Respiratory Distress Syndrome IAP UG Teaching slides 2015
- Slides: 25
Respiratory Distress Syndrome IAP UG Teaching slides 2015 -16 1
What the Medical student or primary care physician should know • Purpose: • Simple intervention CPAP can save many preterm babies with moderately severe RDS • Surfactant therapy – cost effective / life saving • ANS – prevention of RDS • Detailed – skill to be acquired • ANS • RD scores • Basic knowledge IAP UG Teaching slides 2015 -16 2
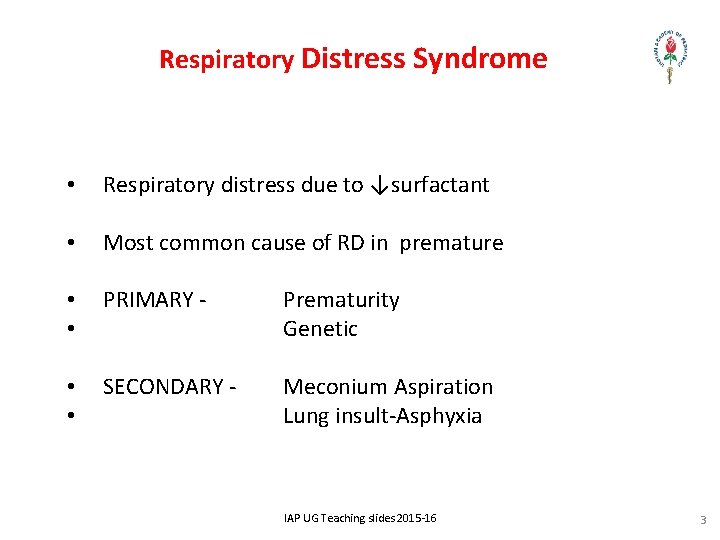
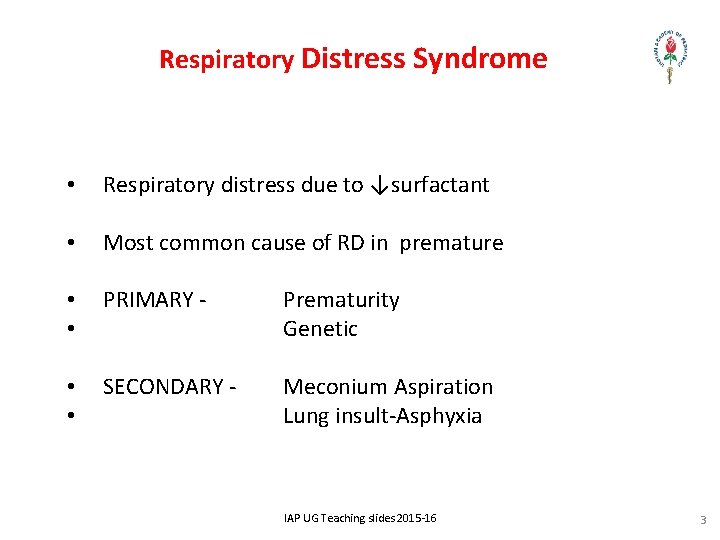
Respiratory Distress Syndrome • Respiratory distress due to ↓surfactant • Most common cause of RD in premature • • PRIMARY - Prematurity Genetic • • SECONDARY - Meconium Aspiration Lung insult-Asphyxia IAP UG Teaching slides 2015 -16 3
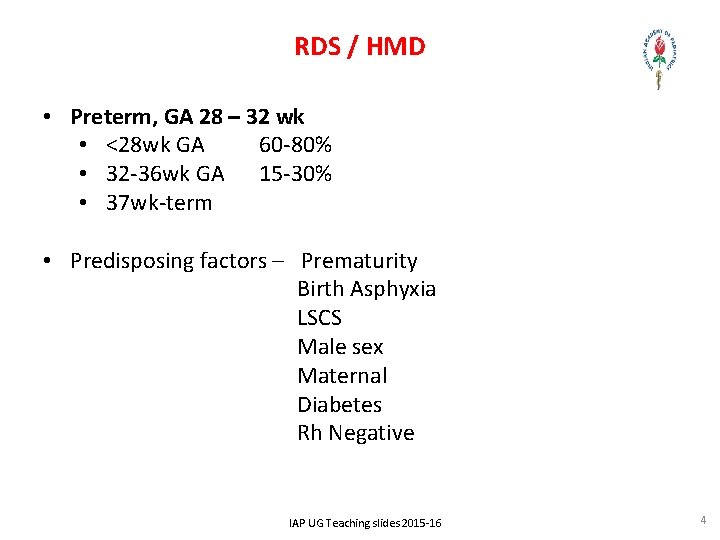
RDS / HMD • Preterm, GA 28 – 32 wk • <28 wk GA 60 -80% • 32 -36 wk GA 15 -30% • 37 wk-term • Predisposing factors – Prematurity Birth Asphyxia LSCS Male sex Maternal Diabetes Rh Negative IAP UG Teaching slides 2015 -16 4
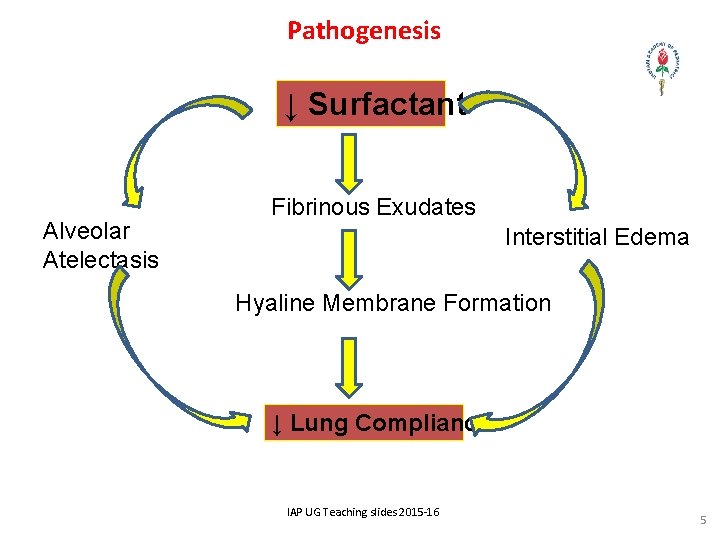
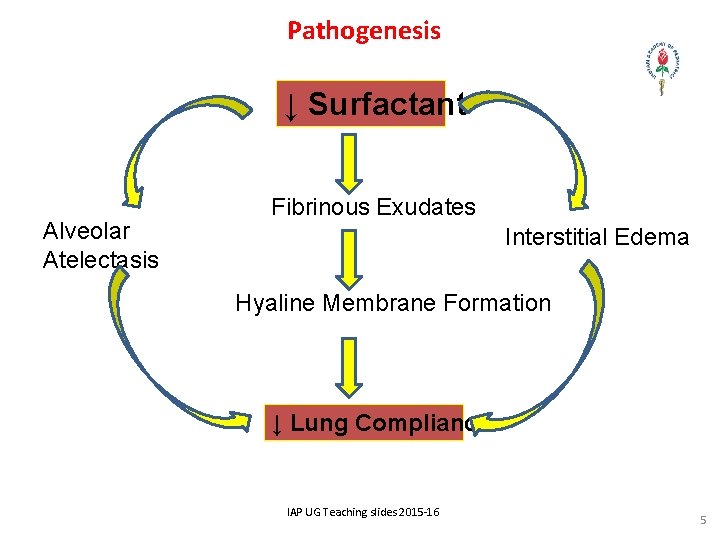
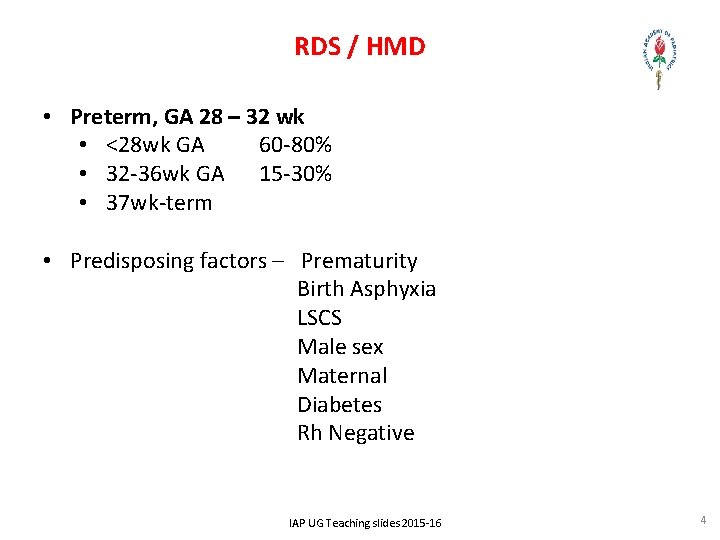
Pathogenesis ↓ Surfactant Alveolar Atelectasis Fibrinous Exudates Interstitial Edema Hyaline Membrane Formation ↓ Lung Compliance IAP UG Teaching slides 2015 -16 5
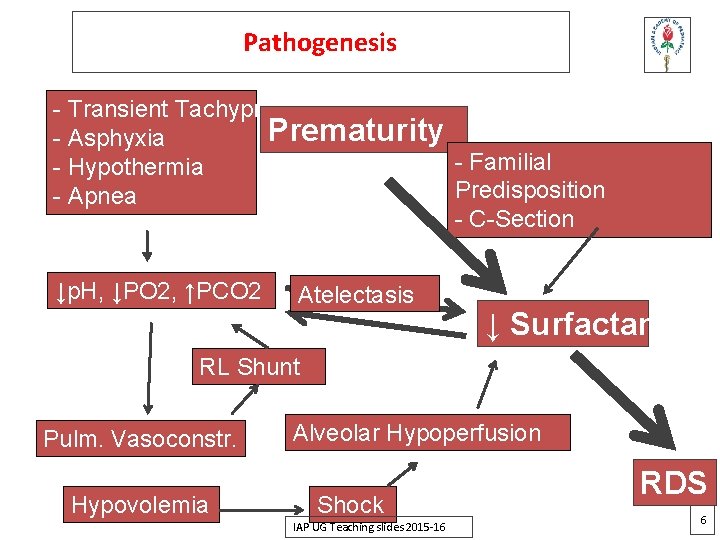
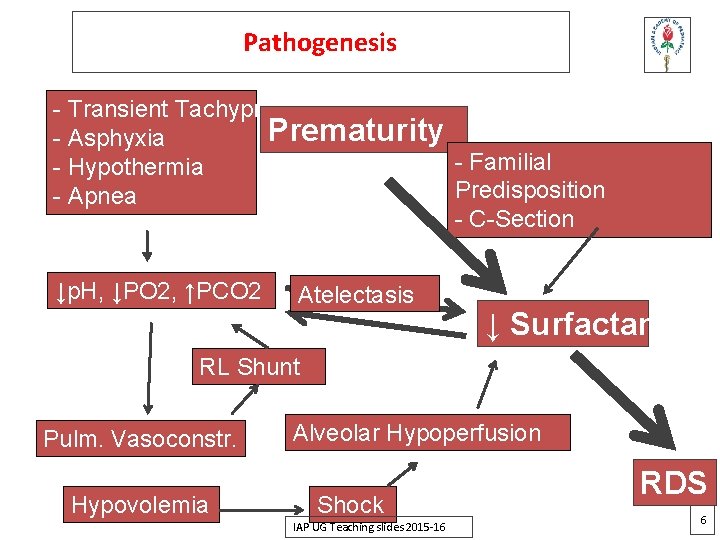
Pathogenesis - Transient Tachypnea Prematurity - Asphyxia - Familial - Hypothermia Predisposition - Apnea - C-Section ↓p. H, ↓PO 2, ↑PCO 2 Atelectasis ↓ Surfactant RL Shunt Pulm. Vasoconstr. Hypovolemia Alveolar Hypoperfusion Shock IAP UG Teaching slides 2015 -16 RDS 6
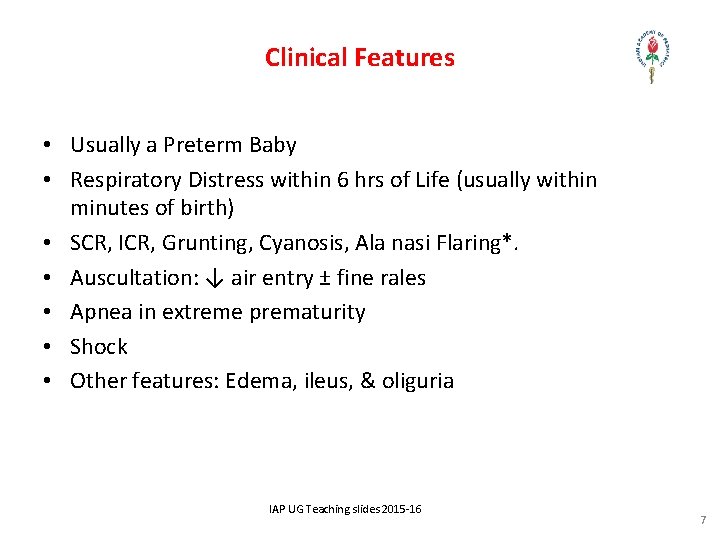
Clinical Features • Usually a Preterm Baby • Respiratory Distress within 6 hrs of Life (usually within minutes of birth) • SCR, ICR, Grunting, Cyanosis, Ala nasi Flaring*. • Auscultation: ↓ air entry ± fine rales • Apnea in extreme prematurity • Shock • Other features: Edema, ileus, & oliguria IAP UG Teaching slides 2015 -16 7
Clinical Course • Severe cases develop respiratory failure needing ventilation / surfactant / CPAP – and may tire and develop apnea / die if care not offered • Mild cases – can be managed with only oxygen • Symptoms progress to peak in 3 days • Improvement thereafter (often heralded by spontaneous diuresis) IAP UG Teaching slides 2015 -16 8
Differential Diagnosis • Early onset sepsis / congenital Pneumonia • TTNB • CHD (TAPVC) IAP UG Teaching slides 2015 -16 9
Investigations • Amniotic fluid – Lecithin to Sphingomyelin ratio • (L/S) ratio • >2. 5 = 0. 5%, >2 =10% , • 1. 5 -2 = 15 -20%, <1. 5 = 60% risk of developing RDS • Blood & Meconium depress mature L/S ratio and may elevate immature ratio • Exceptions : IDM, Asphyxia- can develop RDS even if ratio ok • Phosphatidylglycerol = present • Saturated Phosphatidylcholine (SPC) > 500 ug/dl IAP UG Teaching slides 2015 -16 1 0
Investigations – Cont. . . Gastric Aspirate – Shake Test • Mix 0. 5 ml of gastric aspirate & 0. 5 ml of absolute alcohol • Shake for 15 seconds & allow the solution to settle for 15 seconds • If no bubbles – 60 % chances of RDS • Small bubbles to the extent of 1/3 rd of the circle of the test tube – 20% chances of RDS • All around the circle – bubbles in two circle in some places – bubbles in two row & above <1% chances of RDS IAP UG Teaching slides 2015 -16 1 1
Investigations (cont…) • Lamellar body counts (phospholipid “packages” produced by type 2 alveolar cells) in amniotic fluid • >50, 000 lamellar bodies/μL → lung maturity IAP UG Teaching slides 2015 -16 1 2
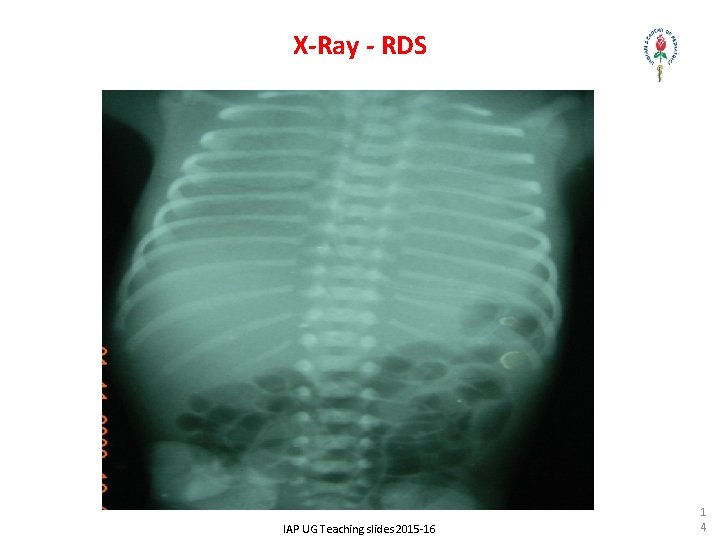
Investigations - Contd. . • X-Ray Chest: • Reticulo granular pattern • Air bronchogram • Ground Glass opacity • White wash appearance in severe RDS IAP UG Teaching slides 2015 -16 1 3
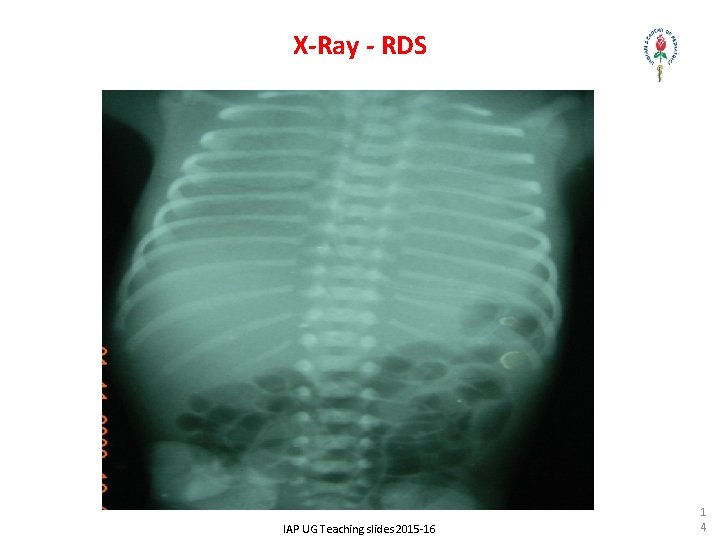
X-Ray - RDS IAP UG Teaching slides 2015 -16 1 4
Investigations – Cont. . . Related to Acute Care & DD • Blood Gases – hypoxia and hypercarbia • Echo – for associated PDA / exclude CHD • Supportive care • Cranial Ultra sonography • Blood Chemistry • Sepsis Screening IAP UG Teaching slides 2015 -16 1 5
PREVENTION • Induction of labour should preferably be delayed till lung maturity • Prevent fetal asphyxia by antenatal & intranatal monitoring • Antenatal Steroids (to Mother) • Betamethasone 12 mg IM 2 doses in 24 hrs interval (preferred) • Dexamethasone 4 doses in 12 hrs interval IAP UG Teaching slides 2015 -16 1 6
Antenatal steroids • Must be given to all mothers in preterm labor (<37 weeks) • Decreases incidence of severe RDS, IVH, mortality by half • Can be given even if mother has HTN, diabetes IAP UG Teaching slides 2015 -16 1 7
Treatment SPECIFIC – Surfactant Therapy • Types of surfactants: • Natural – Bovine, Calf, Porcine • Synthetic • Timing of intervention: • Prophylaxis (before onset of RD) • Treatment (rescue – after onset of RD) IAP UG Teaching slides 2015 -16 1 8
Surfactant therapy • Given in to trachea • Produces immediate improvement in lung condition • Relatively costly drug • No serious side effects in immediate period / long term IAP UG Teaching slides 2015 -16 1 9
Supportive Rx • Ventilatory Support - CPAP & Positive pressure ventilation • Maintain Pa. O 2 50 -80 mm Hg (Sp. O 2 85 -95%) • Maintain Pa. CO 2 45 -55 mm Hg • O 2 should be warm, humidified, & delivered by a blender • Monitor O 2 by concentration IAP UG Teaching slides 2015 -16 2 0
Supportive Rx (Cont…) • Shock – Fluids, inotropes • Temperature Control • Nutrition – TPN • Sepsis Rx – Antibiotics till infection is ruled out • Developmental friendly nursing policy IAP UG Teaching slides 2015 -16 2 1
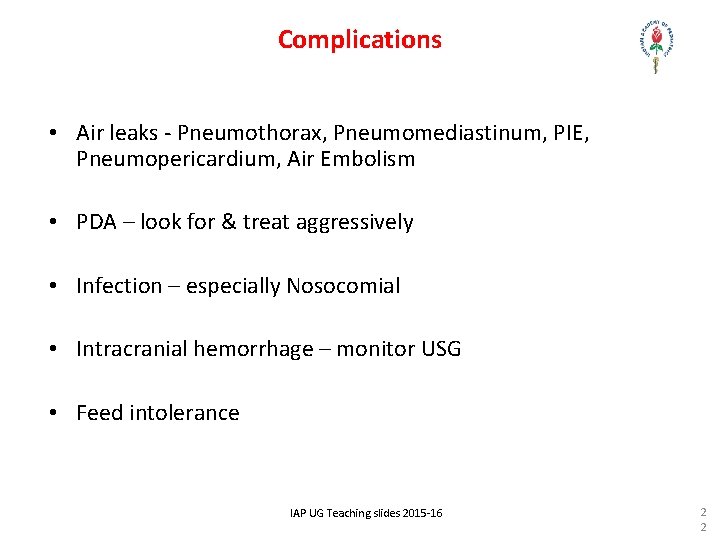
Complications • Air leaks - Pneumothorax, Pneumomediastinum, PIE, Pneumopericardium, Air Embolism • PDA – look for & treat aggressively • Infection – especially Nosocomial • Intracranial hemorrhage – monitor USG • Feed intolerance IAP UG Teaching slides 2015 -16 2 2
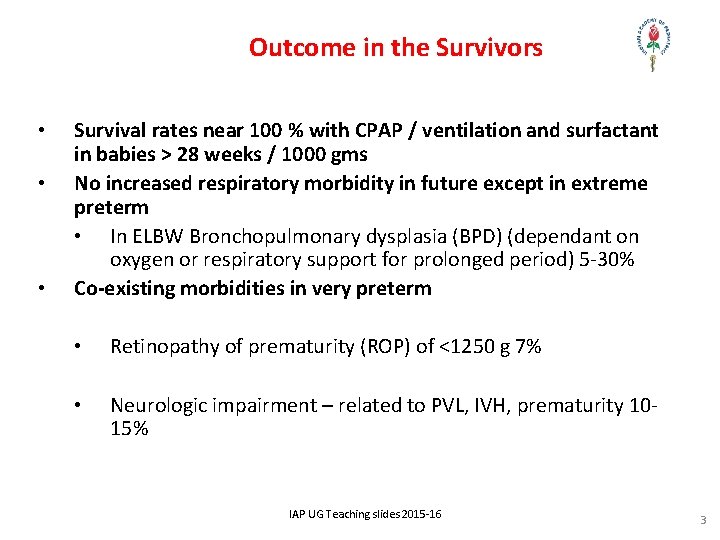
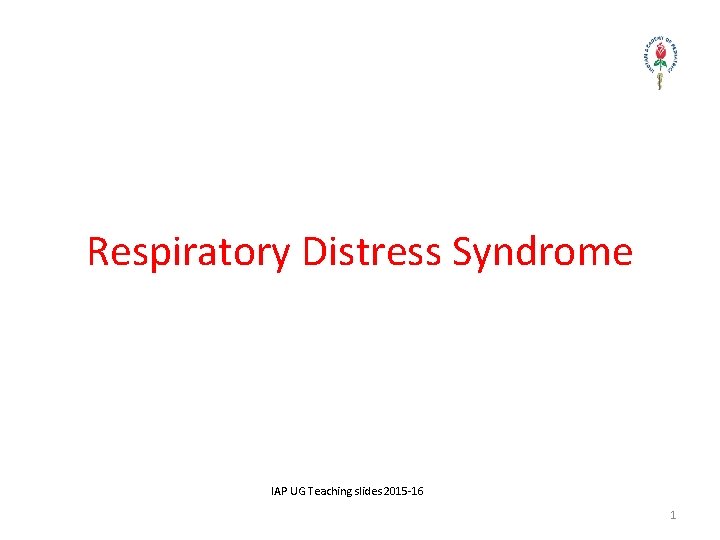
Outcome in the Survivors • • • Survival rates near 100 % with CPAP / ventilation and surfactant in babies > 28 weeks / 1000 gms No increased respiratory morbidity in future except in extreme preterm • In ELBW Bronchopulmonary dysplasia (BPD) (dependant on oxygen or respiratory support for prolonged period) 5 -30% Co-existing morbidities in very preterm • Retinopathy of prematurity (ROP) of <1250 g 7% • Neurologic impairment – related to PVL, IVH, prematurity 1015% IAP UG Teaching slides 2015 -16 3
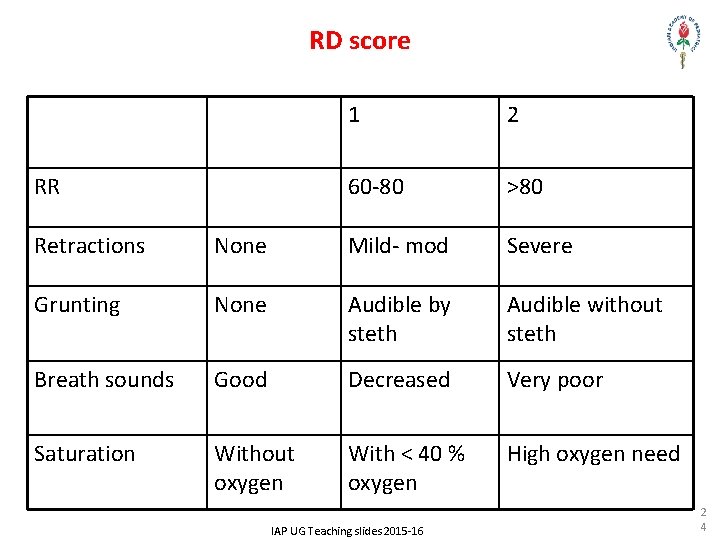
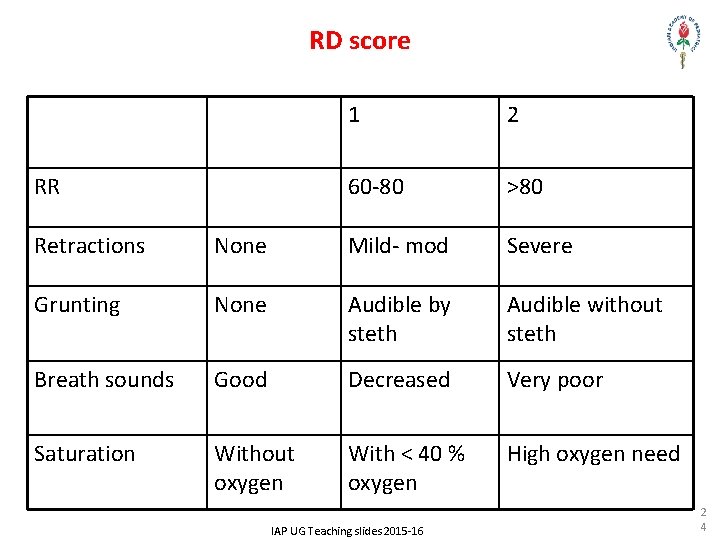
RD score RR 1 2 60 -80 >80 Retractions None Mild- mod Severe Grunting None Audible by steth Audible without steth Breath sounds Good Decreased Very poor Saturation Without oxygen With < 40 % oxygen High oxygen need IAP UG Teaching slides 2015 -16 2 4
IAP UG Teaching slides 2015 -16 2 5
 Bidextrous approach
Bidextrous approach Iap ug teaching slides
Iap ug teaching slides Sarnat score
Sarnat score Ug teaching slides
Ug teaching slides Iap ug teaching slides
Iap ug teaching slides Downe score
Downe score Respiratory distress
Respiratory distress Respiratory distress
Respiratory distress Respiratory distress nasal flaring
Respiratory distress nasal flaring Respiratory zone of the respiratory system
Respiratory zone of the respiratory system A small child slides down the four frictionless slides
A small child slides down the four frictionless slides Change in energy quick check
Change in energy quick check Culturally responsive teaching and the brain powerpoint
Culturally responsive teaching and the brain powerpoint Macro teaching is a scaled down teaching
Macro teaching is a scaled down teaching Write a short note on stress management
Write a short note on stress management Pearlin theory
Pearlin theory Leonard pearlin’s theory of psychological distress
Leonard pearlin’s theory of psychological distress Nst vs ctg
Nst vs ctg The damsel in distress archetype examples
The damsel in distress archetype examples Temptress archetype examples
Temptress archetype examples Psychology, mental health and distress
Psychology, mental health and distress Nursing responsibility of tocolytics
Nursing responsibility of tocolytics Distress words survival
Distress words survival Distress signal x1
Distress signal x1 Fetal distress definition
Fetal distress definition Konsep spiritual dalam keperawatan
Konsep spiritual dalam keperawatan