Referral Patterns for Gynecologic Oncology Consultation David I
- Slides: 1
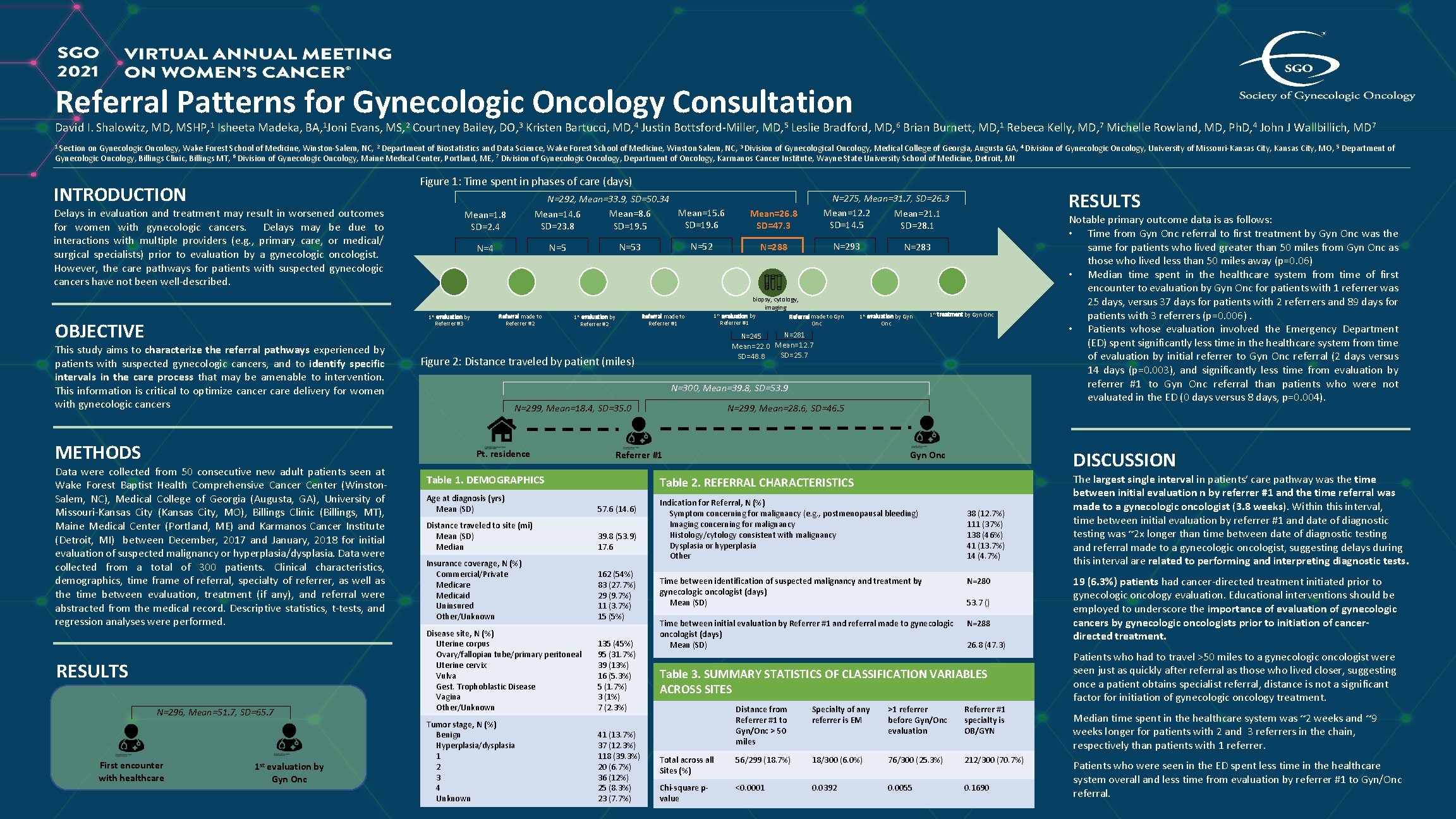
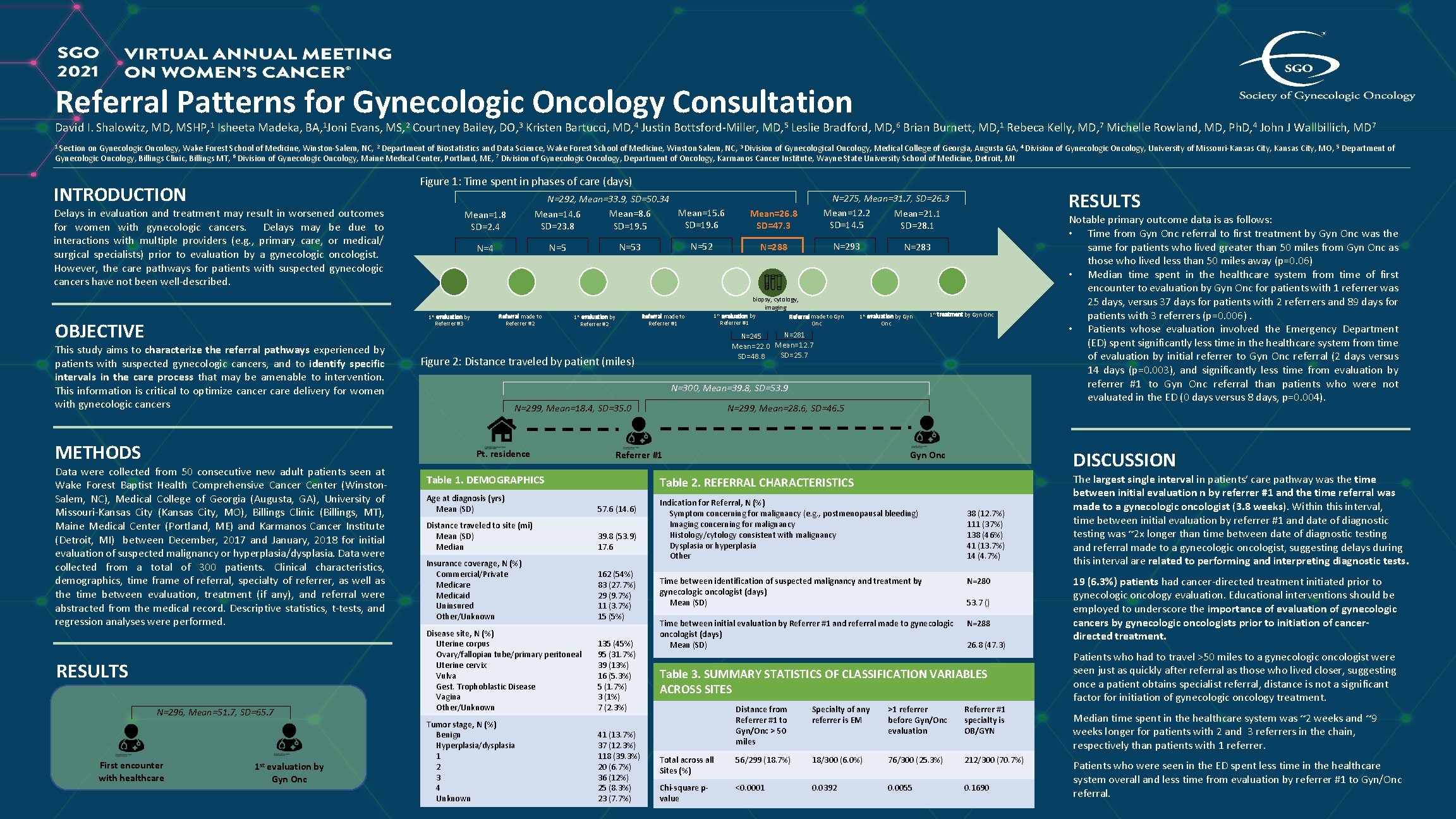
Referral Patterns for Gynecologic Oncology Consultation David I. Shalowitz, MD, MSHP, 1 Isheeta Madeka, BA, 1 Joni Evans, MS, 2 Courtney Bailey, DO, 3 Kristen Bartucci, MD, 4 Justin Bottsford-Miller, MD, 5 Leslie Bradford, MD, 6 Brian Burnett, MD, 1 Rebeca Kelly, MD, 7 Michelle Rowland, MD, Ph. D, 4 John J Wallbillich, MD 7 1 Section on Gynecologic Oncology, Wake Forest School of Medicine, Winston-Salem, NC, 2 Department of Biostatistics and Data Science, Wake Forest School of Medicine, Winston Salem, NC, 3 Division of Gynecological Oncology, Medical College of Georgia, Augusta GA, 4 Division of Gynecologic Oncology, University of Missouri-Kansas City, MO, 5 Department of Gynecologic Oncology, Billings Clinic, Billings MT, 6 Division of Gynecologic Oncology, Maine Medical Center, Portland, ME, 7 Division of Gynecologic Oncology, Department of Oncology, Karmanos Cancer Institute, Wayne State University School of Medicine, Detroit, MI Figure 1: Time spent in phases of care (days) INTRODUCTION Delays in evaluation and treatment may result in worsened outcomes for women with gynecologic cancers. Delays may be due to interactions with multiple providers (e. g. , primary care, or medical/ surgical specialists) prior to evaluation by a gynecologic oncologist. However, the care pathways for patients with suspected gynecologic cancers have not been well-described. N=292, Mean=33. 9, SD=50. 34 Mean=15. 6 Mean=8. 6 Mean=14. 6 SD=19. 5 SD=23. 8 Mean=1. 8 SD=2. 4 Mean=26. 8 SD=47. 3 N=52 N=53 N=5 N=4 N=293 N=288 N=283 biopsy, cytology, imaging 1 st evaluation by Referrer #3 OBJECTIVE Referral made to Referrer #2 1 st evaluation by Referrer #2 Referral made to Referrer #1 1 st evaluation by Referrer #1 N=245 This study aims to characterize the referral pathways experienced by patients with suspected gynecologic cancers, and to identify specific intervals in the care process that may be amenable to intervention. This information is critical to optimize cancer care delivery for women with gynecologic cancers METHODS RESULTS N=296, Mean=51. 7, SD=65. 7 First encounter with healthcare 1 st evaluation by Gyn Onc Referral made to Gyn Onc 1 st evaluation by Gyn Onc 1 st treatment by Gyn Onc N=281 Mean=22. 0 Mean=12. 7 SD=25. 7 SD=48. 8 Figure 2: Distance traveled by patient (miles) N=300, Mean=39. 8, SD=53. 9 N=299, Mean=28. 6, SD=46. 5 N=299, Mean=18. 4, SD=35. 0 Pt. residence Data were collected from 50 consecutive new adult patients seen at Wake Forest Baptist Health Comprehensive Cancer Center (Winston. Salem, NC), Medical College of Georgia (Augusta, GA), University of Missouri-Kansas City (Kansas City, MO), Billings Clinic (Billings, MT), Maine Medical Center (Portland, ME) and Karmanos Cancer Institute (Detroit, MI) between December, 2017 and January, 2018 for initial evaluation of suspected malignancy or hyperplasia/dysplasia. Data were collected from a total of 300 patients. Clinical characteristics, demographics, time frame of referral, specialty of referrer, as well as the time between evaluation, treatment (if any), and referral were abstracted from the medical record. Descriptive statistics, t-tests, and regression analyses were performed. RESULTS N=275, Mean=31. 7, SD=26. 3 Mean=12. 2 Mean=21. 1 SD=14. 5 SD=28. 1 Referrer #1 Table 1. DEMOGRAPHICS DISCUSSION Gyn Onc Table 2. REFERRAL CHARACTERISTICS Age at diagnosis (yrs) Mean (SD) 57. 6 (14. 6) Distance traveled to site (mi) Mean (SD) Median 39. 8 (53. 9) 17. 6 Insurance coverage, N (%) Commercial/Private Medicare Medicaid Uninsured Other/Unknown 162 (54%) 83 (27. 7%) 29 (9. 7%) 11 (3. 7%) 15 (5%) Disease site, N (%) Uterine corpus Ovary/fallopian tube/primary peritoneal Uterine cervix Vulva Gest. Trophoblastic Disease Vagina Other/Unknown 135 (45%) 95 (31. 7%) 39 (13%) 16 (5. 3%) 5 (1. 7%) 3 (1%) 7 (2. 3%) Tumor stage, N (%) Benign Hyperplasia/dysplasia 1 2 3 4 Unknown 41 (13. 7%) 37 (12. 3%) 118 (39. 3%) 20 (6. 7%) 36 (12%) 25 (8. 3%) 23 (7. 7%) Indication for Referral, N (%) Symptom concerning for malignancy (e. g. , postmenopausal bleeding) Imaging concerning for malignancy Histology/cytology consistent with malignancy Dysplasia or hyperplasia Other Notable primary outcome data is as follows: • Time from Gyn Onc referral to first treatment by Gyn Onc was the same for patients who lived greater than 50 miles from Gyn Onc as those who lived less than 50 miles away (p=0. 06) • Median time spent in the healthcare system from time of first encounter to evaluation by Gyn Onc for patients with 1 referrer was 25 days, versus 37 days for patients with 2 referrers and 89 days for patients with 3 referrers (p=0. 006). • Patients whose evaluation involved the Emergency Department (ED) spent significantly less time in the healthcare system from time of evaluation by initial referrer to Gyn Onc referral (2 days versus 14 days (p=0. 003), and significantly less time from evaluation by referrer #1 to Gyn Onc referral than patients who were not evaluated in the ED (0 days versus 8 days, p=0. 004). 38 (12. 7%) 111 (37%) 138 (46%) 41 (13. 7%) 14 (4. 7%) Time between identification of suspected malignancy and treatment by gynecologic oncologist (days) Mean (SD) N=280 Time between initial evaluation by Referrer #1 and referral made to gynecologic oncologist (days) Mean (SD) N=288 53. 7 () 26. 8 (47. 3) Table 3. SUMMARY STATISTICS OF CLASSIFICATION VARIABLES ACROSS SITES Distance from Referrer #1 to Gyn/Onc > 50 miles Specialty of any referrer is EM >1 referrer before Gyn/Onc evaluation Referrer #1 specialty is OB/GYN Total across all Sites (%) 56/299 (18. 7%) 18/300 (6. 0%) 76/300 (25. 3%) 212/300 (70. 7%) Chi-square pvalue <0. 0001 0. 0392 0. 0055 0. 1690 The largest single interval in patients’ care pathway was the time between initial evaluation n by referrer #1 and the time referral was made to a gynecologic oncologist (3. 8 weeks). Within this interval, time between initial evaluation by referrer #1 and date of diagnostic testing was ~2 x longer than time between date of diagnostic testing and referral made to a gynecologic oncologist, suggesting delays during this interval are related to performing and interpreting diagnostic tests. 19 (6. 3%) patients had cancer-directed treatment initiated prior to gynecologic oncology evaluation. Educational interventions should be employed to underscore the importance of evaluation of gynecologic cancers by gynecologic oncologists prior to initiation of cancerdirected treatment. Patients who had to travel >50 miles to a gynecologic oncologist were seen just as quickly after referral as those who lived closer, suggesting once a patient obtains specialist referral, distance is not a significant factor for initiation of gynecologic oncology treatment. Median time spent in the healthcare system was ~2 weeks and ~9 weeks longer for patients with 2 and 3 referrers in the chain, respectively than patients with 1 referrer. Patients who were seen in the ED spent less time in the healthcare system overall and less time from evaluation by referrer #1 to Gyn/Onc referral.