Renal Replacement Therapy Dialysis Melba DSouza RRT Dialysis
Renal Replacement Therapy Dialysis Melba DSouza
RRT/ Dialysis Process by which the solute composition of a solution “A” is altered by exposing it to a second solution “B” through a semipermeable membrane
Necessary pre-requisites for Hemodialysis 1) Semi-permeable membrane 2) Anticoagulation 3) Knowing what to remove and how much of it
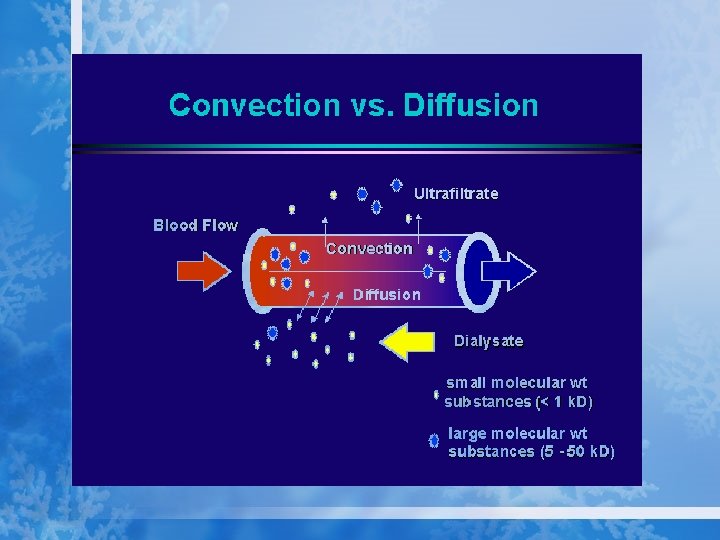
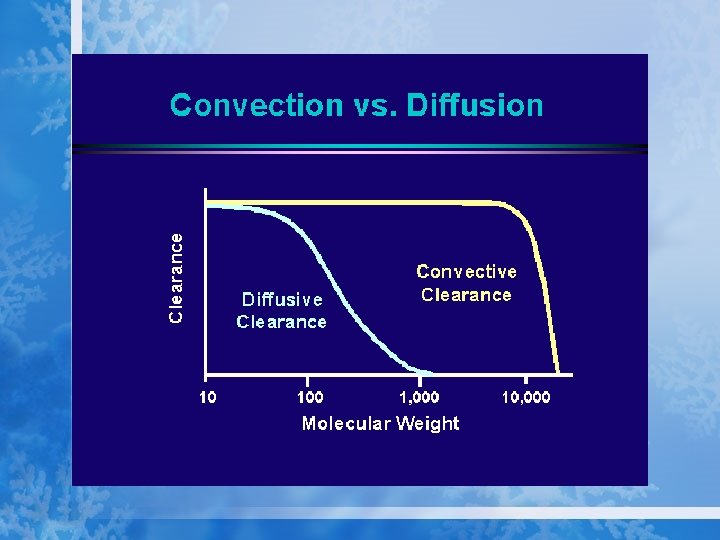
Mechanisms of Solute transfer • Diffusion • Convection
Diffusive Clearance • A result of random molecular motion • Influenced by concentration gradient of the solute and its Molecular weight as well as by the membrane permeability to the solute
Convective Clearance • Water molecules passing through a SPM carry with them the solutes in their original concentration. This is called the “solvent drag phenomenon” • Water can be made to move across a SPM by the application of either a hydrostatic or an osmotic gradient
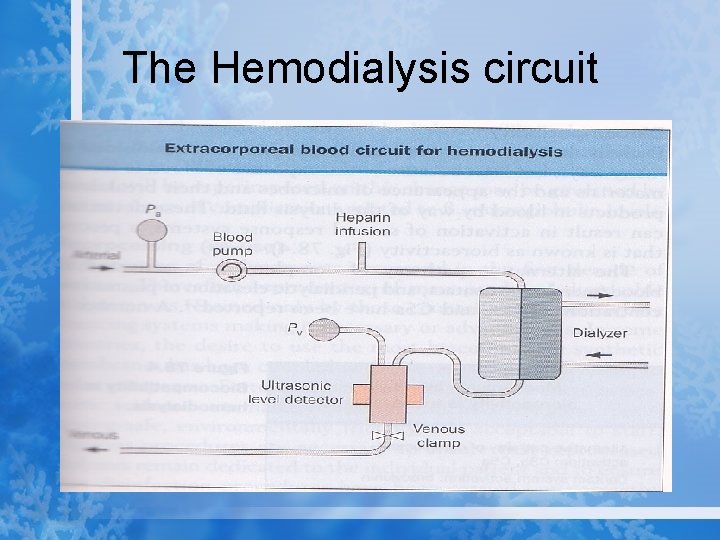
The Hemodialysis circuit
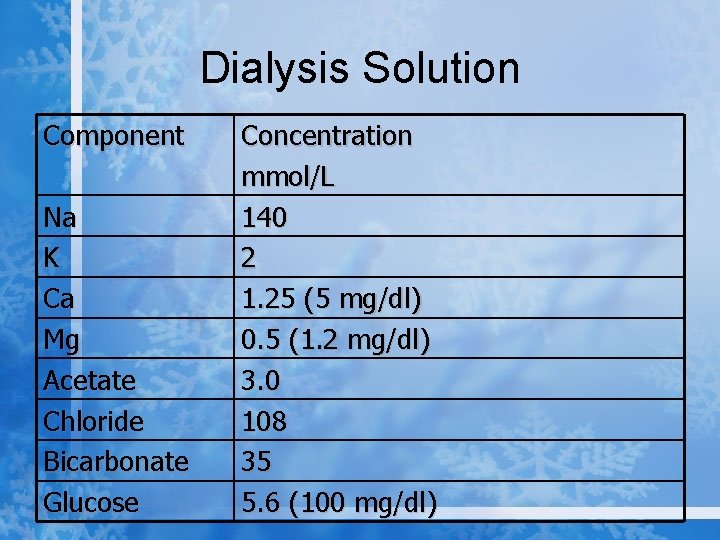
Dialysis Solution Component Na K Ca Mg Acetate Chloride Bicarbonate Glucose Concentration mmol/L 140 2 1. 25 (5 mg/dl) 0. 5 (1. 2 mg/dl) 3. 0 108 35 5. 6 (100 mg/dl)
Indications for initiating Hemodialysis • In patients with calculated creatinine clearance <20 ml/min/1. 73 m 2 the onset of: *Uremic symptoms Nausea/emesis Altered sleep pattern *Altered mental status Coma Stupor Tremor Asterixis Clonus Seizures
Indications for Hemodialysis *Pericarditis or Tamponade (urgent indication) *Uremic platelet dysfunction (urgent indication) *Refractory volume overload *Refractory hyperkalemia *Refractory Metabolic acidosis with anuria
Indications for Hemodialysis • Steadily worsening renal function in a patient with measured 24 hour urinary creatinine clearance<15 ml/min when accompanied by worsening azotemia, poor nutritional status and refractory edema
Measurement of nutritional status • Physical Exam Skin fold thickness Mid arm muscle thickness • Protein catabolic rate <1* • Serum Albumin • Serum Cholesterol • Blood Lymphocyte count
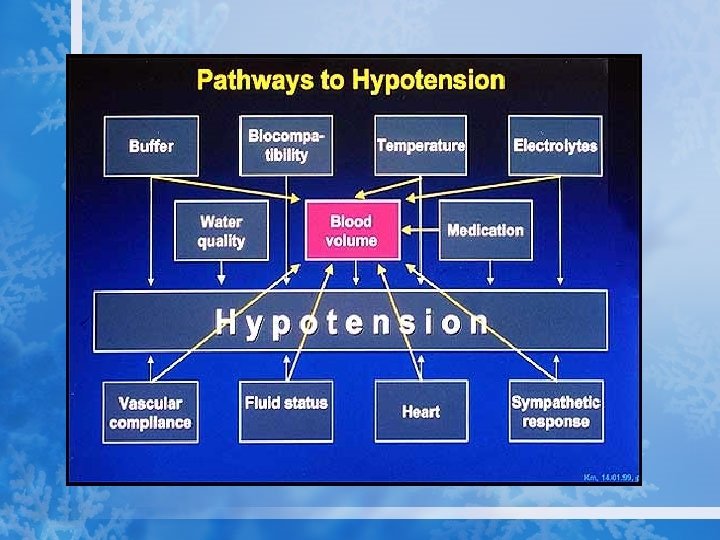
Complications of Hemodialysis 1. Dialysis Reactions 2. Intradialytic Hypotension 3. Neuromuscular complications 4. Dialysis dysequilibrium 5. Hemolysis 6. Intradialytic hypoxemia 7. Postdialysis syndrome 8. Cardiac arrhythmia and sudden death 9. Steal syndrome 10. Dialysis associated hypoxemia 11. Air embolism 12. Metabolic derangements
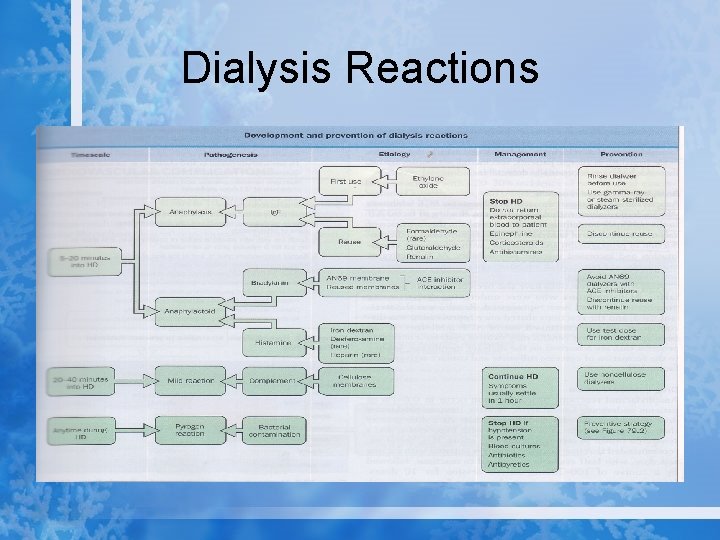
Dialysis Reactions
Management of Intradialytic Hypotension 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Assess dry weight frequently Avoid BP meds before HD Avoid rapid UF Use sequential UF and HD Avoid feeding patients on HD Use Sodium modeling Use HCO 3 based dialysate Keep Hct >33 Use non Cellulosic membranes Keep Dialysate temperature<37 degrees Celsius Assess cardiac function, r/o pericardial effusion/tamponade
Neuromuscular Complications: Muscle Cramps • • Etiology: Hypo-osmolality, Carnitine deficiency, Hypomagnesemia, excessive inter-dialytic weight gain Rx: Dietary counseling, Sodium modeling, Saline or 50% dextrose bolus, ? Prophylactic Quinine sulfate or Oxazepam
Neuromuscular complications • Seizures • Restless legs syndrome • Headache
Dialysis Disequilibrium Syndrome (DDS) • Risk factors: Young age, severe and chronic azotemia, Initial dialysis treatment, High flux/ large surface area dialyzer • Symptoms: Headache, nausea, emesis, blurred vision, hypertension, disorientation, muscle twitching
DDS • Pathogenesis: 1. Reverse urea effect ( rapid reduction of serum urea while CSF urea concentration remains high) 2. Paradoxical CSF acidosis 3. Intracerebral accumulation of idiogenic osmoles in uremia
DDS • Treatment 1. Early detection of uremia, early intervention with dialysis 2. First few treatments should aim to achieve modest reduction in serum urea concentration ( 30% or less) 3. Sodium modeling, use of Bicarbonate dialysis, slow QB 4. Prophylactic use of Mannitol is not recommended
Intradialytic Hemolysis • Uncommon • From contamination of dialysate with Chloramine or Copper (deionization failure) • From Methemoglobinemia from nitrate contamination
Intradialytic Hypoxemia • Arterial p O 2 drops by 5 to 30 mm Hg during Hemodialysis due to central Hypoxemia. • This is a result of a drop in CO 2 that accompanies correction of acidosis on dialysis • V/Q mismatch can occur due to pulmonary sequestration of activated leukocytes • Acetate can induce respiratory muscle fatigue
Intradialytic Hypoxemia • Treatment : Supplemental oxygen during Hemodialysis in susceptible patients

KIDNEY TRANSPLANT MELBA DSOUZA
Definition • Kidney transplantation or renal transplantation is the organ transplant of a kidney from a living donor or human cadaver in a patient with end-stage renal disease • Sources of kidneys • Most donated kidneys come from deceased donors, some come from living donors.
Classification Kidney transplantation is typically classified as 1. deceased-donor (formerly known as cadaveric) 2. living-donor transplantation. 1. living-unrelated (non-related) transplants, 2. living-related (genetically related)
Living donors • Potential donors evaluated medically and psychologically - the donor is fit for surgery and has no kidney disease. • Traditionally the donor procedure has been through an incision but live donation has increasingly proceeded by laproscopic surgery. • This reduces pain and accelerates return to work for the donor with minimal effect on the outcome of the kidney.
Deceased Donors Deceased donors can be divided in two groups: • Brain-dead (BD) donors • Donation after Cardiac Death(DCD) donors • Kidneys from braindead donors are generally of a superior quality, since they have not been exposed to warm ischemia (the time between the stopping and the
Indications The indication for kidney transplantation is endstage renal disease (ESRD), Common diseases leading to ESRD include • hypertension, • infections, • diabetes mellitus and • glomerulonephritis; • genetic causes include polycystic kidney disease.
Contraindications • • Recent cancer, active substance abuse, Aids or failure to adhere to prescribed medical regimens
Kidney transplant requirements • INCLUSION CRITERIA • donor and recipient have to be ABO blood group compatible
Kidney transplant requirements Exclusion criteria • cardiovascular disease, • Incurable terminal infectious diseases (e. g. AIDS) and cancer. • Mental illness • Significant on-going substance abuse. Compliance with medications are tested.
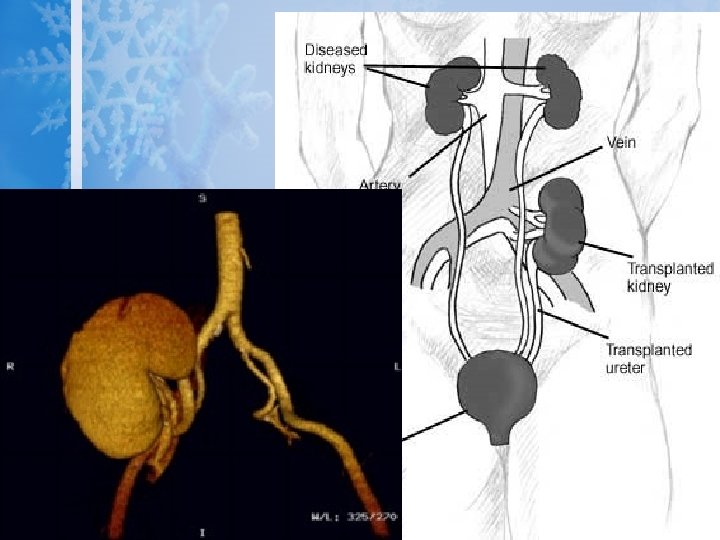
Procedure • In most cases the barely functioning existing kidneys are not removed, • the kidney is usually placed in a location different from the original kidney (often in the ilac fossa), • and as a result it is often necessary to use a different blood supply:
Procedure • The renal artery of the kidney, previously branching from the abdominal aorta in the donor, is often connected to the external iliac artery in the recipient. • The renal vein of the new kidney, previously draining to the inferior vena cava in the donor, is often connected to the external iliac vein in the recipient.
Pre – operative management Goals include • Bring the patient’s metabolic state to normal level as possible • Prevention of infection • Preparation of the patient for surgery
Medical management • Complete physical examination – to detect conditions that can cause complications • Tissue typing • Blood typing • Antibody screening • Psychosocial evaluation • Treat the infections • Hemodialysis is performed the day before.
Nursing management • Preoperative teaching which includes – Orientation to the area and procedure – Pain management options – Dietary restrictions – Intravenous and arterial lines Help to relive the anxiety related to the surgery
Post operation • The transplant surgery lasts about three hours. • The donor kidney will be placed in the lower abdomen and its blood vessels connected to arteries and veins in the recipient's body. • When this is complete, blood will be allowed to flow through the kidney again, so the ischemia time is minimized. • In most cases, the kidney will soon start producing urine. • The final step is connecting the ureter from the donor kidney to the bladder.
• Depending on its quality, the new kidney usually begins functioning immediately. • Hospital stay is typically for four to seven days. • If complications arise, additional medicines may be administered to help the kidney produce urine.
• Medicines are used to suppress the immune system from rejecting the donor kidney. • These medicines must be taken for the rest of the patient's life. • The most common medication regimen today is : tacrolimus, mycophenolate, and prednisone. Some patients may instead take cyclosporine, rapamycin, or azathioprine.
• Acute rejection occurs in 10% to 25% of people after transplant during the first sixty days. • Rejection does not mean loss of the organ, but may require additional treatment.
Complications Problems after a transplant may include: • Transplant rejection (hyperacute, acute or chronic) • Infections and sepsis due to the immunosuppressant drugs that are required to decrease risk of rejection
Complications • Post-transplant lymphoproliferative disorder • Imbalances in electrolytes including Calcium and Phosphate which can lead to bone problems amongst other things • Other side effects of medications including gastrointestinal inflammation and ulceration of the stomach and esophagus, hirsutism, hair loss, obesity, acne, diabetes mellitus, hypercholesterolemia and others.
• The average lifetime for a donor kidney is ten to fifteen years. When a transplant fails a patient may opt for a second transplant, and may have to return to dialysis for some time
Prognosis • Kidney transplantation is a life-extending procedure. • The typical patient will live ten to fifteen years longer with a kidney transplant than if kept on dialysis. • The years of life gained is greater for younger patients, but even 75 year-old recipients gain an average four more years' life.
Post operative nursing management Nursing assessment • S/S of kidney rejection such as – Oliguria – Edema – Fever – Increasing BP – Swelling or tenderness over the transplanted kidney or graft • Results of blood chemistry tests – BUN and creatinine
Preventing infection • Urinary cultures are performed frequently • Catheter and drain tips cultured when removed • Ensure that the patient is protected from any exposure to infection from hospital staff, visitors or other patients
Monitoring the urinary function • Monitor the vascular access for hemodialysis - to check infection • Hemodialysis may be needed till the kidney starts functioning properly • I/O monitoring • IV fluid administration based on the output
Managing potential complications • Careful monitoring • Encourage the strategy to promote recovery – breathing exercises, – early ambulation, – care of surgical incision
- Slides: 61