Reproductive Cancers Endometrial Uterine CA Cervical CA Ovarian
- Slides: 35
Reproductive Cancers Endometrial (Uterine) CA Cervical CA Ovarian CA Testicular CA
Endometrial (Uterine) Cancer n n n Most common malignancy of female genital tract Adenocarcinoma is the most common type of tumor Related to overstimulation of endometrium by excessive circulating estrogen High cumulative exposure to estrogen is strong risk factor (Brunner, p. 1459 Chart 47 -7)
Endometrial (Uterine) Cancer n n n Most common GYN malignancy Develops in glandular cells – inner, endometrial lining Endometrial hyperplasia is precursor of endometrial cancer Risk factors: (see table next slide) Manifestation: post menopausal bleeding Annual screening with biopsy for high risk cases
Endometrial (Uterine) Cancer n n n Most common GYN malignancy Develops in glandular cells – inner, endometrial lining Endometrial hyperplasia is precursor of endometrial cancer Risk factors: (see table next slide) Manifestation: post menopausal bleeding Annual screening with biopsy for high risk cases
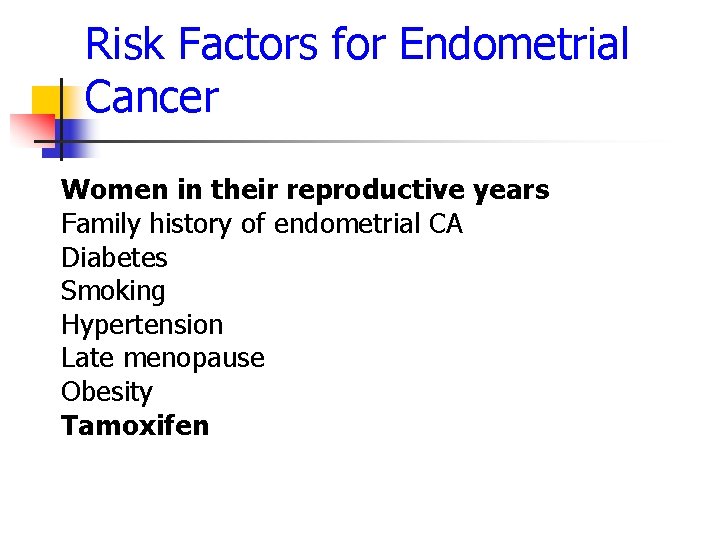
Risk Factors for Endometrial Cancer Women in their reproductive years Family history of endometrial CA Diabetes Smoking Hypertension Late menopause Obesity Tamoxifen
Endometrial Cancer. Treatment n n n Medical intervention- internal radiation therapy (IRT) radioisotope placed in vagina. . 1 -3 days. Management of Internal Radium: Restrict to bed rest and visitors; elevate head bed 20 degree External radiation: for Stage II or II cancers Surgical intervention- total hysterectomy and bilateral salpingoophorectomy (BSO)- removal of uterus, fallopian tubes, and ovaries Complications: vaginal and rectal bleeding, hematuria, foulsmelling discharge, abdominal pain or distension to be reported
Cervical Cancer n n n Most arise from columnar cells on the outer cervix; may be the reason why adolescents are more vulnerable to sexually transmitted infections (STIs) Incidence rates have decreased steadily over past several decades in both white and African Americans African American and Native American have higher incidence
Risk Factors for Cervical Cancer n n n Infection with human papilloma virus (HPV) Multiple sex partners Early age sexual intercourse Low socioeconomic status Untreated chronic cervicitis n n n STI Sexual partner with history of penile or prostate cancer Chart 47 -5 p. 1457 Brunner
Cervical Cancer n n n Early Symptoms: Thin watery vaginal discharge Bloody spotting after coitus or douching Metrorrhagia or Polymenorrhea (bleeding not coinciding with menstrual cycle “spotting”) Post menopausal bleeding
Cervical Cancer Late Symptoms: n n n n n Painless vaginal bleeding Dark, foul-smelling vaginal discharge Flank pain or pelvic Weight loss Anorexia Leg edema Hematuria (bloody urine) Dysuria (painful urination) Rectal bleeding
Cervical Cancer Management n n n Pap Smear- primary diagnostic tool for diagnosis Colposcopy- provides an in situ macroscopic exam of vagina and cervix. Performed after abnormal pap smears. Useful in identifying suspicious lesion, definitive dx = biopsy Cryotherapy – freezing and destruction of cells Loop electrocaudery-LEEP procedure. Excision of cervical areas affected Total Hysterectomy - laproscopic
Treatment/Management n n n Radiation- used for early cervical cancer. Curative. Induces menopause. Not given to pelvic wall. Radical hysterectomy with pelvic lymphadectomy Chemotherapy- poor effect, given for unresectable tumors.
Ovarian Cancer n n Ovarian cancer is leading cause of deaths from genital reproductive malignancies Most ovarian cancers are epithelial tumors, some adenocarcimomas, and are rapid growing and spread bilaterally
Ovarian Cancer Manifestations n n n Pelvic pressure on adjacent organs Abdominal distension, constipation, indigestion Spreads to other ovary and associated structures… bowel, omentum, liver, distant mets spread via lymphatic system. Cancer cells spread in peritoneal cavity and by direct invasion of bowel and bladder Involve pelvic and para aortic lymph nodes. Abnormal bleeding if endometrium stimulated
Ovarian Cancer dx. Tests n n Ca 125 - tumor marker highly specific to epithelial ovarian cancer Transvaginal or transabdominal ultrasonography- used to detect ovarian size and detect mass. Laparoscope - determine definitive dx. and organ involvement. Unable to determine benign or malignant. CT scan- reveal areas of metastasis
Treatment of Ovarian Cancer n n n Options include surgery, chemotherapy, and occasional radiation therapy Survival depends on age, women younger than 65 are twice as likely to survive to 5 yrs. following diagnosis than women 65 and older. Chemo - not curative, hope to achieve remission of disease.
Internal Radiation: Reproductive Cancers n Intra-cavity implants n n Usually left in place 24 – 72 hours (in detail in chapter 23) Limit contact with other organs n n n Bowel cleansing and low residue diet to prevent fecal distention Foley catheter prevent bladder distention Vaginal packing to support rectum and bladder away from field
Internal Radiation: Reproductive Cancers n n n May stimulate severe uterine contractions – pain management Body position flat to 20 degrees in bed to prevent dislodgement May develop foul smelling discharge from destruction and sloughing of cells Local and systemic side effects Safety for visitors and health care workers?
Hysterectomy n n n Vaginal Hysterectomy: Uterus is removed through vagina. There is no abdominal incision Abdominal Hysterectomy: Uterus is removed through abdominal incision Total abdominal hysterectomy includes uterus and ovaries, possibly lymphnodes
Collaborative Problems and Potential Complications n n Hemorrhage DVT (avoid knee gatch or pillows rolled behind the knees when the patient is lying in bed); use pneumatic compression stocking, apply antiembolic stockings, and assist with range of motion Bladder dysfunction Infection
Post Operative Management n n Same as all post operative clients n Fluid volume evaluation n Prevention of pulmonary complications n Prevention of DVT n Prevention of infection Assessment of bleeding: n Quality of bleeding: Frank versus serosanginous n Number of vaginal pads per shift n Assessing for blood pooling under client
Nursing Process: The Care of the Patient Undergoing a Hysterectomy—Planning n Goals n n n Relief of anxiety Acceptance of loss of the uterus Absence of pain or discomfort Increased knowledge of self-care requirements Absence of complications
Nursing Process: The Care of the Patient Undergoing a Hysterectomy— n Anxiety n n Allow patient to express feelings Explain physical preparations and procedures Provide emotional support Body image n n Listen and address concerns Provide appropriate reassurance Address sexual issues Approach and evaluate each patient individually
Nursing Process: The Care of the Patient Undergoing a Hysterectomy—Interventions (cont’d) n Educate about self-care and continuing care n n n Surgical incision care Maintain bowel and urinary function Resume activities slowly Showers instead of baths Teach: activities to avoid, symptoms to report, follow-up
Clinical Judgment- Patient Centered Care, Teamwork 34 y. o. woman dx with ovarian CA tells you that she “can’t believe this, ” and that ”this must be a wrong dx. ” She states that she and her husband had planned to get pregnant later this year and that she “cannot lose” her ovaries. She is scheduled for a bilateral oophorectomy and hysterectomy in 2 days. Her oncologist told her after she recovers from surgery she would need adjuvant chemotherapy to destroy any remaining CA cells. 1. What pre-procedure teaching will you provide and why? 2. How will you approach the pts feelings about getting pregnant later this year? 3. Do you believe the patient understands the implications of the surgical procedure? n
Testicular Cancer
Testicular Cancer n n Rarely occurs in men younger than age 15 or older than 40 , occurs between age 15 and 35 Pathophysiology – 90 to 95% germinal cell tumors, arise from germinal cells of testes such as seminoma, teratocarcinoma, embryonal carcinoma, yolk sac carcinoma. Nongerminal tumors- adenomas, usually benign. Metastasis occurs through lymphatic spread, enter retroperitoneal nodes or lungs
Risk Factors n n n Undescended testes (cryptoorchidism) Abnormal testicular development Klinefelter’s syndrome (sterility, low level male hormone, small testes) Family history of testicular cancer HIV (+), exposure to chemicals-oil, gas production (No link to prenatal exposure to diethylstilbesterol ACS , 2009 ) p. 1533
Signs/symptoms n n Mass within scrotum enlarges, gradually Painless swelling or nodule in one testicle Heavy, dull ache or pain, discomfort in scrotum or lower abdomen Back pain suggests mets to retroperitoneal lymph nodes.
Diagnosis of Testicular Cancer n n n Palpation of testicle Testicular sonogram and MRI Elevated serum levels of blood for AFP (alpha-fetoprotein) and HCG (human chorionic gonadotropin) LDH-elevated in test. Ca. Transillumination
Patient education- Testicular Self Examination chart 49 -6 p 1534 n n Once a month, usually after warm bath or shower Teaching starting in adolescence Annual examination by the clinician Notify health care provider if testicleindurated, enlarged, atropied, painful
Testicular Cancer Treatment n n n Radical orchiectomy- used to diagnose and treat. Removal of testes, epididymis, and vas deferens. Spermatic cord ligated just inside internal inguinal ring to prevent seeding cancer. Followed by chemo, radiation Retroperitoneal lymph node dissection- high impotence. Infertility due to retrograde ejaculation. Newer procedure- laparoscope node dissection.
Treatments Continued n n Radiation to perineum, pelvis, mediastinal and supraclavicular nodes. Complications can occur… irritable bowel, skin reactions, fatigue, nausea, temporary or permanent infertility. Prognosis- survival rate 80 -90% if early diagnosis. Staged with MRI, CT scan F/U with self testicular exam, F/U CT scans, regular tumor marker levels.
Chemotherapy n n Cisplatin ( Platinol AQ) in combination with etopside ( Toposar) , paclitaxel (Taxol ) Birth control 18 months- 24 months after last cycle of chemo.
Question (no clicker) n a. b. c. d. A client diagnosed with cancer of the uterus is scheduled to have placement of an intra-uterine radiation device. What precautions must the nurse implement? Select all that apply: Place the client in a private room Wear a dosimeter when entering the room Encourage visitors to stay with the client Organize activities to limit time in the room