Referral Shared Care What is an AOD Referral






- Slides: 21
Referral & Shared Care

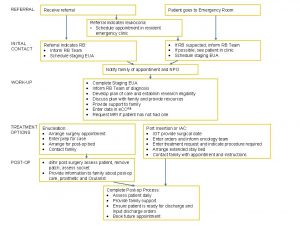
What is an AOD ‘Referral’? • ‘Usual’ referral practice tends to result in relinquishing principal care of a patient to another service. However, for people with AOD problems this frequently results in: – a high attrition rate following 1 st appointment – a high rate of ‘no shows’ – no guarantee of a good match between patient and the service – reluctance of the patient to return to place of initial contact. • The concept of ‘shared care’ has arisen in response to referral problems, and achieves more comprehensive, collaborative care for the patient. Referral & Shared Care
Who to Refer? • Refer any patient who may gain from treatments or services GPs may not be able or willing to provide • Key referrals may include patients with: – severe dependence and long history of psychoactive drug use – polydrug use – chaotic lifestyle with multiple problems – social isolation – legal problems – poor general life/coping skills – poor / lack of social supports. For the client, referral is a voluntary process – it should always involve the client Referral & Shared Care
Typical AOD Referral Options • • Sobering-up services / non-medical withdrawal Out-patient services for cognitive behavioural therapy In-patient withdrawal Pharmacotherapy services Specialist mental health services Residential care / therapeutic community Community-based services – self-help groups (as an adjunct to other treatments) – home-based withdrawal – counselling – youth / welfare / legal services. Referral & Shared Care
Refer When. . . • The patient requests referral • Ongoing contact is not conducive to the GP– patient relationship (and where it seems unlikely to improve) • When the GP is uncomfortable / unable to respond to the needs of the client • When the GP is unable to provide adequate time to ensure benefit from the interaction. Referral & Shared Care

Good Referral Practice (1) Identify and liaise with relevant AOD and welfare services in your area • What is their treatment philosophy? – abstinence, harm minimisation, eclectic approach • What generic or specialist services / treatments do they offer? – 12 -step, harm minimisation, pharmacotherapies, CBT • Do they have a specific orientation? – youth, Indigenous • What are their admission / entry criteria? Referral & Shared Care

Good Referral Practice (2) • Where possible (and with patient consent) provide comprehensive assessment (referral letter) to the new provider • High involvement in referral is associated with higher uptake and retention in treatment – arrange appointments for the patient, give instructions on how to get there – provide information to the patient about the service he or she has been referred to – build expectations of good outcomes – ask permission to call patient to ascertain outcome of referral. Referral & Shared Care
Good Referral Practice (3) • Follow-up to ensure connection occurred • Ensure referral is coordinated: – to prevent polypharmacy – to link other services into care • Establish ‘priority of need’ with patient to ensure success e. g. , ‘non-medical’ needs (e. g. , childcare, housing, food) may be a higher priority for referral than the immediate medical problem / AOD issue • Research suggests that practice nurses who are involved in AOD intervention and referral processes increase the likelihood of good outcomes. Referral & Shared Care

What is ‘Shared Care’? Shared care is: • multidisciplinary and multi-agency • includes prevention and treatment • fundamental to effective harm minimisation Respective roles have to be clearly defined, guidelines and protocols established and structures developed to sustain quality of delivery. Referral & Shared Care

‘Shared Care’ is About • Systemic Cooperation – how systems agree to work together • Operational Cooperation – cooperation at local levels between different groups of clinicians. Referral & Shared Care
“Shared care ensures that people who need ongoing services from GPs and other service providers receive the most effective combination of care. ” The concept of shared care extends beyond simple collaboration to: “… how the team, and functions of the team, are organised and sustained. ” Penrose-Wall et al. (2000, p. 6) Referral & Shared Care
The GP’s Role in Shared Care • Although AOD problems may be the primary presenting problem, they are more commonly detected when the patient presents for another issue • The role of the GP in shared care arrangements will depend on: – the GP’s specific skills, knowledge and abilities to intervene with AOD issues – the amount of time GPs are prepared to invest in responding to these issues – their decision to engage in a shared care relationship with other service providers – relationship and willingness to continue care with the patient. Referral & Shared Care
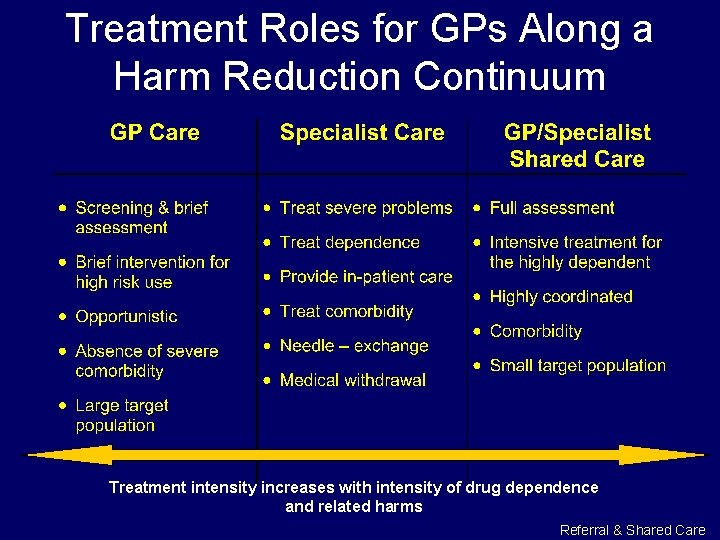
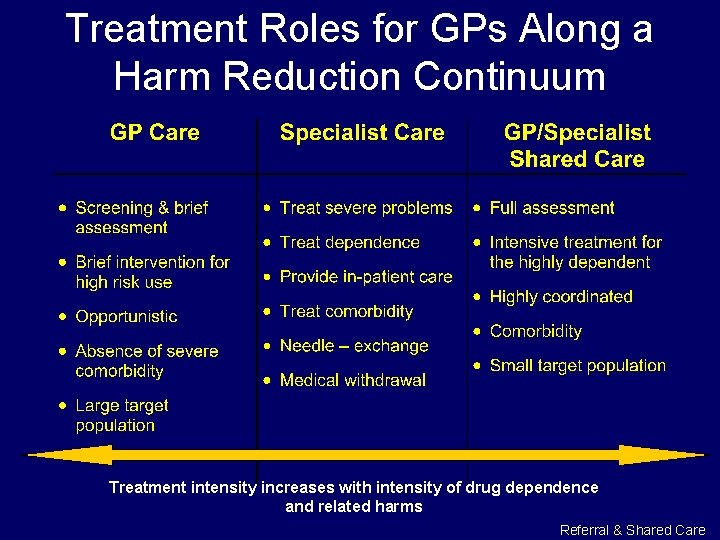
Treatment Roles for GPs Along a Harm Reduction Continuum Treatment intensity increases with intensity of drug dependence and related harms Referral & Shared Care

Illicit Drug Use Shared Care May Include: • Harm reduction and prevention of infectious diseases • Long-term, GP-centred, pharmacotherapy programs • Sharing pharmacotherapy management (e. g. , with specialist service) • Ambulatory withdrawal • Supporting user-led and peer outreach programs • Supporting Indigenous primary care agencies • Comorbidity shared management. Referral & Shared Care
Barriers to GP Involvement in Shared Care Evidence suggests that many GPs: • lack knowledge of illicit drug management • lack confidence to become involved • are concerned they will not receive adequate support from peers, colleagues or community • prefer not to be involved (e. g. , few GPs are involved in pharmacotherapy treatments) • accept they have a role in detection and referral of AOD problems but not treatment. Referral & Shared Care
Current GP Responses to Shared Care • A generational shift is apparent • Medical students are increasingly trained in AOD issues, so their knowledge and confidence to respond is increasing • AOD issues are increasingly accepted as a legitimate part of everyday general practice. Referral & Shared Care
How to Increase GP Involvement • Shared treatment roles increase with: – an increase in knowledge – attitudinal shift – higher confidence – skill attainment – belief in treatment efficacy – appropriate role fit for the GP’s practice • To ensure shared care works, develop protocols and arrange for back-up support. Referral & Shared Care
Successful Shared Care Programs Occur when: • GPs are involved from the outset in designing shared care programs & protocols • barriers to GP involvement are actively removed • GPs have broad preventive-treatment roles (but involvement is optional). Referral & Shared Care
Success Requires • Resources / training for GPs • Patient access to broader services direct from the surgery • A specialist drug unit to coordinate at the macro level – GP initiated programs can be innovative but are not easily sustained without this coordination. Referral & Shared Care
Australian Examples of Shared Care (1) • Mental health workers, specialist AOD services and pharmacists • Private psychiatrists and NGO support services (usually for comorbidity issues) • Primary prevention – attachment to schools, youth centres • GP-run youth health clinics addressing AOD issues within a broad health context. Referral & Shared Care
Australian Examples of Shared Care (2) • Prescribing methadone / pharmacotherapies • After-care services • Special populations (e. g. , prisoners) • Hep C screening and counselling. Referral & Shared Care
 What is aod
What is aod What is aod
What is aod Level of care primary secondary tertiary
Level of care primary secondary tertiary Types of referrals
Types of referrals 866-309-1719
866-309-1719 Shared goals of care
Shared goals of care Care certificate answers standard 3
Care certificate answers standard 3 Palliative care vs hospice care
Palliative care vs hospice care Hip fracture clinical care standard
Hip fracture clinical care standard Animale care nasc pui vii
Animale care nasc pui vii Health and social care values unit 2
Health and social care values unit 2 Care certificate duty of care
Care certificate duty of care Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate Magnetul este un corp care atrage
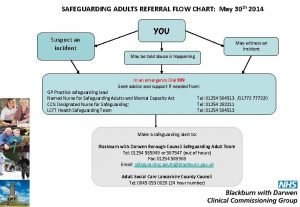
Magnetul este un corp care atrage Safeguarding referral flowchart
Safeguarding referral flowchart Elsa referral form
Elsa referral form Chicago central referral system
Chicago central referral system Targeted local hire program agency referral form
Targeted local hire program agency referral form Safeguarding adults hampshire
Safeguarding adults hampshire Fsp referral
Fsp referral Ktc thompson mb
Ktc thompson mb Suspected cancer recognition and referral
Suspected cancer recognition and referral