Regulatory Considerations for Coronary Drug Coated Balloons Andrew

Regulatory Considerations for Coronary Drug Coated Balloons Andrew Farb, MD Division of Cardiovascular Devices Center for Devices and Radiological Health (CDRH) Food and Drug Administration andrew. farb@fda. hhs. gov DES Bioabsorbable and DCB Technologies: Coronary CRT 2016 Washington, DC February 22, 2016
Conflict of Interest No conflicts of interest to report 2

Components of a Drug-Eluting Balloon (DCB) Combination Product PTCA Balloon Coating Delivery System Therapeutic Agent

DCB Regulatory Pathway CDRH is the lead Center for DCB combination products – Primary DCB mode of action • Arterial dilatation to increase blood flow to target tissue – Secondary DCB mode of action • Drug delivery to target lesion to prevent restenosis 4

DCB Regulatory Submissions • For clinical studies in the US – DCBs are significant risk devices – Investigational Device Exemption (IDE) approved by FDA required to conduct clinical studies of: • An investigational DCB or • An approved DCB for a new indication (e. g. , an approved peripheral DCB being used in the coronary vascular bed • For FDA approval: Premarket Approval Application (PMA) – Comprehensive review of bench testing, animal studies, and all clinical data – Establish a reasonable assurance of safety and effectiveness 5
Types of Device Clinical Studies • Feasibility studies – Early feasibility studies (including some FIH studies) – Traditional feasibility studies • Pivotal studies: Intended to collect definitive evidence of safety and effectiveness 6
Early Feasibility Study (EFS) • Small number of subjects • Device may be early in development, typically before the device design has been finalized – Does not necessarily involve the first clinical use of a device • May involve a new intended use for a device that has already been in clinical use • Needed when the information to advance device development cannot be practically obtained with additional nonclinical assessments, or if nonclinical tests are unavailable • May be done concurrently or in conjunction with non. US clinical studies 7
Targeting IDE Approval • Utilize the pre-submission process to discuss non-clinical test methods with FDA for efficient use of resources – Identify bench and animal studies to provide adequate safety information to support IDE approval • Some nonclinical studies can be performed concurrent with clinical studies • Consider benefit-risk principles – Underlying clinical condition – Limitations of alternative therapies with respect to safety and effectiveness • Include risk mitigation strategies in the clinical study protocol – Particularly important for feasibility studies http: //www. fda. gov/downloads/medicaldevices/deviceregulationandguida nce/guidancedocuments/ucm 311176. pdf 8
DCB Nonclinical Testing Objectives The finalized DCB: • Can be reproducibly manufactured with respect to coating integrity, coating uniformity, and shelf life stability • Retains a consistent uniform amount of residual drug on the balloon following catheter advancement to the target lesion • Does not result in adverse downstream tissue events 9

DCB Nonclinical Testing Objectives The finalized DCB Provides consistent drug delivery to the artery that: • Delivers a uniform concentration of drug along the length of the target lesion • Can inhibit neointimal growth (expectation of effectiveness) • Does not produce local toxic effects acutely or during follow-up (due to excessive drug retention in surrounding tissue) • Does not result in systemic drug concentrations that produce off-target adverse events 10
DCB Bench Testing • Review FDA Guidance documents – For PTCA component: Class II Special Controls Guidance for PTCA Catheters – For Drug component: Draft Coronary DES Guidance • Discuss specific bench tests to support intended indication (e. g. , coronary vs. peripheral arteries, ISR, small vessels, bifurcation side branches) • Conduct testing to evaluate expected worst case clinical use and corners of product matrix • Address use of DCB for multiple inflations (if applicable) 11
Limitations of Bench Testing • Some bench tests lack recognized acceptance criteria • Acceptable in vivo animal study safety data (and available clinical data if available) can address potential safety concerns regarding: – High local drug concentrations – Particulate generation 12
In Vitro and In Vivo PK Evaluation • Assess – Retained vs. lost drug during catheter transit to target site – Serum and tissue drug levels • Local tissue dose/response helpful to establish the lowest effective dose 13
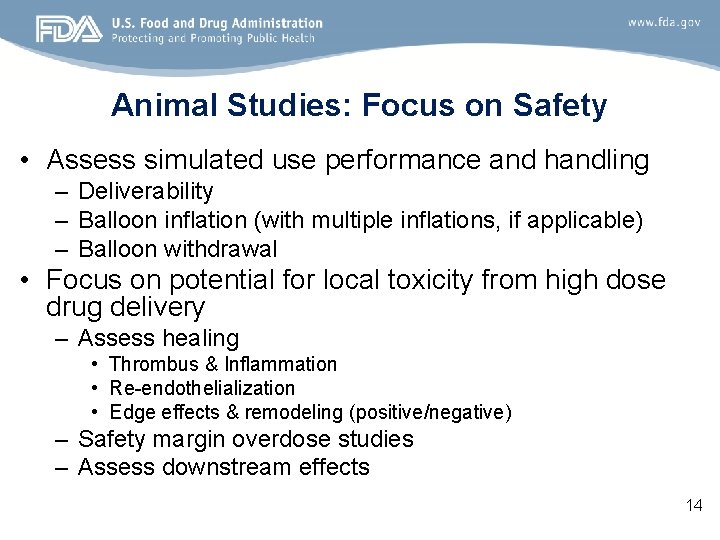
Animal Studies: Focus on Safety • Assess simulated use performance and handling – Deliverability – Balloon inflation (with multiple inflations, if applicable) – Balloon withdrawal • Focus on potential for local toxicity from high dose drug delivery – Assess healing • Thrombus & Inflammation • Re-endothelialization • Edge effects & remodeling (positive/negative) – Safety margin overdose studies – Assess downstream effects 14
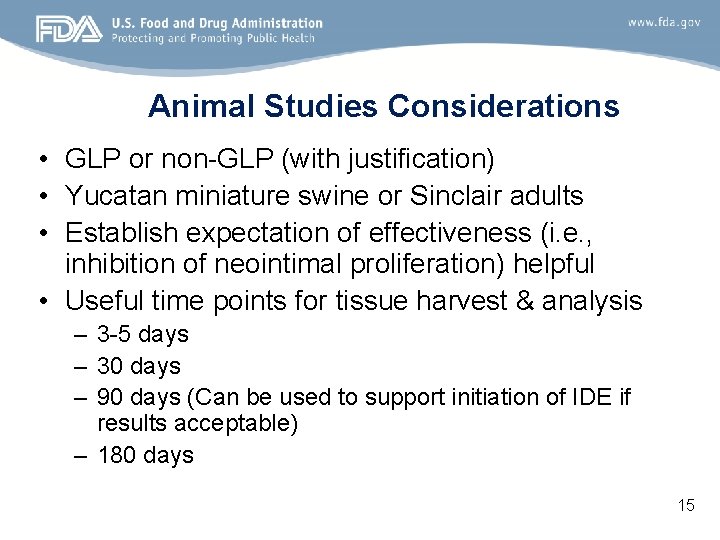
Animal Studies Considerations • GLP or non-GLP (with justification) • Yucatan miniature swine or Sinclair adults • Establish expectation of effectiveness (i. e. , inhibition of neointimal proliferation) helpful • Useful time points for tissue harvest & analysis – 3 -5 days – 30 days – 90 days (Can be used to support initiation of IDE if results acceptable) – 180 days 15
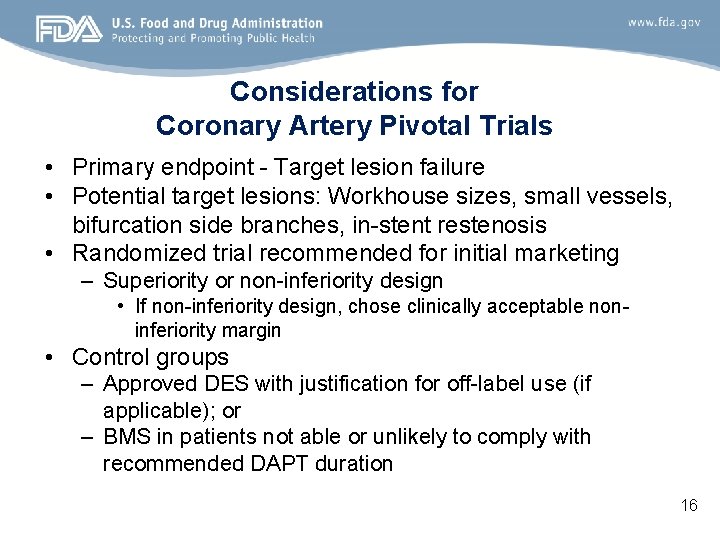
Considerations for Coronary Artery Pivotal Trials • Primary endpoint - Target lesion failure • Potential target lesions: Workhouse sizes, small vessels, bifurcation side branches, in-stent restenosis • Randomized trial recommended for initial marketing – Superiority or non-inferiority design • If non-inferiority design, chose clinically acceptable noninferiority margin • Control groups – Approved DES with justification for off-label use (if applicable); or – BMS in patients not able or unlikely to comply with recommended DAPT duration 16
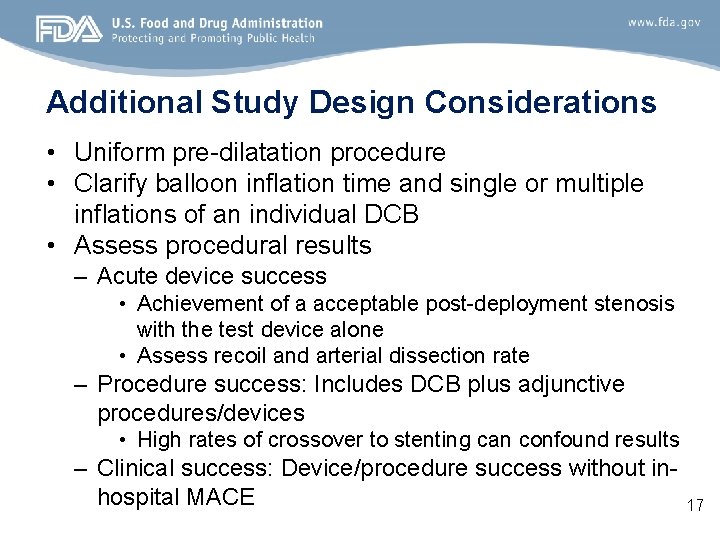
Additional Study Design Considerations • Uniform pre-dilatation procedure • Clarify balloon inflation time and single or multiple inflations of an individual DCB • Assess procedural results – Acute device success • Achievement of a acceptable post-deployment stenosis with the test device alone • Assess recoil and arterial dissection rate – Procedure success: Includes DCB plus adjunctive procedures/devices • High rates of crossover to stenting can confound results – Clinical success: Device/procedure success without inhospital MACE 17
Final Regulatory Comments • Post-approval studies (PAS) – Long-term follow-up of subjects in pre-market studies – Separate PAS cohort to evaluate real world use, operator training programs, and increase precision around the rates of low frequency events • Early discussions with FDA via the pre-submission program recommended – Nonclinical data for non-coronary use does not automatically satisfy requirements for a coronary use (and vice versa) – Use of non-US clinical data to support IDE and PMA approval 18
- Slides: 18