Reproductive system AP mod 16 Reproductiv e system




- Slides: 40
Reproductive system A&P mod 16
Reproductiv e system 4 main functions: • Production of gametes • Fertilization • Development • Production of reproductive hormones
Males
Functional unit Both endocrine and exocrine glands Housed outside the body in scrotum Testes: Formed by 2 months of development but don’t descend until 8 months Covered with thick protective tissue capsule Divided into several hundred lobules Seminiferous tubules empty into rete testes Rete testes empty into epididymis
Sperm • Move from testes to epididymis to mature • Once mature, move to vas deferens • Move around bladder to ejaculatory ducts which are connected to seminal vesicles • Ejaculatory ducts push sperm through urethra and out • Internal urethral sphincter closes off bladder during intercourse • Seminal vesicles secrete seminal fluid • Smallest of all human cells
Prostate gland Exocrine gland that surrounds the urethra at the base of the bladder Produces prostatic fluid
Bulbourethral glands • Two of them • Secrete mucus that is viscous and basic to lubricate urethra for the semen to easily pass through
Penis • Shaft covered with loosely connected skin to allow for expansion • Skin at tip is firmly attached (unless uncircumcised) • Three erectile tissues that fill with blood when aroused • When a man ejaculates he releases 3 -4 ml of semen
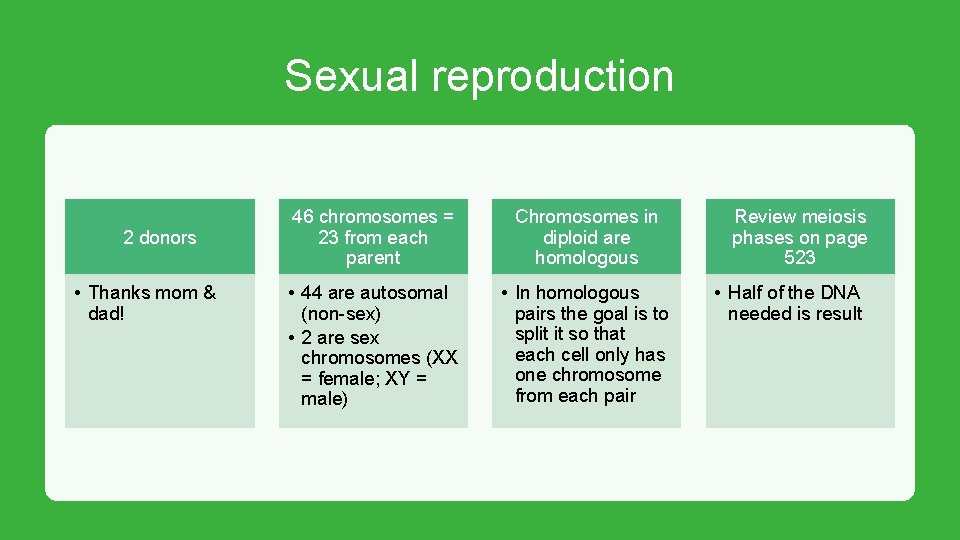
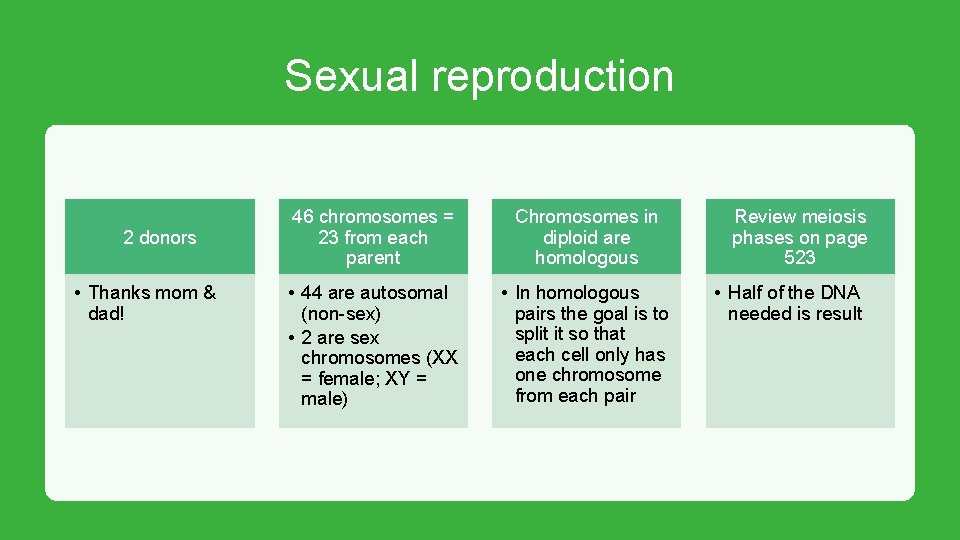
Sexual reproduction 2 donors • Thanks mom & dad! 46 chromosomes = 23 from each parent Chromosomes in diploid are homologous • 44 are autosomal (non-sex) • 2 are sex chromosomes (XX = female; XY = male) • In homologous pairs the goal is to split it so that each cell only has one chromosome from each pair Review meiosis phases on page 523 • Half of the DNA needed is result
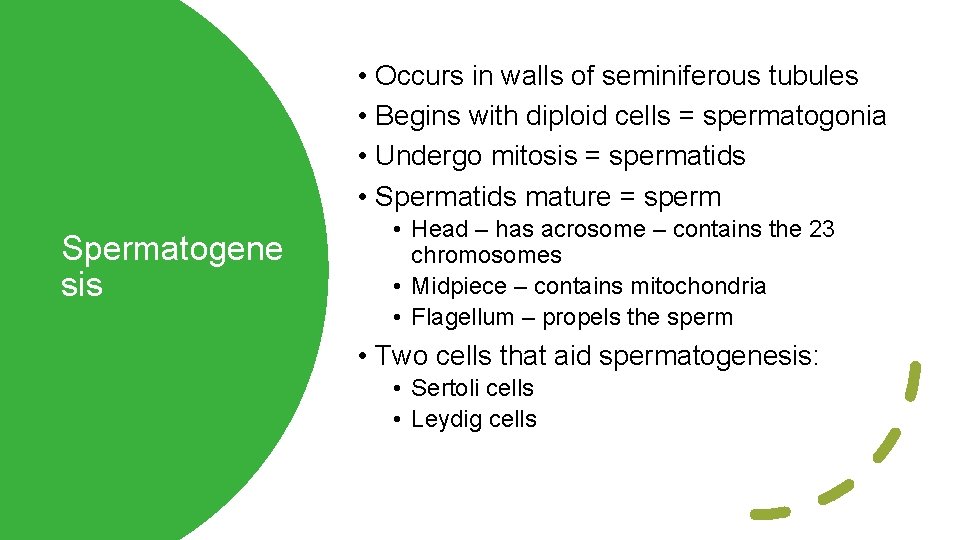
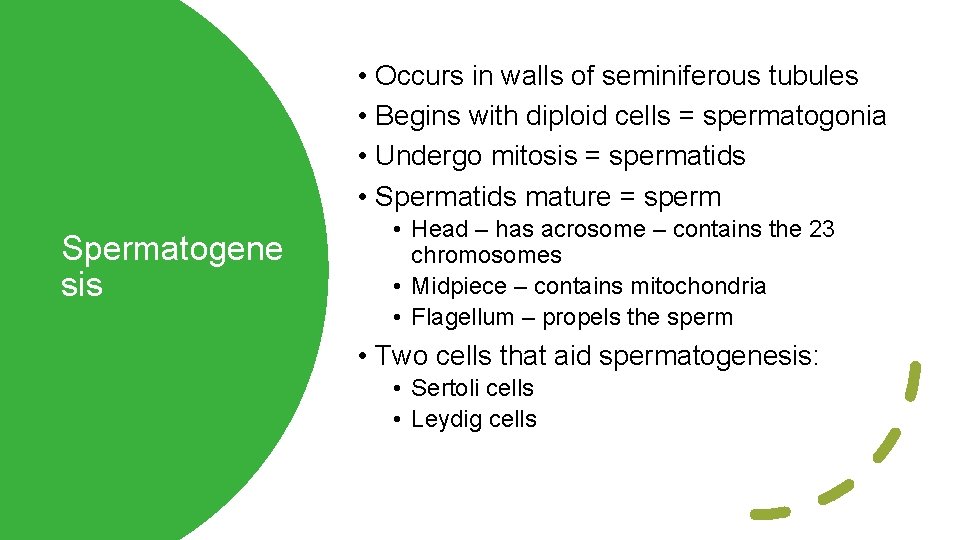
• Occurs in walls of seminiferous tubules • Begins with diploid cells = spermatogonia • Undergo mitosis = spermatids • Spermatids mature = sperm Spermatogene sis • Head – has acrosome – contains the 23 chromosomes • Midpiece – contains mitochondria • Flagellum – propels the sperm • Two cells that aid spermatogenesis: • Sertoli cells • Leydig cells
Hormonal control = testosterone • Male embryo must produce testosterone to form male reproductive organs • If embryo does not produce testosterone the testes will not descend • Affect secondary sex characteristics • Also helps to maintain male reproductive organs • Necessary for spermatogenesis • Release begins with Gn. RH – stimulates release of LH & FSH
Females
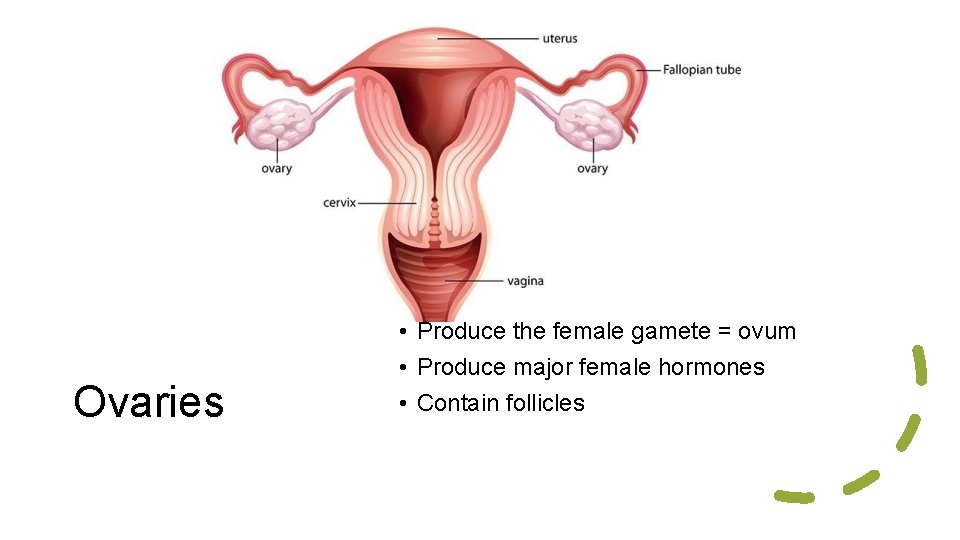
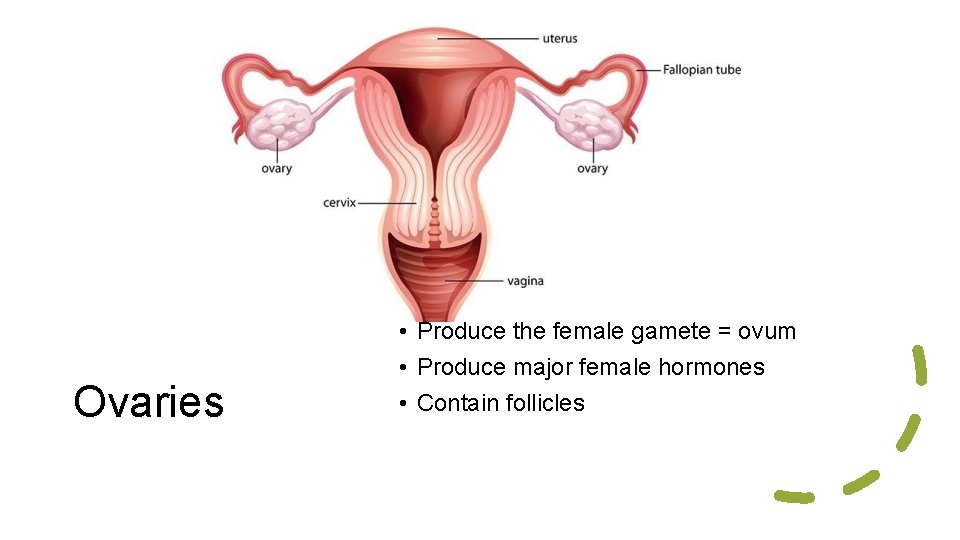
Ovaries • Produce the female gamete = ovum • Produce major female hormones • Contain follicles
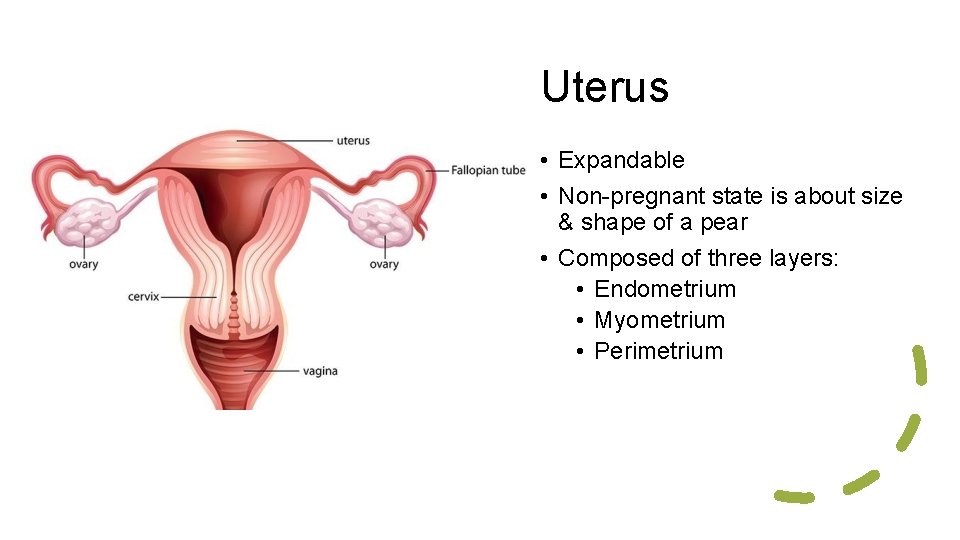
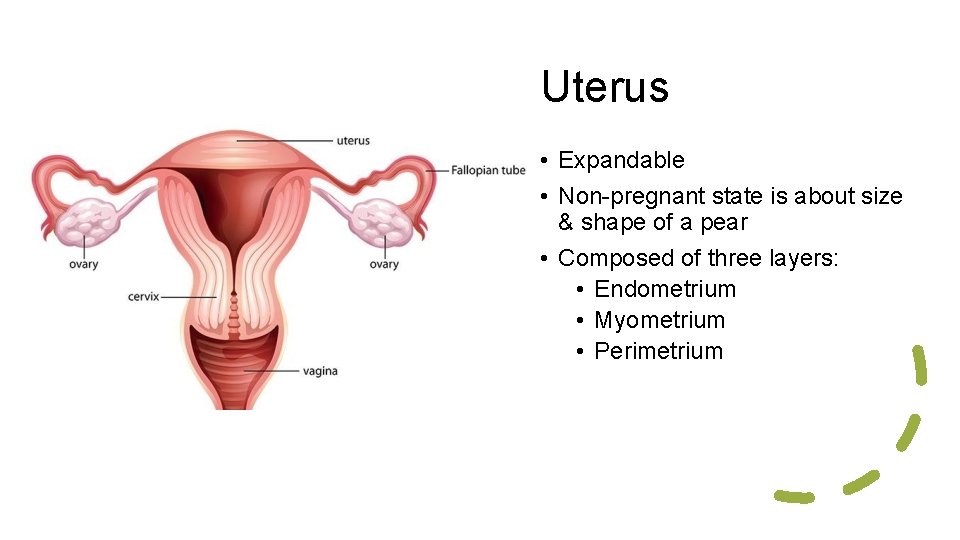
Uterus • Expandable • Non-pregnant state is about size & shape of a pear • Composed of three layers: • Endometrium • Myometrium • Perimetrium
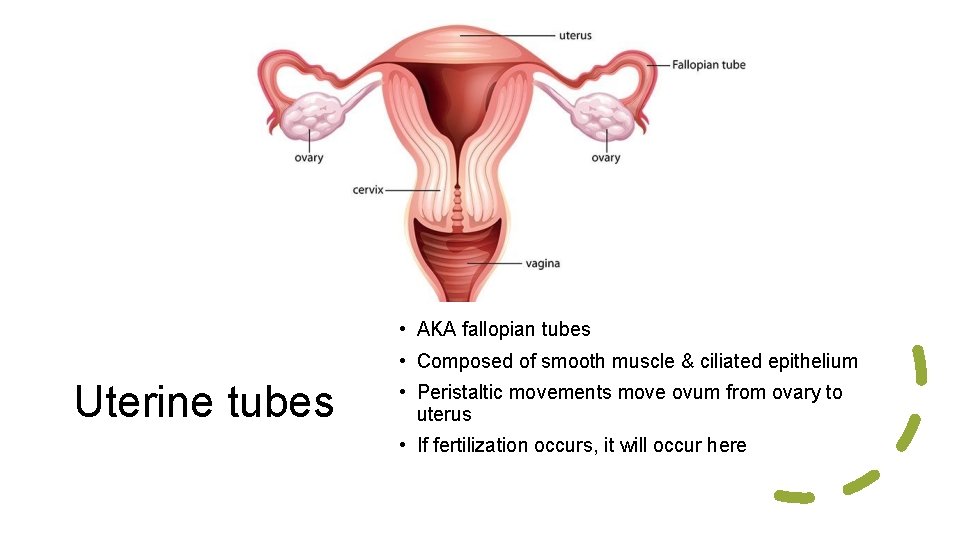
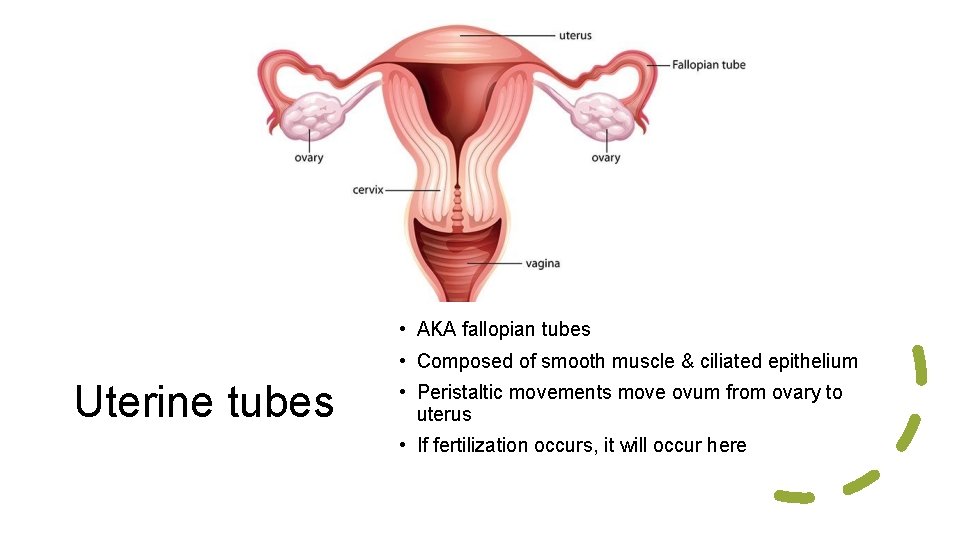
• AKA fallopian tubes • Composed of smooth muscle & ciliated epithelium Uterine tubes • Peristaltic movements move ovum from ovary to uterus • If fertilization occurs, it will occur here
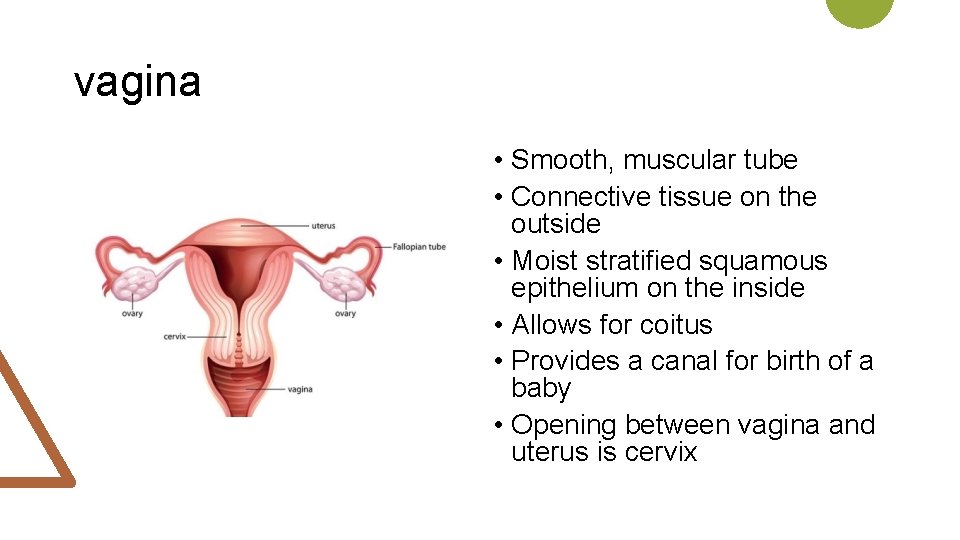
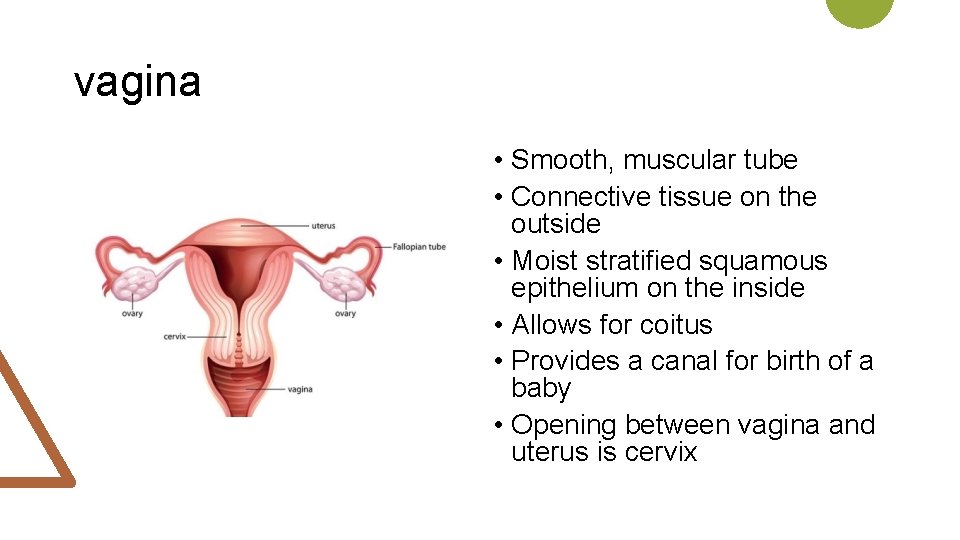
vagina • Smooth, muscular tube • Connective tissue on the outside • Moist stratified squamous epithelium on the inside • Allows for coitus • Provides a canal for birth of a baby • Opening between vagina and uterus is cervix
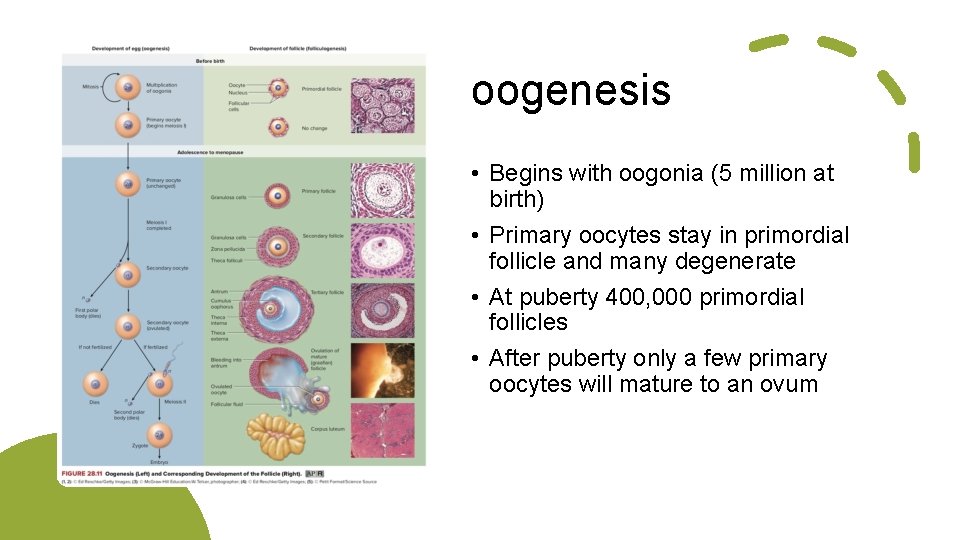
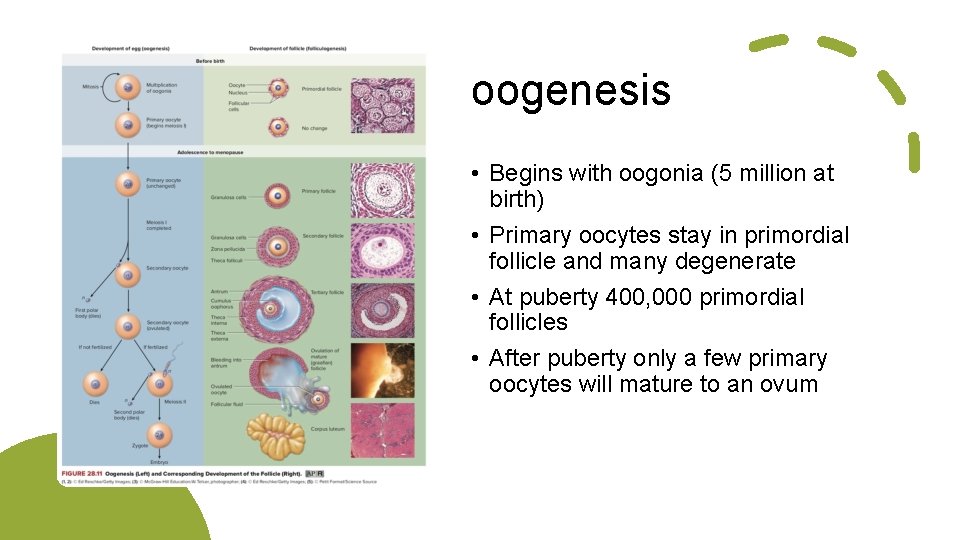
oogenesis • Begins with oogonia (5 million at birth) • Primary oocytes stay in primordial follicle and many degenerate • At puberty 400, 000 primordial follicles • After puberty only a few primary oocytes will mature to an ovum
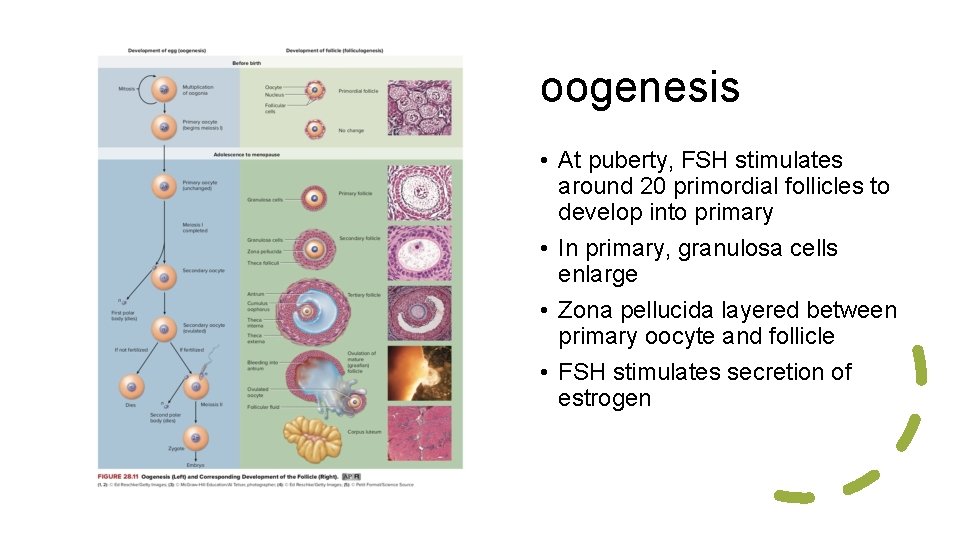
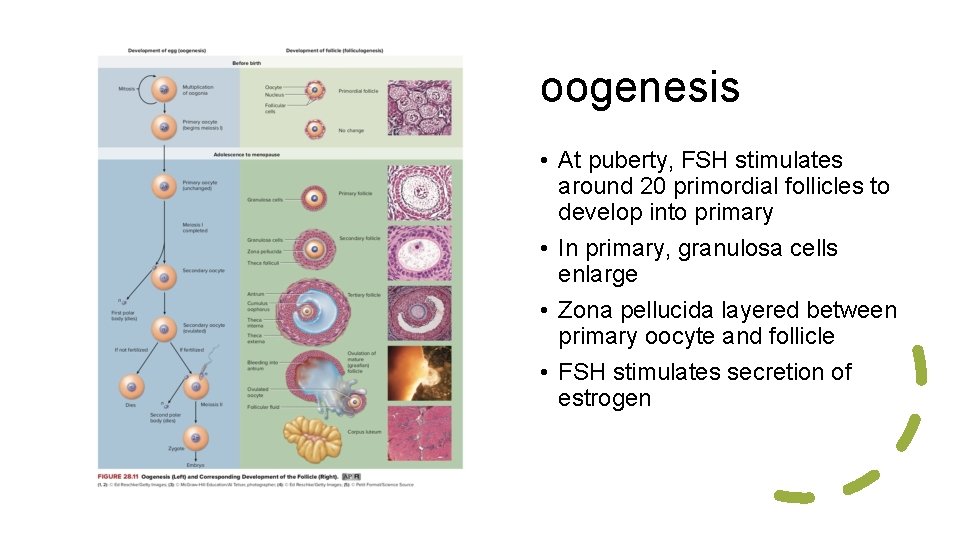
oogenesis • At puberty, FSH stimulates around 20 primordial follicles to develop into primary • In primary, granulosa cells enlarge • Zona pellucida layered between primary oocyte and follicle • FSH stimulates secretion of estrogen
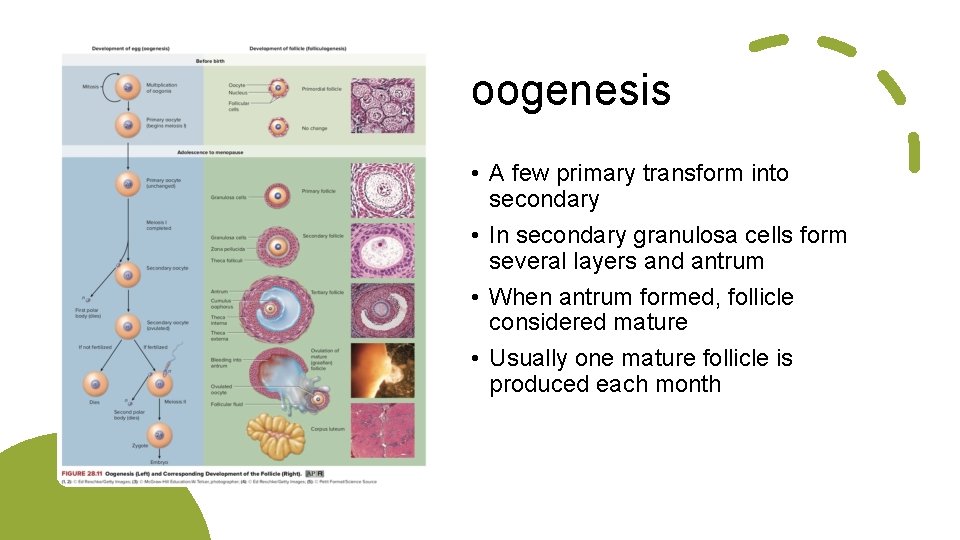
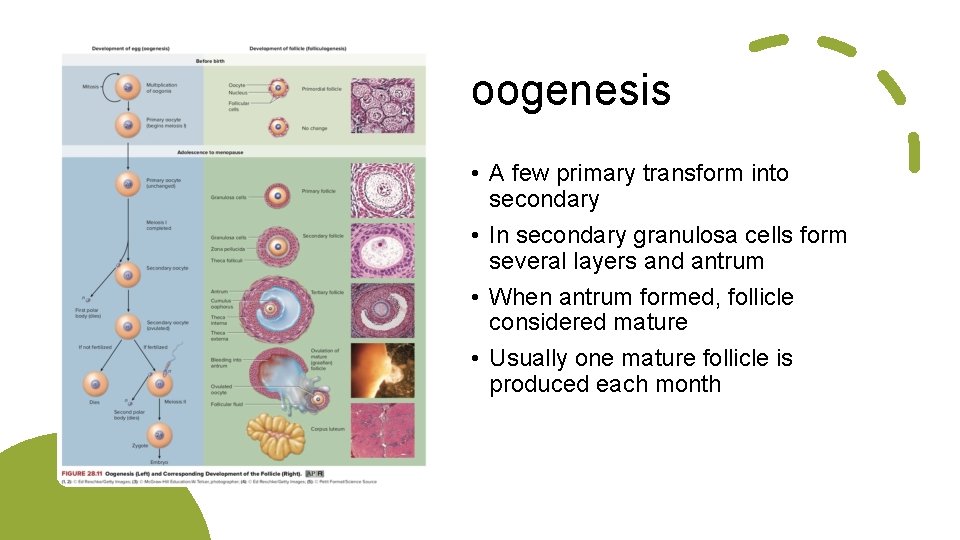
oogenesis • A few primary transform into secondary • In secondary granulosa cells form several layers and antrum • When antrum formed, follicle considered mature • Usually one mature follicle is produced each month
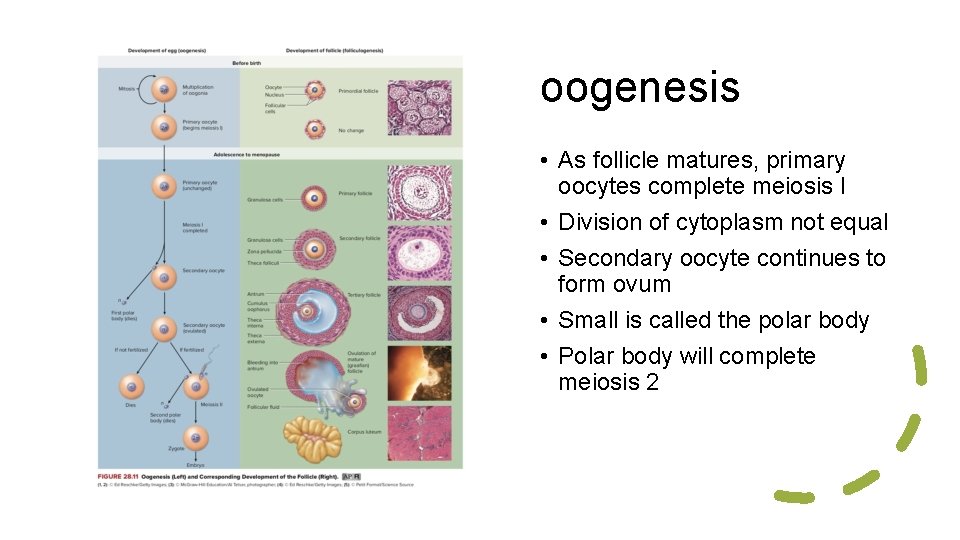
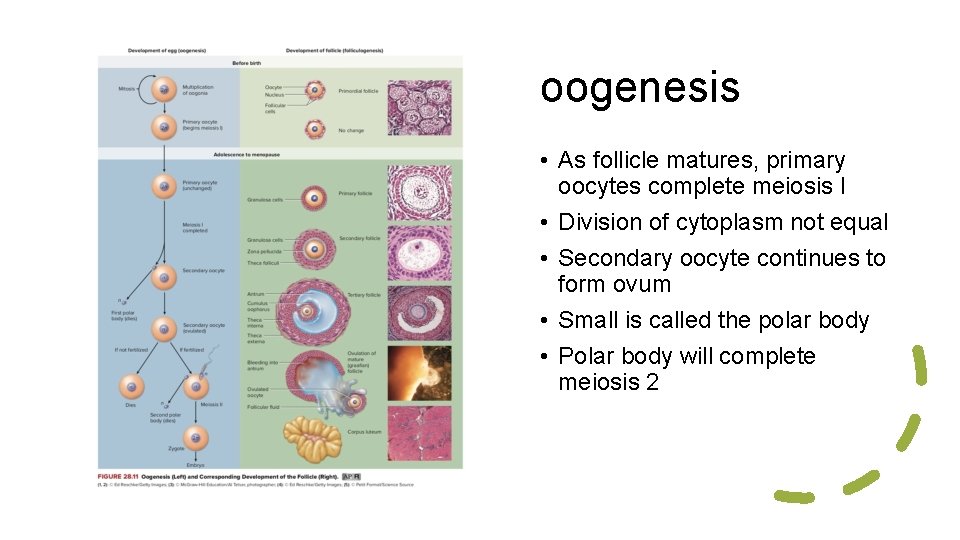
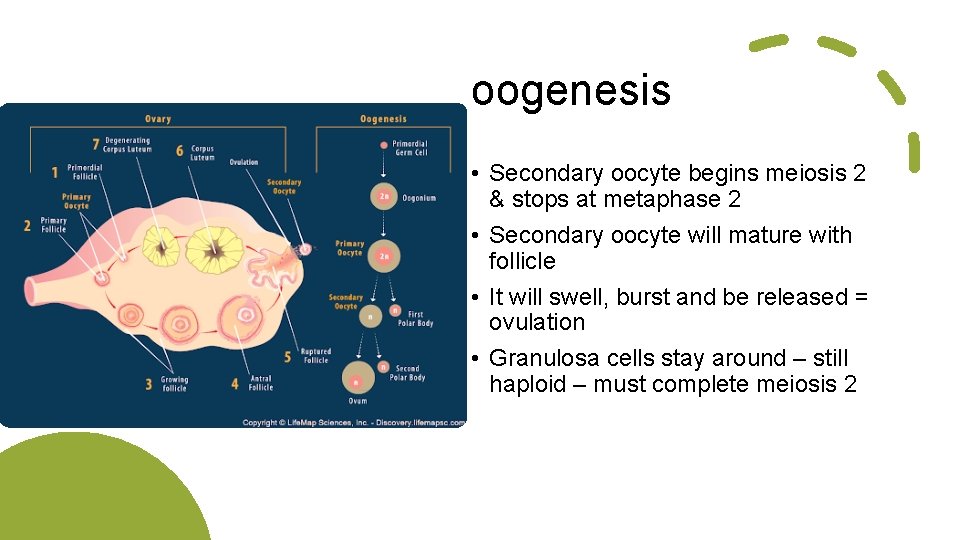
oogenesis • As follicle matures, primary oocytes complete meiosis I • Division of cytoplasm not equal • Secondary oocyte continues to form ovum • Small is called the polar body • Polar body will complete meiosis 2
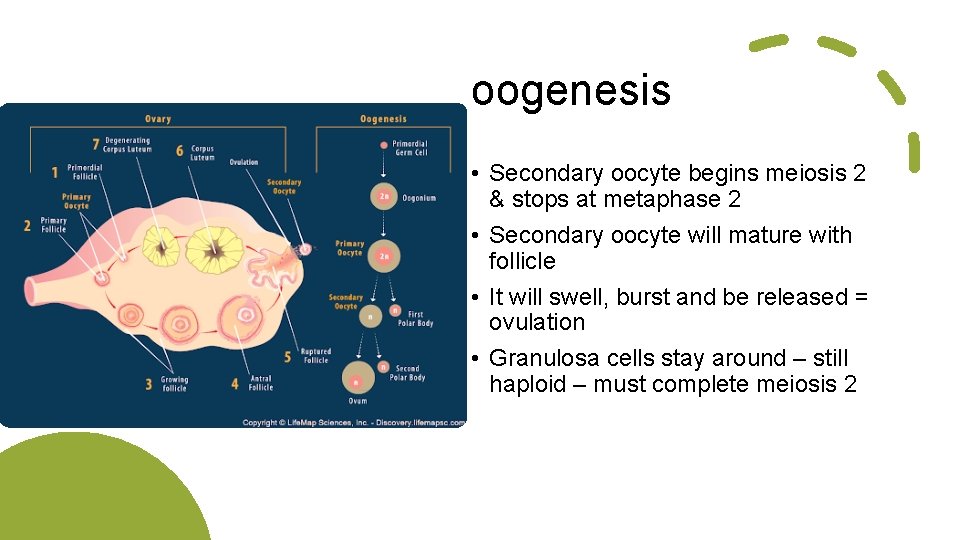
oogenesis • Secondary oocyte begins meiosis 2 & stops at metaphase 2 • Secondary oocyte will mature with follicle • It will swell, burst and be released = ovulation • Granulosa cells stay around – still haploid – must complete meiosis 2
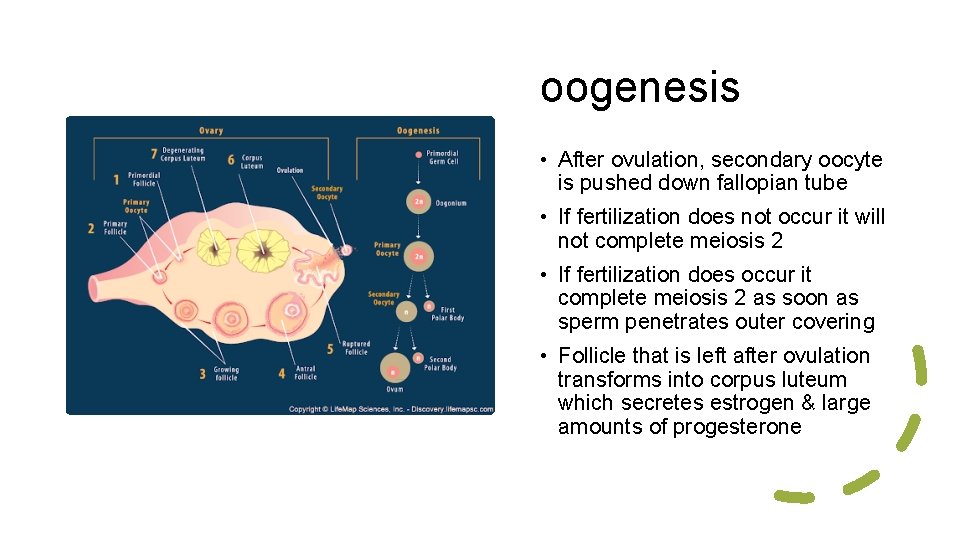
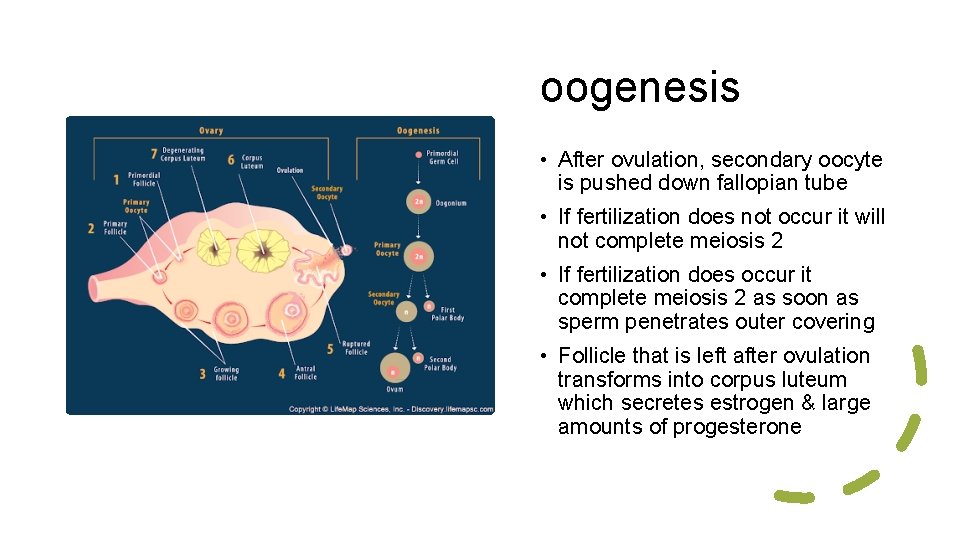
oogenesis • After ovulation, secondary oocyte is pushed down fallopian tube • If fertilization does not occur it will not complete meiosis 2 • If fertilization does occur it complete meiosis 2 as soon as sperm penetrates outer covering • Follicle that is left after ovulation transforms into corpus luteum which secretes estrogen & large amounts of progesterone
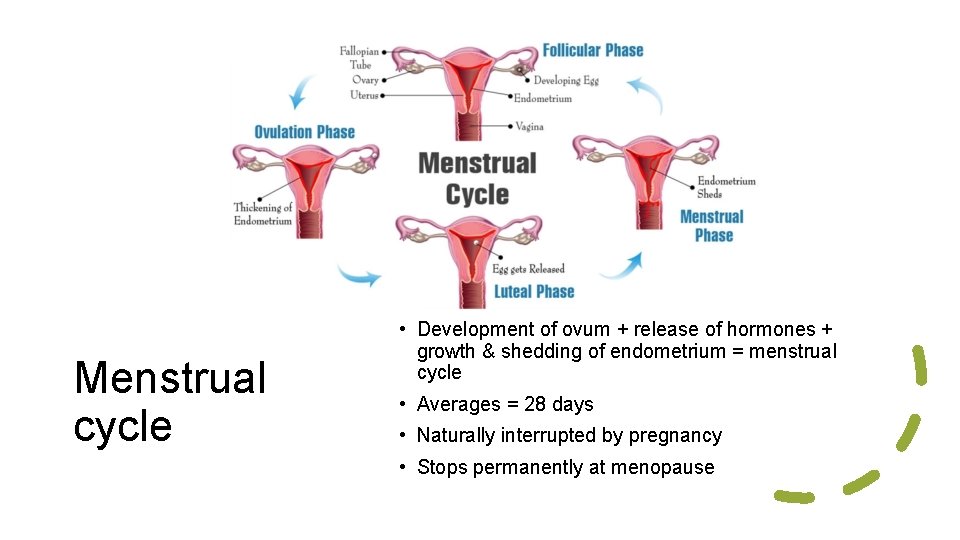
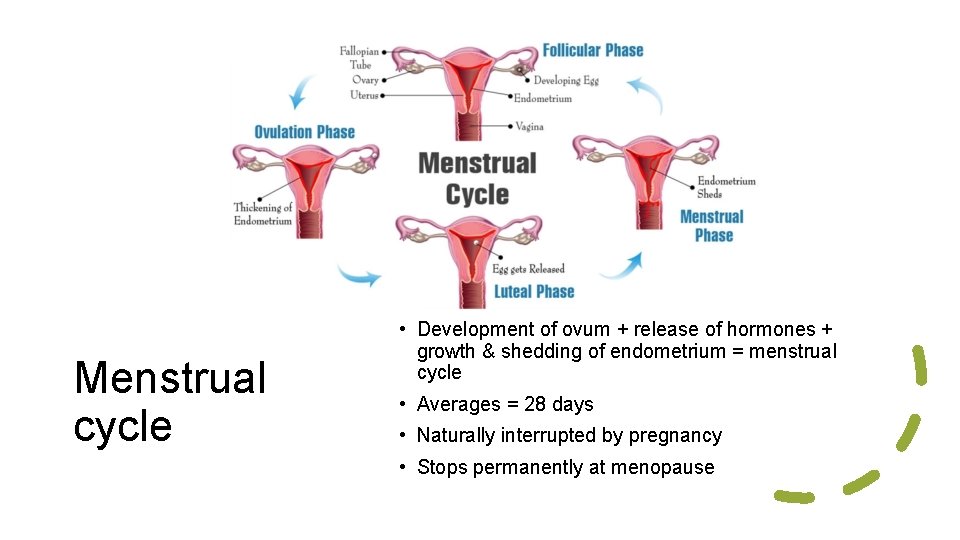
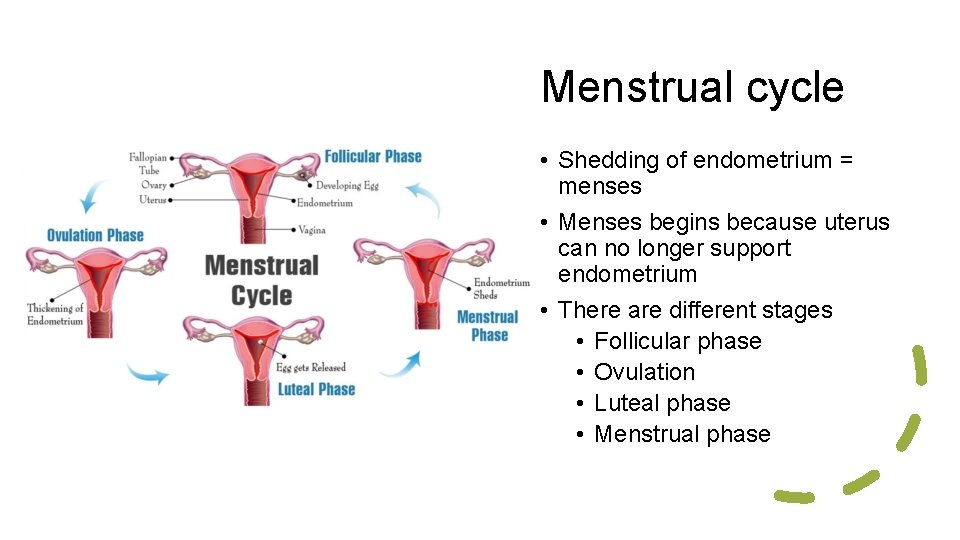
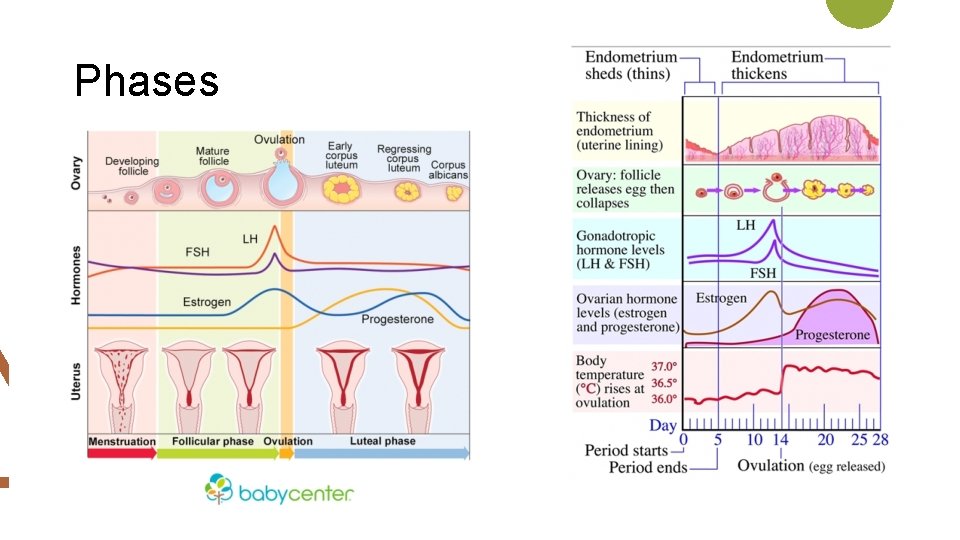
Menstrual cycle • Development of ovum + release of hormones + growth & shedding of endometrium = menstrual cycle • Averages = 28 days • Naturally interrupted by pregnancy • Stops permanently at menopause
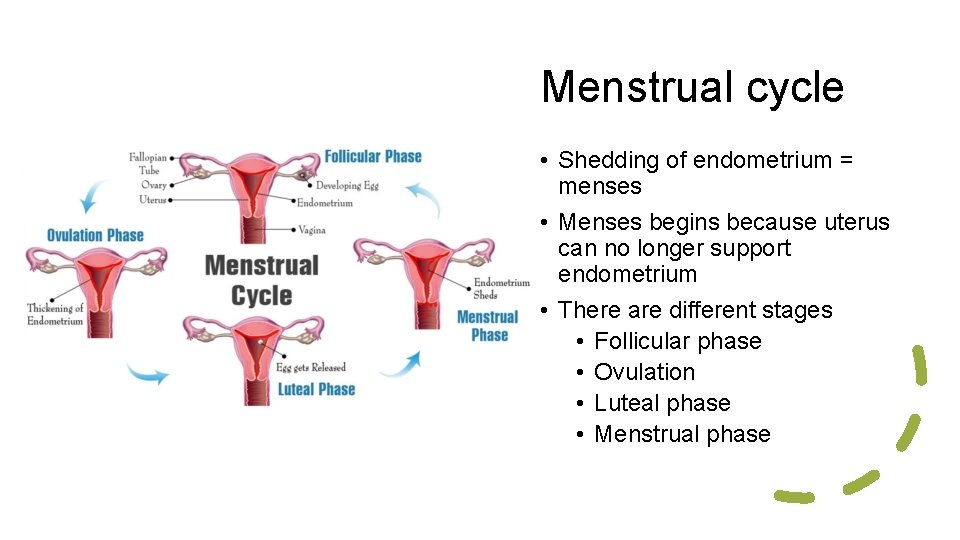
Menstrual cycle • Shedding of endometrium = menses • Menses begins because uterus can no longer support endometrium • There are different stages • Follicular phase • Ovulation • Luteal phase • Menstrual phase
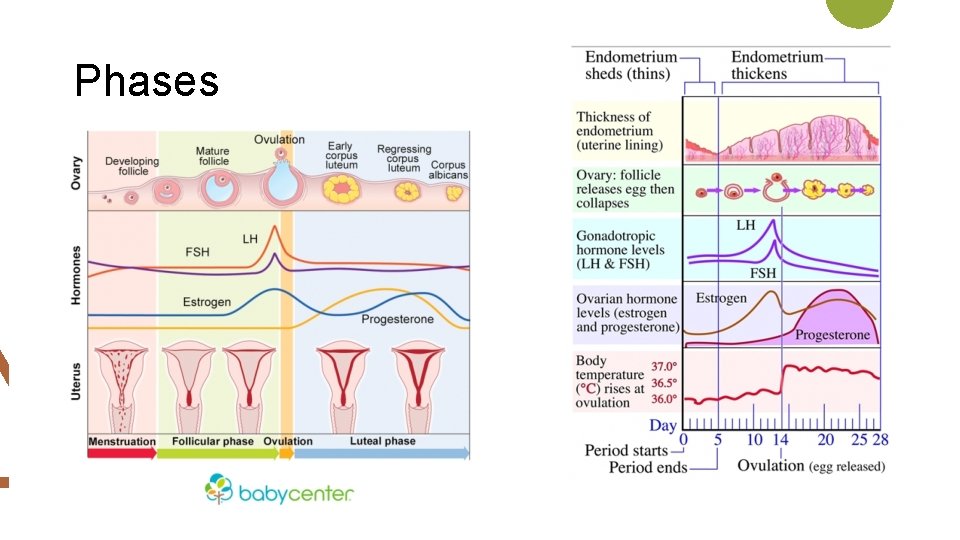
Phases
If fertilization occurs = BIG, BIG changes occur Usually “missing” a period signals pregnancy, but other things can cause one to miss a period Female hormones Progesterone: • Increase endometrium for pregnancy • Causes smooth muscle to relax in order to stretch • Functions mainly during luteal phase & pregnancy Estrogen • Maintains female reproductive organs • Initiates female secondary sex characteristics Both levels raise during pregnancy

Fertilization, development & parturition
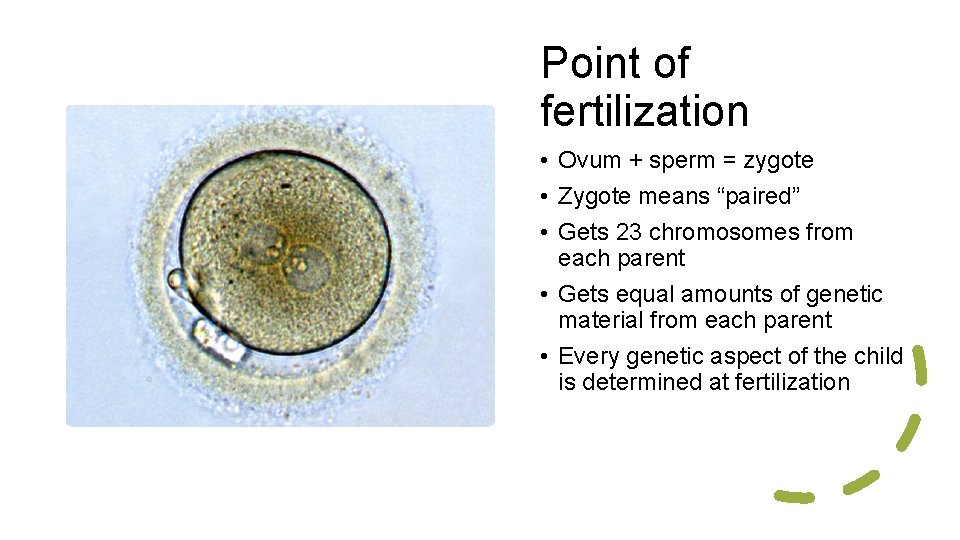
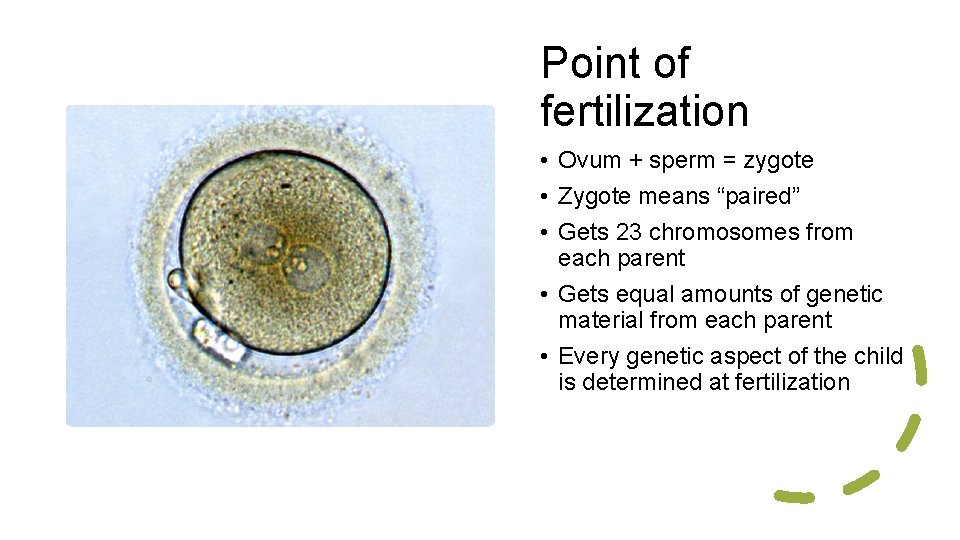
Point of fertilization • Ovum + sperm = zygote • Zygote means “paired” • Gets 23 chromosomes from each parent • Gets equal amounts of genetic material from each parent • Every genetic aspect of the child is determined at fertilization
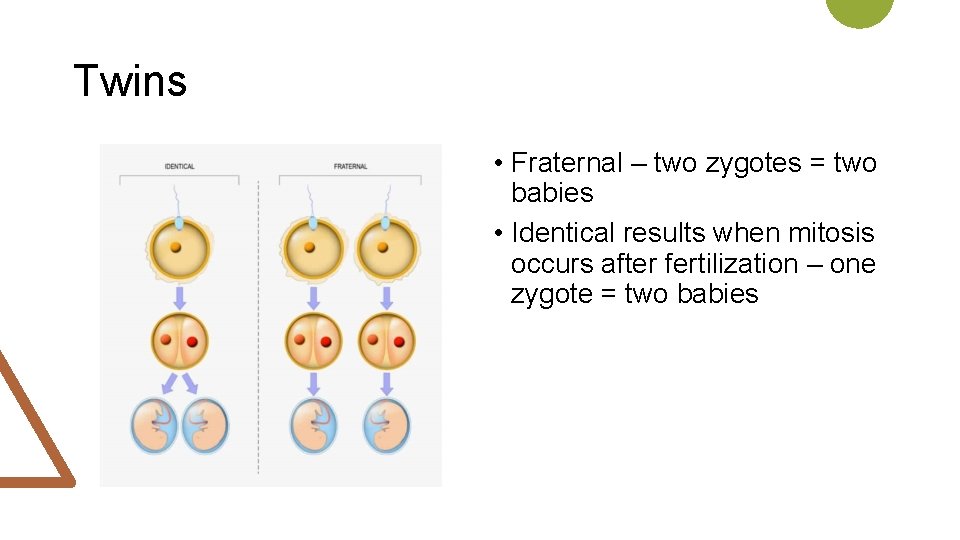
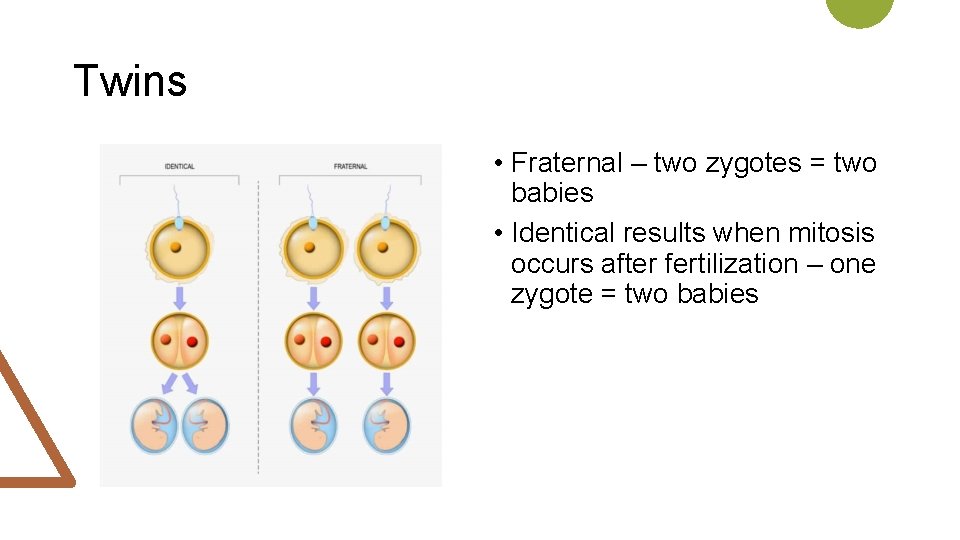
Twins • Fraternal – two zygotes = two babies • Identical results when mitosis occurs after fertilization – one zygote = two babies
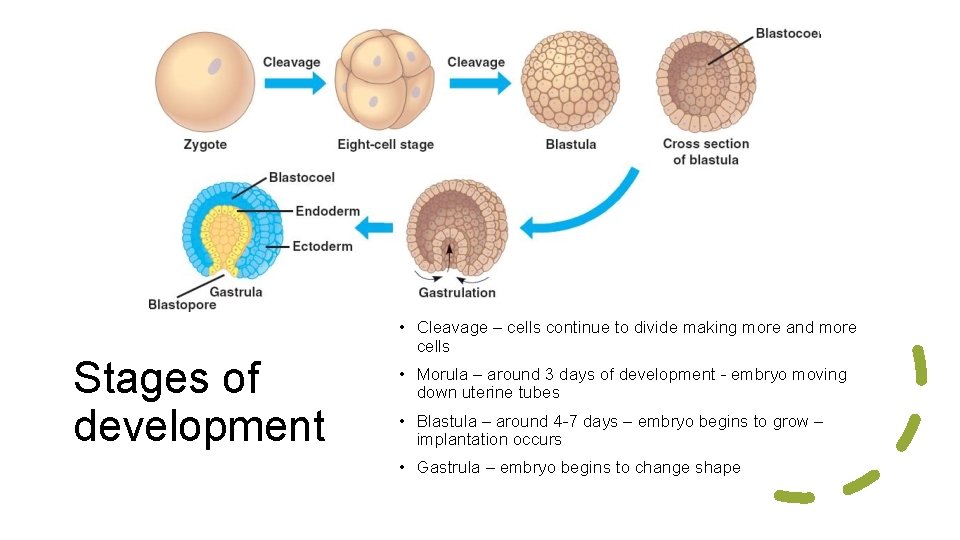
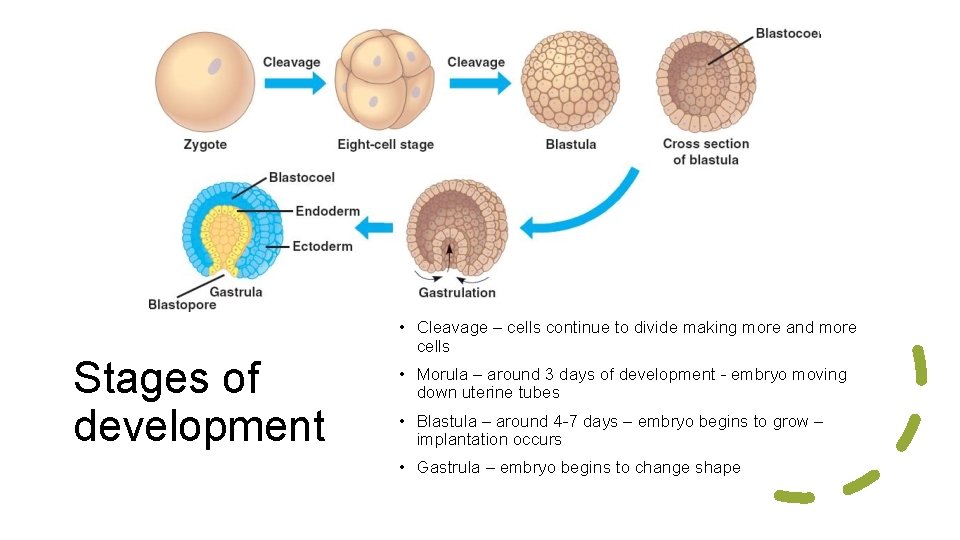
Stages of development • Cleavage – cells continue to divide making more and more cells • Morula – around 3 days of development - embryo moving down uterine tubes • Blastula – around 4 -7 days – embryo begins to grow – implantation occurs • Gastrula – embryo begins to change shape
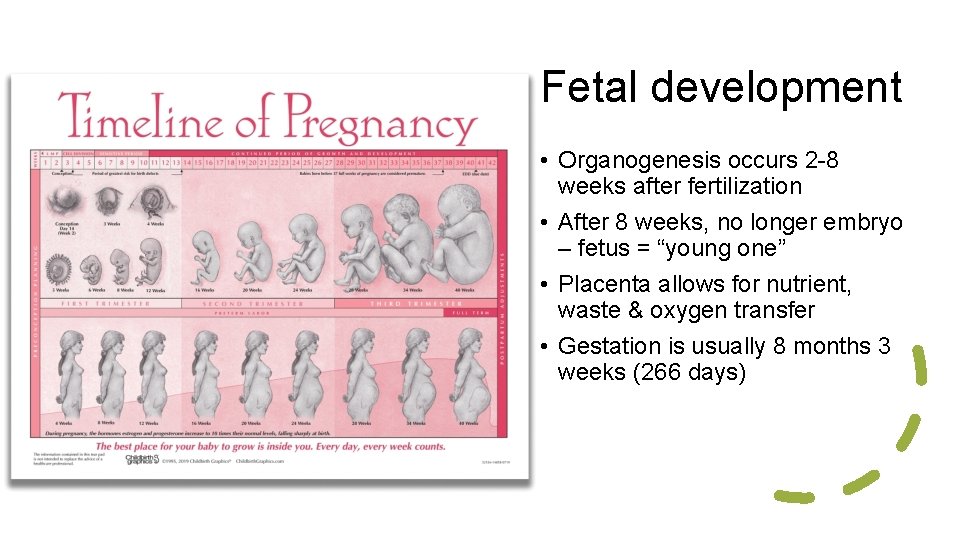
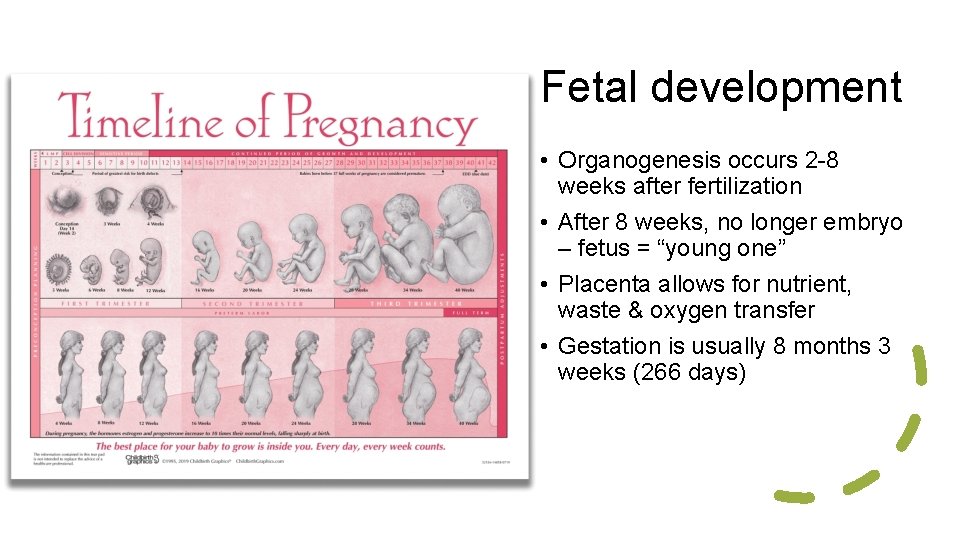
Fetal development • Organogenesis occurs 2 -8 weeks after fertilization • After 8 weeks, no longer embryo – fetus = “young one” • Placenta allows for nutrient, waste & oxygen transfer • Gestation is usually 8 months 3 weeks (266 days)
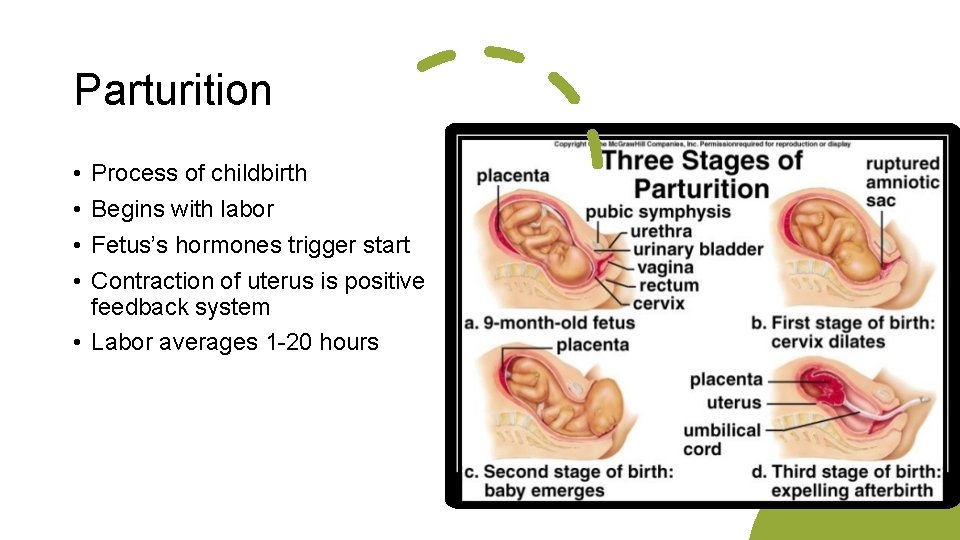
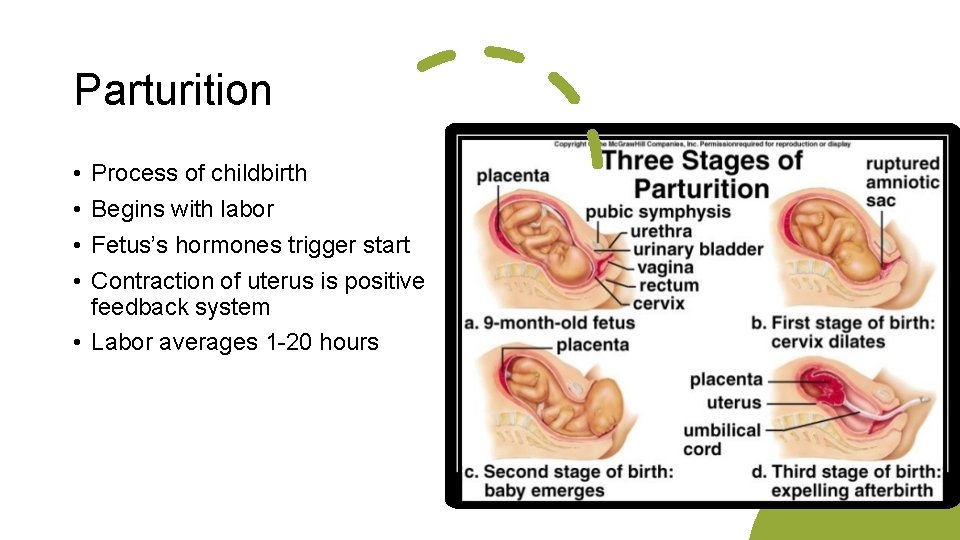
Parturition • • Process of childbirth Begins with labor Fetus’s hormones trigger start Contraction of uterus is positive feedback system • Labor averages 1 -20 hours
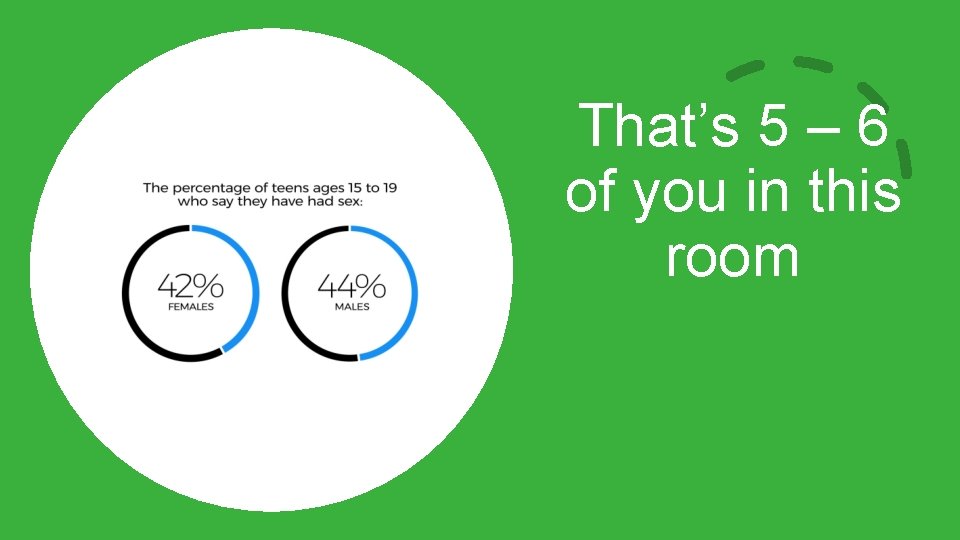
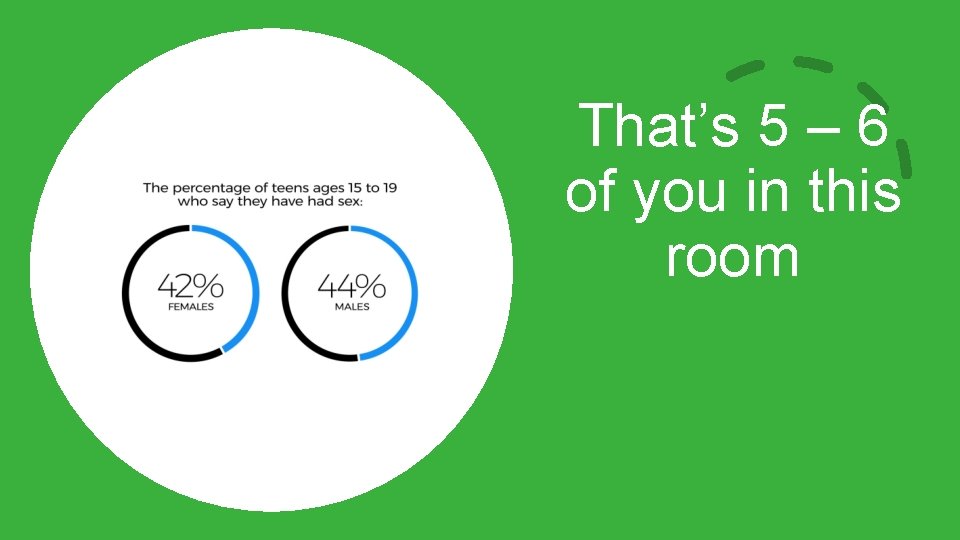
That’s 5 – 6 of you in this room

How far is too far?
Real love waits – and does not ask you to sin!
Pornography is sex Matthew 5: 27 -29
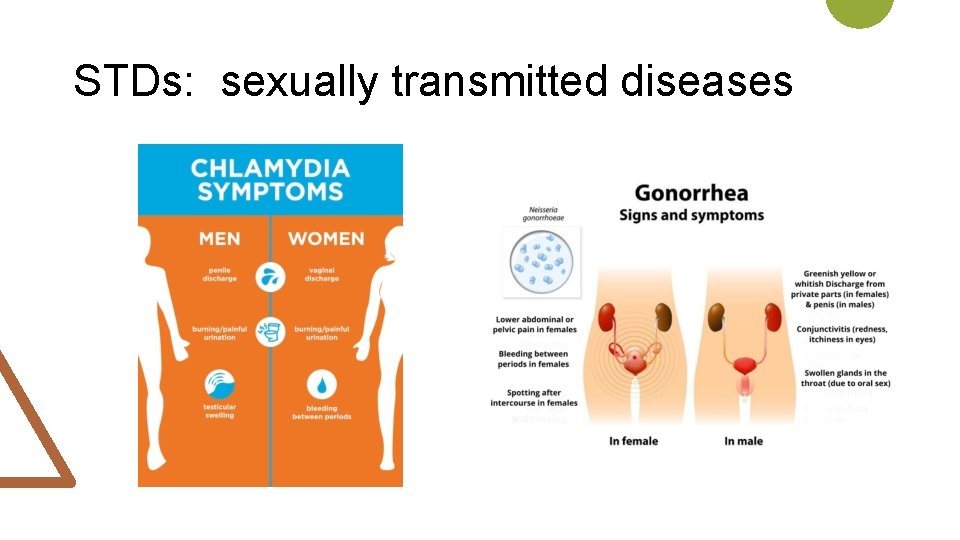
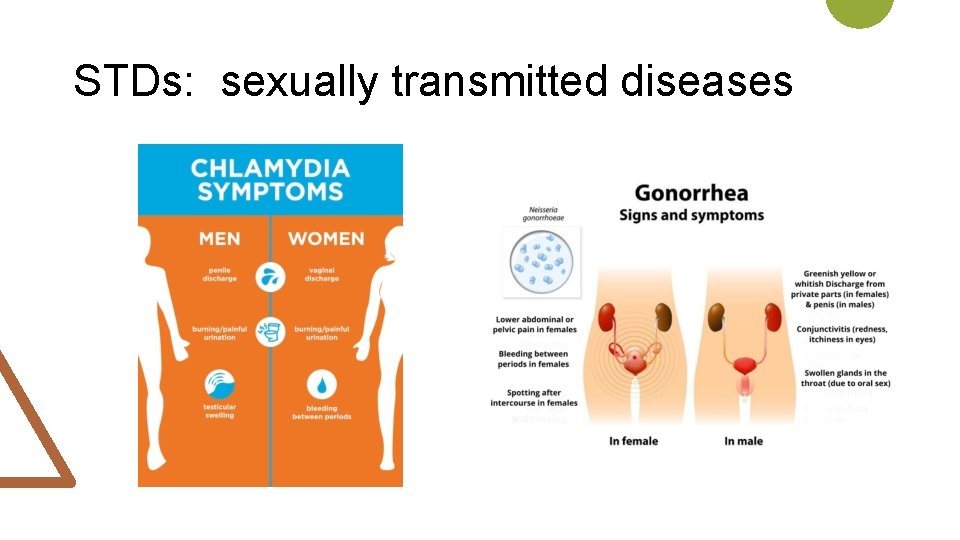
STDs: sexually transmitted diseases
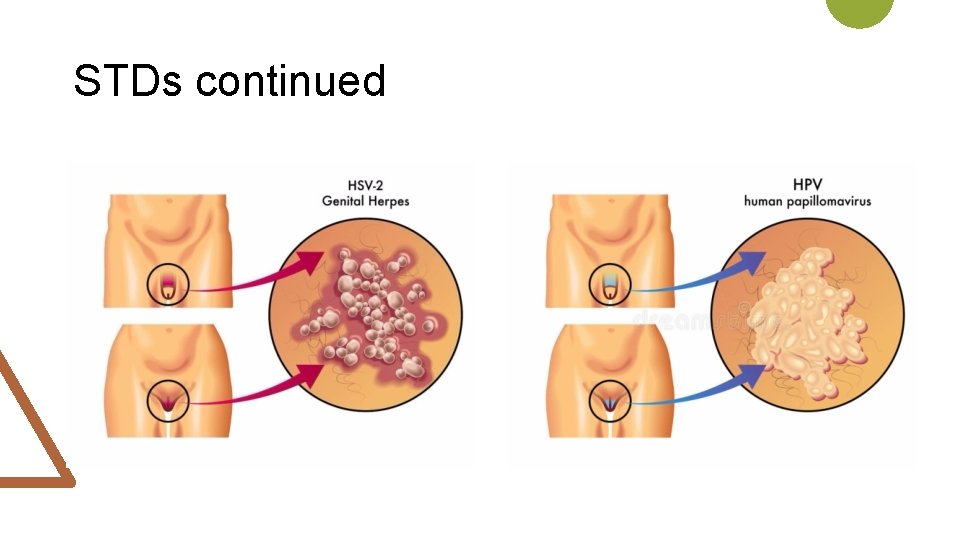
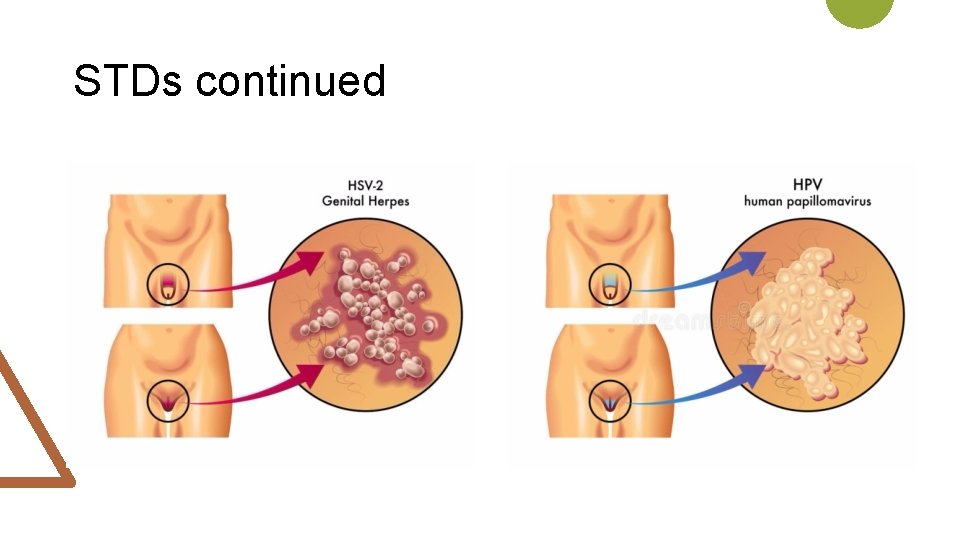
STDs continued

STDs continued

Best prevention: Abstinence