Reproduction in Humans Introduction Male and female reproductive



- Slides: 36

Reproduction in Humans
Introduction • Male and female reproductive systems • Function together to produce offspring • Female reproductive system nurtures developing offspring • Produce important hormones
MALE REPRODUCTIVE SYSTEM
Male reproductive System • Essentially 4 parts: • Testes • Gonads, in scrotum; make gamates and releases sex hormones • Ducts • Epididymis, sperm ducts • Glands • Seminal vesicles, prostate gland • Penis • Urethra and erectile tissue. Arousal leads to filling of the tissue with blood erection. Enables it to function as a penetrating organ in intercourse
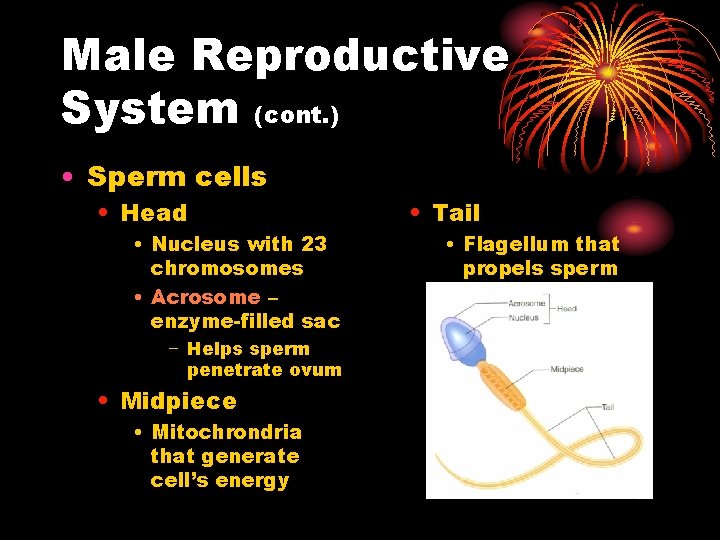
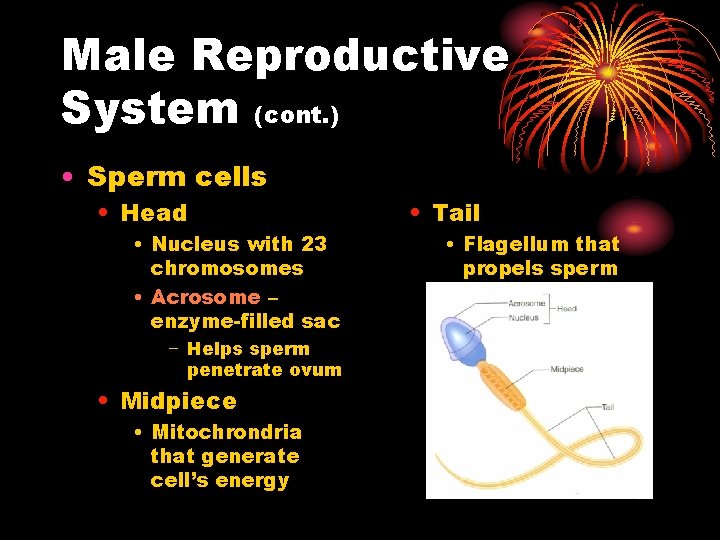
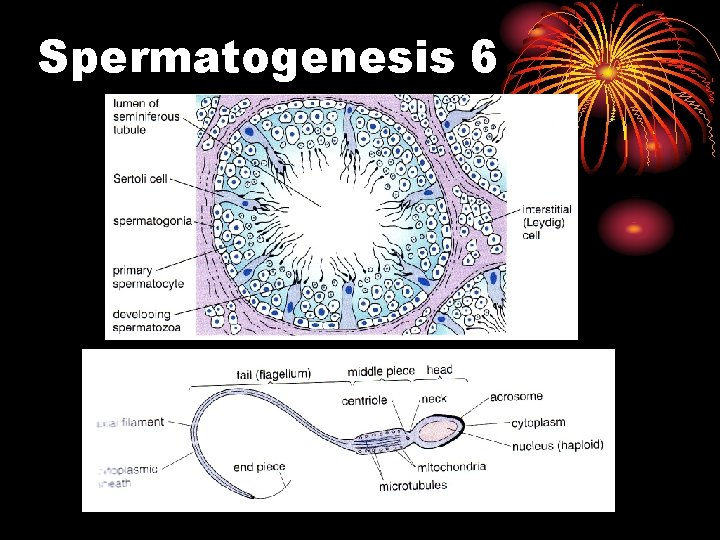
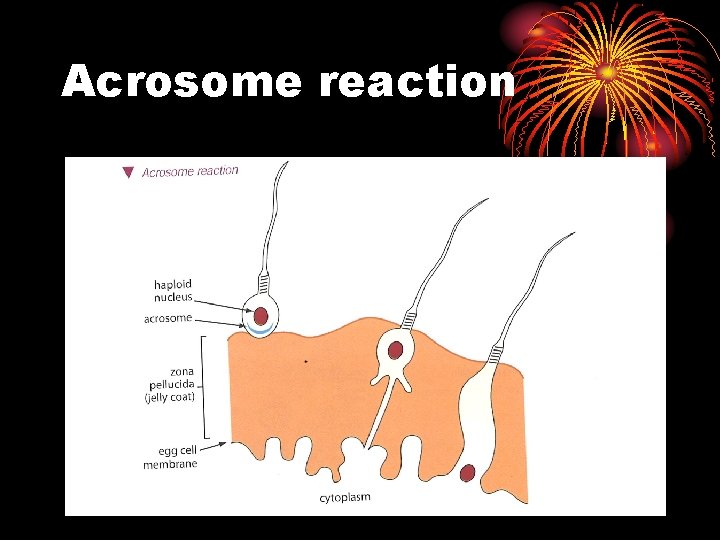
Male Reproductive System (cont. ) • Sperm cells • Head • Nucleus with 23 chromosomes • Acrosome – enzyme-filled sac − Helps sperm penetrate ovum • Midpiece • Mitochrondria that generate cell’s energy • Tail • Flagellum that propels sperm forward
Male Reproductive System: Erection, Orgasm, and Ejaculation • Erection • Parasympathetic nervous system stimulates erectile tissue • Become engorged with blood • Orgasm • Sperm cells propelled out of testes into urethra • Secretions from accessory organs also released into urethra • Ejaculation • Semen is forced out of urethra • Sympathetic nerves then stimulate erectile tissue to release blood • Penis returns to flaccid state
FEMALE REPRODUCTIVE SYSTEM
Female reproductive System I • Function is to: • Produce gamates (ova) • Receive the male gamates • Provide a suitable environment for: • fertilisation • Development of fetus • Provide a means of expelling the developed fetus during parturition (birth)
Female reproductive System II • Consists of: • Ovaries • Produce Ova, secrete progesterone + oestrogen • Oviducts (Fallopian Tubes) • Uterus • Hollow, pearshaped, muscular. Lining – endometrium – undergoes cyclical changes. Cervix part of uterus that projects thru’ from vagina • Vagina • Muscular tube adapted for reception of the penis and passage of baby out during birth.
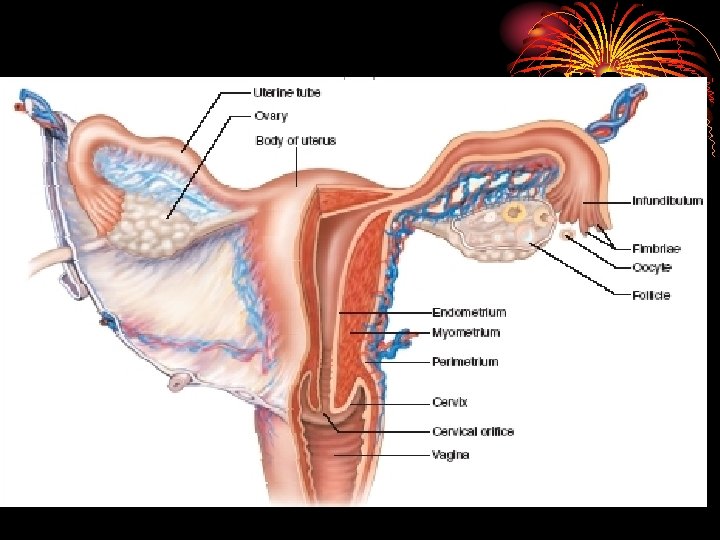
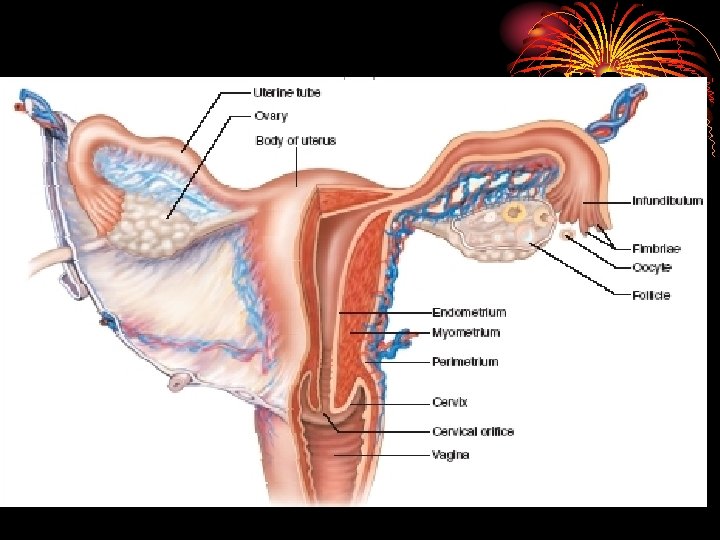
Internal Female Organs

GAMETE PRODUCTION
Production of Gametes • Production of Gametes – Gametogenesis • Involves special cell division – meiosis • Spermatogenesis • Oogenesis
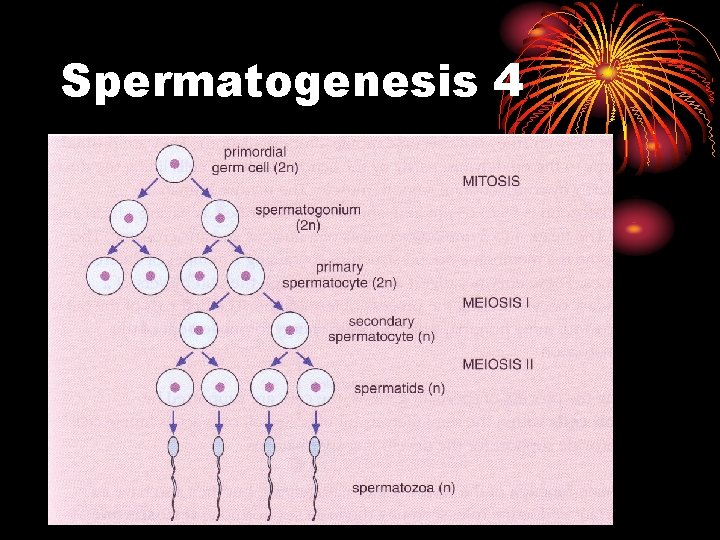
Spermatogenesis 1 • Each testis is packed with seminiferous tubules • In these Spermatogenesis takes place • Spermatogonia (germ cells) line the tubules dividing my mitosis to give more spermatogonia (Type A and Type B)
Spermatogenesis 2 • Type B Spermatogonia will undergo meiosis to eventually form spermatozoa • Type B also known as primary spermatocytes • After the first meiotic division they become secondary spermatocytes
Spermatogenesis 3 • Secondary spermatocytes rapidly under go the second meiotic division to form spermatids • Spermatids undergo development into spermatozoa
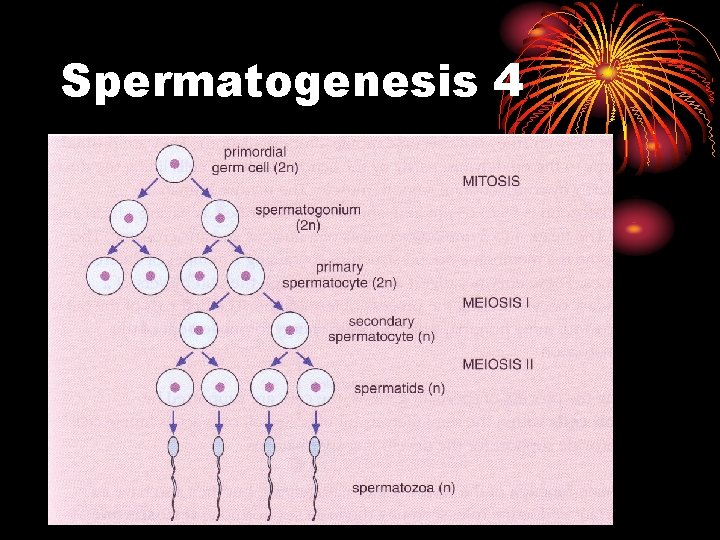
Spermatogenesis 4
Spermatogenesis 5 • During spermatogenesis, cells are supported by Sertoli Cells • Testes also produce testosterone from Leydig cells • Controls rate of sperm production and male characteristics
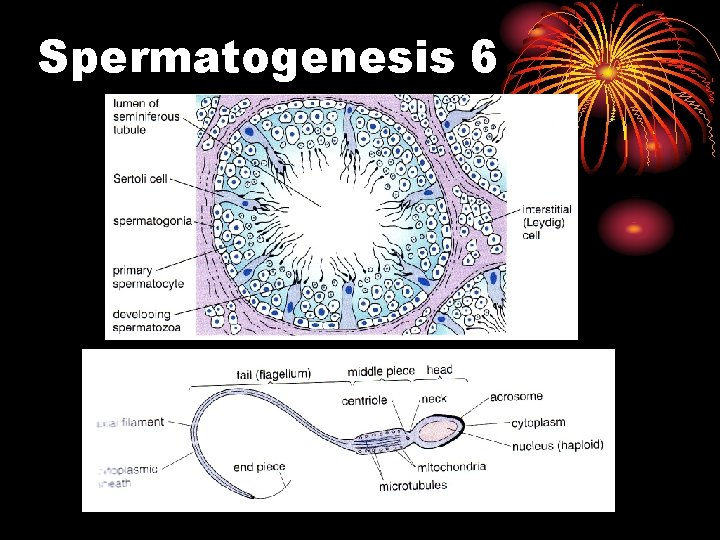
Spermatogenesis 6
Spermatogenesis 6 • Testes controlled by the anterior pituitary gland • Follicle stimulating hormone (FSH) • Interstitial Cell Stimulating Hormone (ICSH) • ICSH stimulates leydig cells to secrete testosterone inhibits FSH and ICSH secretion. Negative feedback.
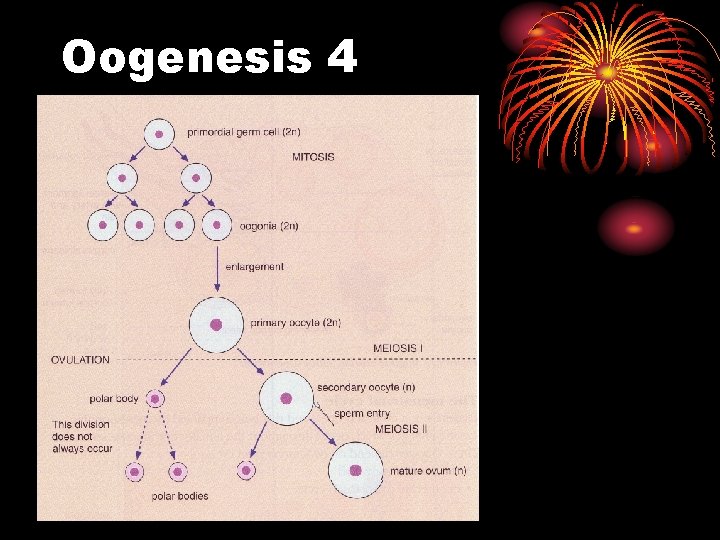
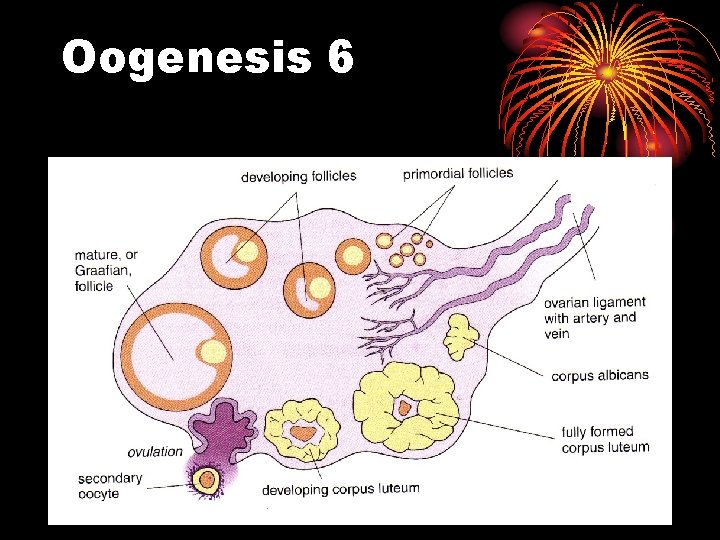
Oogenesis 1 • The process primordial germ cells (oogonia) become ova • Begins in fetus – oogonia divide by mitosis • By 4 or 5 months, some are enlarged – potential to become gametes • Now called primary oocyte
Oogenesis 2 • Primary oocytes begin first stage of meiosis • By month 7 they are surrounded by follicular cells to form primary follicles • Then Meiosis stops until puberty
Oogenesis 3 • Once a month some of the primary oocytes continue meiosis • move to surface of ovary • One reaches maturity, others degenerate • First meiotic division finishes – secondary oocyte • Ovulation follicle ruptures, oocyte released (once released called ovum) • 2 nd Meiotic division doesn’t occur until the head of a spermatozoan enters the ovum
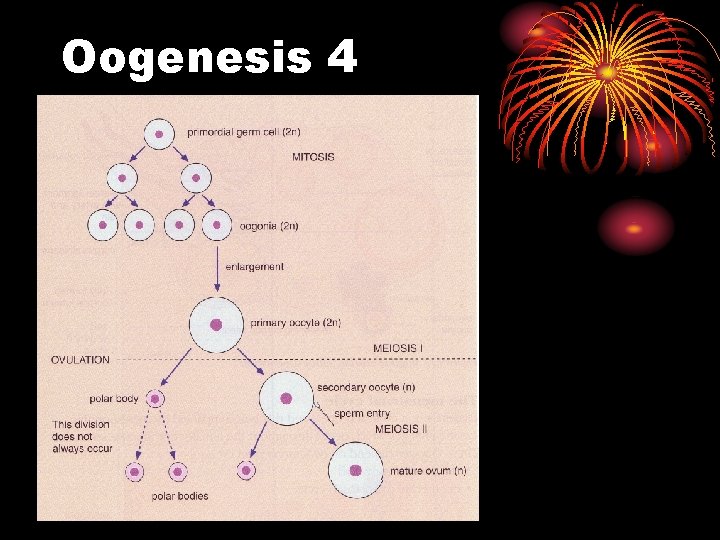
Oogenesis 4
Oogenesis 5 • After ovulation, the ruptured follicle fills with a blood clot • Cells enlarge • temporary endocrine structure, the corpus luteum • Grows for 7 – 8 days secreting progesterone and oestrogen • If fertilisation/implantation don’t occur, corpus luteum degenerates after 12 – 14 days.
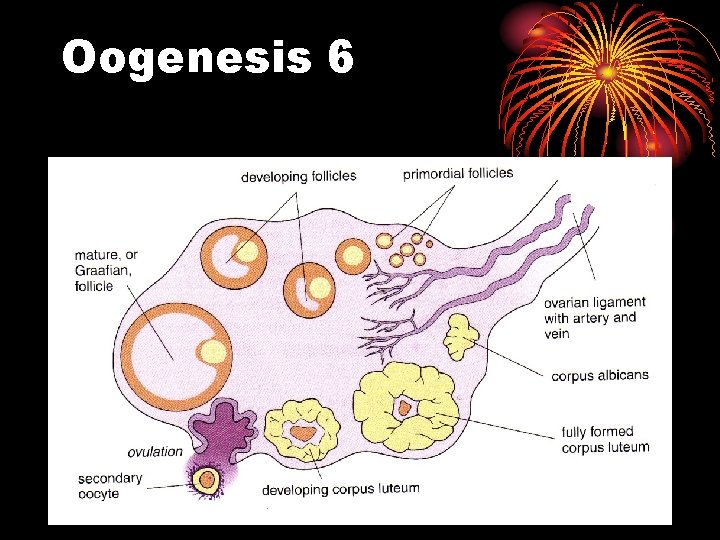
Oogenesis 6

FERTILISATION & PREGNANCY
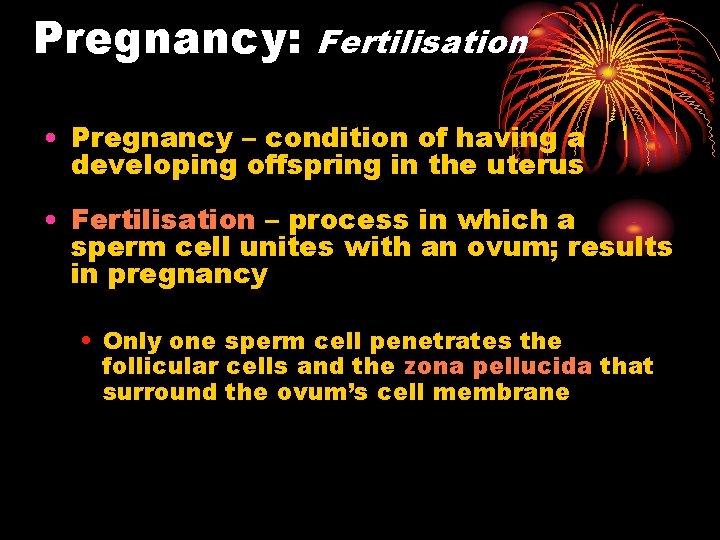
Pregnancy: Fertilisation • Pregnancy – condition of having a developing offspring in the uterus • Fertilisation – process in which a sperm cell unites with an ovum; results in pregnancy • Only one sperm cell penetrates the follicular cells and the zona pellucida that surround the ovum’s cell membrane
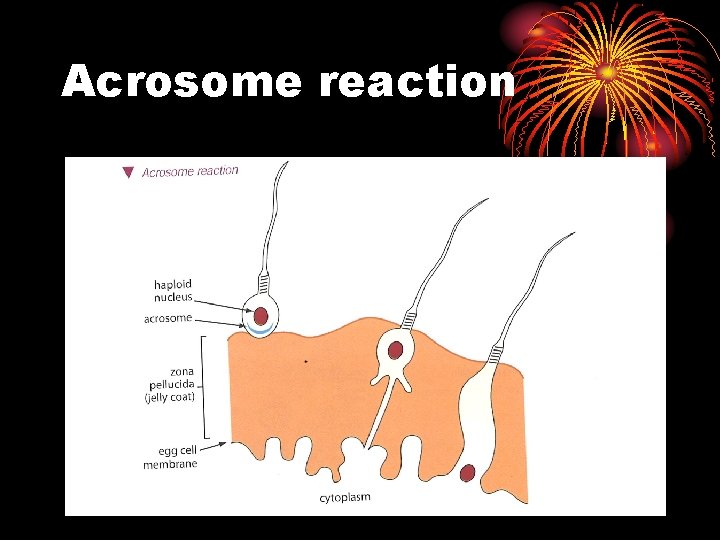
Acrosome reaction
• After fertilization, ovum releases enzymes that cause the zona pellucida to become impenetrable to other sperm • Zygote forms from union of ovum and sperm • Contains 46 chromosomes
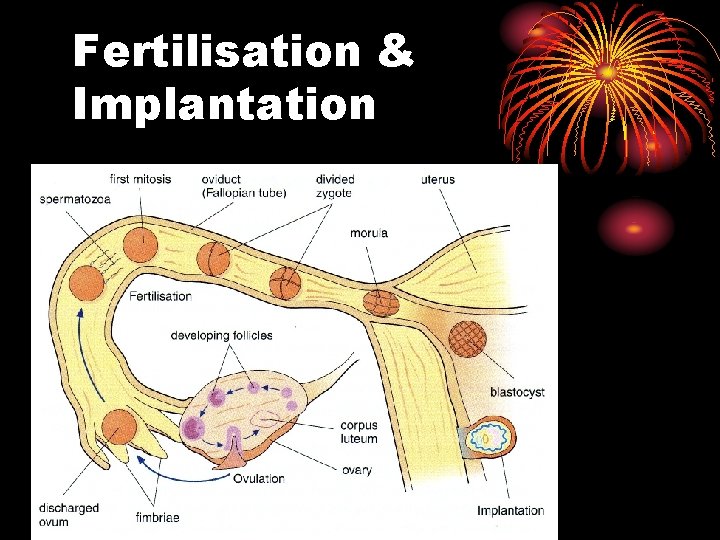
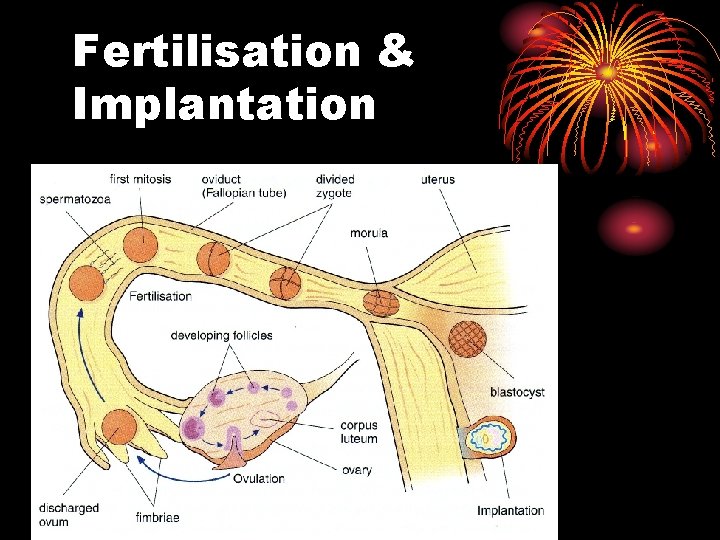
Fertilisation & Implantation
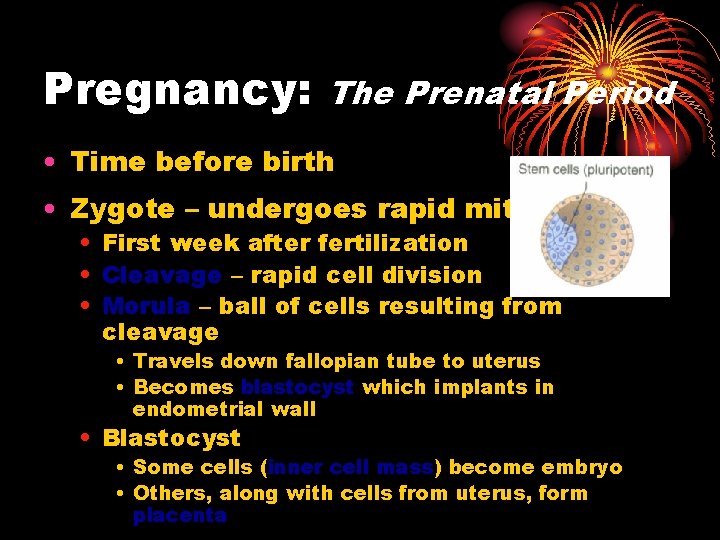
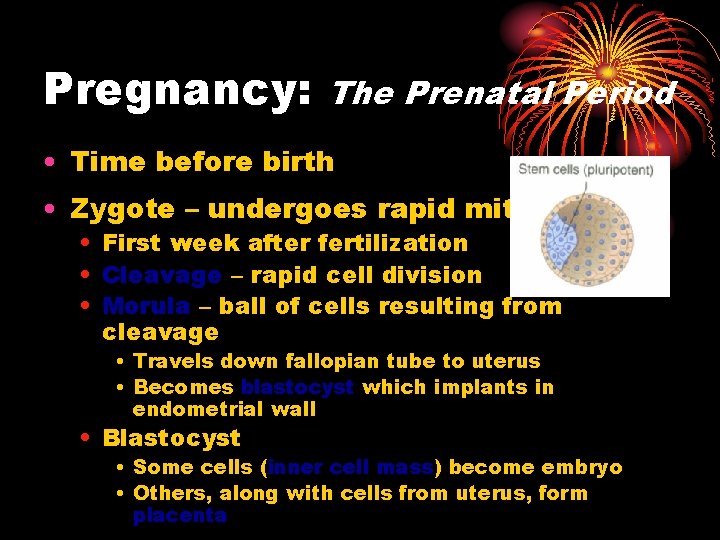
Pregnancy: The Prenatal Period • Time before birth • Zygote – undergoes rapid mitosis • First week after fertilization • Cleavage – rapid cell division • Morula – ball of cells resulting from cleavage • Travels down fallopian tube to uterus • Becomes blastocyst which implants in endometrial wall • Blastocyst • Some cells (inner cell mass) become embryo • Others, along with cells from uterus, form placenta
Fertilisation & Implantation (brief) • Sperm motile – 1 mm/min • With muscular movements of uterus get through cervix into oviducts • Fertilisation takes place (diploid) • Fertilised ovum – zygote – begins mitosis • 3 days – morula – 16 cells, enters uterus • Fluid enters morula, cells rearrange to become hollow – blastocyst • Blastocyst implants into endometrium – total 10 days
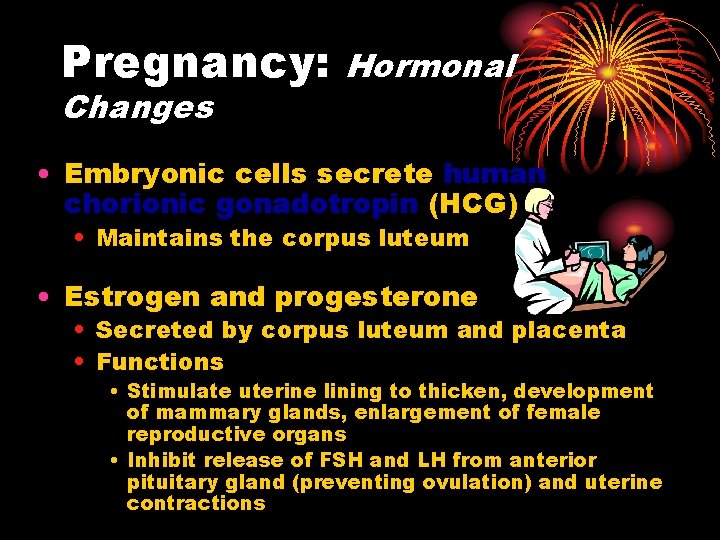
Pregnancy: Changes Hormonal • Embryonic cells secrete human chorionic gonadotropin (HCG) • Maintains the corpus luteum • Estrogen and progesterone • Secreted by corpus luteum and placenta • Functions • Stimulate uterine lining to thicken, development of mammary glands, enlargement of female reproductive organs • Inhibit release of FSH and LH from anterior pituitary gland (preventing ovulation) and uterine contractions
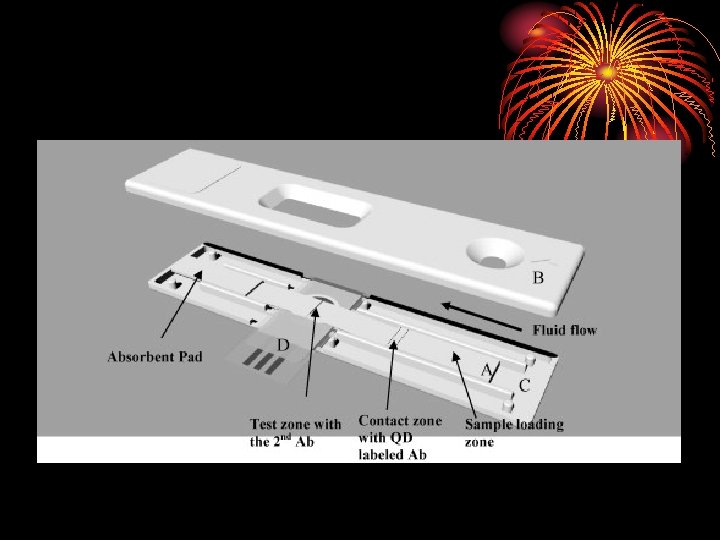
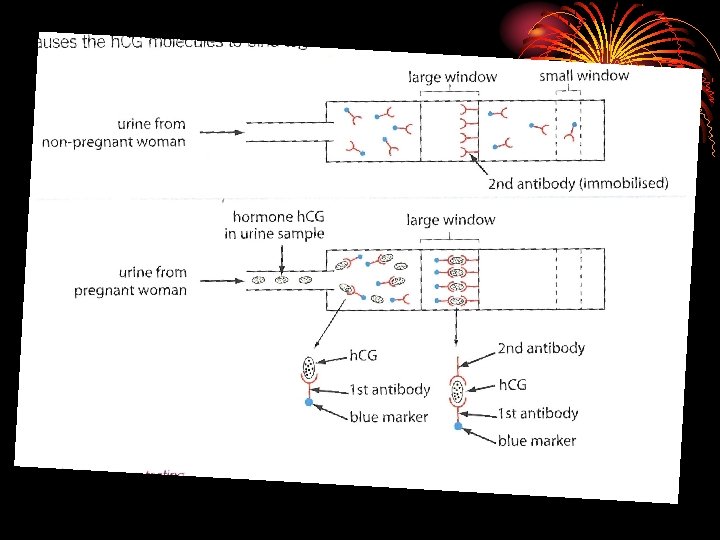
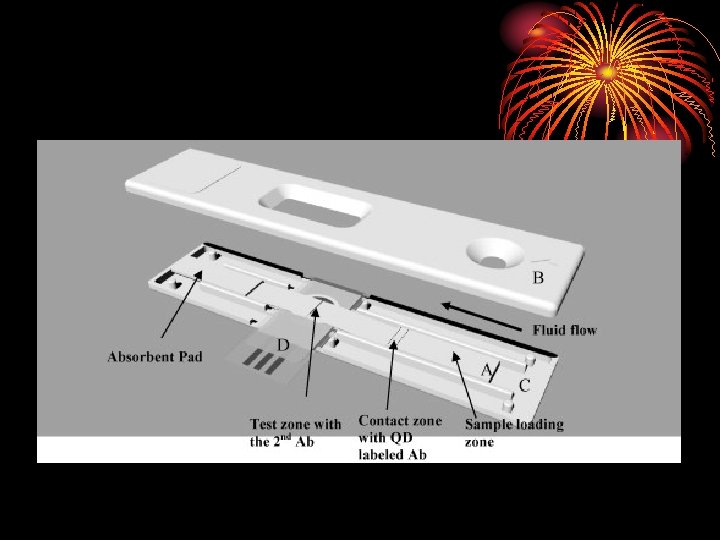
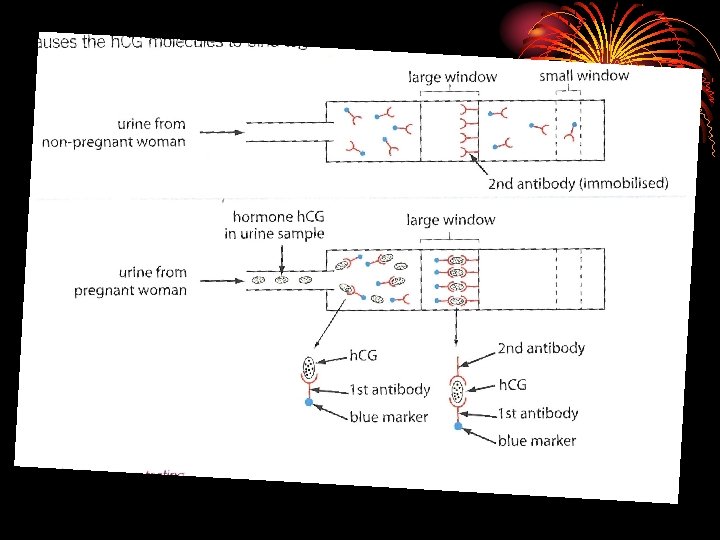
Pregnancy Testing Kits • These use monoclonal antibodies to test for hormone h. CG • h. CG produced by placenta • The test relies on the reaction between h. CG and antibodies bound to coloured latex beads