Regional Citrate Anticoagulation RCA in CRRT Dr Anne


- Slides: 83
Regional Citrate Anticoagulation (RCA) in CRRT Dr Anne Leung QEH ICU 2010
Overview Ø Mechanism of action and metabolism of citrate Ø Formulation of citrate Ø Advantage and disadvantage of using citrate anticoagulant Ø RCA CRRT circuit options –Gambro vs Fresenius Ø Monitoring during citrate anticoagulation Ø QEH ICU Citrate anticoagulation regime
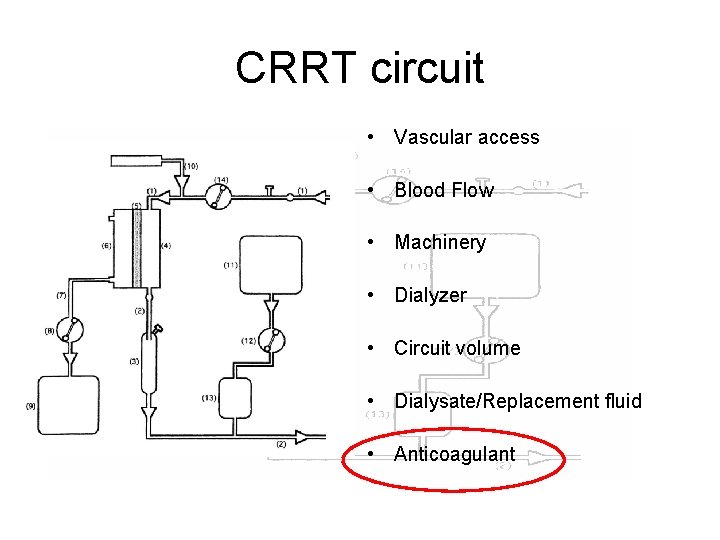
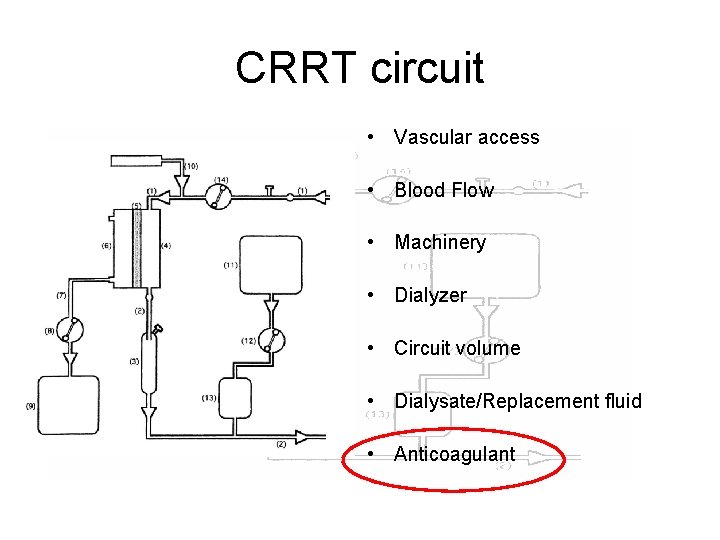
CRRT circuit • Vascular access • Blood Flow • Machinery • Dialyzer • Circuit volume • Dialysate/Replacement fluid • Anticoagulant
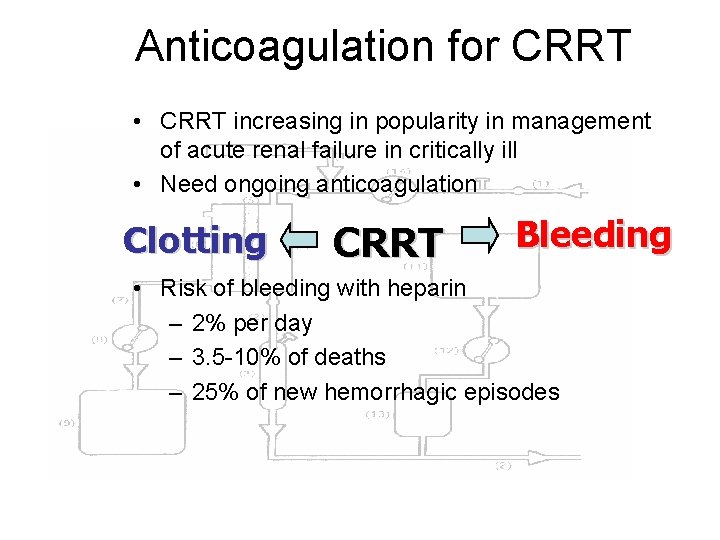
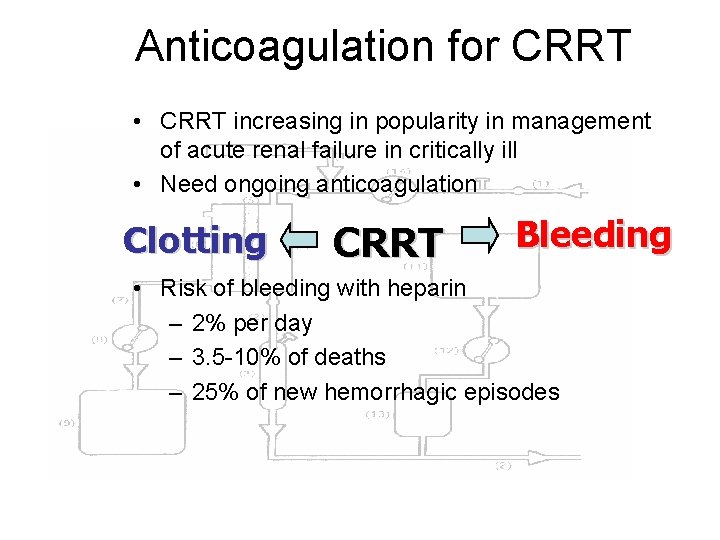
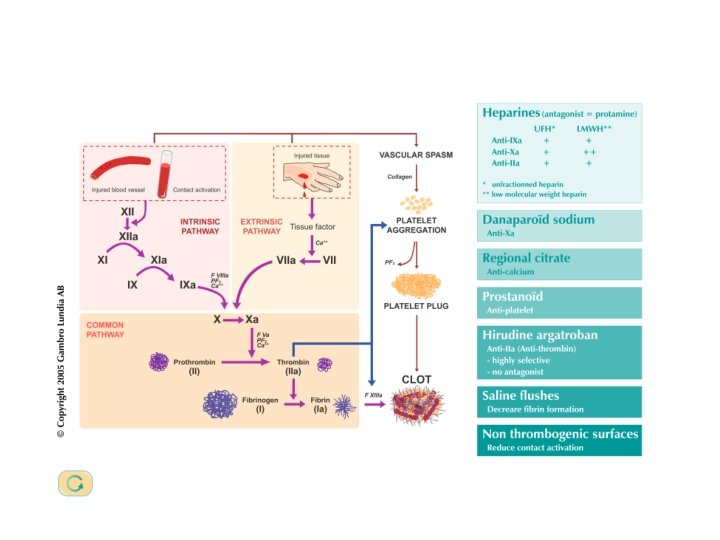
Anticoagulation for CRRT • CRRT increasing in popularity in management of acute renal failure in critically ill • Need ongoing anticoagulation Clotting CRRT Bleeding • Risk of bleeding with heparin – 2% per day – 3. 5 -10% of deaths – 25% of new hemorrhagic episodes
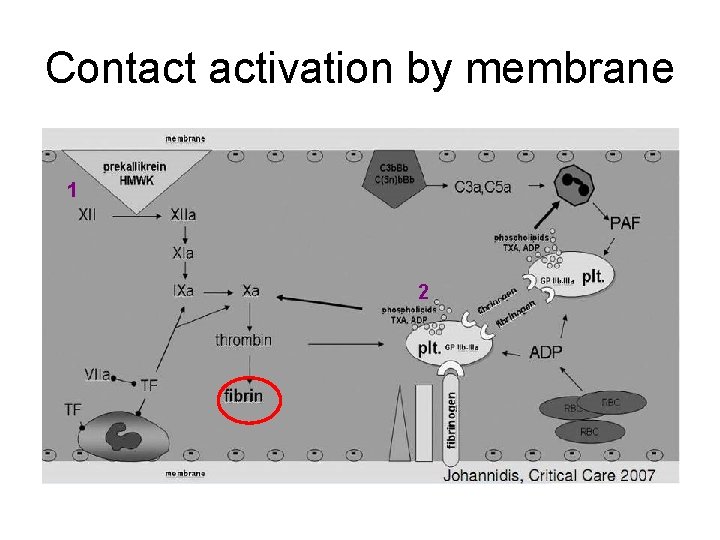
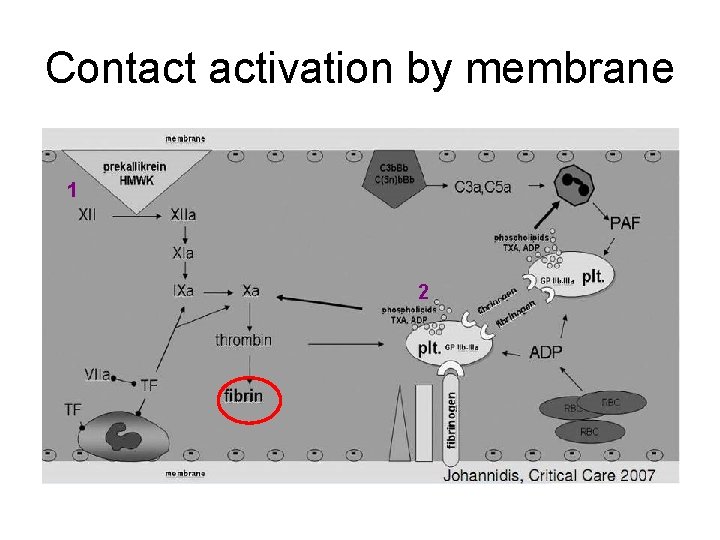
Contact activation by membrane 1 2
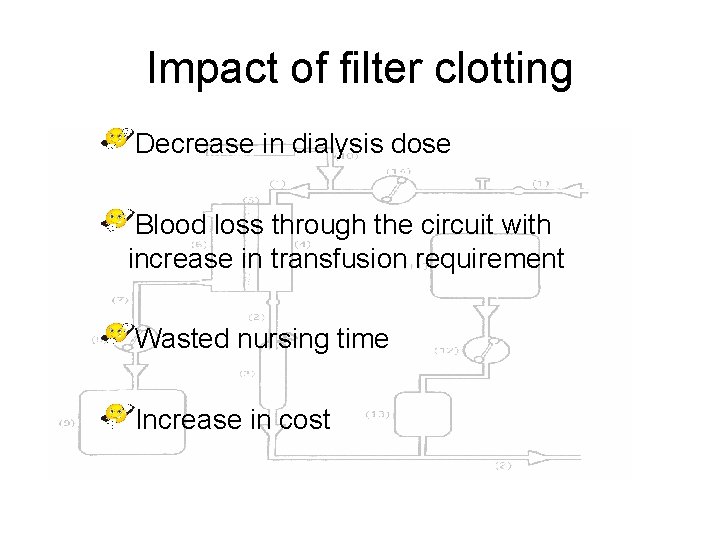
Impact of filter clotting Decrease in dialysis dose Blood loss through the circuit with increase in transfusion requirement Wasted nursing time Increase in cost
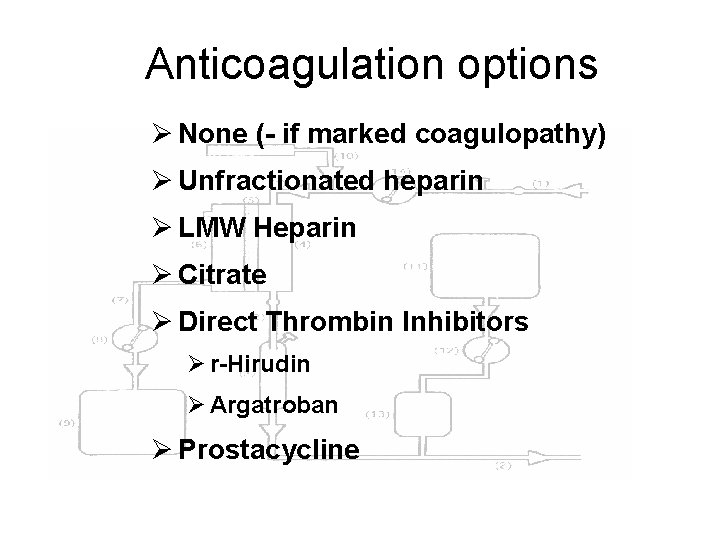
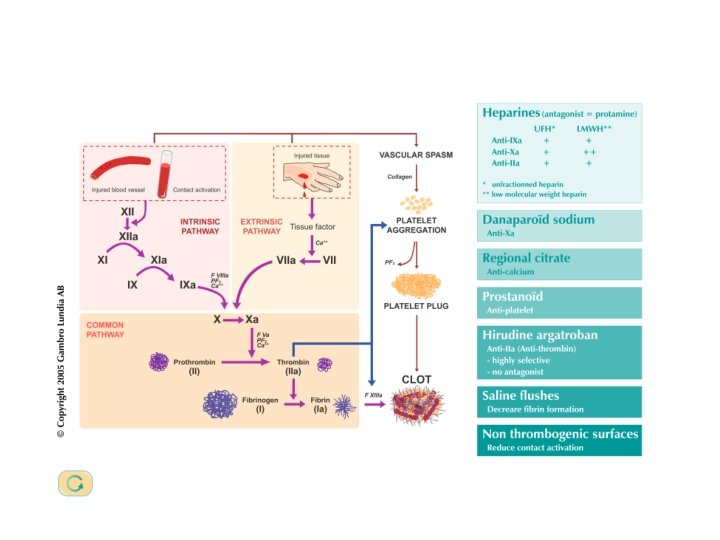
Anticoagulation options Ø None (- if marked coagulopathy) Ø Unfractionated heparin Ø LMW Heparin Ø Citrate Ø Direct Thrombin Inhibitors Ø r-Hirudin Ø Argatroban Ø Prostacycline
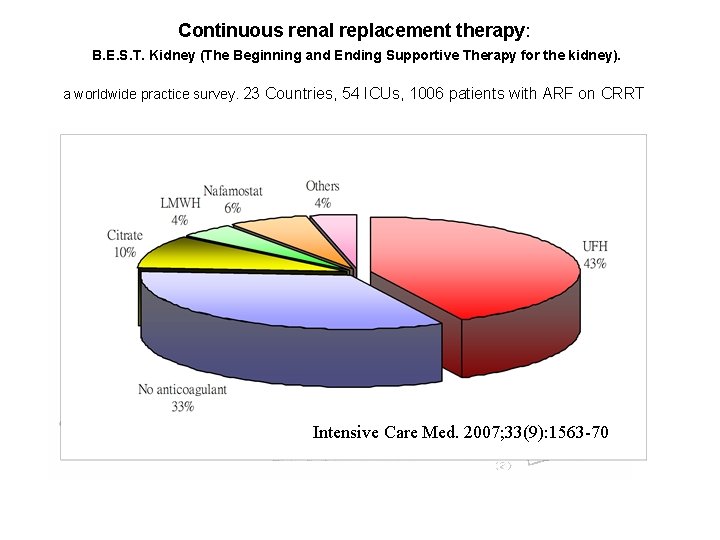
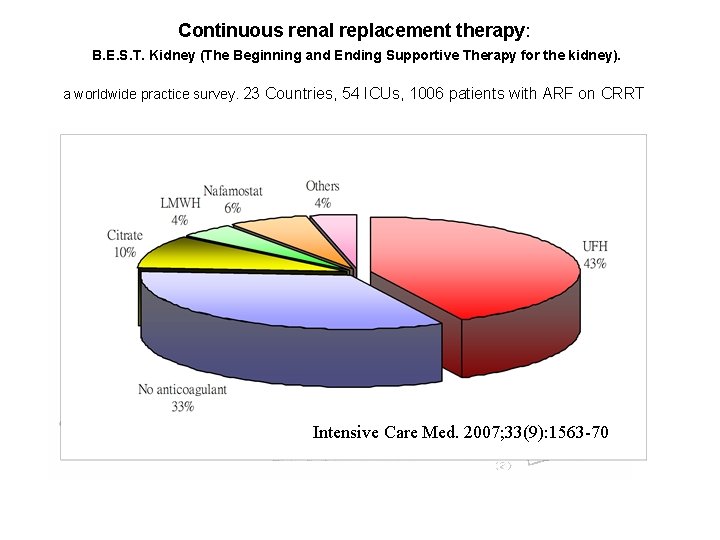
Continuous renal replacement therapy: B. E. S. T. Kidney (The Beginning and Ending Supportive Therapy for the kidney). a worldwide practice survey. 23 Countries, 54 ICUs, 1006 patients with ARF on CRRT Intensive Care Med. 2007; 33(9): 1563 -70
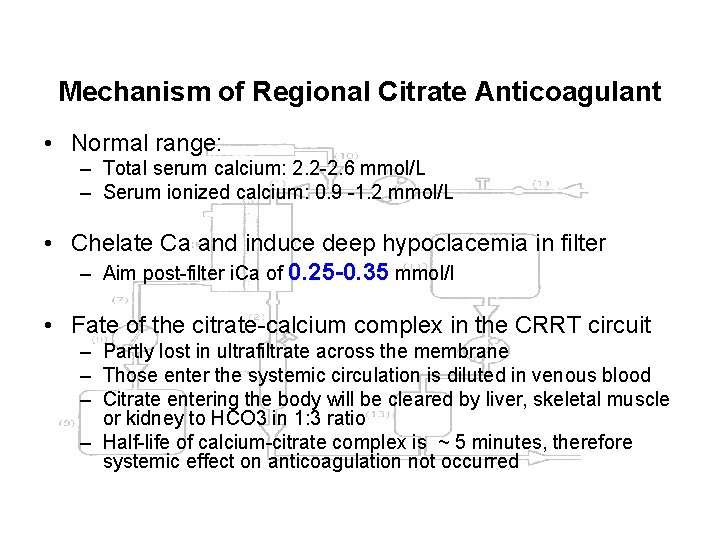
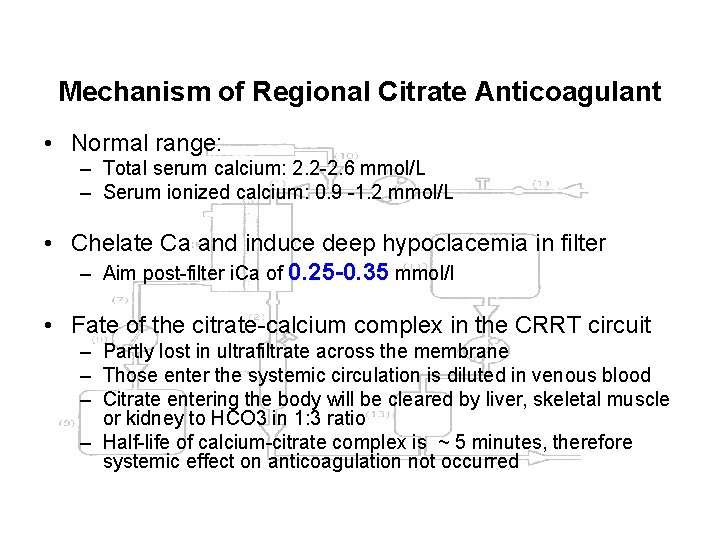
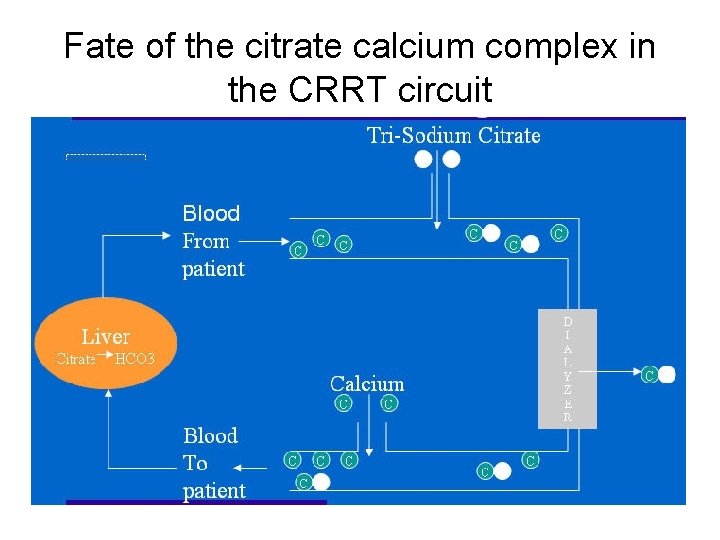
Mechanism of Regional Citrate Anticoagulant • Normal range: – Total serum calcium: 2. 2 -2. 6 mmol/L – Serum ionized calcium: 0. 9 -1. 2 mmol/L • Chelate Ca and induce deep hypoclacemia in filter – Aim post-filter i. Ca of 0. 25 -0. 35 mmol/l • Fate of the citrate-calcium complex in the CRRT circuit – Partly lost in ultrafiltrate across the membrane – Those enter the systemic circulation is diluted in venous blood – Citrate entering the body will be cleared by liver, skeletal muscle or kidney to HCO 3 in 1: 3 ratio – Half-life of calcium-citrate complex is ~ 5 minutes, therefore systemic effect on anticoagulation not occurred
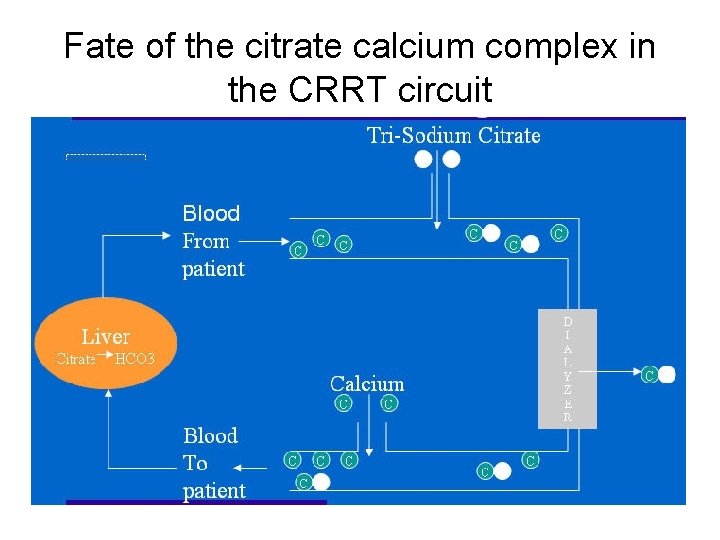
Fate of the citrate calcium complex in the CRRT circuit
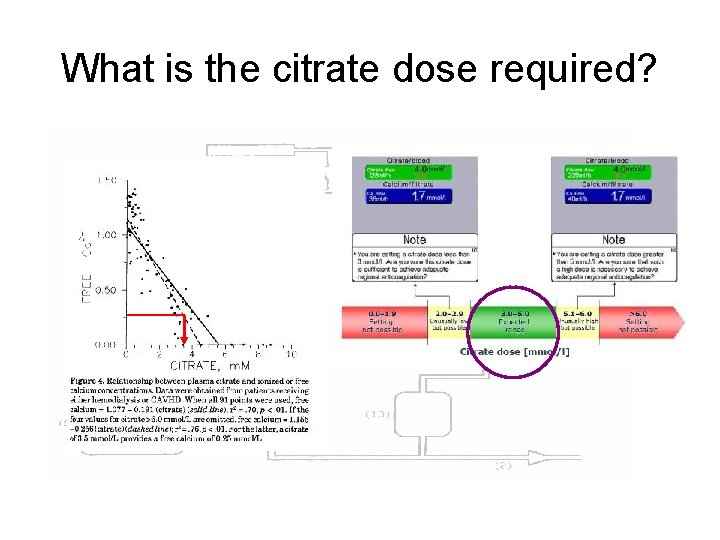
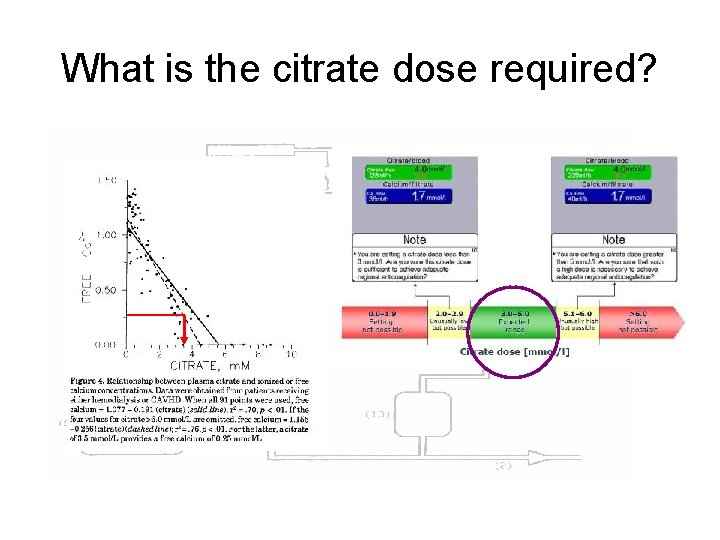
What is the citrate dose required?
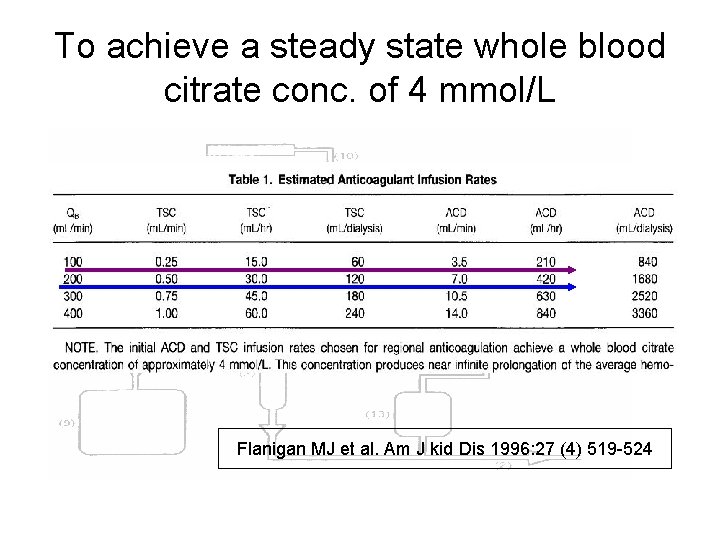
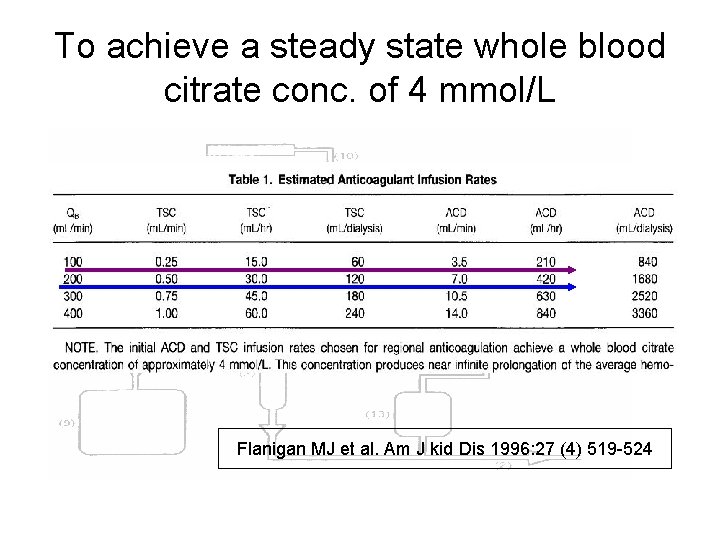
To achieve a steady state whole blood citrate conc. of 4 mmol/L Flanigan MJ et al. Am J kid Dis 1996: 27 (4) 519 -524
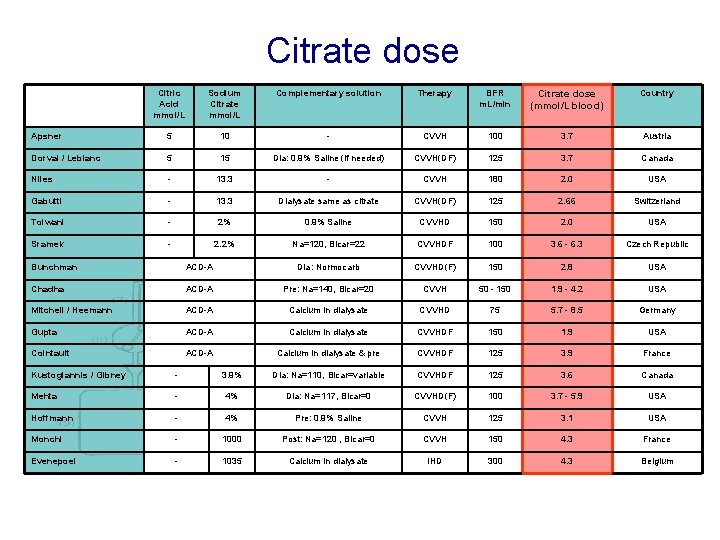
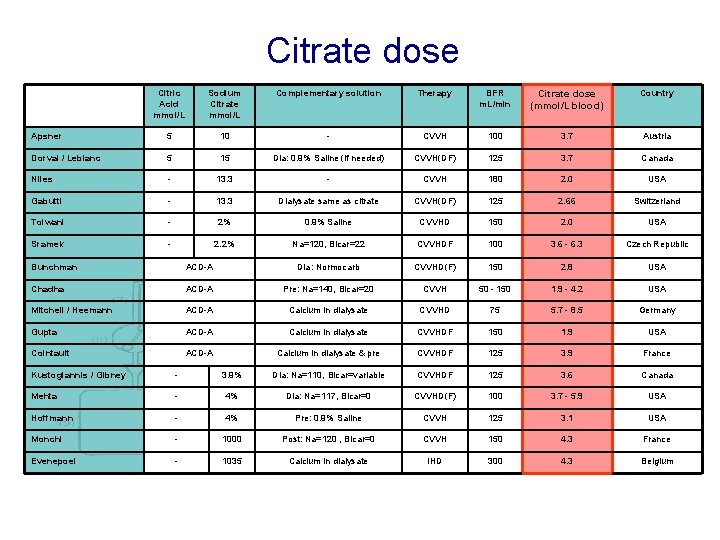
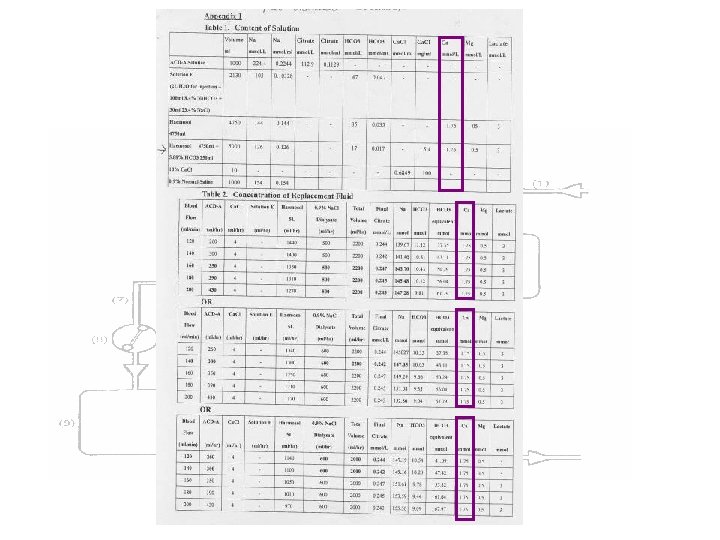
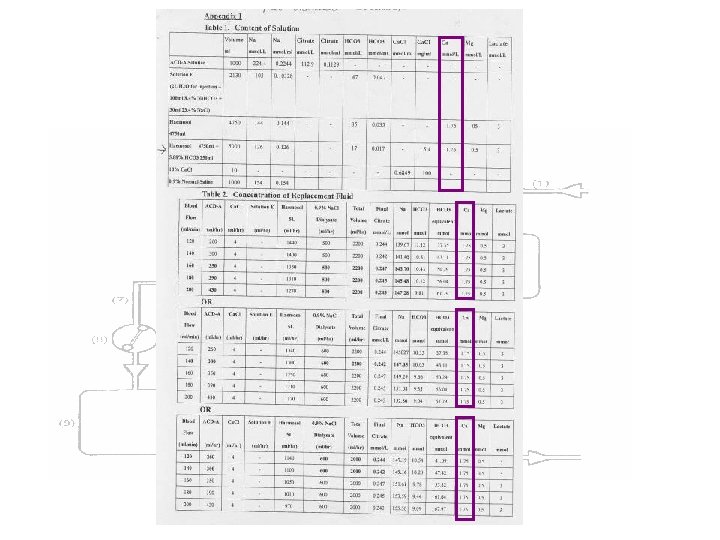
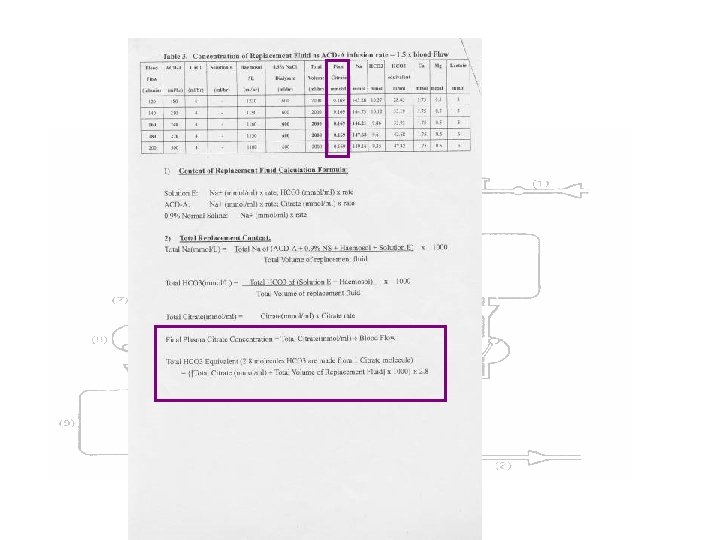
Citrate dose Citric Acid mmol/L Sodium Citrate mmol/L Complementary solution Therapy BFR m. L/min Citrate dose (mmol/L blood) Country Apsner 5 10 - CVVH 100 3. 7 Austria Dorval / Leblanc 5 15 Dia: 0. 9% Saline (if needed) CVVH(DF) 125 3. 7 Canada Niles - 13. 3 - CVVH 180 2. 0 USA Gabutti - 13. 3 Dialysate same as citrate CVVH(DF) 125 2. 66 Switzerland Tolwani - 2% 0. 9% Saline CVVHD 150 2. 0 USA Sramek - 2. 2% Na=120, Bicar=22 CVVHDF 100 3. 6 - 6. 3 Czech Republic Bunchman ACD-A Dia: Normocarb CVVHD(F) 150 2. 8 USA Chadha ACD-A Pre: Na=140, Bicar=20 CVVH 50 - 150 1. 9 - 4. 2 USA Mitchell / Heemann ACD-A Calcium in dialysate CVVHD 75 5. 7 - 8. 5 Germany Gupta ACD-A Calcium in dialysate CVVHDF 150 1. 9 USA Cointault ACD-A Calcium in dialysate & pre CVVHDF 125 3. 9 France Kustogiannis / Gibney - 3. 9% Dia: Na=110, Bicar=variable CVVHDF 125 3. 6 Canada Mehta - 4% Dia: Na=117, Bicar=0 CVVHD(F) 100 3. 7 - 5. 9 USA Hoffmann - 4% Pre: 0. 9% Saline CVVH 125 3. 1 USA Monchi - 1000 Post: Na=120 , Bicar=0 CVVH 150 4. 3 France Evenepoel - 1035 Calcium in dialysate IHD 300 4. 3 Belgium
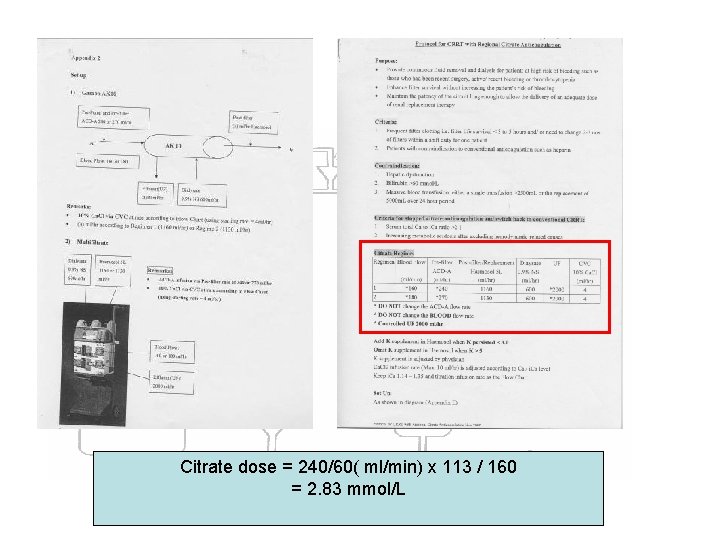
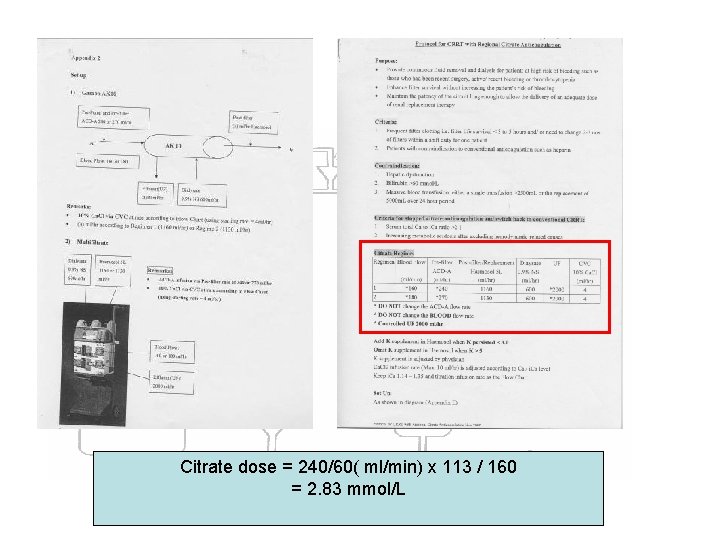
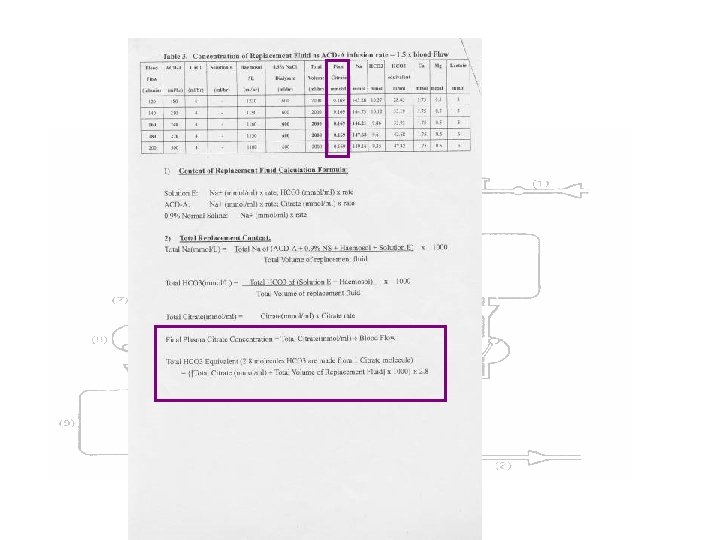
Citrate dose = 240/60( ml/min) x 113 / 160 = 2. 83 mmol/L
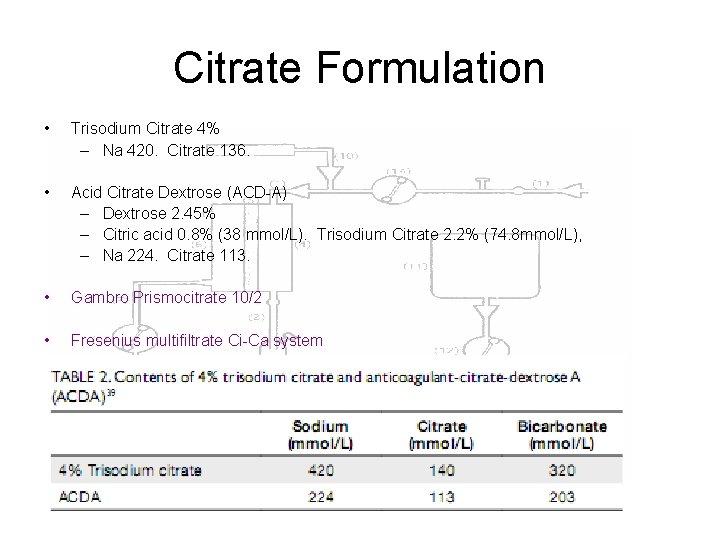
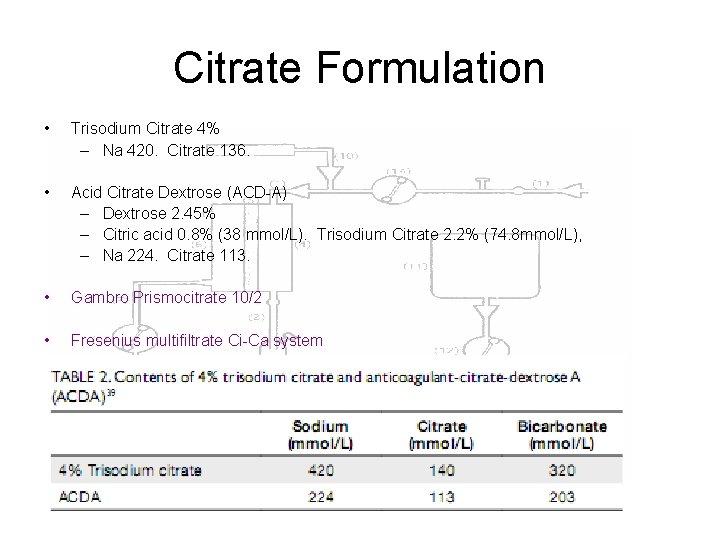
Citrate Formulation • Trisodium Citrate 4% – Na 420. Citrate 136. • Acid Citrate Dextrose (ACD-A) – Dextrose 2. 45% – Citric acid 0. 8% (38 mmol/L). Trisodium Citrate 2. 2% (74. 8 mmol/L), – Na 224. Citrate 113. • Gambro Prismocitrate 10/2 • Fresenius multifiltrate Ci-Ca system
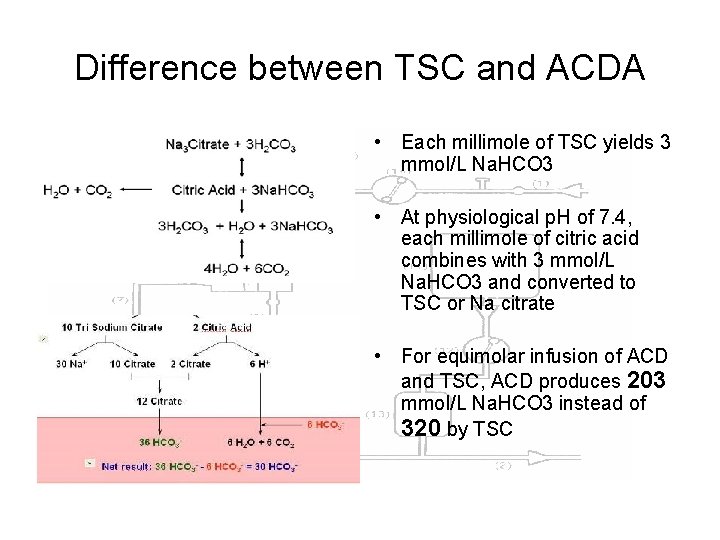
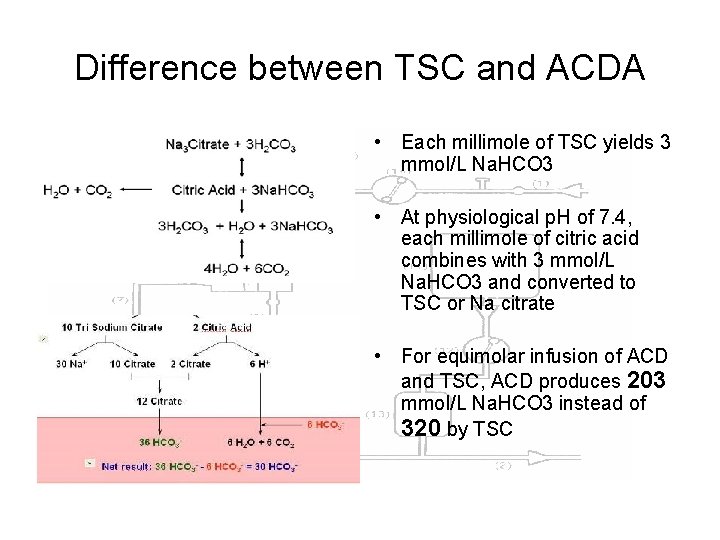
Difference between TSC and ACDA • Each millimole of TSC yields 3 mmol/L Na. HCO 3 • At physiological p. H of 7. 4, each millimole of citric acid combines with 3 mmol/L Na. HCO 3 and converted to TSC or Na citrate • For equimolar infusion of ACD and TSC, ACD produces 203 mmol/L Na. HCO 3 instead of 320 by TSC
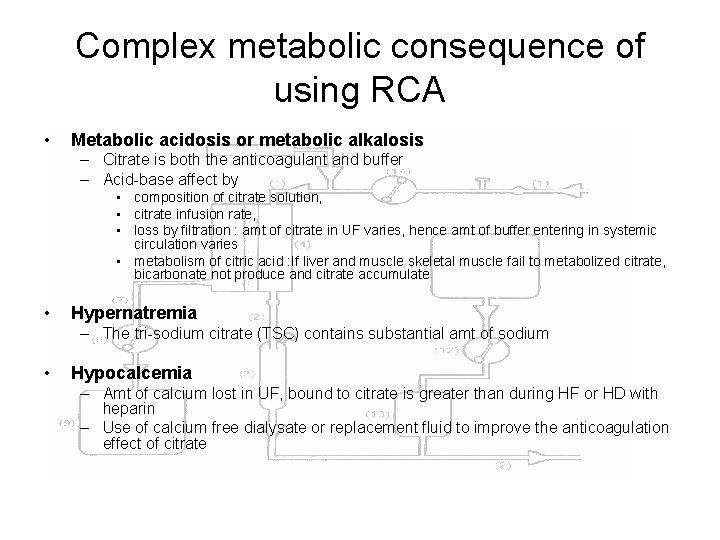
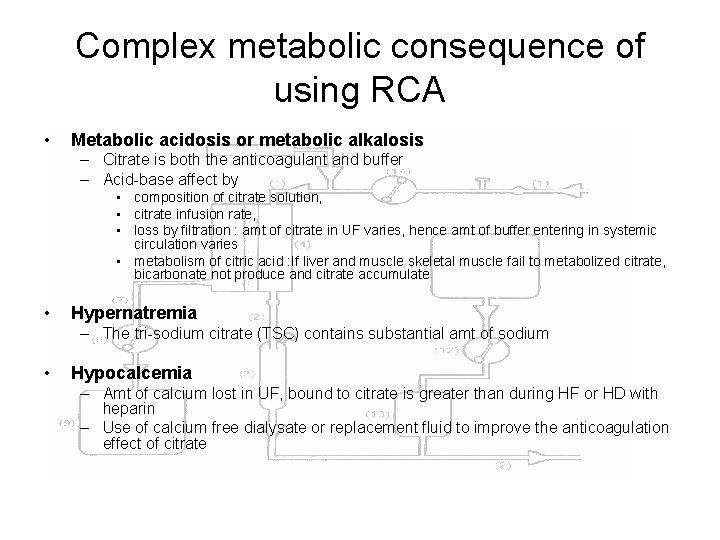
Complex metabolic consequence of using RCA • Metabolic acidosis or metabolic alkalosis – Citrate is both the anticoagulant and buffer – Acid-base affect by • composition of citrate solution, • citrate infusion rate, • loss by filtration : amt of citrate in UF varies, hence amt of buffer entering in systemic circulation varies • metabolism of citric acid : If liver and muscle skeletal muscle fail to metabolized citrate, bicarbonate not produce and citrate accumulate • Hypernatremia – The tri-sodium citrate (TSC) contains substantial amt of sodium • Hypocalcemia – Amt of calcium lost in UF, bound to citrate is greater than during HF or HD with heparin – Use of calcium free dialysate or replacement fluid to improve the anticoagulation effect of citrate
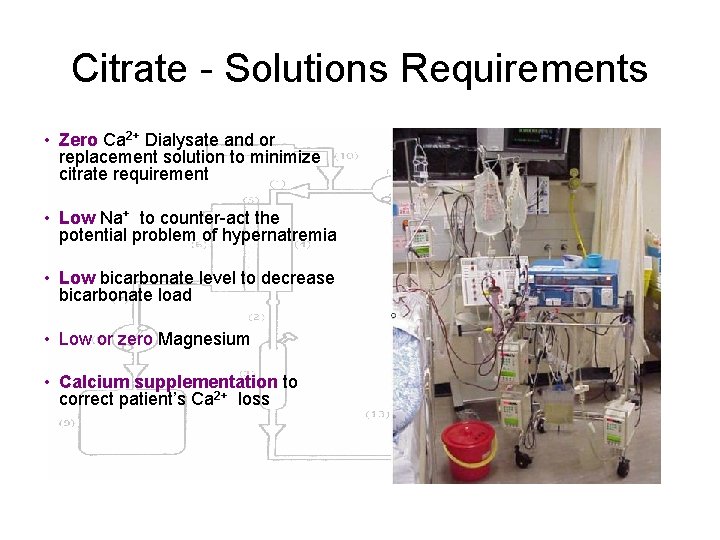
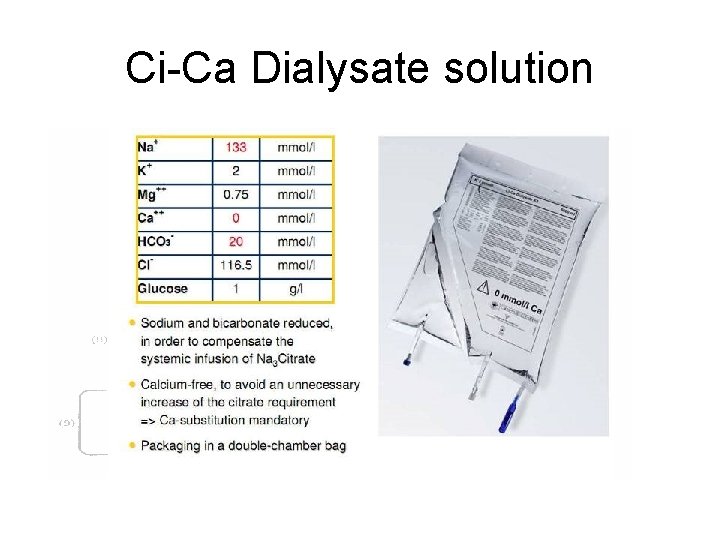
Citrate - Solutions Requirements • Zero Ca 2+ Dialysate and or replacement solution to minimize citrate requirement • Low Na+ to counter-act the potential problem of hypernatremia • Low bicarbonate level to decrease bicarbonate load • Low or zero Magnesium • Calcium supplementation to correct patient’s Ca 2+ loss
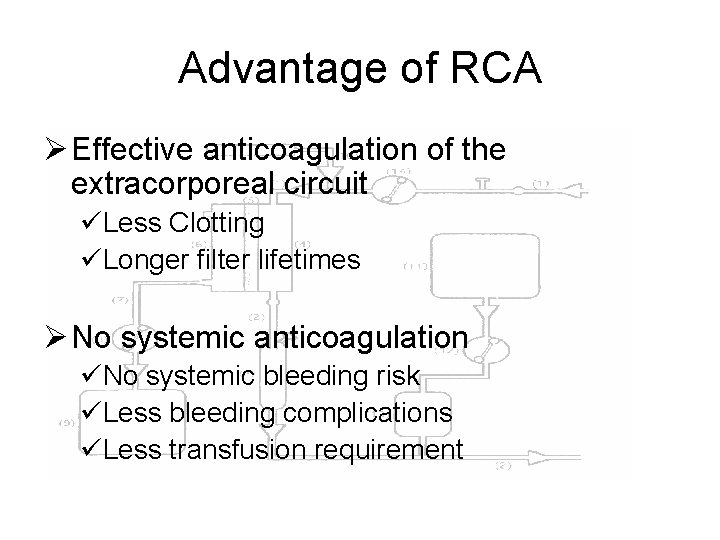
Advantage of RCA Ø Effective anticoagulation of the extracorporeal circuit üLess Clotting üLonger filter lifetimes Ø No systemic anticoagulation üNo systemic bleeding risk üLess bleeding complications üLess transfusion requirement
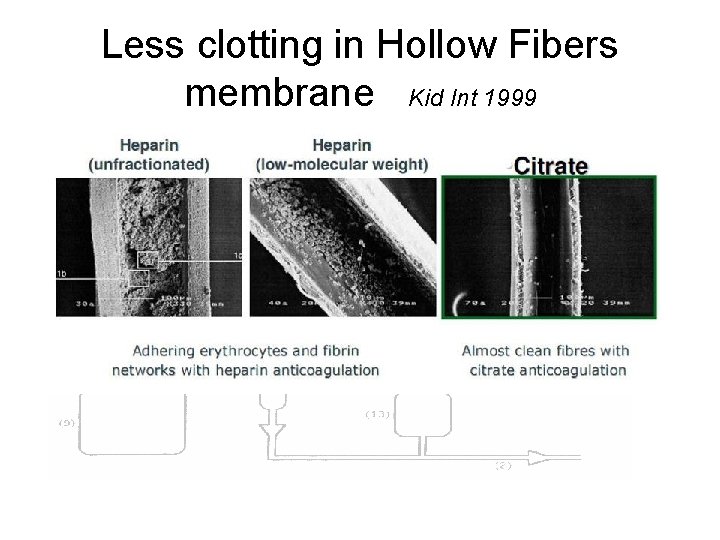
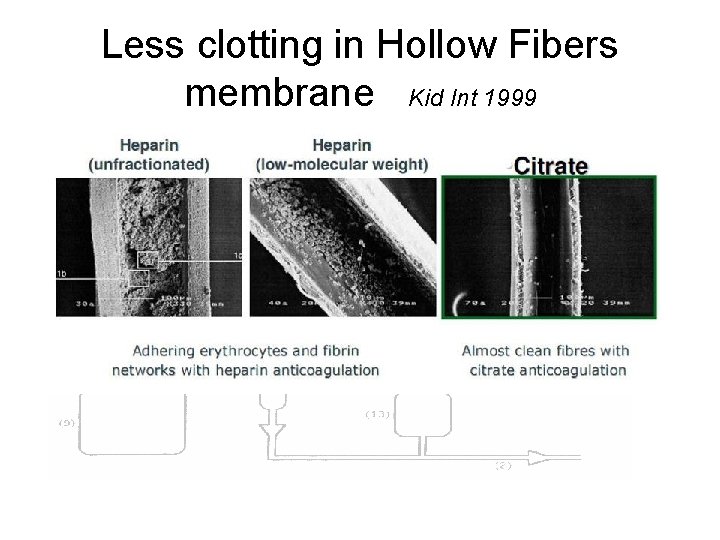
Less clotting in Hollow Fibers membrane Kid Int 1999
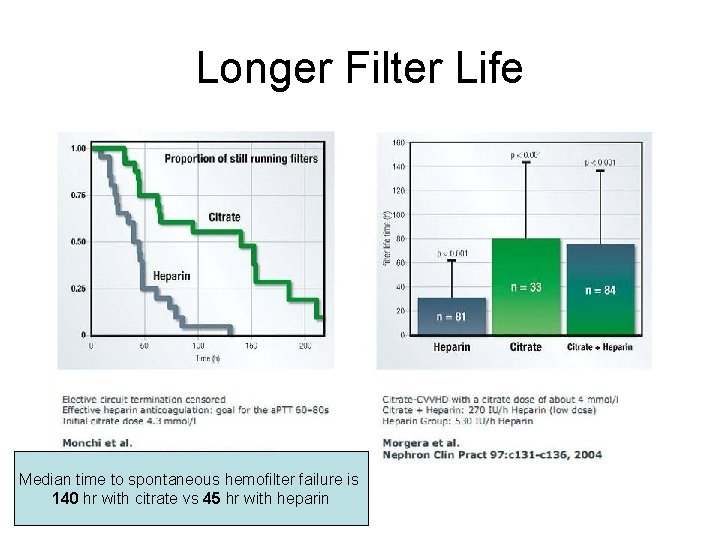
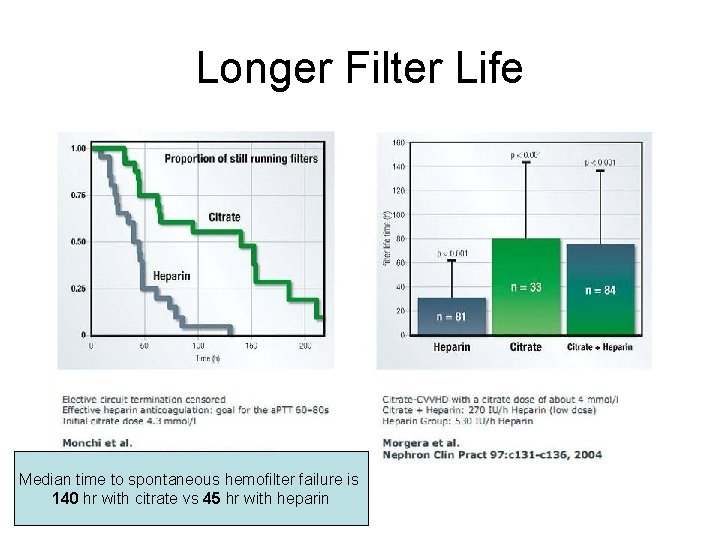
Longer Filter Life Median time to spontaneous hemofilter failure is 140 hr with citrate vs 45 hr with heparin

Less Bleeding Episode 9 put of 12 4 out of 12
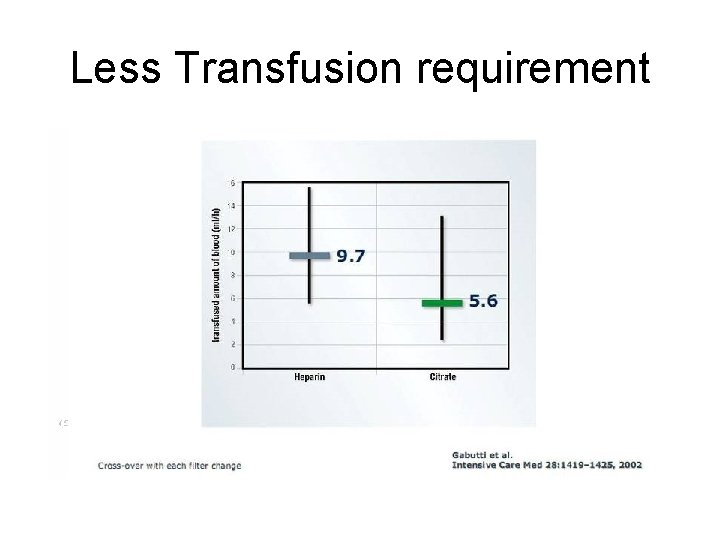
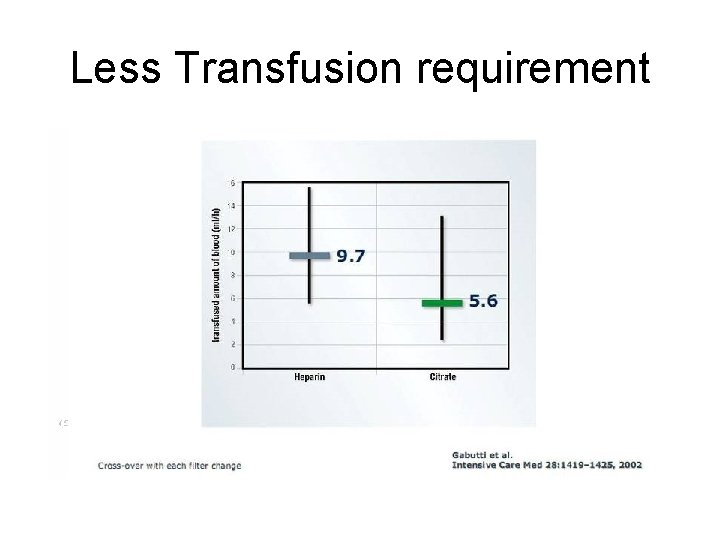
Less Transfusion requirement
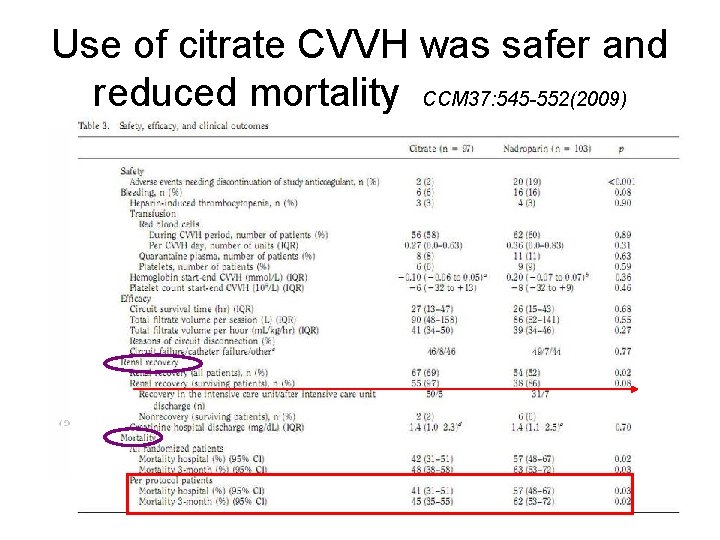
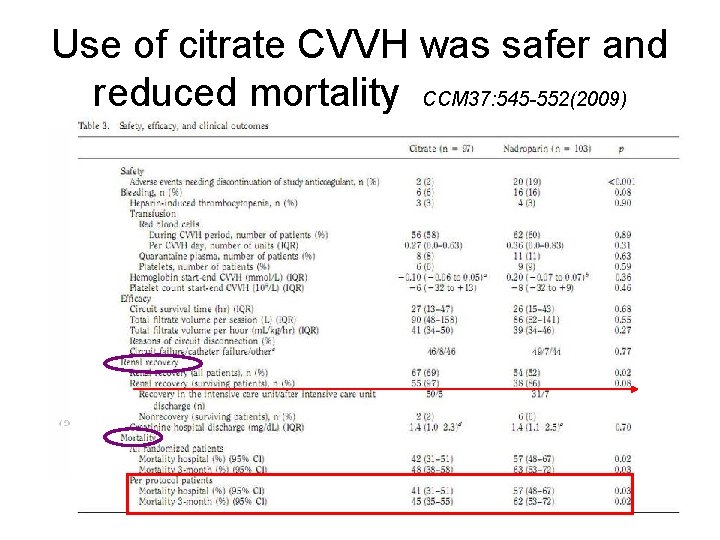
Use of citrate CVVH was safer and reduced mortality CCM 37: 545 -552(2009)
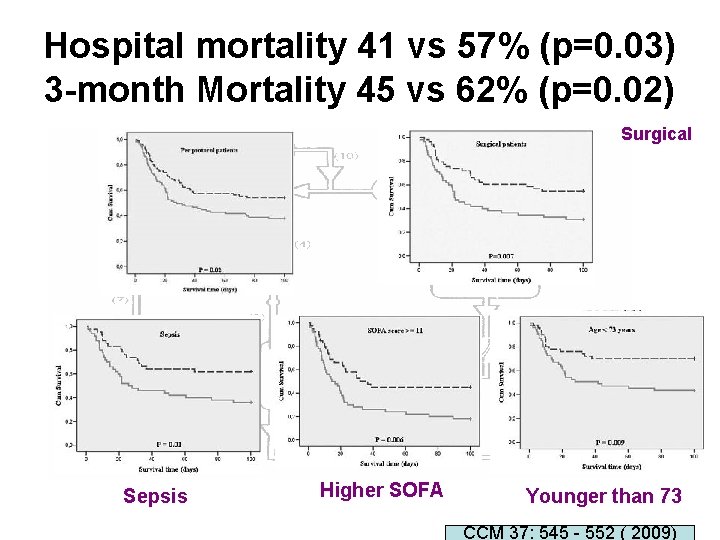
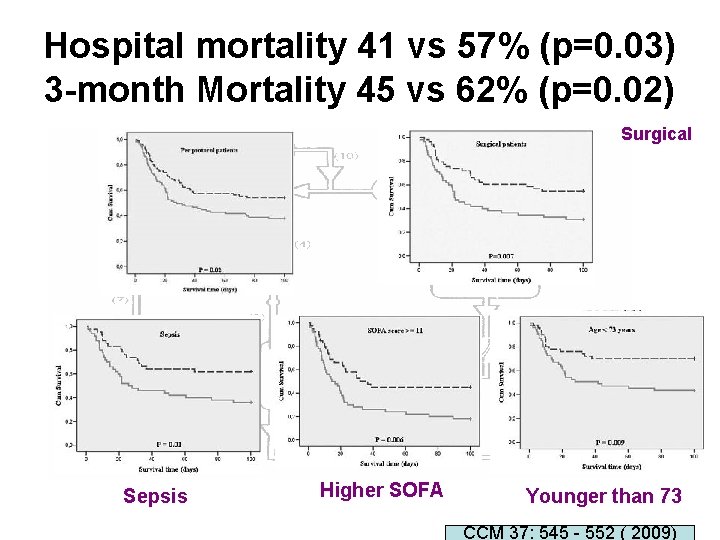
Hospital mortality 41 vs 57% (p=0. 03) 3 -month Mortality 45 vs 62% (p=0. 02) Surgical Sepsis Higher SOFA Younger than 73 CCM 37: 545 - 552 ( 2009)
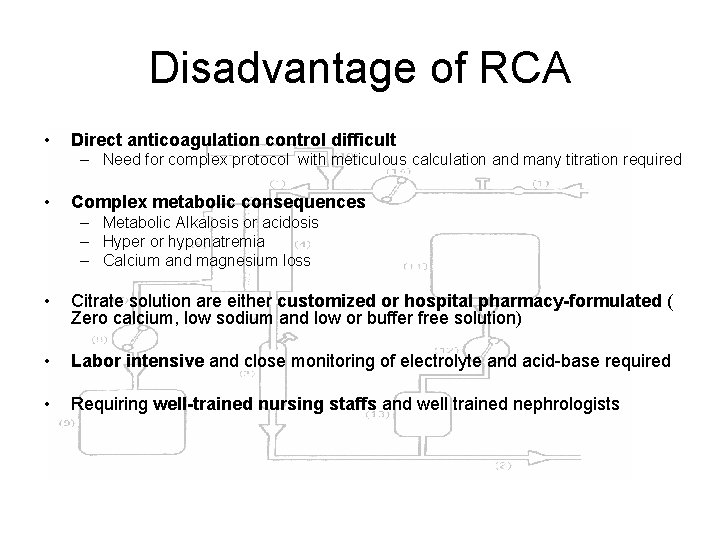
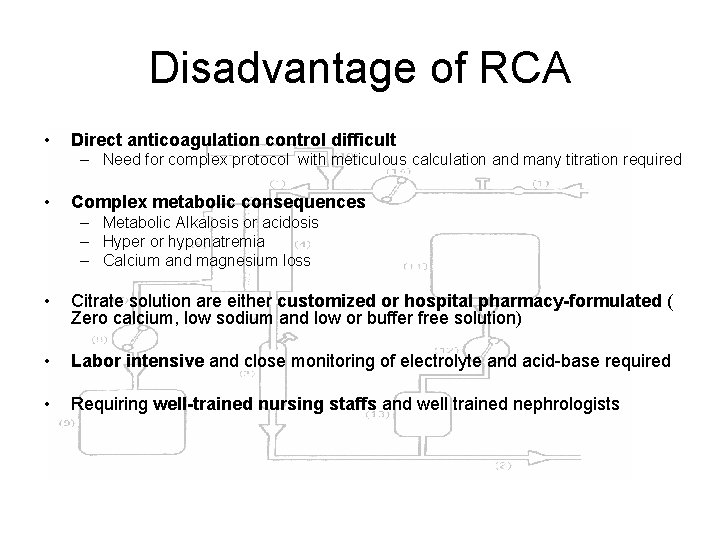
Disadvantage of RCA • Direct anticoagulation control difficult – Need for complex protocol with meticulous calculation and many titration required • Complex metabolic consequences – Metabolic Alkalosis or acidosis – Hyper or hyponatremia – Calcium and magnesium loss • Citrate solution are either customized or hospital pharmacy-formulated ( Zero calcium, low sodium and low or buffer free solution) • Labor intensive and close monitoring of electrolyte and acid-base required • Requiring well-trained nursing staffs and well trained nephrologists
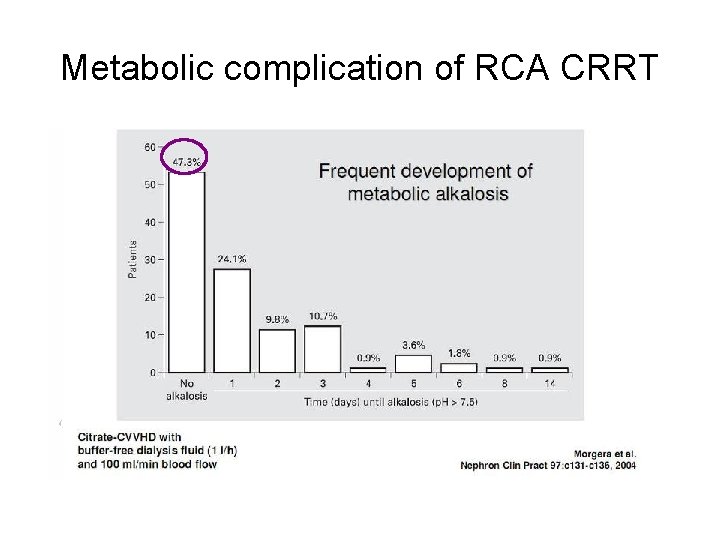
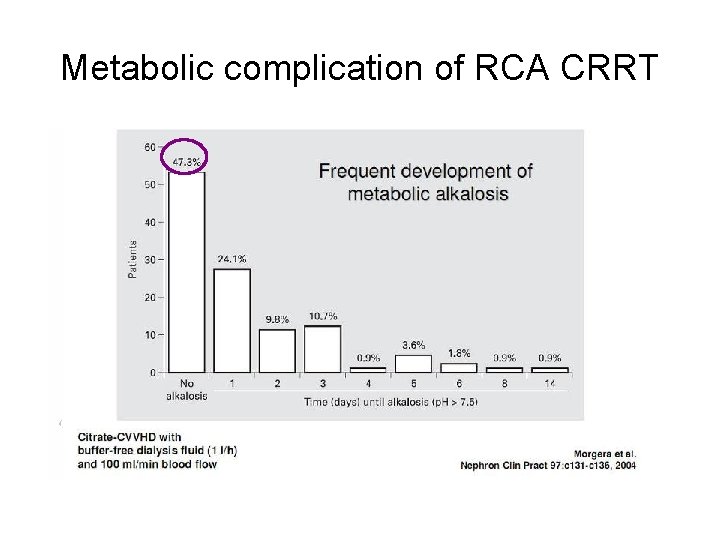
Metabolic complication of RCA CRRT
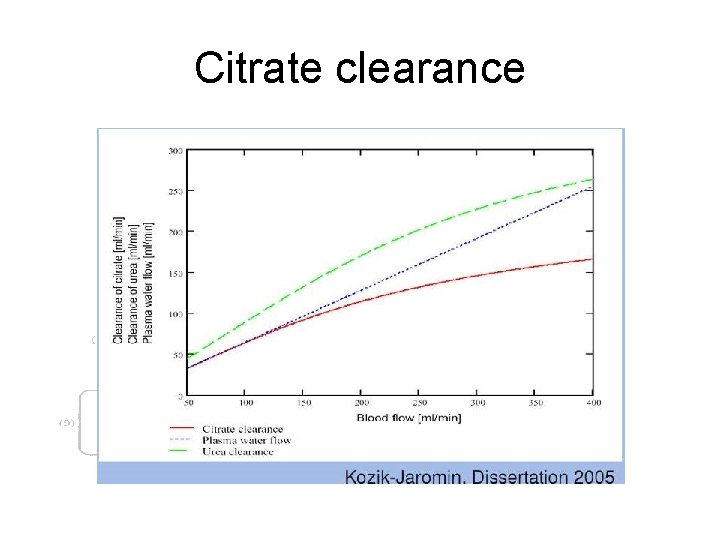
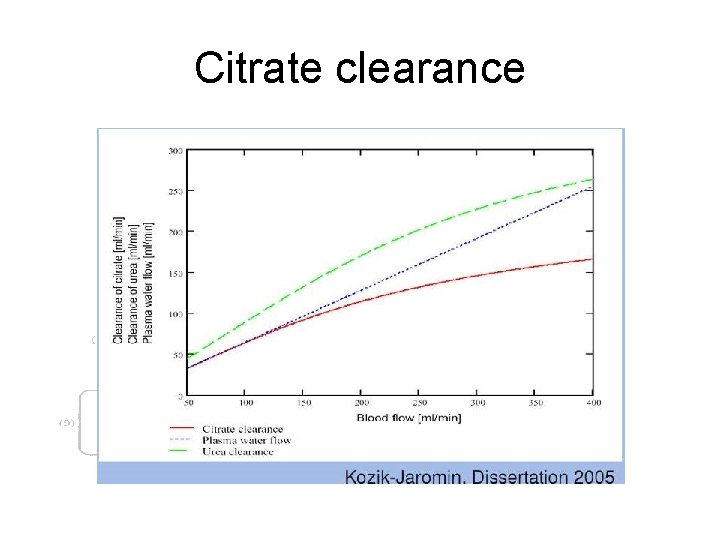
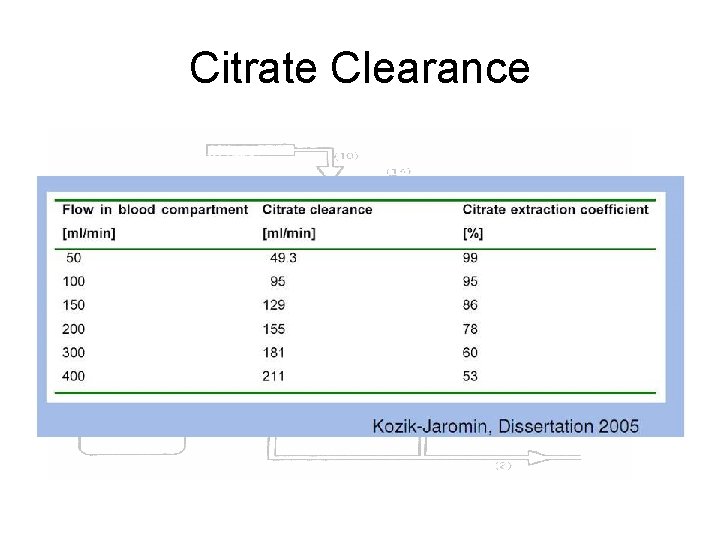
Citrate clearance
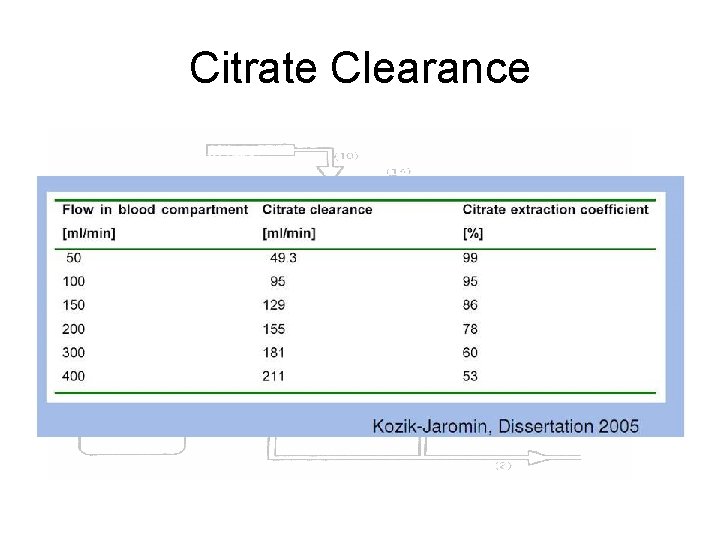
Citrate Clearance
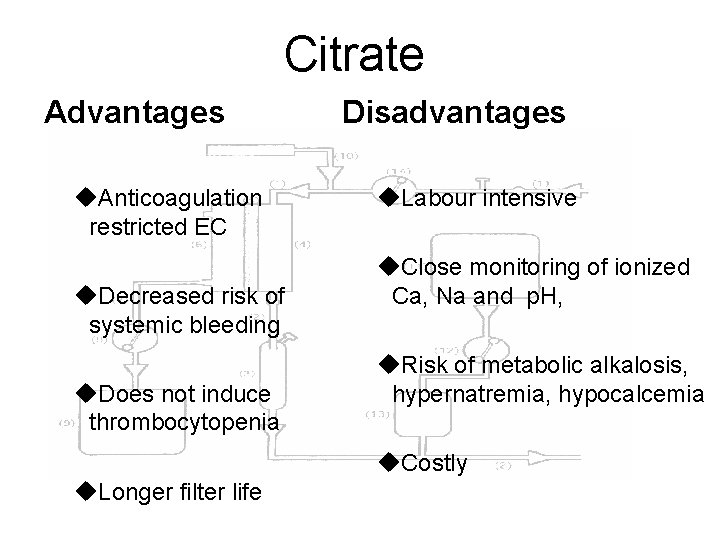
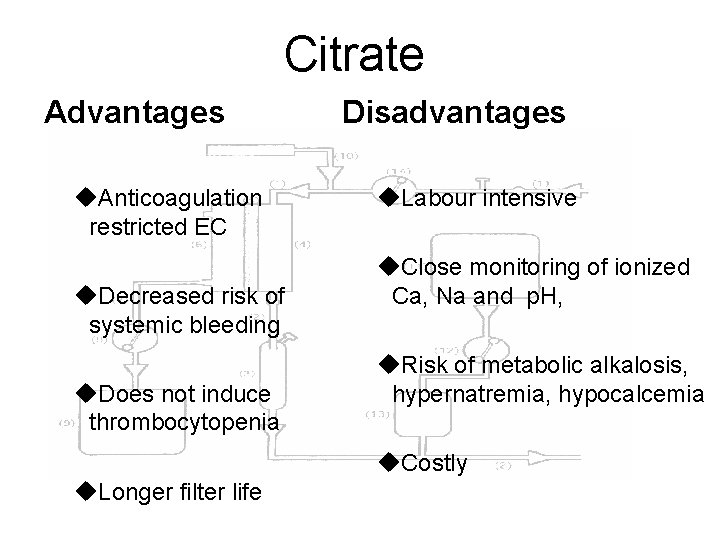
Citrate Advantages u. Anticoagulation restricted EC u. Decreased risk of systemic bleeding u. Does not induce thrombocytopenia Disadvantages u. Labour intensive u. Close monitoring of ionized Ca, Na and p. H, u. Risk of metabolic alkalosis, hypernatremia, hypocalcemia u. Costly u. Longer filter life
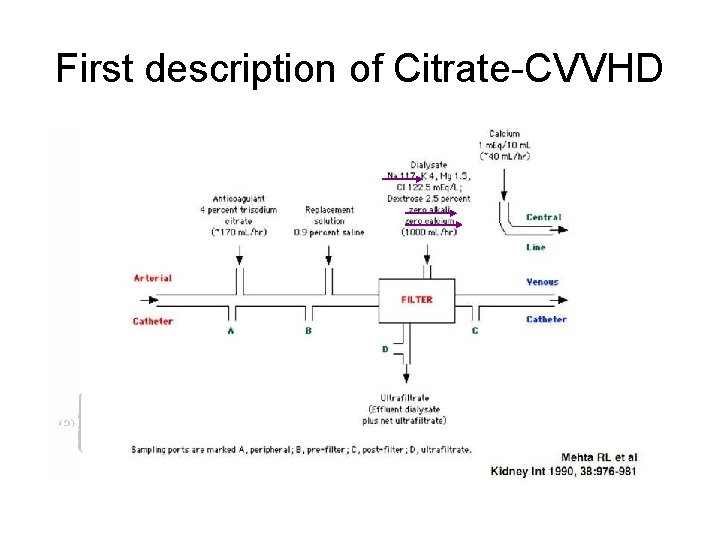
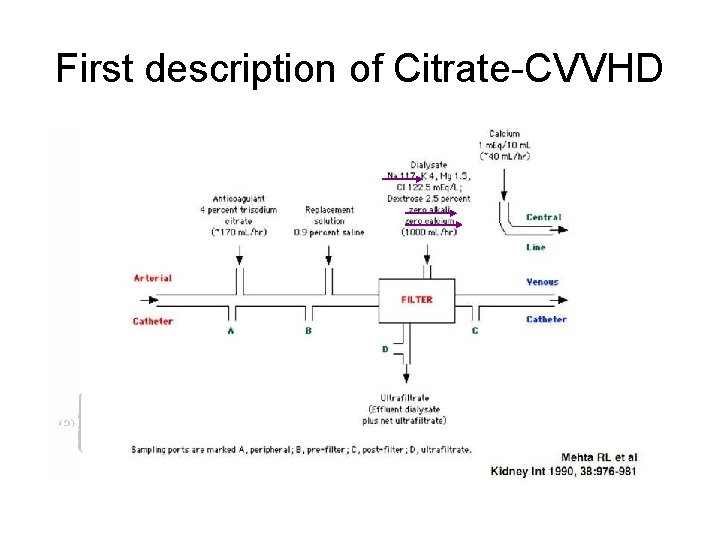
First description of Citrate-CVVHD
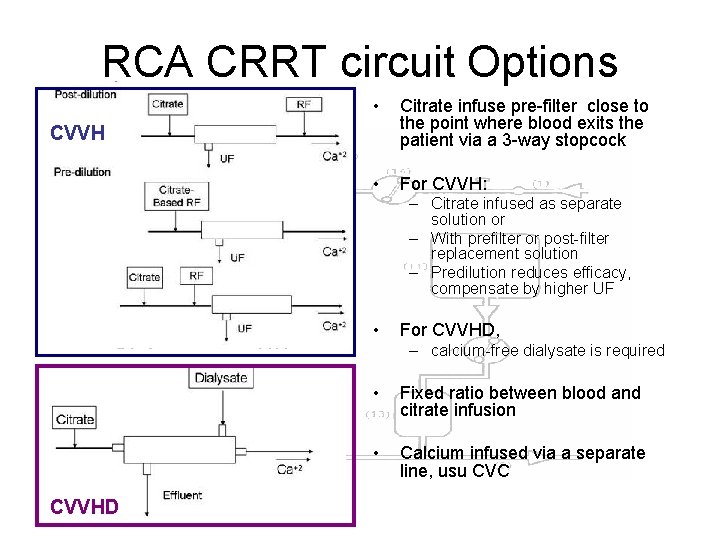
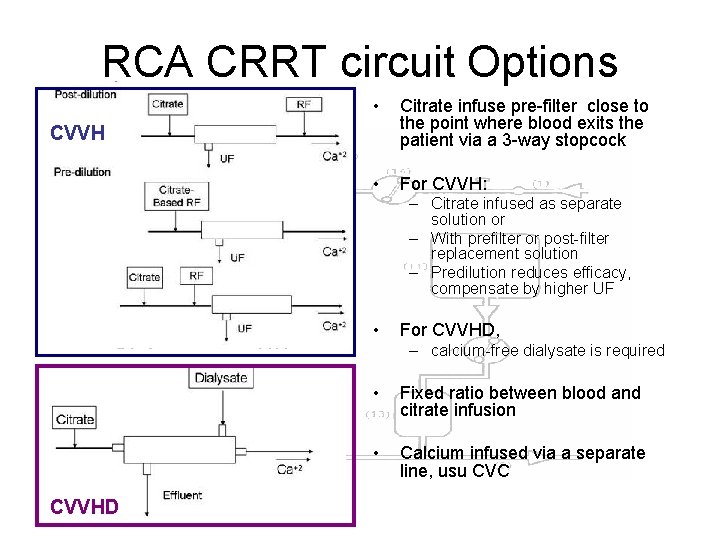
RCA CRRT circuit Options • Citrate infuse pre-filter close to the point where blood exits the patient via a 3 -way stopcock • For CVVH: CVVH – Citrate infused as separate solution or – With prefilter or post-filter replacement solution – Predilution reduces efficacy, compensate by higher UF • For CVVHD, – calcium-free dialysate is required CVVHD • Fixed ratio between blood and citrate infusion • Calcium infused via a separate line, usu CVC
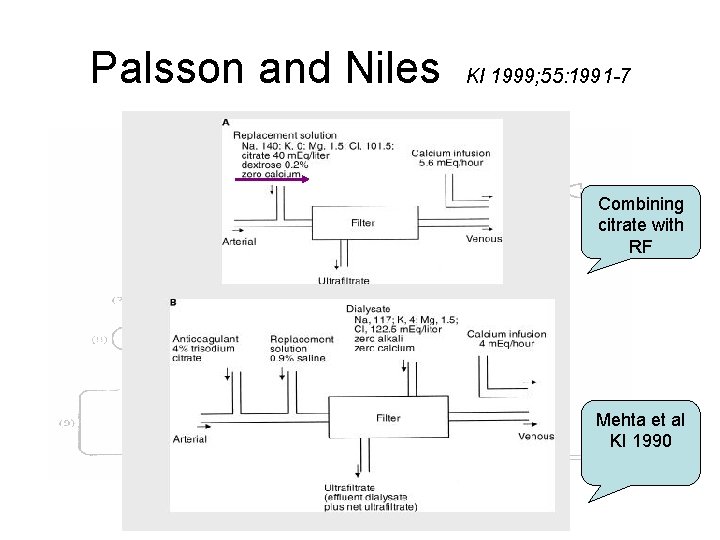
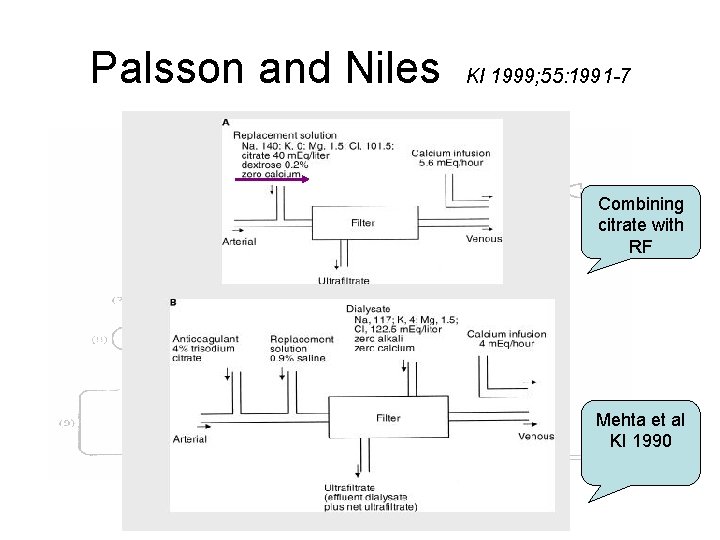
Palsson and Niles KI 1999; 55: 1991 -7 Combining citrate with RF Mehta et al KI 1990
Who can do that ?
PYNEH ICU (1995 -2003)
PYNEH ICU ( 2004 …. .
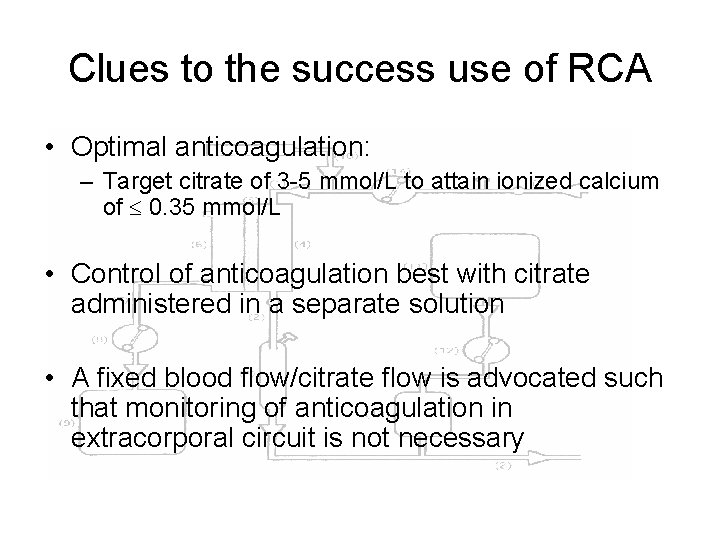
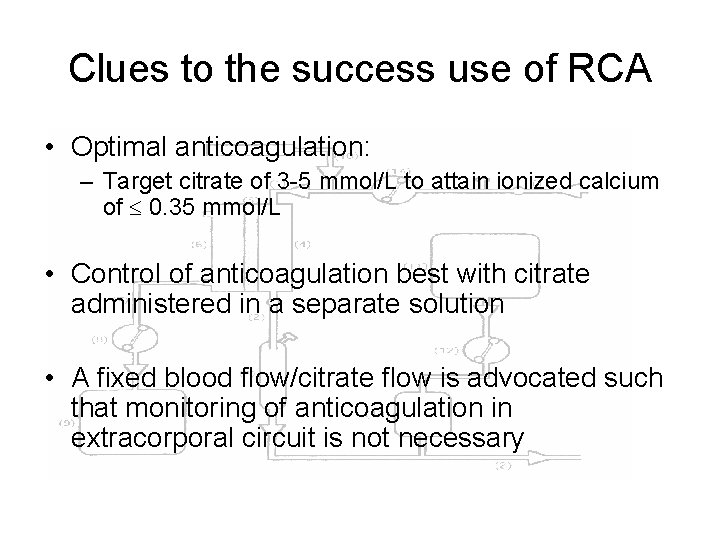
Clues to the success use of RCA • Optimal anticoagulation: – Target citrate of 3 -5 mmol/L to attain ionized calcium of 0. 35 mmol/L • Control of anticoagulation best with citrate administered in a separate solution • A fixed blood flow/citrate flow is advocated such that monitoring of anticoagulation in extracorporal circuit is not necessary
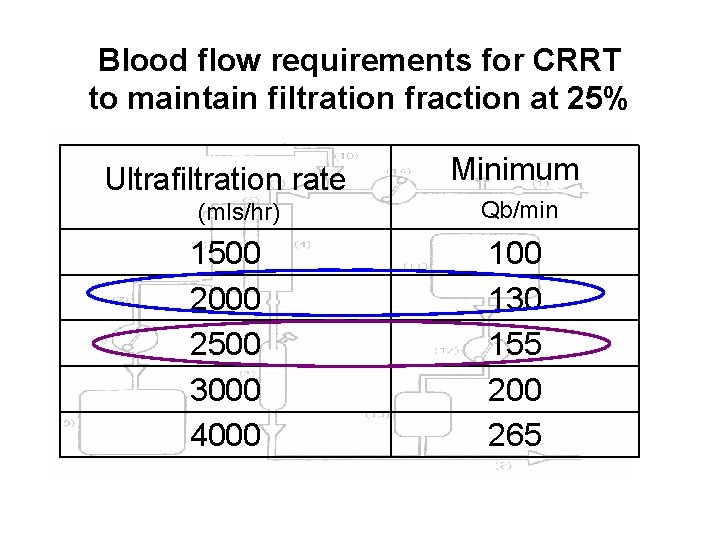
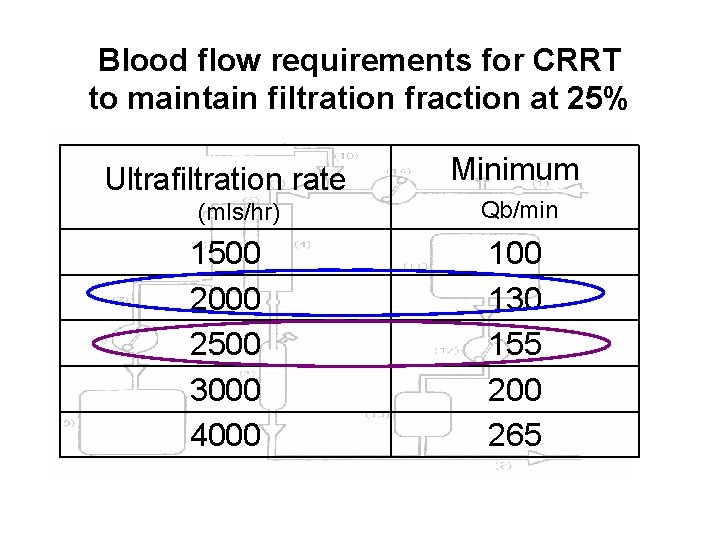
Blood flow requirements for CRRT to maintain filtration fraction at 25% Ultrafiltration rate (mls/hr) 1500 2000 2500 3000 4000 Minimum Qb/min 100 130 155 200 265
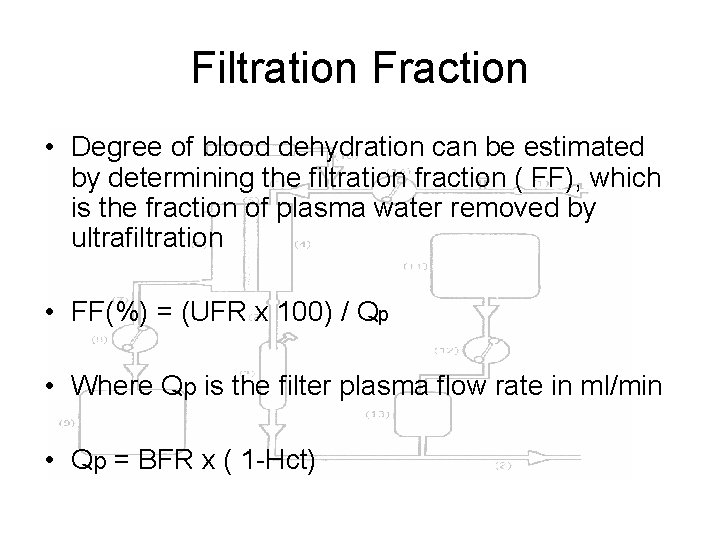
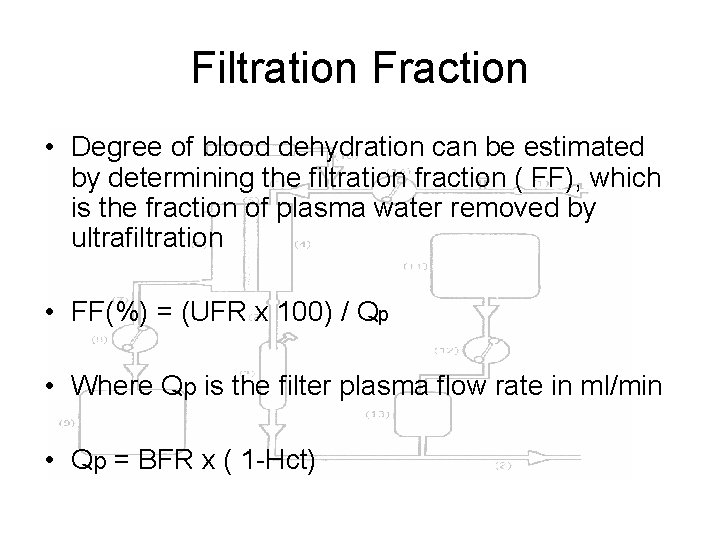
Filtration Fraction • Degree of blood dehydration can be estimated by determining the filtration fraction ( FF), which is the fraction of plasma water removed by ultrafiltration • FF(%) = (UFR x 100) / Qp • Where Qp is the filter plasma flow rate in ml/min • Qp = BFR x ( 1 -Hct)
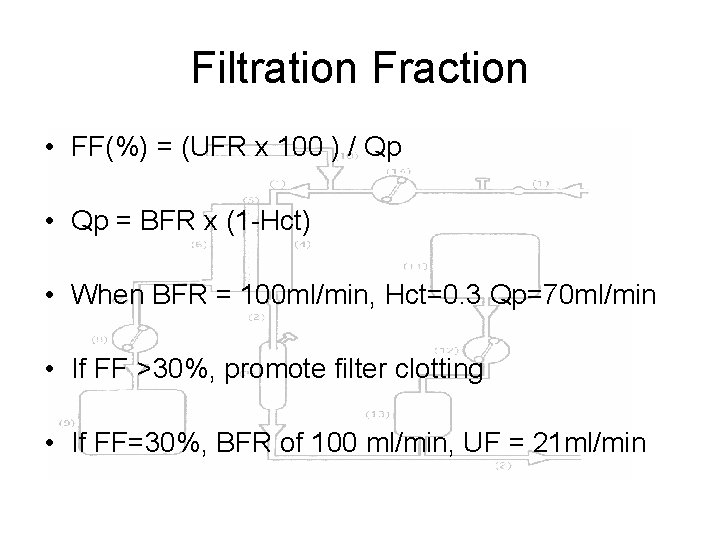
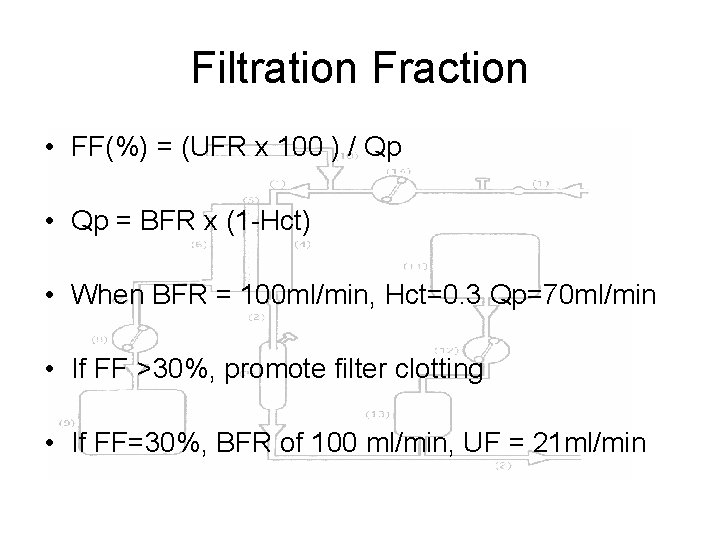
Filtration Fraction • FF(%) = (UFR x 100 ) / Qp • Qp = BFR x (1 -Hct) • When BFR = 100 ml/min, Hct=0. 3 Qp=70 ml/min • If FF >30%, promote filter clotting • If FF=30%, BFR of 100 ml/min, UF = 21 ml/min
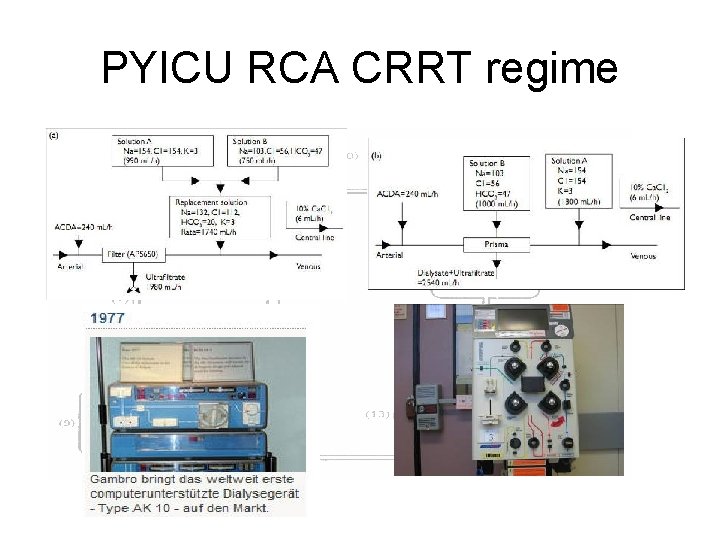
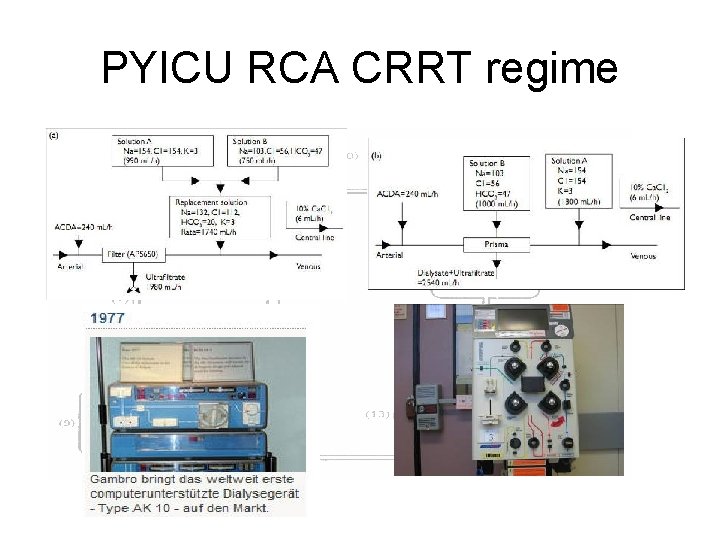
PYICU RCA CRRT regime
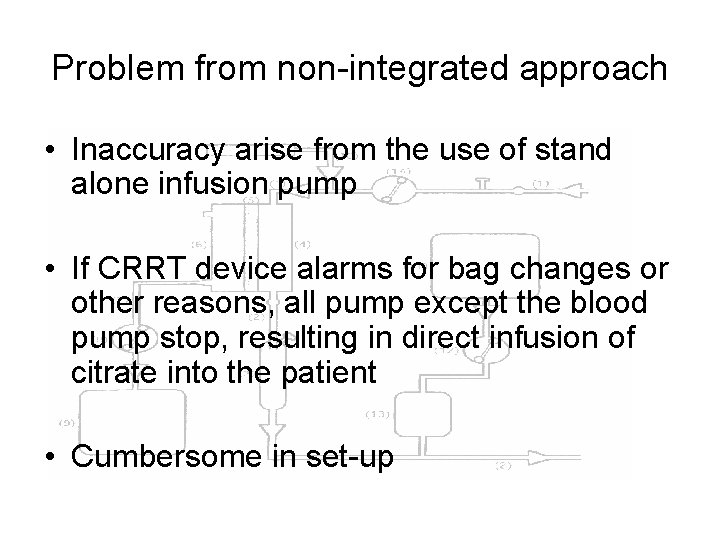
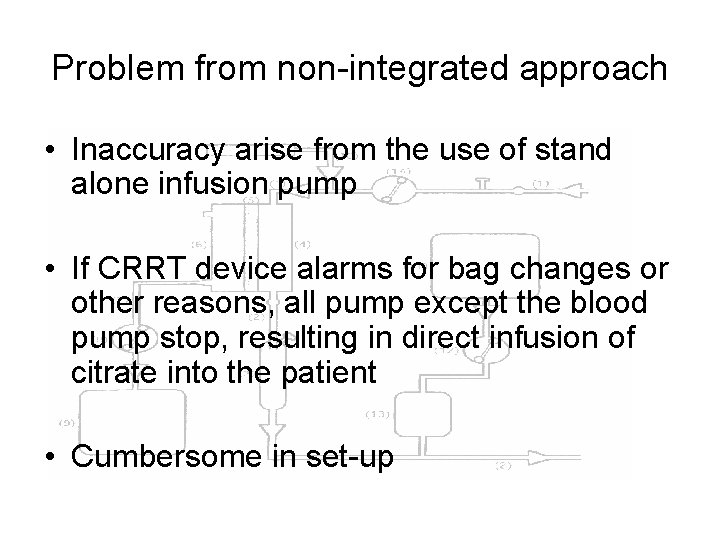
Problem from non-integrated approach • Inaccuracy arise from the use of stand alone infusion pump • If CRRT device alarms for bag changes or other reasons, all pump except the blood pump stop, resulting in direct infusion of citrate into the patient • Cumbersome in set-up
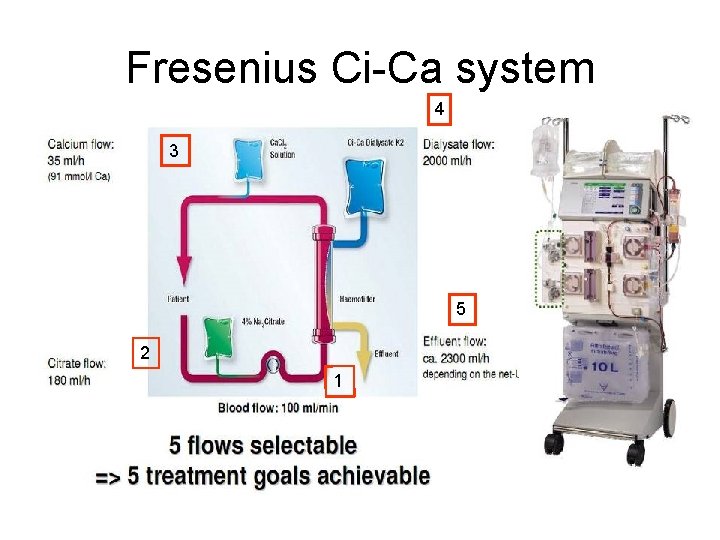
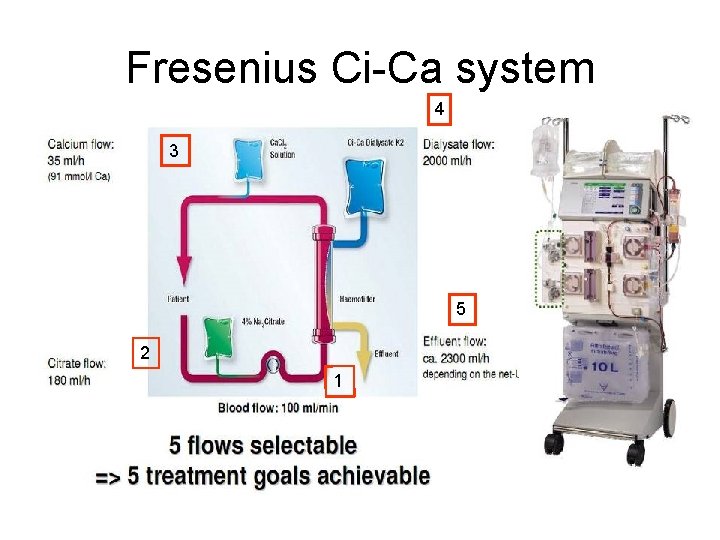
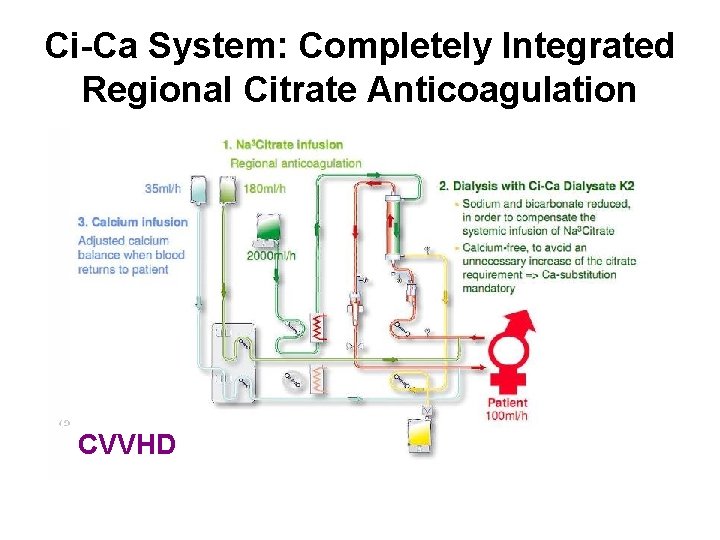
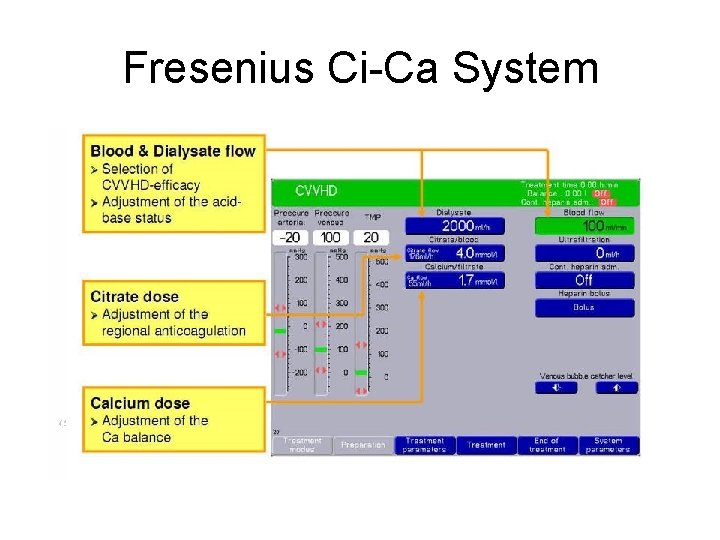
Fresenius Ci-Ca system 4 3 5 2 1
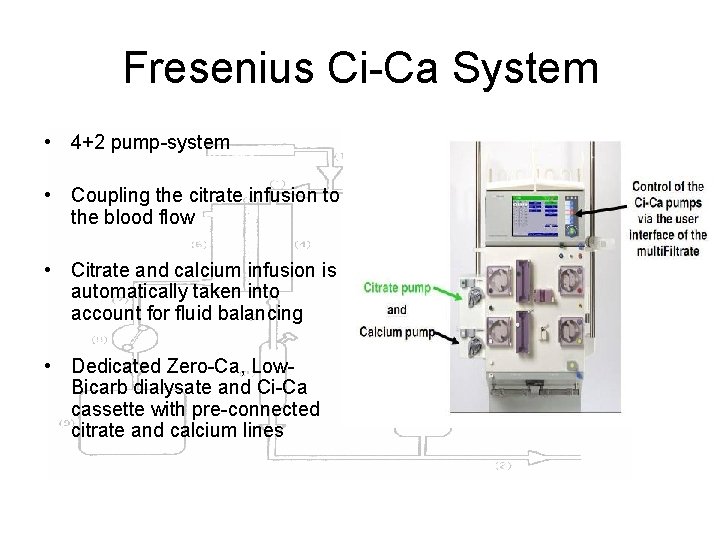
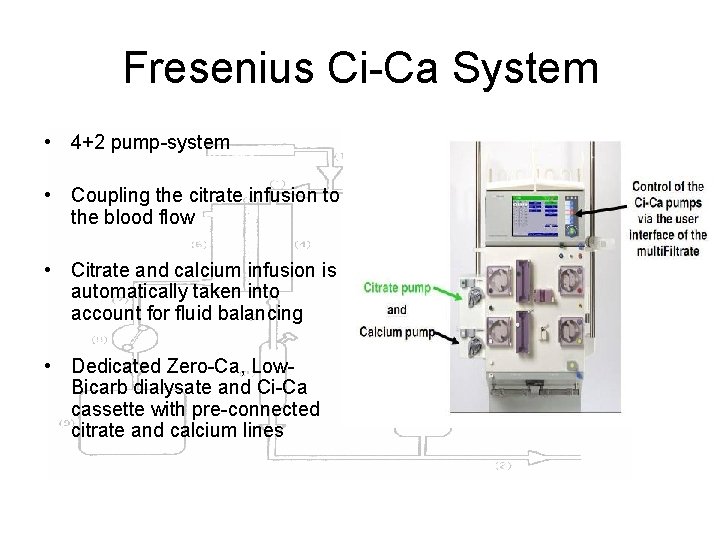
Fresenius Ci-Ca System • 4+2 pump-system • Coupling the citrate infusion to the blood flow • Citrate and calcium infusion is automatically taken into account for fluid balancing • Dedicated Zero-Ca, Low. Bicarb dialysate and Ci-Ca cassette with pre-connected citrate and calcium lines
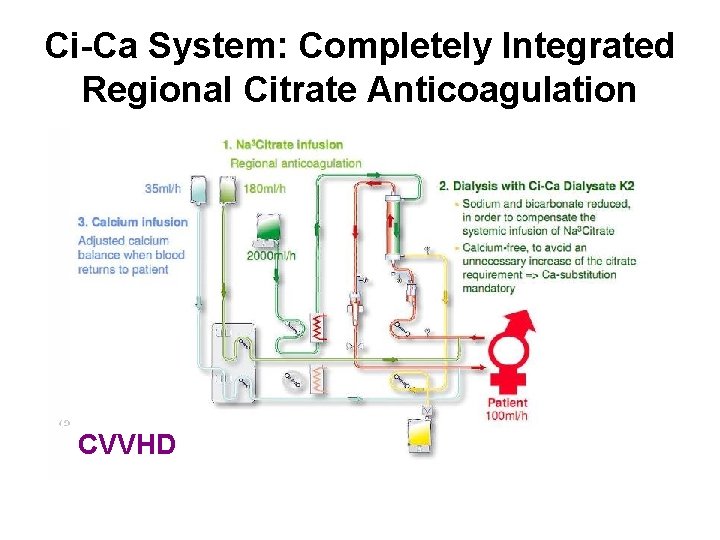
Ci-Ca System: Completely Integrated Regional Citrate Anticoagulation CVVHD
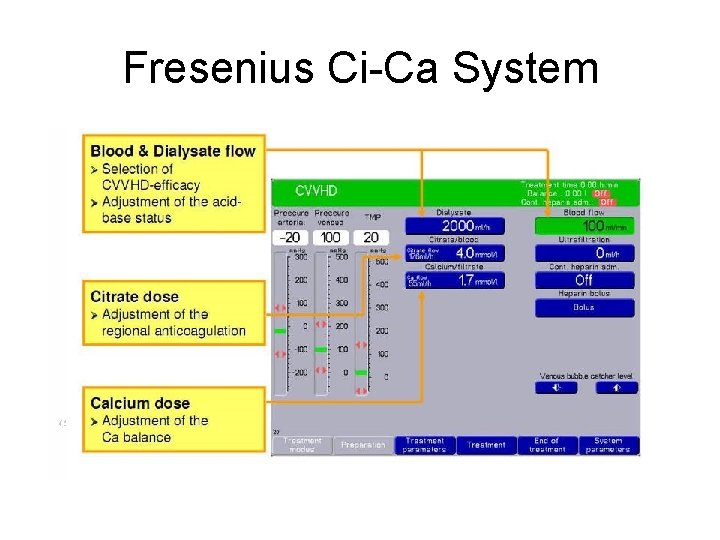
Fresenius Ci-Ca System
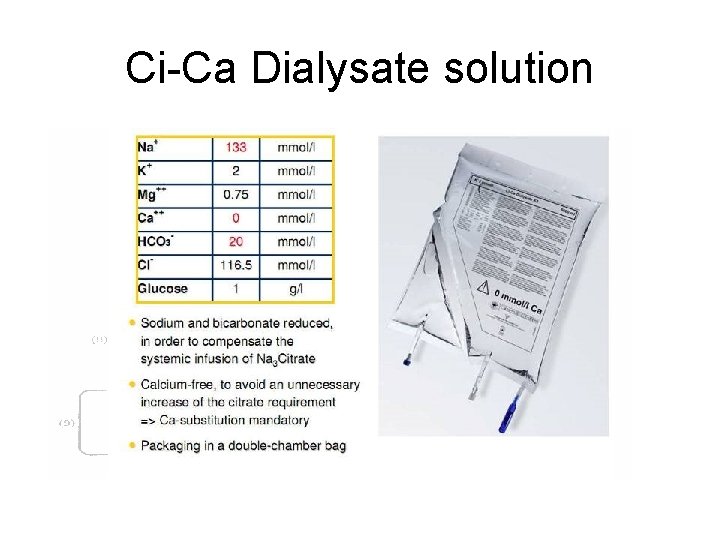
Ci-Ca Dialysate solution
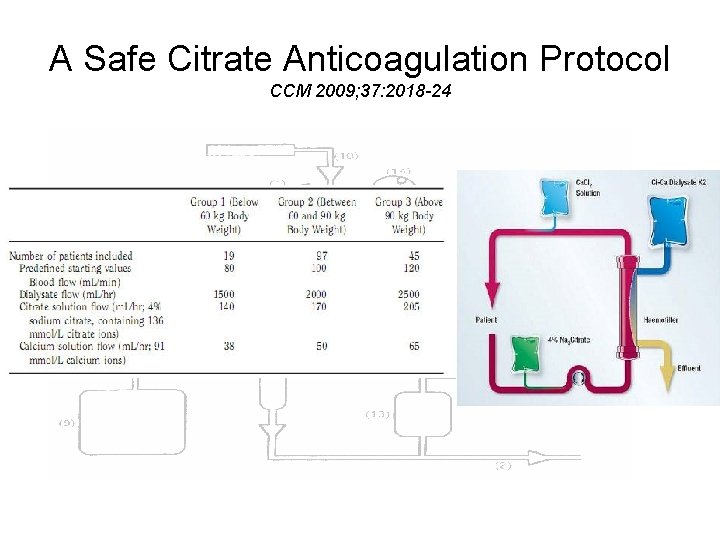
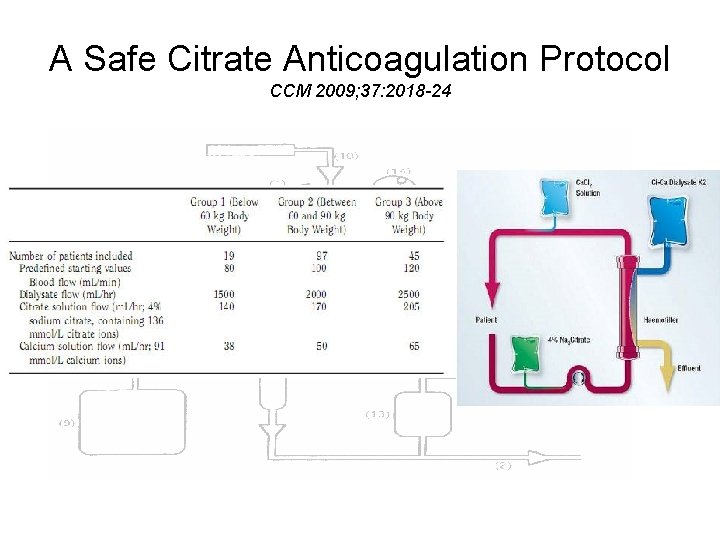
A Safe Citrate Anticoagulation Protocol CCM 2009; 37: 2018 -24
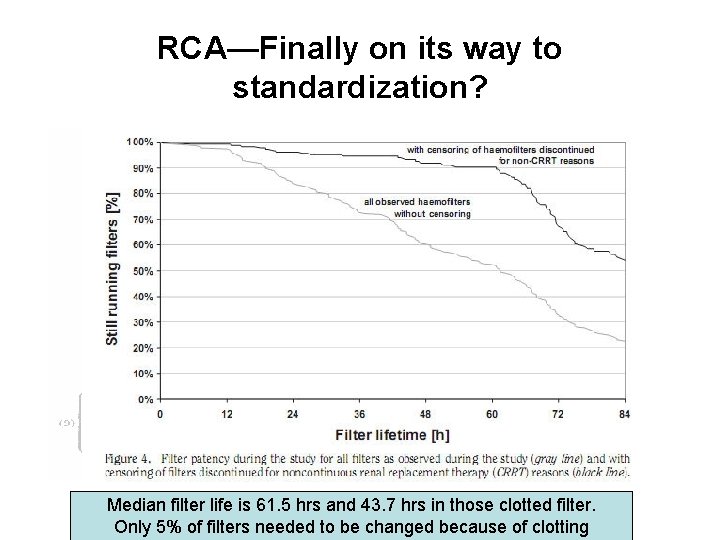
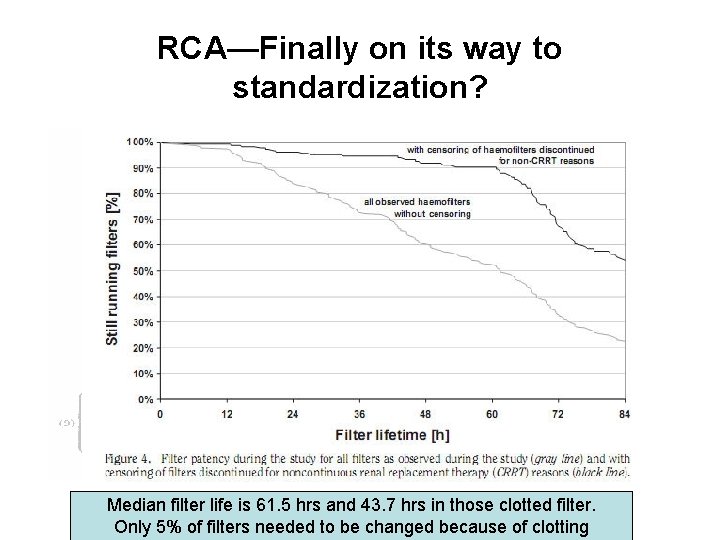
RCA—Finally on its way to standardization? Median filter life is 61. 5 hrs and 43. 7 hrs in those clotted filter. Only 5% of filters needed to be changed because of clotting
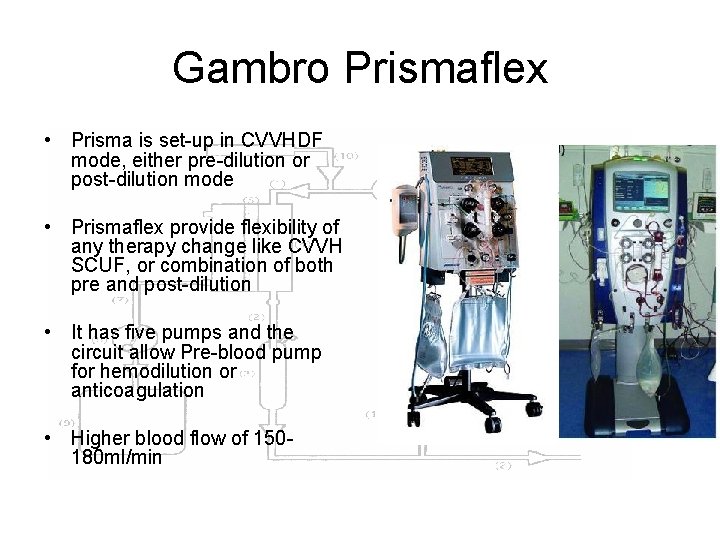
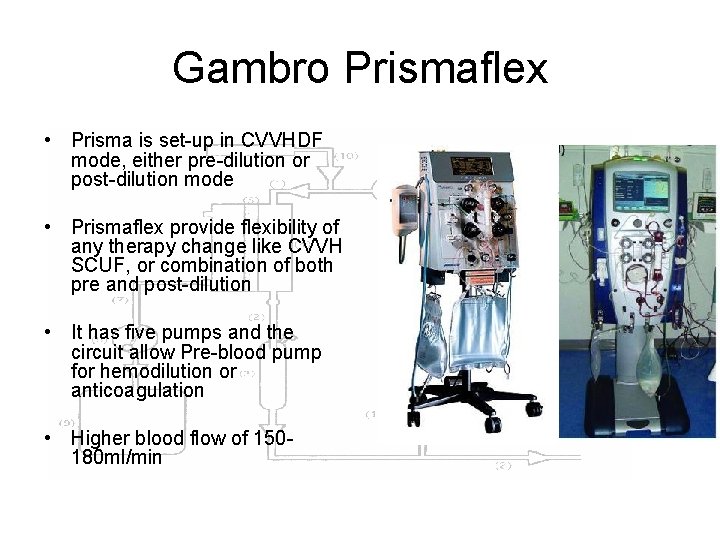
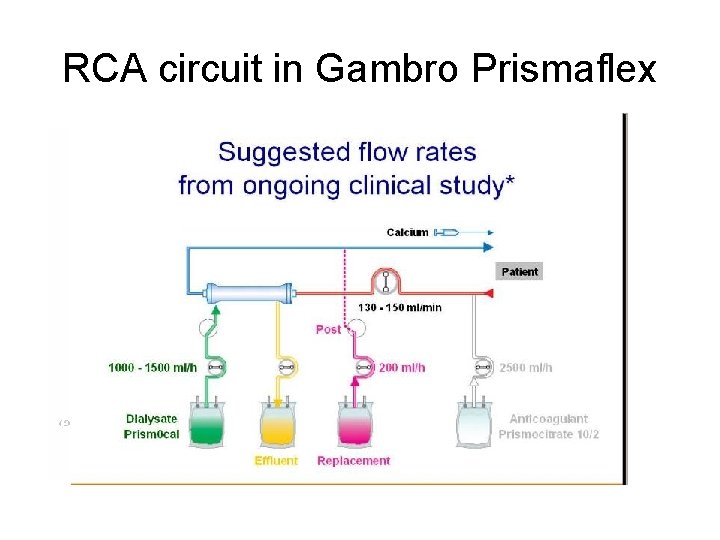
Gambro Prismaflex • Prisma is set-up in CVVHDF mode, either pre-dilution or post-dilution mode • Prismaflex provide flexibility of any therapy change like CVVH SCUF, or combination of both pre and post-dilution • It has five pumps and the circuit allow Pre-blood pump for hemodilution or anticoagulation • Higher blood flow of 150180 ml/min
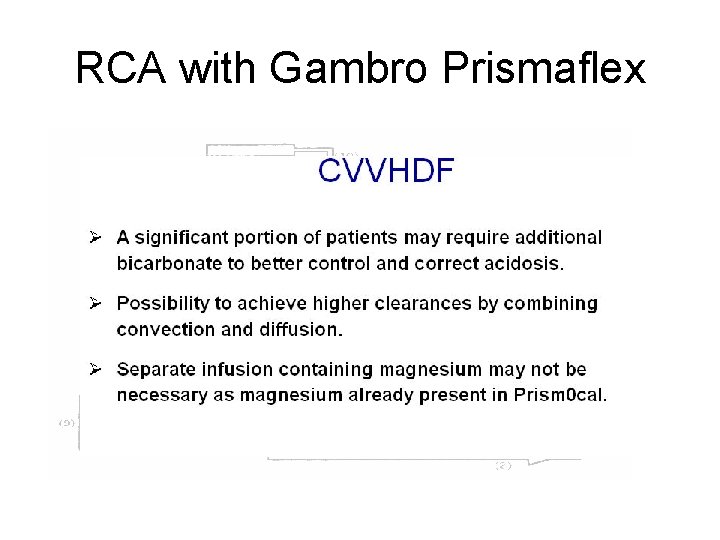
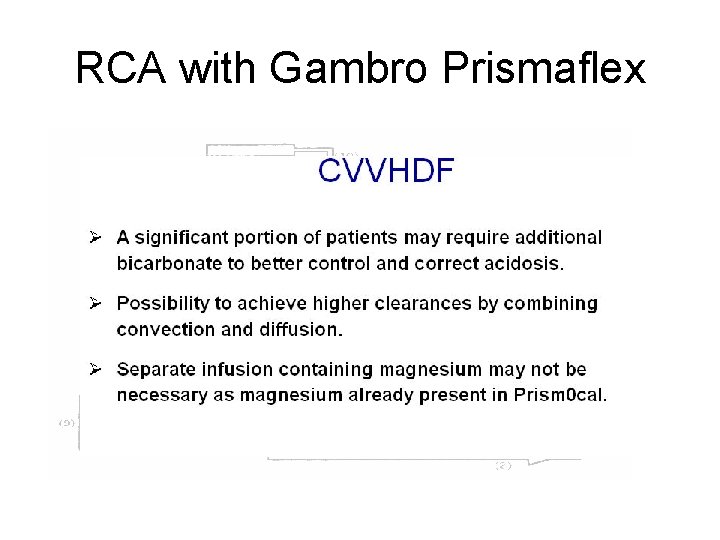
RCA with Gambro Prismaflex
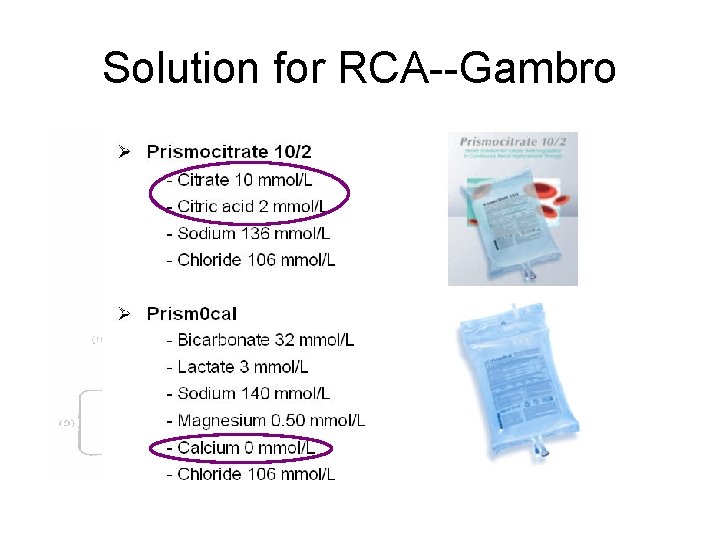
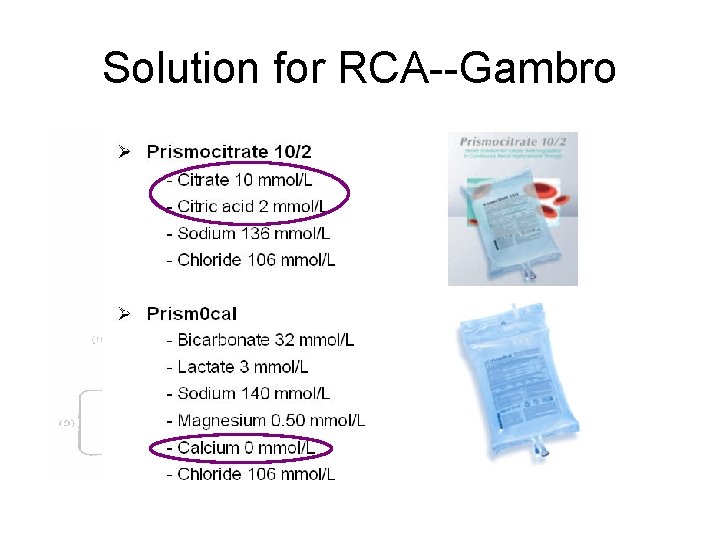
Solution for RCA--Gambro
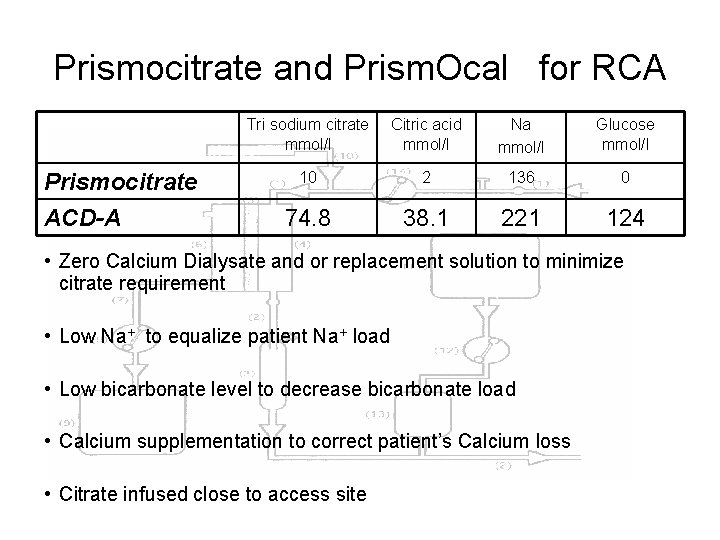
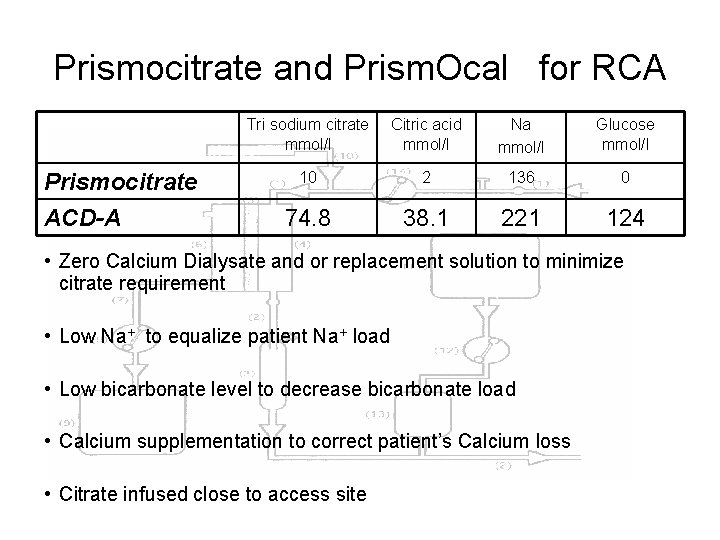
Prismocitrate and Prism. Ocal for RCA Prismocitrate ACD-A Tri sodium citrate mmol/l Citric acid mmol/l Na mmol/l Glucose mmol/l 10 2 136 0 74. 8 38. 1 221 124 • Zero Calcium Dialysate and or replacement solution to minimize citrate requirement • Low Na+ to equalize patient Na+ load • Low bicarbonate level to decrease bicarbonate load • Calcium supplementation to correct patient’s Calcium loss • Citrate infused close to access site
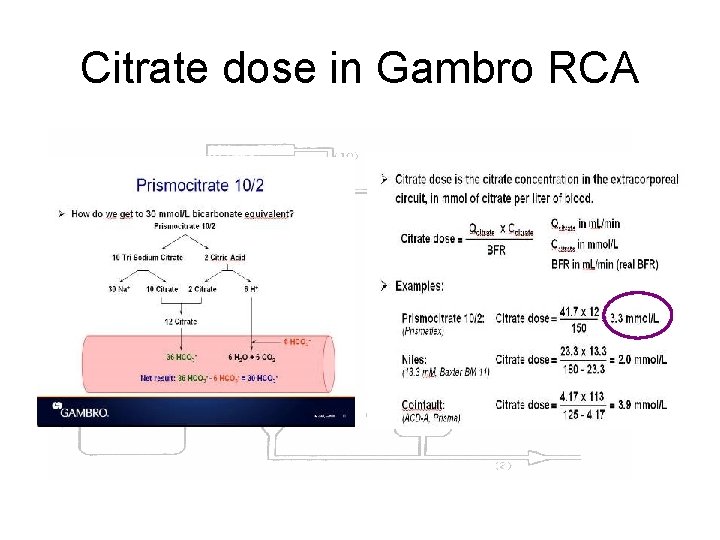
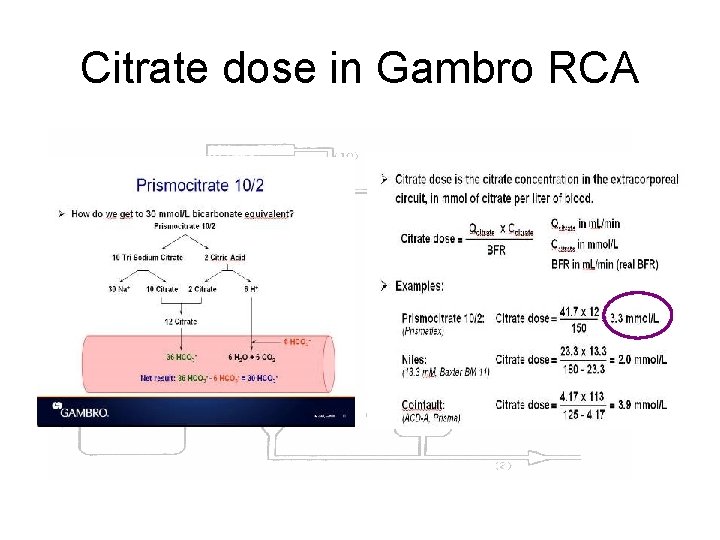
Citrate dose in Gambro RCA
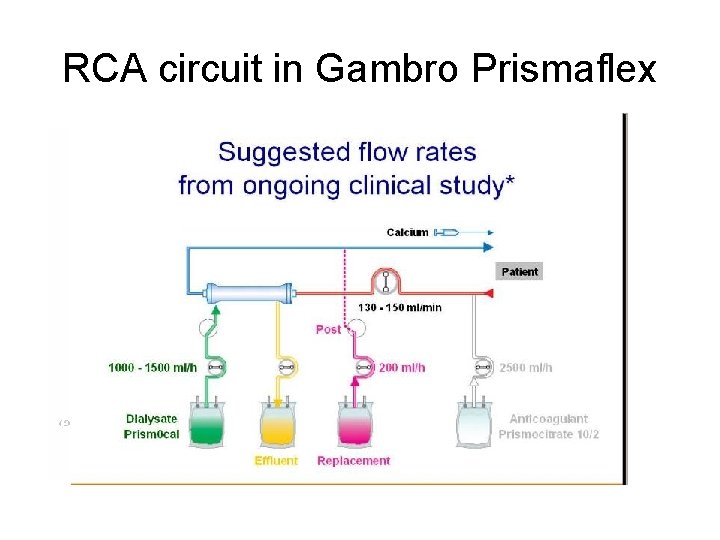
RCA circuit in Gambro Prismaflex
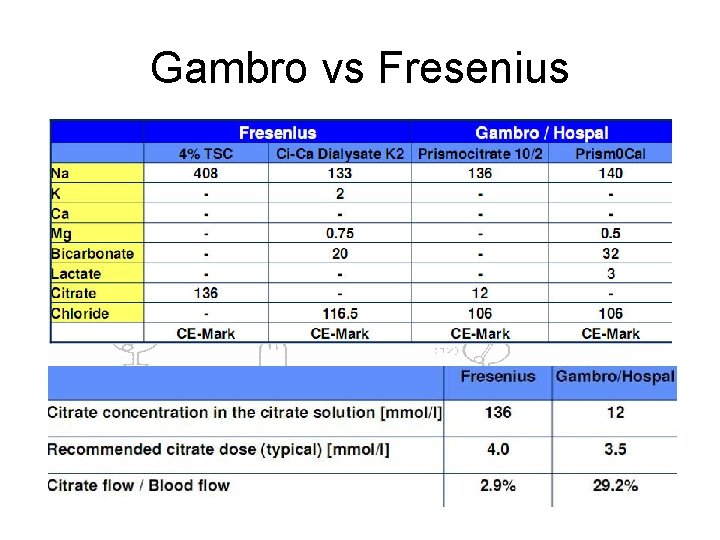
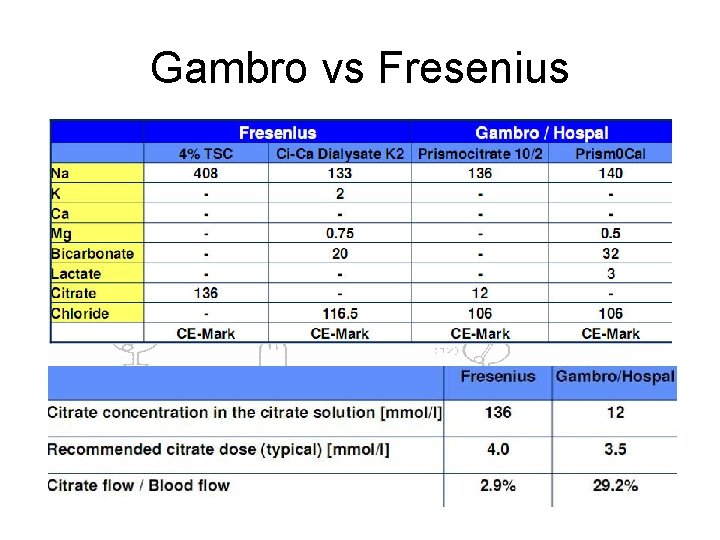
Gambro vs Fresenius
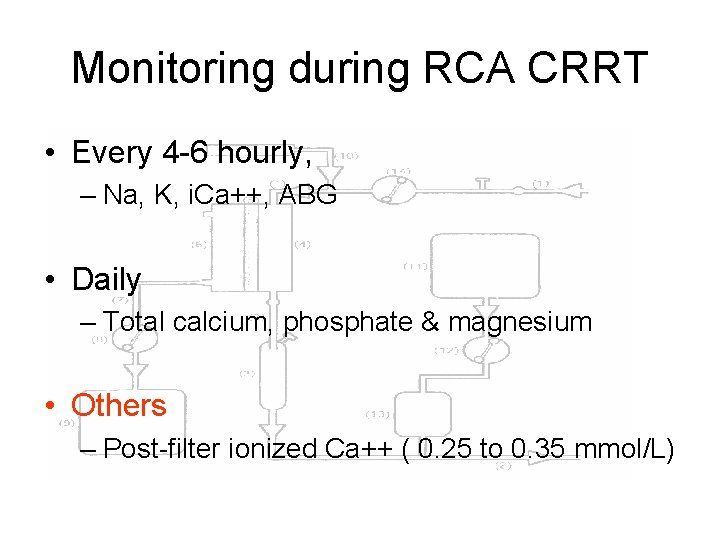
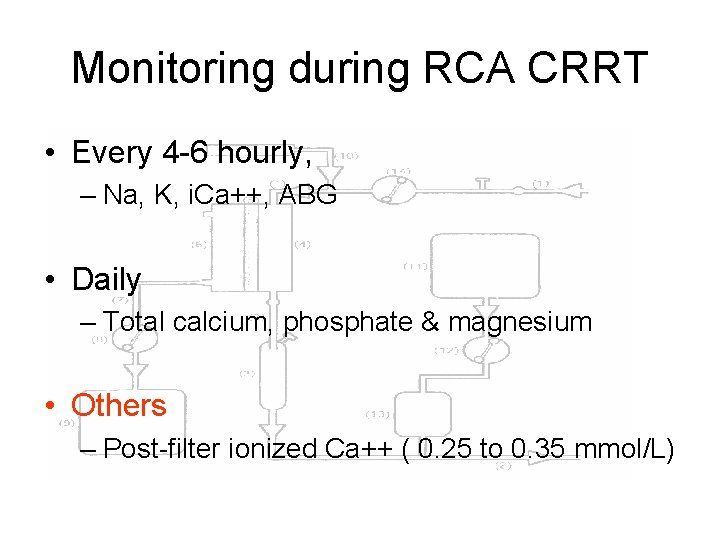
Monitoring during RCA CRRT • Every 4 -6 hourly, – Na, K, i. Ca++, ABG • Daily – Total calcium, phosphate & magnesium • Others – Post-filter ionized Ca++ ( 0. 25 to 0. 35 mmol/L)
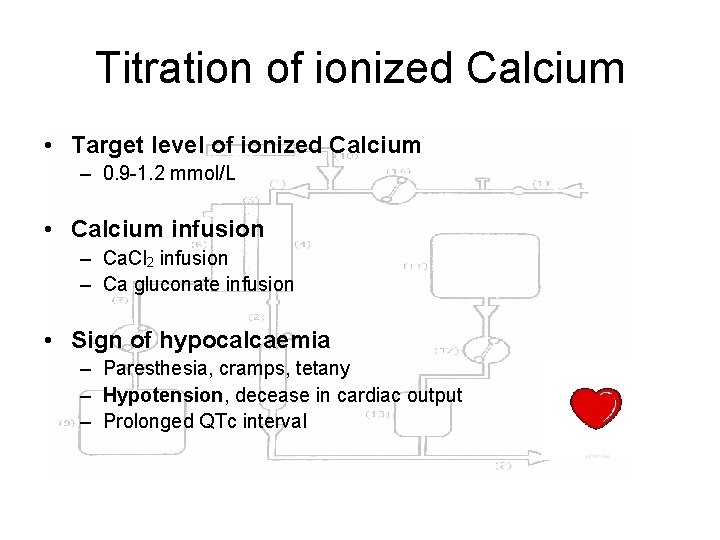
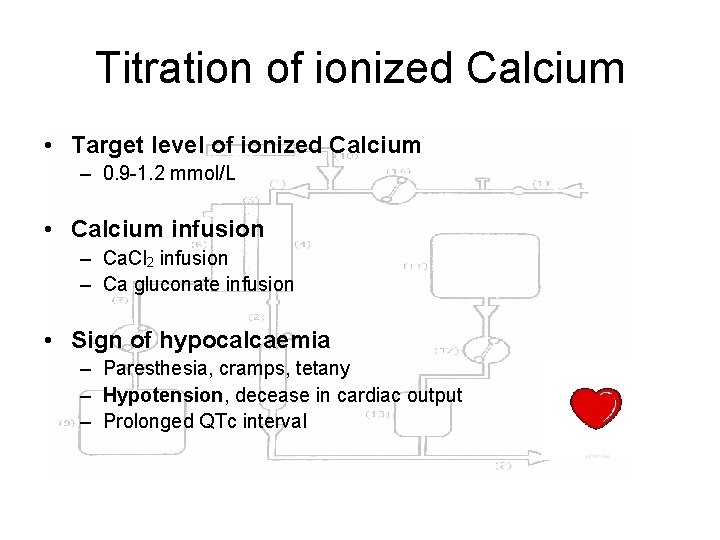
Titration of ionized Calcium • Target level of ionized Calcium – 0. 9 -1. 2 mmol/L • Calcium infusion – Ca. Cl 2 infusion – Ca gluconate infusion • Sign of hypocalcaemia – Paresthesia, cramps, tetany – Hypotension, decease in cardiac output – Prolonged QTc interval
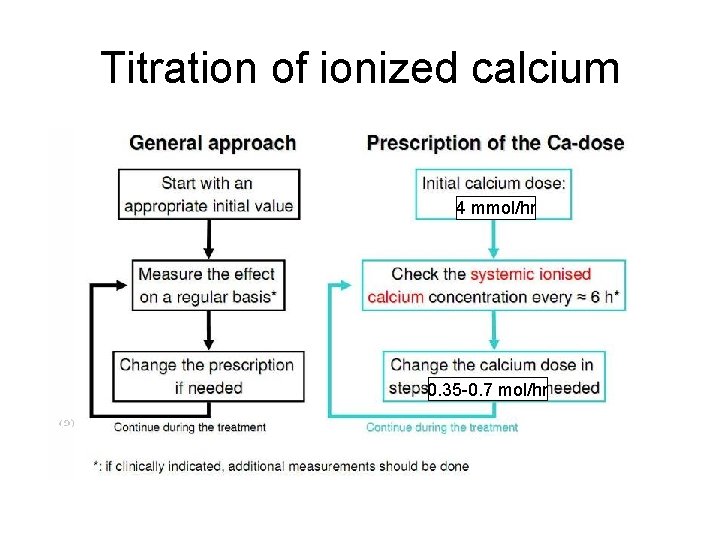
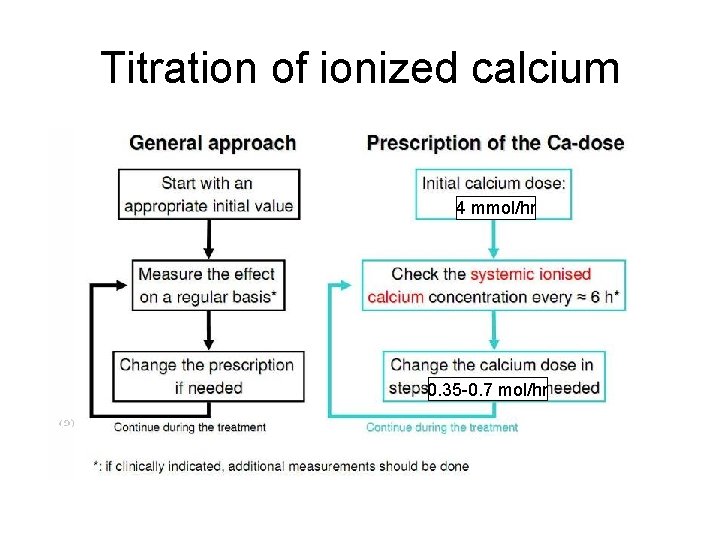
Titration of ionized calcium 4 mmol/hr 0. 35 -0. 7 mol/hr
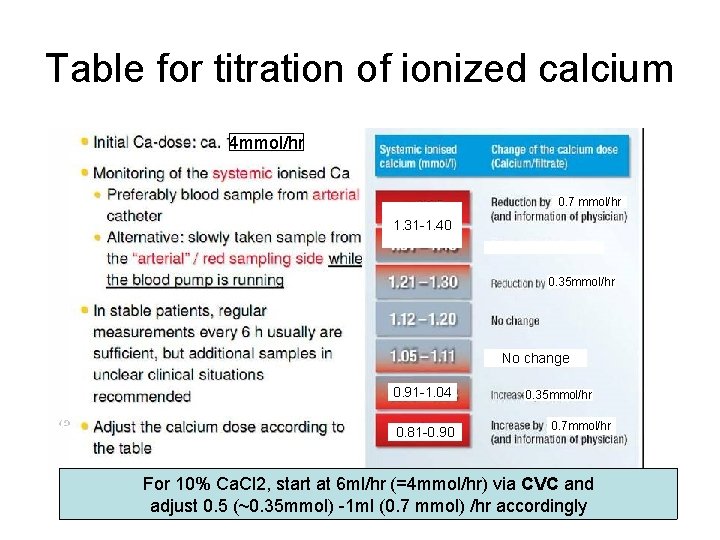
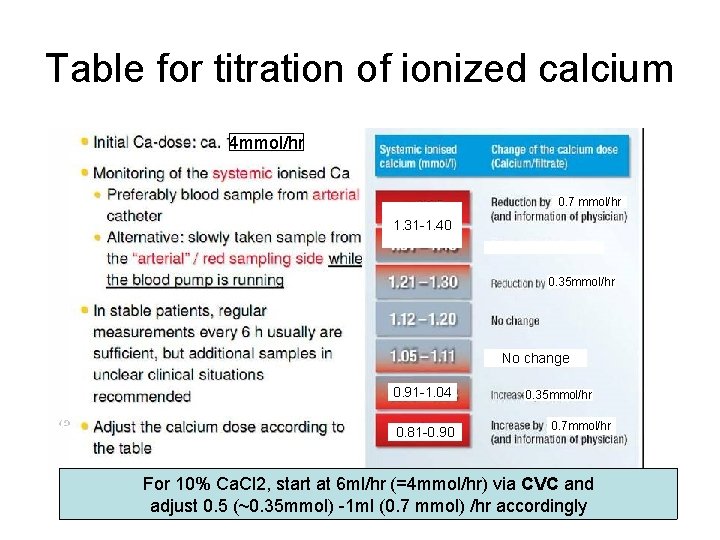
Table for titration of ionized calcium 4 mmol/hr 0. 7 mmol/hr 1. 31 -1. 40 0. 35 mmol/hr No change 0. 91 -1. 04 0. 81 -0. 90 0. 35 mmol/hr 0. 7 mmol/hr For 10% Ca. Cl 2, start at 6 ml/hr (=4 mmol/hr) via CVC and adjust 0. 5 (~0. 35 mmol) -1 ml (0. 7 mmol) /hr accordingly
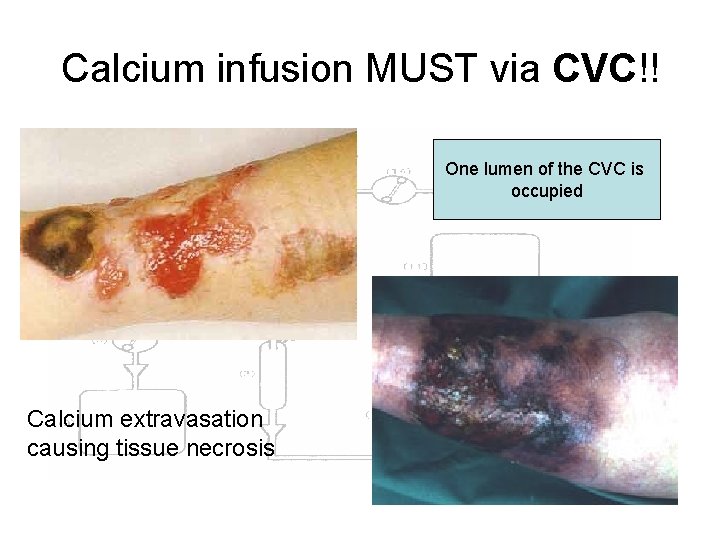
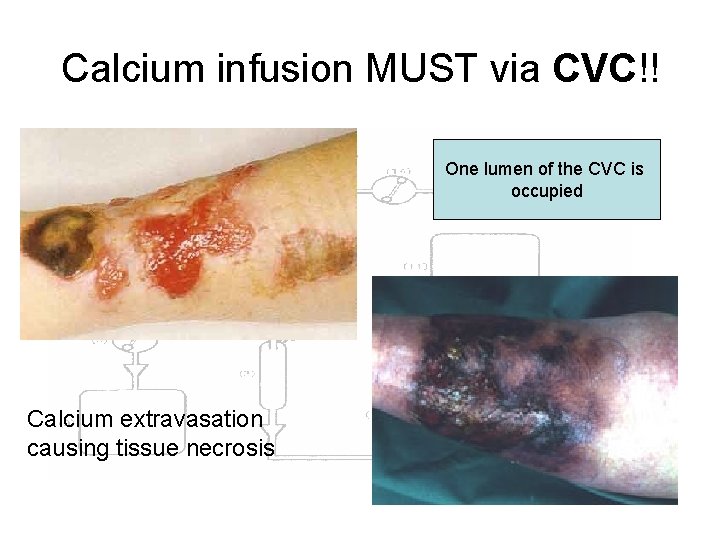
Calcium infusion MUST via CVC!! One lumen of the CVC is occupied Calcium extravasation causing tissue necrosis
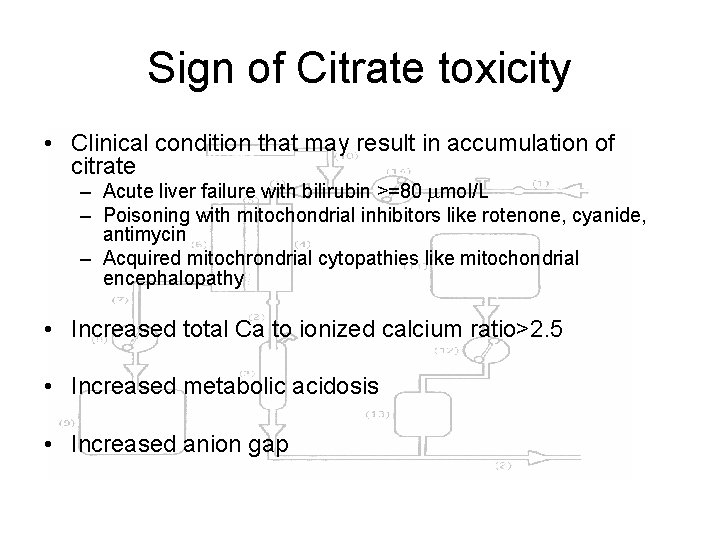
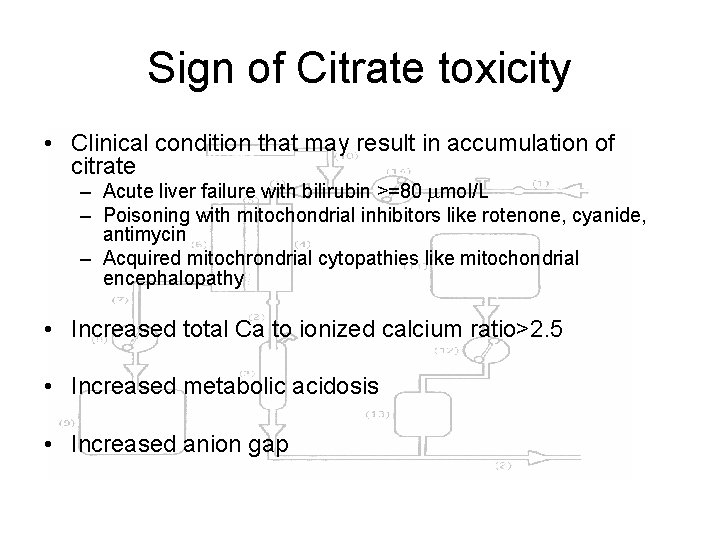
Sign of Citrate toxicity • Clinical condition that may result in accumulation of citrate – Acute liver failure with bilirubin >=80 mol/L – Poisoning with mitochondrial inhibitors like rotenone, cyanide, antimycin – Acquired mitochrondrial cytopathies like mitochondrial encephalopathy • Increased total Ca to ionized calcium ratio>2. 5 • Increased metabolic acidosis • Increased anion gap
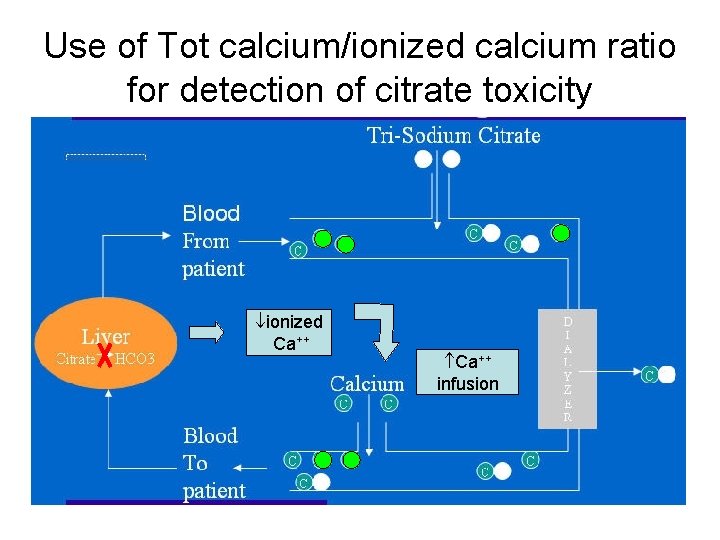
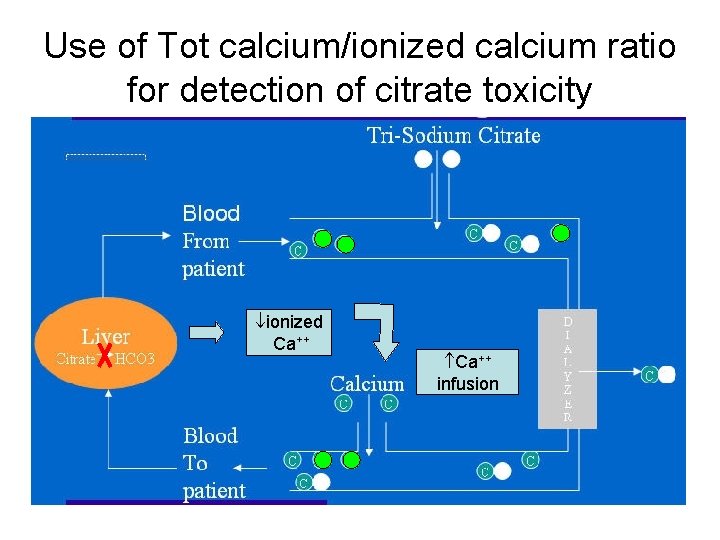
Use of Tot calcium/ionized calcium ratio for detection of citrate toxicity ionized Ca++ infusion
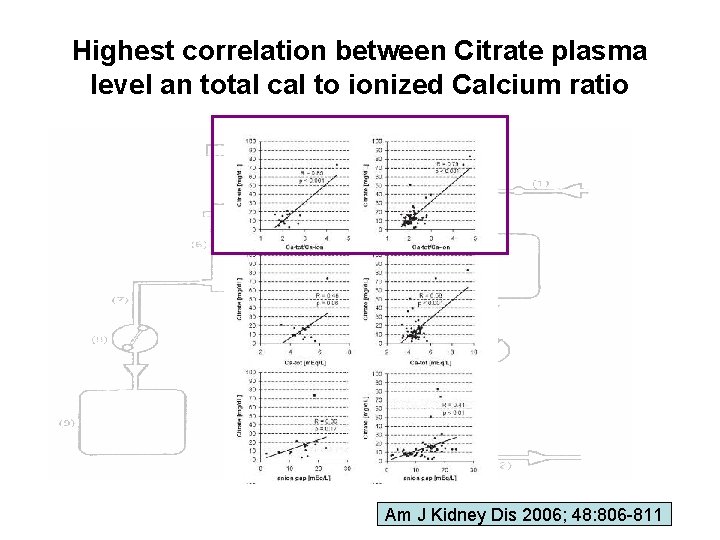
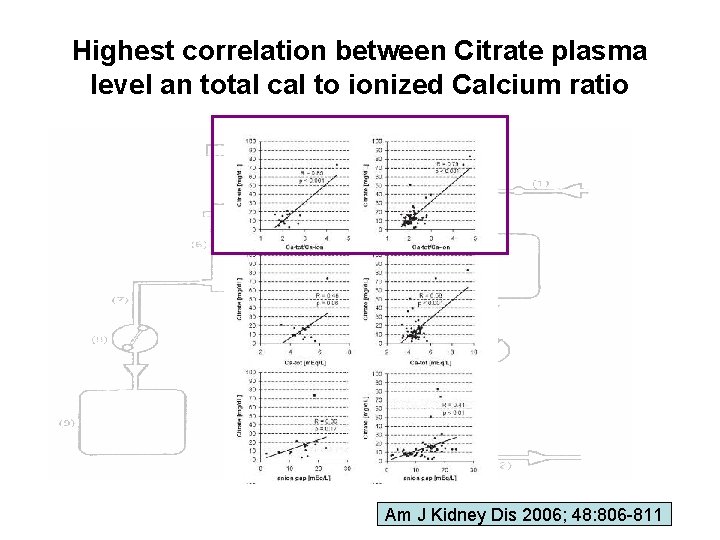
Highest correlation between Citrate plasma level an total cal to ionized Calcium ratio Am J Kidney Dis 2006; 48: 806 -811
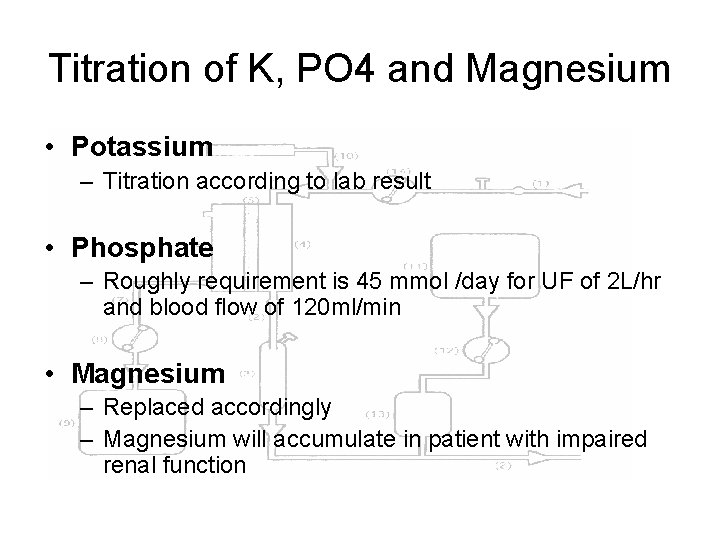
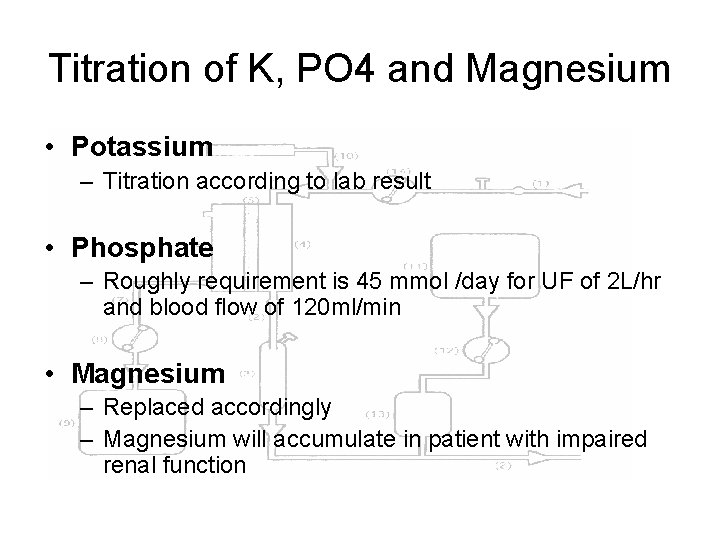
Titration of K, PO 4 and Magnesium • Potassium – Titration according to lab result • Phosphate – Roughly requirement is 45 mmol /day for UF of 2 L/hr and blood flow of 120 ml/min • Magnesium – Replaced accordingly – Magnesium will accumulate in patient with impaired renal function
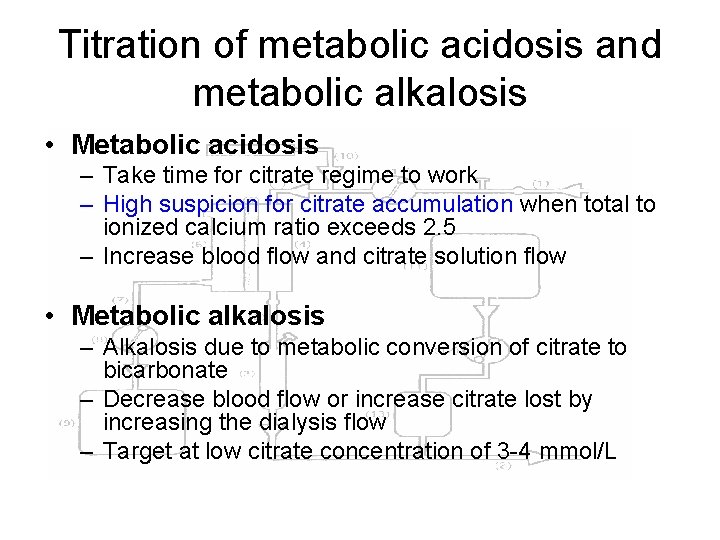
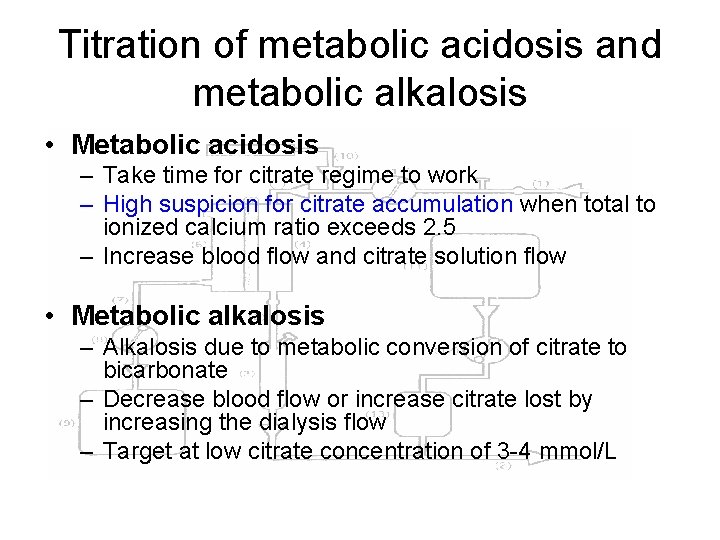
Titration of metabolic acidosis and metabolic alkalosis • Metabolic acidosis – Take time for citrate regime to work – High suspicion for citrate accumulation when total to ionized calcium ratio exceeds 2. 5 – Increase blood flow and citrate solution flow • Metabolic alkalosis – Alkalosis due to metabolic conversion of citrate to bicarbonate – Decrease blood flow or increase citrate lost by increasing the dialysis flow – Target at low citrate concentration of 3 -4 mmol/L
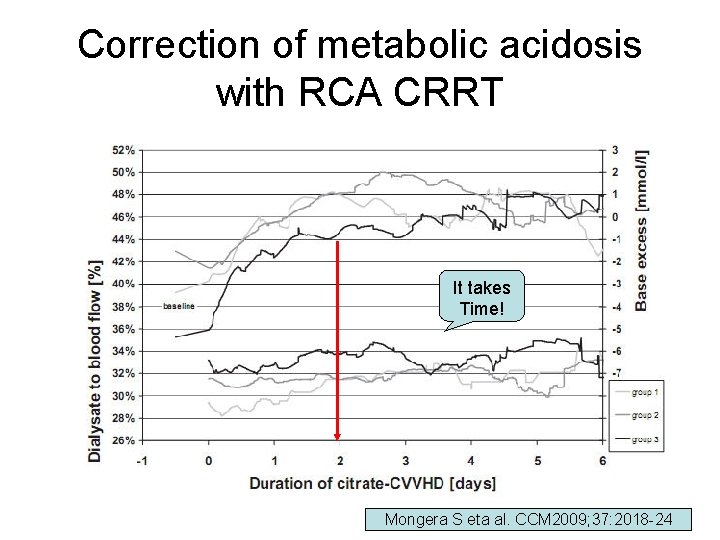
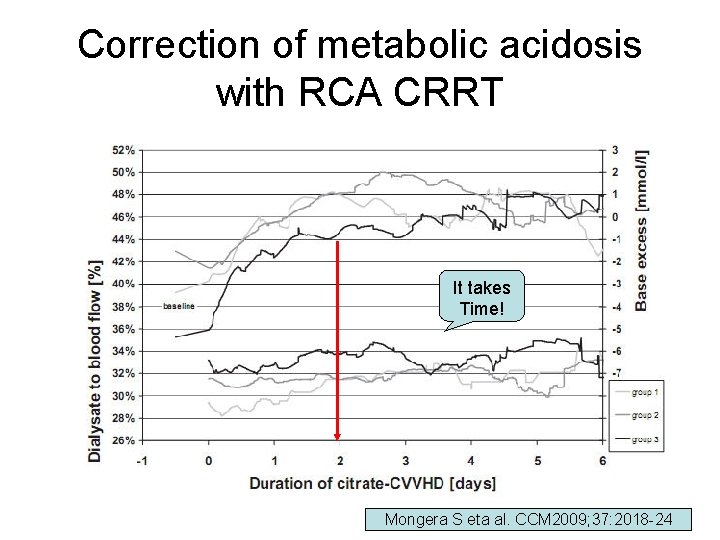
Correction of metabolic acidosis with RCA CRRT It takes Time! Mongera S eta al. CCM 2009; 37: 2018 -24
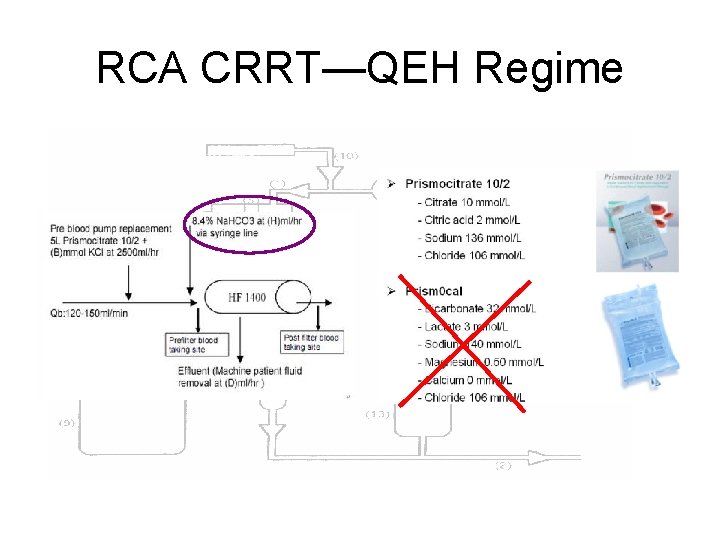
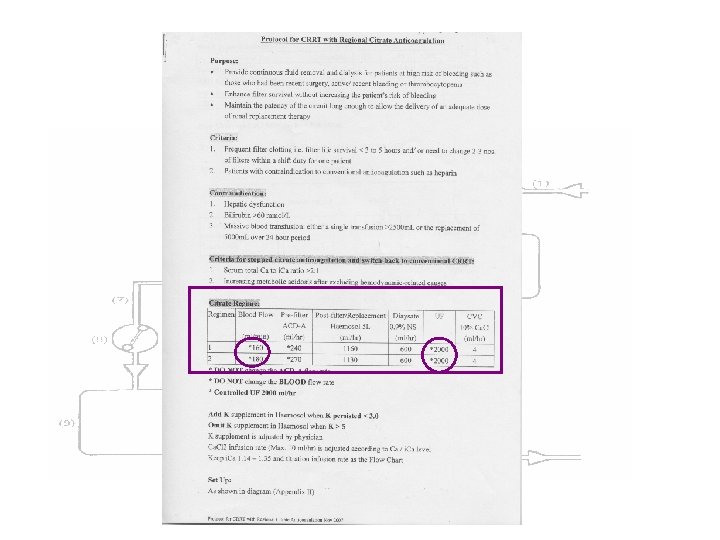
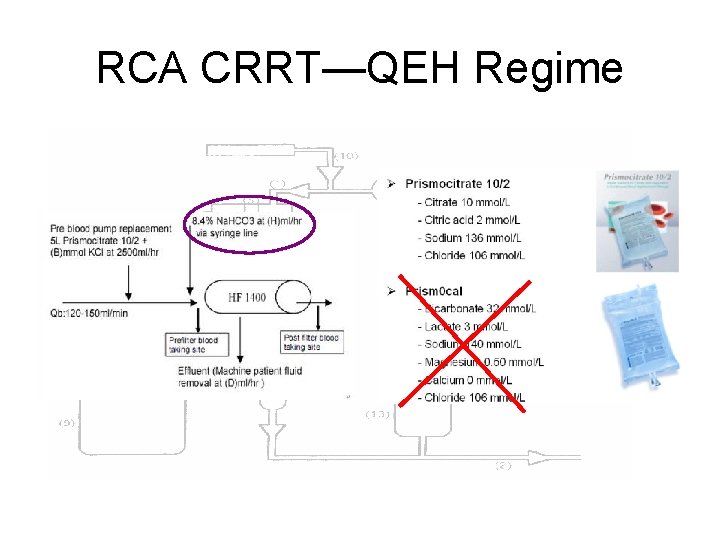
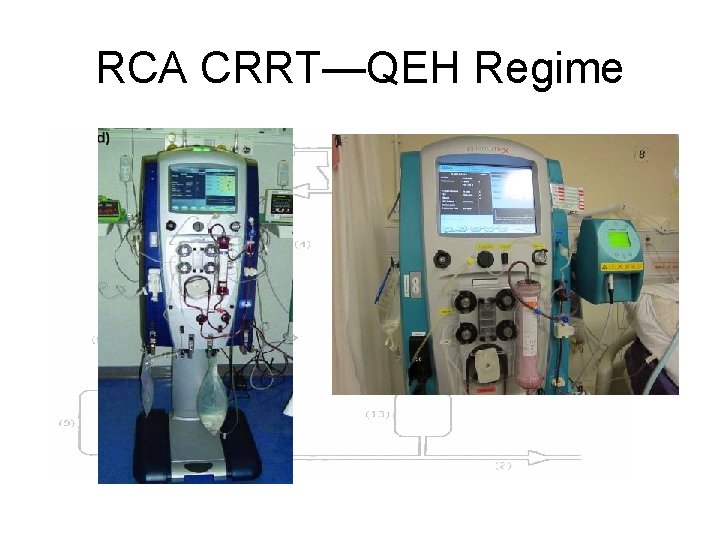
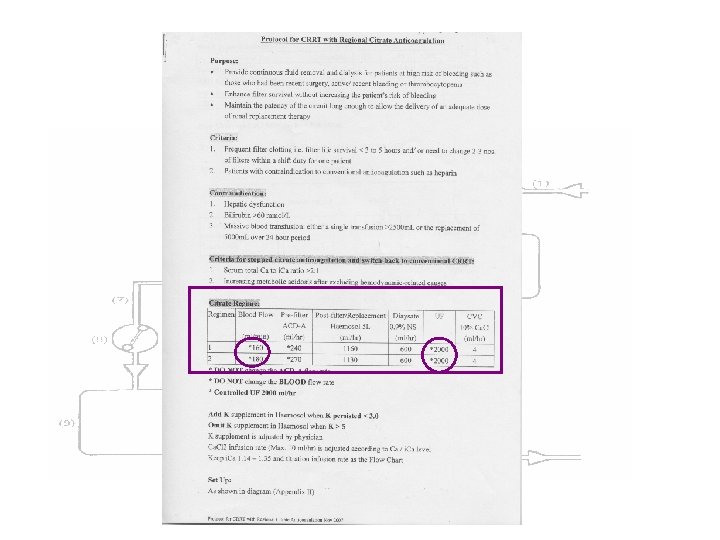
RCA CRRT—QEH Regime
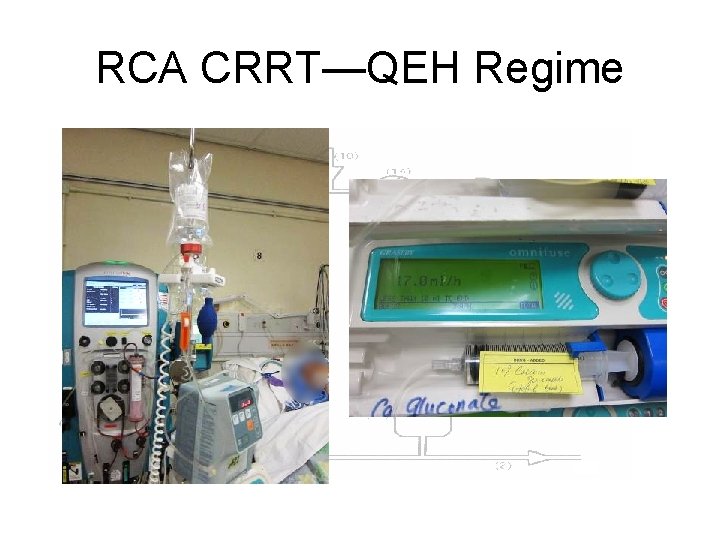
RCA CRRT—QEH Regime
RCA CRRT—QEH Regime
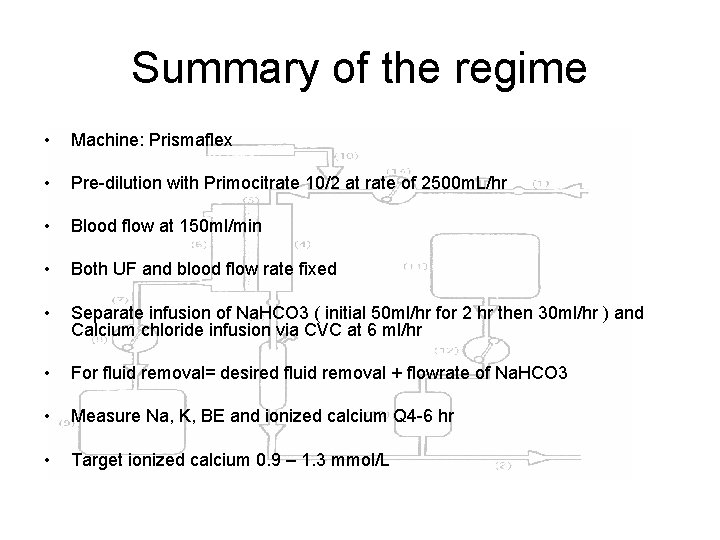
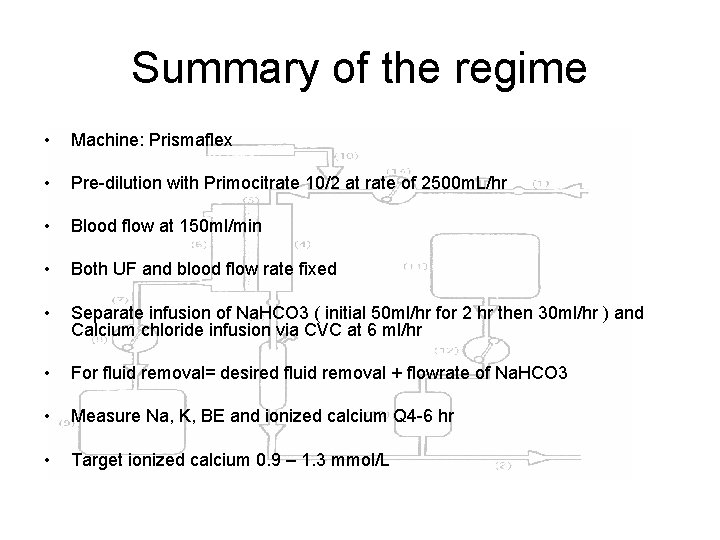
Summary of the regime • Machine: Prismaflex • Pre-dilution with Primocitrate 10/2 at rate of 2500 m. L/hr • Blood flow at 150 ml/min • Both UF and blood flow rate fixed • Separate infusion of Na. HCO 3 ( initial 50 ml/hr for 2 hr then 30 ml/hr ) and Calcium chloride infusion via CVC at 6 ml/hr • For fluid removal= desired fluid removal + flowrate of Na. HCO 3 • Measure Na, K, BE and ionized calcium Q 4 -6 hr • Target ionized calcium 0. 9 – 1. 3 mmol/L
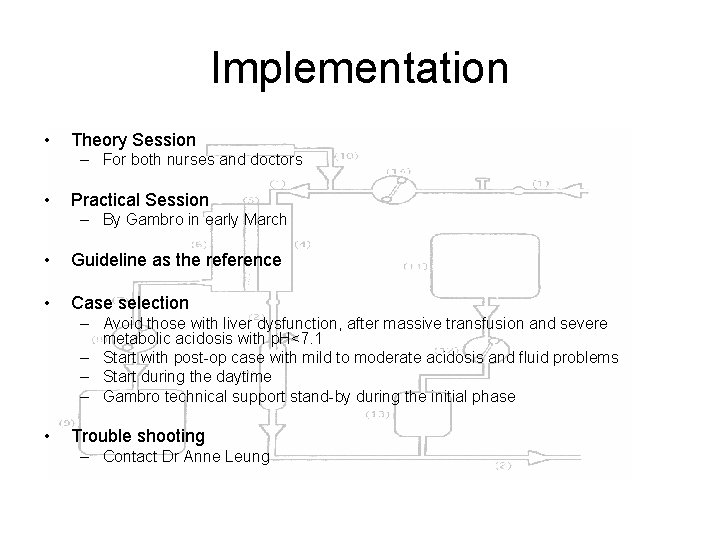
Implementation • Theory Session – For both nurses and doctors • Practical Session – By Gambro in early March • Guideline as the reference • Case selection – Avoid those with liver dysfunction, after massive transfusion and severe metabolic acidosis with p. H<7. 1 – Start with post-op case with mild to moderate acidosis and fluid problems – Start during the daytime – Gambro technical support stand-by during the initial phase • Trouble shooting – Contact Dr Anne Leung
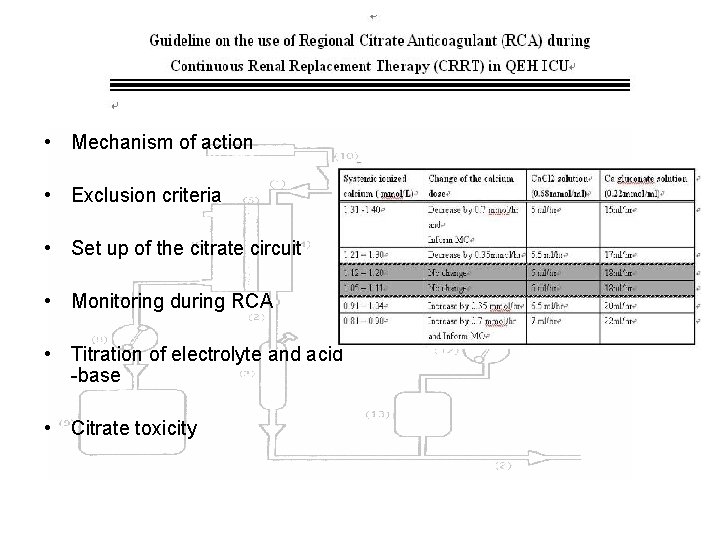
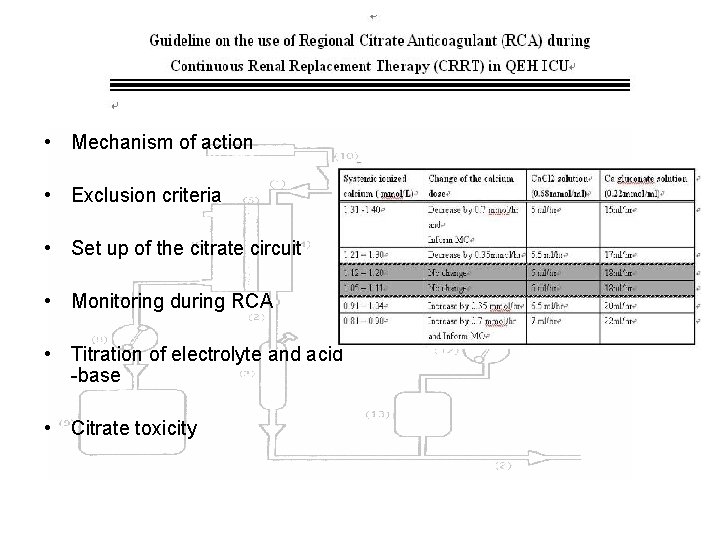
• Mechanism of action • Exclusion criteria • Set up of the citrate circuit • Monitoring during RCA • Titration of electrolyte and acid -base • Citrate toxicity
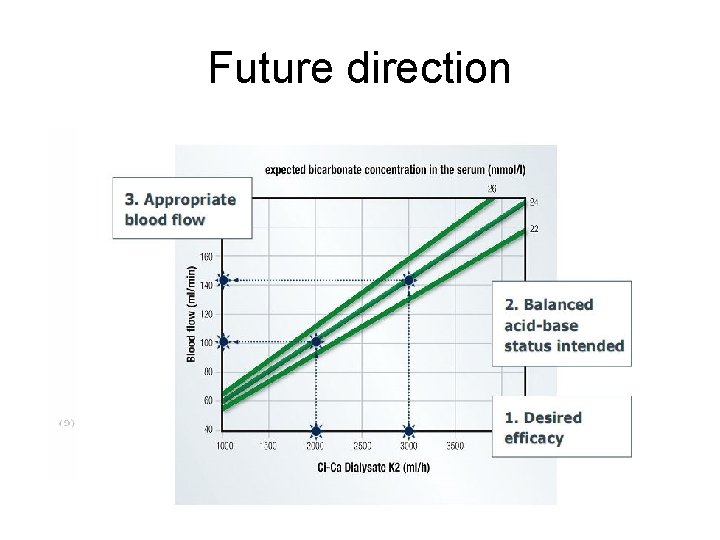
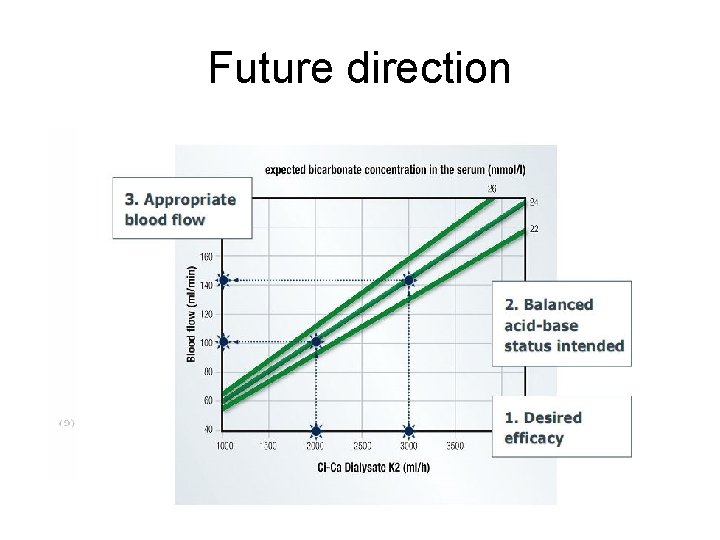
Future direction
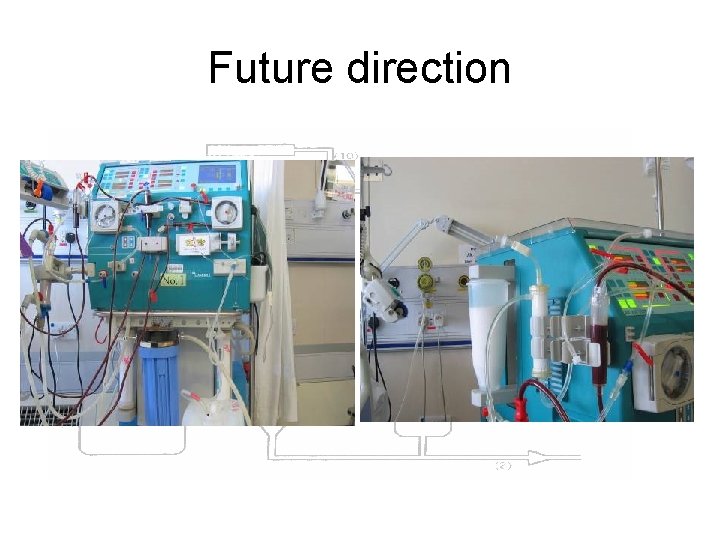
Future direction

With you, we should overcome!
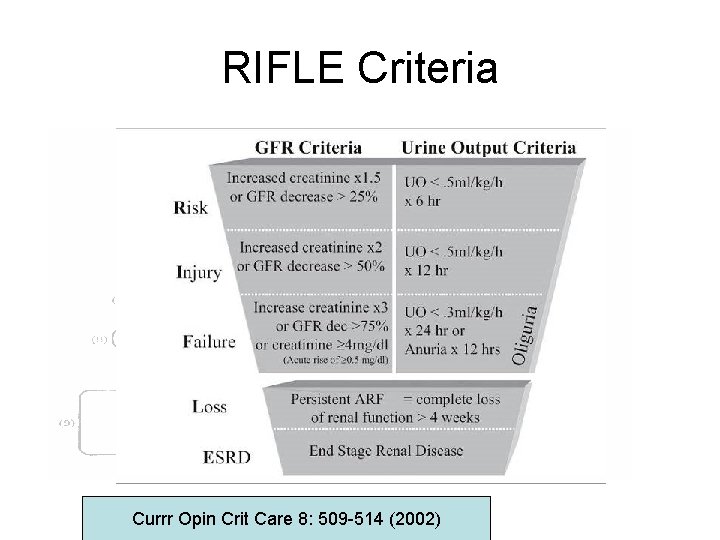
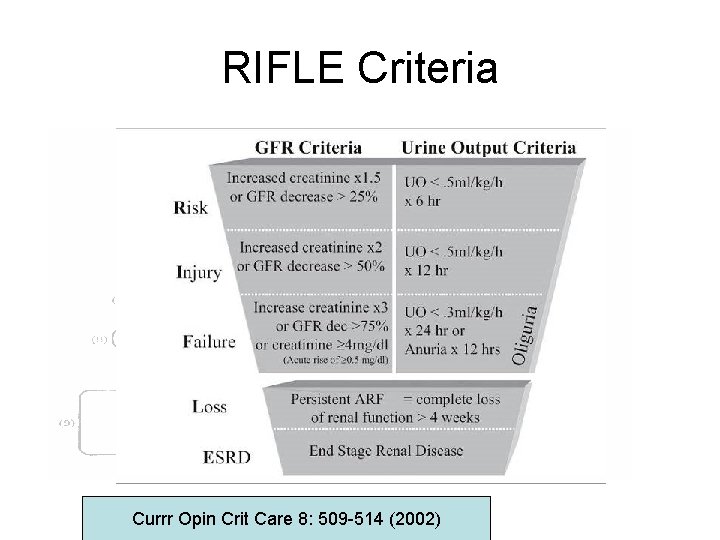
RIFLE Criteria Currr Opin Crit Care 8: 509 -514 (2002)
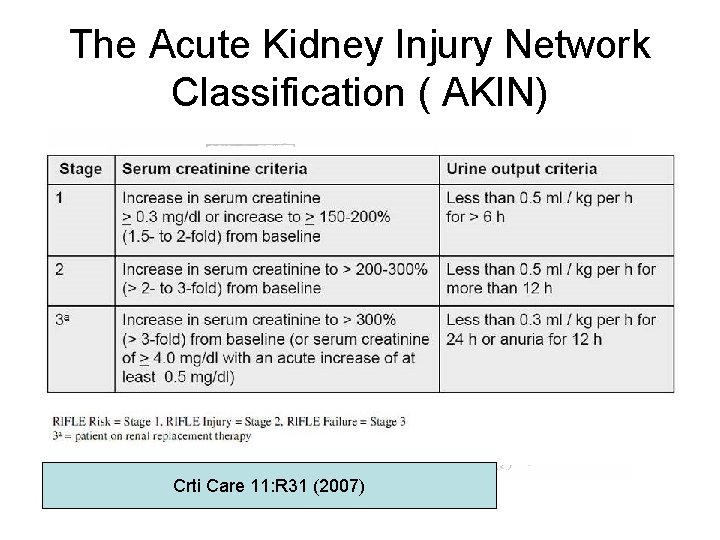
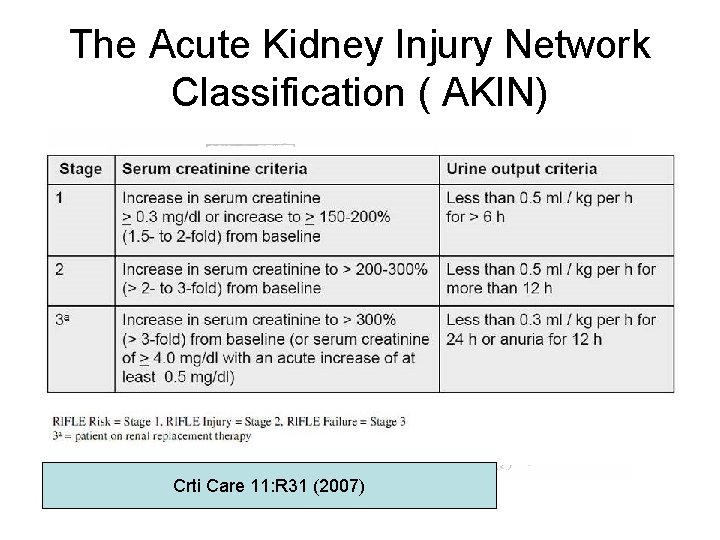
The Acute Kidney Injury Network Classification ( AKIN) Crti Care 11: R 31 (2007)