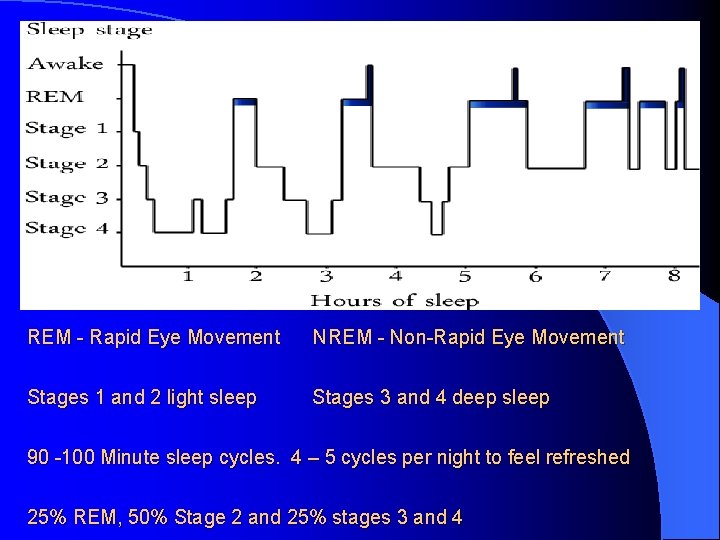
REM Rapid Eye Movement NREM NonRapid Eye Movement



- Slides: 61
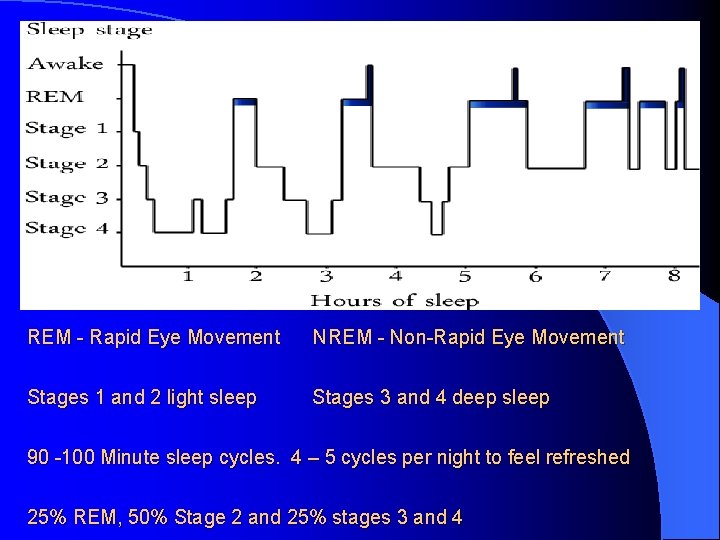
REM - Rapid Eye Movement NREM - Non-Rapid Eye Movement Stages 1 and 2 light sleep Stages 3 and 4 deep sleep 90 -100 Minute sleep cycles. 4 – 5 cycles per night to feel refreshed 25% REM, 50% Stage 2 and 25% stages 3 and 4

Parasomnias: In REM Sleep Behaviour Disorder. (REM without muscle atonia) REMdisorder. mp 4 behavior
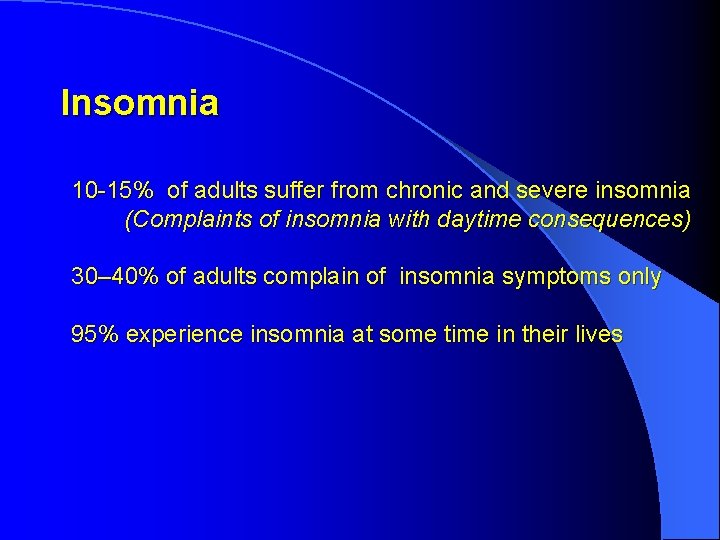
The most common sleep disorders are associated with: 1) Shiftwork Up to 20% of the workforce are shiftworkers 2) Insomnia 10 – 15% of adults suffer from chronic and severe insomnia that affects daytime performance. 3) Snoring and Obstructive Sleep Apnoea (OSA) Snoring – up to 60% adults snore regularly OSAS – 9% of males, 4% females over 40
Circadian Rhythms Circa Dies = About a day Controlled by Internal body clock - The Suprachiasmatic Nucleus (SCN) - Core body temperature circadian cycle - The role of our own Melatonin External environment cues – Zeitgebers (Time keepers) - The effect of light Exercise Meals
Insomnia
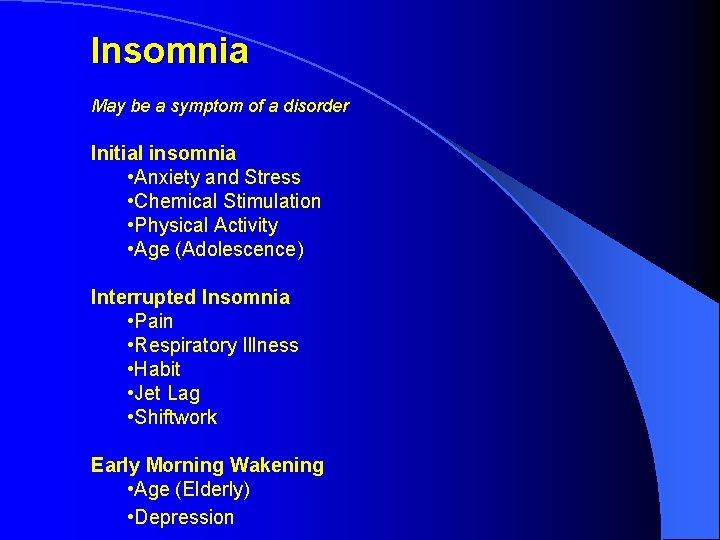
Insomnia May be a symptom of a disorder Initial insomnia • Anxiety and Stress • Chemical Stimulation • Physical Activity • Age (Adolescence) Interrupted Insomnia • Pain • Respiratory Illness • Habit • Jet Lag • Shiftwork Early Morning Wakening • Age (Elderly) • Depression
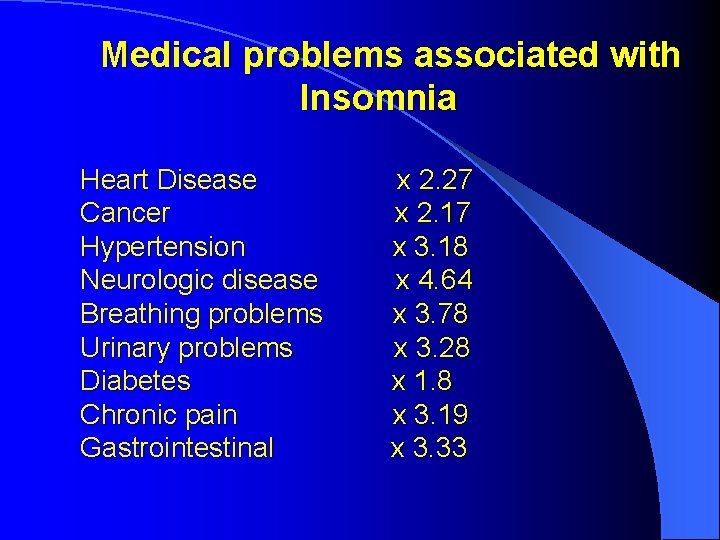
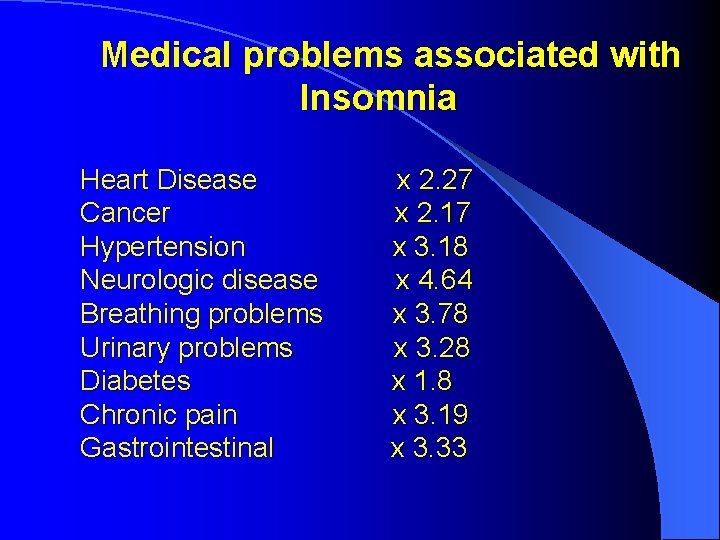
Medical problems associated with Insomnia Heart Disease Cancer Hypertension Neurologic disease Breathing problems Urinary problems Diabetes Chronic pain Gastrointestinal x 2. 27 x 2. 17 x 3. 18 x 4. 64 x 3. 78 x 3. 28 x 1. 8 x 3. 19 x 3. 33
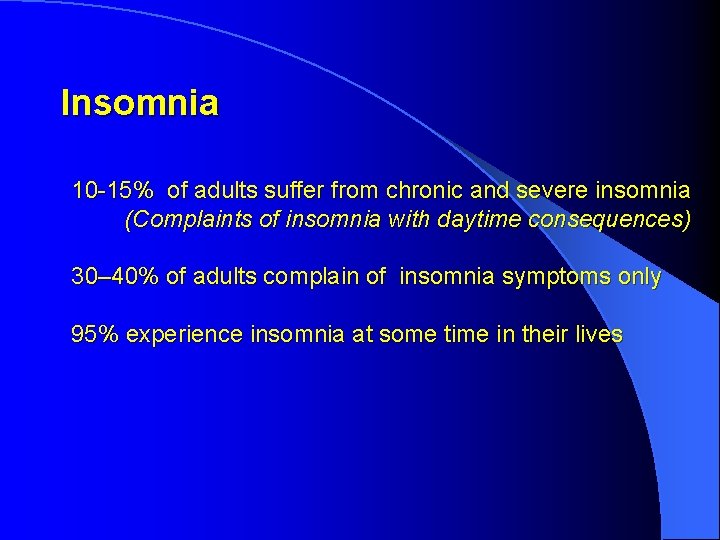
Insomnia 10 -15% of adults suffer from chronic and severe insomnia (Complaints of insomnia with daytime consequences) 30– 40% of adults complain of insomnia symptoms only 95% experience insomnia at some time in their lives
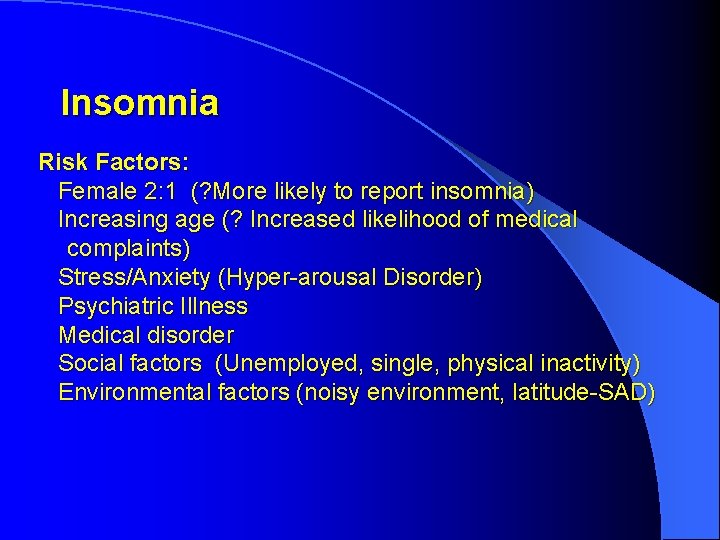
Insomnia Risk Factors: Female 2: 1 (? More likely to report insomnia) Increasing age (? Increased likelihood of medical complaints) Stress/Anxiety (Hyper-arousal Disorder) Psychiatric Illness Medical disorder Social factors (Unemployed, single, physical inactivity) Environmental factors (noisy environment, latitude-SAD)
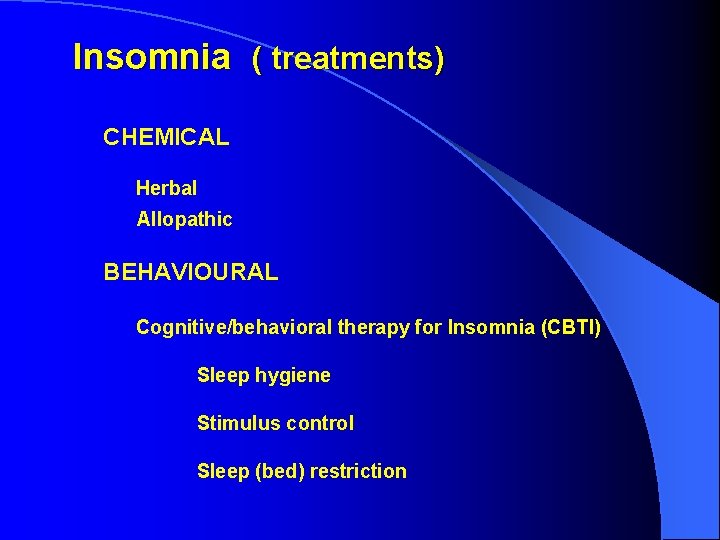
Insomnia ( treatments) CHEMICAL Herbal Allopathic BEHAVIOURAL Cognitive/behavioral therapy for Insomnia (CBTI) Sleep hygiene Stimulus control Sleep (bed) restriction
Insomnia HERBAL MEDICINES VALARIAN KAVA ST JOHN WORT MELATONIN CHAMOMILLE OTHERS
Insomnia Melatonin Two therapeutic uses: 1. As a chronobiotic Use a small dose (0. 5 mg), 5 hrs before desired sleep onset 2. As a soporific Use a larger dose (2 mg or 3 mg) ½ -1 hr before desired sleep onset
Insomnia Melatonin Two therapeutic uses: 1. As a chronobiotic Melatonin in the evening will advance the sleep phase (Earlier to sleep and earlier to wake) Melatonin in the morning will (theoretically) delay the sleep phase (Later to sleep and later to wake)
Insomnia Melatonin Two therapeutic uses: 2. As a soporific For children with ADHD or ASD Some small evidence that their melatonin levels are low For those over 55 yrs Melatonin levels tend to fall with age Not helpful for those under 55 yrs
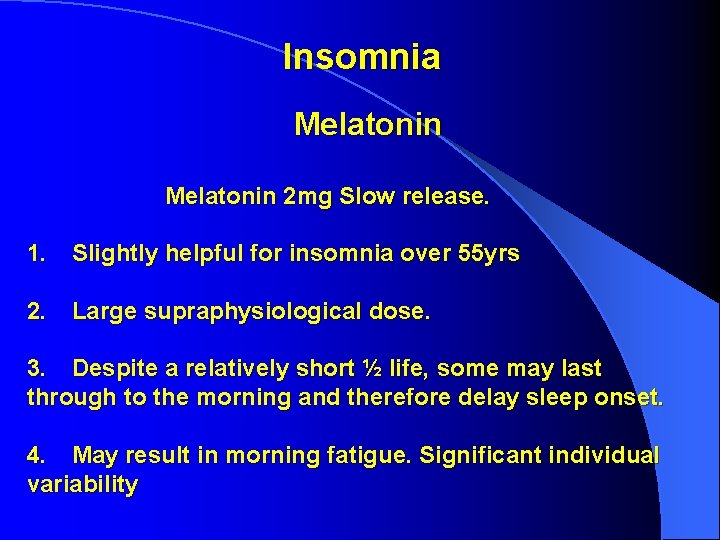
Insomnia Melatonin 2 mg Slow release. 1. Slightly helpful for insomnia over 55 yrs 2. Large supraphysiological dose. 3. Despite a relatively short ½ life, some may last through to the morning and therefore delay sleep onset. 4. May result in morning fatigue. Significant individual variability
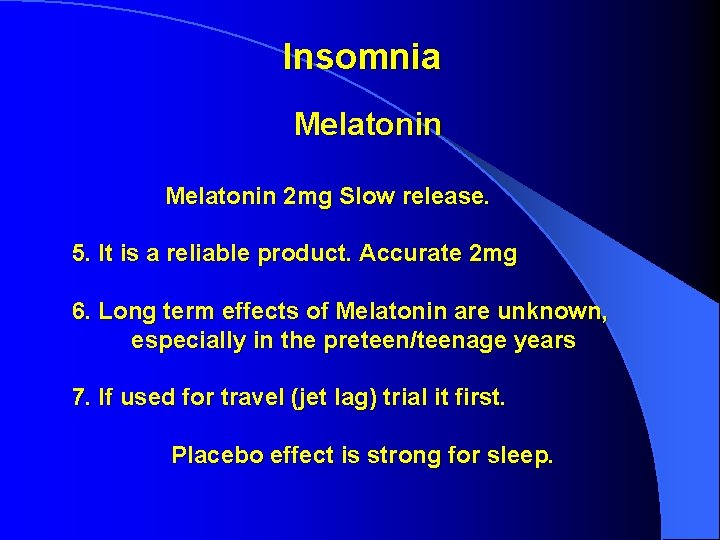
Insomnia Melatonin 2 mg Slow release. 5. It is a reliable product. Accurate 2 mg 6. Long term effects of Melatonin are unknown, especially in the preteen/teenage years 7. If used for travel (jet lag) trial it first. Placebo effect is strong for sleep.
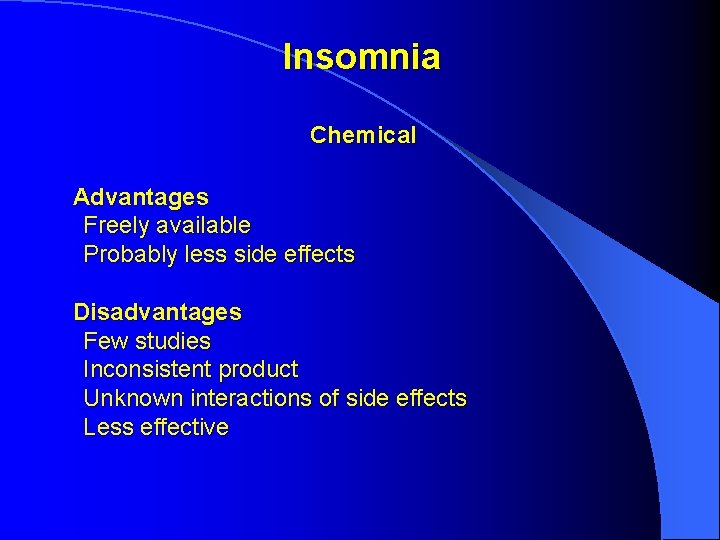
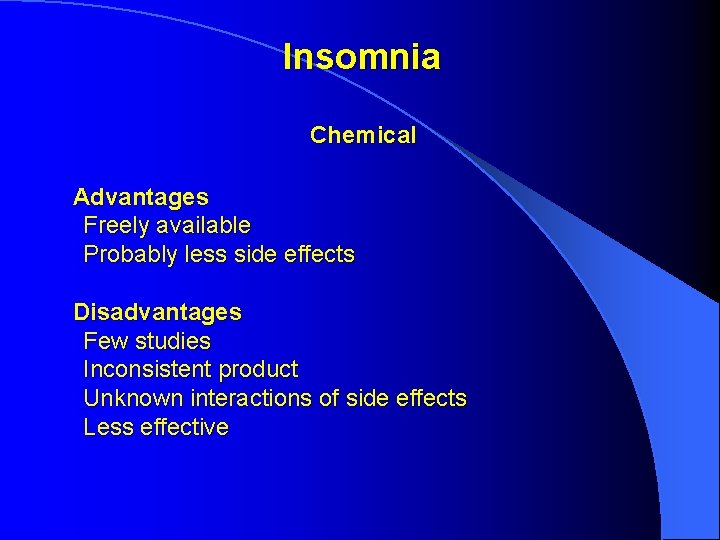
Insomnia Chemical Advantages Freely available Probably less side effects Disadvantages Few studies Inconsistent product Unknown interactions of side effects Less effective
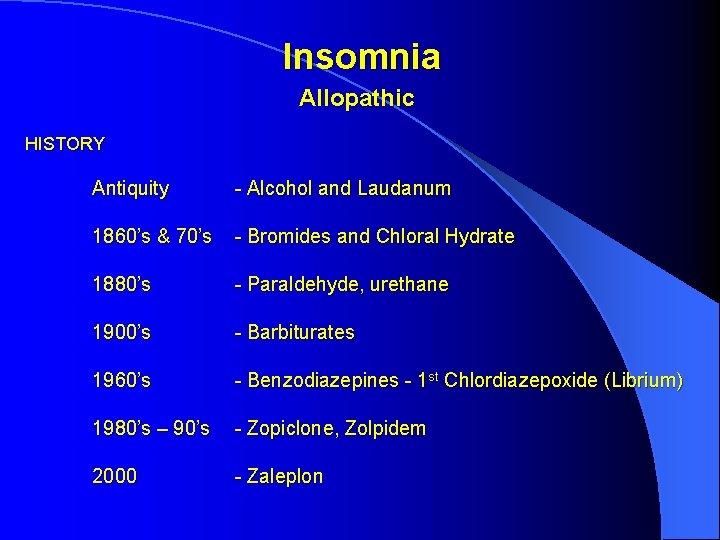
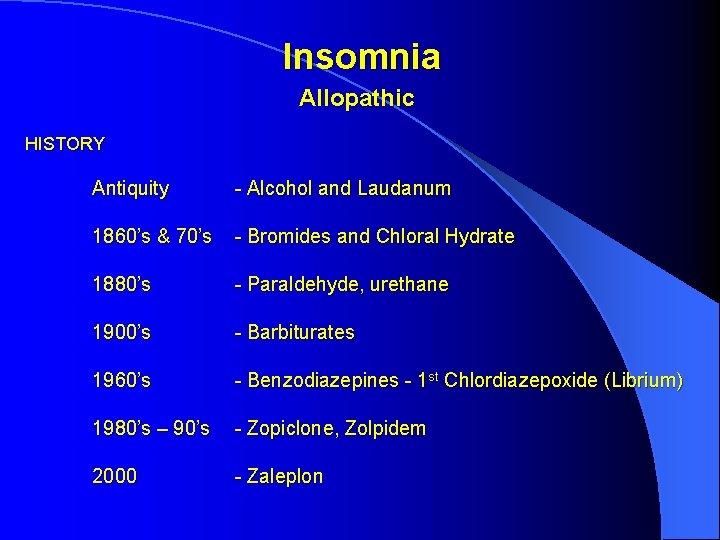
Insomnia Allopathic HISTORY Antiquity - Alcohol and Laudanum 1860’s & 70’s - Bromides and Chloral Hydrate 1880’s - Paraldehyde, urethane 1900’s - Barbiturates 1960’s - Benzodiazepines - 1 st Chlordiazepoxide (Librium) 1980’s – 90’s - Zopiclone, Zolpidem 2000 - Zaleplon
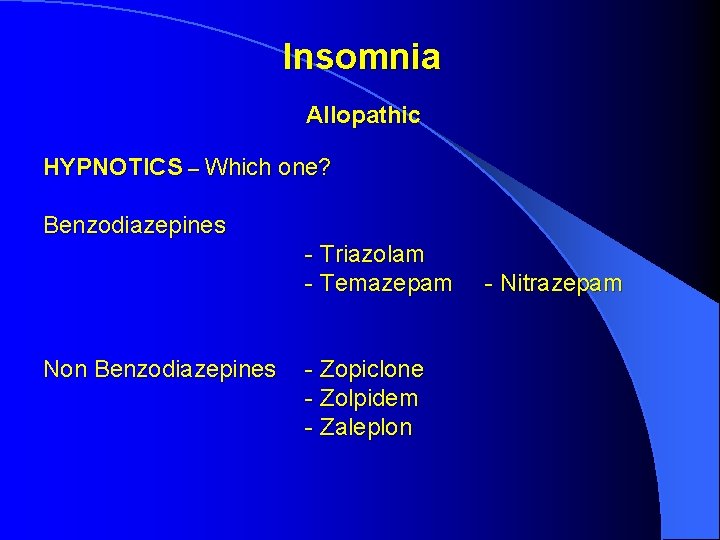
Insomnia Allopathic HYPNOTICS – Which one? Benzodiazepines - Triazolam - Temazepam Non Benzodiazepines - Zopiclone - Zolpidem - Zaleplon - Nitrazepam
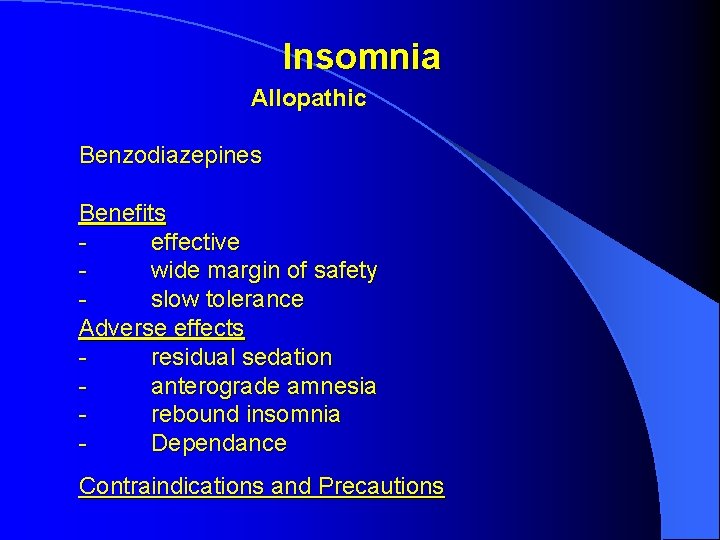
Insomnia Allopathic Benzodiazepines Benefits effective wide margin of safety slow tolerance Adverse effects residual sedation anterograde amnesia rebound insomnia Dependance Contraindications and Precautions
Insomnia Allopathic Hi Antihistamine daytime drowsiness impaired learning Sedating Antidepressants cardiotoxic anticholinergic increase RLS/P. L. M. s impaired daytime performance rapid tolerance
Insomnia Allopathic Use short acting hypnotics for short term treatment in low dose Use sedating antidepressants in full doses for insomnia associated with depression
Insomnia Evaluation: The three P’s - Predisposing Factors Genetics, Personality type, Social Pressures - Precipitating Factors Stressful life event(s). “Trigger” for insomnia. - Perpetuating Factors. Compensatory strategies. Eg longer in bed. Staying in bed. Alcohol use
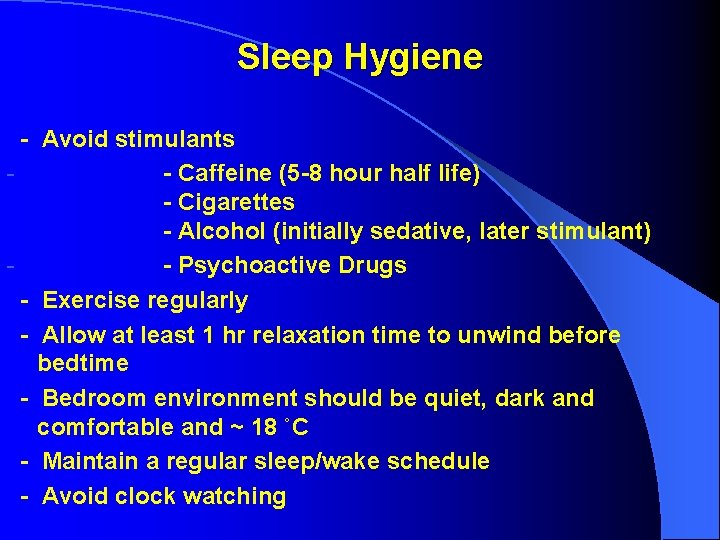
Sleep Hygiene To Provide information about lifestyle, and environment that might interfere with sleep, or promote better sleep. These strategies are important as a baseline, and should be combined with the other treatments. As a sole therapy, it is not effective for the more severe insomnia, but should be addressed in therapy.
Sleep Hygiene - Avoid stimulants - Caffeine (5 -8 hour half life) - Cigarettes - Alcohol (initially sedative, later stimulant) - Psychoactive Drugs - Exercise regularly - Allow at least 1 hr relaxation time to unwind before bedtime - Bedroom environment should be quiet, dark and comfortable and ~ 18 ˚C - Maintain a regular sleep/wake schedule - Avoid clock watching
Stimulus Control is based on classical conditioned response to certain stimuli. This involves strengthening the relationship between bed and sleep, and breaking the negative relationship between bed anxiety and wakefulness Important and Effective
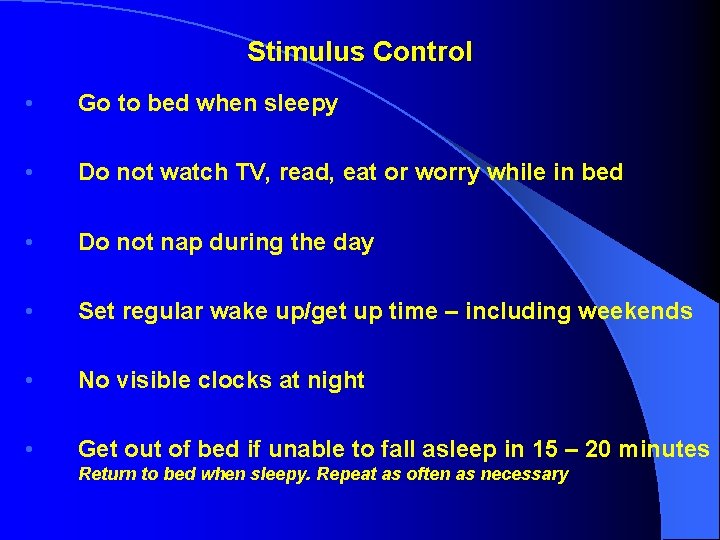
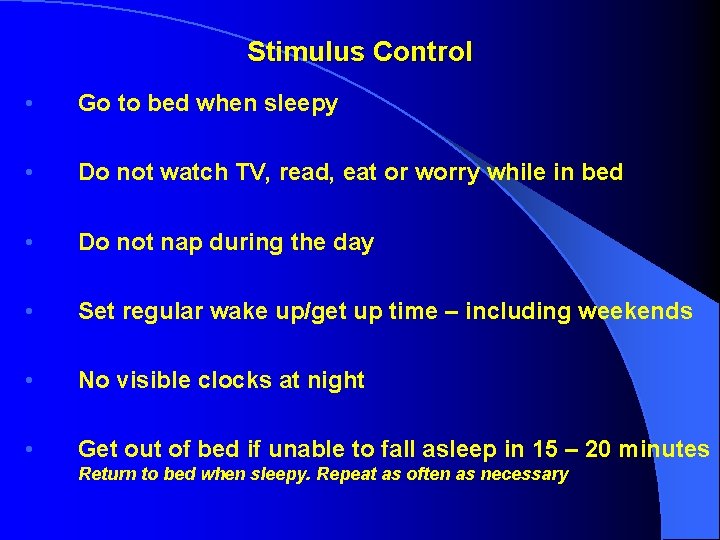
Stimulus Control • Go to bed when sleepy • Do not watch TV, read, eat or worry while in bed • Do not nap during the day • Set regular wake up/get up time – including weekends • No visible clocks at night • Get out of bed if unable to fall asleep in 15 – 20 minutes Return to bed when sleepy. Repeat as often as necessary
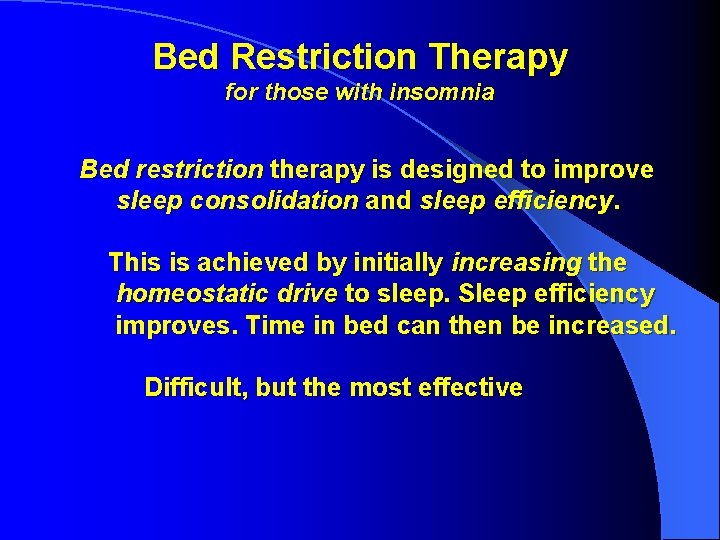
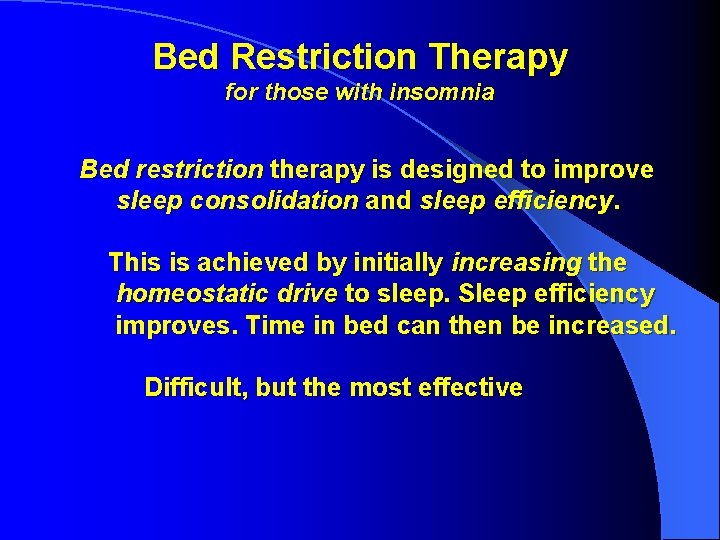
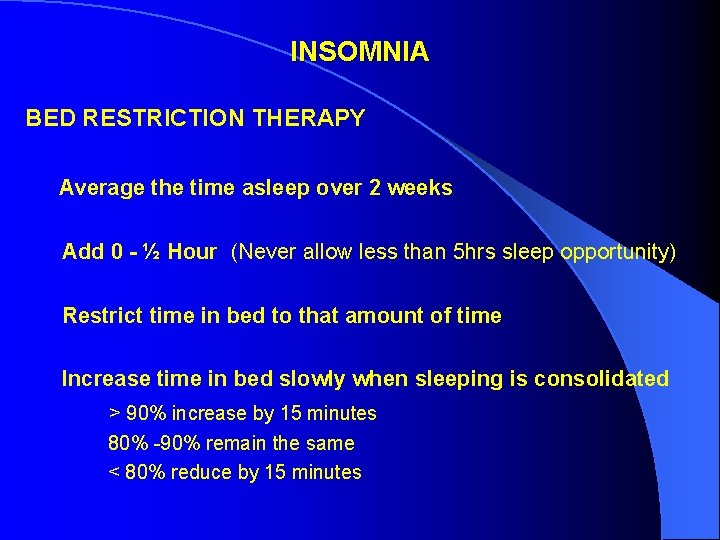
Bed Restriction Therapy for those with insomnia Bed restriction therapy is designed to improve sleep consolidation and sleep efficiency. This is achieved by initially increasing the homeostatic drive to sleep. Sleep efficiency improves. Time in bed can then be increased. Difficult, but the most effective
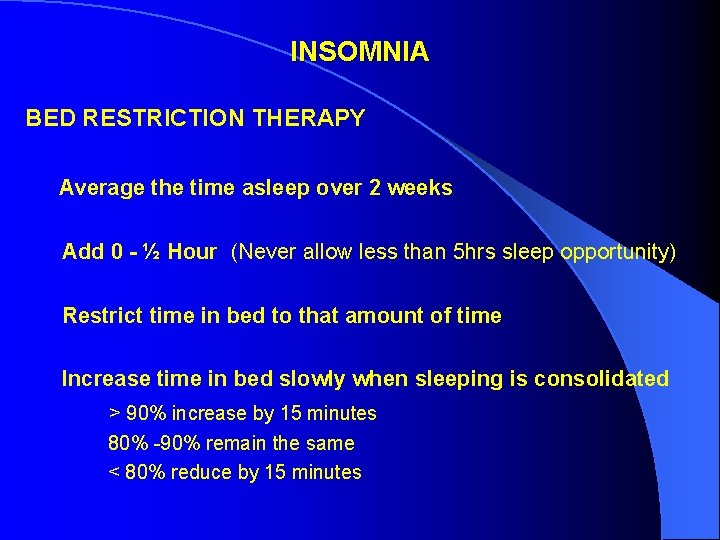
INSOMNIA BED RESTRICTION THERAPY Average the time asleep over 2 weeks Add 0 - ½ Hour (Never allow less than 5 hrs sleep opportunity) Restrict time in bed to that amount of time Increase time in bed slowly when sleeping is consolidated > 90% increase by 15 minutes 80% -90% remain the same < 80% reduce by 15 minutes
A Therapeutic model Having discussed Sleep Hygiene, and Relaxation therapies, discuss Stimulus Control, and Bed Restriction.
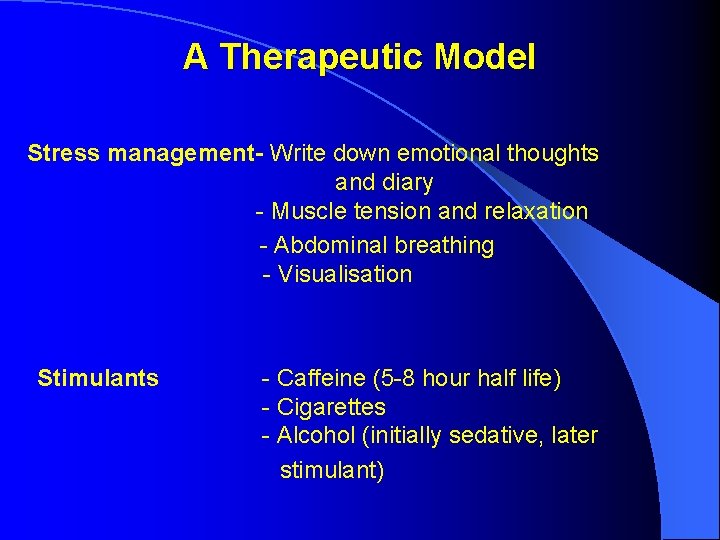
A Therapeutic Model Stress management- Write down emotional thoughts and diary - Muscle tension and relaxation - Abdominal breathing - Visualisation Stimulants - Caffeine (5 -8 hour half life) - Cigarettes - Alcohol (initially sedative, later stimulant)
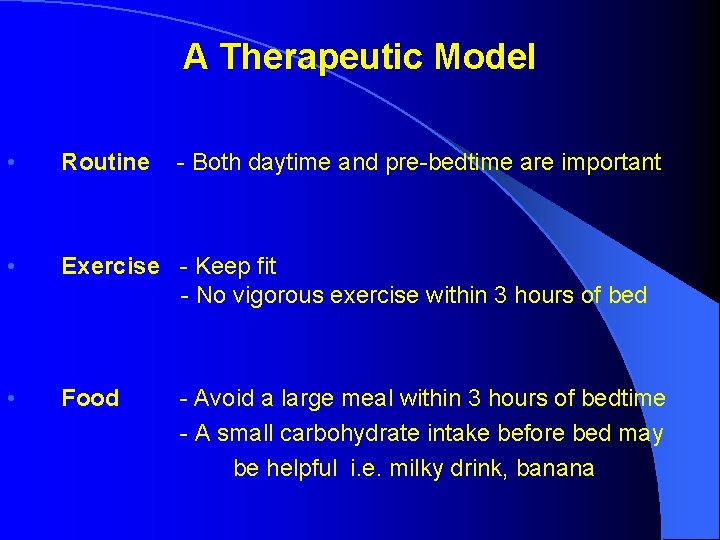
A Therapeutic Model • Routine • Exercise - Keep fit - No vigorous exercise within 3 hours of bed • Food - Both daytime and pre-bedtime are important - Avoid a large meal within 3 hours of bedtime - A small carbohydrate intake before bed may be helpful i. e. milky drink, banana
A Therapeutic Model • Temperature - Avoid extremes of temperature - Cooling will keep sleep • Light - Light stimulates serotonin and inhibits melatonin and sleep. - Be outside in the day as much as possible • Dark - Stimulates Melatonin that helps sleep therefore keep bedroom dark at night
A Therapeutic model • Noise - Sudden noise awakens. A constant low intensity noise may be helpful • The bed - Firmer and larger rather than sagging and small - Avoid synthetic sheets - Use feather or down unless allergic to house dust mite
Stimulus Control • In Bed - If awake after 20 minutes or your mind is alert, get up for 20 -30 minutes. - use time out of bed to “wind down” and prepare again for sleep (warm, dim light, write down what is on your mind, light reading material, comfortable chair), return to bed and repeat as necessary - Avoid working or playing in bedroom - The bedroom is for sleep and sex only
The Agony or the Ecstasy Familiar?
Snoring Related Complaints - Drives wife from bedroom - Girlfriend won’t marry me - Shakes entire house - Ask me to leave movies and church - Has had to leave boat so friends could sleep - Fall asleep at traffic lights waiting for red light to change
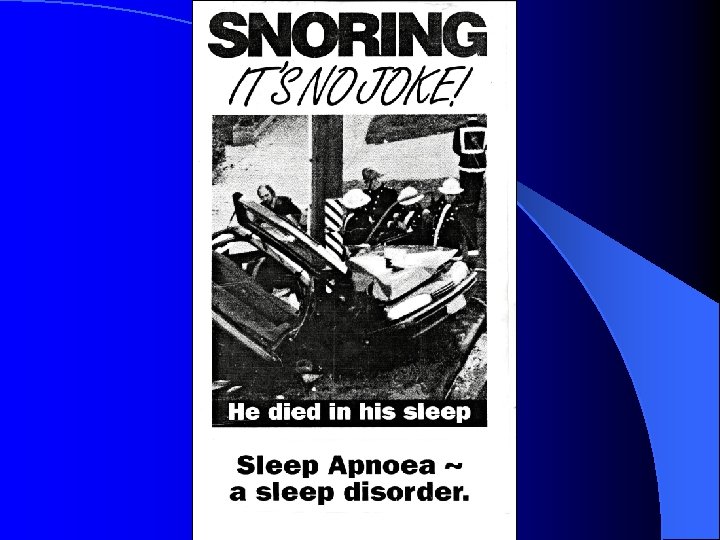
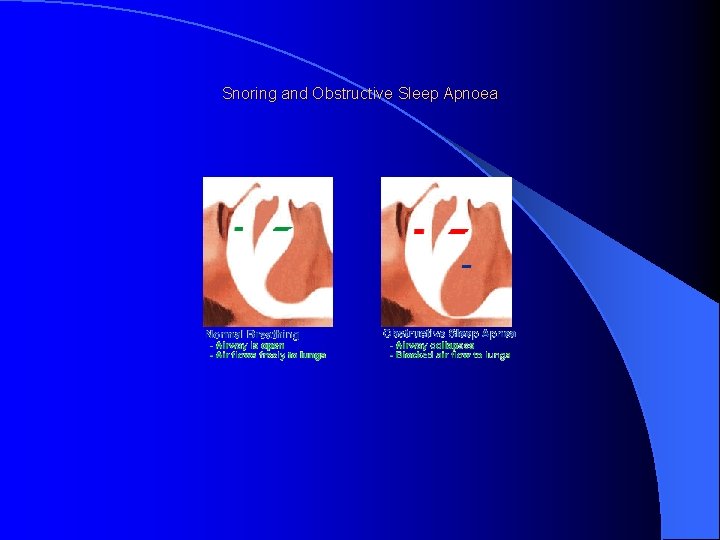
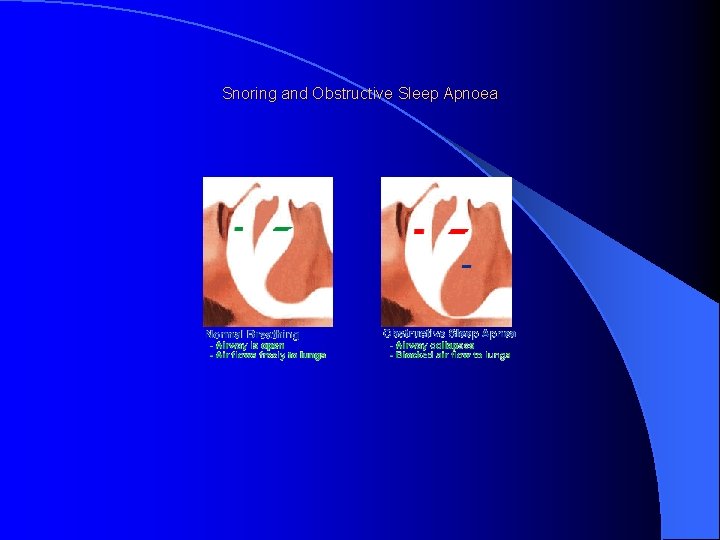
Snoring and Obstructive Sleep Apnoea
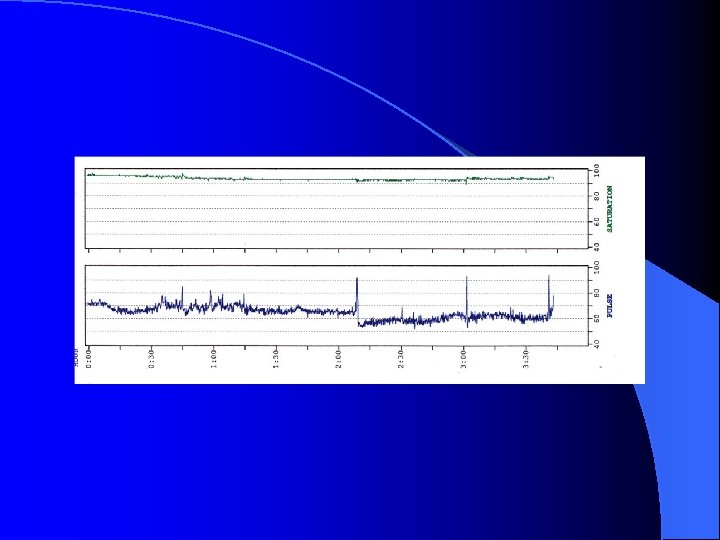
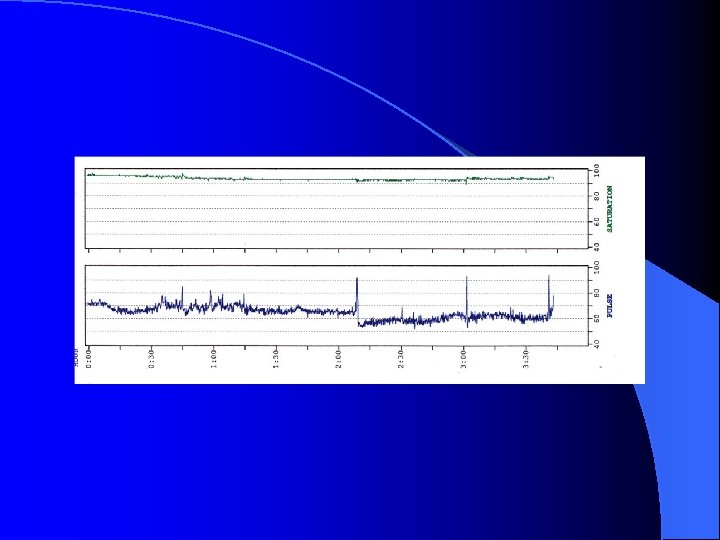
Consequences of Sleep Apnoea 1. Daytime fatigue, especially sleepiness 2. Bed partner sleep disturbance 3. Cardiovascular complications
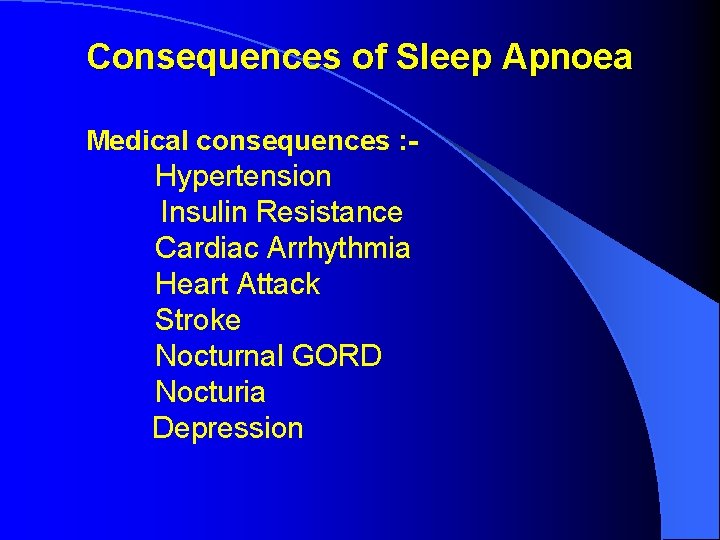
Consequences of Sleep Apnoea Medical consequences : - Hypertension Insulin Resistance Cardiac Arrhythmia Heart Attack Stroke Nocturnal GORD Nocturia Depression
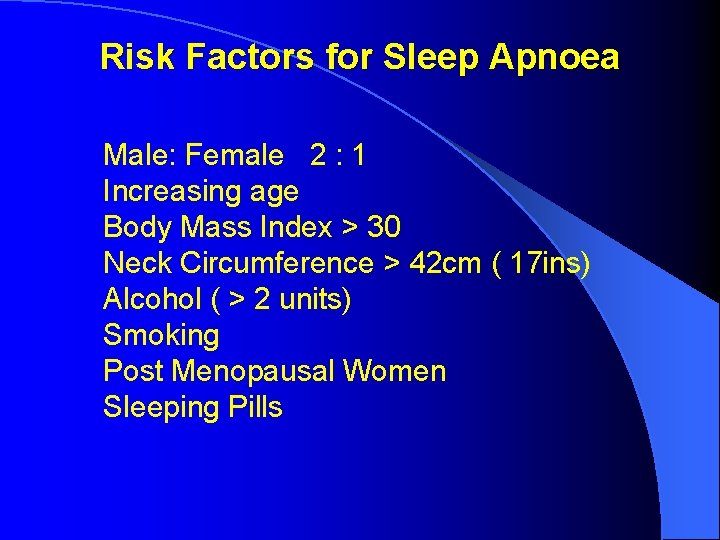
Risk Factors for Sleep Apnoea Male: Female 2 : 1 Increasing age Body Mass Index > 30 Neck Circumference > 42 cm ( 17 ins) Alcohol ( > 2 units) Smoking Post Menopausal Women Sleeping Pills
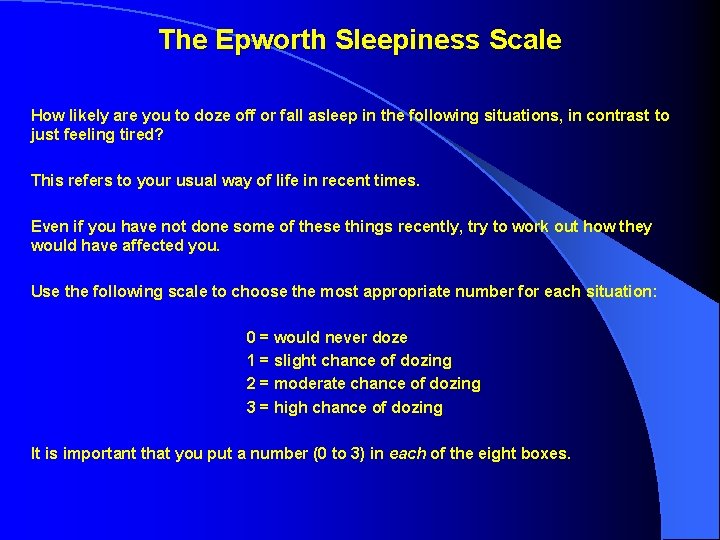
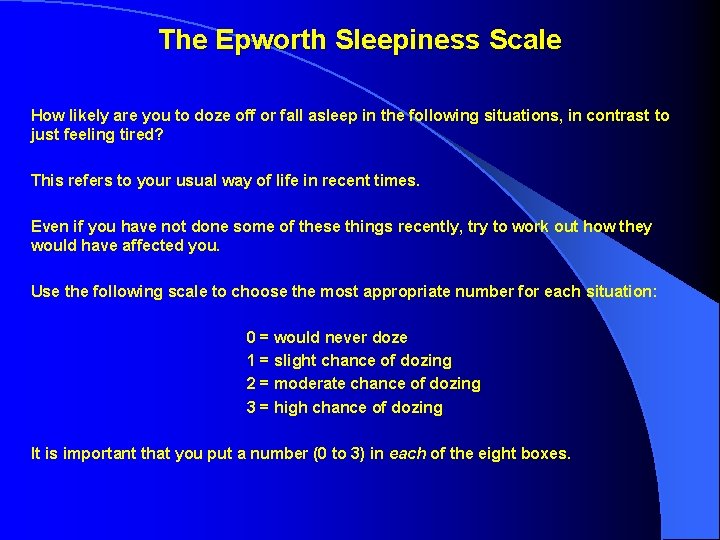
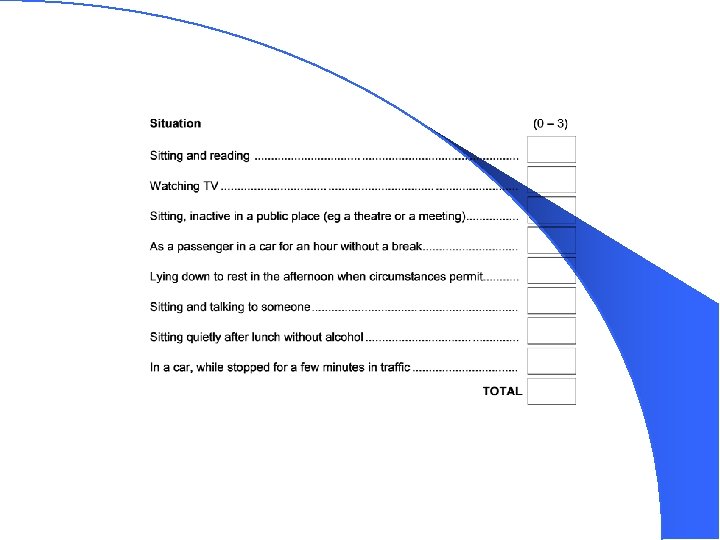
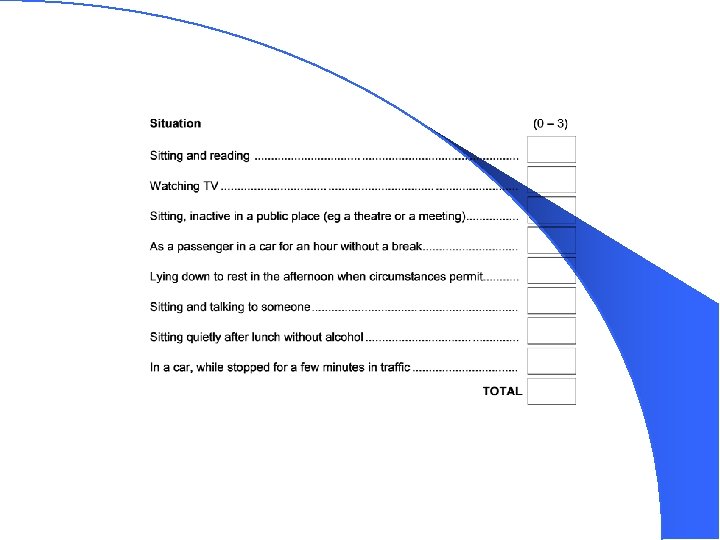
The Epworth Sleepiness Scale How likely are you to doze off or fall asleep in the following situations, in contrast to just feeling tired? This refers to your usual way of life in recent times. Even if you have not done some of these things recently, try to work out how they would have affected you. Use the following scale to choose the most appropriate number for each situation: 0 = would never doze 1 = slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing It is important that you put a number (0 to 3) in each of the eight boxes.
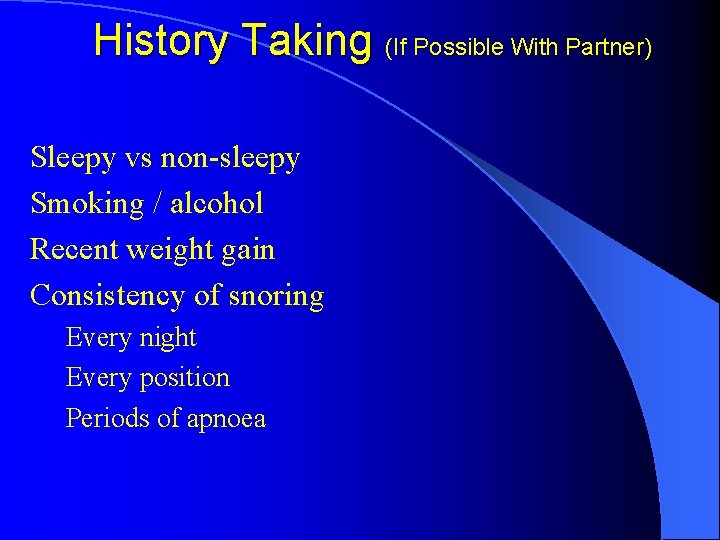
History Taking (If Possible With Partner) Sleepy vs non-sleepy Smoking / alcohol Recent weight gain Consistency of snoring Every night Every position Periods of apnoea
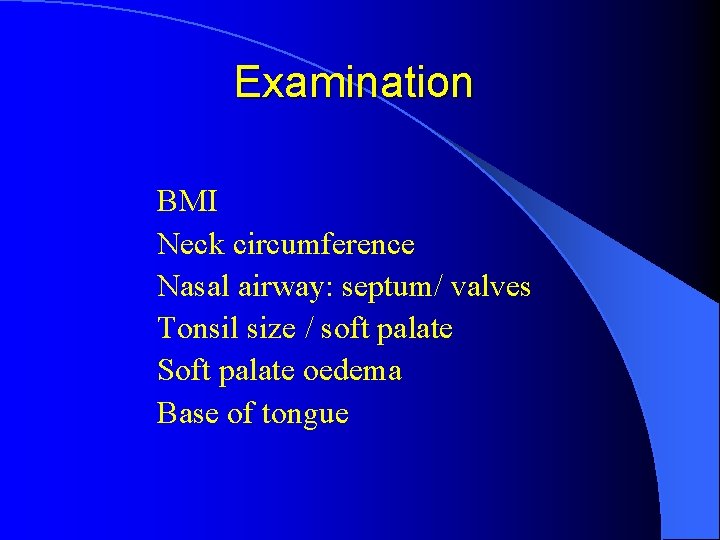
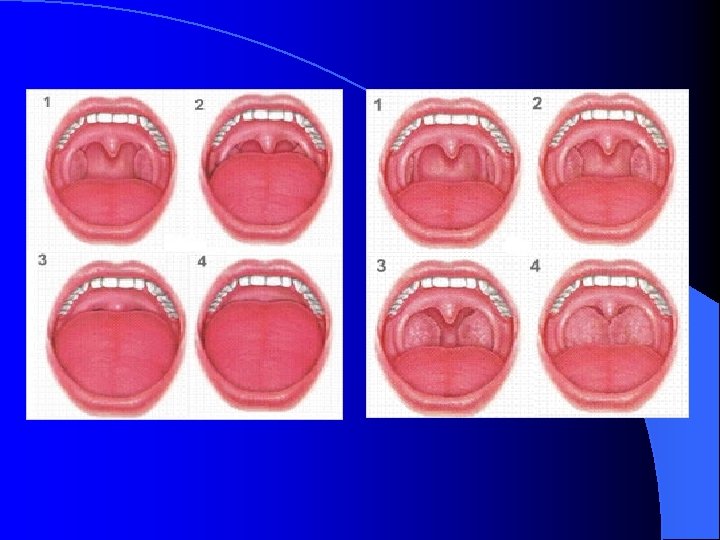
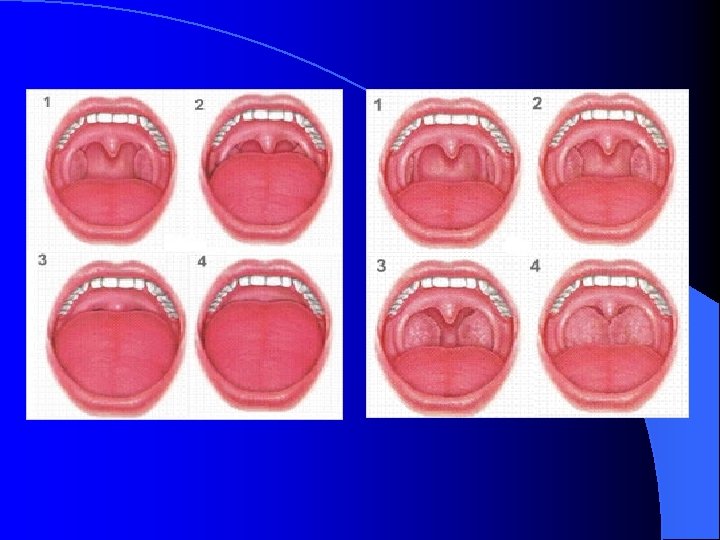
Examination BMI Neck circumference Nasal airway: septum/ valves Tonsil size / soft palate Soft palate oedema Base of tongue
Conservative Weight loss Alcohol reduction Stop smoking Avoid sleeping tablets Keep off back
Managements Lifestyle Sleep position, i. e. Side Upright Control of Obesity Avoidance of alcohol and drugs (especially BZD’s)
Surgical Managements Adenotonsilectomy -- especially in children, rarely in adults Uvulopalatopharyngoplasty (UPPP) -- rarely helpful Nasal surgery generally unhelpful Palatal surgery

Surgical Managements Other surgery Tracheostomy Weight loss surgery
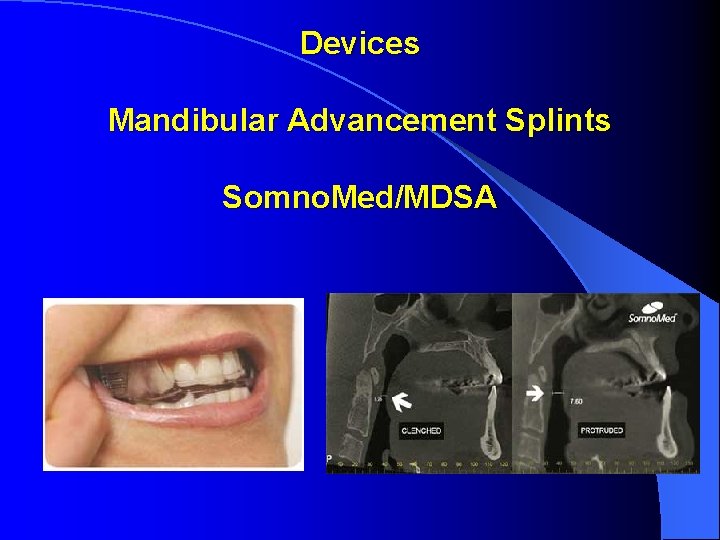
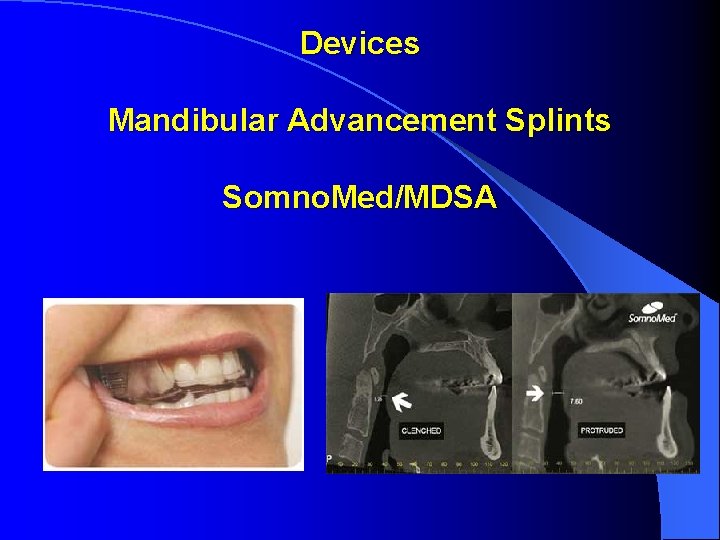
Devices Mandibular Advancement Splints Somno. Med/MDSA
Devices Aveo TSD Tongue Stabilising Device
Devices External nasal splints Not helpful Internal nasal splints
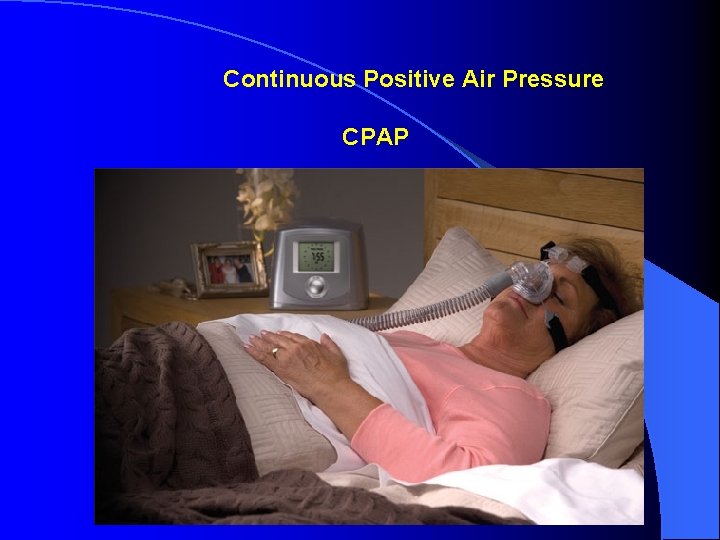
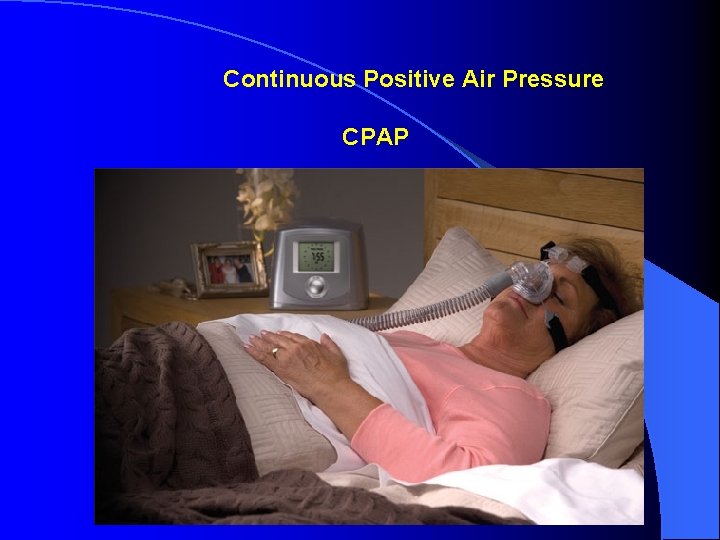
Continuous Positive Air Pressure CPAP
KEY QUESTIONS: 1. Do you snore? 2. Are you sleepy?
Laugh and the world laughs with you… …snore and you sleep alone.

Thank You Dr Alex Bartle MB BS FRNZCGP Dip Obst MMed (Sleep Medicine) SLEEP WELL CLINIC Auckland Christchurch Wellington Tauranga Whangarei Nelson & Invercargill