RESORPTION AND ITS MANAGEMENT BY DR SYED MUKHTAR
RESORPTION AND ITS MANAGEMENT BY DR SYED MUKHTAR UN NISAR ANDRABI ASSTT. PROF. CONSERVATIVE DENTISTRY & ENDODONTICS
INTRODUCTION • Defn: resorption is the loss of dental hard tissues as a result of clastic activities. • It may occur as a physiologic or pathologic phenomenon. • Root resorption in the primary dentition is a normal physiologic process except when the resorption occurs prematurely • Root resorption in the permanent dentition is a pathologic event; if left untreated, it may result in premature loss of the affected teeth

CLASSIFICATION • External • • • External inflammatory resorption Replacement resorption External/invasive cervical resorption • Internal • • Inflamatory resorption Replacement resorption
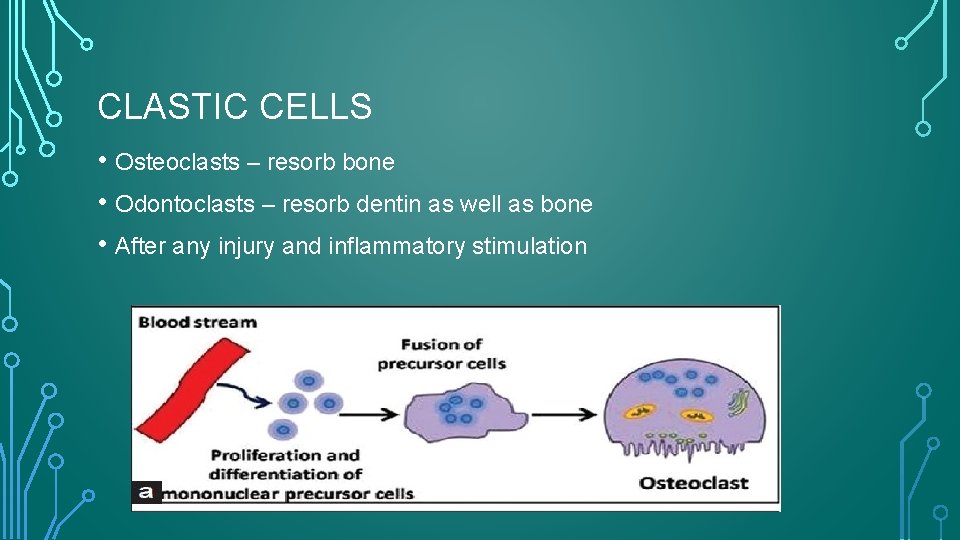
CLASTIC CELLS • Osteoclasts – resorb bone • Odontoclasts – resorb dentin as well as bone • After any injury and inflammatory stimulation
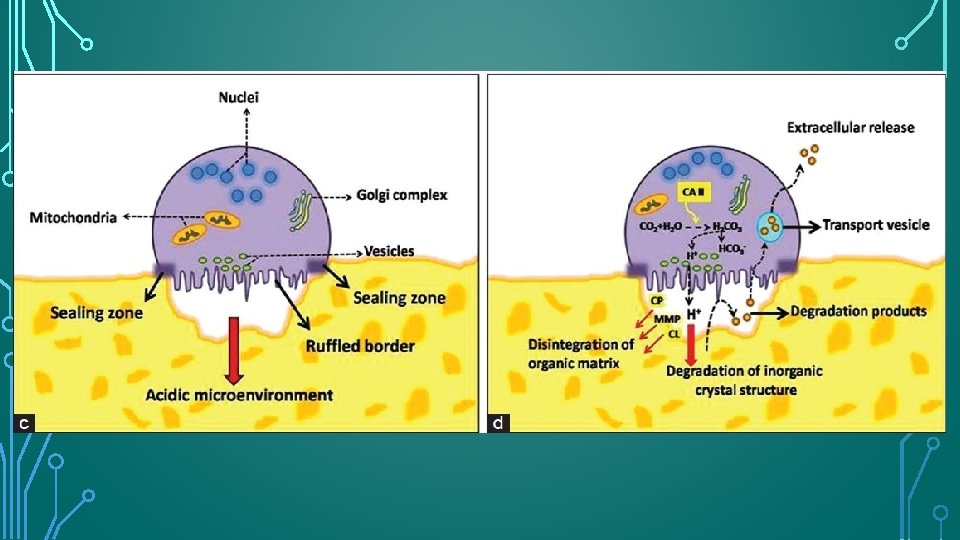
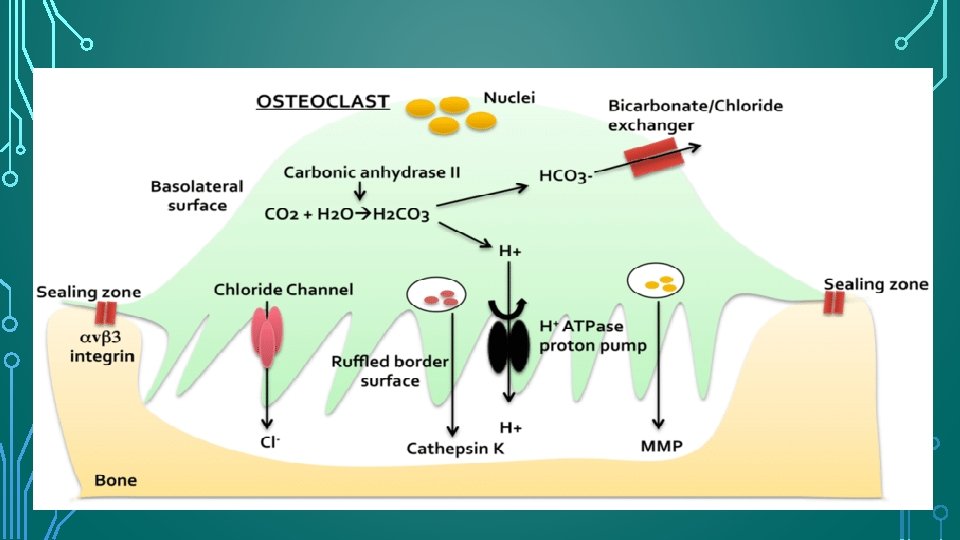
OSTEOCLAST FUNCTION • Osteoclasts are recruited to the site of. injury or irritation by the release of many proinflammatory cytokines. To perform their function, osteoclasts must attach themselves to the bone surface. On contact with mineralized extracellular matrices, osteoclast produces an organelle-free zone of sealing cytoplasm (clear zone) to achieve intimate contact with the hard tissue surface. • The clear zone surrounds a series of fingerlike projections (podosomes) of cell membrane, known as the ruffled border, beneath which bone resorption occurs. The resorptive area within the clear zone, therefore, is isolated from the extracellular environment, creating an acidic microenvironment for the resorption of hard tissues
ODONTOCLAST FUNCTION • Odontoclasts differ from osteoclasts in that they are smaller, have fewer nuclei, and have smaller sealing zones. • Odontoclasts and osteoclasts are functionally similar, have similar enzymatic properties, show similar cytologic features, and create resorption depressions, termed Howship lacunae.
• 119 • Wesselink et al. demonstrated that odontoclasts can simultaneously have two areas of ruffle border, which can resorb bone and hard dental tissue concurrently. • Based on this evidence, Jones and Boyd and Pierce have stated that odontoclasts and osteoclasts are effectively the same cell type, differing only in their respective substrata.
PROPERTY OF CLASTIC CELLS Osteoclasts and odontoclasts do not adhere to non-mineralized collagen matrices.

PROPERTY OF DENTIN 1. Predentin and odontoblastic cell layer 2. Precementum
MOLECULAR SIGNALING • the OPG/RANKL/ RANK transcription factor system that controls clastic functions during bone remodeling has also been identified in root resorption. • OPG- osteoprotegrin- prevents binding of RANKL to RANK- prevents activation of osteoclasts • RANKL: receptor activator of NF-κb ligand : responsible for activation of osteoclasts after binding to RANK on the surface of their precursors • RANK: present on the surface of osteoclastic precursors.
• Once the clastic cells have established contact with the cementum, any subsequent resorption is self-limiting unless the bound cells are subject to continued stimulation. • Progressive root resorption requires a source of stimulation for the resorbing cells. • Sources of stimulation can be: • persistent pressure and forces associated with continued orthodontic treatment; • persistent impacted teeth; untreated cysts, granulomas, and tumors; • Endodontic inflammation and/or infection; and • periodontal inflammation and/or infection
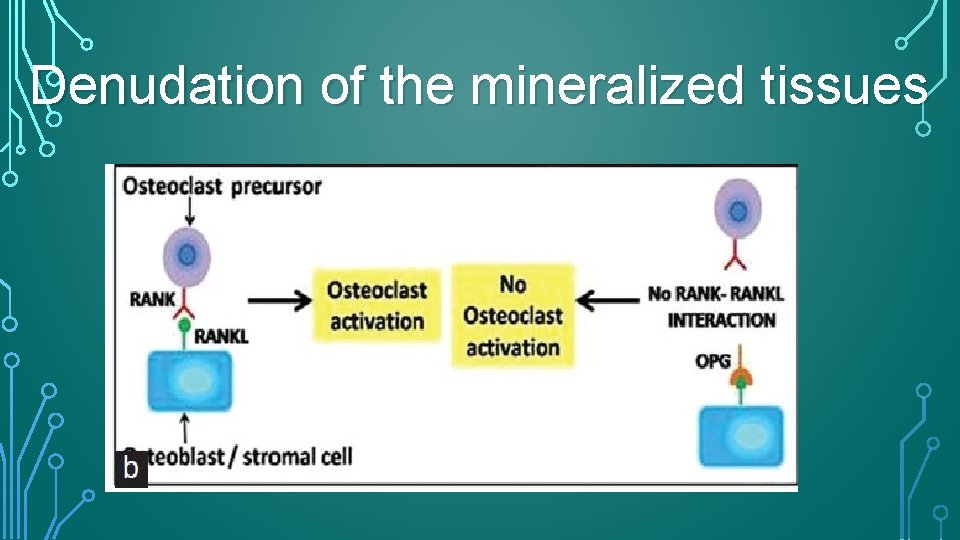
Denudation of the mineralized tissues
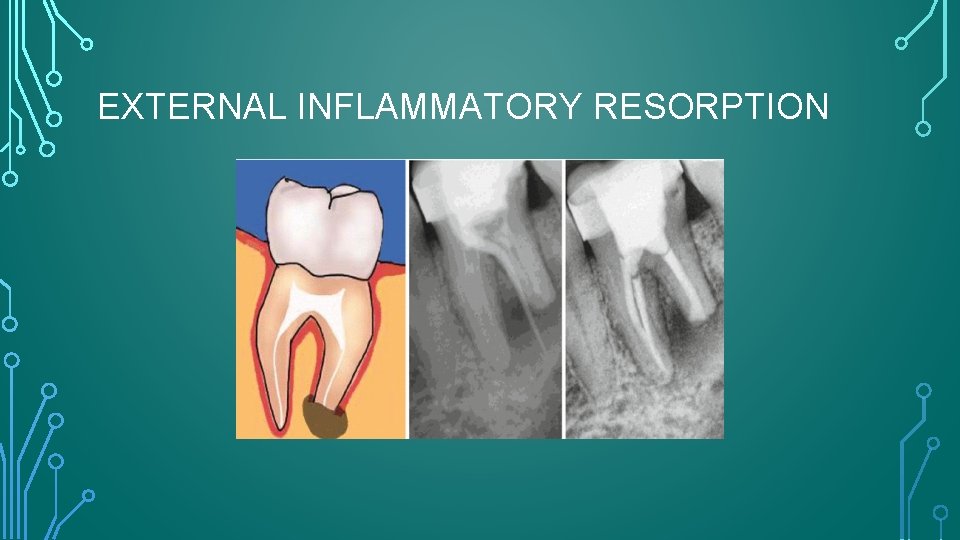
EXTERNAL INFLAMMATORY RESORPTION
• Traumatic dental injuries (e. g. , intrusion, lateral luxation, and avulsion) and subsequent replantation often result in contusion injuries to the periodontal ligament (PDL). • Damage to the precementum, with a resultant breach in its integrity, is the precipitating factor in all types of external resorption • The precise type depends on the severity of the initial injury, the stage of root development, and the pulp status of the affected tooth
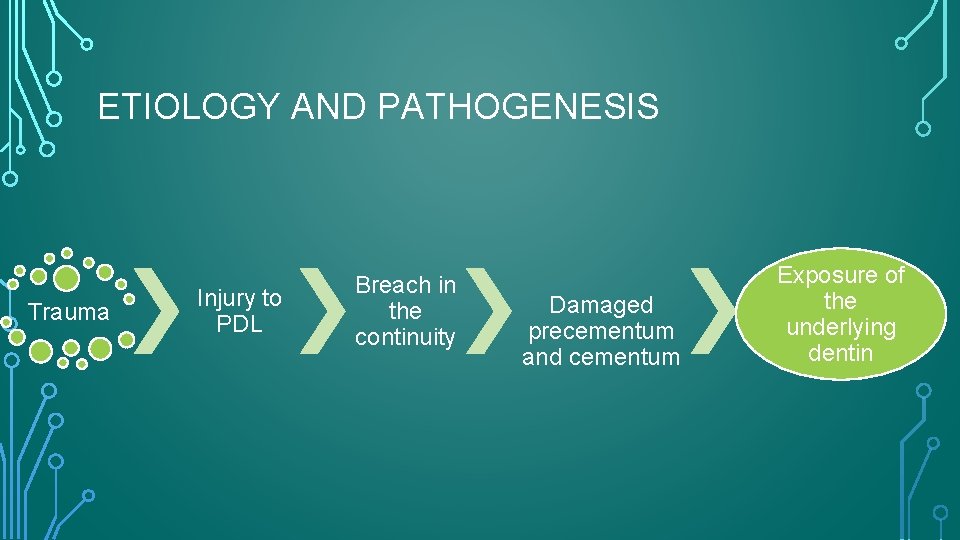
ETIOLOGY AND PATHOGENESIS Trauma Injury to PDL Breach in the continuity Damaged precementum and cementum Exposure of the underlying dentin
• Once the clastic cells have established contact with the cementum or dentin, any subsequent resorption is self limiting unless the cells are subject to continued stimulation.
EIR AND TRAUMATIC INJURIES • • Occurrence of EIR is correlated with the specific types of luxation injury: • • • Concussion injuries : 0% Andreasen and Vestergaard Pedersen prospectively followed up 637 permanent luxated teeth in 400 patients for up to 10 years and found EIR to be related as follows: Subluxation: 0. 5% Lateral luxation: 3% Extrusion: 6% Intrusion: 38% Avulsion: ♒�approx. ♒� 60%
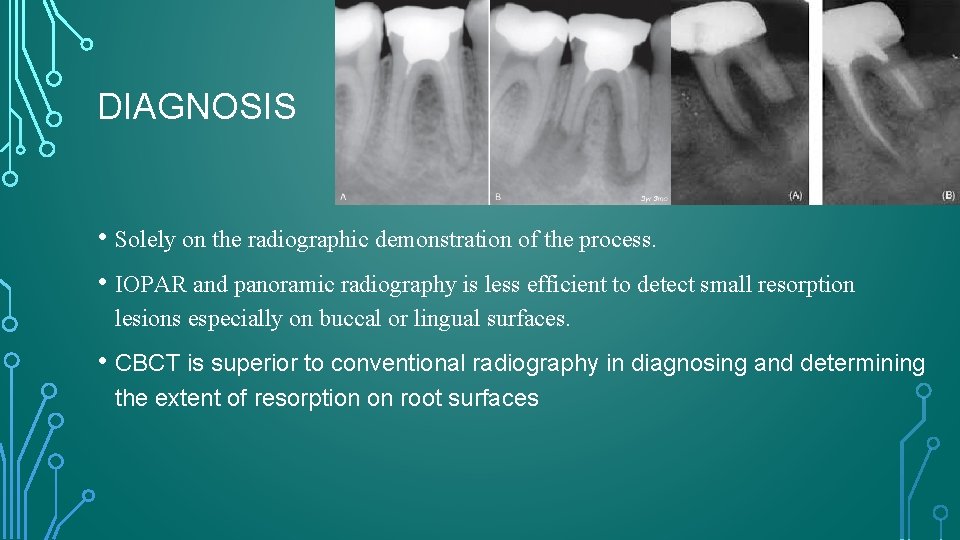
DIAGNOSIS • Solely on the radiographic demonstration of the process. • IOPAR and panoramic radiography is less efficient to detect small resorption lesions especially on buccal or lingual surfaces. • CBCT is superior to conventional radiography in diagnosing and determining the extent of resorption on root surfaces
Andersen et al. and Goldberg et al. concluded that “radiology is not a very accurate procedure for achieving an early and precise diagnosis of resorption defects. ” This study further reported that lesions created on the proximal root surfaces were easier to detect than those on the buccal/lingual surfaces and that the best results were achieved when multiple angled views and preoperative radiographs were available. A more recent study by the King’s College London (KCL) group concluded that CBCT was a reliable and valid method of detecting simulated EIR, and performed significantly better than intraoral periapical radiography.
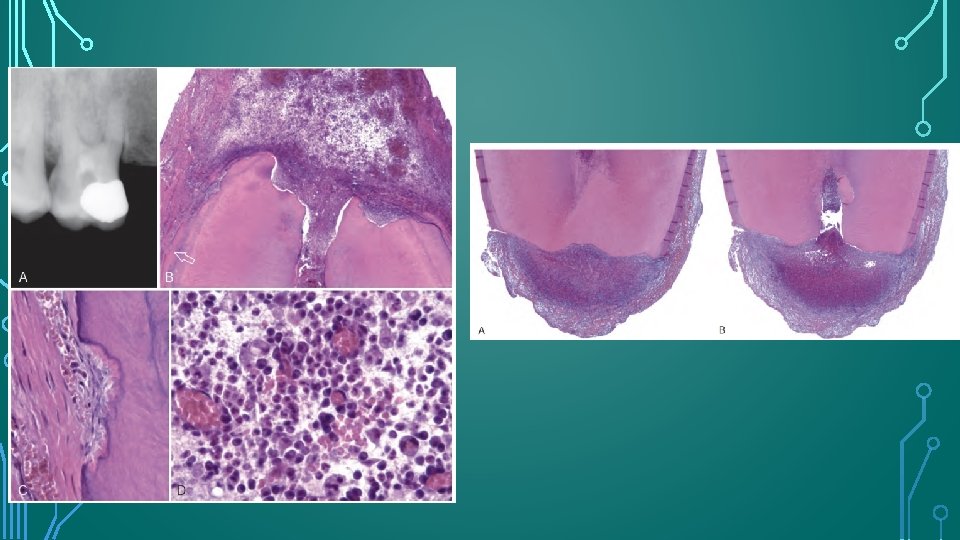
RADIOGRAPHIC FEATURES • Radiolucent , concave and sometimes ragged bowl shaped excavations • Associated radiolucency in the adjacent alveolar bone. • Complete loss of the lamina dura. • Can be seen as early as 3 - 4 weeks after traumatic dental injuries, and if it will develop , EIR always seen within 1 year after the injury. • Can have rapid onset and aggressive progression, such that complete resorption can occur within 3 months.
CLINICAL FEATURES • Look normal • But it will not respond positively to vitality testing • Advanced cases signs of pulpal or periapical periodontitis may be present.
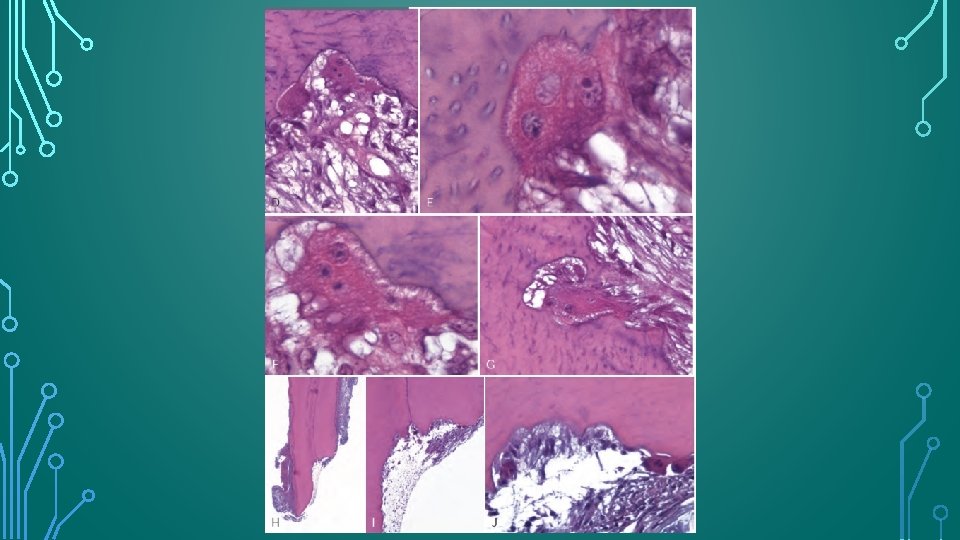
HISTOLOGIC APPEARANCE • Saucer or bowl shaped areas of resorption in both the cementum and dentin, with concomitant inflammation in the adjacent periodontal membrane. • Howship’s lacunae occupied by odontoclasts. • Intense inflammatory reaction in the periodontal membrane consists of a mixed-cell infiltrate that includes plasma cells, lymphocytes, and polymorphonuclear leukocytes in a granulation tissue matrix showing proliferation of capillaries. • EIR can be identified histologically 1 week after experimental replantation of teeth.
MANAGEMENT • Effective removal of the causal agent, the necrotic pulpal tissue in the root canal space. • It is essential to initiate root canal treatment as soon as radiographic signs of EIR are identified. • But in case of replanted teeth with closed apices , root canal should be carried out 7 - 10 days after replantation even if there are no radiographic signs of EIR. • Long term dressing of the root canal with calcium hydroxide may be beneficial in the treatment of established EIR.
• EIR differs from the surface resorption in that it is a progressive event that relies on the microbial stimulation from the infected necrotic pulp of the affected tooth for its progression.

REPLACEMENT RESORPTION • When extensive damage occurs to the innermost layer of the periodontal ligament , competitive healing events takes place. • Healing from the socket wall and healing from the adjacent PDL occurs simultaneously. • Ankylosis occurs and tooth becomes an integral part of the bone remodeling system.
DIAGNOSIS • Immobile • High percussive tone • PDL space is absent and a direct union is seen between alveolar bone and the root. • In time, infraocclusion relative to adjacent teeth can be seen both clinically and radiographically
TREATMENT • Can not be arrested or repaired.

EXTERNAL CERVICAL RESORPTION • Invasive and aggressive nature • Originates on the external root surface , but may invade dentin in any direction and to varying degrees. • Develops immediately apical to the epithelial attachment of the tooth
ETIOLOGY AND PATHOGENESIS Anatomic profile of the CEJ Intra-coronal bleaching Ortho treatment -21% Dental trauma -14% Oral surgery-6% Periodontal therapy. Bruxism Intracoronal restorations Delayed eruption Enamel stripping Developmental defects
POLARIZATION OF THOUGHTS • Microorganisms originating from the gingival sulcus provide the stimulus for continued resorption. • Opposing hypothesis by Heithersay suggests that ECR is a type of “benign proliferative fibrovascular or fibroosseos disorder” in which microorganisms play no active role and either absent from the site of resorption or invade it only secondarily.
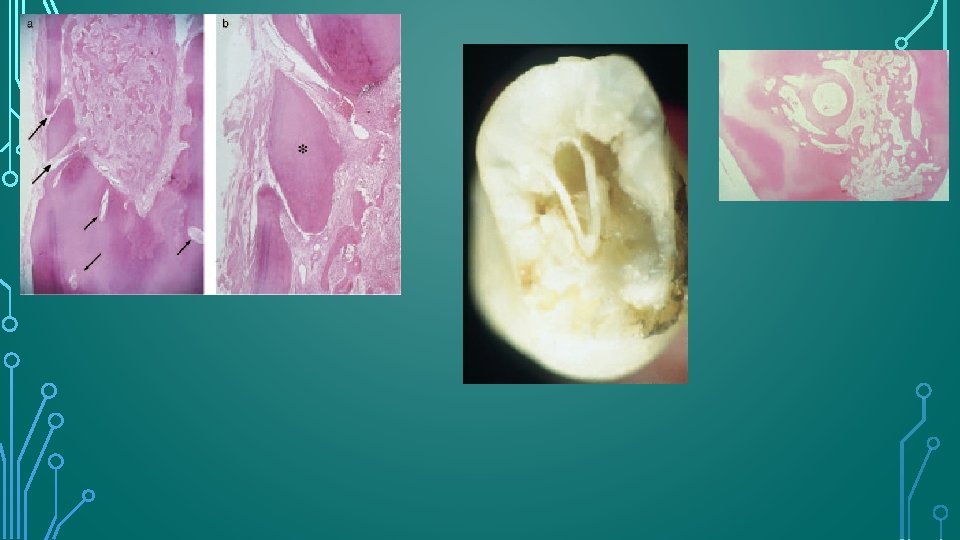
HISTOLOGIC APPEARANCE • Same as that of other forms of resorption , with certain unique feature reflecting the invasive nature of the process. • Narrow “channels” of resorption extend through the dentin and may communicate with the periodontal ligament.
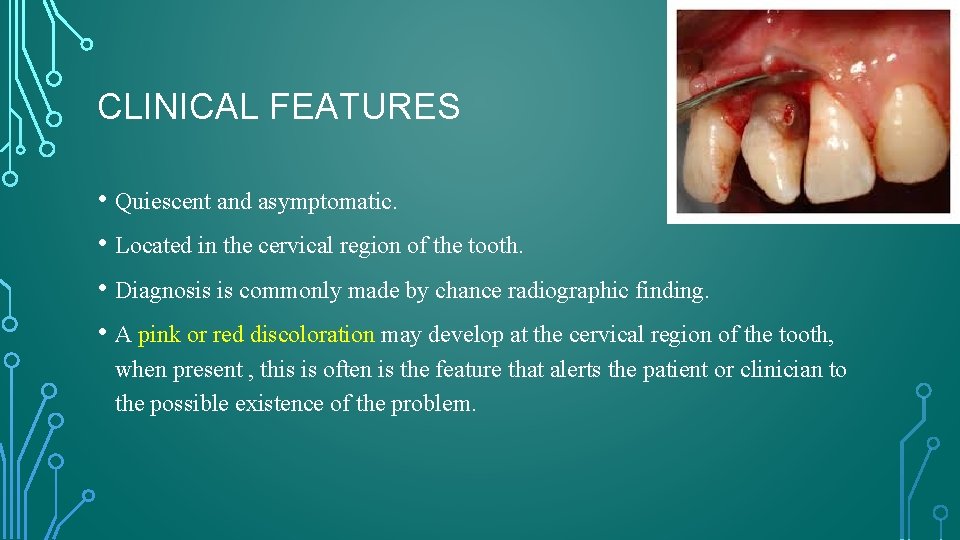
CLINICAL FEATURES • Quiescent and asymptomatic. • Located in the cervical region of the tooth. • Diagnosis is commonly made by chance radiographic finding. • A pink or red discoloration may develop at the cervical region of the tooth, when present , this is often is the feature that alerts the patient or clinician to the possible existence of the problem.
• Discoloration is due to the fibrovascular granulation tissue occupying the resorptive defect. • Loss of periodontal attachment may occur in the region of the resorption , and probing of the resorptive defect or the associated periodontal pocket causes the granulation tissue to bleed profusely.
• As the process progresses, perforation of the root canal wall and bacterial contamination of the pulp may occur. • The affected tooth may develop pulpitis and the associated clinical symptoms.
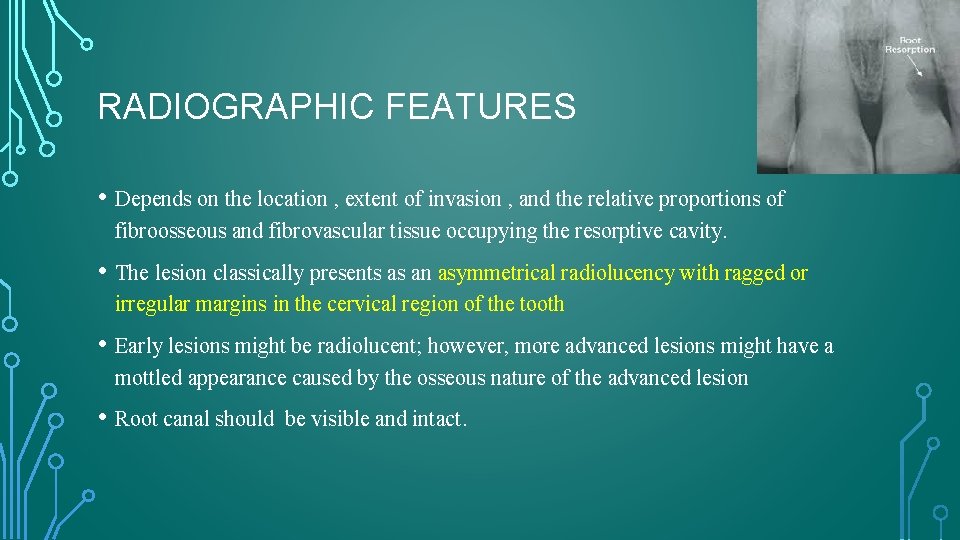
RADIOGRAPHIC FEATURES • Depends on the location , extent of invasion , and the relative proportions of fibroosseous and fibrovascular tissue occupying the resorptive cavity. • The lesion classically presents as an asymmetrical radiolucency with ragged or irregular margins in the cervical region of the tooth • Early lesions might be radiolucent; however, more advanced lesions might have a mottled appearance caused by the osseous nature of the advanced lesion • Root canal should be visible and intact.

HEITHERSAY CLASSIFICATION FOR ECR • Class 1 –Denotes a small invasive resorptive lesion near the cervical area with shallow penetration into dentine. • Class 2 – Denotes a well-defined invasive resorptive lesion that has penetrated close to the coronal pulp chamber but shows little or no extension into the radicular dentine. • Class 3 – Denotes a deeper invasion of dentine by resorbing tissue, not only involving the coronal dentine but also extending into the coronal third of the root. • Class 4 – Denotes a large invasive resorptive process that has extended beyond the coronal third of the root.

HEITHERSAY CLASSIFICATION FOR ECR. •  

Class 1 Class 2 Class 3
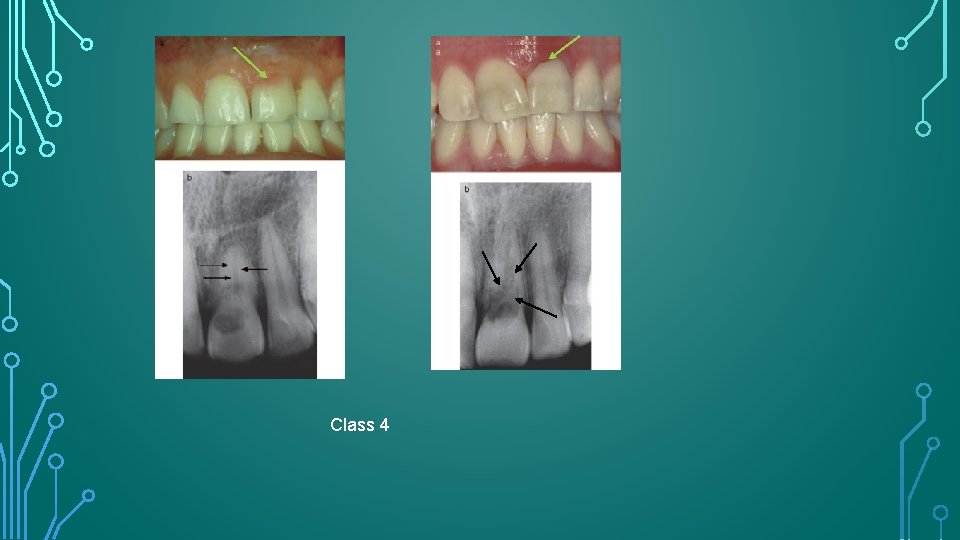
Class 4
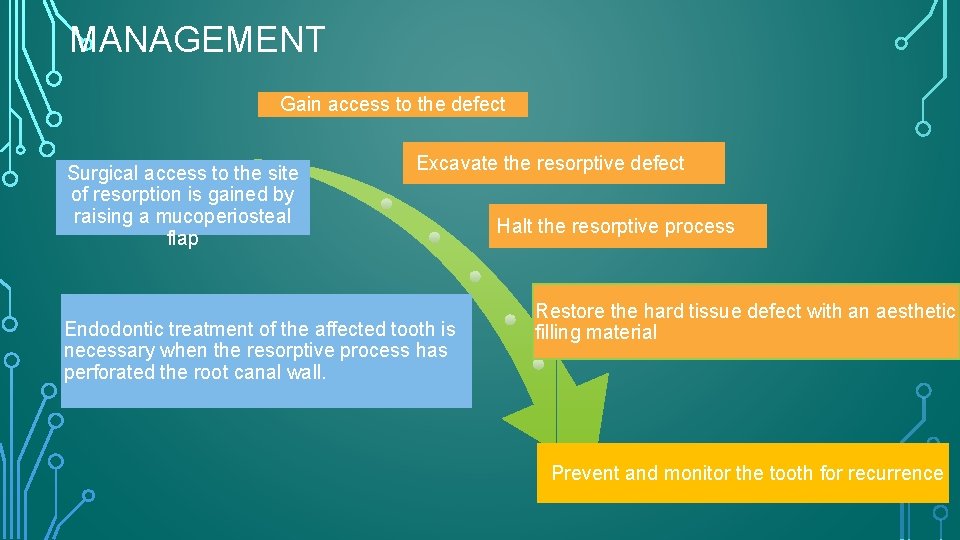
MANAGEMENT Gain access to the defect Surgical access to the site of resorption is gained by raising a mucoperiosteal flap Excavate the resorptive defect Endodontic treatment of the affected tooth is necessary when the resorptive process has perforated the root canal wall. Halt the resorptive process Restore the hard tissue defect with an aesthetic filling material Prevent and monitor the tooth for recurrence
TREATMENT • Treatment depends on the severity, location, whether the defect has perforated the root canal system, and the restorability of the tooth. • These include intentional replantation, guided tissue regeneration, treating the ECR lesion by an internal approach only, and forced orthodontic eruption.
• Once the resorptive tissue has been removed , the cavity may be treated with a 90% aqueous solution of trichloracetic acid ; this causes coagulation necrosis of the resorptive tissue without damaging the periodontal tissue. • This acid also penetrates and treats small channels of resorption that are not accessible to mechanical instrumentation.
• Once the defect has been excavated and treated with trichloracetic acid, any undermined dentin or enamel at the peripheries of the cavity are removed with a bur in a high speed handpiece and the cavity is restored with an aesthetically acceptable restorative material , such as composite resin or glass ionomer cement. • Biodentin may prove to be particularly suitable material for restoring these defects because it may combine acceptable aesthetics with the ability to support PDL attachment.

INTERNAL ROOT RESORPTION • Originates in and affects the root canal wall. • It is further classified as either inflammatory or replacement. • The replacement type is associated with the deposition of mineralized tissue in the root canal space after the initial loss of dentin.
ETIOLOGY • Trauma , (45%) • Caries (25%) • periodontal infections (14%) • Excessive heat generated during restorative procedures on vital teeth, • Calcium hydroxide procedures, • Vital root resections, • Anachoresis , • Orthodontic treatment, • Cracked teeth , • Idiopathic dystrophic changes in normal pulps
• Trauma and pulpal inflammation/infection are the major contributory factors in the initiation of internal resorption.
PATHOGENESIS • For IRR to occur , the outermost protective odontoblast layer and the predentin of the canal wall must be damaged , resulting in exposure of the underlying mineralized dentin to odontoclasts.
• Damage to the odontoblast layer and predentin of the canal wall is a prerequisite for initiation of internal root resorption. • However progression of IRR depends on bacterial stimulation of the clastic cells involved in hard tissue resorption • Without this stimulation , the resorption is self – limiting • For IRR to continue, the pulp tissue apical to the resorptive lesion must have a viable blood supply; this provides clastic cells and their nutrients , and the infected necrotic coronal pulp tissue provides stimulation for those clastic cells.
HISTOLOGIC APPEARANCE • Pulpal tissue was populated to varying degrees in all teeth with an inflammatory infiltrate composed predominantly of lymphocytes and macrophages. • The odontoblast layer and predentin were absent from the affected dentinal walls, which were populated by large, multinucleated odontoclasts occupying resorption lacunae. • Islands of mineralized tissue occupying the root canal space are the defining feature of internal replacement resorption.
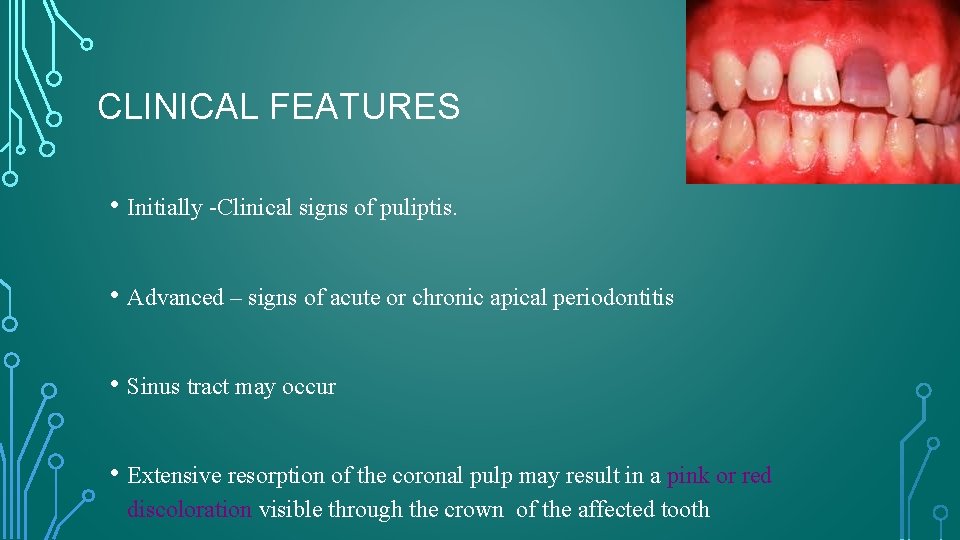
CLINICAL FEATURES • Initially -Clinical signs of puliptis. • Advanced – signs of acute or chronic apical periodontitis • Sinus tract may occur • Extensive resorption of the coronal pulp may result in a pink or red discoloration visible through the crown of the affected tooth
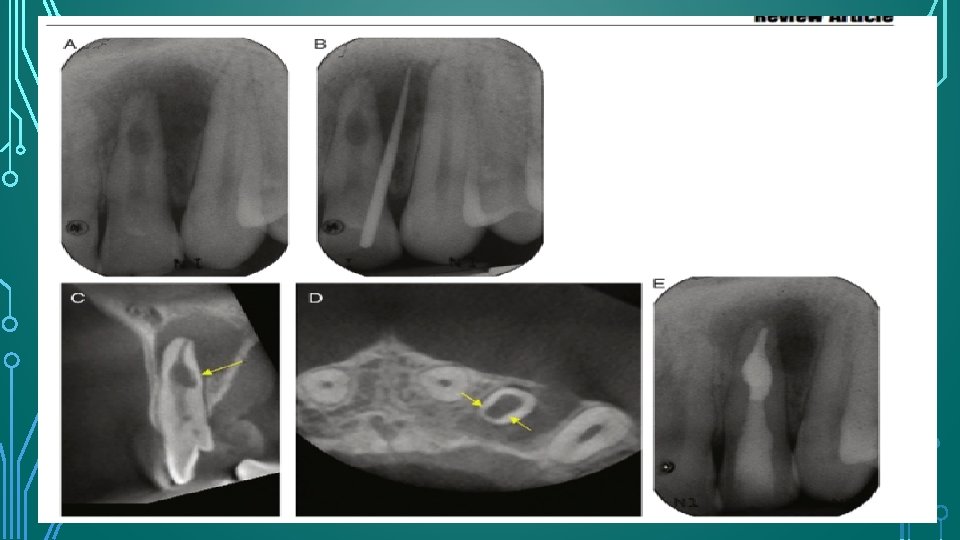
RADIOGRAPHIC FEATURES AND DIAGNOSIS • Gartner – radiolucency of uniform density that have a smooth outline and are symmetrically distributed over the root of the affected tooth • The outline of the root canal wall should not be traceable through the resorption defect because the root canal wall balloons out. • Oval, circumscribed radiolucency in continuity with the root canal wall. • Internal replacement root resorption – somewhat mottled or clouded appearance as a result of the radiopaque nature of the calcified material occupying the lesion.
MANAGEMENT Check prognosis Root canal treatment Remove the intraradicular bacteria and disinfect the root canal system Intracanal antibacterial medicament should be used to further reduce the microbial load and improve the disinfection of the root canal space Obturation with Obtura II and Microseal (MS) thermoplastic
Because root sealers shrink on setting and degrade to varying degrees in the presence of moisture , fillings with higher GP/ sealer ratios reduce the risk of void formation and leakage of contaminants into the root canal system. If perforation has occurred , MTA should be considered the material of choice to repair the root wall.
SUMMARY • The prevalence, etiology, and pathogenesis of various types of root resorption are not fully understood, and more research is required in these areas. • More clinical data are required on the presenting features of ECR because this particular type of resorption may vary significantly in its presentation. • Early detection of root resorption is essential for successful management and favorable outcomes. • CBCT is an excellent diagnostic tool for confirming the presence of ECR and IRR and also for appreciating the true nature of these conditions and managing them.
- Slides: 60