Respiratory anatomy and Physiology Caia Francis Chair RCN

- Slides: 24
Respiratory anatomy and Physiology Caia Francis Chair RCN Respiratory Forum Senior Lecturer- Respiratory Specialist 0117 32 88631 caia. francis@uwe. ac. uk
Outline of session 4 Review and orientation to respiratory anatomy and physiology. 4 Learning outcomes: – Understand fundamental law of diffusion and apply it to gas exchange. – Understand the mechanics of breathing and how this is influenced to maintain ‘normal’ respiratory functioning.
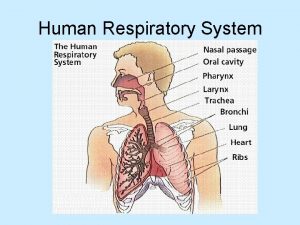
Respiratory Physiology. 4 Lung is for gas exchange. 4 Prime function is to allow oxygen to move from the air into the venous blood and carbon dioxide to move out. 4 Metabolizes some compounds, filters toxic materials from the circulation and acts as a reservoir for blood.
4 Oxygen and carbon dioxide move between air and blood by simple diffusion, i. e. from an area of high to low partial pressure. (Fick’s law of diffusion). Blood- gas barrier is exceedingly thin and has an area of between 50 - 100 m 2. 4 Large surface area is obtained by wrapping capillaries around air sacs (form alveoli). 300 million alveoli in human lungs.
4 Airways consist of a series of branching tubes, becoming narrower, shorter and more numerous as they penetrate deeper into the lung. 4 Trachea divides into right and left main bronchi, divide into lobar, then segmental bronchi. This process continues down to terminal bronchioles, smallest airways outside the alveoli.
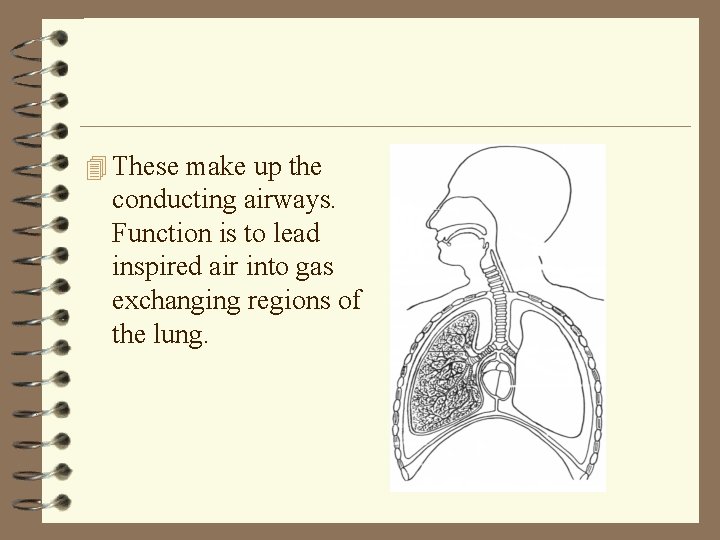
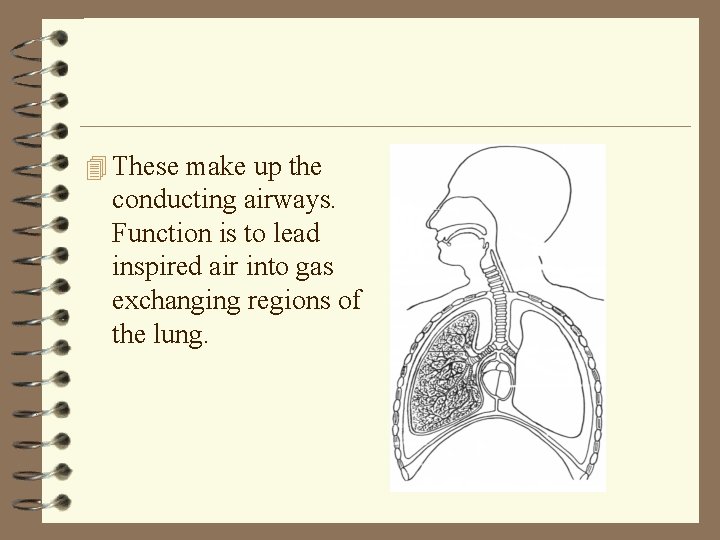
4 These make up the conducting airways. Function is to lead inspired air into gas exchanging regions of the lung.
4 Terminal bronchioles divide into respiratory bronchioles, finally arriving at the alveolar ducts, which are completely lined with alveoli. 4 This region is known as the respiratory zone. 4 Portion of lung distal to a terminal bronchiole forms an anatomical unit called acinus or lobule.
Ventilation 4 Static volumes of the lung can be measured mainly by spirometry. 4 Tidal volume 4 Vital capacity. 4 Minute volume. 4 But some gas remains in the lungs, residual volume and functional residual volume. Measured by body plesthysmography.
Ventilation -part 2 4 Volume exhaled with each breath is 500 ml, 15 breaths per minute; total volume leaving the lung each minute is? 4 500*15 = 7500 ml/min. 4 =Total ventilation or minute volume. 4 But not all air that passes lips reaches the aleovlar gas compartment where gas exchange occurs.
Anatomic dead space. 4 Volume of the conducting airways. 4 Normal value is circa 150 ml, but depends upon the size of inspiration and posture of subject.
Physiologic dead space. 4 Volume of the lung which does not eliminate CO 2. 4 In normal subjects this is nearly the same as anatomic dead space. 4 However in patients with lung disease the physiologic dead space may be considerably larger because of inequality of blood flow and ventilation within the lung.
Regional differences in ventilation (V) (upright person) 4 Upper zone lowest ventilation 4 Lower zone greatest ventilation.
Blood flow (Q) through the lungs 4 Regional variations in blood flow through the lungs. 4 Lowest blood flow 4 Highest blood flow.
In ‘well’ human 4 O 2 will have fully diffused across alveolar membrane to bind with Hb within 0. 25 s. 4 C 02 will have diffused across the alveolar membrane within 0. 25 s to be expired. 4 Blood will take 0. 5 s to traverse pulmonary capillary in association with alveolar sac.
Respiratory disease. 4 Asthma… mucus, airway thickening (hypertrophy) will increase ‘width’ of alveolar membrane and thus delay diffusion across membrane of both CO 2 and O 2. 4 COPD as above plus pulmonary and cardiac circulation problems will delay the above. 4 Genetic conditions eg cystic fibrosis will compromise blood flow through alveolar.
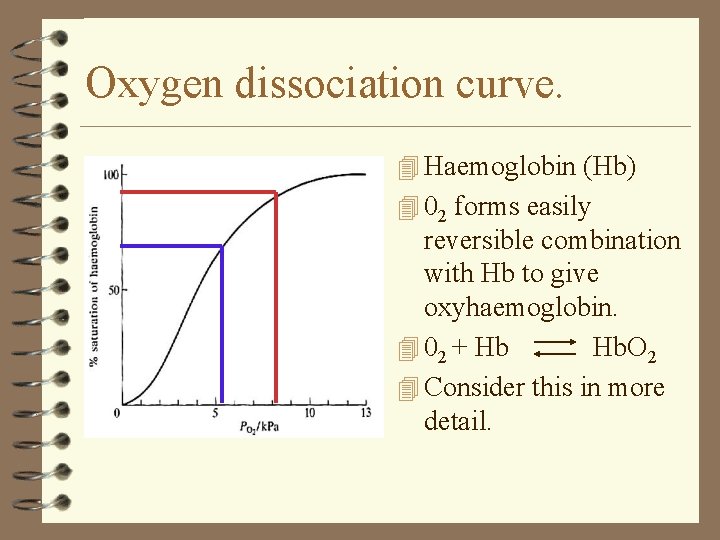
What happens once oxygen is delivered to the alveoli? 4 Oxygen dissociation curve. 4 Dissolved oxygen in blood, in some cases of significance in respiratory disease.
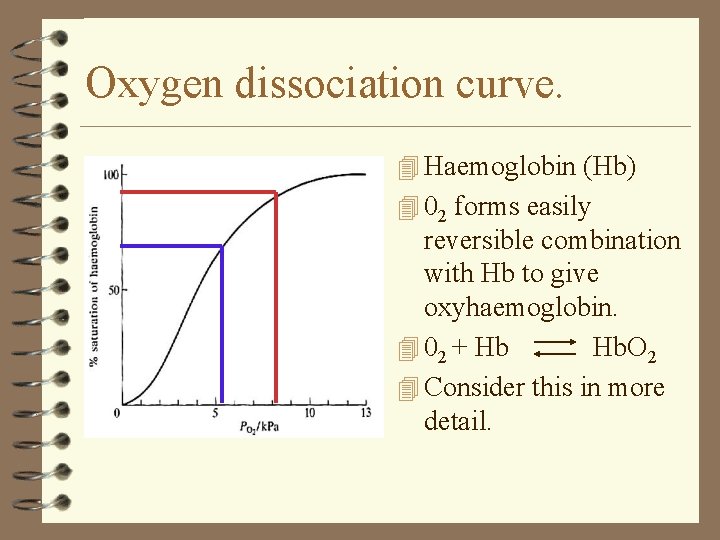
Oxygen dissociation curve. 4 Haemoglobin (Hb) 4 02 forms easily reversible combination with Hb to give oxyhaemoglobin. 4 02 + Hb Hb. O 2 4 Consider this in more detail.
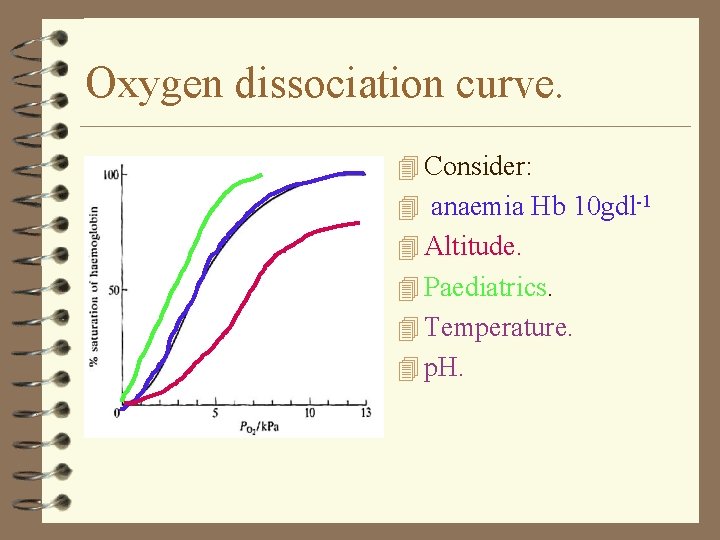
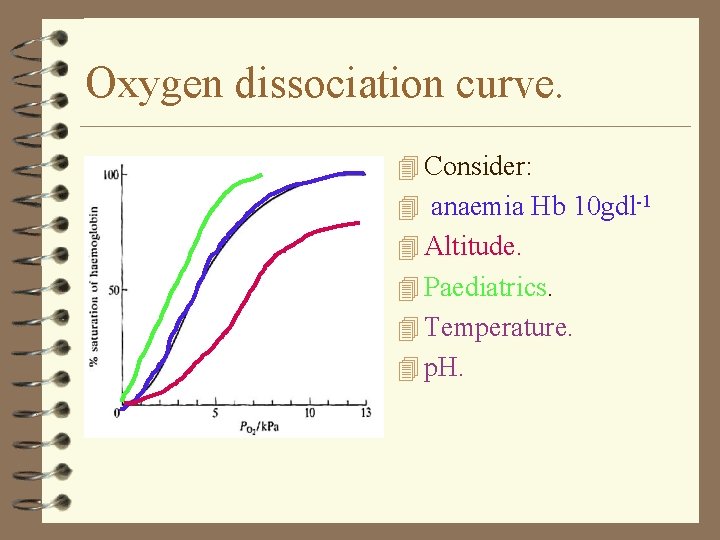
Oxygen dissociation curve. 4 Consider: 4 anaemia Hb 10 gdl-1 4 Altitude. 4 Paediatrics. 4 Temperature. 4 p. H.

Why do you need to know this? 4 Understand normal respiration and its measurement, function. 4 Establish a common frame of reference. 4 Revise known anatomy and physiology. 4 Introduce some issues of importance in respiratory disesase.
Mechanics of breathing. 4 Inspiration: lower intra-thoracic pressure to allow air to pass by diffusion into lungs. Usually only 1 cm. H 20 lower but in respiratory disease can be many times greater. 4 Diaphragm moving down in quiet breathing. 4 Expansion of rib cage in rapid deep breathing and using accessory muscles.
4 Expiration. Diaphragm returning to rest. 4 Ribs returning to status quo. 4 Increases slightly intra- thoracic pressure higher than the atmosphere and allows expiration. Usually only 1 cm. H 20 higher but in respiratory disease can be many times greater.
4 Positive end expiratory pressure (PEEP) aides in complete expiration. 4 Occurs in ‘well individuals’ easily and automatically.
References. 4 Francis C. , (2006) “Respiratory care” Blackwell 4 4 4 Publishing Oxford Jevon P. , Ewens B. , (Eds) (2002) “Monitoring the critically ill patient” Blackwell Science Oxford. Levitzky M. (2002) 7 th Edition “Pulmonary Physiology” Mc. Graw Hill New York. West J. , (2010) 8 th Edition. “Pulmonary Pathophysiology” Lippincott Williams & Wilkins London. West J. , (2009) 10 th Edition. “Respiratory Physiology the essesentials” Lippincott Williams & Wilkins London. Woodcock A. , Partridge M. , (1995) “Respiratory Handbook” Boehringer Ingelheim.
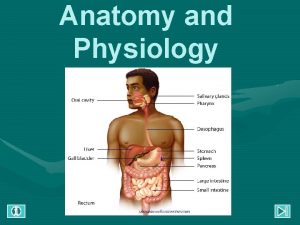
 Respiratory system of human
Respiratory system of human Integramais.caoxa
Integramais.caoxa Caia level 2 exam weights
Caia level 2 exam weights Caia torrent
Caia torrent Upper respiratory tract organs
Upper respiratory tract organs Bronchial tree
Bronchial tree Conducting zone of the respiratory system
Conducting zone of the respiratory system Tattoo anatomy and physiology
Tattoo anatomy and physiology Science olympiad anatomy and physiology
Science olympiad anatomy and physiology Incomplete flower
Incomplete flower Anatomy and physiology of bone
Anatomy and physiology of bone Stomach ulcer
Stomach ulcer Sheep liver lobes
Sheep liver lobes Podbřišek
Podbřišek Epigastric region
Epigastric region The blood anatomy and physiology
The blood anatomy and physiology Chapter 14 anatomy and physiology
Chapter 14 anatomy and physiology Endomysium
Endomysium Http://anatomy and physiology
Http://anatomy and physiology Waistline
Waistline Appendix anatomy and physiology
Appendix anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomical planes
Anatomical planes Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses