Respiratory Arrest Versus Cardiac Arrest PALS Presented by
Respiratory Arrest Versus Cardiac Arrest (PALS) Presented by Danyel Dorn RN, MSN, CPN, Clinical Nurse Educator-Pediatric Service Line
Purpose • Nurses must recognize deterioration and shock in the pediatric patient and identify priorities in assessment and management of the ill or injured child. The Nurse caring for the pediatric patient must also demonstrate cardiopulmonary resuscitation using PALS guidelines. Completion of this chapter does not indicate completion of the AHA PALS certification program.
Competency Statement • The perianesthesia registered nurse will be able to identify and provide appropriate emergency care in the perianesthesia setting for the deteriorating pediatric patient.
Priorities • Requires rapid recognition of deterioration and systematic intervention • Cardiopulmonary arrest in pediatric PACU patients occurs most commonly in children less than 5 years old (especially infants) and pediatric patients with comorbidities • The cause of most arrests is respiratory
Primary Assessment • • Airway Breathing Circulation Disability
AVPU Scale • • • A = alert V = voice P = pain U = unresponsive Pediatric response scale, pupil reaction and blood glucose • The AVPU scale has four possible outcomes
AVPU Outcomes • Alert: The patient is fully awake (although not necessarily oriented). This patient will have spontaneously open eyes, will respond to voice (although may be confused) and will have bodily motor function • Voice: The patient makes some kind of response when spoken to, which could be in any of the three component measures of eyes, voice or motor (ex: patient’s eyes open on being asked “are you ok? ”) The response could be as little as a grunt, moan or slight move of a limb when prompted by the voice of the rescuer
AVPU Outcomes • Pain: The patient makes a response on any of the three component measures as a response to painful stimulus (squeezing fingers) • A patient with some level of consciousness (a fully conscious patient would not require a pain stimulus) may respond by using his/her voice, moving their eyes, or moving part of their body (including posturing)
AVPU Outcomes • Unresponsive: This outcome is recorded if the patient does not give any eye, voice or motor response to voice or pain
Pediatric Information • PALS defines hypoglycemia as a blood glucose < mg/dl in preterm and term neonates and < 60 mg/dl for all other infants, children, and adolescents (See your institutional policy on definition of hypoglycemia) • Prolonged environmental exposure ▫ assess skin and core temperature �Decrease in core temperature could lead to bradycardia and/or asystole
Pals Information • Activate an emergency response • Provide high quality CPR when indicated - Compressions at least 100/minute, depth 1/3 AP diameter, allow complete chest recoil after each compression, minimize interruptions in compressions, avoid excessive ventilation - Two rescuer CPR in pals = 15: 2 - Monitor et. CO 2 for quality of CPR, should be greater than 15 mm Hg
Pals Information • Ensure early use of defibrillator for shockable rhythms (VF/VT) at 2 -4 J/kg • Adult AEDs should ideally be used only in children over 8 years or over 25 kg • For children less than 8 years or less than 25 kg, use manual defibrillation, an AED with attenuated dose or, if nothing else is available, an adult AED
Secondary Assessment • • • S = signs and symptoms A = allergies M = medications P = past medical history, injuries, illnesses L = last meal/intake E = events leading up to the situation or illness
Respiratory Distress Vs. Failure • Increased work of breathing, irregular breathing and inadequate respiratory effort • Resp. Failure include one or more of the following: very rapid or inadequate respiratory rate, significant or inadequate respiratory effort, low oxygen saturation despite high flow oxygen, bradycardia (ominous sign), cyanosis, and decreased level of consciousness
Upper Airway Obstruction • • • Increased respiratory rate and effort Decreased air movement Stridor, barking cough Snoring or gurgling Hoarseness Tx: 100% O 2, position for comfort, anticipate IM epinephrine for anaphylaxis and additional interventions as indicated including racemic epinephrine and IV dexamethasone, CPAP, CXR
Lower Airway Obstruction • • • Increased respiratory rate and effort Decreased air movement Prolonged expiration Wheezing TX: albuterol nebulizer, CPAP, Steroids, CXR
Lung Tissue Disease • • • Increased respiratory rate and effort Decreased air movement Grunting, crackles Ex: pneumonia TX: 100% O 2, antibiotics, albuterol, CPAP
Disordered Control of Breathing • Irregular respiratory pattern • Inadequate or irregular respiratory depth and effort • Normal or decreased air movement, signs of upper airway obstruction • Ex: poison ingestion • TX: Support ventilation as needed, treat underlying cause
Shock • Hypovolemic or obstructive shock (tension pneumothorax, cardiac tamponade, massive pulmonary embolism, ductal dependent congenital heart lesion)
Poor Perfusion • • Tachycardia Weak peripheral pulses Delayed capillary refill time-mottling Pallor or cyanosis Cool skin Changes in level of consciousness Decreased urine output
Distributive Shock • Signs of poor perfusion • Potential warm flushed skin with brisk capillary refill and bounding pulses • Potential weak pulses (warm shock) • Petechial or purpuric rash (septic shock)
Cardiogenic/Compensated Shock • Signs of poor perfusion • Signs of congestive heart failure (shortness of breath, weakness, fatigue, edema) • Compensated Shock = signs of poor perfusion and normal blood pressure
Hypotensive Shock • Signs of poor perfusion and low blood pressure • Tachycardia is an early sign of shock in children • Hypotension is a late and ominous sign of shock in children whose vasomotor tone and the ability to vasoconstrict allows them to maintain a normal BP in the early stages of shock
Treatment of Shock • Hypovolemic Shock = provide high flow oxygen as indicated, initiate 20 ml/kg isotonic crystalloid rapid IV bolus, repeat as necessary until improved BP, heart rate and distal pulses • Obstructive Shock = 100% Oxygen, consider DOPE (displacement, obstruction, pneumothorax, equipment failure), thoracostomy, chest tube placement, fluid resuscitation
Treatment of Shock • Distributive Shock (sepsis or anaphylaxis) = 20 ml/kg isotonic crystalloid rapid bolus-> repeat as necessary until improved BP, heart rate and distal pulses, obtain blood cultures if stable and administer antibiotics for sepsis, administer epinephrine and steroids for anaphylaxis, anticipate vasoactive infusion if shock is fluid refractory. • Cardiogenic Shock = high flow oxygen, 5 -10 ml/kg isotonic crystalloid IV bolus over 10 -20 minutes, prepare vasoactive or inotropic infusions for persistent shock.
Cardiac Rhythm Disturbances • Bradycardia (symptomatic): heart rate slower than normal for child’s age or baseline (usually < 60 bpm, with cardiopulmonary compromise (shock combined with respiratory distress or failure) despite oxygenation and ventilation. • In children, bradycardia is usually the result of hypoxia
Cardiac Rhythm Disturbances • Tachycardia: heart rate that is fast compared with the normal heart rate for a child’s age • Tachyarrhythmia's: fast abnormal rhythms originating either in the atria or the ventricles of the heart ▫ Stable: normal BP, perfusion and mental status ▫ Unstable: altered mental status, respiratory distress/failure, hypotension and signs of shock
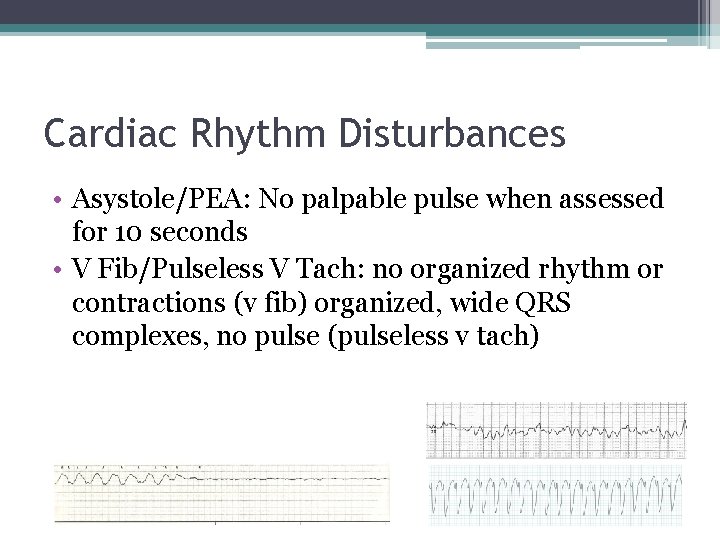
Cardiac Rhythm Disturbances • Asystole/PEA: No palpable pulse when assessed for 10 seconds • V Fib/Pulseless V Tach: no organized rhythm or contractions (v fib) organized, wide QRS complexes, no pulse (pulseless v tach)
Management of Cardiac Rhythm Disturbances • Bradycardia: 100% O 2, ventilation, 12 lead ECG, CPR for symptomatic bradycardia, IV Epinephrine 0. 01 mg/g (0. 1 ml/kg of 1: 10, 000) • Tachyarrhythmia: SVT-Stable: initiate vagal maneuver, rapid push adenosine 0. 1 mg/kg, may repeat adenosine at 0. 2 mg/kg. Unstable: immediate cardioversion 0. 5 -1 J/kg
Management of Cardiac Rhythm Disturbance • Asystole/PEA: high quality CPR, reassess rhythm every 2 minutes, IV/IO Epinephrine 0. 01 mg/kg (0. 1 ml/kg of 1: 10, 000) repeat every 3 -5 minutes • Attempt to identify H’s & T’s (hypovolemia, hypoxia, hypothermia… …Toxins, tamponade, tension pneumothorax…)
Management of Cardiac Rhythm Disturbance • V Fib/Pulseless V Tach: CPR, reassess rhythm every 2 minutes, defibrillate at 2 -4 J/kg, repeat every 2 minutes as necessary, IV/IO Epinephrine 0. 01 mg/kg (0. 1 ml/kg of 1: 10, 000), administer first dose after second rhythm check and repeat every 3 -5 minutes • Consider IV/IO Amiodarone 5 mg/kg bolus, may repeat up to two times
Care Post-Resuscitation • Aim for oxygen saturation 94 -99%; avoid hypoxemia and hyperoxemia, monitor et. CO 2, • Avoid hyperventilation which can cause cerebral vasodilation and increased intracranial pressure • Maintain aggressive hemodynamic support after return of spontaneous circulation • Treat hyperthermia, avoid hyperglycemia and hypoglycemia, monitor for seizures and treat aggressively, EEG may be used as seizures can be clinical or subclinical.
Reference • ASPAN (2016). A Competency Based Orientation and Credentialing Program for the Registered Nurse Caring for the Pediatric Patient in the Perianesthesia Setting.
Answers 1. C 2. B 3. A 4. C 5. B 6. C 7. B 8. A 9. B 10. A
- Slides: 34