Reflective Clinical Journaling Using QSEN Competencies to Promote
- Slides: 10
Reflective Clinical Journaling: Using QSEN Competencies to Promote Student self-Awareness of Quality and Safety in Nursing Practice Kathleen S. Fries, Ph. D Assistant Professor & UG Director Sacred Heart University
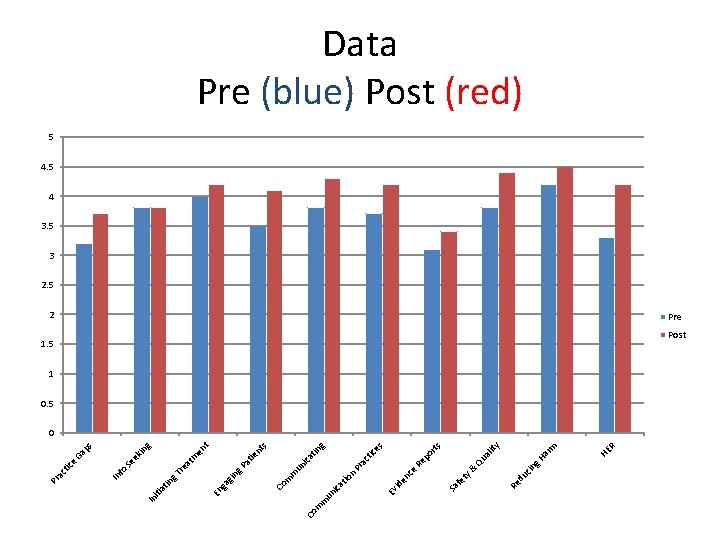
Objectives • Describe Journal Assignment as T-L strategy to implement IOM/QSEN + Essentials Competencies • Discuss Preliminary Research Findings to measure effectiveness of assignment (comparing pre-post means and qualitative data)
The Assignment Directions • Throughout the clinical rotation, you will be evaluated on your ability to demonstrate the knowledge, skills, and attitudes necessary to provide safe family centered care. The competencies outlined below will provide the framework to guide your clinical practice, post-conference dialogue, and journal entries that you will share with clinical supervisor on a weekly basis. • At the end of the semester, you will write about clinical experiences that clearly exemplify how you met each competency. • The paper will be typed and will include at least three outside references, along with textbook or journal articles used in class. • This is a reflective paper, and the use of “I” statements is expected as you describe how your actions met the competencies outlined below. As you write, think about how you might suggest changes in how you would function as a newly graduated RN….
The Assignment (con’t) • These clinical objectives are specifically identified to support the course objectives by using evidence based practice as per the recommendations by the “Quality and Safety Education for Nurses” (QSEN) Core Competencies. For more information, students are encouraged to visit http: //www. qsen. org/competencies. php
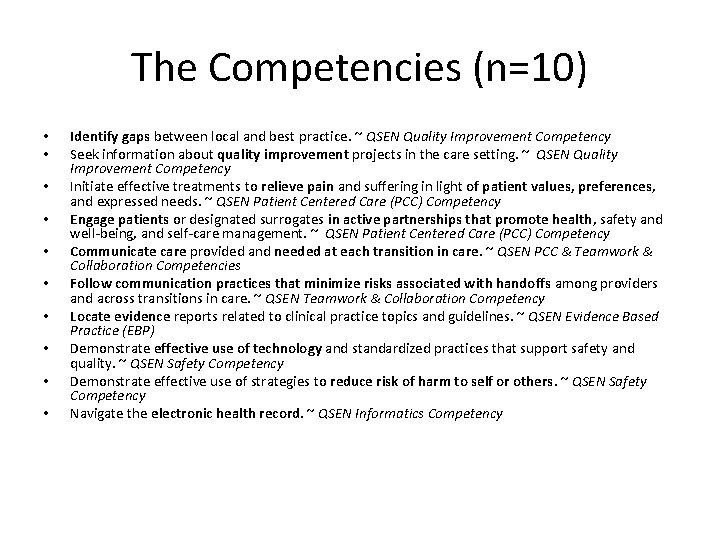
The Competencies (n=10) • • • Identify gaps between local and best practice. ~ QSEN Quality Improvement Competency Seek information about quality improvement projects in the care setting. ~ QSEN Quality Improvement Competency Initiate effective treatments to relieve pain and suffering in light of patient values, preferences, and expressed needs. ~ QSEN Patient Centered Care (PCC) Competency Engage patients or designated surrogates in active partnerships that promote health, safety and well-being, and self-care management. ~ QSEN Patient Centered Care (PCC) Competency Communicate care provided and needed at each transition in care. ~ QSEN PCC & Teamwork & Collaboration Competencies Follow communication practices that minimize risks associated with handoffs among providers and across transitions in care. ~ QSEN Teamwork & Collaboration Competency Locate evidence reports related to clinical practice topics and guidelines. ~ QSEN Evidence Based Practice (EBP) Demonstrate effective use of technology and standardized practices that support safety and quality. ~ QSEN Safety Competency Demonstrate effective use of strategies to reduce risk of harm to self or others. ~ QSEN Safety Competency Navigate the electronic health record. ~ QSEN Informatics Competency
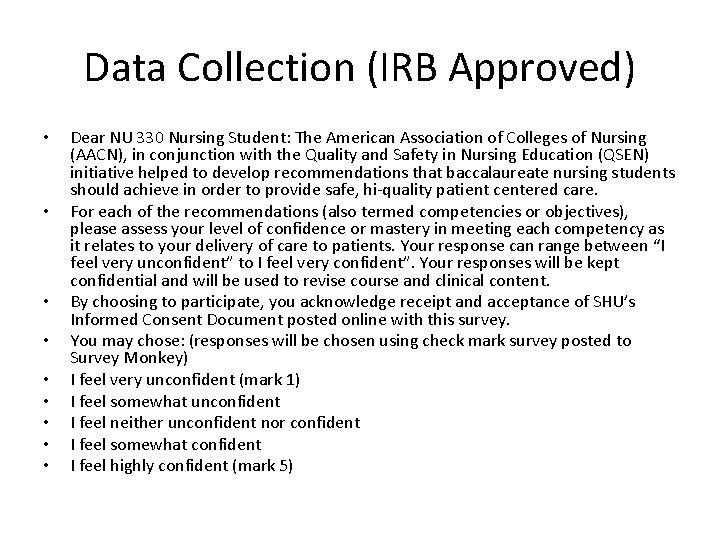
Data Collection (IRB Approved) • • • Dear NU 330 Nursing Student: The American Association of Colleges of Nursing (AACN), in conjunction with the Quality and Safety in Nursing Education (QSEN) initiative helped to develop recommendations that baccalaureate nursing students should achieve in order to provide safe, hi-quality patient centered care. For each of the recommendations (also termed competencies or objectives), please assess your level of confidence or mastery in meeting each competency as it relates to your delivery of care to patients. Your response can range between “I feel very unconfident” to I feel very confident”. Your responses will be kept confidential and will be used to revise course and clinical content. By choosing to participate, you acknowledge receipt and acceptance of SHU’s Informed Consent Document posted online with this survey. You may chose: (responses will be chosen using check mark survey posted to Survey Monkey) I feel very unconfident (mark 1) I feel somewhat unconfident I feel neither unconfident nor confident I feel somewhat confident I feel highly confident (mark 5)
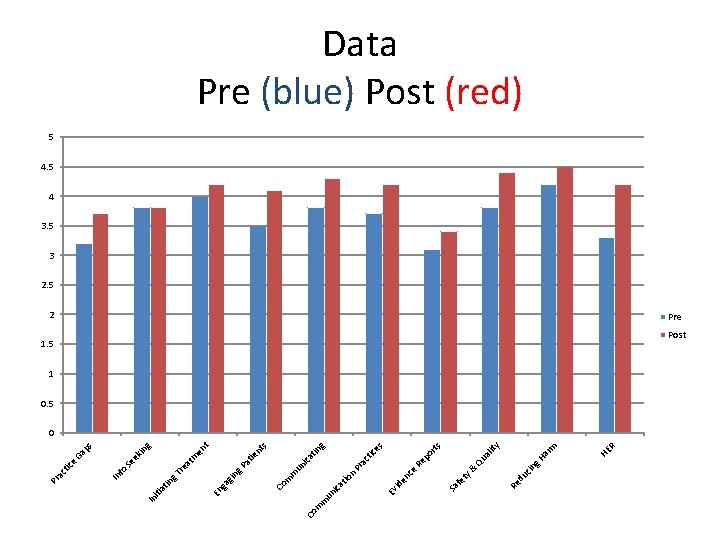
m m Co HE R m ar ity al Qu g. H cin y& du Re fe t Sa ts po r ac tic es Re Pr g tin ica s nt t en ie at un ce en id Ev n tio ica un m m Co g. P gin m at g in ps Ga ek Se g. T re in ga En at iti In fo In e tic ac Pr Data Pre (blue) Post (red) 5 4 3. 5 3 2. 5 2 Pre 1. 5 Post 1 0. 5 0
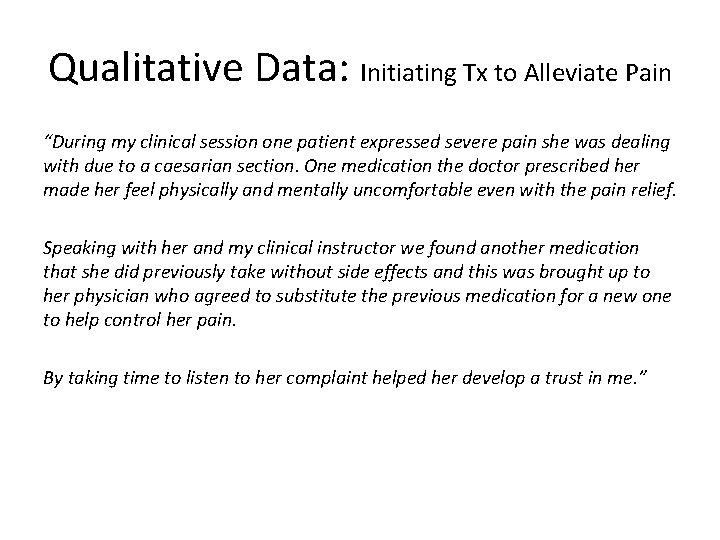
Qualitative Data: Initiating Tx to Alleviate Pain “During my clinical session one patient expressed severe pain she was dealing with due to a caesarian section. One medication the doctor prescribed her made her feel physically and mentally uncomfortable even with the pain relief. Speaking with her and my clinical instructor we found another medication that she did previously take without side effects and this was brought up to her physician who agreed to substitute the previous medication for a new one to help control her pain. By taking time to listen to her complaint helped her develop a trust in me. ”
Qualitative Data: Identifying Gaps in Practice “There were several local practices that differed from the practices we have learned in class or what is recommended. Many of the nurses draw up medications with one needle and administer it with a different needle. This local practice is different from how we were taught. We were taught to use a different needle only if you’re drawing up with a filter needle. If the medication can be drawn up with the same needle you administer it, then we would only use one. Also, one of my patients had a breech birth and when the baby was not wrapped in her blanket, her hips tended to push out to the sides. The parents were told to use two diapers to try and act as a brace to correct her hips, but many other nurses said that the double diapers does not scientifically correct this and a brace would be used later on. In the article ‘Hip, Leg, and Foot Abnormalities, ” Dr. Liptak discusses how many hip displacements occur from breech births and that padded diapers or double diapering is not effective and should not be done to correct this hip displacement. He suggests the Pavlik harness which holds the affected hips together and rotated externally (Liptak, 2010). ”
Summary & Recommendations • Continue to observe for changes in mean scores between pre-post assignment • Clinical Adjuncts report “awareness” re: IOM/QSEN/Essentials • Clinical “challenges” fostered healthy post-clinical discussion • Future assignments with increased focus re: student voice vs. reporting “I observed my nurse meeting QSEN competency when she…. . ” encourage increased citation to support position statements/clinical observations! • Other suggestions from AACN participants? • Questions/comments?