REMEDIATION OF THE STRUGGLING MEDICAL LEARNER Faculty Development


- Slides: 32
REMEDIATION OF THE STRUGGLING MEDICAL LEARNER Faculty Development Alan Finkelstein, MD March 9, 2017
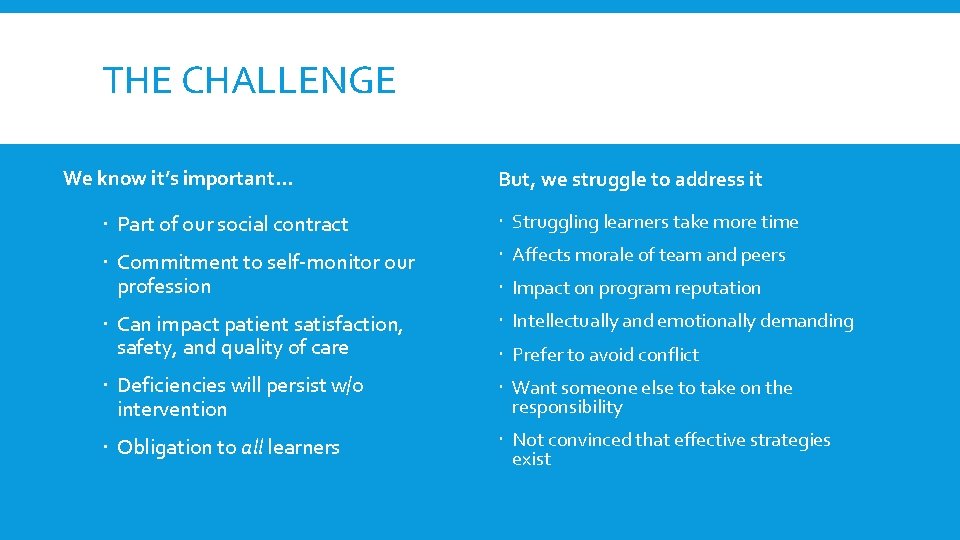
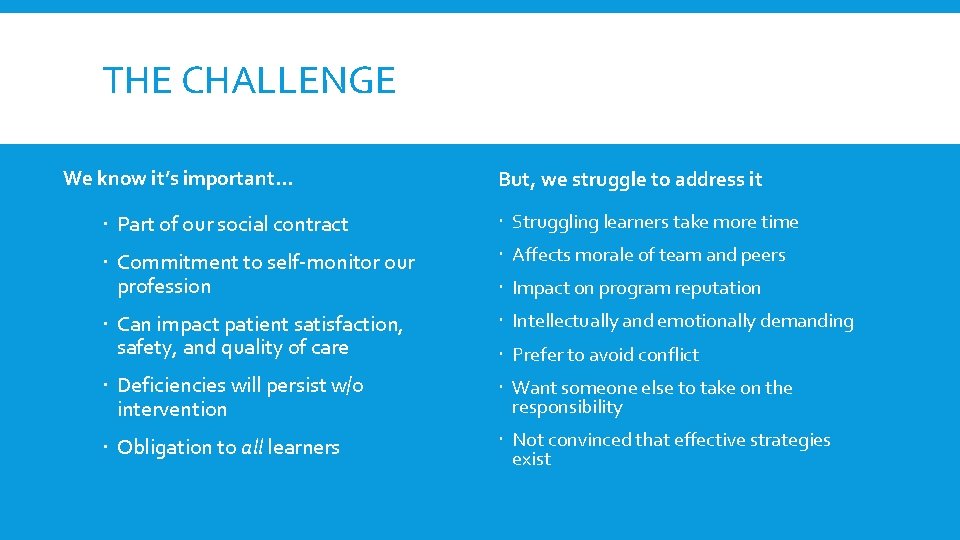
THE CHALLENGE We know it’s important… But, we struggle to address it Part of our social contract Struggling learners take more time Commitment to self-monitor our profession Affects morale of team and peers Can impact patient satisfaction, safety, and quality of care Intellectually and emotionally demanding Deficiencies will persist w/o intervention Want someone else to take on the responsibility Obligation to all learners Not convinced that effective strategies exist Impact on program reputation Prefer to avoid conflict
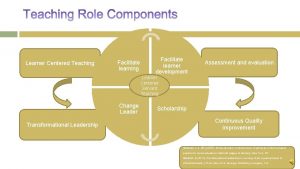
MEDICAL EDUCATORS NEED: A practical structure to identify the struggling learner A framework for diagnosing the learner’s deficit (s) Step-by step approach to remediate most common deficiencies
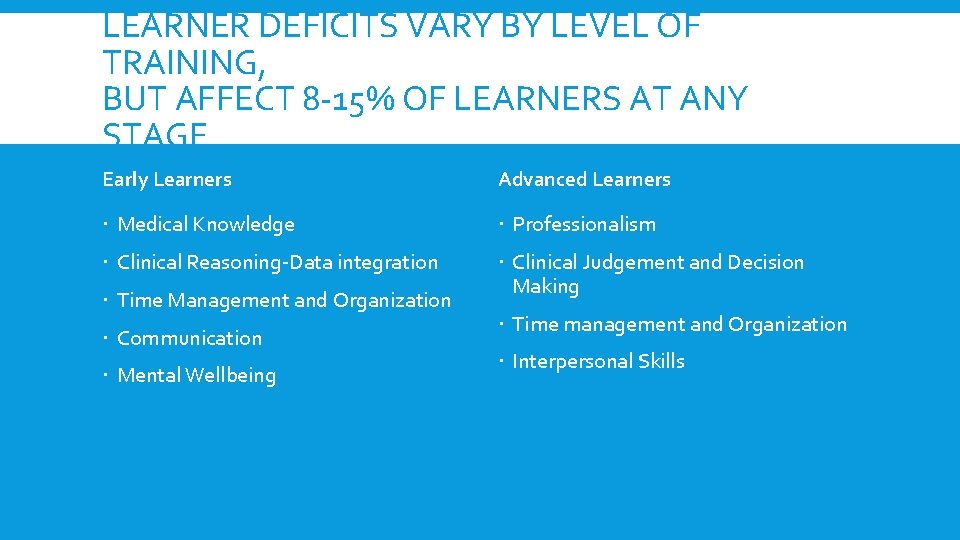
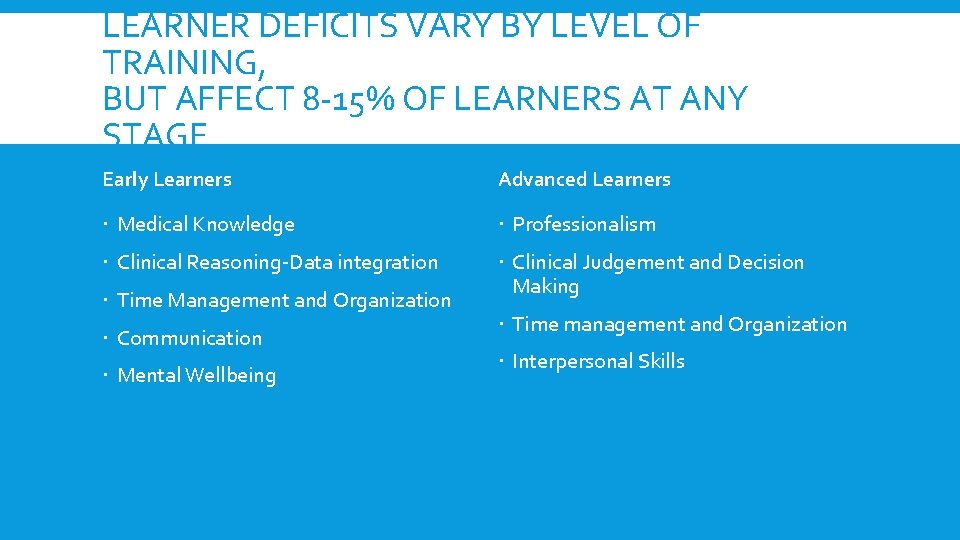
LEARNER DEFICITS VARY BY LEVEL OF TRAINING, BUT AFFECT 8 -15% OF LEARNERS AT ANY STAGE Early Learners Advanced Learners Medical Knowledge Professionalism Clinical Reasoning-Data integration Clinical Judgement and Decision Making Time Management and Organization Communication Mental Wellbeing Time management and Organization Interpersonal Skills
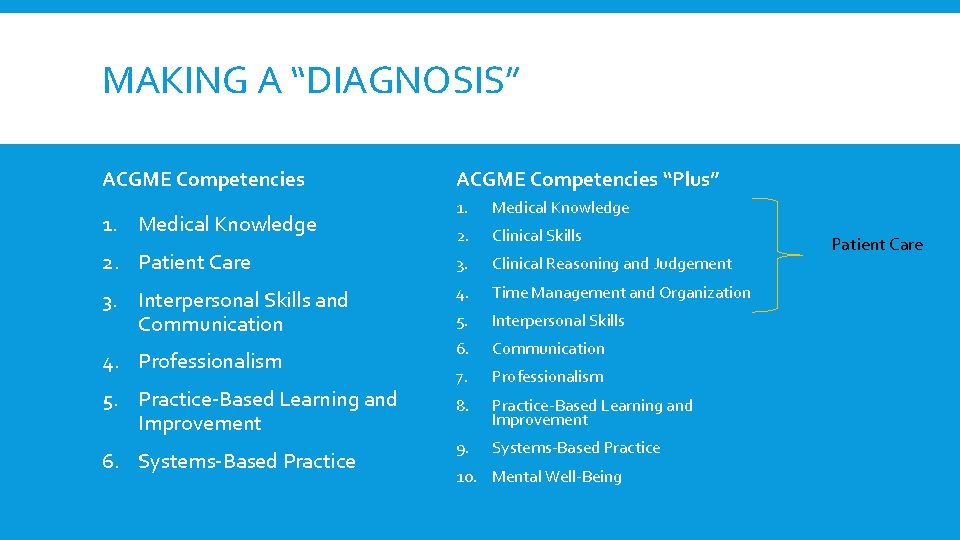
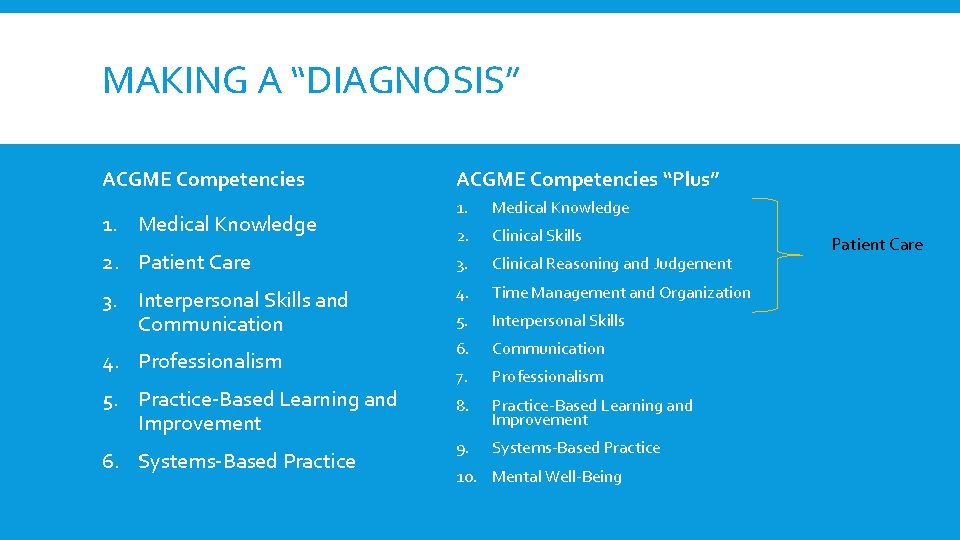
MAKING A “DIAGNOSIS” ACGME Competencies “Plus” 1. Medical Knowledge 2. Clinical Skills 2. Patient Care 3. Clinical Reasoning and Judgement 3. Interpersonal Skills and Communication 4. Time Management and Organization 5. Interpersonal Skills 6. Communication 7. Professionalism 8. Practice-Based Learning and Improvement 9. Systems-Based Practice 1. Medical Knowledge 4. Professionalism 5. Practice-Based Learning and Improvement 6. Systems-Based Practice 10. Mental Well-Being Patient Care
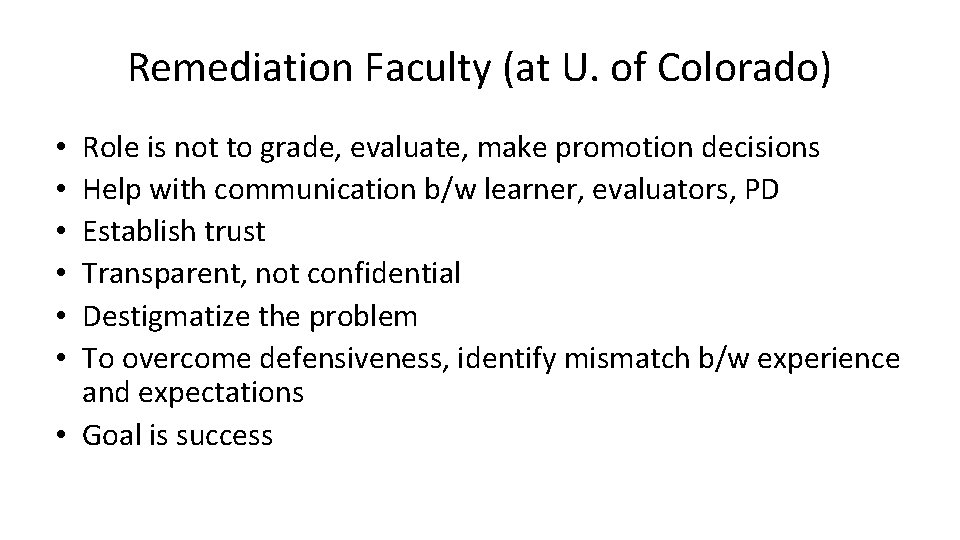
Remediation Faculty (at U. of Colorado) Role is not to grade, evaluate, make promotion decisions Help with communication b/w learner, evaluators, PD Establish trust Transparent, not confidential Destigmatize the problem To overcome defensiveness, identify mismatch b/w experience and expectations • Goal is success • • •
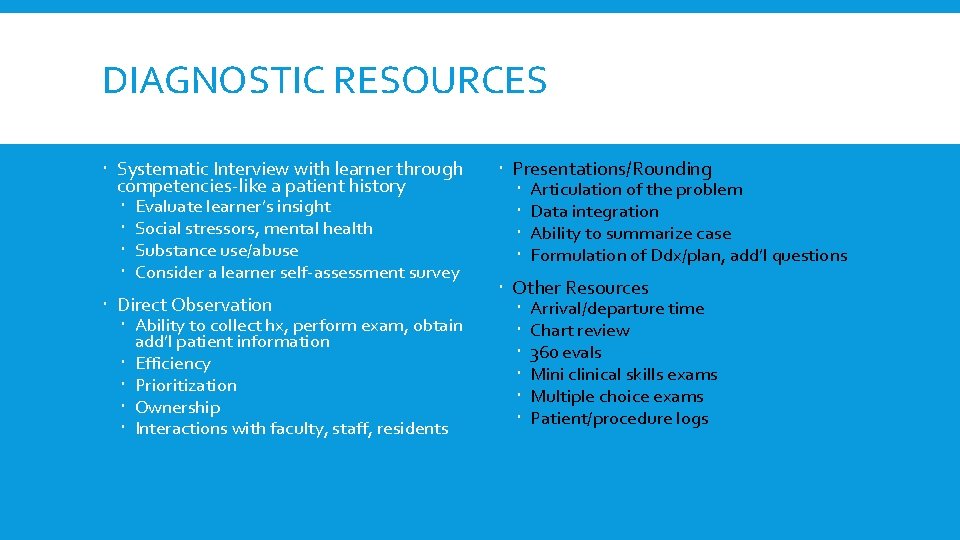
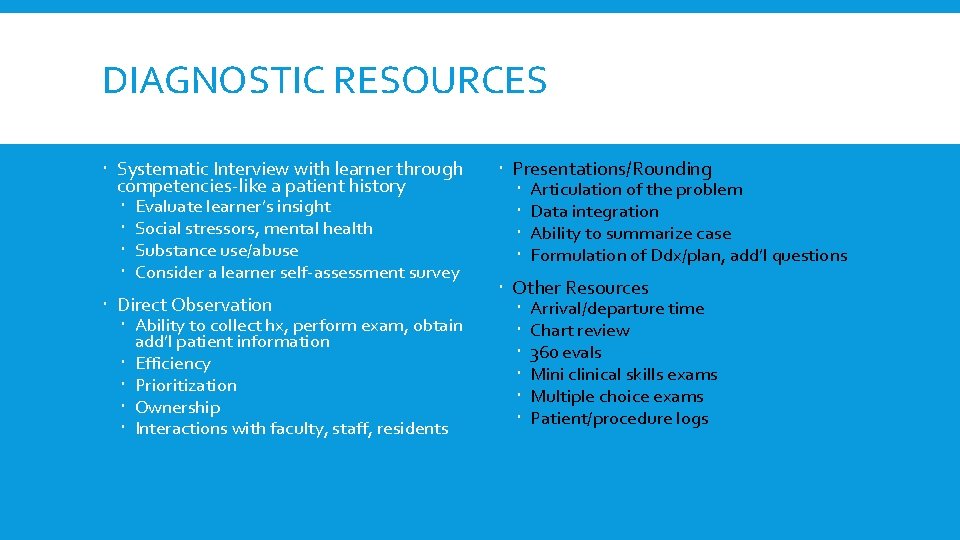
DIAGNOSTIC RESOURCES Systematic Interview with learner through competencies-like a patient history Evaluate learner’s insight Social stressors, mental health Substance use/abuse Consider a learner self-assessment survey Direct Observation Ability to collect hx, perform exam, obtain add’l patient information Efficiency Prioritization Ownership Interactions with faculty, staff, residents Presentations/Rounding Articulation of the problem Data integration Ability to summarize case Formulation of Ddx/plan, add’l questions Other Resources Arrival/departure time Chart review 360 evals Mini clinical skills exams Multiple choice exams Patient/procedure logs
DIAGNOSTIC STRATEGIES BY COMPETENCY How Competency Deficits Present in the Clinical Setting
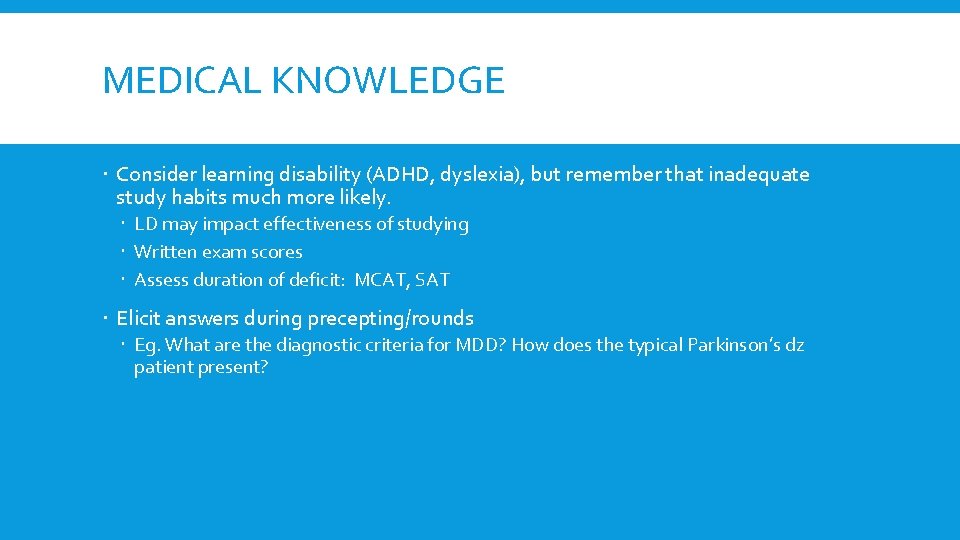
MEDICAL KNOWLEDGE Consider learning disability (ADHD, dyslexia), but remember that inadequate study habits much more likely. LD may impact effectiveness of studying Written exam scores Assess duration of deficit: MCAT, SAT Elicit answers during precepting/rounds Eg. What are the diagnostic criteria for MDD? How does the typical Parkinson’s dz patient present?
CLINICAL SKILLS Direct Observation Physical exam elements Ask about relevance of information obtained from exam findings eg. JVD, rales v rhonchi, etc. Can they manage the tools of the trade? Procedural skills
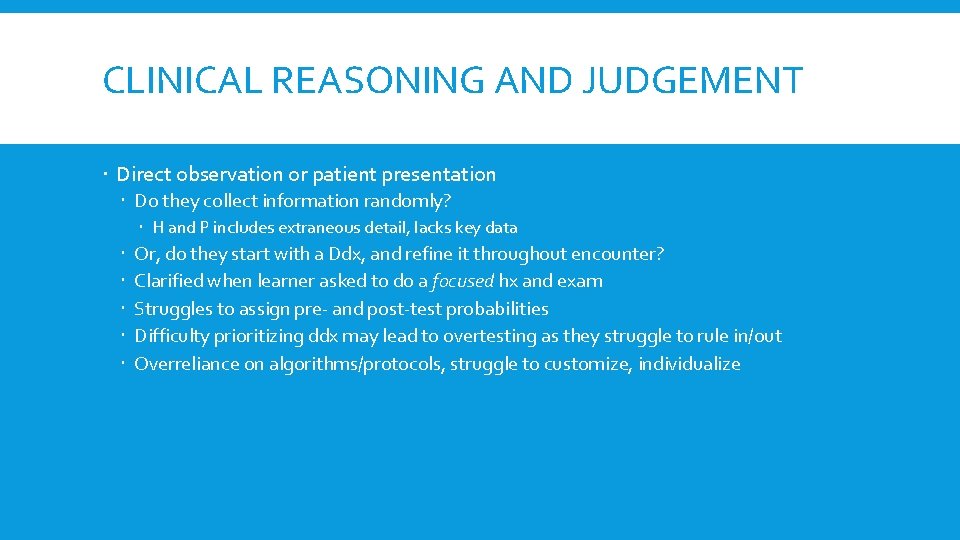
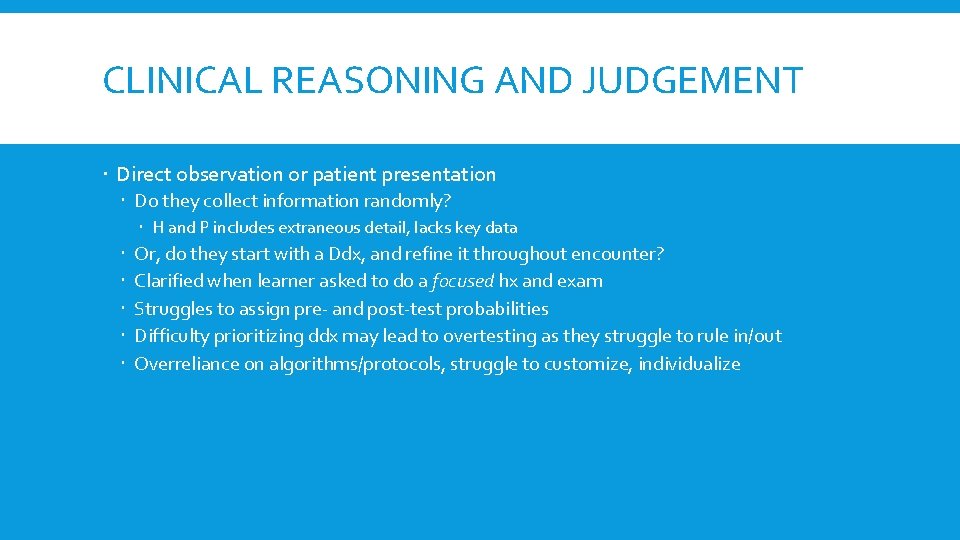
CLINICAL REASONING AND JUDGEMENT Direct observation or patient presentation Do they collect information randomly? H and P includes extraneous detail, lacks key data Or, do they start with a Ddx, and refine it throughout encounter? Clarified when learner asked to do a focused hx and exam Struggles to assign pre- and post-test probabilities Difficulty prioritizing ddx may lead to overtesting as they struggle to rule in/out Overreliance on algorithms/protocols, struggle to customize, individualize
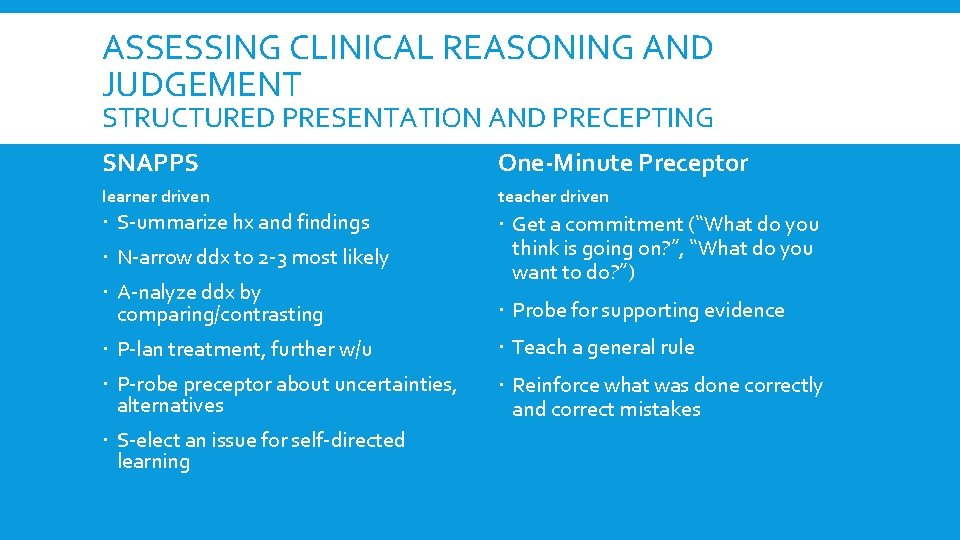
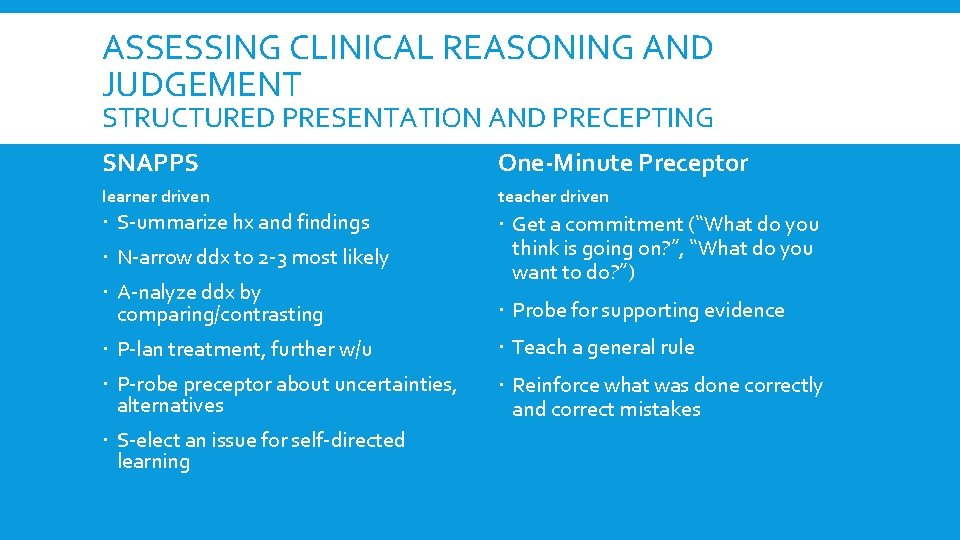
ASSESSING CLINICAL REASONING AND JUDGEMENT STRUCTURED PRESENTATION AND PRECEPTING SNAPPS One-Minute Preceptor learner driven teacher driven S-ummarize hx and findings Get a commitment (“What do you think is going on? ”, “What do you want to do? ”) N-arrow ddx to 2 -3 most likely A-nalyze ddx by comparing/contrasting Probe for supporting evidence P-lan treatment, further w/u Teach a general rule P-robe preceptor about uncertainties, alternatives Reinforce what was done correctly and correct mistakes S-elect an issue for self-directed learning
TIME MANAGEMENT AND ORGANIZATION Time management Late, missed assignments, deadlines May arrive earlier/stay later than peers Runs behind in office, always struggling to catch-up Duty hour violations Organization Disorganized appearance, notes, presentations, thinking Inability to present patients in rational manner Unprepared
INTERPERSONAL SKILLS Direct observation or report Others complain or may not like working with learner with this deficit Conflict with others in various roles Trouble reading social cues Abrasive or inappropriate questions or incongruent body language May transfer blame when brought to their attention Inflexible in negotiating with peers/patients Can lead to over-delegation (bossing around) or assuming too much responsibility themselves Distinguish from professionalism deficit by their desire to self improve
COMMUNICATION Observe presentations or during casual conversation Adequate medical knowledge and organizational skills but may struggle to answer questions (v exam scores) English as second language? Are they shy? Struggles with patient interviews, conveying information, expressing urgency/severity Appropriate non-verbal skills? Can they convey compassion? Written notes may also reflect this deficit
PROFESSIONALISM Direct observation or report Poor doctor-patient relationships, especially continuity relationships Demonstrates lack of respect Inappropriate jargon or body language Seek evidence of ownership and accountability Questionable ethics, honesty, reliability Taking dangerous shortcuts Leaving early, not being available when on-duty, not signing out, not answering pages, deferring work inappropriately
PRACTICE BASED LEARNING AND IMPROVEMENT Inability to accept feedback Do they not seek or avoid feedback? May be argumentative/defensive about it May not understand own limitations or seek help when needed Absence of self-directed learning Lack evidence of reading about patient care Depend on others to give information May confabulate or guess Fail to use learning goals or QI methods for self-improvement “Doesn’t know what s/he doesn’t know”
SYSTEMS-BASED PRACTICE Trouble functioning in their role on the team or don’t see value in other team members Don’t know, or ignore, available resources Don’t attend to cost Ignore risk-benefit analysis May not do appropriate hand-offs
MENTAL WELLBEING Identify through direct questioning Includes psychosocial stressors, psychiatric diagnoses, learning disabilities, substance abuse Inconsistency in performance Consider neuropsychiatric testing
DIAGNOSTIC CASE Its 2 AM…your pager goes off… “Hi, doc. You’re on call tonight, right? This is Martin. I’ve got one for ya. ”
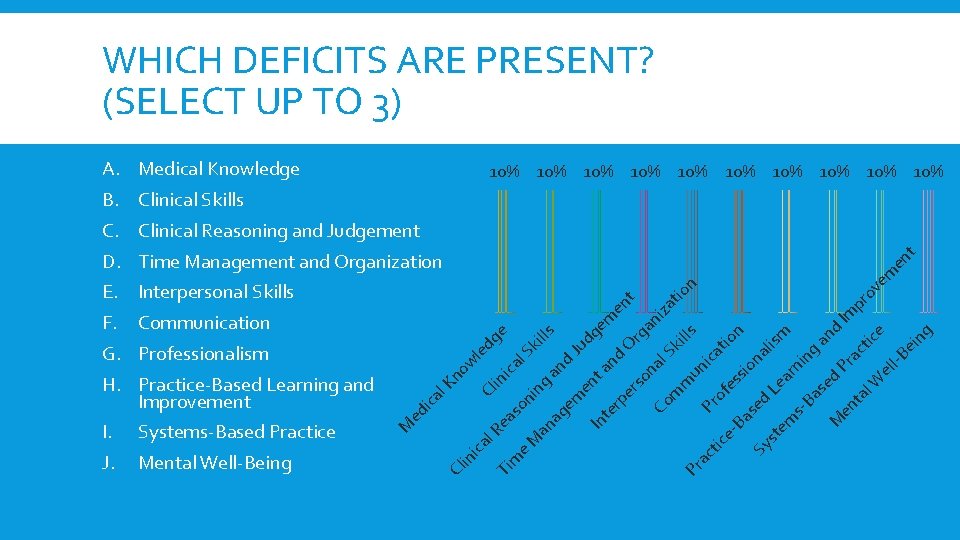
WHICH DEFICITS ARE PRESENT? (SELECT UP TO 3) A. Medical Knowledge 10% 10% 10% B. Clinical Skills D. Time Management and Organization t en es of Ba Pr Co m m un ica Sk al on rs tio ills an i rg O an te rp e en t em etic ac ag In Pr e. M an so ni ng an d Ju ki l. S ica ea Ti m l. R ica d lls e dg Cl in no w l. K ica in Mental Well-Being Cl J. ed Systems-Based Practice M I. le G. Professionalism dg e m F. Communication H. Practice-Based Learning and Improvement za tio n E. Interpersonal Skills n sio se na Sy d lis st m em Lea r ni sng Ba se an d M d Pr Im en ac ta tic pro l. W ve e el m l-B en ei t ng C. Clinical Reasoning and Judgement
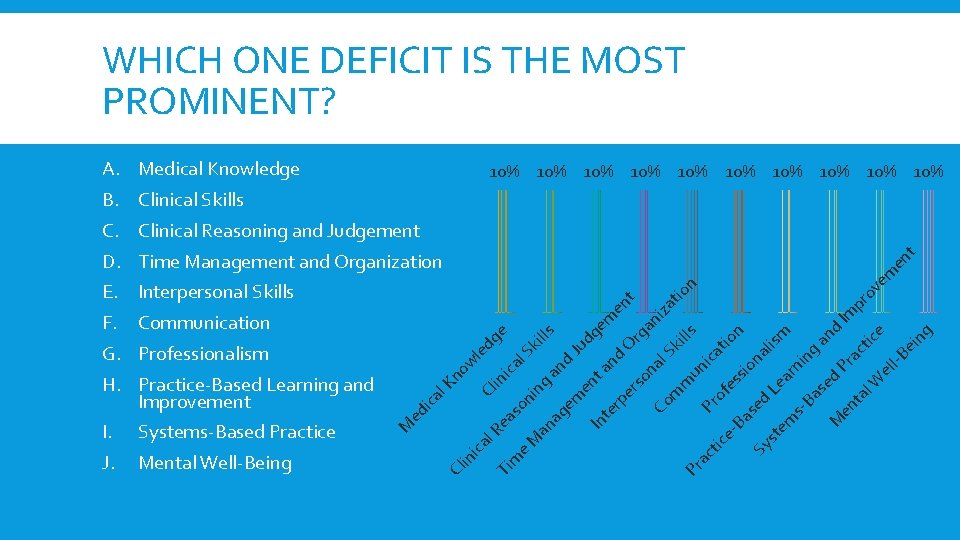
WHICH ONE DEFICIT IS THE MOST PROMINENT? A. Medical Knowledge 10% 10% 10% B. Clinical Skills D. Time Management and Organization t en es of Ba Pr Co m m un ica Sk al on rs tio ills an i rg O an te rp e en t em etic ac ag In Pr e. M an so ni ng an d Ju ki l. S ica ea Ti m l. R ica d lls e dg Cl in no w l. K ica in Mental Well-Being Cl J. ed Systems-Based Practice M I. le G. Professionalism dg e m F. Communication H. Practice-Based Learning and Improvement za tio n E. Interpersonal Skills n sio se na Sy d lis st m em Lea r ni sng Ba se an d M d Pr Im en ac ta tic pro l. W ve e el m l-B en ei t ng C. Clinical Reasoning and Judgement
MULTIPLE DEFICITS ARE COMMON Prioritize Work on the most severe one first
EVALUATOR’S RESPONSIBILITY Give learner feedback Provide examples Review standard expectations for learner’s level of training Avoid comparison to peers (norm-based assessment) d/t bias Demonstrates that concerns are not arbitrary Document learner deficits in writing with examples Help identify greatest deficit and address it first Notify program leadership
RIME CRITERION-BASED ASSESSMENT Reporter-3 rd year med student Requires good communication, interpersonal skills, medical knowledge, professionalism Interpreter-4 th year med student Creating Ddx, prioritizing, analyzing Manager-Intern Manage and propose diagnostic and therapeutic options Educator-Senior resident and beyond Teach patients and colleagues
WHO NEEDS REMEDIATION? Any learner who is one RIME level behind target Seek help immediately for any learner who Can’t continue to care for patients safely Is incapable of learning given circumstances Is a danger to self/others Is greatly impeding learning of other residents/students Can’t teach peers/students, if expected
REMEDIATION GOALS Target and correct the greatest deficit Less overwhelming to learner More likely to be successful, builds learner confidence Leads to positive reinforcement that can help with addressing next deficit Caveats: If mental well-being or professionalism are in question, start there Learner must be teachable If medical knowledge and clinical reasoning and judgement deficits coexist, start with MK is prerequisite to clinical reasoning
DEVELOPING A SUCCESS-ORIENTED STRATEGY Success Team PD, faculty members who have worked closely with learner, a remediation faculty member, learner Elicit suggestions from learner Demonstrates insight, willingness to participate and gives control 3 Key principles to address any deficit Deliberate practice Feedback Self-assessment Document meetings with items covered, educational pearls, learner responsibilities, date of next meeting Maintain a supportive environment

REMEDIATION STRATEGIES BY DEFICIT

DETERMINING SUCCESS OF REMEDIATION 2 criteria Has the learner shown significant improvement in the deficient competency, and caught up to expected level of training? Is improvement sustainable? To avoid conflict of interest, remediation faculty should not do reassessment Resources Repeat rotation OSCE-type encounter Simulated patients Directly observed patient encounters Chart review Supervisor/peer observation
WHEN TO STOP REMEDIATION Learner is working at full capacity and not making adequate progress Learner is not engaged, despite attempts to address individual barriers Learner is non-compliant with treatment of psychiatric or substance abuse problem Learner has a mental or physical health problem making them unfit for duty Learner has timed out
SUMMARY OF KEY STEPS 1. Document observations/assessment honestly with examples in evaluations 2. Compare performance with expected for level of training (eg. RIME) 3. Use ACGME Competencies “Plus” to identify deficits 4. Collect additional information to diagnose/confirm deficits 5. Select ONE greatest deficit to build customized remediation plan 6. Use deliberate practice, feedback, and self-reflection to address targeted deficit
 Remediation of the struggling medical learner
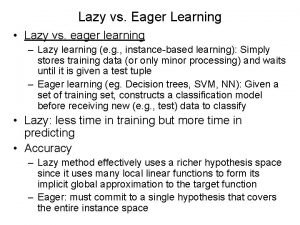
Remediation of the struggling medical learner Lazy learning vs eager learning
Lazy learning vs eager learning Struggling toward saratoga section 3
Struggling toward saratoga section 3 Struggling in silence
Struggling in silence Chapter 4 section 3 struggling toward saratoga
Chapter 4 section 3 struggling toward saratoga The outsiders adapted for struggling readers
The outsiders adapted for struggling readers Medical faculty in novi sad dean
Medical faculty in novi sad dean Ascaris lumbricoides ova
Ascaris lumbricoides ova Masaryk university medical faculty
Masaryk university medical faculty Mold remediation somerset
Mold remediation somerset Network access quarantine control
Network access quarantine control Ckla assessment and remediation guide
Ckla assessment and remediation guide Site remediation toronto
Site remediation toronto Sox remediation
Sox remediation Dlp incident management process
Dlp incident management process Bolter grusin remediation
Bolter grusin remediation Wcp envelope
Wcp envelope Nevada eits
Nevada eits Remediation plan in change lifecycle
Remediation plan in change lifecycle Fulbright faculty development program
Fulbright faculty development program Feedback for faculty development programme
Feedback for faculty development programme Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worm breton là gì
Tư thế worm breton là gì Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ