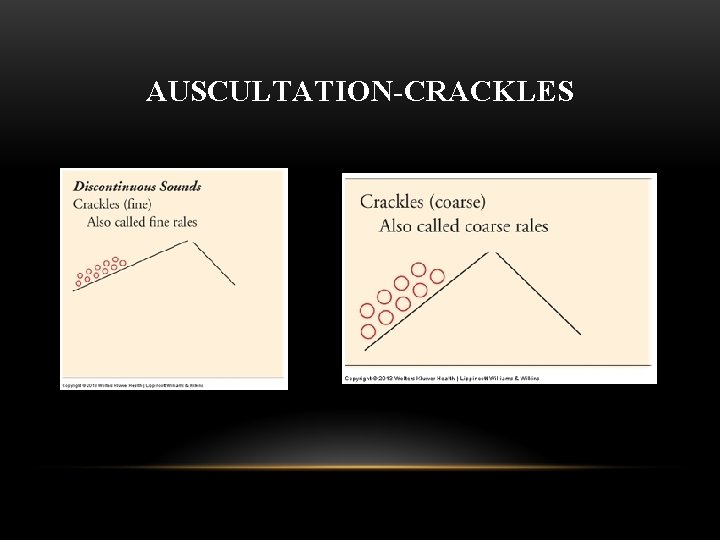
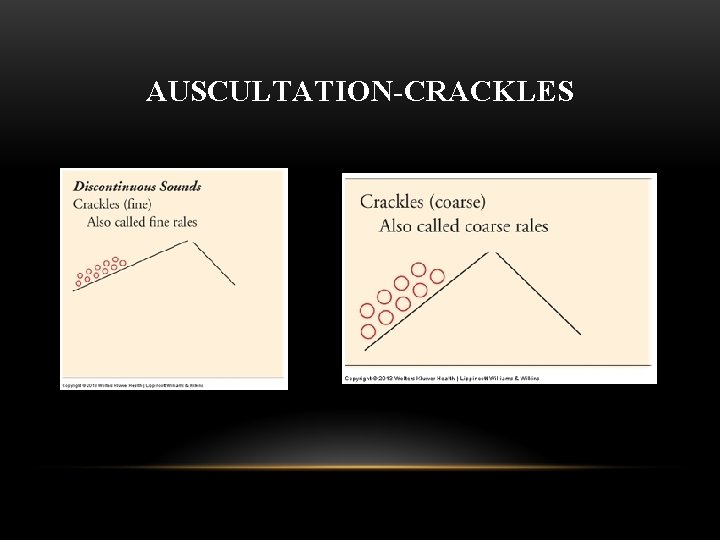
AUSCULTATION-CRACKLES
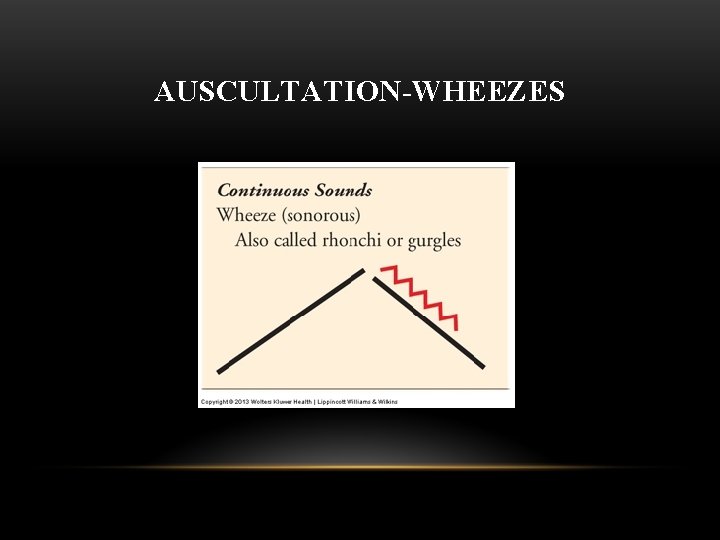
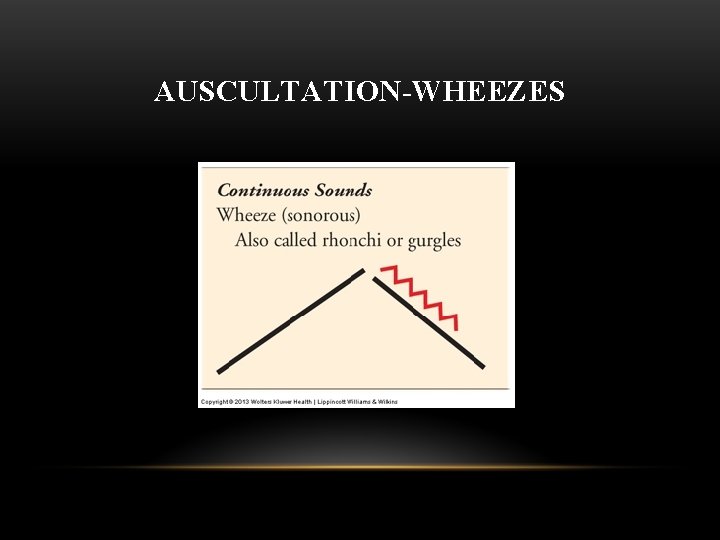
AUSCULTATION-WHEEZES

DIAGNOSTIC TESTS AND PROCEDURES • Sputum culture- Culture & Sensitivity Ø Thick and sticky Ø Yellow or green Ø Putrid or musty odor Ø Blood streaked Ø Frankly red, bloody (hemoptysis)
DIAGNOSTIC TESTS AND PROCEDURES Arterial blood gas (ABG) monitoring • Arterial blood levels of oxygen, carbon dioxide and PH are the best indicator of gas exchange. • Hyperventilation • Hypoventilation
DIAGNOSTIC TESTS AND PROCEDURES • Chest x-ray • Pulmonary function tests (PFT) • Bronchoscopy • Lung scan/CT/MRI
DIAGNOSTIC TESTS AND PROCEDURES • Throat culture • Sputum specimens • Cytology • Thoracentesis • Skin tests – PPD given to test TB exposure – Allergy tests identify airway hypersensitivity in asthmatics
NURSING DIAGNOSES • Ineffective Breathing Pattern-monitor the patient and encourage slow, deep breathing, turning and coughing • Ineffective Airway Clearance-ensure adequate hydration, instruct on how to cough effectively • Impaired Gas Exchange- monitor cognitive changes, ABG, O 2 Saturation, S & S of respiratory failure
OUTCOMES IDENTIFICATION AND PLANNING • Knowledge regarding prevention of respiratory dysfunction • Adequate oxygenation • Mobilize pulmonary secretions • Cope with changes in self-concept and lifestyle
IMPLEMENTATION Health promotion • Preventing respiratory infections • Encouraging smoking cessation • Reducing allergens • Monitoring peak flow
IMPLEMENTATION Health promotion • Providing adequate hydration • Positioning and ambulation • Deep breathing and coughing • Assisting with incentive spirometry
NURSING INTERVENTIONS Coughing • Deep cough • Stacked cough • Low-flow (huff) cough • Quad cough
NURSING INTERVENTIONS • Pursed-lip breathing • Chest physiotherapy – Percussion – Vibration – Postural drainage
NURSING INTERVENTIONS Aerosol Therapy – Aerosol medications-a suspension of liquid droplets in air or oxygen – Aerosols can be uses for several reasons: • Adds moisture to oxygen • Hydrates mucus to prevent mucus plugs • Used to administer drugs, such as: ü Bronchodilator ü Corticosteroids ü Antibiotics
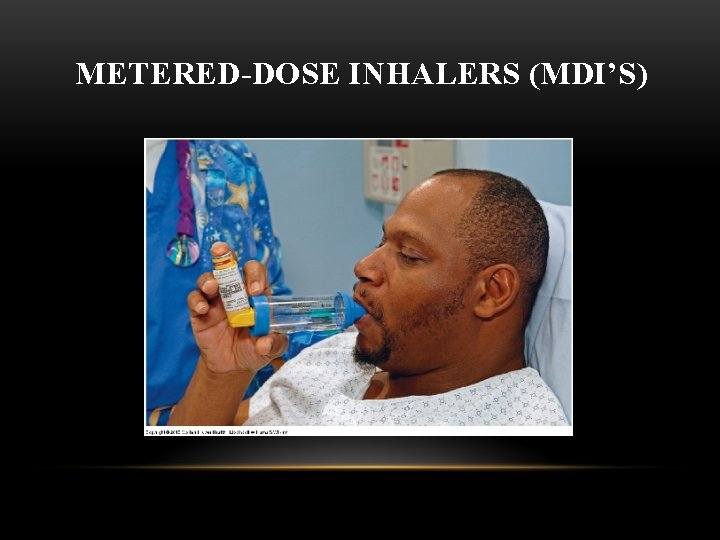
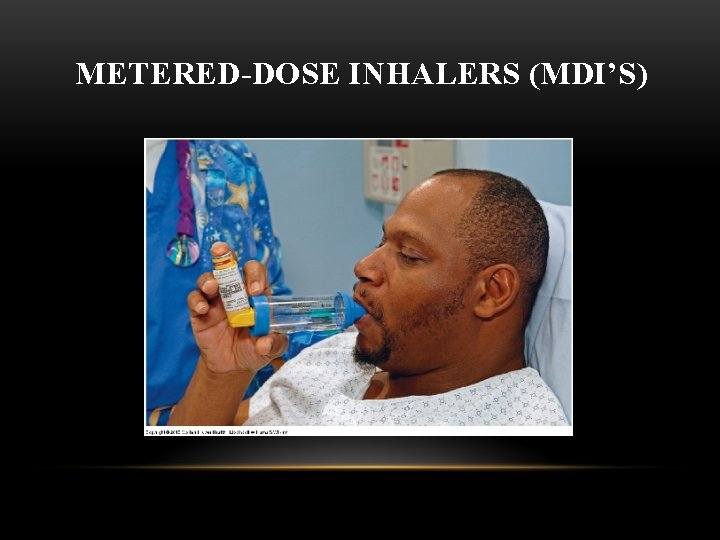
METERED-DOSE INHALERS (MDI’S)
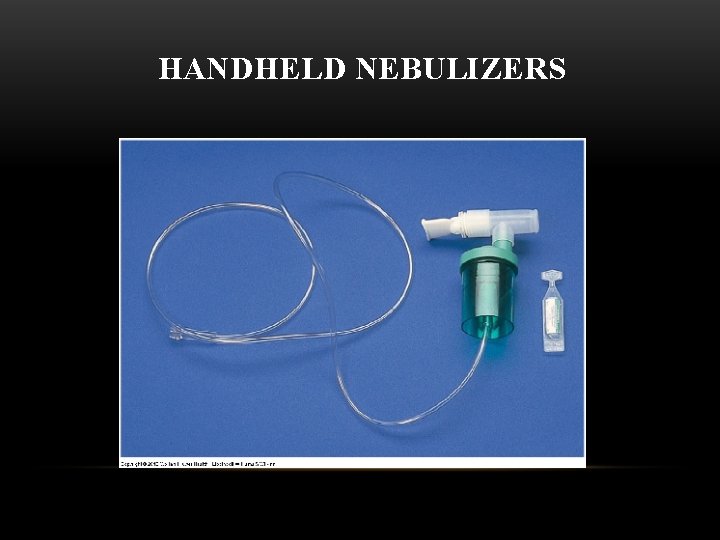
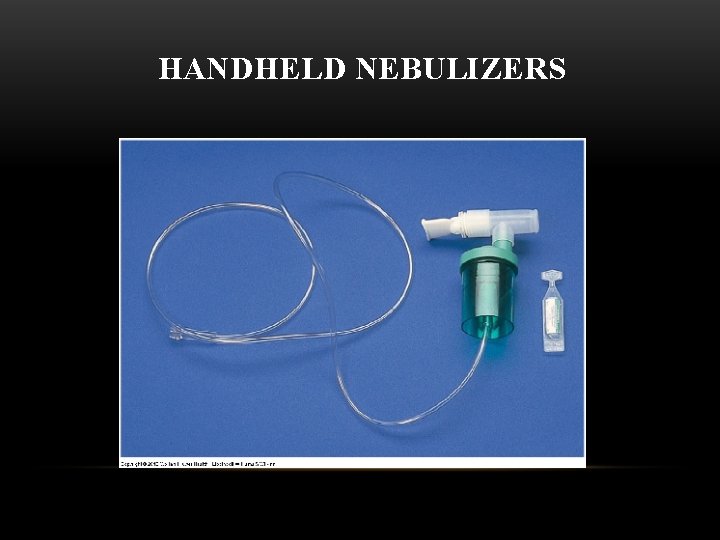
HANDHELD NEBULIZERS
OXYGEN THERAPY ADMINISTRATION • Oxygen therapy can be used to accomplish three fundamental goals in patient care: • Improves tissue oxygenation allowing for better healing to occur- when in the healing process, the body’s metabolic demand for oxygen is increased. • Helps decrease work of breathing in patients with shortness of breath or dyspnea • Decreases the work of the heart in patients with cardiac diseases
OXYGEN THERAPY ADMINISTRATION • Oxygen flow is ordered in liters per minute. General rule in the use of O 2 therapy is to use the lowest amount possible to achieve an acceptable blood oxygen level. • You will find that most patients’ will have an order for Oxygen if the Sa. O 2 is below 93%. Oxygen is used to help stabilize the patient and then they will be slowly weaned off O 2 therapy. You will monitor for color, alertness, heart rate, O 2 Sat, and breathing effort. • *ENSURE THAT THE APPROPRIATE AMOUNT OF OXYGEN PRESCRIBED IS BEING DELIVERED!
SELECTION OF OXYGEN SYSTEMS • Various devices are available for providing oxygen at different flow rates and concentrations • Device used depends on patients oxygenation status • Best oxygen device is provided with consideration of comfort for the patient
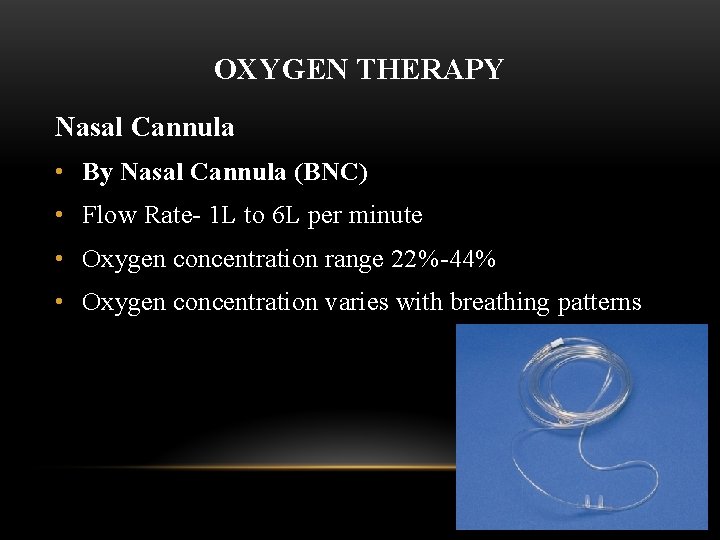
OXYGEN THERAPY Nasal Cannula • By Nasal Cannula (BNC) • Flow Rate- 1 L to 6 L per minute • Oxygen concentration range 22%-44% • Oxygen concentration varies with breathing patterns
OXYGEN THERAPY Venturi mask • Flow rate- 3 L to 8 L per minute • Oxygen concentration range- 24% to 50%
OXYGEN THERAPY Simple mask • Flow rate- 6 to 10 L per minute • Oxygen concentration range 40%-60% • Oxygen concentration varies with breathing patterns
OXYGEN THERAPY Reservoir (Non-rebreather) mask • Flow rate- 10 to 15 L per minute • Oxygen concentration range 90%+ • Used for critically ill patients
OXYGEN SAFETY • Oxygen is a drug; an order is required • Monitor flow rate to ensure accurate amount is being administered • Normal range for oxygen saturation is 95 -100%; O 2 for <93% • Teach the importance of wearing oxygen device • Smoking is prohibited
OXYGEN SAFETY • Review the Safety Alerts in Craven regarding COPD & oxygen • The normal drive to breath is high carbon dioxide level (hypercapnia); however, the patient with COPD has become accustomed to this, therefore their drive to breath is hypoxemia (low oxygen level). • Patients with COPD must be maintained with low concentrations of oxygen. • Oxygen therapy requires physician order-may see oxygen initiated, changed and discontinued without a written order on the chart if respiratory therapy utilizes oxygen protocol. This protocol has medical staff approval.
NURSING INTERVENTIONS • Dyspnea management • Hyperventilation management • Assisted ventilation – Bi. PAP (Bilevel Positive Airway Pressure) – CPAP (Continuous Positive Airway Pressure)
NURSING INTERVENTIONS Artificial Airways • Oral or Nasal Pharyngeal Airways • Endotracheal Tubes • Trachesotomy

PHARYNGEAL AIRWAYS Oral Airways Nasal Trumpets
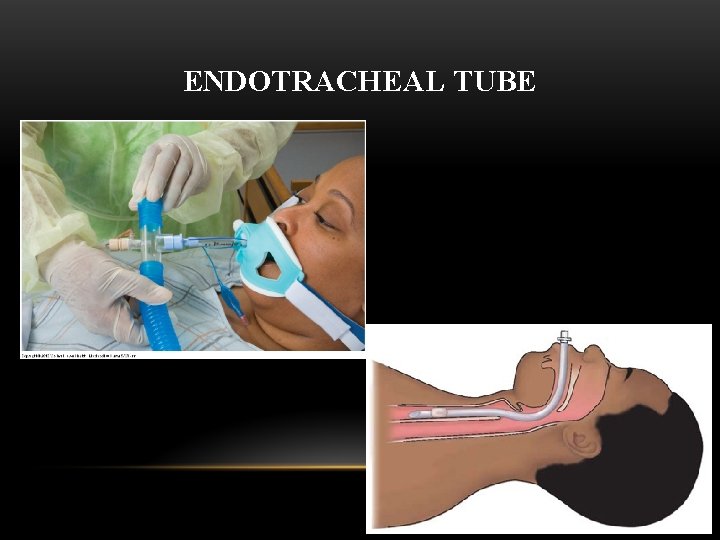
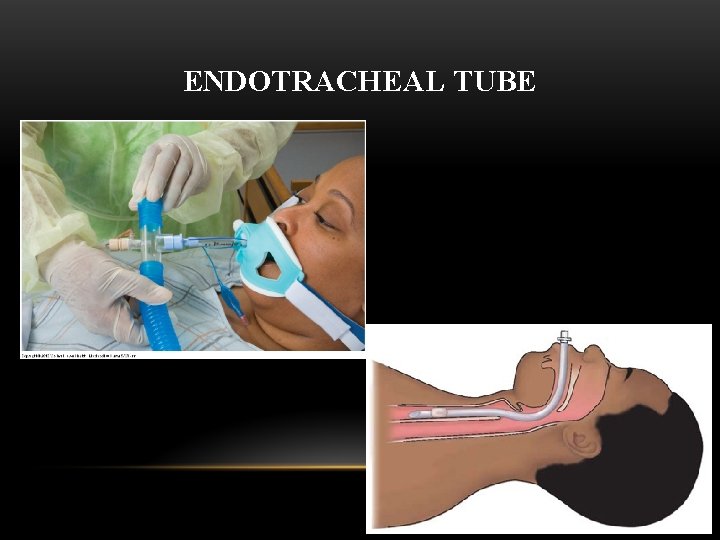
ENDOTRACHEAL TUBE
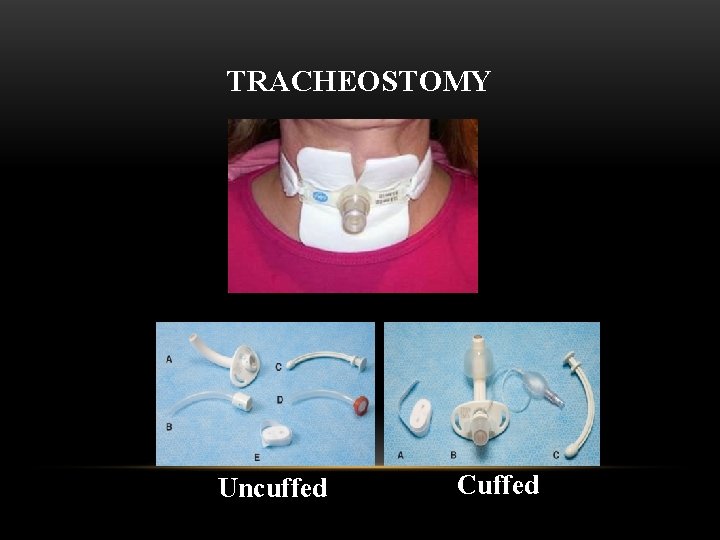
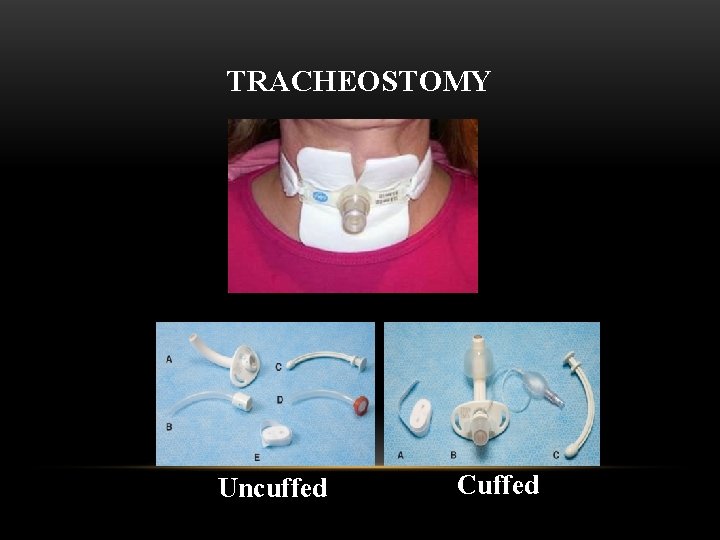
TRACHEOSTOMY Uncuffed Cuffed
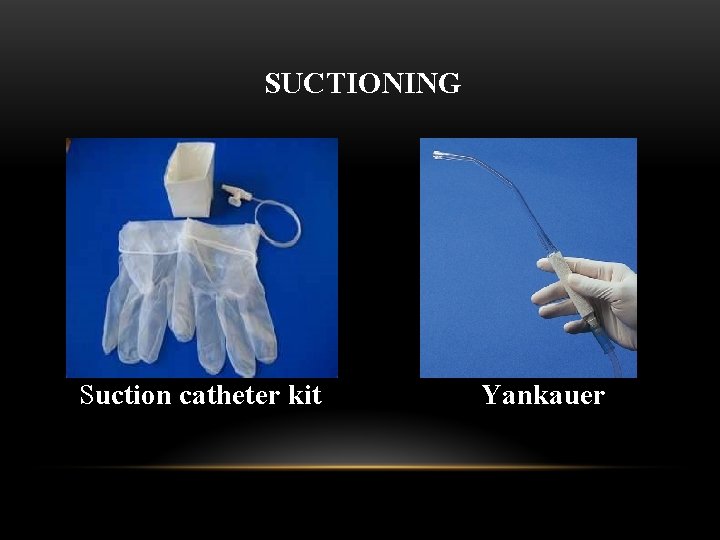
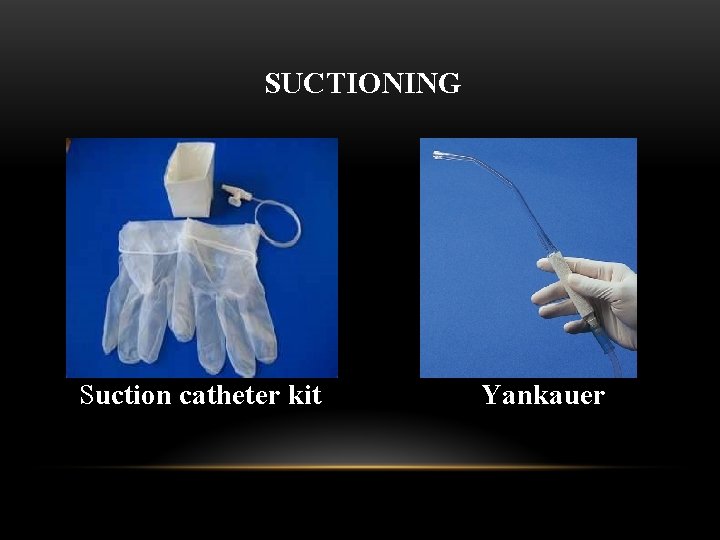
SUCTIONING Suction catheter kit Yankauer
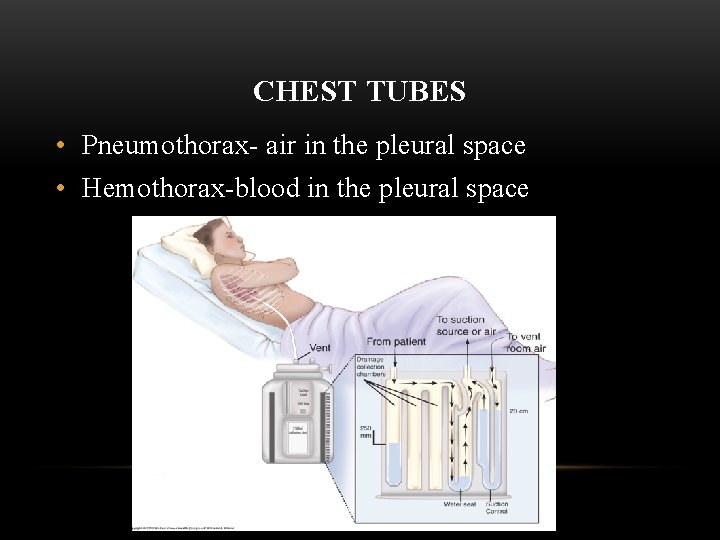
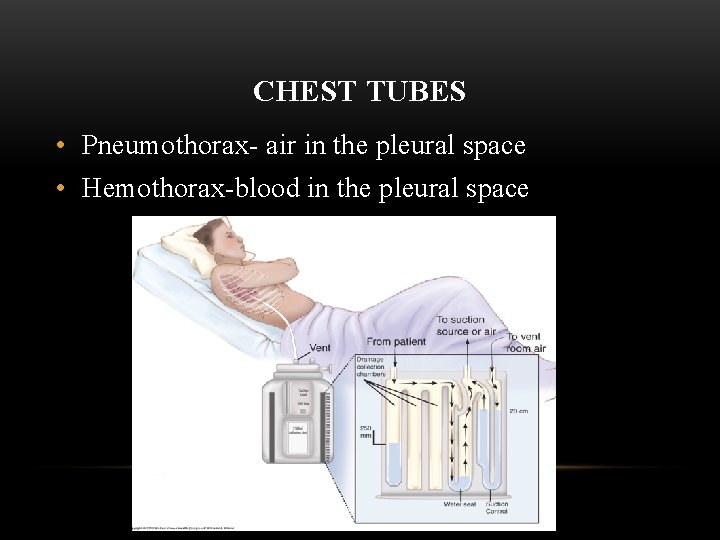
CHEST TUBES • Pneumothorax- air in the pleural space • Hemothorax-blood in the pleural space
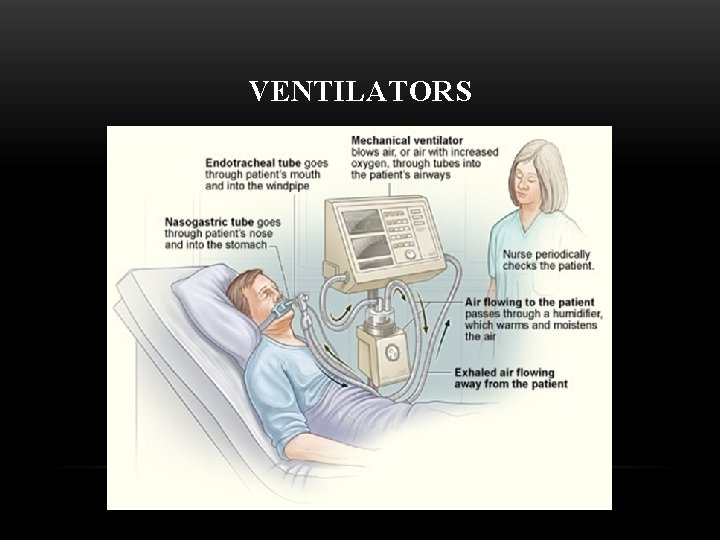
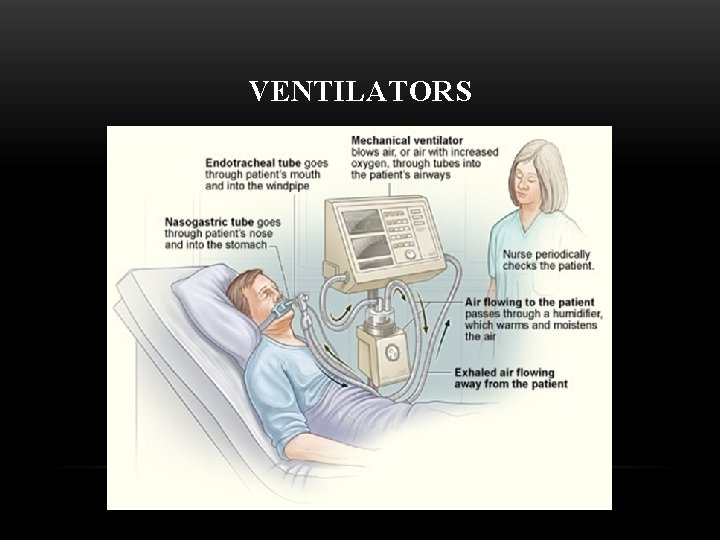
VENTILATORS

DISCHARGE NEEDS • Infection control • Medications • Home oxygen systems • Energy conservation • Fostering self-esteem
REFERENCES • Craven, R, Hirnle, C. & Jensen, S. (2013). Fundamentals of Nursing (7 th ed. ). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. Chapter 25.