Regional Spinal Dr Anesthesia epidural Anesthesia moradi Objectives
Regional Spinal Dr Anesthesia &epidural Anesthesia moradi
Objectives ◦ Describe anatomy of spinal canal ◦ Identify anatomic landmarks for proper placement of a spinal needle ◦ Define appropriate steps for placement of spinal, epidural, or caudal needle ◦ Distinguish level of anesthesia after administration of regional ◦ State factors affecting level and duration of spinal vs. epidural block ◦ Explain potential complications and corresponding treatments associated with administration of regional anesthetics
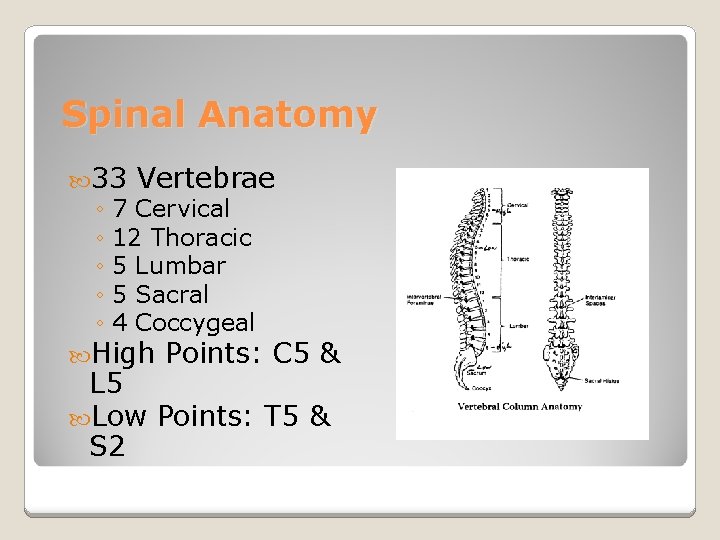
Spinal Anatomy 33 Vertebrae ◦ 7 Cervical ◦ 12 Thoracic ◦ 5 Lumbar ◦ 5 Sacral ◦ 4 Coccygeal High Points: C 5 & L 5 Low Points: T 5 & S 2
Spinal Cord ◦ Adult Begins: Foramen Magnum Ends: L 1 ◦ Newborn Begins: Foramen Magnum Ends: L 3 ◦ Terminal End: Conus Medullaris ◦ Filum Terminale: Anchors in sacral region ◦ Cauda Equina: Nerve group of lower dural sac
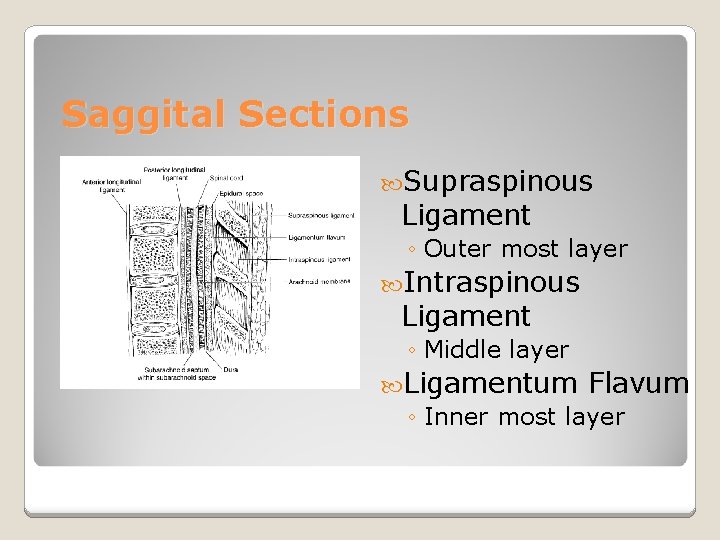
Saggital Sections Supraspinous Ligament ◦ Outer most layer Intraspinous Ligament ◦ Middle layer Ligamentum Flavum ◦ Inner most layer
Space that surrounds ◦ Potential space the spinal meninges Ligamentum Flavum ◦ Binds epidural space posteriorly Widest at Level L 2 (5 -6 mm) Narrowest at Level C 5 (1 -1. 5 mm) Epidural Space
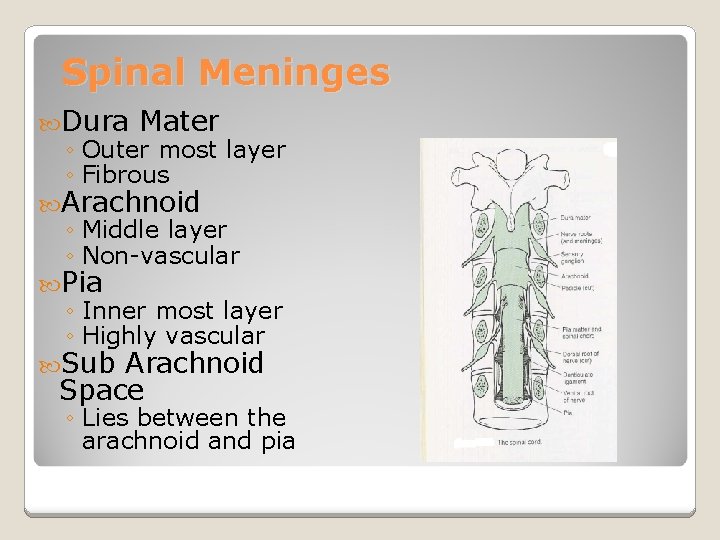
Spinal Meninges Dura Mater ◦ Outer most layer ◦ Fibrous Arachnoid ◦ Middle layer ◦ Non-vascular Pia ◦ Inner most layer ◦ Highly vascular Sub Arachnoid Space ◦ Lies between the arachnoid and pia
Vasoconstrictors ◦ Prolong duration of spinal block ◦ No increase in duration with lidocaine & bupivacaine ◦ Significant increase with tetracaine (double duration) Spinal Pharmacology
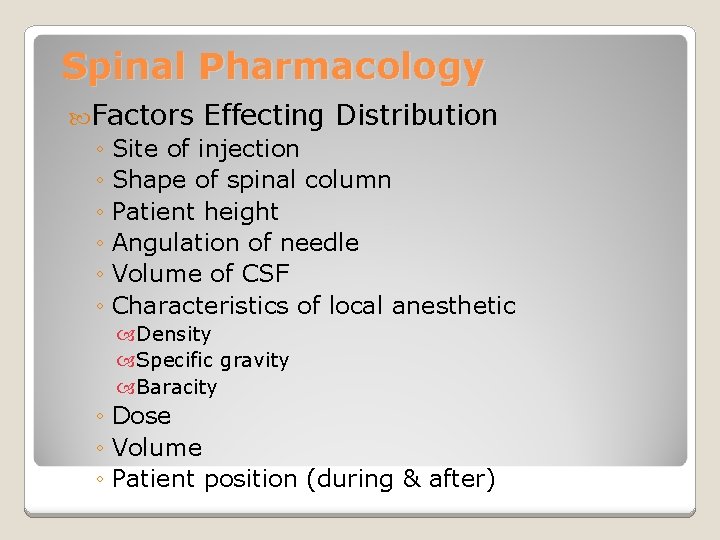
Spinal Pharmacology Factors Effecting Distribution ◦ Site of injection ◦ Shape of spinal column ◦ Patient height ◦ Angulation of needle ◦ Volume of CSF ◦ Characteristics of local anesthetic Density Specific gravity Baracity ◦ Dose ◦ Volume ◦ Patient position (during & after)
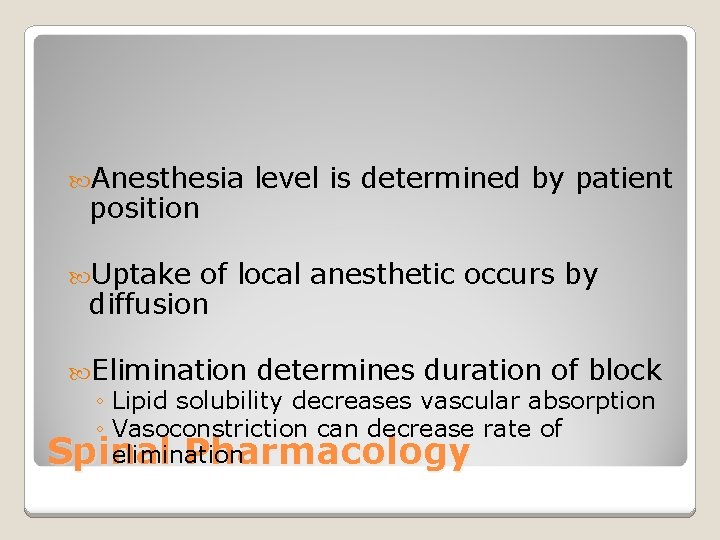
Anesthesia position level is determined by patient Uptake of local anesthetic occurs by diffusion Elimination determines duration of block ◦ Lipid solubility decreases vascular absorption ◦ Vasoconstriction can decrease rate of elimination Spinal Pharmacology
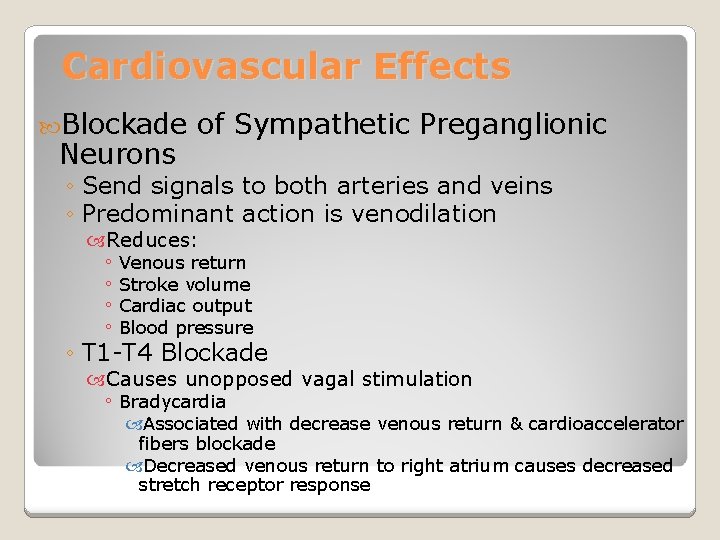
Cardiovascular Effects Blockade Neurons of Sympathetic Preganglionic ◦ Send signals to both arteries and veins ◦ Predominant action is venodilation Reduces: ◦ Venous return ◦ Stroke volume ◦ Cardiac output ◦ Blood pressure ◦ T 1 -T 4 Blockade Causes unopposed vagal stimulation ◦ Bradycardia Associated with decrease venous return & cardioaccelerator fibers blockade Decreased venous return to right atrium causes decreased stretch receptor response
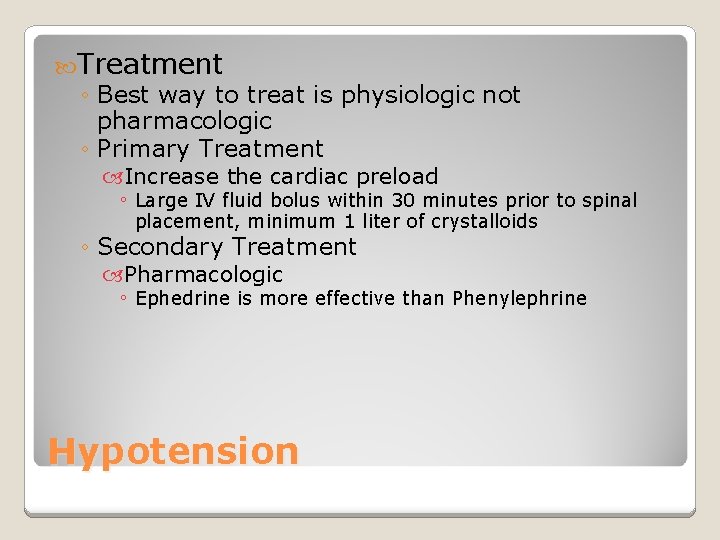
Treatment ◦ Best way to treat is physiologic not pharmacologic ◦ Primary Treatment Increase the cardiac preload ◦ Large IV fluid bolus within 30 minutes prior to spinal placement, minimum 1 liter of crystalloids ◦ Secondary Treatment Pharmacologic ◦ Ephedrine is more effective than Phenylephrine Hypotension
Healthy Patients ◦ Appropriate spinal blockade has little effect on ventilation High Spinal ◦ Decrease functional residual capacity (FRC) Paralysis of abdominal muscles Intercostal muscle paralysis interferes with coughing and clearing secretions Apnea is due to hypoperfusion of respiratory center Respiratory System
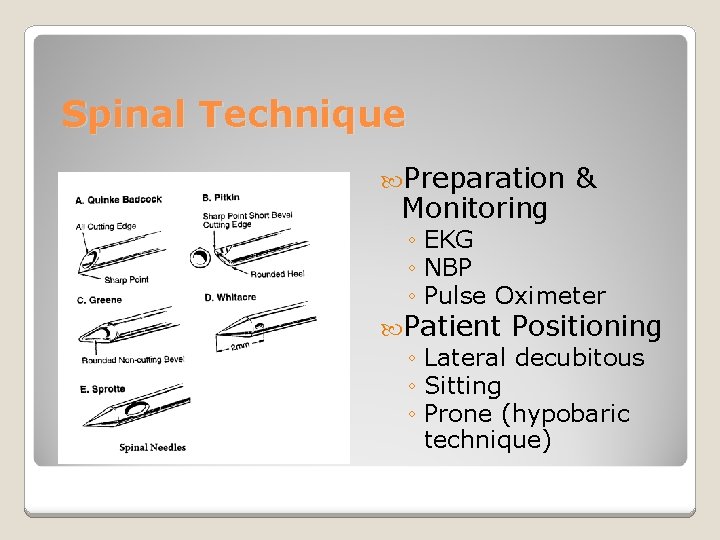
Spinal Technique Preparation Monitoring & ◦ EKG ◦ NBP ◦ Pulse Oximeter Patient Positioning ◦ Lateral decubitous ◦ Sitting ◦ Prone (hypobaric technique)
Spinal Technique Midline Approach ◦ Skin ◦ Subcutaneous tissue ◦ Supraspinous ligament ◦ Interspinous ligament ◦ Ligamentum flavum ◦ Epidural space ◦ Dura mater ◦ Arachnoid mater Paramedian or Lateral Approach ◦ Same as midline excluding supraspinous & interspinous ligaments
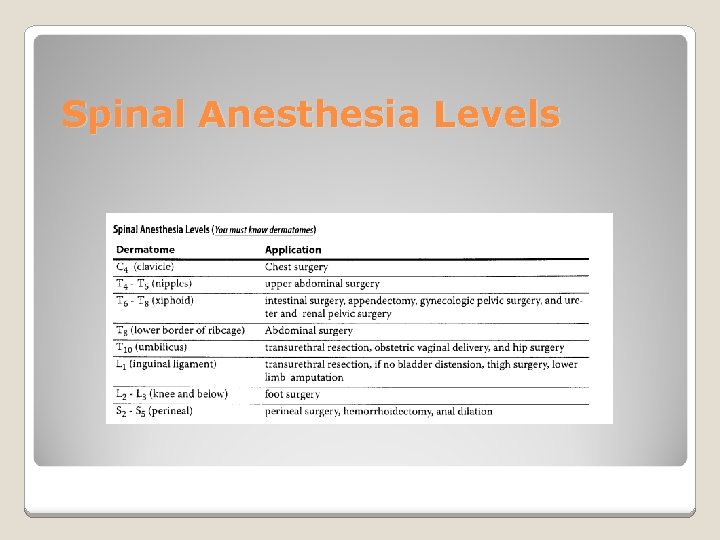
Spinal Anesthesia Levels
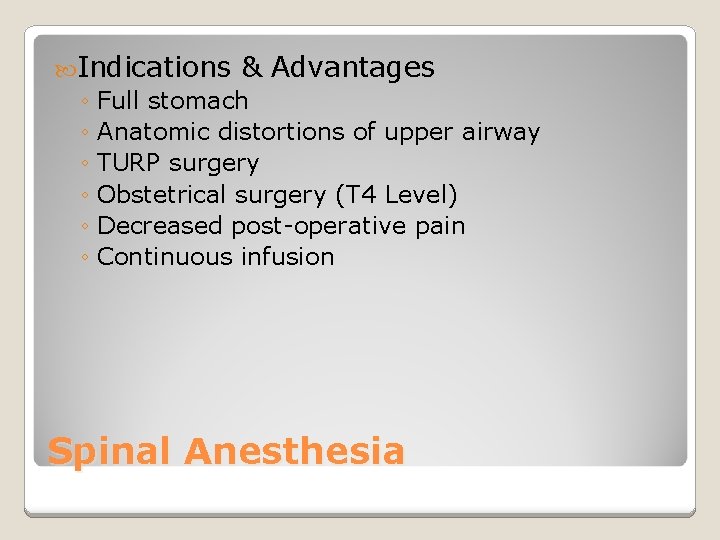
Indications & Advantages ◦ Full stomach ◦ Anatomic distortions of upper airway ◦ TURP surgery ◦ Obstetrical surgery (T 4 Level) ◦ Decreased post-operative pain ◦ Continuous infusion Spinal Anesthesia
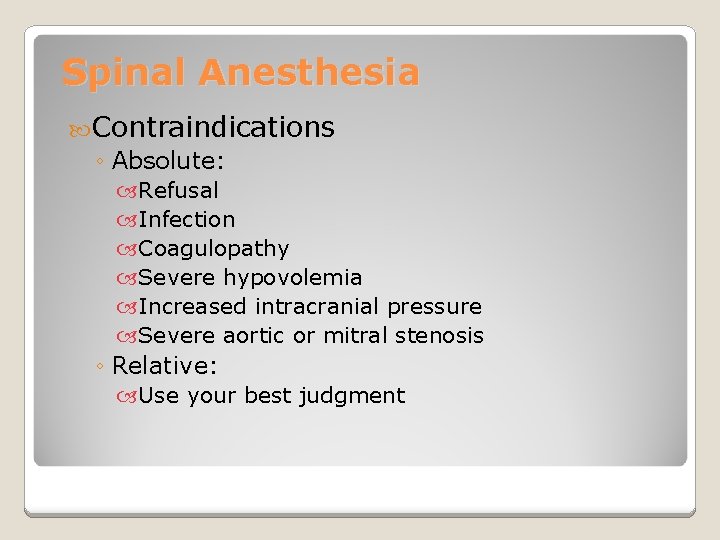
Spinal Anesthesia Contraindications ◦ Absolute: Refusal Infection Coagulopathy Severe hypovolemia Increased intracranial pressure Severe aortic or mitral stenosis ◦ Relative: Use your best judgment
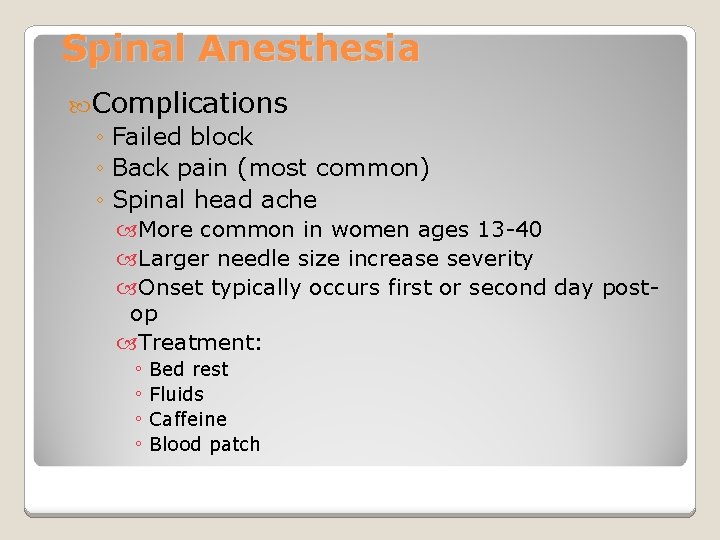
Spinal Anesthesia Complications ◦ Failed block ◦ Back pain (most common) ◦ Spinal head ache More common in women ages 13 -40 Larger needle size increase severity Onset typically occurs first or second day postop Treatment: ◦ Bed rest ◦ Fluids ◦ Caffeine ◦ Blood patch
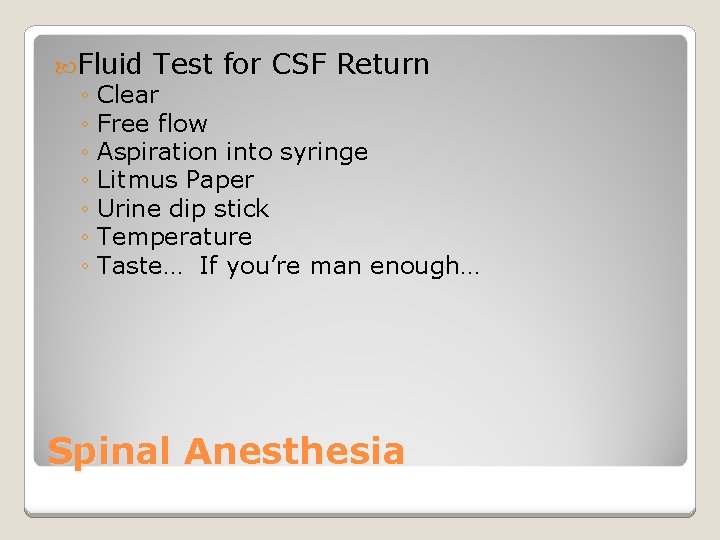
Fluid Test for CSF Return ◦ Clear ◦ Free flow ◦ Aspiration into syringe ◦ Litmus Paper ◦ Urine dip stick ◦ Temperature ◦ Taste… If you’re man enough… Spinal Anesthesia
Blood Patch Increase pressure of CSF by placing blood in epidural space If more than one puncture site use lowest site due to rosteral spread May do no more than two 95% success with first patch Second patch may be done 24 hours after first
Spread of Local Anesthetics ◦ First to cauda equina ◦ Laterally to nerve rootlets and nerve roots ◦ May defuse to spinal cord ◦ Primary Targets: Rootlets Roots Spinal cord Spinal Anesthesia
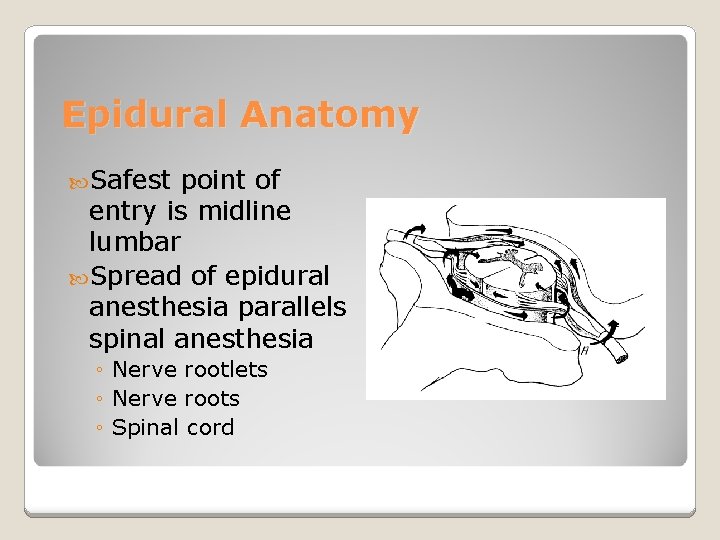
Epidural Anatomy Safest point of entry is midline lumbar Spread of epidural anesthesia parallels spinal anesthesia ◦ Nerve rootlets ◦ Nerve roots ◦ Spinal cord
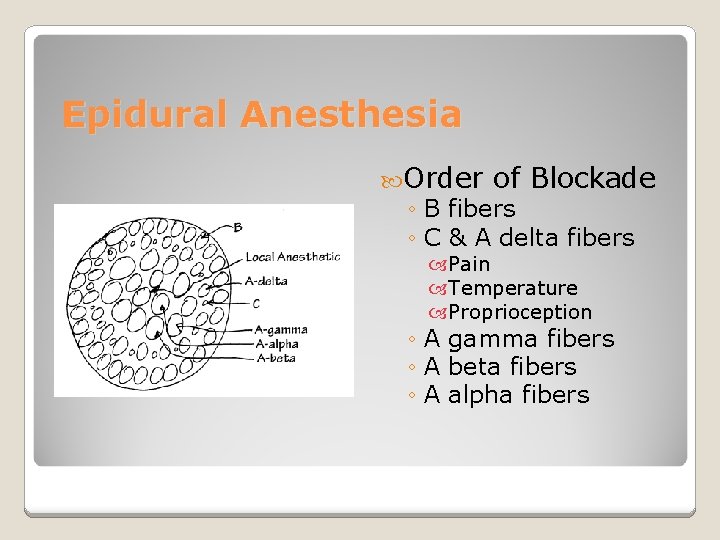
Epidural Anesthesia Order of Blockade ◦ B fibers ◦ C & A delta fibers Pain Temperature Proprioception ◦ A gamma fibers ◦ A beta fibers ◦ A alpha fibers
Epidural Anesthesia Test Dose: 1. 5% Lido with Epi 1: 200, 000 ◦ Tachycardia (increase >30 bpm over resting HR) ◦ High blood pressure ◦ Light headedness ◦ Metallic taste in mouth ◦ Ring in ears ◦ Facial numbness ◦ Note: if beta blocked will only see increase in BP not HR Bolus Dose: Preferred Local ◦ 10 milliliters for labor pain ◦ 20 -30 milliliters for C-section of Choice
Distances from Skin to Epidural Space ◦ Average adult: 4 -6 cm ◦ Obese adult: up to 8 cm ◦ Thin adult: 3 cm Assessment of Sensory Blockade ◦ Alcohol swab Most sensitive initial indicator to assess loss of temperature ◦ Pin prick Most accurate assessment of overall sensory block Epidural Anesthesia
Complications ◦ Penetration of a blood vessel ◦ Hypotension (nausea & vomiting) ◦ Head ache ◦ Back pain ◦ Intravascular catheterization ◦ Wet tap ◦ Infection Epidural Anesthesia
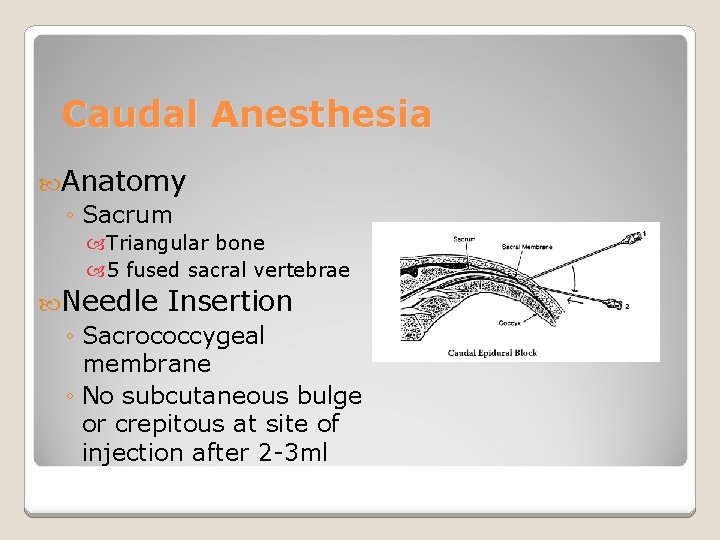
Caudal Anesthesia Anatomy ◦ Sacrum Triangular bone 5 fused sacral vertebrae Needle Insertion ◦ Sacrococcygeal membrane ◦ No subcutaneous bulge or crepitous at site of injection after 2 -3 ml
Post Operative Problems ◦ Pain at injection site is most common ◦ Slight risk of neurological complications ◦ Risk of infection Dosages ◦ S 5 -L 2: 15 -20 ml ◦ S 5 -T 10: 25 ml Caudal Anesthesia
Ankle Blockade of ◦ Tibial nerve 5 Nerves Largest Heal & medial side sole of foot ◦ Superficial perineal nerve Branch of common perineal Dorsal (top) portion of foot ◦ Saphenous nerve Branch of femoral nerve Medial side of leg, ankle, & foot ◦ Sural nerve Branch of posterior tibial nerve Posterior lateral half of calf, lateral side of foot, & 5 th toe ◦ Deep perineal nerve Continuation of common perineal nerve
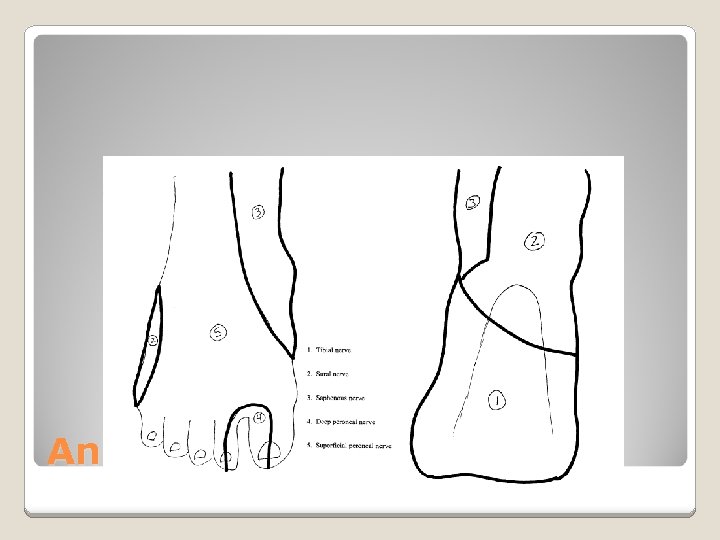
Ankle Block
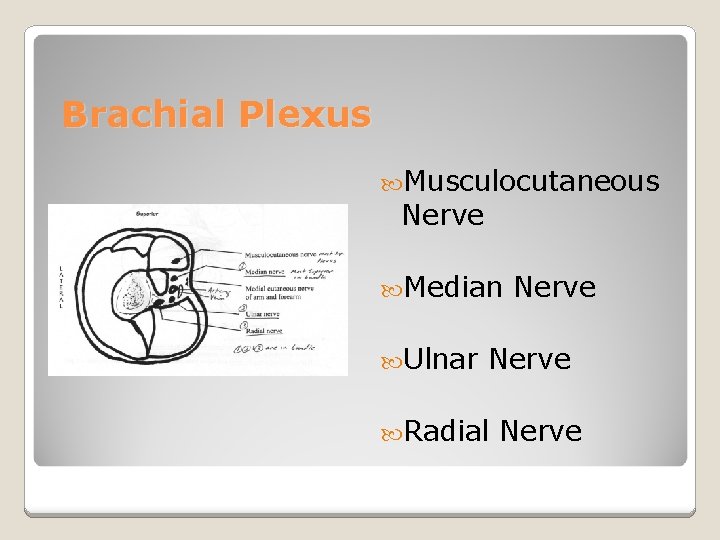
Brachial Plexus Musculocutaneous Nerve Median Ulnar Nerve Radial Nerve
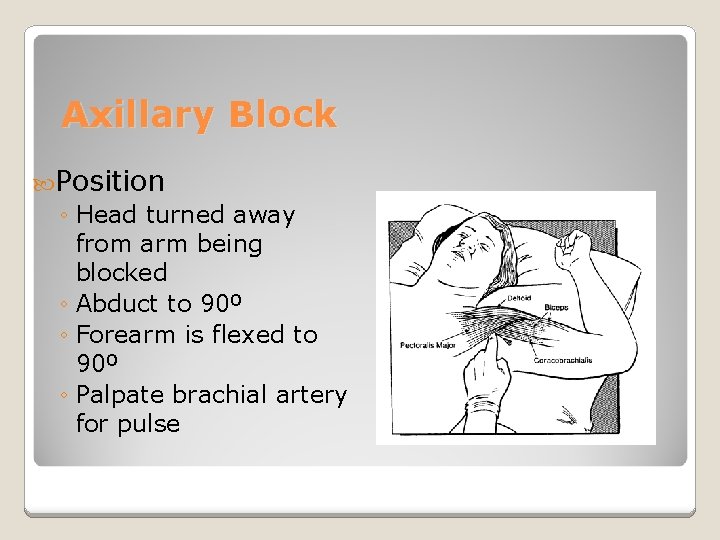
Axillary Block Position ◦ Head turned away from arm being blocked ◦ Abduct to 90º ◦ Forearm is flexed to 90º ◦ Palpate brachial artery for pulse
Axillary Block Advantages ◦ Provides anesthesia forearm & wrist ◦ Fewer complications than a supraclavicular block Limitations ◦ Not for shoulder or upper arm surgery ◦ Musculocutaneous nerve lies outside of the sheath and must be blocked separately Complications ◦ Intravascular injection ◦ Elevated bleeding time increases risk for hematoma
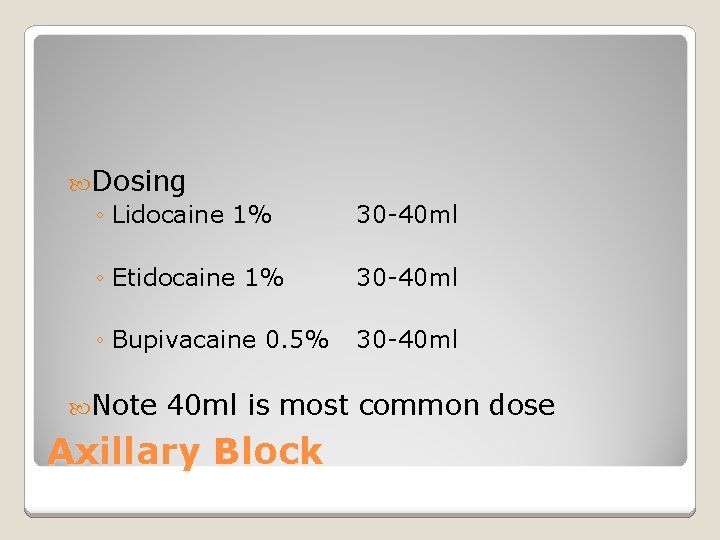
Dosing ◦ Lidocaine 1% 30 -40 ml ◦ Etidocaine 1% 30 -40 ml ◦ Bupivacaine 0. 5% 30 -40 ml Note 40 ml is most common dose Axillary Block
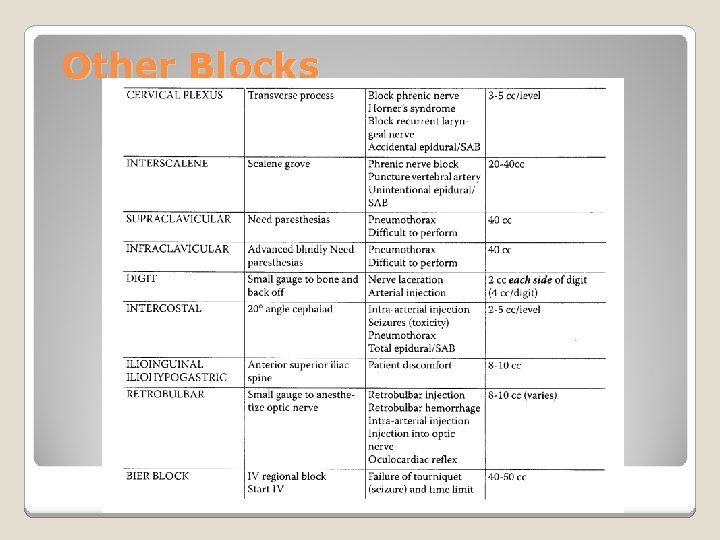
Other Blocks
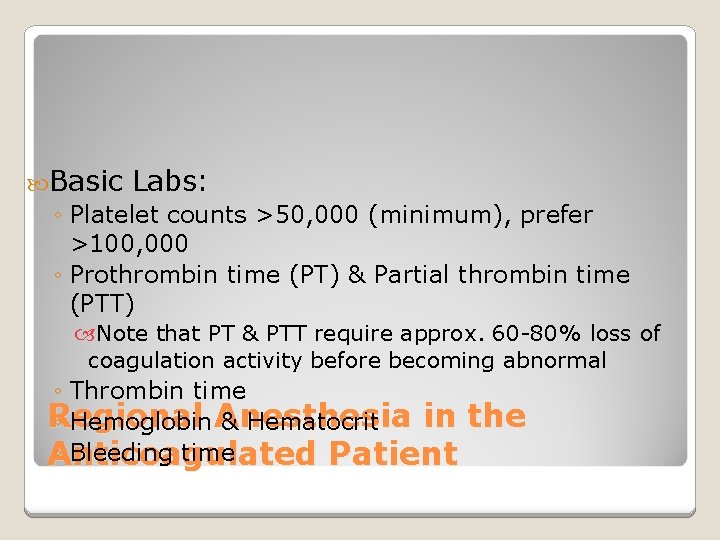
Basic Labs: ◦ Platelet counts >50, 000 (minimum), prefer >100, 000 ◦ Prothrombin time (PT) & Partial thrombin time (PTT) Note that PT & PTT require approx. 60 -80% loss of coagulation activity before becoming abnormal ◦ Thrombin time Regional in the ◦ Hemoglobin Anesthesia & Hematocrit ◦ Bleeding time Anticoagulated Patient
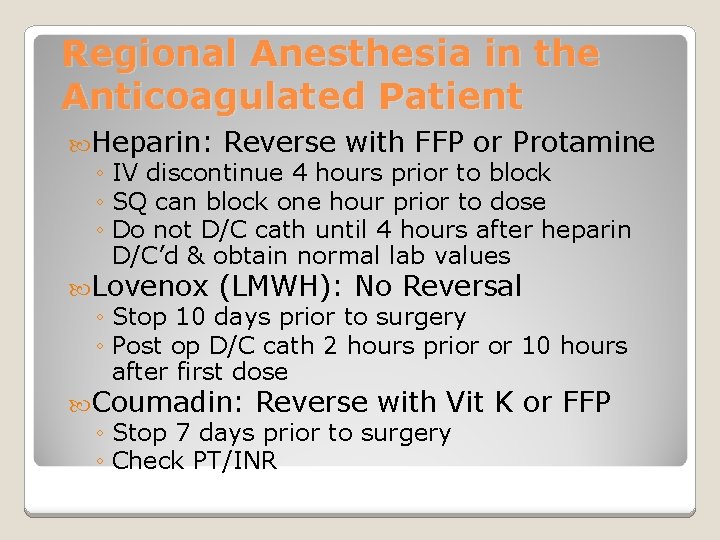
Regional Anesthesia in the Anticoagulated Patient Heparin: Reverse with FFP or Protamine ◦ IV discontinue 4 hours prior to block ◦ SQ can block one hour prior to dose ◦ Do not D/C cath until 4 hours after heparin D/C’d & obtain normal lab values Lovenox (LMWH): No Reversal ◦ Stop 10 days prior to surgery ◦ Post op D/C cath 2 hours prior or 10 hours after first dose Coumadin: Reverse with Vit K or FFP ◦ Stop 7 days prior to surgery ◦ Check PT/INR
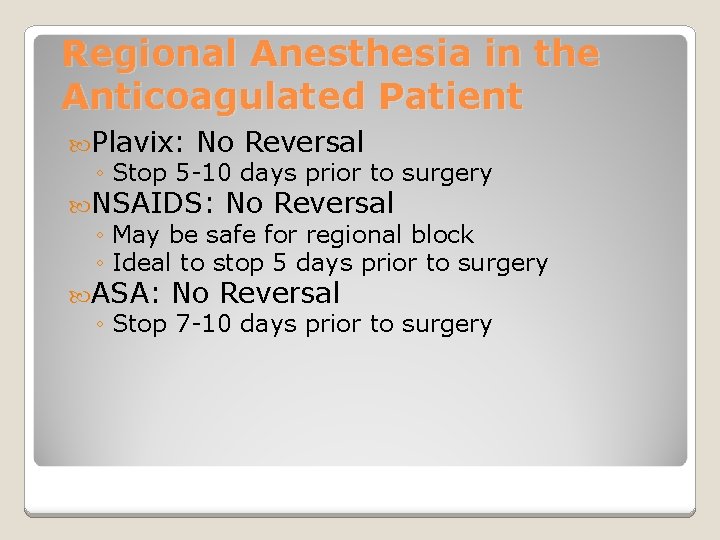
Regional Anesthesia in the Anticoagulated Patient Plavix: No Reversal ◦ Stop 5 -10 days prior to surgery NSAIDS: No Reversal ◦ May be safe for regional block ◦ Ideal to stop 5 days prior to surgery ASA: No Reversal ◦ Stop 7 -10 days prior to surgery
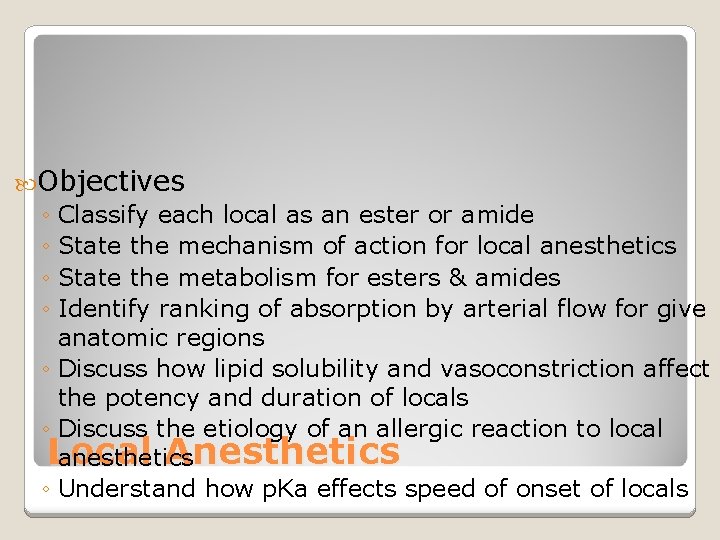
Objectives ◦ Classify each local as an ester or amide ◦ State the mechanism of action for local anesthetics ◦ State the metabolism for esters & amides ◦ Identify ranking of absorption by arterial flow for give anatomic regions ◦ Discuss how lipid solubility and vasoconstriction affect the potency and duration of locals ◦ Discuss the etiology of an allergic reaction to local Local Anesthetics anesthetics ◦ Understand how p. Ka effects speed of onset of locals
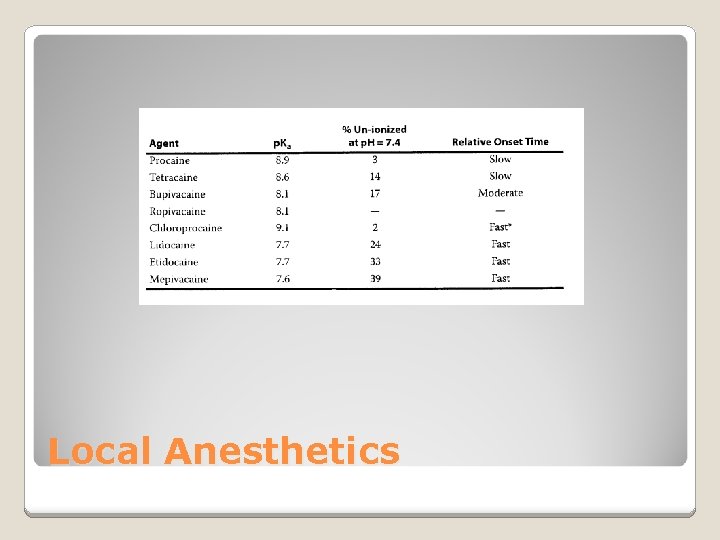
Speed of Onset ◦ Based on p. Ka Lower p. Ka equals more un-ionized at p. H 7. 4 Un-ionized drug penetrates lipid bilayer of nerve ◦ More un-ionized form of local equals faster penetration, which equals quicker onset of action Local anesthetics + Na. HCO 3 (High p. H) = more un-ionized Local Anesthetics
Local Anesthetics
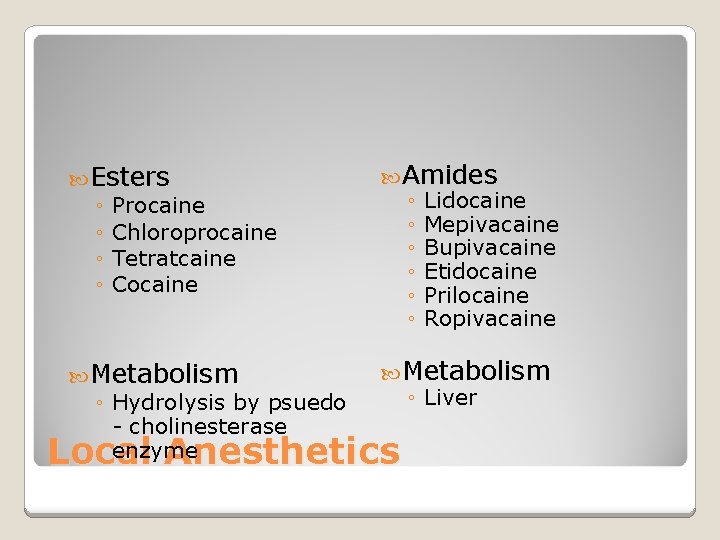
Esters ◦ Procaine ◦ Chloroprocaine ◦ Tetratcaine ◦ Cocaine Amides ◦ Lidocaine ◦ Mepivacaine ◦ Bupivacaine ◦ Etidocaine ◦ Prilocaine ◦ Ropivacaine Metabolism ◦ Hydrolysis by psuedo - cholinesterase enzyme Metabolism ◦ Liver Local Anesthetics
Toxicity & Allergies ◦ Esters: Increase risk for allergic reaction due to para-aminobenzoic acid produced through ester-hydralysis ◦ Amides: Greater risk of plasma toxicity due to slower metabolism in liver Local Anesthetics
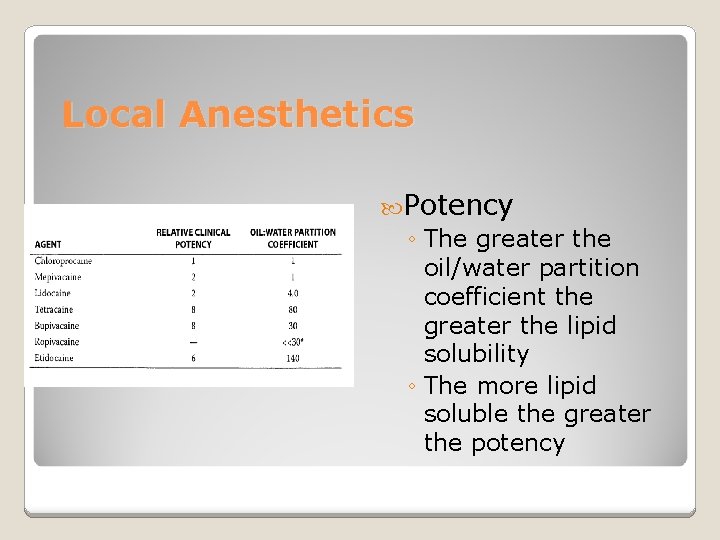
Local Anesthetics Potency ◦ The greater the oil/water partition coefficient the greater the lipid solubility ◦ The more lipid soluble the greater the potency
Duration of Action ◦ The degree of protein binding is the most important factor ◦ Lipid solubility is the second leading determining factor ◦ Greater protein bound + increase lipid solubility = longer duration of action Local Anesthetics
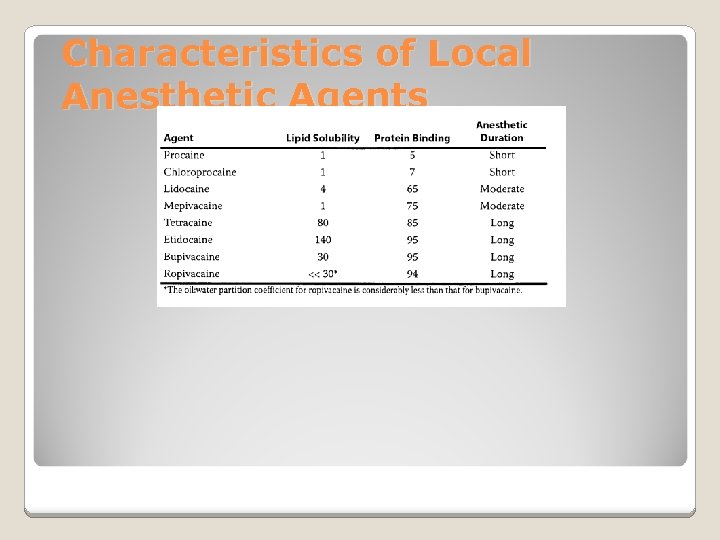
Characteristics of Local Anesthetic Agents
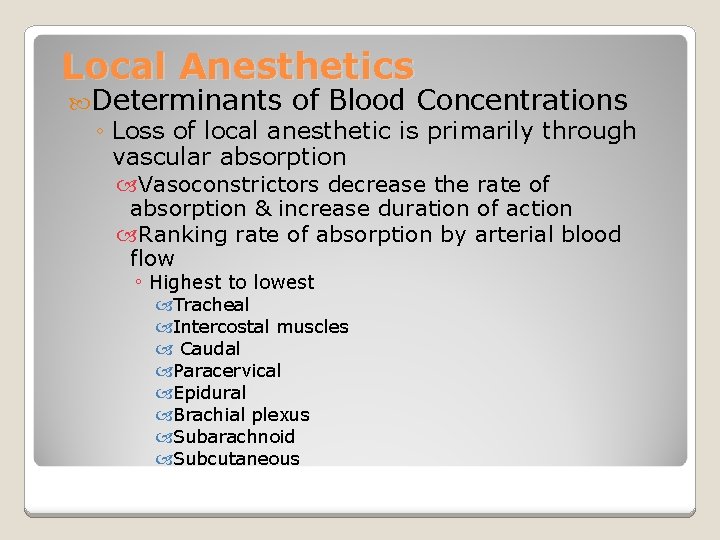
Local Anesthetics Determinants of Blood Concentrations ◦ Loss of local anesthetic is primarily through vascular absorption Vasoconstrictors decrease the rate of absorption & increase duration of action Ranking rate of absorption by arterial blood flow ◦ Highest to lowest Tracheal Intercostal muscles Caudal Paracervical Epidural Brachial plexus Subarachnoid Subcutaneous
Local Anesthetics & Baracity Hyperbaric ◦ Typically prepared by mixing local with dextrose ◦ Flow is to most dependent area due to gravity Hypobaric ◦ Prepared by mixing local with sterile water ◦ Flow is to highest part of CSF column Isobaric ◦ Neutral flow that can be manipulated by positioning ◦ Very predictable spread ◦ Increased dose has more effect on duration than dermatomal spread Note: Be cognizant of high & low regions of spinal column
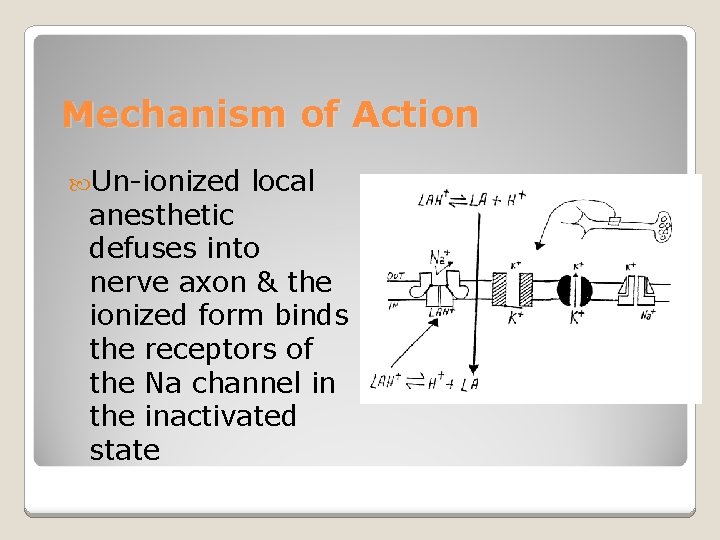
Mechanism of Action Un-ionized local anesthetic defuses into nerve axon & the ionized form binds the receptors of the Na channel in the inactivated state
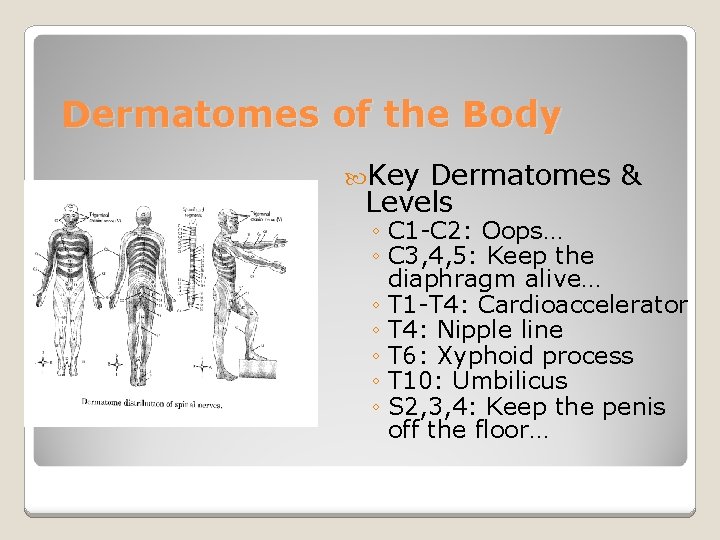
Dermatomes of the Body Key Dermatomes & Levels ◦ C 1 -C 2: Oops… ◦ C 3, 4, 5: Keep the diaphragm alive… ◦ T 1 -T 4: Cardioaccelerator ◦ T 4: Nipple line ◦ T 6: Xyphoid process ◦ T 10: Umbilicus ◦ S 2, 3, 4: Keep the penis off the floor…
Spinal Injection ◦ Sympathetic block is 2 -6 dermatomes higher than sensory block ◦ Motor block is 2 dermatomes lower than sensory block Sensory vs. Motor Blockade
Metabolism ◦ Ester locals are metabolized by plasma psuedocholinesterase ◦ Amide locals are metabolized by the liver Toxicity ◦ Determined by blood concentration of local anesthetics Metabolism & Toxicity
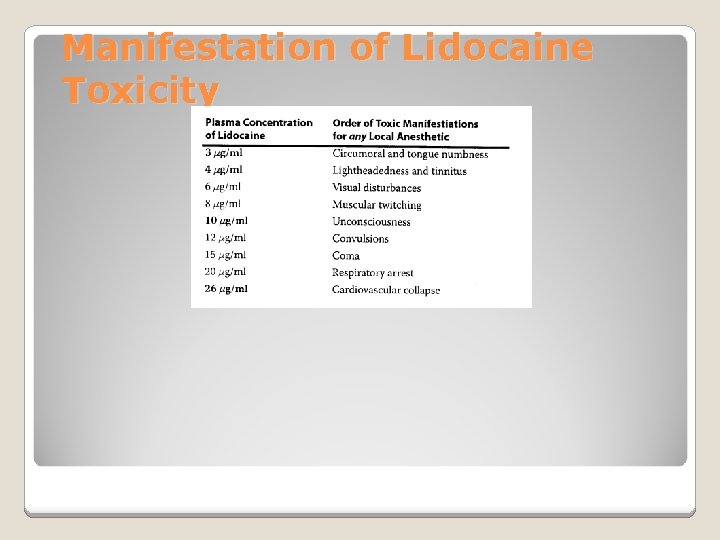
Manifestation of Lidocaine Toxicity
- Slides: 54