Resistive Exercise Testing in Cardiopulmonary Rehabilitation Special Populations
“Resistive Exercise Testing in Cardiopulmonary Rehabilitation Special Populations and the Elderly” NCCRA Annual Symposium March 5 -6, 2015 Dave Verrill, MS, CES, RCEP, FAACVPR Past-President of NCCRA and CEPA Lecturer and Exercise Laboratory Director University of North Carolina at Charlotte, NC
• This presentation will only focus on muscular strength and endurance testing • There also multiple tests for balance, gait, agility and flexibility that are in use today for various patient populations • Cardiopulmonary testing protocols are well -established and are also necessary for each type of patient population
WHICH SPECIAL POPULATIONS DO WE TREAT IN CARDIOPULMONARY REHABILITATION? Cardiac (MI, CABG, Valvular, Stent, CHF, Transplant) Cardiovascular (PAD, Stroke, HTN, TIA) Metabolic (Diabetes, Obesity, Hyperlipidemia, Renal) Geriatric (Frail, Elderly, Higher Risk Older Populations) Immunologic (Cancer, AIDS, Fibromyalgia, CFS) Neuromuscular (MS, ALS, Cerebral Palsy, Parkinson’s) Musculoskeletal (Osteoporosis, Arthritis, Low back pain)

Chronic muscle deconditioning leads to: energy expenditure basal metabolic rate muscular strength activity level falls disability injuries sedentary living
NO ONE TEST IS SUITABLE ALL TYPES OF PATIENTS!

Why do we Need to Perform Strength Testing for Our Rehabilitation Patients?
Must have pre- & post-rehab strength measurements for strength improvement outcomes documentation Need to test after 3, 6, 12, 18 and 24 months (or whatever outcome follow-up intervals you prefer) For AACVPR Program Certification and AACVPR Cardiopulmonary Rehab Outcomes Registries To let the patient know how they stand up compared to those in their age and gender groups strength-wise To let the patient know how much they are improving (or regressing) throughout their rehabilitation program
To help determine the patient’s ability to perform basic ADL’s (walking, dressing, picking things up, housework, squatting) To measure individual success in resistive exercises with validated norms To boost confidence and self-efficacy To help assess posture and balance issues and to prescribe posture and balance exercises To assess and determine the individual needs of the patient with respect to their unique overall muscular weaknesses
WHY IS RESISTIVE EXERCISE TESTING UNDERUTILIZED? q Few (if any) evidenced-based guidelines and lack of research q Fear of the patient becoming injured q Lack of testing protocols and knowledge of existing protocols q Each special population has their own unique and specific characteristics q Time factor—do you perform different tests for different patients for their individualized ITP?
HOW DO YOU SELECT THE PROPER RESISTIVE TESTING PROTOCOL FOR YOUR PATIENTS WITH VARYING TYPES OF DISEASES?
The CEP should look for established protocols with normative data in the literature. The test need not necessarily be designed specifically for that type of patient. There is a significant lack of testing research for special populations in the literature—thus, the CEP must often use their own best judgment on which test to use for which type of patient.
A good place to start is the “Senior Fitness Test Manual, 2 nd edition” (Rikli & Jones, 2013, Human Kinetics)
How do we Measure Resistive Exercise Testing Outcomes?
1. Properly screen the patient! 2. Test with the appropriate testing modality. 3. Record entry strength testing measurements. 3. Test again at 12 -16 weeks (or whatever followup interval your institution utilizes) and throughout program participation. 5. Subtract the entry test value from the post-test value and divide by the post-test value for the % improvement.
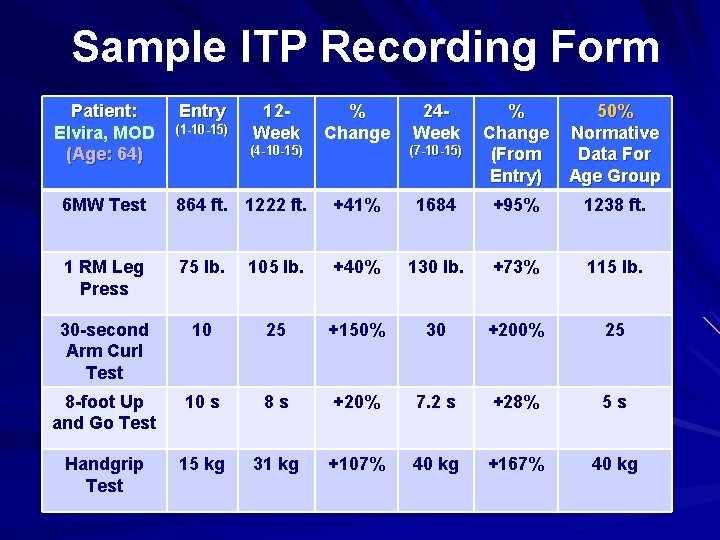
Sample ITP Recording Form Patient: Elvira, MOD (Age: 64) Entry (1 -10 -15) 12 Week % Change (4 -10 -15) 24 Week (7 -10 -15) % Change (From Entry) 50% Normative Data For Age Group 6 MW Test 864 ft. 1222 ft. +41% 1684 +95% 1238 ft. 1 RM Leg Press 75 lb. 105 lb. +40% 130 lb. +73% 115 lb. 30 -second Arm Curl Test 10 25 +150% 30 +200% 25 8 -foot Up and Go Test 10 s 8 s +20% 7. 2 s +28% 5 s Handgrip Test 15 kg 31 kg +107% 40 kg +167% 40 kg
WHO SHOULD NOT PERFORM RESISTIVE TESTING?
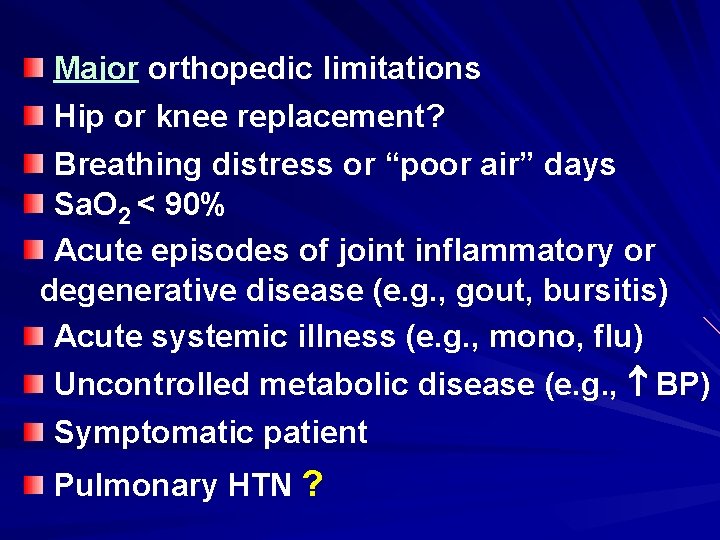
Major orthopedic limitations Hip or knee replacement? Breathing distress or “poor air” days Sa. O 2 < 90% Acute episodes of joint inflammatory or degenerative disease (e. g. , gout, bursitis) Acute systemic illness (e. g. , mono, flu) Uncontrolled metabolic disease (e. g. , BP) Symptomatic patient Pulmonary HTN ?
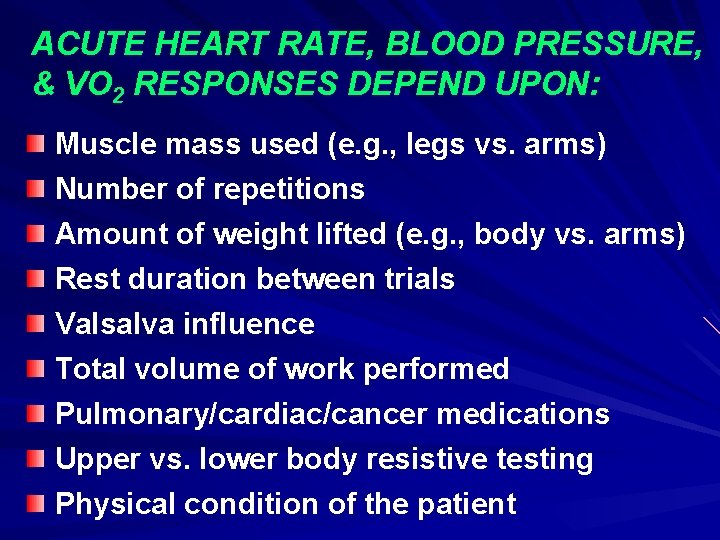
ACUTE HEART RATE, BLOOD PRESSURE, & VO 2 RESPONSES DEPEND UPON: Muscle mass used (e. g. , legs vs. arms) Number of repetitions Amount of weight lifted (e. g. , body vs. arms) Rest duration between trials Valsalva influence Total volume of work performed Pulmonary/cardiac/cancer medications Upper vs. lower body resistive testing Physical condition of the patient
SAFETY ISSUES • Always perform strength testing with a focus on safety first. • Be sure that your equipment set-up and maintenance follows the specifications from national organizations (e. g. , ACSM’s Health/Fitness Facility Standards and Guidelines, 4 th edition). • Always provide the patient with proper instructions on resistive exercise testing from start to finish. • Stay very close to the deconditioned or frail patient throughout testing—be there if they start to fall (1 on 1 instruction).
SAFETY ISSUES 1 -RM testing is OK in properly screened patients if performed by properly certified clinical exercise staff! If the patient complains of mild muscle soreness 12 -24 hours after resistive testing, this is normal. If the patient complains of chronic (> 1 week) muscle soreness after resistive testing, this is not normal. Demonstrate the test yourself first. Report any significant injuries or complications to the supervising physician and the patient’s physician.
ADMINISTERING THE TESTS
Have the patient perform at least 5 -8 minutes of warm-up and stretching activities (typical rehab warm-up activities) OK to test the patient after group warm-up Typically no additional physiologic monitoring needed (telemetry ECG or SAO 2 OK) Include dynamic stretching that exercises the muscle groups being tested Prior to the test tell the patient to “Do the best they can, but not to the point of overexertion or beyond what they think is safe for them”
Stop testing immediately if the patient is using improper technique or form Stop testing if any clinically abnormal signs or symptoms For those with visual or auditory limitation, make the appropriate testing adjustments (e. g. , have cleared area, ask if you can help, large cones) Demonstrate the testing protocol For those with chronic pain, if > 5 on a 0 -10 scale best to delay testing until the pain level is lower
TESTING THOSE WITH COGNITIVE IMPAIRMENT • Use simple words • Speak slowly and distinctly • Be calm, reassuring and positive • Maintain eye contact • Don’t give excessive verbal instructions • Use non-verbal gestures • Allow the patient adequate time to respond
COMMON TESTS OF MUSCULAR STRENGTH AND ENDURANCE
MACHINE WEIGHT TESTING • Demonstrate proper position of the seat and other attachments on the machine weights. • Demonstrate proper pin placement in the weight stack. • Demonstrate proper placement of additional weight on the weight stack. • Reinforce proper breathing techniques and posture on the machine (i. e. , exhale with the muscle contraction, pursed-lip breathing).
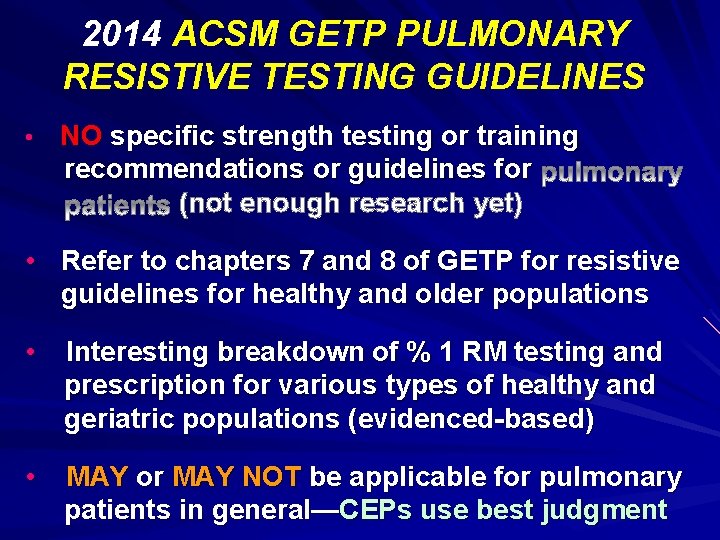
2014 ACSM GETP PULMONARY RESISTIVE TESTING GUIDELINES • NO specific strength testing or training recommendations or guidelines for (not enough research yet) • Refer to chapters 7 and 8 of GETP for resistive guidelines for healthy and older populations • Interesting breakdown of % 1 RM testing and prescription for various types of healthy and geriatric populations (evidenced-based) • MAY or MAY NOT be applicable for pulmonary patients in general—CEPs use best judgment
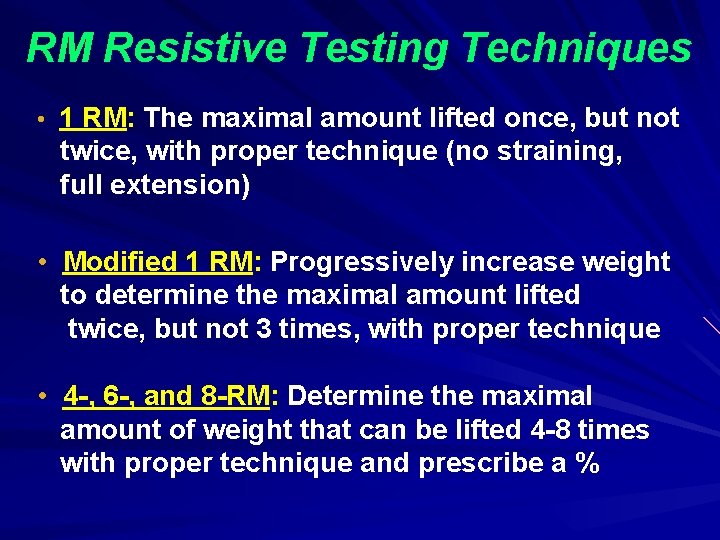
RM Resistive Testing Techniques • 1 RM: The maximal amount lifted once, but not twice, with proper technique (no straining, full extension) • Modified 1 RM: Progressively increase weight to determine the maximal amount lifted twice, but not 3 times, with proper technique • 4 -, 6 -, and 8 -RM: Determine the maximal amount of weight that can be lifted 4 -8 times with proper technique and prescribe a %
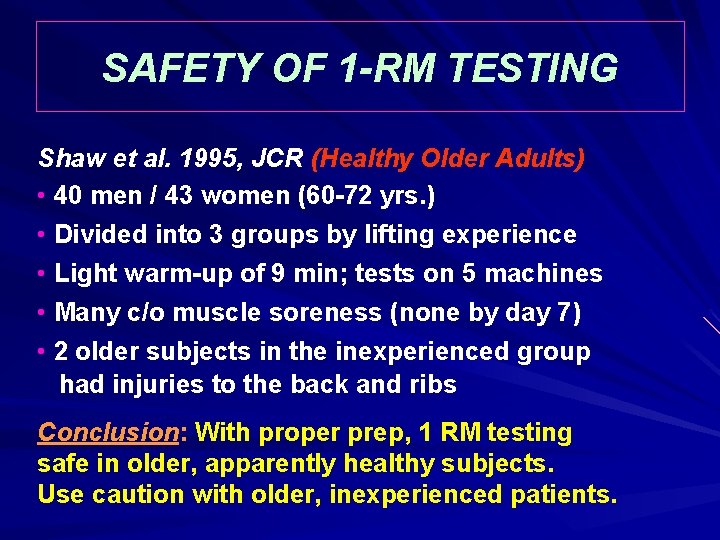
SAFETY OF 1 -RM TESTING Shaw et al. 1995, JCR (Healthy Older Adults) • 40 men / 43 women (60 -72 yrs. ) • Divided into 3 groups by lifting experience • Light warm-up of 9 min; tests on 5 machines • Many c/o muscle soreness (none by day 7) • 2 older subjects in the inexperienced group had injuries to the back and ribs Conclusion: With proper prep, 1 RM testing safe in older, apparently healthy subjects. Use caution with older, inexperienced patients.
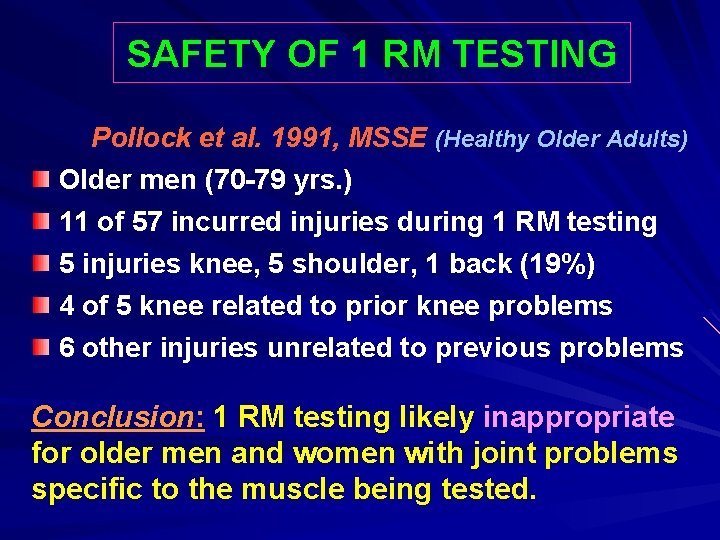
SAFETY OF 1 RM TESTING Pollock et al. 1991, MSSE (Healthy Older Adults) Older men (70 -79 yrs. ) 11 of 57 incurred injuries during 1 RM testing 5 injuries knee, 5 shoulder, 1 back (19%) 4 of 5 knee related to prior knee problems 6 other injuries unrelated to previous problems Conclusion: 1 RM testing likely inappropriate for older men and women with joint problems specific to the muscle being tested.
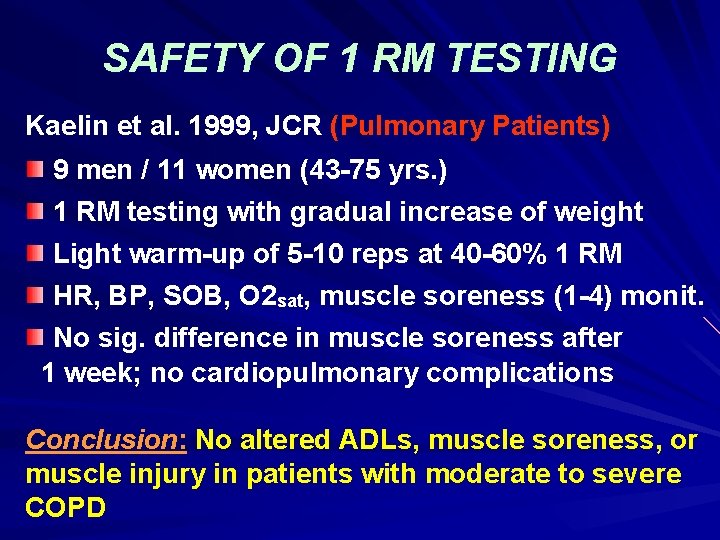
SAFETY OF 1 RM TESTING Kaelin et al. 1999, JCR (Pulmonary Patients) 9 men / 11 women (43 -75 yrs. ) 1 RM testing with gradual increase of weight Light warm-up of 5 -10 reps at 40 -60% 1 RM HR, BP, SOB, O 2 sat, muscle soreness (1 -4) monit. No sig. difference in muscle soreness after 1 week; no cardiopulmonary complications Conclusion: No altered ADLs, muscle soreness, or muscle injury in patients with moderate to severe COPD
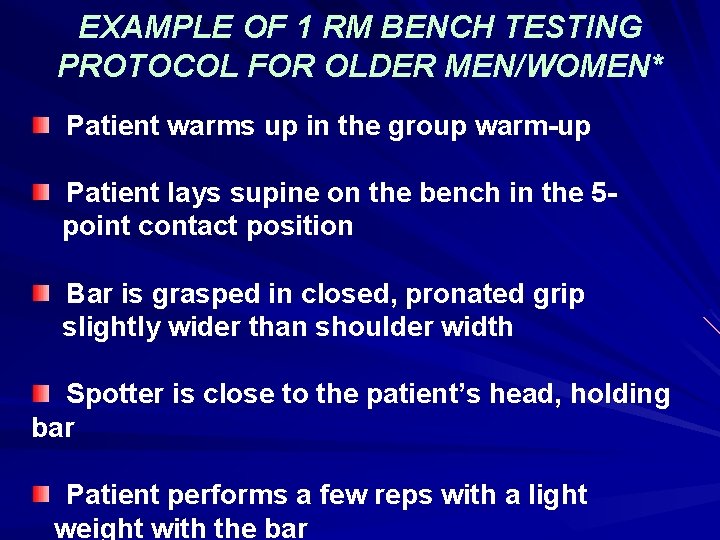
EXAMPLE OF 1 RM BENCH TESTING PROTOCOL FOR OLDER MEN/WOMEN* Patient warms up in the group warm-up Patient lays supine on the bench in the 5 point contact position Bar is grasped in closed, pronated grip slightly wider than shoulder width Spotter is close to the patient’s head, holding bar Patient performs a few reps with a light weight with the bar
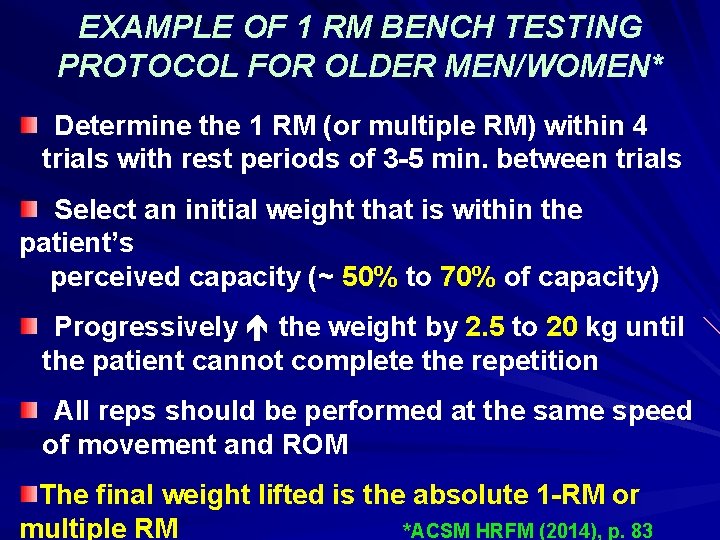
EXAMPLE OF 1 RM BENCH TESTING PROTOCOL FOR OLDER MEN/WOMEN* Determine the 1 RM (or multiple RM) within 4 trials with rest periods of 3 -5 min. between trials Select an initial weight that is within the patient’s perceived capacity (~ 50% to 70% of capacity) Progressively the weight by 2. 5 to 20 kg until the patient cannot complete the repetition All reps should be performed at the same speed of movement and ROM The final weight lifted is the absolute 1 -RM or multiple RM *ACSM HRFM (2014), p. 83
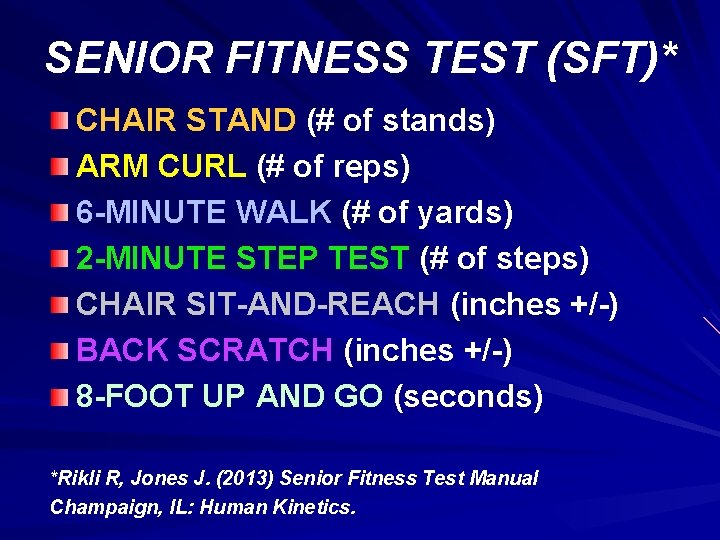
SENIOR FITNESS TEST (SFT)* CHAIR STAND (# of stands) ARM CURL (# of reps) 6 -MINUTE WALK (# of yards) 2 -MINUTE STEP TEST (# of steps) CHAIR SIT-AND-REACH (inches +/-) BACK SCRATCH (inches +/-) 8 -FOOT UP AND GO (seconds) *Rikli R, Jones J. (2013) Senior Fitness Test Manual Champaign, IL: Human Kinetics.
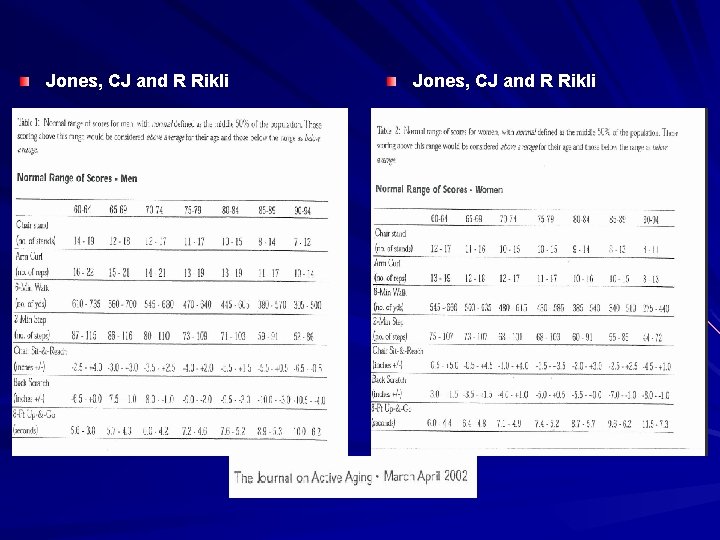
Jones, CJ and R Rikli
Jug Shelf Test 1 6 -Minute Peg Board and Ring Test 2 Grip Dynamometer Test 3 1 Signorile et. al. , J Aging Phys Act 2007; 15: 56 -74. 2 Su Zhan et. al. , JCR 2006; 26: 180 -187. 3 Kaminsky LA. ACSM’s Health Related Physical Fitness Assessment Manual, 4 th edition. Philadelphia: Wolters Kluwer/LWW, 2014, pp. 80 -81.
The 30 -Second Arm (or Biceps) Curl Test
Equipment Needed – Stopwatch – Straight-back or folding chair with NO arms – 5 -lb (2. 3 kg) dumbbell for women – 8 -lb (3. 6 kg) dumbbell for men
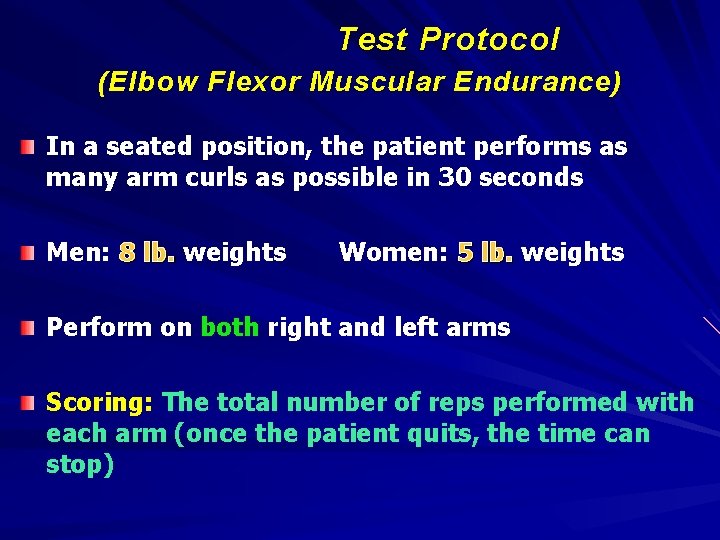
Test Protocol (Elbow Flexor Muscular Endurance) In a seated position, the patient performs as many arm curls as possible in 30 seconds Men: 8 lb. weights Women: 5 lb. weights Perform on both right and left arms Scoring: The total number of reps performed with each arm (once the patient quits, the time can stop)
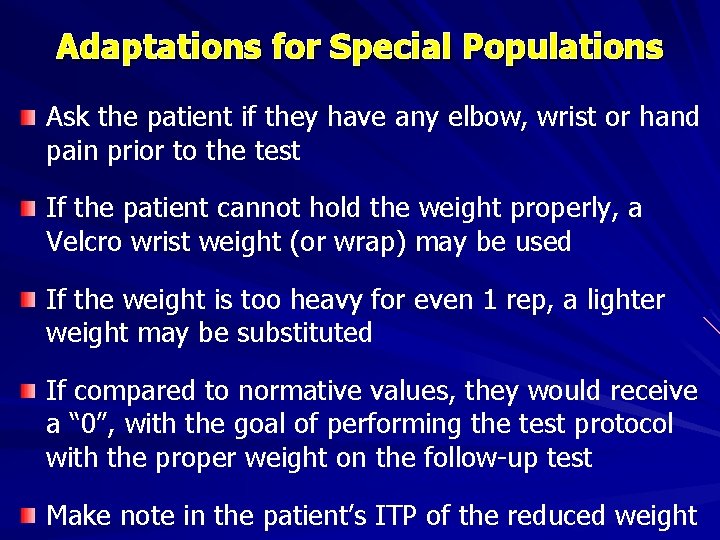
Adaptations for Special Populations Ask the patient if they have any elbow, wrist or hand pain prior to the test If the patient cannot hold the weight properly, a Velcro wrist weight (or wrap) may be used If the weight is too heavy for even 1 rep, a lighter weight may be substituted If compared to normative values, they would receive a “ 0”, with the goal of performing the test protocol with the proper weight on the follow-up test Make note in the patient’s ITP of the reduced weight
The 2 -Minute Step Test
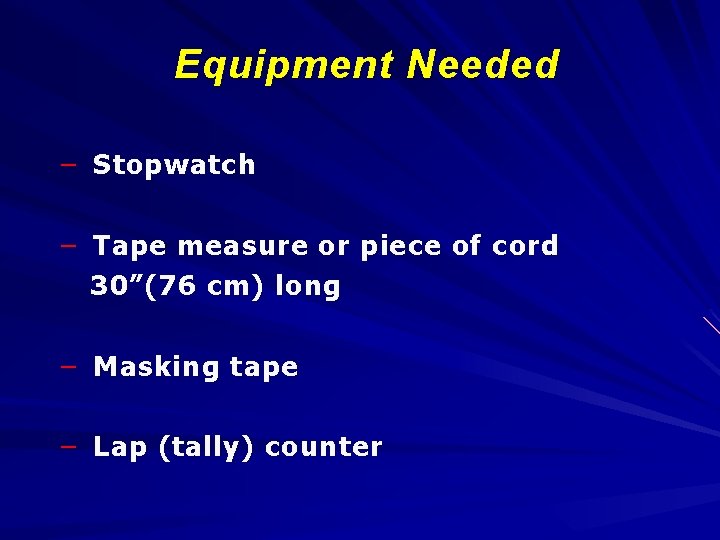
Equipment Needed – Stopwatch – Tape measure or piece of cord 30”(76 cm) long – Masking tape – Lap (tally) counter
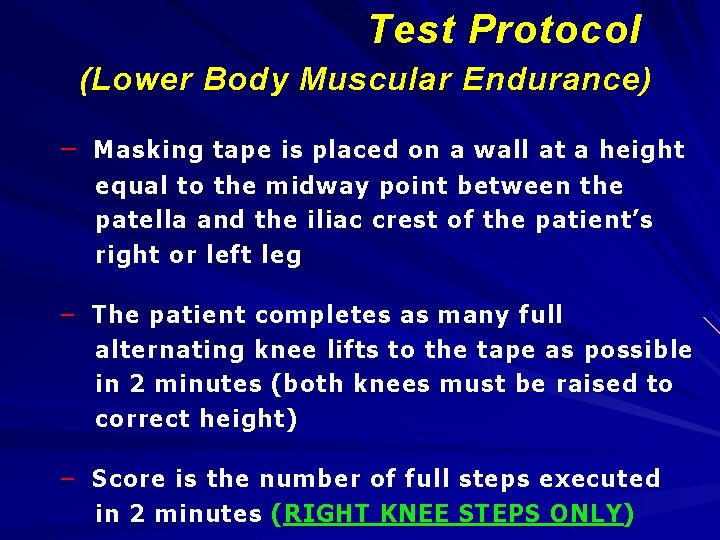
Test Protocol (Lower Body Muscular Endurance) – Masking tape is placed on a wall at a height equal to the midway point between the patella and the iliac crest of the patient’s right or left leg – The patient completes as many full alternating knee lifts to the tape as possible in 2 minutes (both knees must be raised to correct height) – Score is the number of full steps executed in 2 minutes ( RIGHT KNEE STEPS ONLY )
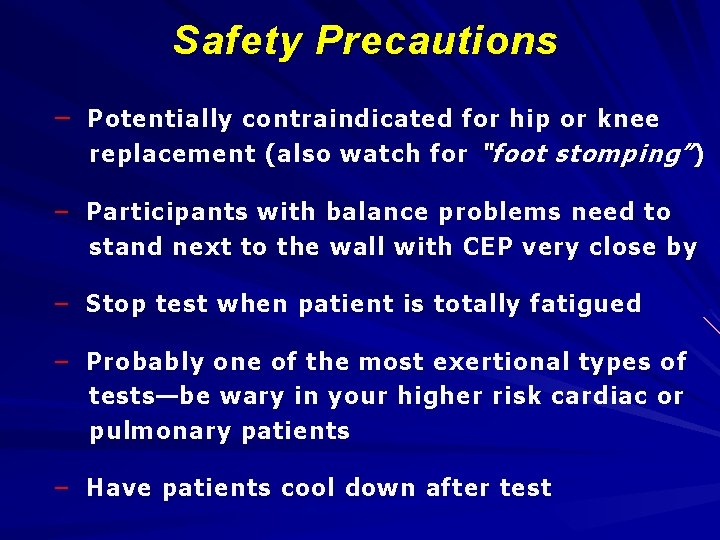
Safety Precautions – Potentially contraindicated for hip or knee replacement (also watch for “foot stomping” ) – Participants with balance problems need to stand next to the wall with CEP very close by – Stop test when patient is totally fatigued – Probably one of the most exertional types of tests—be wary in your higher risk cardiac or pulmonary patients – Have patients cool down after test
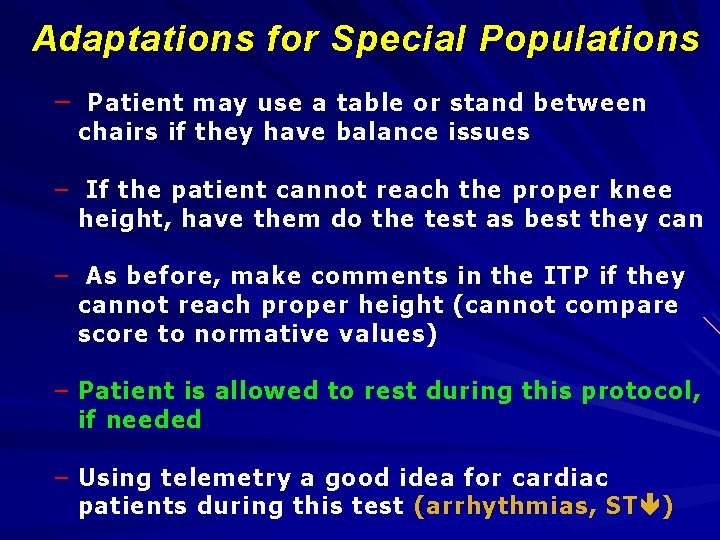
Adaptations for Special Populations – Patient may use a table or stand between chairs if they have balance issues – If the patient cannot reach the proper knee height, have them do the test as best they can – As before, make comments in the ITP if they cannot reach proper height (cannot compare score to normative values) – Patient is allowed to rest during this protocol, if needed – Using telemetry a good idea for cardiac patients during this test (arrhythmias, ST )
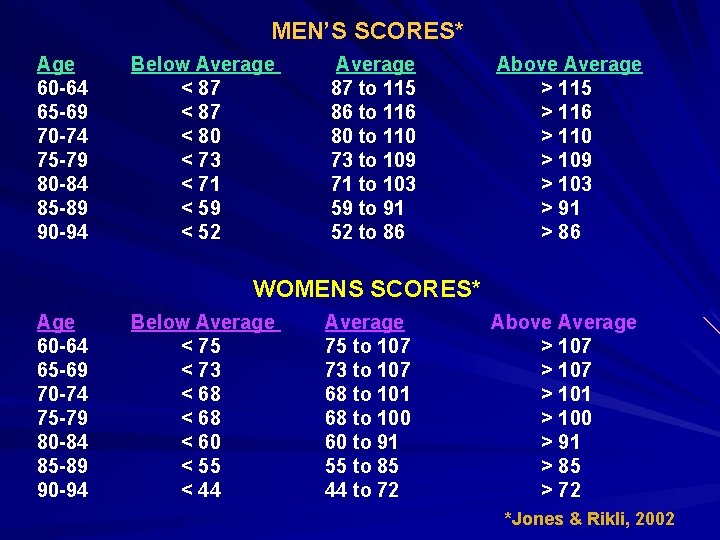
MEN’S SCORES* Age 60 -64 65 -69 70 -74 75 -79 80 -84 85 -89 90 -94 Below Average < 87 < 80 < 73 < 71 < 59 < 52 Average 87 to 115 86 to 116 80 to 110 73 to 109 71 to 103 59 to 91 52 to 86 Above Average > 115 > 116 > 110 > 109 > 103 > 91 > 86 WOMENS SCORES* Age 60 -64 65 -69 70 -74 75 -79 80 -84 85 -89 90 -94 Below Average < 75 < 73 < 68 < 60 < 55 < 44 Average 75 to 107 73 to 107 68 to 101 68 to 100 60 to 91 55 to 85 44 to 72 Above Average > 107 > 101 > 100 > 91 > 85 > 72 *Jones & Rikli, 2002
The 30 -Second Chair Stand Test
Equipment Needed – Stopwatch – Straight-back or folding chair with a seat height of 17” (43 cm) – Chair is placed against a wall or beam to prevent slipping
Test Protocol (Lower Body Muscular Strength & Endurance ) – The patient starts seated in chair with arms folded across chest, feet flat on the floor – The patient completes as many full stands as possible in 30 seconds – Score is the number stands executed correctly (if > ½ way up at end of 30 seconds, counts as a full stand)
Potential Contraindications – Chronic low back pain – Hip or knee replacement – Severe hip or knee osteoporosis or arthritis – If the patient is very frail, have them perform a practice stand before proceeding with the test
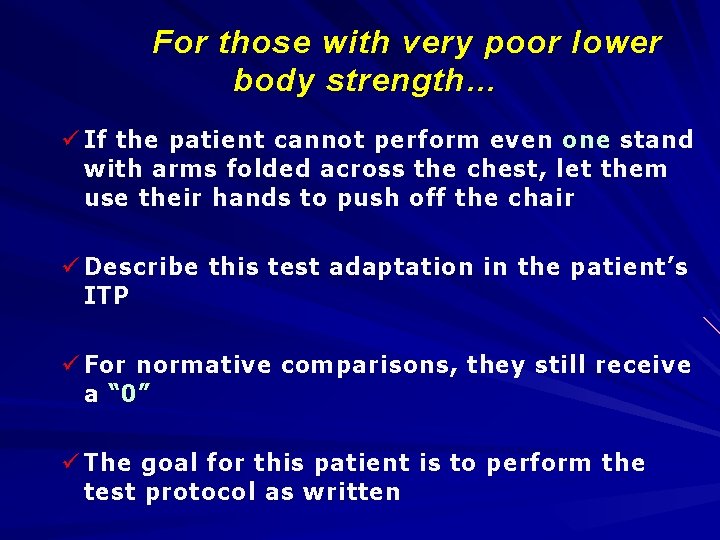
For those with very poor lower body strength… ü If the patient cannot perform even one stand with arms folded across the chest, let them use their hands to push off the chair ü Describe this test adaptation in the patient’s ITP ü For normative comparisons, they still receive a “ 0 ” ü The goal for this patient is to perform the test protocol as written
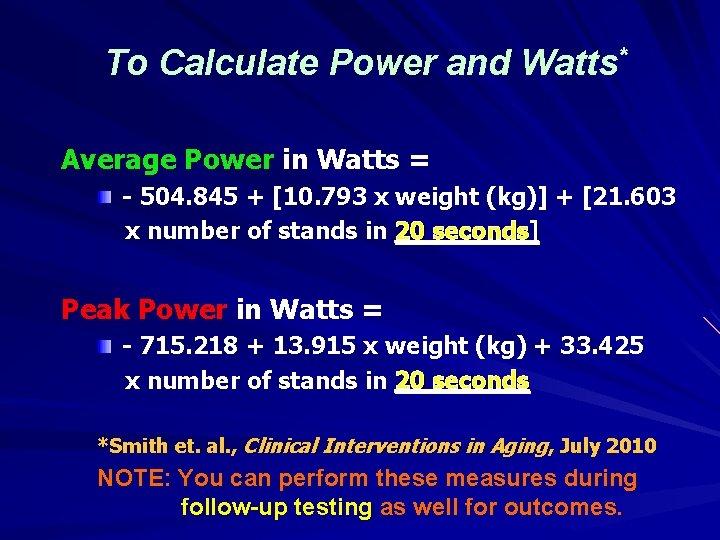
To Calculate Power and Watts* Average Power in Watts = - 504. 845 + [10. 793 x weight (kg)] + [21. 603 x number of stands in 20 seconds] Peak Power in Watts = - 715. 218 + 13. 915 x weight (kg) + 33. 425 x number of stands in 20 seconds *Smith et. al. , Clinical Interventions in Aging, July 2010 NOTE: You can perform these measures during follow-up testing as well for outcomes.
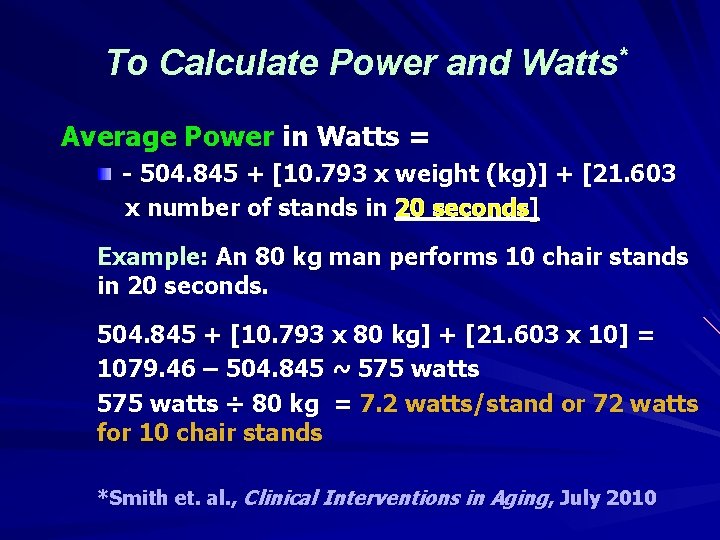
To Calculate Power and Watts* Average Power in Watts = - 504. 845 + [10. 793 x weight (kg)] + [21. 603 x number of stands in 20 seconds] Example: An 80 kg man performs 10 chair stands in 20 seconds. 504. 845 + [10. 793 x 80 kg] + [21. 603 x 10] = 1079. 46 – 504. 845 ~ 575 watts ÷ 80 kg = 7. 2 watts/stand or 72 watts for 10 chair stands *Smith et. al. , Clinical Interventions in Aging, July 2010
The 8 -Foot Up and Go Test
The 8 Foot “Up-and-Go” Test – Indicates the level of the participant's motor agility and dynamic balance – Also a measure of muscular endurance of the leg muscles – Associated with the lifestyle tasks of maneuvering in a crowd, getting on or off a train/bus or moving around the house
The 8 Foot “Up-and-Go” Test Required Equipment – Chair with a straight back (17” or 43 cm) – Chair legs should be placed against wall to stop the chair from sliding backwards – Cone placed so the rear of the marker is 2. 44 meters (8 feet) from the front of the chair – Stopwatch and tape measure
The 8 foot “Up-and-Go” Test Instructions Ø The subject starts fully seated in the middle of the chair with back straight. Ø The hands should rest on the thighs. Ø One foot is placed slightly in front of the other, but both must be flat on the floor. Ø The subject leans slightly forward.
The 8 foot “Up-and-Go” Test Instructions On the command "Go" the time is started and the subject stands and walks (no running) as quickly as possible (and safely) around the cone, returning to the chair to sit down Timing stops as they sit down Two trials are performed Scoring: The best time of the two trials is taken to the nearest 1/10 th second
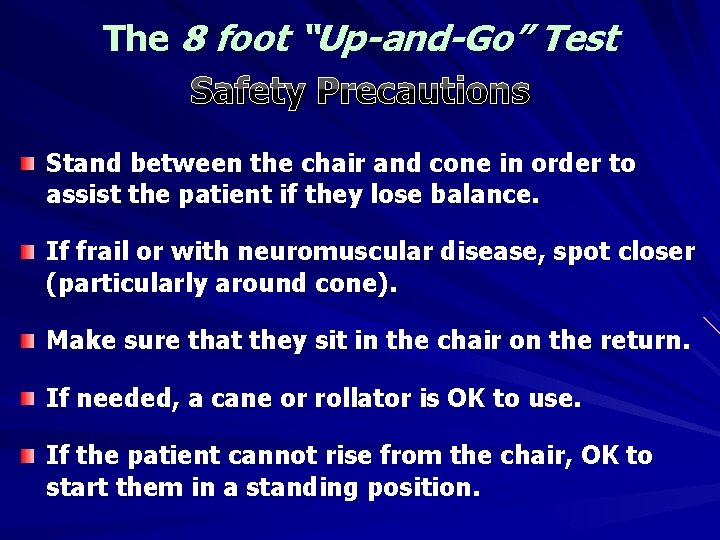
The 8 foot “Up-and-Go” Test Safety Precautions Stand between the chair and cone in order to assist the patient if they lose balance. If frail or with neuromuscular disease, spot closer (particularly around cone). Make sure that they sit in the chair on the return. If needed, a cane or rollator is OK to use. If the patient cannot rise from the chair, OK to start them in a standing position.
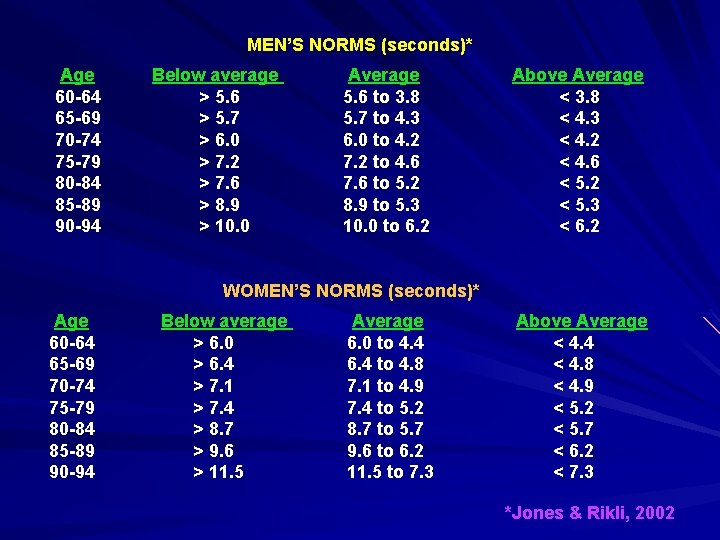
MEN’S NORMS (seconds)* Age 60 -64 65 -69 70 -74 75 -79 80 -84 85 -89 90 -94 Below average > 5. 6 > 5. 7 > 6. 0 > 7. 2 > 7. 6 > 8. 9 > 10. 0 Average 5. 6 to 3. 8 5. 7 to 4. 3 6. 0 to 4. 2 7. 2 to 4. 6 7. 6 to 5. 2 8. 9 to 5. 3 10. 0 to 6. 2 Above Average < 3. 8 < 4. 3 < 4. 2 < 4. 6 < 5. 2 < 5. 3 < 6. 2 WOMEN’S NORMS (seconds)* Age 60 -64 65 -69 70 -74 75 -79 80 -84 85 -89 90 -94 Below average > 6. 0 > 6. 4 > 7. 1 > 7. 4 > 8. 7 > 9. 6 > 11. 5 Average 6. 0 to 4. 4 6. 4 to 4. 8 7. 1 to 4. 9 7. 4 to 5. 2 8. 7 to 5. 7 9. 6 to 6. 2 11. 5 to 7. 3 Above Average < 4. 4 < 4. 8 < 4. 9 < 5. 2 < 5. 7 < 6. 2 < 7. 3 *Jones & Rikli, 2002
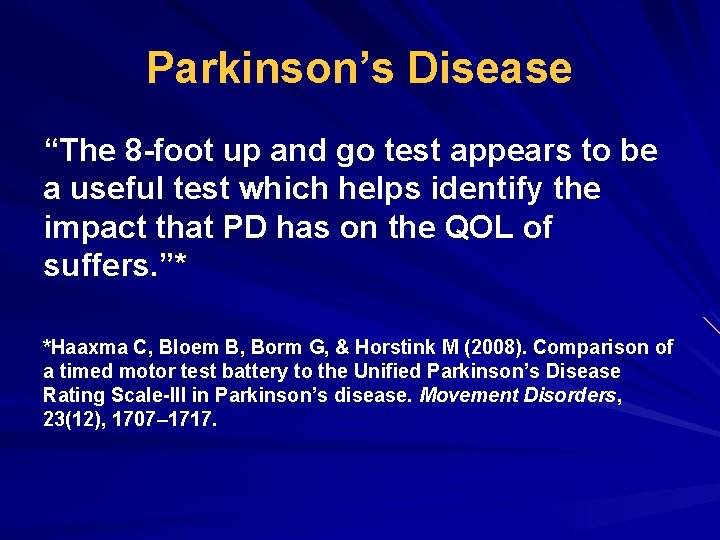
Parkinson’s Disease “The 8 -foot up and go test appears to be a useful test which helps identify the impact that PD has on the QOL of suffers. ”* *Haaxma C, Bloem B, Borm G, & Horstink M (2008). Comparison of a timed motor test battery to the Unified Parkinson’s Disease Rating Scale-III in Parkinson’s disease. Movement Disorders, 23(12), 1707– 1717.
The 6 -Minute Pegboard and Ring Test
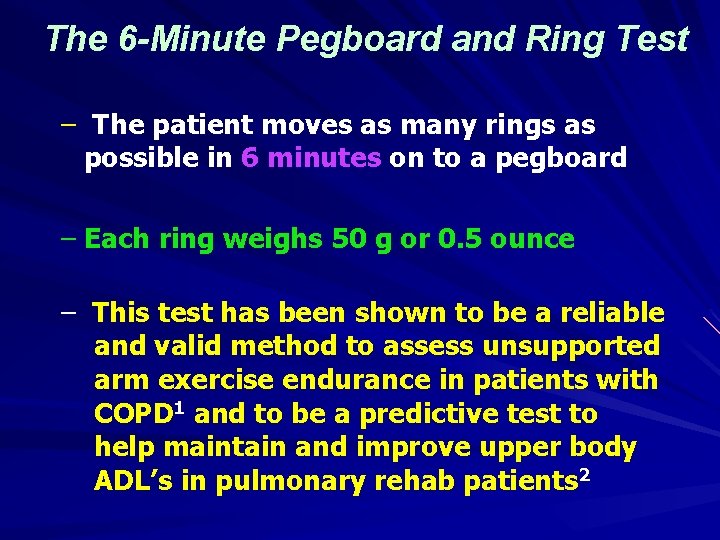
The 6 -Minute Pegboard and Ring Test – The patient moves as many rings as possible in 6 minutes on to a pegboard – Each ring weighs 50 g or 0. 5 ounce – This test has been shown to be a reliable and valid method to assess unsupported arm exercise endurance in patients with COPD 1 and to be a predictive test to help maintain and improve upper body ADL’s in pulmonary rehab patients 2
FOR MORE INFO ON THIS TEST 1. Zhan S, Cerny F, Gibbons W, Mador J, Wu YW. Development of an Unsupported Arm Exercise Test in Patients With Chronic Obstructive Pulmonary Disease. Journal of Cardiopulmonary Rehabilitation. 2006; 26(3): 180 -187. 1. Takeda et. al. The 6 -minute pegboard and ring test is correlated with upper extremity activity of daily living in chronic obstructive pulmonary disease. International Journal of COPD. 2013; 8: 347 -351.
The Signorile Gallo Jug Shelf Test
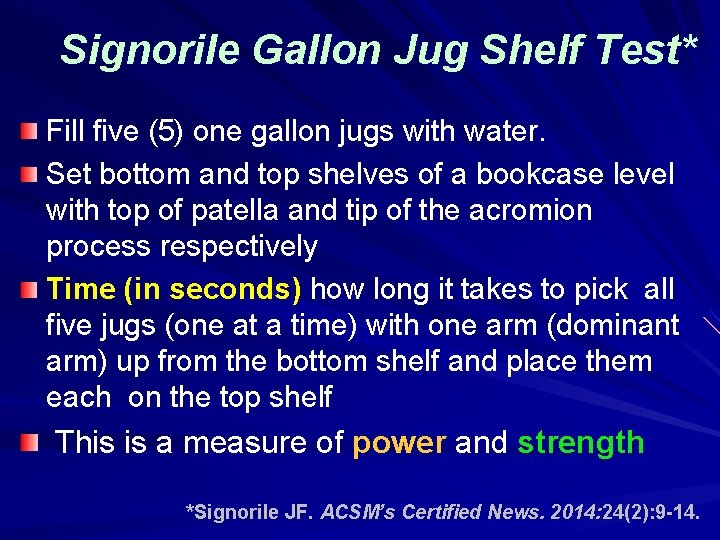
Signorile Gallon Jug Shelf Test* Fill five (5) one gallon jugs with water. Set bottom and top shelves of a bookcase level with top of patella and tip of the acromion process respectively Time (in seconds) how long it takes to pick all five jugs (one at a time) with one arm (dominant arm) up from the bottom shelf and place them each on the top shelf This is a measure of power and strength *Signorile JF. ACSM’s Certified News. 2014: 24(2): 9 -14.
Signorile Gallon Jug Shelf Test Equipment Needed Five (5) one gallon jugs filled with water. Bookshelf (84” H x 42” W x 12” D) Stopwatch
Signorile Gallon Jug Shelf Test Equipment Needed QUESTION: Where would I find such a bookcase with adjustable shelves? ANSWER: Have a patient with carpentry skills make a bookcase with shelving that is adjustable with “fine tuning. ” REWARD: Give the patient 1 -2 free months of maintenance exercise in your program for building this bookcase!
Signorile Gallon Jug Shelf Test Set-up Align the lower shelf with the participant’s patella. Align the upper shelf with the top of the patient’s shoulder (acromion process). Place the 5 one-gallon jugs on the bottom shelf. Provide detailed instructions prior to testing. Demonstrate the test protocol.
Signorile Gallon Jug Shelf Test Procedure Patient sits comfortably in front of bookcase. Instruct the patient to keep back straight, head up, not lean forward, use legs as primary source of power for lift, and abort if any feelings of discomfort. Provide a test trial and evaluate/correct form. Remind patient to move 1 jug at a time, not alternate hands, and begin test standing up. Begin trial with “Ready” followed by “Go!” Stop test when 5 th jug placed on the top shelf.
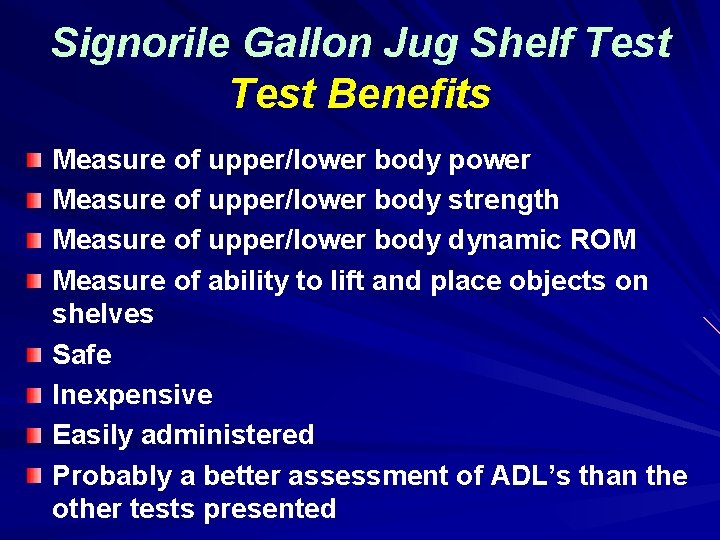
Signorile Gallon Jug Shelf Test Benefits Measure of upper/lower body power Measure of upper/lower body strength Measure of upper/lower body dynamic ROM Measure of ability to lift and place objects on shelves Safe Inexpensive Easily administered Probably a better assessment of ADL’s than the other tests presented
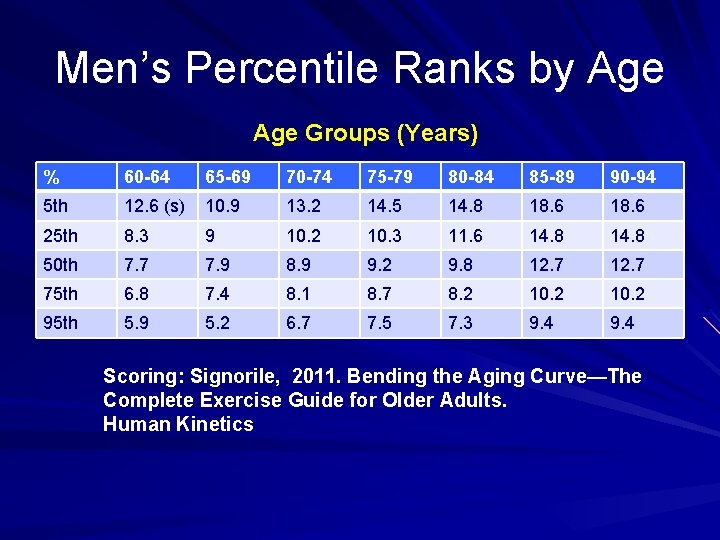
Men’s Percentile Ranks by Age Groups (Years) % 60 -64 65 -69 70 -74 75 -79 80 -84 85 -89 90 -94 5 th 12. 6 (s) 10. 9 13. 2 14. 5 14. 8 18. 6 25 th 8. 3 9 10. 2 10. 3 11. 6 14. 8 50 th 7. 7 7. 9 8. 9 9. 2 9. 8 12. 7 75 th 6. 8 7. 4 8. 1 8. 7 8. 2 10. 2 95 th 5. 9 5. 2 6. 7 7. 5 7. 3 9. 4 Scoring: Signorile, 2011. Bending the Aging Curve—The Complete Exercise Guide for Older Adults. Human Kinetics
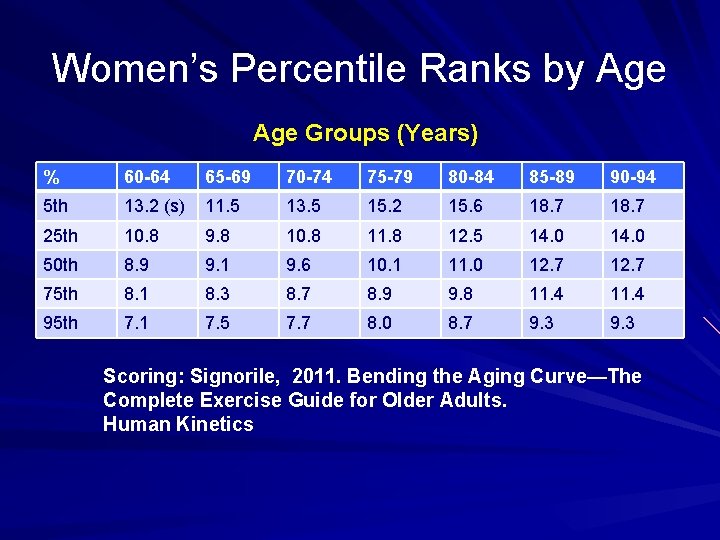
Women’s Percentile Ranks by Age Groups (Years) % 60 -64 65 -69 70 -74 75 -79 80 -84 85 -89 90 -94 5 th 13. 2 (s) 11. 5 13. 5 15. 2 15. 6 18. 7 25 th 10. 8 9. 8 10. 8 11. 8 12. 5 14. 0 50 th 8. 9 9. 1 9. 6 10. 1 11. 0 12. 7 75 th 8. 1 8. 3 8. 7 8. 9 9. 8 11. 4 95 th 7. 1 7. 5 7. 7 8. 0 8. 7 9. 3 Scoring: Signorile, 2011. Bending the Aging Curve—The Complete Exercise Guide for Older Adults. Human Kinetics

The Handgrip Dynamometer Test
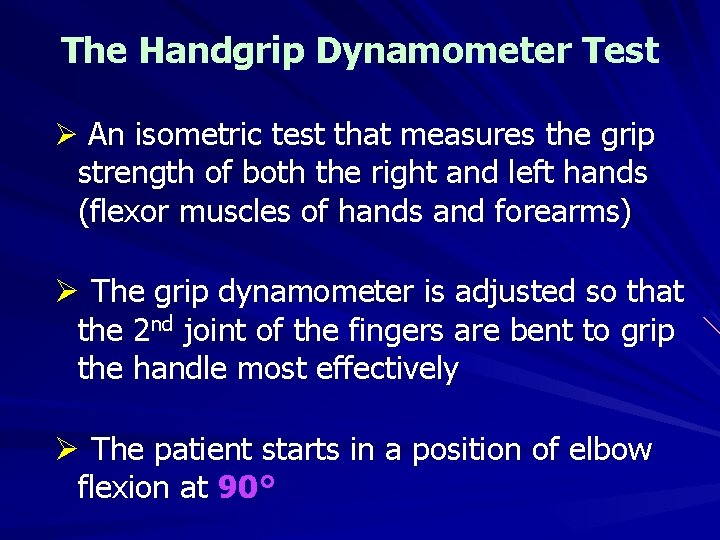
The Handgrip Dynamometer Test Ø An isometric test that measures the grip strength of both the right and left hands (flexor muscles of hands and forearms) Ø The grip dynamometer is adjusted so that the 2 nd joint of the fingers are bent to grip the handle most effectively Ø The patient starts in a position of elbow flexion at 90°
The Handgrip Dynamometer Test Ø The patient squeezes the handgrip dynamometer as hard as possible without holding their breath in each hand Ø The patient may extend the elbow to 180° if desired Ø Grip strength is recorded in kg
The Handgrip Dynamometer Test Ø The patient performs a total of 3 trials Ø The highest if the 3 readings for each hand are combined and compared to the normative values* Ø This test can be used for multiple patient populations, but normative data is lacking Ø Grip strength does not correlate with overall body strength (in most studies) *Normative values for healthy men and women can be found in the ACSM Health-Related Physical Fitness Assessment Manual (2014) Philadelphia: Wolters/Kluwer, LWW, p. 80
IN CONCLUSION… Maintaining muscular strength and endurance is critical for longevity, daily functioning and QOL for all patients in cardiopulmonary or cancer rehab. While musculoskeletal testing may not be a “billable” procedure, we should all be doing this for “best practices” and optimal patient assessment and feedback, as well as patient outcomes. Muscular strength and endurance testing should become a significant component of the patient’s ITP, regardless of what type of chronic disease(s) that may be present.
- Slides: 78