References Huff coughing technique Sit up straight with
- Slides: 2
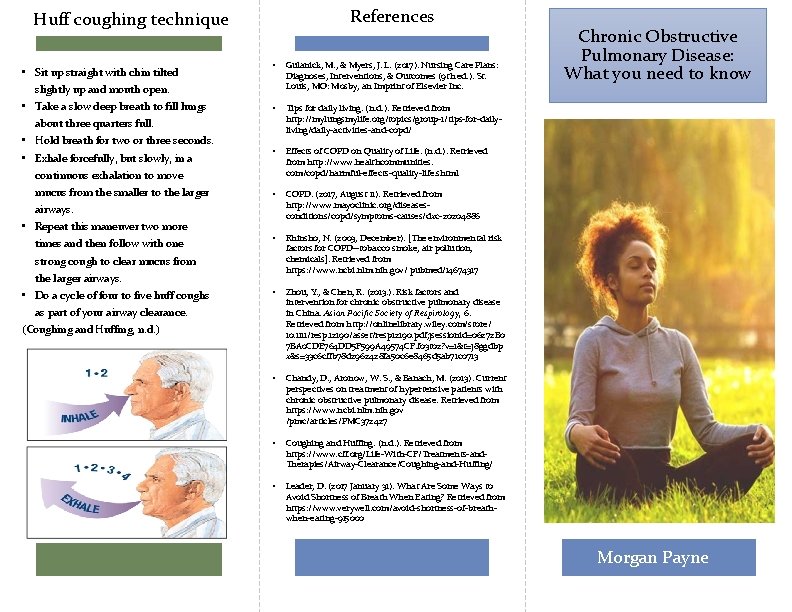
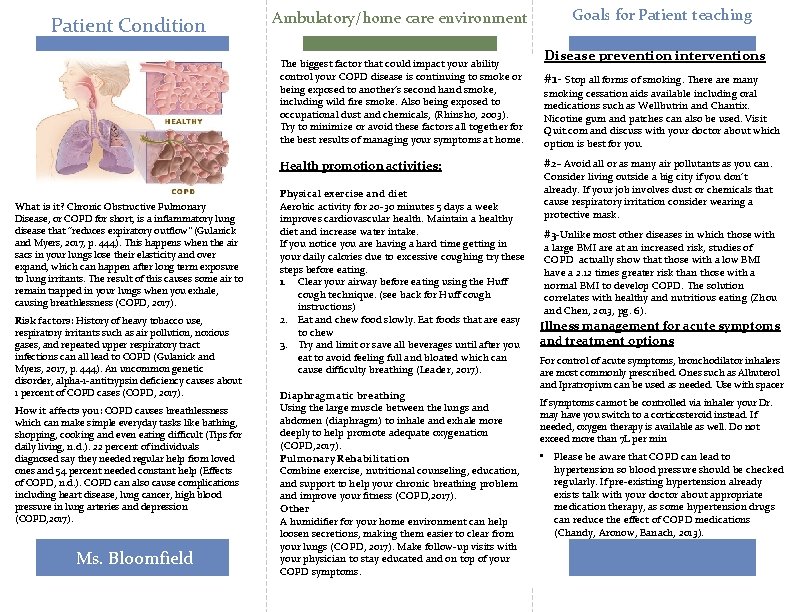
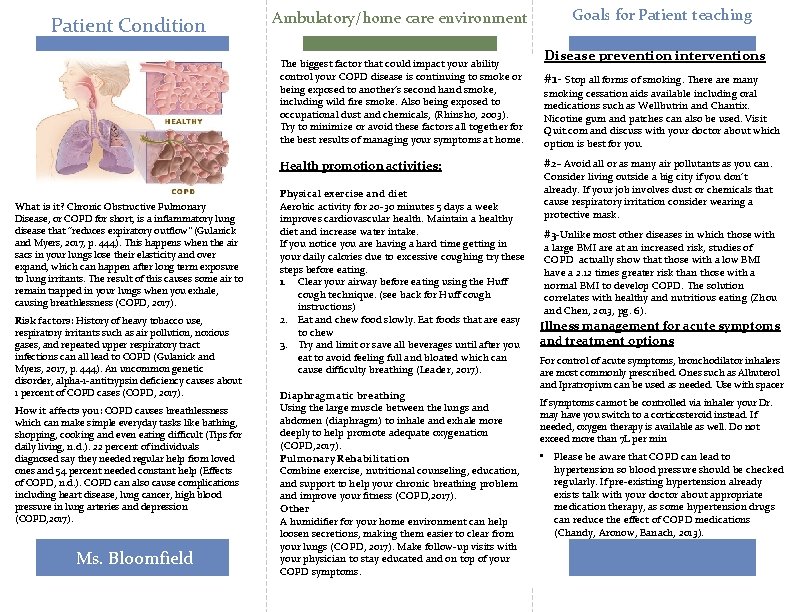
References Huff coughing technique • Sit up straight with chin tilted slightly up and mouth open. • Take a slow deep breath to fill lungs about three quarters full. • Hold breath for two or three seconds. • Exhale forcefully, but slowly, in a continuous exhalation to move mucus from the smaller to the larger airways. • Repeat this maneuver two more times and then follow with one strong cough to clear mucus from the larger airways. • Do a cycle of four to five huff coughs as part of your airway clearance. (Coughing and Huffing, n. d. ) • Gulanick, M. , & Myers, J. L. (2017). Nursing Care Plans: Diagnoses, Interventions, & Outcomes (9 th ed. ). St. Louis, MO: Mosby, an Imprint of Elsevier Inc. • Tips for daily living. (n. d. ). Retrieved from http: //mylungsmylife. org/topics/group-1/tips-for-dailyliving/daily-activities-and-copd/ • Effects of COPD on Quality of Life. (n. d. ). Retrieved from http: //www. healthcommunities. com/copd/harmful-effects-quality-life. shtml • COPD. (2017, August 11). Retrieved from http: //www. mayoclinic. org/diseasesconditions/copd/symptoms-causes/dxc-20204886 • Rhinsho, N. (2003, December). [The environmental risk factors for COPD--tobacco smoke, air pollution, chemicals]. Retrieved from https: //www. ncbi. nlm. nih. gov/ pubmed/14674317 • Zhou, Y. , & Chen, R. (2013. ). Risk factors and intervention for chronic obstructive pulmonary disease in China. Asian Pacific Society of Respirology, 6. Retrieved from http: //onlinelibrary. wiley. com/store/ 10. 1111/resp. 12190/asset/resp 12190. pdf; jsessionid=06272 B 0 7 BA 0 CDE 764 DD 5 F 599 A 49574 CF. f 03 t 02? v=1&t=j 8 ggdbp x&s=33 c 6 cffb 78 d 2962428 fa 50 c 6 e 8465 d 5 ab 71 c 0713 • Chandy, D. , Aronow, W. S. , & Banach, M. (2013). Current perspectives on treatment of hypertensive patients with chronic obstructive pulmonary disease. Retrieved from https: //www. ncbi. nlm. nih. gov /pmc/articles/PMC 372427 • Coughing and Huffing. (n. d. ). Retrieved from https: //www. cff. org/Life-With-CF/Treatments-and. Therapies/Airway-Clearance/Coughing-and-Huffing/ • Leader, D. (2017 January 31). What Are Some Ways to Avoid Shortness of Breath When Eating? Retrieved from https: //www. verywell. com/avoid-shortness-of-breathwhen-eating-915000 Chronic Obstructive Pulmonary Disease: What you need to know Morgan Payne
Patient Condition Ambulatory/home care environment The biggest factor that could impact your ability control your COPD disease is continuing to smoke or being exposed to another’s second hand smoke, including wild fire smoke. Also being exposed to occupational dust and chemicals, (Rhinsho, 2003). Try to minimize or avoid these factors all together for the best results of managing your symptoms at home. Health promotion activities: What is it? Chronic Obstructive Pulmonary Disease, or COPD for short, is a inflammatory lung disease that “reduces expiratory outflow” (Gulanick and Myers, 2017, p. 444). This happens when the air sacs in your lungs lose their elasticity and over expand, which can happen after long term exposure to lung irritants. The result of this causes some air to remain trapped in your lungs when you exhale, causing breathlessness (COPD, 2017). Risk factors: History of heavy tobacco use, respiratory irritants such as air pollution, noxious gases, and repeated upper respiratory tract infections can all lead to COPD (Gulanick and Myers, 2017, p. 444). An uncommon genetic disorder, alpha-1 -antitrypsin deficiency causes about 1 percent of COPD cases (COPD, 2017). How it affects you: COPD causes breathlessness which can make simple everyday tasks like bathing, shopping, cooking and even eating difficult (Tips for daily living, n. d. ). 22 percent of individuals diagnosed say they needed regular help from loved ones and 54 percent needed constant help (Effects of COPD, n. d. ). COPD can also cause complications including heart disease, lung cancer, high blood pressure in lung arteries and depression (COPD, 2017). Ms. Bloomfield Physical exercise and diet Aerobic activity for 20 -30 minutes 5 days a week improves cardiovascular health. Maintain a healthy diet and increase water intake. If you notice you are having a hard time getting in your daily calories due to excessive coughing try these steps before eating. 1. Clear your airway before eating using the Huff cough technique. (see back for Huff cough instructions) 2. Eat and chew food slowly. Eat foods that are easy to chew 3. Try and limit or save all beverages until after you eat to avoid feeling full and bloated which can cause difficulty breathing (Leader, 2017). Diaphragmatic breathing Using the large muscle between the lungs and abdomen (diaphragm) to inhale and exhale more deeply to help promote adequate oxygenation (COPD, 2017). Pulmonary Rehabilitation Combine exercise, nutritional counseling, education, and support to help your chronic breathing problem and improve your fitness (COPD, 2017). Other A humidifier for your home environment can help loosen secretions, making them easier to clear from your lungs (COPD, 2017). Make follow-up visits with your physician to stay educated and on top of your COPD symptoms. Goals for Patient teaching Disease prevention interventions #1 - Stop all forms of smoking. There are many smoking cessation aids available including oral medications such as Wellbutrin and Chantix. Nicotine gum and patches can also be used. Visit Quit. com and discuss with your doctor about which option is best for you. #2 - Avoid all or as many air pollutants as you can. Consider living outside a big city if you don’t already. If your job involves dust or chemicals that cause respiratory irritation consider wearing a protective mask. #3 -Unlike most other diseases in which those with a large BMI are at an increased risk, studies of COPD actually show that those with a low BMI have a 2. 12 times greater risk than those with a normal BMI to develop COPD. The solution correlates with healthy and nutritious eating (Zhou and Chen, 2013, pg. 6). Illness management for acute symptoms and treatment options For control of acute symptoms, bronchodilator inhalers are most commonly prescribed. Ones such as Albuterol and Ipratropium can be used as needed. Use with spacer If symptoms cannot be controlled via inhaler your Dr. may have you switch to a corticosteroid instead. If needed, oxygen therapy is available as well. Do not exceed more than 7 L per min • Please be aware that COPD can lead to hypertension so blood pressure should be checked regularly. If pre-existing hypertension already exists talk with your doctor about appropriate medication therapy, as some hypertension drugs can reduce the effect of COPD medications (Chandy, Aronow, Banach, 2013).