Respiratory Distress in newborn Examination STOPS Sensorium Temperature
Respiratory Distress in newborn
Examination – STOPS • • • Sensorium Temperature Oxygenation Perfusion Sugar
Respiratory Distress Syndrome Oxygenation n Respiratory rate >60/min n Recessions (ICS, SCR) n Expiratory grunt n Flarinf of alanasi n Presents within 4 hours of birth.
Respiratory Distress Syndrome Oxygenation n Chest expansion n Air Entry n Sp. O 2 in air Sp. O 2 – pre ductal Sp. O 2 – post ductal n Paradoixcal breathing n n

SCORE FOR RESPIRATORY DISTRESS Downe’s score – Term babies score > 6 – severe distress Score 0 <60 1 60 -80 2 >80 Central cyanosis None with 40% Fi. O 2 Needs>40% Fi. O 2 Retractions None Mild Severe Grunting None Minimal Obvious Air entry Good Decreased Very poor Resp rate
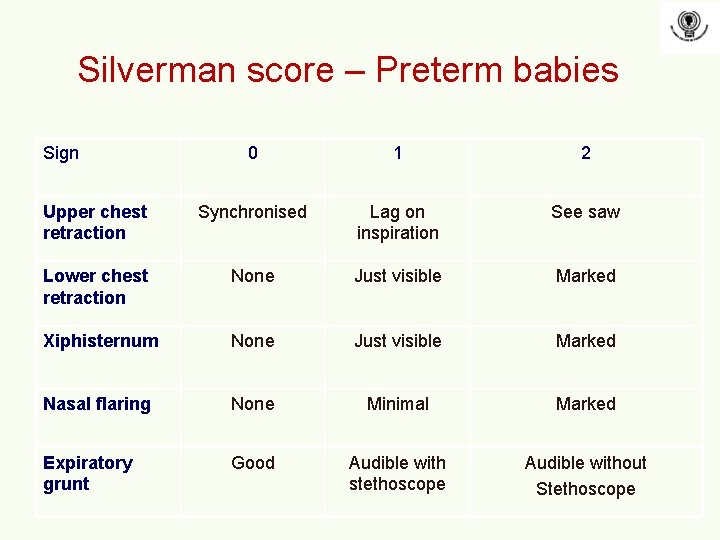
Silverman score – Preterm babies Sign 0 1 2 Upper chest retraction Synchronised Lag on inspiration See saw Lower chest retraction None Just visible Marked Xiphisternum None Just visible Marked Nasal flaring None Minimal Marked Expiratory grunt Good Audible with stethoscope Audible without Stethoscope
Examination Perfusion n n n Heart rate Heart sounds – prominent side Pulse rate Femoral pulse CRFT NIBP
Examination S n n Sugar CBG
CAUSES
Respiratory Causes • • Sdd TTN MAS Congenital Pneumonia (Viral / Bacterial) Pneumothorax CDH Aspiration – TOF Cystic adenomatous malformation
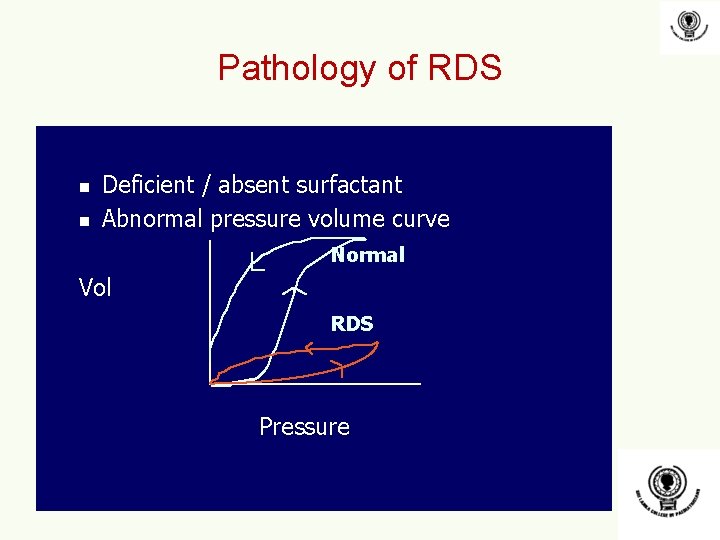
Pathology of RDS n n Deficient / absent surfactant Abnormal pressure volume curve Normal Vol RDS Pressure
Management of respiratory Causes n Lung recruitment n n Improve oxygenation n PEEP titration Non invasive ventilation IMV Head box oxygenation Nasal prong Improve ventilation
Saturation Targets n Sick Term babies 90 – 93% n Preterm 85 -92%
Respiratory Causes • • Sdd – CPAP / Surfactant TTN – CPAP Congenital Pneumonia – CPAP + antibiotics Viral Pneumonia Pneumothorax – Needle thrococentesis CDH – Ventilation + surgical refferal Aspiration - CPAP Cystic adenomatous malformation - /+ Surgery
Cardiac Causes • • • Coaction of aorta PDA PPHN Heart failure Cyanotic Congenital heart diseases Pneumopericardium
Investigations • • • CXR Septic screen Arterial Blood Gas 2 D ECHO USS brain
Sdd • • • Self limiting Ante natal steroids Postnatal surfactant – recue therapy Lung recruitment Minimizing V/Q mismatch
Indications for surfactant n n 27 weeks and above > 900 grams
Surfactant dosing n n n Curosurf 100 mg/kg (1 ml/kg) Survanta 100 mg/kg (4 ml/kg given as 2 aliquots) Second dose 12 hours later
Adverse effects of surfactant • Transient hypoxia, bradycardia • Transient BP, CBFV, cerebral activity on EEG • Pulmonary Hemorrhage
Combined antenatal steroids & postnatal surfactant therapy Significant decrease in incidence of RDS, PTX, IVH, PDA, and Mortality (White et al ’ 95, Jobe et al ’ 93)
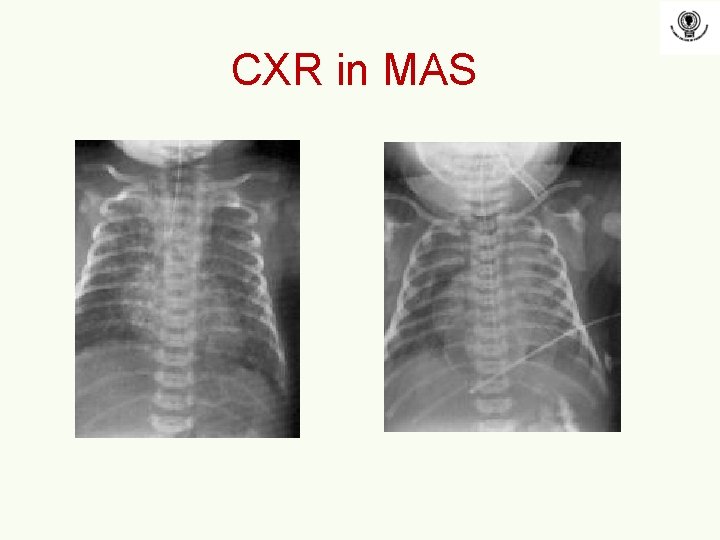
CXR in MAS
Clinical features of MAS n Tachypnea ( 60 to 100/min) n Hyper-inflated chest n Flaring of alae nasi n ± Grunt and Retraction n Meconium staining of umbilical cord, nails & skin n Pushed down Liver and Spleen CXR
Complications of MAS n Respiratory failure (hypoxia, acidosis, p. CO 2) n PPHN n Secondary to hypoxia or acidosis n Chronic hypoxia : pulmonary artery muscularization n Air leaks (pneumothorax, pneumomediastenum, PIE) n Secondary infections n Prolonged oxygen requirement (5% at 1 month) n Long term morbidities n 40% asthma, bronchospasm, abnormal PFTs
- Slides: 24